Abstract
Introduction
There are multiple dimensions of HIV-related stigma that can compromise the mental and physical health of people living with HIV (PLWH). We focused on the dimension of experienced stigma, defined as exposure to acts of discrimination, devaluation, and prejudice, and investigated its relationship with HIV health and psychosocial outcomes.
Methods
We examined associations between experienced stigma in the community and healthcare settings and psychosocial and health outcomes for PLWH (N=203) receiving care at an urban HIV clinic in the Southeastern United States. We also investigated whether those effects are unique to experienced stigma or are mediated by other dimensions of HIV-related stigma.
Results
Experienced stigma was associated with suboptimal clinical outcomes like viral non-suppression, as well as poor affective, cognitive, and mental health outcomes (self-esteem, depressive symptoms, avoidance coping, and blame coping) and interpersonal outcomes like social support and physician trust. Furthermore, serial mediation models suggested significant indirect effects of experienced stigma through internalized stigma and anticipated stigma from various theoretically expected sources of stigma (e.g., community members, friends and family, and healthcare workers), with varying effects depending on the source.
Conclusions
These findings suggest nuanced mechanisms for the effects of experienced HIV-related stigma, especially in healthcare settings, and may be used to inform stigma-reduction interventions. Interventions designed to address experienced stigma in healthcare settings might be more tailored to specific outcomes, like depression and physician trust, than interventions designed to address experienced stigma in the community.
INTRODUCTION
HIV stigma is a social, context-driven process that interferes with the psychological and physical well-being of people living with HIV (PLWH).1,2,3 Through contextual stigma mechanisms, PLWH respond to social cues that they are not valued due to their HIV status, which may undermine their sense of self-worth.3 HIV-related stigma can also negatively affect health by acting as a barrier to retention in HIV care and adherence to antiretroviral therapy (ART),4,5 both of which are integral components of the HIV care continuum6 and are necessary for viral suppression.7
Stigma may be conceptualized in terms of different dimensions.3 These include perceived community stigma (sensed/believed existence and severity of stigmatizing attitudes in the community against PLWH), experienced stigma (exposure to acts of discrimination, devaluation, and prejudice), anticipated stigma (expectation of being treated negatively), and internalized stigma (acceptance of negative societal characterizations and applying these to oneself).2,3 There are also different sources of HIV-related stigma, which may include institutions, healthcare workers, coworkers, community members, family, friends, and sexual partners.8
The multi-dimensionality of HIV-related stigma is of increasing interest due to evidence that different stigma dimensions have distinct effects on specific psychosocial and health outcomes.3,9 In their seminal HIV Stigma Framework, Earnshaw and Chaudoir conceptualized how different dimensions of stigma (experienced, anticipated, and internalized) are associated with distinct, measurable outcomes for PLWH.3 For example, internalized stigma is uniquely associated with poorer psychological well-being (e.g., depressive symptomology), and anticipated stigma is associated with suboptimal health service utilization (e.g., lower adherence to ART).2,9 A recent meta-analysis also supports this framework; for example, while internalized and anticipated stigma consistently predict health ART adherence, experienced stigma does not.10 Instead, prior research has suggested that experienced stigma has a direct effect on physical health (e.g., viral load) due to the toll it takes on the body as a chronic stressor.9
It is possible that other dimensions of stigma mediate the effects of experienced stigma on adherence and other outcomes. Indeed, a recent conceptual framework on the effects of HIV-related stigma suggests that one dimension of HIV-related stigma may mediate the effect of another dimension.8 This conceptual framework also added the dimension of perceived stigma to the HIV Stigma Framework,8 as supported by recent empirical findings that internalized stigma mediates the effect of perceived stigma on relevant affective, cognitive, and mental health outcomes, as well as health outcomes.2 In the present study, we explore whether other dimensions of stigma may mediate the effect of experienced stigma on outcomes. As was found with perceived community stigma,2 we hypothesize that internalized and anticipated HIV-related stigma may mediate the effect of experienced stigma on psychosocial and health outcomes for PLWH. That is, when PLWH experience stigma and discrimination from others, this may lead them to internalize and anticipate stigma, which is often automatic in nature.11,12 Internalized and anticipated stigma, in turn, may have downstream negative effects on physical and psychological health.
Sources of stigma are also relevant to health outcomes. Experienced stigma in healthcare settings can manifest as refusal of treatment to PLWH and failure to protect the confidentiality of patients’ HIV status.13,14 Some PLWH have described feeling particularly affected by the stigma and discrimination they experience as patients, given the expectations that providers have expert medical knowledge and adhere to the value of beneficence.15 In these circumstances, PLWH report negative emotional reactions, such as offense and humiliation,16 and depressive symptoms.17 Additionally, PLWH who experience stigma in health care settings may also anticipate stigma in the same setting and, consequently, have lower trust in healthcare providers.18 Mistrust interferes with the physician-provider relationship19,20 and may increase counterproductive health behaviors, such as ART non-adherence.21
In contrast, experienced stigma in community settings can manifest as expression of negative attitudes toward PLWH and social isolation and rejection of PLWH in places of public accommodation (e.g., parks, schools, restaurants, retail stores, etc.).22,23 Prior scientific literature suggests that PLWH who experience HIV-related stigma in community settings may also anticipate and internalize stigma,9,23 presumably in the same settings. Thus, experienced stigma in the community can increase levels of psychological distress (i.e., anxiety and depression) among PLWH.24 In the current study, we expect that the specific health effects of experienced stigma differ depending on the source or context (i.e., healthcare providers and staff versus the community).
In order to better inform the development of health interventions for PLWH, it is important to differentiate between dimensions and sources of HIV-related stigma and to identify mediating pathways between HIV-related stigma and health outcomes.8 In this study, we examined several relationships not yet explored in the extant scientific literature. Specifically, we examined associations between experienced HIV stigma (in both community and healthcare settings) and interpersonal, psychological, mental health factors, and HIV-related health outcomes. Additionally, we examined whether these relationships are mediated by other dimensions of HIV-related stigma (i.e., internalized and anticipated).
METHODS
Participants and procedures
We used purposive sampling to identify patients from an HIV clinic at a large urban university in the Southeast using the following inclusion criteria: current ART use, substance nonuse, and recent (in the six months preceding the time of the study) clinic record of viral load (Table 1). We contacted eligible participants and invited them to complete computer-based study measures at a separate research visit. Among the eligible participants, 74 female-identified and 129 male-identified individuals (73 White and 130 Black) with an average age of 44.8 years (SD=11.1 years) completed computer-based study measures. Clinic records data were obtained for these patients on depressive symptoms, duration of ART, and viral load. The final sample included 203 patients.
TABLE 1.
Background characteristics for study participants (N=203)
| Characteristic | n (%) |
|---|---|
| Sex | |
| Male | 129 (63.5) |
| Female | 74 (36.5) |
| Race | |
| Black/African American | 130 (64.0) |
| White | 73 (36.0) |
| Mean (SD) | |
| Age (in years) | 44.8 (11.1) |
| Socioeconomic status* | 2.7 (1.0) |
| Time on ART (months) | 95.8 (63.1) |
Defined as socioeconomic status level, indicated from lower (1) to upper (5).
HIV Clinical Outcomes
Lu et. al’s25 one-item measure was utilized to assess ART adherence: “In the past 4 weeks, how was your ability to take all of your anti-HIV medications prescribed by your doctor?” Participants responded using a self-report measure that asked them to indicate how adherent they believe themselves to be. The response choices were: 1- Very poor; 2- Poor; 3- Fair; 4- Good; 5- Very good; 6- Excellent. Previous literature suggests this subjective and relative measure of adherence is as useful and reliable as other self-report measures of adherence.26 In our sample, 71% of participants reported excellent adherence. Therefore, responses were dichotomized (“excellent” adherence vs. all other response options).27 Although self-report measures tend to over-estimate adherence, previous research supports the predicted value of self-reported non-optimal adherence.28 Viral load data from each participant’s last clinic visit was extracted from clinic data as not suppressed (≥ 200 c/mL) versus suppressed (<200 c/mL).
HIV-related stigma dimensions
To our knowledge, no single existing psychometric stigma tool measures all stigma dimensions and sources that we sought to examine. Therefore, we used separate measures. We included two subscales of the revised HIV Stigma Scale,29 each of which showed evidence of internal consistency in the current study sample: internalized stigma (seven items, α =.85) and experienced stigma in the community (11 items, α=. 93). We adapted nine items from the Stigma Mechanisms measure8 to quantify anticipated stigma from the three following sources: friends and family, neighbors and others in the community, and healthcare workers. All anticipated stigma subscales were highly reliable in the present sample (α=.90, α=.94, and α=.83 for friends and family, neighbors, and healthcare workers, respectively, each consisting of three items).
Experienced stigma in the healthcare setting was assessed using eight items adapted from the field-tested version of the enacted stigma section of an international tool for measuring HIV-related stigma among healthcare workers (not necessarily HIV healthcare setting).30 Two of the items were not positively correlated with the rest of the items, thereby reducing Cronbach’s alpha. Therefore, the mean of the remaining six items were used for the present analysis (Cronbach’s α=.73). The rating scale for experienced stigma in the healthcare setting included the following responses: 1- Never; 2- Rarely; 3- A lot of the time; 4- Most of the time (see Appendix for items and rating scale used in the study).
Cognitive, Affective, and Mental Health Factors
Rosenberg’s 10-item Self-Esteem Scale was used to measure global self-esteem (α=.81).30 The nine-item Patient Health Questionnaire (PHQ-9) measured depressive symptoms (α=.87).31 To assess coping by avoidance and coping by blaming, we employed two subscales from the Ways of Coping measure (10 items, α=.76 and three items, α=.81, for coping by avoidance and by blaming, respectively).32
Interpersonal Factors
The 16-item Interpersonal Support Evaluation List (ISEL) assessed social support with good reliability (α=.88).33 The 10-item Wake Forest Physician Trust Scale also showed internal consistency in our study (α=.82).34
Statistical Analyses
All analyses conducted were cross-sectional. First, we examined descriptive statistics for the present sample. Then, we tested associations between experienced stigma in the community and experienced stigma in healthcare settings with ART adherence or viral suppression using logistic regression. We also tested the associations between experienced stigma in the community and experienced stigma in healthcare settings and psychosocial outcomes (that were assessed as continuous measures) using linear multiple regression analyses. In all regression analyses, the following covariates were included: sex, race, age, socioeconomic status, and time on ART. These covariates were chosen based on previous research.6
Hypothesized mediation models were informed by the recent conceptual framework8 on the effects of HIV-related stigma and included single-mediator models (as depicted in Figure 1) in addition to serial mediation models as depicted in Figure 3. Models were tested with the regression-based Process procedure, a statistical software macro that is compatible with SAS and SPSS.35 The Process macro calculates an indirect effect between a predictor and an outcome from the product of path coefficients when the mediator(s) is present. Using this approach, the direct effect does not necessarily have to be significant for mediation to be present due to inconsistent mediation.36,37 We calculated bias-corrected 95% confidence intervals (CIs) for the indirect effects using bootstrapping. A significant indirect effect is revealed when the CI does not include the value zero, which suggests that statistical mediation is present.
Figure 1.
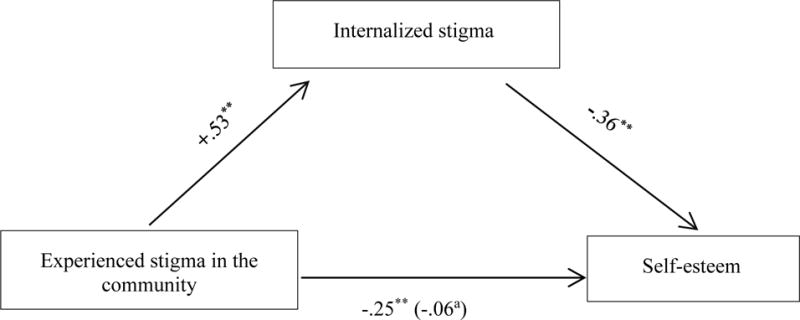
Internalized stigma mediates the effect of experienced stigma in the community on self-esteem.
Note. Path coefficients are unstandardized. Sex, race, age, socio-economic status, and time on ART are also controlled.
a When internalized stigma is in the model.
Figure 3.
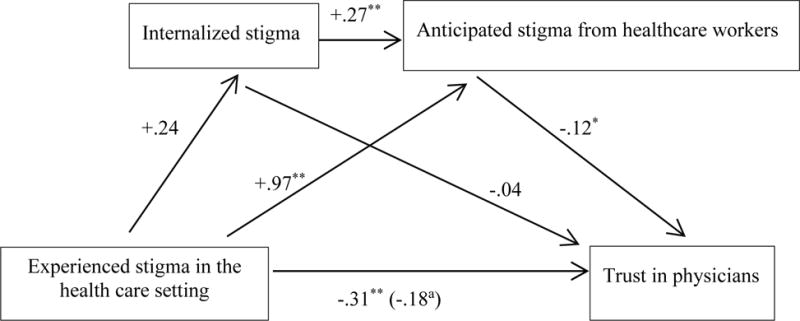
Internalized stigma and anticipated stigma from healthcare workers mediate the effect of experienced stigma in healthcare settings on trust in physicians (serial mediation).
Note. Path coefficients are unstandardized. Sex, race, age, socio-economic status, and time on ART are also controlled.
a When internalized stigma and anticipated stigma from healthcare workers are in the model.
RESULTS
HIV Clinical Outcomes
Neither experienced stigma in the community nor experienced stigma in the healthcare setting was associated with medication adherence. Nevertheless, we tested the indirect effects of the two experienced stigma dimensions on medication adherence, since indirect effects can be significant even in the absence of non-significant total effects due to inconsistent mediation.36 The indirect effect of experienced stigma in the healthcare setting on medication adherence through internalized stigma was not significant. However, the indirect effect of experienced stigma in the community on medication adherence through internalized stigma was significant (B= −0.42, SE=.24, 95% CI [−.93, −.06]).
The majority of participants (n=184) had viral loads <200 c/mL (suppressed). Results of logistic regression analyses using viral load (not suppressed=1 versus suppressed=0) as the dependent variable revealed a significant effect of experienced stigma in the healthcare setting on non-suppressed viral load (AOR=3.23, p=.03, 95% CI [1.15, 9.06]). When added to the model, ART adherence was also a significant predictor of viral load non-suppression (AOR=0.17, p=.01, 95% CI [0.05, 0.61]). In this model including ART adherence, the effect of experienced stigma in the healthcare setting changed very little (AOR=3.33, p=.03, 95% CI [1.15, 9.66]), suggesting that ART adherence does not mediate the association between experienced stigma in healthcare settings and viral non-suppression. On the other hand, the association between experienced stigma and viral non-suppression outside of healthcare settings was not significant (AOR=1.32, p=.57, 95% CI [0.51, 3.38]). Supplementary analyses examining inconsistent mediation effects did not reveal significant indirect effects through internalized stigma for either experienced stigma in the healthcare setting or in the community.
Affective, Cognitive, and Mental Health Factors
We conducted linear regression analyses to examine the relationships between stigma in healthcare and community settings and affective, cognitive, and mental health factors (i.e., depressive symptoms, self-esteem, avoidance coping, and blame coping) (Table 2). For experienced stigma in the community, all associations were significant. Positive associations were found with depressive symptoms (B=1.75, SE=0.50, t=3.50, p=0.001), avoidance coping (B=0.53, SE=0.07, t=7.44, p<0.001), and blame coping (B=0.39, SE=0.11, t=3.71, p<0.001). On the other hand, a negative association was found with self-esteem (B= −0.25, SE=0.05, t= −5.33, p<0.001). Similar to experienced stigma in the community, stigma experienced in healthcare settings was positively associated with both depressive symptoms (B=1.76, SE=0.79, t=2.24, p=0.03) and avoidance coping (B=0.46, SE=0.12, t=3.81, p<0.001). However, it was not significantly associated with coping by blaming or with self-esteem.
TABLE 2.
Associations between community and healthcare setting experienced HIV-related stigma and affective, cognitive, mental health, and interpersonal factors
| Community Stigma | Healthcare Setting Stigma | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| Factor | B | SE | p | B | SE | p |
| Self-esteem | −0.25 | 0.05 | <0.001 | −0.07 | 0.08 | 0.38 |
| Depressive symptoms | 1.75 | 0.50 | <0.001 | 1.76 | 0.79 | <0.05 |
| Avoidance coping | 0.53 | 0.72 | <0.001 | 0.46 | 0.12 | <0.001 |
| Blame coping | 0.39 | 0.11 | <0.001 | 0.19 | 0.17 | 0.26 |
| Interpersonal support | −0.37 | 0.05 | <0.001 | −0.27 | 0.09 | <0.01 |
| Physician trust | −0.09 | 0.06 | 0.17 | −0.31 | 0.09 | <0.01 |
Covariates sex, race, age, socioeconomic status, and time on ART were also entered in all analyses
We tested whether the effect of experienced stigma in the community on affective, cognitive, and mental health outcomes was mediated by internalized stigma. The indirect effect of experienced stigma in the community on self-esteem through internalized stigma was significant (B= −0.19, SE=.04, 95% CI [−.27, −.13]), suggesting that internalized stigma mediates the effect of experienced stigma on self-esteem (see Figure 1 for all path coefficients). Similarly, mediation analyses of depressive symptoms and coping outcomes yielded significant indirect effects of experienced stigma in the community through internalized stigma. Indirect effects for depressive symptoms, avoidance coping, and blame coping, respectively, were as follows: (B=0.67, SE=.36, 95% CI [.02 1.43]; B=0.24, SE=.05, 95% CI [.14, .35]; B=0.45, SE=.09, 95% CI [.31, .64]).
We also tested whether the associations between experienced stigma in healthcare settings and affective, cognitive, and mental health outcomes were mediated by internalized stigma. The indirect effects were significant only for depressive symptoms (B=0.40, SE=.26, 95% CI [0.04, 1.17]) and blame coping (B=0.20, SE=0.11, 95% CI [0.001, 0.43]).
Interpersonal Factors
We examined the relationships between experienced stigma in the community and experienced stigma in healthcare settings and interpersonal factors (i.e., social support and physician trust). In linear regression analyses, experienced stigma in the community (B=−0.37, SE=0.05, t=−6.97, p<0.001) and experienced stigma in healthcare settings (B=−0.27, SE=0.09, t=−3.03, p=0.003) were both significant predictors of social support. Only stigma experienced in healthcare settings was significantly associated with physician trust (B=−0.31, SE=0.09, t=−3.25, p=0.001).
Next, we used a serial mediation model to examine the indirect effect of experienced stigma on physician trust and social support through internalized stigma and anticipated stigma. The indirect effect of experienced stigma in the community on social support through first internalized stigma and then stigma anticipated from the community (Figure 2) was significant (B= −.03, SE=.01, CI [−.06, −.01]). The indirect effect of experienced stigma in the community on social support through internalized stigma and stigma anticipated from friends and family was also significant (B= −.03, SE=.01, CI [−.06, −.01]).
Figure 2.
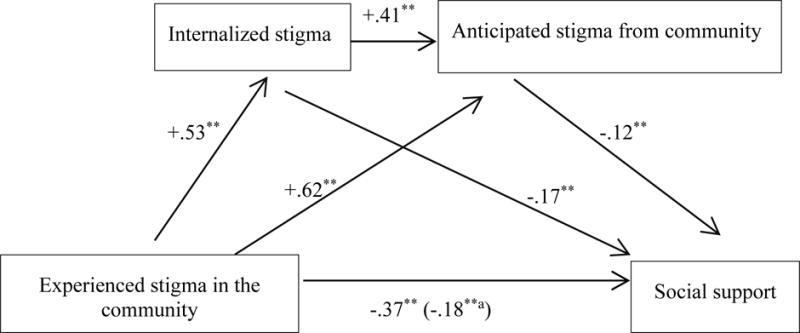
Internalized stigma and anticipated stigma from the community mediate the effect of experienced stigma in the community on social support (serial mediation).
Note. Path coefficients are unstandardized. Sex, race, age, socio-economic status, and time on ART are also controlled.
a When internalized stigma and anticipated stigma from the community are in the model.
When examining physician trust, the indirect effect of experienced stigma in healthcare settings on physician trust through internalized stigma and stigma anticipated from healthcare workers (Figure 3) was significant (B=−.01, SE=.01, CI [−.03, −.0007]). However, the indirect effect on physician trust was not significant when anticipated stigma from friends and family or the community were added to the serial mediation model. As a whole, these results suggest that experienced stigma in healthcare and community settings may have differential effects on interpersonal outcomes.
DISCUSSION
We examined associations between different sources of experienced HIV-related stigma and pertinent health, psychosocial, and interpersonal outcomes and investigated whether these effects are mediated by other dimensions of HIV-related stigma. As in previous research,9 our findings suggest that experienced stigma manifests in suboptimal physical health outcomes for PLWH. Although experienced stigma in healthcare settings was significantly associated with viral suppression, the same was not found for experienced stigma in community settings. Thus, experiencing stigma in healthcare settings rather than in the community appears to have a greater impact on HIV-related health. This finding has implications for healthcare workers, as respectful interactions with PLWH are critical to health. Our findings also suggest that experiencing stigma in healthcare settings can hinder progress through steps of the HIV care continuum, ultimately undermining achievement of undetectable viral load. Participatory methods of care may promote feelings of empowerment and inclusivity among PLWH with those who provide their care.13,38 While all persons who work in healthcare settings where PLWH receive services may benefit from training on stigma reduction, previous focus group feedback from PLWH suggests that non-medical frontline personnel (e.g., receptionists) may particularly benefit from these kinds of interventions, as they are typically not as familiar with the needs and concerns of PLWH.13
We did not find significant associations between community experienced stigma or healthcare experienced stigma and adherence. When also considering that the relationship between experienced stigma in healthcare settings and viral suppression was not found to be mediated by ART adherence, it seems likely that experienced stigma in the healthcare setting has a direct physiological effect.9 Furthermore, previous research has suggested that stigma is a variable, within-person trait elicited by specific acts of discrimination.11 Taken together, these results suggest that the effect of experienced stigma on adherence outcomes is most likely proximal, whether from community or healthcare settings.10 These results also correspond with extant literature, as studies that have examined multiple dimensions of HIV-related stigma have found that other dimensions of stigma (anticipated, perceived, and internalized) are more likely to predict non-adherence than experienced stigma.10,39 The HIV Stigma Framework in particular distinguishes experienced stigma as a dimension of stigma not connected to behavioral outcomes, but, rather, physical outcomes, given that experiences of stigma are uniquely stressful experiences which may chronically impact HIV disease progression.9
In examining psychosocial outcomes, our results on the effects of experienced HIV-related stigma echo previous research related to the effects of perceived HIV-related stigma in the community6 and provide a novel understanding of the nuances of experienced stigma. We found that experienced stigma in the community was associated with all affective, cognitive, and mental health outcomes (depressive symptoms, avoidance coping, blame coping, and self-esteem), and these associations were each mediated by internalized stigma. Interventions aimed at reducing stigma at the community level may help prevent PLWH from experiencing these negative psychosocial outcomes by mitigating the internalization and subsequent anticipation of stigma. For example, Project CHHANGE (Challenge HIV Stigma and Homophobia and Gain Empowerment) has been shown to be both feasible and acceptable to community residents.39
As for interpersonal outcomes, while experienced stigma in community and healthcare settings were both significant predictors of social support, only experienced stigma in healthcare settings was associated with physician trust. Serial mediation models added granularity to the complexity of the effects of experienced stigma on interpersonal outcomes. When examining effects on social support, anticipated stigma from the community and anticipated stigma from friends and family were both mediators on the pathway from experienced stigma in the community through internalized stigma. These results suggest that some of the effects of experienced and anticipated stigma are context-specific and expand on existing literature2 by suggesting that experienced stigma in healthcare settings is more germane to anticipated stigma within (rather than outside of) the healthcare setting.
HIV-related experienced stigma in healthcare settings (but not experienced stigma in the community) was associated with physician trust, and this association was first mediated by internalized stigma and then by stigma anticipated from healthcare workers (but not by stigma anticipated from friends and family or from the community). As in previous work,2 these findings help substantiate the idea that the source of anticipated stigma, as well as the context of experienced stigma, are differential contributors to key psychosocial and interpersonal outcomes for PLWH. These results suggest that experienced stigma in the community may impact PLWH more broadly, whereas the scope of experienced stigma in healthcare settings may be narrower and may particularly benefit from targeted interventions.
This research should be interpreted in light of its limitations. The research design was cross-sectional, and, as such, we are unable to ascribe causality or gain insight into the temporality of the effects of experienced stigma. Furthermore, the self-reported measures of experienced stigma and adherence may have introduced bias into the analysis. In addition, although anticipated stigma from friends and family was grouped into a single category in this analysis, it is possible that it comprises two distinct categories. Anticipated stigma from sexual partners, though not explicitly measured in this study, may represent an additional distinct stigma dimension. Similarly, salient context for experienced stigma may exist outside of the healthcare/non-healthcare dichotomy used in this research. Future research should investigate additional sources and settings of experienced and anticipated stigma. The present results may serve as an initial attempt to identify mediating pathways that can be tested in future studies using longitudinal designs.
Despite their limitations, these findings help illuminate the ways in which different experienced HIV stigma mechanisms affect the health and well-being of PLWH. One way in which clinicians and public health practitioners can translate these findings into practice is by providing healthcare providers and frontline staff with targeted interventions aimed at reducing stigma. Providers can also work with PLWH directly to address and ameliorate various dimensions of stigma. By understanding the complexities of stigma, researchers, clinicians, and public health practitioners are better equipped to reduce its overall harmful effects on the health and well-being of PLWH.
Acknowledgments
We would like to thank Maria Lechtreck, C. Blake Helms, Christy Thai, and all the research assistants for their help in data collection.
SOURCES OF SUPPORT
This research was supported by the University of Alabama at Birmingham (UAB) Center for AIDS Research CFAR, an NIH funded program (P30 AI027767) that was made possible by the following institutes: NIAID, NCI, NICHD, NHLBI, NIDA, NIA, NIDDK, NIGMS, and OAR. W.S.R. and K.B.C. are supported by a T32 in Health Services and Outcomes Research (Agency for Healthcare Research and Quality [AHRQ] T32HS013852). Investigator support for this study was also provided by a Women’s Interagency HIV Study sub-study grant from the National Institute of Mental Health, R01MH104114. The contents of this publication are the sole responsibility of the authors and do not represent the official views of the NIH or AHRQ.
Appendix
The measure used to assess HIV-related stigma among health facility staff. The two items that were excluded from the current analyses are indicated with an asterisk (*).
In the past 12 months, how often have you experienced the following at a health facility (clinic, doctor’s office etc.)?
Healthcare workers were unwilling to care for you because you are living with HIV.
Healthcare workers provided poorer quality of care to you than to other patients because you are living with HIV.
Healthcare workers talked badly about people living with HIV.
Healthcare workers confronted or educated someone who was mistreating a patient living with HIV. *
Healthcare workers disclosed or told your HIV status to others without your permission.
Healthcare workers used extra infection control precautions (like wearing extra gloves) when caring for you because you are a person living with HIV.
Healthcare workers provided extra support or care to you because you are living with HIV or they think that you are living with HIV. *
Healthcare workers sent or referred you to another health facility because the workers do not want to treat you there.
Rating Scale for Experienced Stigma in the Healthcare Setting:
| Never | Rarely | A lot of the time | Most of the time |
|---|---|---|---|
| 1 | 2 | 3 | 4 |
Footnotes
PRIOR MEETING PRESENTATIONS
11th International Conference on HIV Treatment and Prevention Adherence, Ft. Lauderdale, FL, May 9–11, 2016
International Conference on Stigma, Washington, D.C., November 18, 2016
New York State Department of Health AIDS Institute Quality of Care Clinical and Consumer Advisory Committee Meetings, New York, NY, December 13–14, 2016
References
- 1.Herek GM, Glunt EK. An epidemic of stigma: Public reactions to AIDS. Am Psychol. 1988;43(11):886–891. doi: 10.1037//0003-066x.43.11.886. [DOI] [PubMed] [Google Scholar]
- 2.Turan B, Budhwani H, Fazeli PL, et al. How does stigma affect people living with HIV? The mediating roles of internalized and anticipated HIV stigma in the effects of perceived community stigma on health and psychosocial outcomes. AIDS Behav. 2017;21:283–291. doi: 10.1007/s10461-016-1451-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: a review of HIV stigma mechanism measures. AIDS Behav. 2009;13(6):1160–1177. doi: 10.1007/s10461-009-9593-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rueda S, Mitra S, Chen S, et al. Examining the associations between HIV-related stigma and health outcomes in people living with HIV/AIDS: a series of meta-analyses. BMJ Open. 2016;6(7):e011453. doi: 10.1136/bmjopen-2016-011453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Katz IT, Ryu AE, Onuegbu AG, et al. Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. J Int AIDS Soc. 2013;16(3 Suppl 2):18640. doi: 10.7448/IAS.16.3.18640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mugavero MJ, Amico KR, Horn T, et al. The state of engagement in HIV care in the United States: from cascade to continuum to control. Clin Infect Dis. 2013;57(8):1164–1171. doi: 10.1093/cid/cit420. [DOI] [PubMed] [Google Scholar]
- 7.Bangsberg DR, Perry S, Charlebois ED, et al. Non-adherence to highly active antiretroviral therapy predicts progression to AIDS. AIDS. 2001;15(9):1181–1183. doi: 10.1097/00002030-200106150-00015. [DOI] [PubMed] [Google Scholar]
- 8.Turan B, Hatcher AM, Weiser SD, et al. Framing mechanisms linking HIV-related stigma, adherence to treatment, and health outcomes. Am J Public Health. 2017;107(6):863–869. doi: 10.2105/AJPH.2017.303744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Earnshaw VA, Smith LR, Chaudoir SR, et al. HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS Behav. 2013;17(5):1785–1795. doi: 10.1007/s10461-013-0437-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sweeney SM, Vanable PA. The association of HIV-related stigma to HIV-related medication adherence: A systematic review and synthesis of the literature. AIDS Behav. 2016;20(1):29–50. doi: 10.1007/s10461-015-1164-1. [DOI] [PubMed] [Google Scholar]
- 11.Fazeli P, Turan JM, Budhwani H, et al. Moment-to-moment within-person associations between acts of discrimination and internalized stigma in people living with HIV: An experience sampling study. Stigma Health. 2016 doi: 10.1037/sah0000051. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cox WT, Abramson LY, Devine PG, Hollon SD. Stereotypes, prejudice, and depression the integrated perspective. Perspect Psychol Sci. 2012;7(5):427–49. doi: 10.1177/1745691612455204. [DOI] [PubMed] [Google Scholar]
- 13.Batey DS, Whitfield S, Mulla M, et al. Adaptation and implementation of an intervention to reduce HIV-related stigma among healthcare workers in the United States: Piloting of the FRESH workshop. AIDS Patient Care STDS. 2016;30(11):519–527. doi: 10.1089/apc.2016.0223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stringer KL, Turan B, McCormick L, et al. HIV-related stigma among healthcare providers in the Deep South. AIDS Behav. 2016;20(1):115–125. doi: 10.1007/s10461-015-1256-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sayles JN, Ryan GW, Silver JS, et al. Experiences of social stigma and implications for healthcare among a diverse population of HIV positive adults. J Urban Health. 2007;84(6):814. doi: 10.1007/s11524-007-9220-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zukoski AP, Thorburn S. Experiences of stigma and discrimination among adults living with HIV in a low HIV-Prevalence context: A qualitative analysis. AIDS Patient Care STDs. 2009;23(4):267–276. doi: 10.1089/apc.2008.0168. [DOI] [PubMed] [Google Scholar]
- 17.Davtyan M, Farmer S, Brown B, et al. Women of color reflect on HIV-related stigma through PhotoVoice. J Assoc Nurses AIDS Care. 2016;27(4):404–418. doi: 10.1016/j.jana.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 18.Holmes JG. Interpersonal expectations as the building blocks of social cognition: An interdependence theory perspective. Pers Relatsh. 2002;9(1):1–26. [Google Scholar]
- 19.Gaston GB, Alleyne-Green B. The impact of African Americans’ beliefs about HIV medical care on treatment adherence: a systematic review and recommendations for interventions. AIDS Behav. 2013;17(1):31–40. doi: 10.1007/s10461-012-0323-x. [DOI] [PubMed] [Google Scholar]
- 20.Flickinger TE, Saha S, Moore RD, et al. Higher quality communication and relationships are associated with improved patient engagement in HIV care. J Acquir Immune Defic Syndr. 2013;63(3):362. doi: 10.1097/QAI.0b013e318295b86a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schneider J, Kaplan SH, Greenfield S, et al. Better physician-patient relationships are associated with higher reported adherence to antiretroviral therapy in patients with HIV infection. J Gen Intern Med. 2004;19(11):1096–1103. doi: 10.1111/j.1525-1497.2004.30418.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Visser MJ, Makin JD, Lehobye K. Stigmatizing attitudes of the community towards people living with HIV/AIDS. J Community Appl Soc Psychol. 2006;16(1):42–58. [Google Scholar]
- 23.Varni SE, Miller CT, McCuin T, Solomon S. Disengagement and engagement coping with HIV/AIDS stigma and psychological well-being of people with HIV/AIDS. J Soc Clin Psychol. 2012;31(2):123–150. doi: 10.1521/jscp.2012.31.2.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Miller CT, Varni SE, Solomon SE, DeSarno MJ, Bunn JY. Macro-level implicit HIV prejudice and the health of community residents with HIV. Health Psychol. 2016;35(8):807–815. doi: 10.1037/hea0000314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lu M, Safren SA, Skolnik P, et al. Optimal recall period and response task for self – reported HIV medication adherence. AIDS Behav. 2008;12:86–94. doi: 10.1007/s10461-007-9261-4. [DOI] [PubMed] [Google Scholar]
- 26.Feldman B, Fredericksen R, Crane P, et al. Evaluation of the single-item self-rating adherence scale for use in routine clinical care of people living with HIV. AIDS Behav. 2013;17(1):307–318. doi: 10.1007/s10461-012-0326-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thompson MA, Mugavero MJ, Amico KR, et al. Guidelines for improving entry into and retention in care and antiretroviral adherence for persons with HIV: evidence-based recommendations from an International Association of Physicians in AIDS Care panel. Ann Intern Med. 2012;156(11):817–833. doi: 10.7326/0003-4819-156-11-201206050-00419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bunn JY, Solomon SE, Miller C, et al. Measurement of stigma in people with HIV: A reexamination of the HIV Stigma Scale. AIDS Educ Prev. 2007;19(3):198–208. doi: 10.1521/aeap.2007.19.3.198. [DOI] [PubMed] [Google Scholar]
- 29.Nyblade L, Jain A, Benkirane M, et al. A brief, standardized tool for measuring HIV- related stigma among health facility staff: results of field testing in China, Dominica, Egypt, Kenya, Puerto Rico and St. Christopher & Nevis. J Acquir Immune Defic Syndr. 2013;16(3 Suppl 2):18718. doi: 10.7448/IAS.16.3.18718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rosenberg M. Society and the adolescent self-image. Princeton, NJ: Princeton University Press; 1965. [Google Scholar]
- 31.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Folkman S, Lazarus RS. If it changes it must be a process: study of emotion and coping during three stages of a college examination. J Pers Soc Psychol. 1985;48(1):150. doi: 10.1037//0022-3514.48.1.150. [DOI] [PubMed] [Google Scholar]
- 33.Payne TJ, Andrew M, Butler KR, et al. Psychometric evaluation of the interpersonal support evaluation list–short form in the ARIC study cohort. SAGE Open. 2012;2(3):2158244012461923. [Google Scholar]
- 34.Hall MA, Zheng B, Dugan E, et al. Measuring patients’ trust in their primary care providers. Med Care Res Rev. 2002;59(3):293–318. doi: 10.1177/1077558702059003004. [DOI] [PubMed] [Google Scholar]
- 35.Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York: Guilford Press; 2013. [Google Scholar]
- 36.Hayes AF. Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Commun Monogr. 2009;76(4):408–420. [Google Scholar]
- 37.MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7(1):83. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nyblade N, Stangl A, Weiss E, et al. Combating HIV stigma in health care settings: what works? JIAS. 2009;12(15) doi: 10.1186/1758-2652-12-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Frye V, Paige MQ, Gordon S, et al. Developing a community-level anti-HIV/AIDS stigma and homophobia intervention in New York city: The project CHHANGE model. Eval Program Plann. 2017 Aug;63:45–53. doi: 10.1016/j.evalprogplan.2017.03.004. [DOI] [PubMed] [Google Scholar]


