Abstract
Berberine is an isoquinoline alkaloid plant extract that is widely available as a dietary supplement in the United States and has demonstrated efficacy in the treatment of type 2 diabetes mellitus and dyslipidemia. Because of its increased use and purported pharmacological properties, potential variations in product quality could pose a barrier to berberine’s safety and effectiveness in clinical practice. Thus, this study evaluated the potency of dietary supplements containing berberine available in the U.S. commercial market. Fifteen unique dietary supplements containing berberine were purchased through U.S. dietary supplement vendors. For each product, berberine was extracted from 3 unique capsules and analyzed by ultra-high-performance liquid chromatography tandem mass spectrometry. Percentage content based on the product label claim was determined for each product. The average berberine content across the products was found to be 75% ± 25% of the product label claim, with product potency ranging from ±33% to 100%. Nine of the 15 tested products (60%) failed to meet the potency standards of 90% to 110% of labeled content claim, as commonly required of pharmaceutical preparations by the U.S. Pharmacopeial Convention. Evaluation of the relationship between product cost and the measured potency failed to demonstrate an association between quality and cost. Variability in product quality may significantly contribute to inconsistencies in the safety and effectiveness of berberine. In addition, the quality of the berberine product cannot be inferred from its cost.
Keywords: berberine, dietary supplement, natural product, potency
Introduction
Berberine is an isoquinoline plant alkaloid (Figure 1) that has been used for centuries in traditional Chinese medicine for its antidiabetic and anti-inflammatory properties to treat a host of disorders (Sha et al., 2013). The agent is derived from the roots, stems, rhizomes, and bark of various plants including Berberis vulgaris (barberry), Berberis aristata (tree turmeric), and Hydrastis canadensis (goldenseal) (Singh and Mahajan, 2013). Berberine has a distinct yellow color and fluorescence, allowing for utility as a dye in the textile industry and as a histology stain (Haji, 2010; Enerbäck, 1974). More recently, berberine has become available in the United States as a dietary supplement, individually or in combination with other supplements, and continues to be increasingly used as a complementary and alternative medicine.
Figure 1.
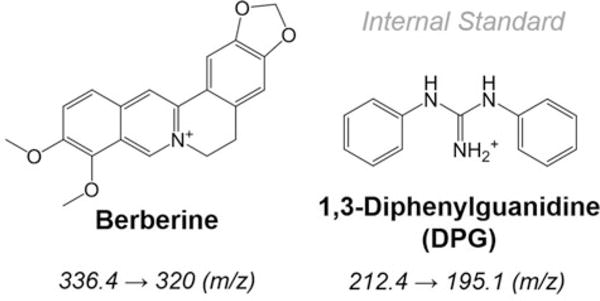
Chemical structures of berberine and 1,3-diphenylguanidine (DPG). Similar in structure to berberine, DPG was used as an internal standard for the UHPLC-MS/MS based quantification of berberine in 15 dietary supplements commercially available in the US market. The mass transitions, used to detect the two analytes by mass spectrometry, are provided.
Compared to most dietary supplements, berberine is well studied in humans and animal models. Multiple pharmacological properties have been identified, resulting in numerous clinical applications, including antimicrobial, anti-inflammatory, antitumor, blood pressure lowering, weight loss, and reductions in low-density lipoprotein cholesterol (LDL-C) and glucose parameters (Pirillo and Catapano, 2015). Because of the latter, there has been considerable interest in the utilization of berberine in the treatment of common metabolic disorders such as type 2 diabetes mellitus (DM) and dyslipidemia. Several mechanisms are responsible for the cholesterol- and glucose-lowering effects, many of which are similar to those observed with prescription medications. For example, berberine has been shown to increase hepatic LDL receptor expression (Kong et al., 2004) and, of particular interest, limit the expression and amount of proprotein convertase subtilisin/kexin type 9 (PCSK9) secreted by hepatic cells (Cameron et al., 2008), both of which are key elements for lowering LDL-C and common properties of HMG CoA reductase inhibitors (statins) and the recently approved PCSK9-inhibitors, respectively (Krahenbuhl, Pavik-Mezzour, and von Eckardstein, 2016). Similarly, berberine appears to improve glucose homeostasis via multiple mechanisms. In diabetic animals, berberine induces glucagon-like peptide 1 (GLP1) (Lu et al., 2009) and increases glucose uptake by enhancing the activity of glucose transporters (GLUT) 1 and 4 (Kim et al., 2007). Such pharmacological activity is related to that noted for the GLP-1 receptor agonists (e.g., liraglutide) and metformin, respectively (Wright and Tylee, 2016).
Small clinical trials performed mostly in China have evaluated the effect of berberine on key lipid and glucose markers. Overall, ∼1,000–1,500 mg of berberine daily resulted in significant reductions of LDL-C (∼25%) and HbA1c (∼1%–2%) during the 8- to 12-week studies (Pirillo and Catapano, 2015). No serious adverse effects were reported; however, other data indicate gastrointestinal complaints are common with berberine (Pang et al., 2015). Other concerns with the agent include the potential for drug interactions. Berberine is a substrate for many important transport and metabolic pathways, including P-glycoprotein (P-gp), organic cation transporters 1 (OCT1) and 2 (OCT2), and the cytochrome P450 (CYP) 3A4 isoenzyme (Pirillo and Catapano, 2015). Notable medications that are substrates for these pathways include metformin (OCT2), cyclosporine (P-gp), and for the CYP3A4 enzyme, certain statins (e.g., lovastatin, simvastatin), antiretroviral agents (e.g., saquinavir, darunavir), and immunosuppressants (e.g., sirolimus, tacrolimus, cyclosporine) (Kellick et al., 2014; Pirillo and Catapano, 2015). Thereby, berberine may increase the systemic exposure of many commonly prescribed medications and predispose patients to adverse effects.
Overall, berberine has broad potential for clinical application and a reasonably short-term safety profile, but long-term data are lacking and the agent has the propensity for clinically relevant drug interactions (Pirillo and Catapano, 2015). In addition, the U.S. Food and Drug Administration (FDA) has limited oversight of dietary supplements (Brown, 2016). As such, we sought to formally evaluate multiple preparations for clinical utilization. Because of previously documented variations in quality among dietary supplements, we expect variability in product potency to represent a significant barrier to the safe and effective use of berberine in clinical practice (Srinivasan, 2006). Therefore, the aim of this study was to evaluate the quality of commercially available preparations of berberine through the determination of potency among berberine preparations available in the United States.
Materials and methods
Product selection
An Internet search for commercial products advertising 400 mg to 500 mg per capsule of berberine yielded 15 available preparations. Any formulation containing additional active ingredients was excluded from the study. All products were purchased online through common retailers (e.g., Amazon) in May 2016, and analysis was completed by July 2016. At the time of analysis, none of the products tested had reached their expiration date according to the product labeling.
Sample extraction
The contents of three capsules from each preparation were individually weighed. The weight of the capsule contents was determined by subtracting the weight of the empty capsule from the weight of the filled capsule on a Mettler-Toledo XS3DU microbalance (Columbus, OH). A sample from each capsule containing approximately 5 mg of berberine was added to a 50 mL conical vial containing 50 mL of ACS- (American Chemical Society)grade methanol containing 0.1 mg/mL of the internal standard 1,3-diphenylguanidine (DPG) (Figure 1), yielding a berberine concentration of approximately 0.1 mg/mL. The samples were sonicated for 15 minutes, followed by vortex shaking for 30 seconds, and finally were centrifuged at 1,500 rcf for 5 minutes. The resulting supernatant was further diluted 1:100 in ACS-grade methanol, and the sonication, vortexing, and centrifugation steps were repeated. Finally, the resulting supernatant was diluted 1:100 in 75:25 (v/v) water (H2O):acetonitrile (ACN) containing 0.1% (v/v) formic acid (FA). For determination of extraction efficiency, 500 mg cinnamon dietary supplement capsules purchased from CVS Health (Woonsocket, RI, USA) were used as a blank matrix, and berberine at concentrations ranging from 0.01 to 80 mg/mL and DPG at 0.1 mg/mL were extracted and compared to nonextracted standards.
Sample analysis
Standard stocks of berberine (0.01–0.2 mg/mL) were made in methanol using the US Pharmacopeial (USP) reference standard (Rockville, MD, USA). The standard stocks were diluted 1:100 into methanol, then 1:100 into 75:25 (v/v) H2O:ACN containing 0.1% (v/v) FA, as outlined in the preceding section. The calibration standards and the extracted and diluted berberine samples were analyzed by ultra-high-performance liquid chromatography tandem mass spectrometry (UHPLC-MS/MS) (Zhang et al., 2014). Mobile phase A consisted of 0.1% FA in H2O and mobile phase B consisted of 0.1% FA in ACN with a flow rate of 0.4 mL/min. The analytes were resolved on a Phenomenex (Torrance, CA) Luna Omega C18 column (100 × 2.1 mm, 1.6 μm, 100Å) at 25°C using the following linear gradient: isocratic hold for 0.5 minutes at 25% mobile phase B, 98% B at 5.5 minutes, and 25% B at 5.6 minutes with a re-equilibration time of 1 minute. Analytes were detected on a Waters (Milford, MA) Quattro Premier XE dual quadrupole mass spectrometer with an electrospray ionization source operated in positive ion mode and controlled by Waters Mass Lynx 4.1 software with the following settings: source/desolvation temperatures of 100°C/450°C, and source/desolvation N2 gas flow at 50 L/hr/650 L/hr. Multiple-reaction monitoring, with argon collision gas at 0.16 mL/min, was used to detect both berberine (336.4→320.0) and DPG (212.4→195.1). Optimal cone voltage/collision energy settings of 55 V/35 V and 41 V/25 V were used for berberine and DPG, respectively. The MS peaks were integrated using QuanLynx software (version 4.1, Waters Corp., Milford, MA). Sample concentrations were determined by interpolation of the analyte/internal standard peak area ratios calculated from a 7-point calibration curve ranging from 1 to 20 ng/mL of berberine.
Statistical analysis
The resulting potency data were found to display a normal distribution and were analyzed by standard parametric statistical testing. Comparison of product potency based on cost was determined by unpaired t-test analysis and by Pearson’s correlation analysis. A p value less than .05 was considered statistically significant. Data analysis was conducted using JMP software v11 from SAS Institute Inc. (Cary, NC).
Results
Berberine dietary supplements were purchased online from 15 unique manufacturers (Table 1). All of the preparations contained berberine as the sole listed active ingredient. The labeled berberine content for the preparations was either 400 mg or 500 mg per capsule. The average (± SD) monthly cost based on a dose of 800 to 1,000 mg/day for the preparations was $21.97 ± $9.18 and ranged from $8.48 to $47.40. All of the preparations were analyzed prior to the labeled expiration date.
Table 1.
Fifteen commercial preparations of berberine available in the United States tested for product potency.
| Product name | Manufacturer | Labeled content (mg) | Monthly cost ($) |
|---|---|---|---|
| 1. Berberine 500 mg | Vital Nutrients | 500 | 47.40 |
| 2. Organic Berberine HCl | Pura Organics | 500 | 24.95 |
| 3. Berberine-500 | Thorne Research | 500 | 32.60 |
| 4. Berberine Metabolic Support | Integrative Therapeutics | 500 | 27.00 |
| 5. Pure Berberine | Lean Nutraceuticals | 500 | 21.77 |
| 6.Berberine 500 mg | Double Wood | 500 | 19.95 |
| 7. Berberine | Vitacost | 500 | 15.35 |
| 8. Berberine HCL | Pure Science | 500 | 22.40 |
| 9. Activated Berberine | Nutritional Concepts | 400 | 13.35 |
| 10. Berberine 1,000 | Only Natural | 500 | 21.83 |
| 11. Berberine Ultra Complex | LongLifeNutri | 500 | 21.97 |
| 12. Berberine | Swanson | 400 | 8.48 |
| 13. Berberine HCl | Biotics Research Corp | 500 | 25.80 |
| 14. WellBetX Berberine 500 mg | Natural Factors | 500 | 27.95 |
| 15. Dr. Whitaker Clinical Grade Berberine | Healthy Directions | 500 | 14.93 |
To analyze the berberine content in each product, a UHPLC-MS/MS assay was developed for berberine using DPG as the internal standard (Figure 1). The berberine USP reference standard was used to prepare the calibration standards for the assay. A capsule formulation of cinnamon was used as the matrix background for the methanol-based extraction procedure and yielded an average (± SD) extraction efficiency of 95% ± 7%. The analysis run time was 6.6 minutes and resulted in a good baseline separation of DPG and berberine as illustrated for a matrix extracted and diluted standard solution containing 10 ng/mL each of DPG and berberine (Figure 2A). The ratio of the peak area of berberine and DPG was used to construct the standard calibration curve (Figure 2B). The average coefficient of variation for the analytical assay was 5.9%.
Figure 2.
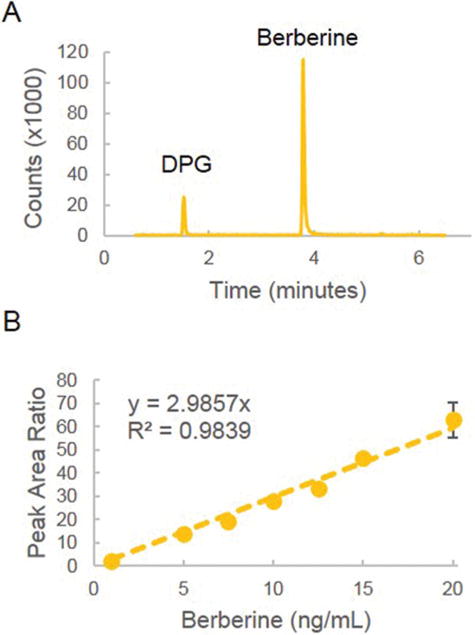
Quantification of berberine by UHPLC-MS/MS. (A) A representative multiple-reaction-monitoring (MRM) chromatogram for berberine (336.4→320.0) and 1,3-diphenylguanidine (DPG) (212.4→195.1) detected in matrix extracted and diluted berberine standard at a final concentration of 10 ng/mL berberine and 10 ng/mL DPG. (B) The 7-point calibration curve was plotted as the concentration of berberine versus the peak area ratio of berberine and DPG and was fitted to a weighted (1/x), linear least-squares regression.
Three capsules from each preparation were extracted individually and assayed for berberine content. Among the products tested, the average (± SD) content of berberine was 75% ± 25% of the label claim, and the content ranged from 33% to 100% of the expected dose (Figure 3). Of the products tested, 60% had an average berberine content of less than 90% of the label claim. Interestingly, several of the products failing to achieve 90% potency had label claims of manufacturing under Good Manufacturing Practice conditions in Food and Drug Administration inspected facilities, as well as guarantees of purity and potency.
Figure 3.
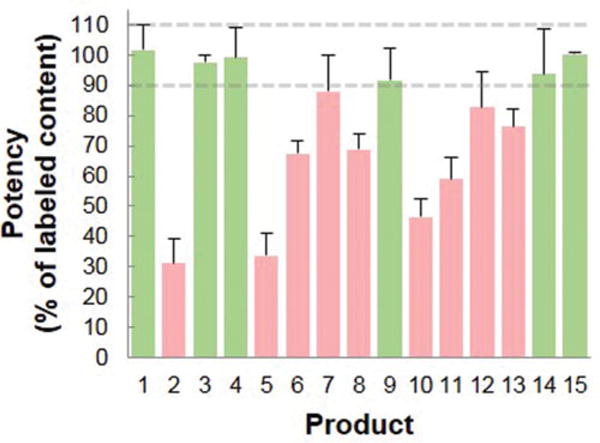
Percentage of berberine content based on the label claim in commercial preparations of berberine. The average (± SD) of the percentage of berberine based on the label claim for each of the 15 commercially available berberine products is presented. The average (± SD) of the percentage of berberine based on the label claim for each of the 15 commercially available products listed in Table 1 is presented. The products in green are those with an average berberine content between 90% and 110% of the label claim. The products in red are those with an average berberine content less than 90% of the label claim.
Analysis of product quality based on the average monthly cost failed to yield a significant relationship between quality and cost. The average (±SD) cost of products containing at least 90% of the labeled berberine content was not significantly ± different from products failing to meet the 90% potency standard ($27.21 ± $12.49 vs. $20.28 ± 5.34, respectively, p =.25). Similarly, Pearson’s pairwise analysis of potency, based on the label claim, and product monthly cost failed to yield a significant relationship between cost and quality (r = .17, p = .53).
Discussion
Our results demonstrate marked variability in the content of berberine among products available from U.S. manufacturers. Further, variation in quality was not associated with variability in product cost. Potency standards set forth by the USP Convention commonly require pharmaceutical preparations contain between 90% and 110% of the labeled content claim. Despite increased regulatory oversight by the FDA, dietary supplements continue to lack potency standards, resulting in significant product quality variations among commercially available preparations (Gershwin et al., 2010; Sarma, Giancaspro, and Venema, 2016). The final guidance on the Current Good Manufacturing Practices (cGMP) for dietary supplements issued by the FDA in 2007 required that manufacturers establish and document their own quality-control standards (Marcus, 2016). However, these regulations failed to include specific definitions regarding the purity and potency of the manufactured product. As a result, compliance with cGMP standards does not necessarily translate to the achievement of conventional product potency standards, as demonstrated in this work. Together, these findings highlight a continued shortfall in the dietary supplement industry to ensure product quality. The potential risks of these shortfalls are expected to become increasingly evident as variation in product quality results in measureable impact on the effectiveness and toxicity of these products. This translates clinically to inconsistencies in measures of disease response to therapy, such as LDL-C and HbA1c, and the presence or absence of common dose-dependent adverse effects (e.g., gastrointestinal complaints). This may become more unpredictable if patients are switching between berberine products. Since most of the products that we analyzed contained less than the stated label amount, a subtherapeutic clinical response would likely be expected.
A number of other factors must also be discussed regarding the utilization of berberine in clinical practice. Small studies, performed primarily in China, indicate that berberine is an effective agent for significantly reducing HbA1c and LDL-C. Comparable studies have not been performed in the United States; however, various favorable characteristics make berberine attractive for the clinical treatment of type 2 DM and dyslipidemia. For example, patients typically have a positive view of complementary and alternative medicine and may be more willing to add berberine to their regimen than they are to add standard agents (Vincent and Furnham, 1996). Other notable attributes include lower cost than many prescription medications (< $25/month), similar pharmacology to established DM and lipid therapies (e.g., GLP-1 agonists, metformin, statins) (Pang et al., 2015; Pirillo and Catapano, 2015), and presumed safety since berberine has been utilized as a traditional Chinese medicine for centuries. Conversely, few studies have established the efficacy of berberine outside of China, and although the short-term clinical trials did not report serious adverse effects, little is known regarding long-term use. Further, berberine is a substrate of common metabolic pathways and has the potential for clinically relevant drug interactions. Finally, other studies have provided mixed results regarding safety, with animal data suggesting an increase in hepatic tumors (Dunnick et al., 2011), while other studies, including human cell models, indicate potential anticancer benefit (Diogo et al., 2011). Nevertheless, well-designed, long-term randomized controlled trials are needed to better assess safety and efficacy and determine the impact of berberine on clinical outcomes.
There are limitations to our study. Primarily, we analyzed the berberine content of one individual bottle from each manufacturer. A more comprehensive approach would involve analyzing the content of multiple bottles from the same manufacturer with different lot numbers, accounting for any batch-to-batch variability.
Conclusion
Berberine is an emerging dietary supplement in the United States with multiple pharmacological properties and broad potential for clinical application. However, there is significant variation in product content among the majority of U.S. preparations analyzed, thereby hindering the agent’s safety and effectiveness. In addition, the quality of the berberine product should not be inferred from its cost. Presently, clinicians should be cautious when recommending berberine for any purported therapeutic treatment.
Acknowledgments
Funding
The work was supported in part by the National Institute of General Medical Sciences [P20GM103549 and P30GM118247].
Biographies
Ryan S. Funk, PharmD, PhD, is Assistant Professor of Pharmacy Practice at the University of Kansas School of Pharmacy. He holds a joint appointment within the Department of Pharmacology, Toxicology and Therapeutics at the University of Kanas Medical Center. Dr. Funk received both his Pharm.D. and Ph.D. in Pharmaceutical Chemistry at the University of Kansas. Subsequently, he completed an NICHD sponsored T32 training program in Pediatric Clinical Pharmacology at Children’s Mercy-Kansas City under the direction of J. Steven Leeder. His current research focuses on molecular mechanisms of variability in drug response to immunologically active agents in the treatment of pediatric autoimmune disease, but has maintained an academic interest in drug formulation and analysis.
Rakesh K. Singh, PhD, is a Senior Scientist in the Department of Pharmacy Practice at the University of Kansas School of Pharmacy. Dr. Singh received his B.S. in Pharmaceutical Sciences from the Birla Institute of Technology in India, and his Ph.D. in Pharmacology and Toxicology from the University of Kansas. He completed a postdoctoral fellowship at the University of Illinois at Chicago College of Medicine and is currently studying the biochemical pharmacology of methotrexate in autoimmune arthritis. His current research seeks to understand the role of NAD metabolism by nicotinamide phosphoribosyltranserase and signaling via the JAK/STAT pathway impact response to methotrexate.
Robert D. Winefield, PhD, is Research Assistant Professor of Pharmacology, Toxicology and Therapeutics and the Director of the Analytical Core laboratory at the University of Kansas Medical Center. Dr. Winefield received his Ph.D. degree from Massey University in New Zealand. He completed postdoctoral training at the University of Kansas in the fields of molecular biology and bioanalytical chemistry. His current research efforts are focused on the development of custom analytical methods using UHPLC-MS/MS.
Sylvie E. Kandel, PhD, is a Senior Scientist at the University of Kansas Medical Center. She obtained a Ph.D. in Biochemistry and Molecular Biology in the Pinot laboratory at the Institut de Biologie Moléculaire de Plantes with subsequent postdoctoral training in the laboratory of Ortiz de Montellano at the University of California, San Francisco. Following four years of industry-based pre-clinical drug development research on drug metabolism and mass spectrometry at Sekisui XenoTech, Dr. Kandel joined the University of Kansas Medical center and currently divides her time between the laboratory of Dr. Jed Lampe and the Analytical Core laboratory. In the Lampe laboratory, her current research seeks to characterize the role of CYP3A7 in drug metabolism and toxicity in neonates. Within the Analytical Core laboratory, she provides analytical support to help develop small molecule analytical methods for users of the core lab.
Janelle F. Ruisinger, PhD, is Clinical Professor of Pharmacy Practice at the University of Kansas School of Pharmacy. Dr. Ruisinger earned her Pharm.D. degree from the University of Kansas, then completed a residency with an emphasis on community care at The Ohio State University College of Pharmacy. She is also a Clinical Pharmacist in the KU Medical Center Atherosclerosis and LDL-Apheresis Center which serves as her practice site and primary source for her practice based research.
Patrick M. Moriarty, MD, is Professor of Internal Medicine and Division Director of Clinical Pharmacology at the University of Kansas Medical Center. Dr. Moriarty earned his M.D. at the University of Rome and completed his medical residency at the University of Kansas Medical Center. He serves as the Director of the Atherosclerosis and LDL-Apheresis Center at the University of Kansas Medical Center. His research is focused on atherosclerosis, vascular inflammation and blood rheology.
James M. Backes, PharmD, is Associate Dean for Clinical and Medical Center Affairs at the University of Kansas School of Pharmacy. Dr. Backes earned his B.S. in Pharmacy and Pharm.D. from Creighton University. He is a professor in the Pharmacy Practice and Internal Medicine departments and serves as the Assistant Director of the Atherosclerosis and LDL-Apheresis Center at the University of Kansas Medical Center. His research focus includes the safety and efficacy of lipid-altering agents and limiting the associated adverse events. Previously studied agents include policosanol, almonds, niacin, fibrates, statins (standard and intermittently dosed), apple-pectin, vitamin D, fish oil, krill oil, and red yeast rice.
Footnotes
Declaration of interest
The authors declare no conflicts of interest. The authors alone are responsible for the content and writing of the article.
Color versions of one or more of the figures in the article can be found online at www.tandfonline.com/ijds.
References
- Brown AC. An overview of herb and dietary supplement efficacy, safety and government regulations in the United States with suggested improvements. Part 1 of 5 series [published online ahead of print November 3, 2016] Food Chem Toxicol. doi: 10.1016/j.fct.2016.11.001. [DOI] [PubMed] [Google Scholar]
- Cameron JT, Ranheim MA, Kulseth TP, Leren TP, Berge KE. Berberine decreases PCSK9 expression in HepG2 cells. Atherosclerosis. 2008;201:266–273. doi: 10.1016/j.atherosclerosis.2008.02.004. [DOI] [PubMed] [Google Scholar]
- Diogo CV, Machado NG, Barbosa IA, Serafim TL, Burgeiro A, Oliveira PJ. Berberine as a promising safe anti-cancer agent—is there a role for mitochondria? Curr Drug Targets. 2011;12:850–859. doi: 10.2174/138945011795528930. [DOI] [PubMed] [Google Scholar]
- Dunnick JK, Singh B, Nyska A, Peckham J, Kissling GE, Sanders JM. Investigating the potential for toxicity from long-term use of the herbal products, goldenseal and milk thistle. Toxicol Pathol. 2011;39:398–409. doi: 10.1177/0192623310394211. [DOI] [PubMed] [Google Scholar]
- Enerbäck L. Berberine sulphate binding to mast cell polyanions: a cytofluorometric method for the quantitation of heparin. Histochemistry. 1974;42:301–313. doi: 10.1007/BF00492678. [DOI] [PubMed] [Google Scholar]
- Gershwin ME, Borchers AT, Keen CL, Hendler S, Hagie F, Greenwood MR. Public safety and dietary supplementation. Ann N Y Acad Sci. 2010;1190:104–117. doi: 10.1111/j.1749-6632.2009.05270.x. [DOI] [PubMed] [Google Scholar]
- Haji A. Functional dyeing of wool with natural dye extracted from Berberis vulgaris wood and Rumex Hymenosepolus root as biomordant. Iranian J Chem Chem Eng. 2010;29:55–60. [Google Scholar]
- Kellick KA, Bottorff M, Toth PP, The National Lipid Association’s Safety Task Force A clinician’s guide to statin drug-drug interactions. J Clin Lipidol. 2014;8:S30–S46. doi: 10.1016/j.jacl.2014.02.010. [DOI] [PubMed] [Google Scholar]
- Kim SH, Shin EJ, Kim ED, Bayaraa T, Frost SC, Hyun CK. Berberine activates GLUT1-mediated glucose uptake in 3T3-L1 adipocytes. Biol Pharm Bull. 2007;30:2120–2125. doi: 10.1248/bpb.30.2120. [DOI] [PubMed] [Google Scholar]
- Kong W, Wei J, Abidi P, Lin M, Inaba S, Li C, et al. Berberine is a novel cholesterol-lowering drug working through a unique mechanism distinct from statins. Nat Med. 2004;10:1344–1351. doi: 10.1038/nm1135. [DOI] [PubMed] [Google Scholar]
- Krahenbuhl S, Pavik-Mezzour I, von Eckardstein A. 2016 Unmet needs in LDL-C lowering: when statins won’t do! Drugs. 2016;76:1175–1190. doi: 10.1007/s40265-016-0613-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu SS, Yu YL, Zhu HJ, Liu XD, Liu L, Liu YW, et al. Berberine promotes glucagon-like peptide-1 (7–36) amide secretion in streptozotocin-induced diabetic rats. J Endocrinol. 2009;200:159–165. doi: 10.1677/JOE-08-0419. [DOI] [PubMed] [Google Scholar]
- Marcus DM. 2016 Dietary supplements: What’s in a name? What’s in the bottle? Drug Testing Anal. 2016;8:410–412. doi: 10.1002/dta.1855. [DOI] [PubMed] [Google Scholar]
- Pang B, Zhao LH, Zhou Q, Zhao TY, Wang H, Gu CJ, et al. Application of berberine on treating type 2 diabetes mellitus. Int J Endocrinol. 2015:905749. doi: 10.1155/2015/905749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirillo A, Catapano AL. Berberine, a plant alkaloid with lipid- and glucose-lowering properties: from in vitro evidence to clinical studies. Atherosclerosis. 2015;243:449–461. doi: 10.1016/j.atherosclerosis.2015.09.032. [DOI] [PubMed] [Google Scholar]
- Sarma N, Giancaspro G, Venema J. Dietary supplements quality analysis tools from the United States Pharmacopeia. Drug Test Anal. 2016;8:418–423. doi: 10.1002/dta.1940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sha W, Zhang W, Huang W, Zhou M, Niu J, Jiang H, et al. An ancient Chinese herb berberine: new research in diabetes mellitus. Int J Integr Med. 2013;1:1–3. [Google Scholar]
- Singh IP, Mahajan S. Berberine and its derivatives: a patent review (2009–2012) Expert Opin Ther Pat. 2013;23:215–231. doi: 10.1517/13543776.2013.746314. [DOI] [PubMed] [Google Scholar]
- Srinivasan VS. Challenges and scientific issues in the standardization of botanicals and their preparations. United States Pharmacopeia’s dietary supplement verification program—a public health program. Life Sci. 2006;78:2039–2043. doi: 10.1016/j.lfs.2005.12.014. [DOI] [PubMed] [Google Scholar]
- Vincent C, Furnham A. Why do patients turn to complementary medicine? An empirical study. Br J Clin Psychol. 1996;35(Pt 1):37–48. doi: 10.1111/j.2044-8260.1996.tb01160.x. [DOI] [PubMed] [Google Scholar]
- Wright JJ, Tylee TS. Pharmacologic therapy of type 2 diabetes. Med Clin North Am. 2016;100:647–663. doi: 10.1016/j.mcna.2016.03.014. [DOI] [PubMed] [Google Scholar]
- Zhang Z, Li Q, Li Q, Du S, Zhou Y, Lv C, et al. Simultaneous determination of nineteen major components in Qi She Pill by ultra-high-performance liquid chromatography-tandem mass spectrometry. Acta Pharm Sin B. 2014;4:384–393. doi: 10.1016/j.apsb.2014.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]


