Abstract
Objective
To evaluate concurrent and longitudinal associations between psychosocial functioning and physical activity in adolescent and young adult survivors of early childhood cancer.
Methods
Adolescent survivors of early childhood cancer (diagnosed before age four) participating in the Childhood Cancer Survivor Study completed the Coping Health and Illness Profile–Adolescent Edition (CHIP-AE; n=303; mean age at survey 17.6 years). A subset of these survivors (n=248) completed a follow-up survey an average of 6.0 years later (range: 4–10). Logistic regression identified associations between psychosocial functioning in adolescence and physical activity levels in adolescence and young adulthood.
Results
Survivors reported low physical activity as adolescents (46.1% scored below CHIP-AE cut-point) and young adults (40.8% below CDC guidelines). Poor physical activity during adolescence was associated with female sex (OR=2.06, 95%CI=1.18–3.68), parents with less than a college education (OR=1.91, 95%CI 1.11–3.32), previous treatment with cranial radiation (OR=3.35, 95%CI=1.69–6.88), TV time (OR=1.77, 95%CI=1.00–3.14), and limitations of activity due to health or mobility restrictions (OR=8.28, 95%CI=2.87–30.34). Poor diet (OR=1.84, 95%CI=1.05–3.26) and low self-esteem (OR=1.80, 95%CI=0.99–3.31) during adolescence were associated with lower odds of meeting CDC physical activity guidelines in young adulthood.
Conclusion
These findings provide targets for future interventional studies to improve physical activity in this high-risk population.
Keywords: physical activity, psychological functioning, childhood cancer, survivors
Background
Improvements in treatment for childhood cancer over the past decades have led to improvements in five-year survival rates and late mortality among survivors.1,2 Maximizing quality of life and minimizing late-effects after cancer therapy are central in promoting long-term health and development among survivors. Previous research has shown some childhood cancer survivors are at risk for poor physical fitness and physical inactivity.3–7 This is important as poor physical activity is a recognized risk factor for numerous health problems, including cardiovascular disease and osteoporosis in the general population,8,9 and may exacerbate late-effects of treatment among childhood cancer survivors.10 Reports from the Childhood Cancer Survivor Study (CCSS) cohort demonstrate high rates of insufficient activity among adult survivors of childhood cancer (42–72% in different subgroups).11–13 Factors associated with inactivity among adult survivors of childhood cancer include female sex, black race, older age at study, lower educational attainment, higher body mass index, smoking, depression, diagnosis of medulloblastoma or osteosarcoma, and treatment with cranial radiation or amputation.14
Very few studies have examined correlates of physical activity in adolescent survivors of childhood cancer. Family and peer support for physical activity are associated with higher survivor-reported physical activity during adolescence.15 Adolescent survivors of childhood cancer who report higher self-esteem are more physically active during and after treatment.16 Higher physical activity has been associated with better health-related quality of life and lower cancer worry among this group.17 However, there remains a gap in understanding whether and how adolescent characteristics influence adult physical activity levels among childhood cancer survivors. This understanding can inform development of targeted interventions to improve activity and health in long-term survivors of childhood cancer. Given that vigorous exercise is associated with lower risk of cardiovascular events, independent of treatment-related factors, in adult survivors of childhood cancer,18 early intervention is warranted. Focusing on adolescence may be particularly powerful, as health behaviors acquired during this time are likely carried into adulthood,7,19 yet intervening during the time of transition from adolescence to young adulthood can be challenging. The findings from this study will in part lay the foundation for identifying targets for intervention among this group of childhood cancer survivors.
The goals of this study were to identify factors associated with physical activity in adolescent survivors of childhood cancer and to examine longitudinal associations between adolescent factors (psychosocial, family involvement, behavioral) and future physical activity in young adulthood. Using the CCSS cohort we focused on survivors of early childhood cancers (diagnosed ages 0 to 3), who, because of their young age at treatment, are at higher risk for late-effects and mortality.20–22 Additionally, these survivors underwent treatment prior to the development of leisure-time activity patterns. Factors associated with concurrent and future physical activity among siblings of survivors were also examined.
Methods
Participants
The CCSS is a large, multi-institutional cohort study of long-term survivors of childhood cancer (IRB# FWA00004775). The original CCSS cohort consisted of 14,357 individuals diagnosed 1970–1986 who were under 21 years of age at diagnosis and five or more years post-diagnosis at recruitment.23,24 Eligible diagnoses included leukemia, CNS malignancies, Hodgkin lymphoma, non-Hodgkin lymphoma, kidney tumor, neuroblastoma, soft tissue sarcoma, or bone cancer. The current study examined data from a subset of CCSS participants who completed the Teen Health Survey, administered as an ancillary study between 2001 and 2003.25 Any survivor aged 15–19 years who had been diagnosed prior to age 4 and had parental permission to contact was mailed a survey. Any sibling age 15–19 with parental permission to contact was mailed a survey. Surveys were mailed to 444 survivors; 307 (69%) responded, and the final sample was 303 (see Mertens et al. for more details25). For longitudinal analyses examining physical activity during young adulthood, only survivors who completed the Teen Health Survey and the CCSS Follow-up 4 questionnaire, administered 2007–11, were included (n=248, 81.8%). Average time between surveys was 6.0 years (range 4.6–7.9). Siblings who completed the Teen Health Survey (n=96) and those who completed both the Teen Health Survey and Follow-up 4 (n=73) were included to evaluate similarity of models between groups. Average time between surveys for siblings was 6.5 years (range 5.4–8.0). Given the small sibling sample size and that treatment variables were not applicable for siblings, we did not run multivariable models evaluating survivor status (survivor vs. sibling) as a predictor.
Measures
The Teen Health Survey consisted of the Child Health and Illness Profile-Adolescent Edition (CHIP-AE26,27), a self-report survey designed to evaluate health and quality of life. The CHIP-AE yields six health domains (satisfaction with health, resilience, physical and emotional discomfort, risk behaviors, school and work achievements, and health disorders). Within these broad domains, 20 subdomains representing scales/indices of satisfaction and health-protective or risky behaviors can be scored. Each subdomain is standardized to a mean of 20 and standard deviation of 5.27 Higher scores indicate better functioning, and cut-points of 0.6 SD above/below the mean are used to categorize health as poor (<17), average (17–23), or excellent (>23).27,28 Validity and reliability of the CHIP-AE have been demonstrated in large studies of ethnically and racially diverse urban and rural youth.29 Validity has been supported through demonstrations of differences in outcomes between adolescents with and without chronic health conditions.28,30 Reliability was demonstrated by acceptable Cronbach’s alphas (>.70) for all scales across multiple samples and adequate test-rest intraclass correlations (>.60) for indices of behaviors like physical activity.29 In this study, only the physical activity index and subdomains hypothesized to be relevant to physical activity were analyzed (i.e., self-esteem, emotional discomfort, family involvement, and items from the home and health safety index about TV/video time and dietary intake behaviors).
Demographic/Medical predictors
Demographic variables (age, sex, race, and parental education, used as a proxy for socioeconomic status) were obtained from the CHIP-AE. Medical treatment information, including diagnosis, age at diagnosis, and chemotherapy and cranial radiation, were abstracted from medical records for participants with a signed medical release.23 For analytic purposes, receipt of chemotherapy, radiation, and cranial radiation were dichotomized as yes/no.
Psychological predictors
Adolescent psychological predictors included two subdomains from the CHIP-AE. Self-esteem is the average of five items of self-concept and satisfaction with self (e.g., “I have a lot of good qualities”) using a four-point scale from do not agree to completely agree. Emotional discomfort is a 14-item scale of frequency of emotional feelings and symptoms (e.g., days depressed or nervous in the past four weeks, with response options on a 5-point scale from 15–28 days to no days).
Family predictors
The seven-item family involvement CHIP-AE subdomain measured adolescents’ reports of family activities and family support (e.g., “days family spent time with you” from 15–28 days to no days and “there is an adult you could turn to for help if you have a real problem” with yes or no response options).
Behavioral predictors
Adolescent TV time and limitations of activity
Time spent watching TV or videos, a proxy for sedentary time, was measured using the CHIP-AE item “the amount of time spent watching TV/videos on an average school day in the past four weeks,” with responses ranging from none to 4 or more hours. We dichotomized this variable into 0–2 hours or 3 or more hours based on the American Academy of Pediatrics recommendation.31 The seven-item CHIP-AE limitations of activity subdomain was used to assess restrictions in attending school or completing activities of daily living due to health problems (e.g., “days missed school” with five-point response option from 15–28 days to no days).
Adolescent diet behavior
Intake of healthy and unhealthy foods was derived as recommended in the CHIP-AE manual27 using items from the home safety and health index. Healthy diet behaviors were averaged from four items measuring the frequency of fruit/vegetable, lean meat, lowfat dairy, and whole grain intake within the past four weeks, on a five-point scale ranging from rarely or never to more than once a day. Unhealthy diet behaviors were averaged across three items measuring fast food, salty food, and sweets eaten within the past four weeks, responses ranging from 1=rarely or never to 5=more than once a day. We dichotomized healthy and unhealthy diet behaviors into average or excellent (>3 for healthy, ≤3 for unhealthy) or poor (≤3 for healthy, >3 for unhealthy) categories.
Physical activity outcomes
Adolescent physical activity
The self-reported physical activity index of the CHIP-AE is the average score across four items about activity during the past four weeks (i.e., number of days exercised for 20 minutes or more, number of sit-ups, distance walked without resting or getting tired, and distance ran) and one item about frequency of sports team involvement in the past year (never, once or twice, several times). Per the manual,27 standard scores were used and we dichotomized the primary outcome as poor (score <17) vs. average/excellent (score ≥17).
Young adult physical activity
Young adults reported the number of days per week and minutes per day they completed vigorous (e.g., running) and moderate physical activities (e.g., brisk walking) using six items in Follow-up 4. Total minutes were used to determine if young adults met Centers for Disease Control (CDC) established recommendations for physical activity (i.e., ≥150 weekly minutes of moderate or ≥75 weekly minutes of vigorous aerobic activity).
Statistical analyses
Descriptive statistics were calculated for survivor and sibling characteristics. Bivariate associations between predictors, covariates (i.e., demographic and medical factors), and outcomes (either adolescent or young adult physical activity) were examined (Supplemental Table 1). Variables that were significantly associated with these outcomes in univariate logistic regression analyses or variables that were determined a priori to be important (e.g., sex), were included in the preliminary multivariable logistic regression models; subsets of these candidate variables were selected for final models by assessing goodness of fit and parsimony using Akaike Information Criterion (AIC). Multivariable logistic regression models were generated to evaluate associations between demographic/medical, psychological, family, and behavioral factors and: (1) adolescent physical activity (poor versus average/excellent), and (2) young adult physical activity at follow-up (did not meet versus met CDC recommendations). Odds ratios (OR), 95% confidence intervals (CIs), and two-sided p values are reported. Impairment on predictors and outcomes were compared between survivors and siblings, and then separate models were run to compare the impact of predictors on outcomes for survivors and siblings. The multivariable logistic regression sibling analyses were conducted to provide a comparison population when evaluating non-medical predictors and physical activity outcomes, and the size of the odds ratios can be compared to the survivors. These sibling results are reported in supplemental tables. All analyses were run in SAS 9.4 (SAS Institute, Cary NC).
Results
Participant characteristics
Survivor and sibling demographic and treatment characteristics are provided in Table 1. Mean (SD) age of survivor diagnosis was 1.5 (1.0) years. Survivors were 17.6 (1.1) years at the Teen Health Survey and 23.6 (1.1) years at Follow-up 4; siblings were 16.9 (1.4) years at the Teen Health Study and 23.6 (1.3) years at Follow-up 4. Siblings were younger than survivors at the Teen Health Survey (p<0.001). There were no significant differences between survivors who completed both surveys and those who completed only the Teen Health Survey with two exceptions – a greater percentage of survivors who completed only the Teen survey received chemotherapy (92.5% vs. 79.3%, p=0.03) and reported poor physical activity (63% vs. 42%, p=0.005).
Table 1.
Demographic and treatment characteristics of survivors and siblings who completed Teen Health and Follow-Up4 Surveys
| Survivors completing Teen Health Survey (n=303) |
Survivors completing Teen Health & Follow-Up4 Surveys (n=248) |
Siblings completing Teen Health Survey (n=96) |
Siblings completing Teen Health Survey & Follow-Up4 Surveys (n=73) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| n | % | n | % | pa | n | % | n | % | pb | pc | |
| Sex | 1.00 | 0.02 | 0.37 | ||||||||
| Female | 183 | 60.4 | 147 | 60.2 | 53 | 55.2 | 45 | 61.6 | |||
| Male | 120 | 39.6 | 97 | 39.1 | 43 | 44.8 | 28 | 38.4 | |||
| Age at Survey (yrs) | 0.09 | 0.19 | <0.0001 | ||||||||
| 14 | 0 | 0.0 | 0 | 0.0 | 3 | 3.1 | 1 | 1.4 | |||
| 15 | 12 | 4.0 | 9 | 3.7 | 15 | 15.6 | 10 | 13.7 | |||
| 16 | 36 | 11.9 | 33 | 13.5 | 21 | 21.9 | 17 | 23.3 | |||
| 17 | 81 | 26.7 | 65 | 26.6 | 19 | 19.8 | 14 | 19.2 | |||
| 18 | 106 | 35.0 | 89 | 36.4 | 21 | 21.9 | 15 | 20.5 | |||
| 19 | 68 | 22.4 | 48 | 19.7 | 17 | 17.7 | 16 | 21.9 | |||
| Race/Ethnicity | 0.89 | 0.49 | 0.57 | ||||||||
| White | 267 | 88.4 | 215 | 88.5 | 85 | 90.4 | 66 | 91.7 | |||
| Black | 9 | 3.0 | 7 | 2.9 | 3 | 3.2 | 2 | 2.8 | |||
| Hispanic | 9 | 3.0 | 8 | 3.3 | 2 | 2.1 | 2 | 2.8 | |||
| Other race | 17 | 5.6 | 13 | 5.3 | 4 | 4.3 | 2 | 2.8 | |||
| Diagnosis | 0.67 | — | — | ||||||||
| Leukemia | 94 | 31.0 | 72 | 29.5 | — | — | — | — | |||
| CNS tumor | 40 | 13.2 | 35 | 14.3 | — | — | — | — | |||
| NHL | 4 | 1.3 | 3 | 1.2 | — | — | — | — | |||
| Wilms tumor | 56 | 18.5 | 46 | 18.9 | — | — | — | — | |||
| Neuroblastoma | 89 | 29.4 | 71 | 29.1 | — | — | — | — | |||
| Soft tissue sarcoma | 17 | 5.6 | 15 | 6.1 | — | — | — | — | |||
| Bone tumor | 3 | 1.0 | 2 | 1.0 | — | — | — | — | |||
| Age at Diagnosis (yrs) | 0.65 | — | — | ||||||||
| 0–1 | 194 | 64.0 | 158 | 64.8 | — | — | — | — | |||
| 2–3 | 109 | 36.0 | 86 | 35.2 | — | — | — | — | |||
| Years Since Diagnosis M(SD) | 16.0 (1.1) | 16.0 | (1.1) | 0.45 | — | — | — | — | — | — | |
| Chemotherapy | 0.03 | — | — | ||||||||
| Yes | 240 | 79.2 | 191 | 78.3 | — | — | — | — | |||
| No | 54 | 17.8 | 50 | 20.5 | — | — | — | — | |||
| Cranial Radiation | 0.35 | — | — | ||||||||
| Yes | 61 | 20.1 | 47 | 19.3 | — | — | — | — | |||
| No | 229 | 75.6 | 190 | 77.9 | — | — | — | — | |||
Note. NHL=Non-Hodgkin’s Lymphoma. Comparisons between groups were made using Fisher’s exact test (2×2 tables), chi-square (other categorical variables) and t-tests (continuous variables).
Comparison of survivors completing both surveys vs. only Teen Health Survey;
Comparison of siblings completing both surveys vs. only Teen Health Survey;
Comparison of survivors completing Teen Health Survey vs. siblings completing Teen Health Survey.
Adolescent Predictors and Physical Activity
Descriptive statistics for adolescent predictors and odds of poor outcomes (Supplemental Table 2) showed no significant differences between survivors and siblings except for a trend for lower frequency of healthy foods in diet, such as fruits and vegetables, in survivors (p=0.07).
One hundred thirty-seven survivors (46.1%) reported poor adolescent physical activity. In multivariable analyses, female sex (OR=2.06, CI=1.18–3.68), having parents without a college degree (OR=1.91, CI=1.11–3.32), cranial radiation (OR=3.35, CI=1.69–6.88), high TV/video time (OR=1.77, CI=1.00–3.14), and significant activity limitations due to health conditions (OR=8.28, CI=2.87–30.34) were associated with poor physical activity during adolescence (Table 2). Twenty-nine (30.2%) siblings reported poor physical activity during adolescence. For siblings, high TV/video time (OR=2.97, CI=1.12–8.04) and poor self-esteem (OR=3.94, CI=1.41–11.4) were associated with poor physical activity during adolescence (see Supplemental Table 3).
Table 2.
Multivariable assessment of risk factors for poor physical activity during adolescence
| OR | 95%CI | p | ||
|---|---|---|---|---|
| Sex | Female | 2.06 | 1.18–3.68 | 0.01 |
| Male | 1.00 | |||
| Parent College Graduate | No | 1.91 | 1.11–3.32 | 0.02 |
| Yes | 1.00 | |||
| Cranial Radiation | Yes | 3.35 | 1.69–6.88 | <0.01 |
| No | 1.00 | |||
| TV/Video Hours | 3 or more | 1.77 | 1.00–3.14 | 0.049 |
| 0–2 hours | 1.00 | |||
| Limitations of Activity | Poor (<17) | 8.28 | 2.87–30.34 | <0.01 |
| Average/Excellent (≥17) | 1.00 |
Note. Poor adolescent physical activity was defined as CHIP-AE subdomain score <17. The preliminary multivariable model included the following predictors: sex, parental education, cranial radiation, self-esteem, emotional discomfort, family involvement, TV/video hours, healthy diet behaviors, unhealthy diet behaviors, and limitations of activity. Predictors were selected for the final model by assessing goodness of fit and parsimony using AIC.
Young Adult Physical Activity
Ninety-eight survivors (40.8%) reported not meeting CDC recommendations for physical activity at Follow-up 4. In multivariable analyses, female sex (OR=1.83, CI=1.04–3.14) and reporting low healthy diet behaviors during adolescence (OR=1.84, CI=1.05–3.26) were associated with increased risk of not meeting CDC recommendations during young adulthood (Table 3). For siblings, high TV/video time (OR=3.46, CI=1.02–12.64) and average to excellent scores on emotional discomfort (OR=4.19, CI=1.15–19.15) were associated with increased risk of not meeting CDC guidelines (Supplementary Table 4).
Table 3.
Multivariable assessment of risk factors during adolescence associated with failure to meet CDC physical activity guidelines in young adulthood
| OR | 95%CI | p | ||
|---|---|---|---|---|
| Sex | Female | 1.83 | 1.04–3.14 | 0.03 |
| Male | 1.00 | |||
| Self-esteem | Poor (<17) | 1.80 | 0.99–3.31 | 0.05 |
| Average/Excellent (≥17) | 1.00 | |||
| Healthy Diet Behaviors | Poor (≤ 3) | 1.84 | 1.05–3.26 | 0.03 |
| Average/Excellent (>3) | 1.00 |
Note. Failure to meet CDC physical activity guidelines was ≤150 weekly minutes of moderate-intensity or ≤75 weekly minutes of vigorous-intensity aerobic activity. The preliminary model included the following adolescent predictors: sex, self-esteem, emotional discomfort, family involvement, healthy diet behaviors, and limitations of activity. Predictors were selected for the final model by assessing goodness of fit and parsimony using AIC.
Changes in Physical Activity Status from Adolescence to Adulthood
Among survivors, 39.8% reported adequate physical activity in adolescence and young adulthood (Figure 1). A smaller but substantial number (22.5%) reported low physical activity levels at both times. Similar numbers of survivors reported poor physical activity at only one time point, with similar numbers of survivors reporting decline or improvement in physical activity from adolescence to young adulthood (18.2% and 19.5%, respectively). Among siblings, 51.4% reported adequate physical activity and 12.5% reported low physical activity at both time points, 19.4% reported improvement and 16.7% reported decline from adolescence to adulthood (Figure 1). There were no statistically significant differences between survivors and siblings in any group.
Figure 1. Survivors’ and siblings’ physical activity status in adolescence and young adulthood.
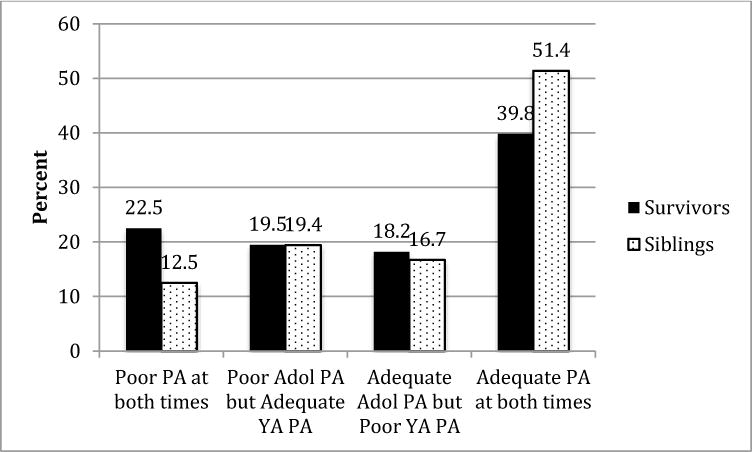
Note. PA=physical activity; Adol=Adolescent; YA=Young Adult. Poor adolescent physical activity = CHIP-AE subdomain score <17. Poor young adult physical activity = not meeting CDC physical activity guidelines. There were no significant differences between survivors and siblings in any group, p=0.07, 0.99, 0.76, and 0.09, respectively.
Discussion
In this longitudinal study of survivors of childhood cancer, we found inadequate levels of physical activity in 46% of adolescent survivors and 41% of young adult survivors, similar to previous cross-sectional reports of insufficient activity among child, adolescent, and young adult survivors of childhood cancer.15,32,33 This study found demographic and medical predictors (i.e., female sex, lower parental education, cranial radiation) that can be used to identify adolescent childhood cancer survivors at risk of poor physical activity and potentially modifiable behavioral targets (TV/video time, healthy diet behaviors) for intervention.
Of particular interest was the opportunity to examine changes in physical activity over time. Nearly one quarter of this childhood cancer survivor sample remained insufficiently active as they aged. Previous data from the CCSS indicate female sex, lower educational attainment, higher body mass index and chronic musculoskeletal conditions are associated with declining physical activity levels during adulthood.13 Identifying factors associated with changing levels of physical activity during the transition period from adolescence to young adulthood is an area for future research. Developmentally-sensitive interventions are needed to help adolescents adopt healthy lifestyle behaviors in the midst of the complex transition from pediatric to adult healthcare.34
Consistent with the general population,35–37 adolescent TV/video time, a proxy for sedentary behavior, was associated with lower adolescent physical activity for both survivors and siblings (and also with adult physical activity for siblings only). High sedentary behavior could reflect few opportunities for physical activity and more opportunities for high caloric intake, upsetting energy balance. Reducing sedentary time may be an important target to improve activity levels and could positively impact body mass index, as reducing sedentary time has been shown to reduce energy intake and increase physical activity for normal weight adolescents.38
Low healthy diet behaviors during adolescence were risk factors for poor physical activity as young adults. An unhealthy diet may be an indicator of poor lifestyle habits including insufficient activity, rather than a cause of inactivity. Future research would benefit from examining energy balance (calorie intake, energy expenditure) as relevant factors.
In contrast to previous work15 there were no significant associations between positive family involvement and concurrent or future physical activity. Based on a social-ecological framework, we expected adolescent health behaviors to be influenced by family members.39 However, our measure was not specific to family support for physical activity, which may be more proximally related to activity levels than general family support.
The associations between female sex, low socioeconomic status, and low physical activity in adolescence were consistent with previous work in healthy adolescents.40 The pattern of results for demographic factors was similar but not significant in our small sibling sample, suggesting many of the risk factors associated with insufficient physical activity are not specific to cancer survivors, but relevant to adolescents from families affected by early childhood cancer.
Limitations
Despite being one of the first studies to examine associations between childhood cancer survivors’ self-reported psychological functioning during adolescence and future physical activity as young adults, this study had limitations. First, this sample of childhood cancer survivors is relatively small with a limited age range at diagnosis (0 to 3 years), so results may not generalize to survivors diagnosed beyond early childhood. Second, our choice of risk factors was limited to those available on the CHIP-AE, which is a validated tool for adolescents but not a comprehensive measure of all constructs of interest, including dietary habits and sedentary behaviors. Third, the use of self-report measures of physical activity may overestimate physical activity compared to objective measures. Fourth, the sample of siblings included in the Teen Health Survey was small, precluding the ability to directly compare survivors and siblings in the same statistical model and limiting the number of risk factors considered in multivariable models. Relatedly, survivors who had chemotherapy and those with poorer adolescent physical activity were less likely to complete surveys, possibly suggesting that survivors with poorer health habits do not remain engaged over time and biasing our results towards underestimating effects. Finally, we did not have adequate longitudinal data to use path analysis to evaluate causal relationships between baseline psychological and behavioral variables and young adult physical activity.
Clinical Implications
Adolescent survivors of childhood survivors who are female, from low SES backgrounds, with cranial radiation exposure, with physical limitations, and who regularly spend more than 2 hours watching TV per day are at risk for poor physical activity during adolescence. Decreasing sedentary time and improving healthy diet behaviors during adolescence may help increase future physical activity in young adulthood. Behavioral interventions focused on decreasing time spent in sedentary activities, improving diet, or increasing participation in physical activities may be fruitful avenues for research.
Supplementary Material
Acknowledgments
This work was supported by the National Cancer Institute (CA55727). Support to St. Jude Children’s Research Hospital also provided by the Cancer Center Support (CORE) grant (CA21765) and by ACS Grant RSG-01-021-01-CCE (A. Mertens, PI). Support also provided by the American Lebanese-Syrian Associated Charities (ALSAC).
Footnotes
Conflict of Interest Statement
The authors declare no conflicts of interest.
References
- 1.Armstrong GT, Chen Y, Yasui Y, et al. Reduction in late mortality among 5-year survivors of childhood cancer. New England Journal of Medicine. 2016;374(9):833–842. doi: 10.1056/NEJMoa1510795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Howlader N, Noone A, Krapcho M, et al. SEER cancer statistics review, 1975–2013. Bethesda, MD: 2016. [Google Scholar]
- 3.Florin TA, Fryer GE, Miyoshi T, et al. Physical inactivity in adult survivors of childhood acute lymphoblastic leukemia: a report from the childhood cancer survivor study. Cancer Epidemiol Biomarkers Prev. 2007;16(7):1356–1363. doi: 10.1158/1055-9965.EPI-07-0048. [DOI] [PubMed] [Google Scholar]
- 4.Oeffinger KC, Buchanan GR, Eshelman DA, et al. Cardiovascular risk factors in young adult survivors of childhood acute lymphoblastic leukemia. J Pediatr Hematol Oncol. 2001;23(7):424–430. doi: 10.1097/00043426-200110000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Oeffinger K, Mertens A, Sklar C, et al. Obesity in adult survivors of childhood acute lymphoblastic leukemia: a report from the Childhood Cancer Survivor Study. Journal of Clinical Oncology. 2003;21(7):1359. doi: 10.1200/JCO.2003.06.131. [DOI] [PubMed] [Google Scholar]
- 6.De Caro E, Fioredda F, Calevo MG, et al. Exercise capacity in apparently healthy survivors of cancer. Arch Dis Child. 2006;91(1):47–51. doi: 10.1136/adc.2004.071241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.San Juan AF, Wolin K, Lucía A. Physical activity and pediatric cancer survivorship. Recent Results Cancer Res. Physical Activity and Cancer. 2011:319–347. doi: 10.1007/978-3-642-04231-7_14. [DOI] [PubMed] [Google Scholar]
- 8.Penedo FJ, Dahn JR. Exercise and well-being: a review of mental and physical health benefits associated with physical activity. Current opinion in psychiatry. 2005;18(2):189–193. doi: 10.1097/00001504-200503000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Kodama S, Saito K, Tanaka S, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. Jama. 2009;301(19):2024–2035. doi: 10.1001/jama.2009.681. [DOI] [PubMed] [Google Scholar]
- 10.Lipshultz SE, Adams MJ, Colan SD, et al. Long-term Cardiovascular Toxicity in Children, Adolescents, and Young Adults Who Receive Cancer Therapy: Pathophysiology, Course, Monitoring, Management, Prevention, and Research Directions A Scientific Statement From the American Heart Association. Circulation. 2013;128(17):1927–1995. doi: 10.1161/CIR.0b013e3182a88099. [DOI] [PubMed] [Google Scholar]
- 11.Ness KK, Leisenring WM, Huang S, et al. Predictors of inactive lifestyle among adult survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. Cancer. 2009;115(9):1984–1994. doi: 10.1002/cncr.24209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Castellino SM, Casillas J, Hudson MM, et al. Minority Adult Survivors of Childhood Cancer: A Comparison of Long-Term Outcomes, Health Care Utilization, and Health-Related Behaviors From the Childhood Cancer Survivor Study. Journal of Clinical Oncology. 2005;23(27):6499–6507. doi: 10.1200/JCO.2005.11.098. [DOI] [PubMed] [Google Scholar]
- 13.Wilson CL, Stratton K, Leisenring WL, et al. Decline in physical activity level in the childhood cancer survivor study cohort. Cancer Epidemiology Biomarkers & Prevention. 2014;23(8):1619–1627. doi: 10.1158/1055-9965.EPI-14-0213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stolley MR, Restrepo J, Sharp LK. Diet and physical activity in childhood cancer survivors: a review of the literature. Ann Behav Med. 2010;39(3):232–249. doi: 10.1007/s12160-010-9192-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gilliam MB, Madan-Swain A, Whelan K, Tucker DC, Demark-Wahnefried W, Schwebel DC. Social, demographic, and medical influences on physical activity in child and adolescent cancer survivors. Journal of Pediatric Psychology. 2012;37:198–208. doi: 10.1093/jpepsy/jsr085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Keats MR, Courneya KS, Danielsen S, Whitsett SF. Leisure-Time Physical Activity and Psychosocial well-being in adolescents after cancer diagnosis. Journal of Pediatric Oncology Nursing. 1999;16(4):180–188. doi: 10.1177/104345429901600402. [DOI] [PubMed] [Google Scholar]
- 17.Paxton RJ, Jones LW, Rosoff PM, Bonner M, Ater JL, Demark-Wahnefried W. Associations between leisure-time physical activity and health-related quality of life among adolescent and adult survivors of childhood cancers. Psychooncology. 2010;19(9):997–1003. doi: 10.1002/pon.1654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jones LW, Liu Q, Armstrong GT, et al. Exercise and risk of major cardiovascular events in adult survivors of childhood hodgkin lymphoma: a report from the childhood cancer survivor study. J Clin Oncol. 2014;32(32):3643–3650. doi: 10.1200/JCO.2014.56.7511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hallal PC, Victora CG, Azevedo MR, Wells JCK. Adolescent physical activity and health: a systematic review. Sports Medicine. 2006;36(12):1019–1030. doi: 10.2165/00007256-200636120-00003. [DOI] [PubMed] [Google Scholar]
- 20.Mertens AC, Liu Q, Neglia JP, et al. Cause-specific late mortality among 5-year survivors of childhood cancer: the Childhood Cancer Survivor Study. Journal of the National Cancer Institute. 2008;100(19):1368–1379. doi: 10.1093/jnci/djn310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mertens AC, Yasui Y, Neglia JP, et al. Late mortality experience in five-year survivors of childhood and adolescent cancer: the Childhood Cancer Survivor Study. Journal of Clinical Oncology. 2001;19(13):3163–3172. doi: 10.1200/JCO.2001.19.13.3163. [DOI] [PubMed] [Google Scholar]
- 22.Lipshultz SE, Lipsitz SR, Mone SM, et al. Female sex and higher drug dose as risk factors for late cardiotoxic effects of doxorubicin therapy for childhood cancer. New England Journal of Medicine. 1995;332(26):1738–1744. doi: 10.1056/NEJM199506293322602. [DOI] [PubMed] [Google Scholar]
- 23.Robison LL, Armstrong GT, Boice JD, et al. The childhood cancer survivor study: A national cancer institute–supported resource for outcome and intervention research. Journal of Clinical Oncology. 2009;27(14):2308–2318. doi: 10.1200/JCO.2009.22.3339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leisenring WM, Mertens AC, Armstrong GT, et al. Pediatric cancer survivorship research: experience of the Childhood Cancer Survivor Study. Journal of Clinical Oncology. 2009;27(14):2319–2327. doi: 10.1200/JCO.2008.21.1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mertens AC, Brand S, Ness KK, et al. Health and well-being in adolescent survivors of early childhood cancer: a report from the Childhood Cancer Survivor Study. Psycho-Oncology. 2014;23(3):266–275. doi: 10.1002/pon.3414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Starfield B, Riley AW, Green BF, et al. The adolescent child health and illness profile: a population-based measure of health. Medical care. 1995:553–566. doi: 10.1097/00005650-199505000-00008. [DOI] [PubMed] [Google Scholar]
- 27.Starfield BRA, Ensminger M, Green B, Ryan S, Kim-Harris S, Johnston D, Vogel K. Manual for the Child Health and Illness Profile-Adolescent Edition (CHIP-AE) Baltimore, MD: The Johns Hopkins University; 1994/1997/2000. [Google Scholar]
- 28.Forrest CB, Starfield B, Riley AW, Kang M. The impact of asthma on the health status of adolescents. Pediatrics. 1997;99(2):e1–e1. doi: 10.1542/peds.99.2.e1. [DOI] [PubMed] [Google Scholar]
- 29.Riley AW, Forrest CB, Starfield B, Green B, Kang M, Ensminger M. Reliability and validity of the adolescent health profile-types. Medical care. 1998;36(8):1237–1248. doi: 10.1097/00005650-199808000-00011. [DOI] [PubMed] [Google Scholar]
- 30.Starfield B, Forrest CB, Ryan SA, Riley AW, Ensminger ME, Green BF. Health status of well vs ill adolescents. Archives of pediatrics & adolescent medicine. 1996;150(12):1249–1256. doi: 10.1001/archpedi.1996.02170370027003. [DOI] [PubMed] [Google Scholar]
- 31.American Academy of Pediatrics CoCM. Media Education. Pediatrics. 2010;126(5):1012–1017. doi: 10.1542/peds.2010-1636. [DOI] [PubMed] [Google Scholar]
- 32.Krull KR, Huang S, Gurney JG, et al. Adolescent behavior and adult health status in childhood cancer survivors. Journal of Cancer Survivorship. 2010;4(3):210–217. doi: 10.1007/s11764-010-0123-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Demark Wahnefried W, Werner C, Clipp EC, et al. Survivors of childhood cancer and their guardians. Cancer. 2005;103(10):2171–2180. doi: 10.1002/cncr.21009. [DOI] [PubMed] [Google Scholar]
- 34.Freyer DR. Transition of care for young adult survivors of childhood and adolescent cancer: Rationale and approaches. Journal of Clinical Oncology. 2010;28(32):4810–4818. doi: 10.1200/JCO.2009.23.4278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Marshall SJ, Biddle SJH, Gorely T, Cameron N, Murdey I. Relationships between media use, body fatness and physical activity in children and youth: a meta-analysis. International Journal of Obesity. 2004;28(10):1238–1246. doi: 10.1038/sj.ijo.0802706. [DOI] [PubMed] [Google Scholar]
- 36.Richards R, Poulton R, Reeder AI, Williams S. Childhood and contemporaneous correlates of adolescent leisure time physical inactivity: A longitudinal study. Journal of Adolescent Health. 2009;44(3):260–267. doi: 10.1016/j.jadohealth.2008.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Strauss RS, Rodzilsky D, Burack G, Colin M. Psychosocial correlates of physical activity in healthy children. Archives of Pediatrics and Adolescent Medicine. 2001;155(8):897–902. doi: 10.1001/archpedi.155.8.897. [DOI] [PubMed] [Google Scholar]
- 38.Epstein LH, Roemmich JN, Paluch RA, Raynor HA. Influence of changes in sedentary behavior on energy and macronutrient intake in youth. The American journal of Clinical Nutrition. 2005;81(2):361–366. doi: 10.1093/ajcn.81.2.361. [DOI] [PubMed] [Google Scholar]
- 39.Bronfenbrenner U. The ecology of human development: Experiments by nature and design. Cambridge, MA: Harvard University; 1979. [Google Scholar]
- 40.Sallis JF, Prochaska JJ, Taylor WC. A review of correlates of physical activity of children and adolescents. Medicine & Science in Sports & Exercise. 2000;32(5):963–975. doi: 10.1097/00005768-200005000-00014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


