Abstract
Purpose
Health and administrative systems are facing spatial clustering in chronic diseases such as diabetes. This study explores how geographic distribution of diabetes in the U.S. is associated with socioeconomic and built environment characteristics and health-relevant policies.
Methods
We compiled nationally representative county-level data from multiple data sources. We standardized characteristics to a mean=0 and a standard deviation=1 and modeled county-level age-adjusted diagnosed diabetes incidence in 2013 using 2-level hierarchical linear regression.
Results
Incidence of age-standardized diagnosed diabetes in 2013 varied across US counties (n=3,109), ranging from 310 to 2,190 new cases /100,000, with an average of 856.4/100,000. Socio-economic and health-related characteristics explained ~42% of the variation in diabetes incidence across counties. After accounting for other characteristics, counties with higher unemployment, higher poverty and longer commutes had higher incidence rates than counties with lower levels. Counties with more exercise opportunities, access to healthy food, and primary care physicians had fewer diabetes cases.
Conclusions
Features of the socioeconomic and built environment were associated with diabetes incidence; identifying the salient modifiable features of counties can inform targeted policies to reduce diabetes incidence.
Keywords: Diabetes, Disease incidence, Geographic variation, Social determinants of health, Built environment, Health disparities
Type 2 diabetes mellitus is a serious, common, and potentially preventable condition that imposes large health and economic burdens in the United States. In 2014, 29.1 million people, or 9.3% of the population, had diabetes; the proportion of people with diabetes is projected to increase by 54% between 2015 and 2030.(1, 2)
Health and administrative systems are facing spatial clustering in chronic diseases such as diabetes. In the U.S, the rate of occurrence of diabetes shows marked spatial patterning within and between states.(3-5) In 2010, high prevalence of diagnosed diabetes was concentrated primarily in 644 counties within 15 southern states.(4) The prevalence was 40% higher in this ‘diabetes belt’ (11.7%; 95% CI: 11.4%-12.0%) compared to the average of all other U.S. counties (8.5%; 95% CI: 8.3%-8.6%). In 2012, the overall county-level incidence rate of diagnosed diabetes ranged from ≤60/100,000 population to ≥142/100,000 population.(6)
While the focus of many ongoing health interventions has been on individual-level behavior change and medical care, features of the contexts in which people are born, live, work, and age may also be relevant to diabetes risks.(7-9) Geographic variation in health behaviors and environmental factors, for example, food markets, are among the hypothesized contributors to the spatial patterning of diabetes in the U.S.(4, 7, 10) In addition, collective social advantage (e.g., median income) and disadvantage (e.g., proportion unemployed) may play a role in generating environmental conditions that are related to population health, both independently of individuals’ health behaviors and by guiding individuals’ health behaviors. (11-14)
Examining how county-level social and physical characteristics relate to county-level diabetes incidence may provide a clearer understanding of the factors contributing to the high levels of diabetes incidence in the U.S. Identifying and addressing these county-level factors may help to reduce disparities in health, which is a Health People 2020 overarching goal.(15)
Using the most recent small-area county-level estimates of diabetes incidence in the U.S., we investigated which potentially modifiable county-level features were associated with diabetes incidence across U.S. counties. This study builds on recent findings describing geographical variation in diabetes prevalence, incidence, and mortality by identifying county-level characteristics associated with these geographical variations. This approach may help the development, implementation, and evaluation of interventions aimed at reducing disparities in diabetes burden.
RESEARCH DESIGN AND METHODS
Data Sources
We combined county-level data from multiple publically available data sources; details of the variables and data sources are discussed below and shown in Table 1. This was a secondary analysis of nationally representative, publicly available data.
Table 1.
Sources and descriptive characteristics of county-level variables
| Data Source | Quartile 1 | Quartile 3 | Coefficient of Variation | |||||
|---|---|---|---|---|---|---|---|---|
| Mean | Std Dev | Min | Max | |||||
| Diabetes incidence per 100,000, age-adjusted, 2013 | (6) | 856.4 | 233.5 | 700 | 1000 | 27.3 | 310 | 2190 |
| Population (1000) 2009-2013 | (17) | 100.2 | 318.1 | 11.4 | 68.11 | 317.6 | 0.5 | 9893 |
| Social and economic features | ||||||||
| % Urban 2010 | (18) | 41.7 | 31.4 | 14.2 | 67 | 75.3 | 0 | 100 |
| Service-dependent economy 2004 | (18) | 0.5 | 0.5 | 0 | 1 | 93.4 | 0 | 1 |
| % Unemployed 2006-2010 | (19) | 23.7 | 8.4 | 17.8 | 28.7 | 35.5 | 1.7 | 63.1 |
| % Without high school education 2006-2010 | (19) | 16.9 | 7.3 | 11.4 | 21.5 | 43.4 | 0.7 | 52.1 |
| Median income 2006 ($1,000) | (20) | 40.7 | 10.5 | 33.81 | 45.02 | 25.8 | 18.7 | 100.8 |
| % In poverty 2006 | (20) | 15.4 | 6.2 | 11.1 | 18.7 | 40.3 | 2.5 | 48.5 |
| Health-related environment | ||||||||
| % with exercise opportunities 2010-2012 | (21) | 52.2 | 24.4 | 34.77 | 70.12 | 46.8 | 0 | 100 |
| Poor air quality 2004-2006 | (22) | 0.2 | 0.4 | 0 | 0 | 218.4 | 0 | 1 |
| % Long commute 2010 | (21) | 29.6 | 11.9 | 20.7 | 37.9 | 40.3 | 0 | 71.2 |
| Food environment index 2010-2011 | (21) | 7.4 | 1.2 | 6.79 | 8.21 | 16.8 | 0 | 10 |
| Primary care doctors per 100,000 population 2011 | (20) | 53.1 | 34.9 | 31.52 | 70.08 | 65.8 | 0 | 508.3 |
Notes: Data describe the mean of each county-level characteristic across the 3,109 counties analyzed.
Diabetes incidence
The outcome of interest was county-level diabetes incidence. We used county-level, age-adjusted estimates of diagnosed diabetes incidence among adults 20 years of age and older in 2013, the most recent year available at the time of analysis. Incidence estimates were computed by the Centers for Disease Control and Prevention (CDC) using multilevel Poisson regression models and data from the Behavioral Risk Factor Surveillance System (BRFSS) and the U.S Census. These county incidence estimates are publically available(6) and the methods used to produce them were previously described.(16)
County characteristics
We used several sources of data to construct profiles of the demographic, social, economic, and health characteristics of U.S. counties pertaining to the time period prior to the diabetes estimates. Within the constraints of data availability, we selected calendar years that allowed for a lag between these characteristics (exposures) and diabetes incidence in 2013 (outcome). Where possible, we selected estimates that combined data from multiple years to maximize the stability at the county-level. Our final analysis focused on fourteen county characteristics.
The two demographic characteristics were: county population size, obtained from the 2009-2013 5-Year American Community Survey of the US Census Bureau,(17) and percent of the county population that resided in an urbanized area or urban cluster in 2010 as defined by the US Census Bureau.(18) We did not include age and race/ethnicity as predictors of incidence because these variables were used to calculate CDC’s county estimates of incidence, our dependent variable.
We selected five social and economic characteristics to reflect the long-run economic circumstances of counties prior to the 2007-2008 financial crisis. A binary indicator of whether 6 the county was predominantly engaged in a service-dependent economy in 2004 was based on The Economic Research Services 2004 County Typology and obtained from the Area Health Resource File 2012-2013.(18) We obtained the 2006-2010 percent of the county population aged 16-64 years that was unemployed at any time in the past 12 months and the percent of the county population aged 24-65 years with less than high school education from the American Community Survey 5-year estimates.(19) We obtained the percent of the county population in poverty and median county income levels in 2006 from the Small Area Income and Poverty Estimates provided by the U.S. Census Bureau.(20)
We selected six measures to capture components of the health-related environment. The number of primary care physicians in 2011 from the American Hospital Association Annual Survey Database was obtained from the Area Health Resource File 2012-2013(18) and was divided by the county population to derive the number of primary care physicians per 100,000 population. We used exercise opportunities and food environment as developed by County Health Rankings & Roadmaps project.(21) We calculated the percent of the county population with exercise opportunities defined as the proportion residing within ½ mile of a park or within 1 mile (urban) or 3 miles (rural) of a recreational facility using the OneSource Global Business Browser, Delorme map data, Esri, & US Census Tigerline Files.(21) The food environment index is a composite score ranging from 1 (worst) to 10 (best) summarizing access to healthy foods and food insecurity based on data from the United States Department of Agriculture (USDA) Food Environment Atlas “Map the Meal Gap”.(21) The percent of the county population with a commute of at least 30 minutes from home to work alone was based on US Census Bureau American Community Survey Data and obtained from the County Health Rankings & Roadmaps database.(21) Finally, we included a measure of poor air quality, defined as a binary indicator of Green Book non-attainment for at least 1 of 7 criteria air pollutants in 2004-2006: 8-hour ozone, carbon monoxide, nitrogen dioxide, sulfur dioxide, particulate matter PM-10, particulate matter PM-2.5, and/or lead, obtained from the Behavioral Risk Factor Surveillance System 2006 BRFSS County Supplement.(22)
Statistical analysis
We merged data from across sources by the five-digit Federal Information Processing Standard (FIPS) code to create a single dataset of counties and county-equivalents containing all county characteristics, diabetes incidence rates, and an indicator for U.S. state. Of 3,143 U.S. counties and Washington D.C. in the merged data set, 34 counties were excluded from further analysis because they did not have data on all on county-level characteristics. The final analytic sample contained 99% of all counties.
We first described the distribution of all county characteristics and their correlations with each other and with diabetes incidence (see Appendix Table 1). We next employed hierarchical linear mixed models to estimate the association between county characteristics and diabetes incidence by specifying counties as the level-1 unit and states as a level-2 unit with a random intercept. By allowing each state to have its own intercept, county-level coefficients are expected to be robust to omitted state-level factors that influence diabetes incidence and account for clustering of data within states. To facilitate comparisons of coefficients associated with the 14 county characteristics, we standardized all independent variables to have a mean of zero and a standard deviation of one. We modeled county-level age-adjusted diagnosed diabetes incidence (new cases per 100,000 population) in 2013 using 2-level hierarchical linear regression. Multilevel models with county intercept led to 51 random effects, which are shown in Appendix Table 3.
We report bivariate (unadjusted) associations between each county characteristic and diabetes incidence and adjusted associations from a model in which all 14 characteristics were simultaneously included as independent variables. We computed the proportion of variance in diabetes incidence that was modeled by the 14 county characteristics, calculated as 1-residual error of the model/total error and expressed as a %. The total variance of diabetes incidence was estimated by summing the residual square error at the county- and state-levels in a null model with no predictors and a state-level random intercept. Based on variance inflation factors (VIF) estimated from a linear regression model (see Appendix Table 2) and the correlations, we confirmed that no variable was associated with a VIF > 10, nor were any |correlations| >.50; therefore, we did not exclude any variables for collinearity concerns.
We used SAS 9.4 (Cary, NC) software to perform statistical analyses. All counties were weighted equally in the analysis.
RESULTS
Table 1 shows the distribution of diabetes incidence and socioeconomic and health environment characteristics of U.S. counties. Counties had on average 856 new diabetes cases per 100,000 in 2013, ranging between 310 and 2190 cases per 100,000.
Figure 1 shows a map of age-adjusted diabetes incidence across U.S. counties.
Figure 1.
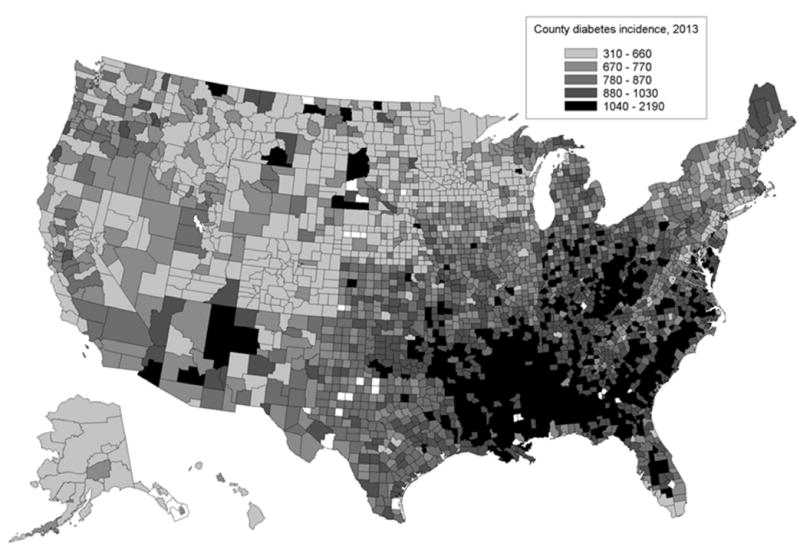
Age-adjusted diabetes incidence across 3109 analyzed U.S. counties, 2013. Incidence is the number of new diagnosed diabetes cases per 100,000 population.
Counties had on average 100,200 residents (ranging from 500 to 9,893,000). On average, almost 42% of counties’ population lived in urban areas (ranging from 0 to 100%). Half of counties were predominantly engaged in a service-dependent economy. In the average county, almost a quarter of the population aged 16-64 years experienced unemployment at any time in the past year and 16.9% of adults had not completed high school. The average median household income in counties was $40,700 (ranging from $18,700 to $100,800) and 15.4% of the population lived in poverty (ranging from 2.5% to 48.5%). In the average county, 52% of the population lived close to a park or recreational facility and almost a third of the population travelled an hour per day or more to work. On average, counties scored 7.4 out of 10 in terms of proximity to grocery stores and access to reliable sources of food. Twenty percent of counties had poor air quality. The average county had 53.1 primary care doctors per 100,000 people (range 0 to 508.3 doctors).
Table 2 shows associations between county-level characteristics and diabetes incidence, both unadjusted (Column 1) and adjusted for the other county-level characteristics (Column 2).
Table 2.
Associations between county features and age-adjusted diabetes incidence in 2013 across US counties
| Unadjusted Bivariate Associations (95% CI) | Adjusted Associations (95% CI) | |
|---|---|---|
|
|
||
| Intercept | 831.03 (793.31,868.76) | |
| Population (1,000) | -4.94 (-10.36, 0.49) | -0.90 (-6.02,4.22) |
| Social and economic features | ||
| % Urban | -11.73 (-17.27, -6.18) | 19.70 (12.57,26.83) |
| Service-dependent economy | -3.37 (-8.78, 2.05) | -1.72 (-6.69,3.25) |
| % Unemployed 2006-2010 | 88.57 (82.26, 94.89) | 38.57 (29.93,47.21) |
| % Without high school education | 66.01 (59.71, 72.31) | -1.75 (-9.97,6.47) |
| Median income 2006 ($1000) | -62.86 (-68.53, -57.19) | -5.00 (-14.92,4.92) |
| % In poverty, 2006 | 87.57 (82.08, 93.06) | 50.67 (39.87,61.47) |
| Health-related environment | ||
| % With exercise opportunities | -29.79 (-35.49, -24.09) | -15.71 (-21.73,-9.69) |
| Poor air quality 2006 | -10.53 (-16.46, -4.59) | 5.26 (-0.56,11.09) |
| % Long commute | -1.62 (-7.44, 4.21) | 9.24 (2.67,15.81) |
| Food environment index | -65.94 (-71.69, -60.18) | -19.69 (-26.53,-12.85) |
| Primary care doctors per 100000, 2011 | -21.25 (-26.65, -15.85) | -7.68 (-13.18,-2.18) |
| Variance components | ||
| Variance modeled, % | n/a | 42.5 |
n=3109
Standardized coefficients are used, so a 1-unit increase in a county characteristic should be interpreted as +1 standard deviation. The adjusted model includes all county characteristics simultaneously.
Adjusting for other characteristics (Column 2), counties with high percentages of the population living in urban areas had higher incidence of diabetes compared to those with lower percentages: there were 19.7/100,000 (95%CI: 12.57-26.83) more cases of diabetes for every SD increase in the proportion of the population living in urban areas (approximately 31% higher). Counties had 38.6/100,000 (95%CI: 29.93-47.21) more incident cases for every SD increase in proportion experiencing unemployment and 50.7/100,000 (95%CI: 39.87-61.47) more cases for each additional SD increase in the percent of the population living in poverty.
Several components of the health-related environment were also significantly associated with county diabetes incidence. The number of new cases was 9.2/100,000 higher (95%CI:2.67-15.81) for each additional SD of the population that commuted more than 60 minutes per day to work. Counties where a higher percent of the population had exercise opportunities and more diverse access to food had fewer new diabetes cases: the number of incident cases was 15.7/100,000 lower (95%CI:-21.73to -9.69) for each additional SD increase in the county population with exercise opportunities and 19.7/100,000 lower (95%CI:-26.53 to -12.85) for each additional point on the food availability index. The indicator of the healthcare environment, availability of primary care doctors was also relevant, with 7.7/100,000 (95%CI:-13.18to – 2.18) fewer cases for each SD increase in the number of doctors.
Collectively, these county characteristics explained 42% of the variation in diabetes incidence across counties.
DISCUSSION
This report presents the associations between contextual characteristics and the rate of occurrence of new cases of diabetes across United States counties to gain insight into which characteristics might have the potential for use in population-level approaches to diabetes prevention. It shows that the incidence of diabetes varies across U.S. counties, ranging from 310 to 2,190 new cases per 100,000 adults, with an average of 856 new cases/100,000 in 2013. The range entails a 6-fold difference between the counties with the lowest and highest diabetes rates. County levels of poverty and unemployment were positively associated with diabetes incidence. Components of the health environment, specifically proximity to grocery stores, long commutes, access to reliable sources of groceries, access to parks and recreational facilities, and density of primary care doctors, were negatively associated with the incidence rate of diabetes.
This study builds on recent papers describing geographical variation in diabetes prevalence, incidence, and mortality.(5) We contribute to this literature by addressing why this geographical variation exists, focusing on aggregate-level characteristics that may be linked with increased incidence of diabetes, especially those that may be amenable to interventions. Although some of these characteristics are interconnected, for example, higher-income counties may also have more parks and recreational facilities, we still detected independent associations with diabetes incidence. The pathways linking these county-level dimensions to diabetes risk should be explored further; they may include perceptions of safety, environmental pollutants, psychosocial stressors, residential segregation, and food insecurity.
The relationships between contextual factors and diabetes incidence are consistent with prior research on county-level diabetes prevalence. A study using modeled county-aggregated data found spatial clustering of diabetes prevalence across counties.(23) Compared with counties with low diabetes prevalence, those with high diabetes prevalence had higher levels of obesity and physical inactivity, were more urban, and had lower health insurance coverage.(23) Another study using the same data with geographically weighted regression also reported that most demographic and economic county characteristics were associated with diabetes prevalence;(24) still, there was great variation in these associations, with large proportions of counties having associations that were null or in the opposite direction from the average estimate.
The patterns reported here indicate concordance between individual and population-level characteristics that may lead to diabetes. They highlight ways in which individuals interact with, or are constrained by their environments. For example, while we found that county-level indicators of access to parks and recreational facilities and varied grocery choices were inversely associated with diabetes incidence rates, previous individual-level studies, such as the Multi-Ethnic Study of Atherosclerosis study, have shown that individuals living in neighborhoods with supermarkets and commercial recreational establishments had lower risk of developing diabetes.(11) These associations are not simply compositional: in a randomized controlled study of a low-income housing mobility program, those who moved to wealthier neighborhoods experienced reductions in the prevalence of extreme obesity and diabetes.(25) The patterns of diabetes incidence are also consistent with findings about the association between place-based characteristics and other components of individuals’ health, such as obesity, HIV, child mortality, and cardiovascular disease.(26-30)
This report presented a cross-sectional analysis and so does not establish causal relationships between county-level characteristics and diabetes incidence. Instead, we describe nationally representative associations between potentially modifiable socio-economic and health environment features and diabetes incidence in U.S. counties. By respecting temporal ordering with county characteristics from 2 to 9 years prior, we ensure that the county-level characteristics used at least predated the incident cases. Some proportion of the population was not living in the same counties several years earlier, when the environmental exposures took place. An estimated 5 to 6 percent of the U.S. population per year moves across counties.(31) Migration across counties may create a mismatch between county-level exposures and mortality; the results would be biased if those who move across counties have different exposures than those who do not move. The study findings are representative of 99% of U.S. counties, as 1% of counties were excluded due to missing data, most frequently on the exercise opportunities variable. Data on diagnosed diabetes are based on respondents’ reports about their diagnosis and so represent an under-estimate of true diabetes rates, as about 30% of people with diabetes are unaware of their condition.(32) Therefore, the estimated relationships would be affected by the extent to which rates of undiagnosed diabetes vary with county levels of socioeconomic factors and access to care. For example, variations in education and income level or access to healthcare across counties may result in differences in diabetes detection. However, the inclusion of county socio-economic characteristics and features of healthcare access in our model reduce this potential for bias. Finally, we did not incorporate the imprecision of the point estimates of county-level diabetes incidence and exposure variables in our analysis; this imprecision may lead to attenuation of the regression coefficients towards the null if there is non-differential measurement error.
CONCLUSION
Socio-economic characteristics of counties and features of livability and healthcare are independently associated with diabetes incidence. In particular, counties with access to diverse food options, parks and recreational facilities, and proximate employment have lower diabetes 14 incidence. The relationships between these modifiable features of counties and population-level diabetes and other health outcomes could be understood better exploiting quasi-experimental data from time- and place-varying policy changes and differences. Another important direction for future research will be to examine the possible causal pathways between county-level circumstances and individual diabetes risks. For example, physical inactivity and obesity are individual-level characteristics that may mediate the pathway between socio-contextual factors and diabetes incidence; such mediating analysis could be explicitly modeled in individual-level analyses. This study, while not able to establish causal relationships, contributes to an evidence base that socioeconomic deprivation is a key predictor of geographic variation in disease.
Acknowledgments
Funding
Neil Mehta was supported by the National Institute on Aging [grant number R01-AG040212]. Shivani Patel and Neil Mehta were supported by funding from the Robert Wood Foundation [grant number 70769].
Appendix
Table A1.
Correlation matrix
| V1 | V2 | V3 | V4 | V5 | V6 | V7 | V8 | V9 | V10 | V11 | V12 | V13 | V14 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| V1 | Population (1000) | 1.00 | . | . | . | . | . | . | . | . | . | . | . | . | . |
| V2 | % Urban | .39 | 1.00 | . | . | . | . | . | . | . | . | . | . | . | . |
| V3 | Service-dependent economy | .16 | .25 | 1.00 | . | . | . | . | . | . | . | . | . | . | . |
| V4 | % Unemployed 2006-2010 | -.05 | -.16 | .00 | 1.00 | . | . | . | . | . | . | . | . | . | . |
| V5 | % Without high school education | -.08 | -.20 | -.17 | .71 | 1.00 | . | . | . | . | . | . | . | . | . |
| V6 | Median income 2006 ($1000) | .29 | .45 | .18 | -.49 | -.57 | 1.00 | . | . | . | . | . | . | . | . |
| V7 | % in poverty 2006 | -.11 | -.19 | -.03 | .71 | .71 | -.77 | 1.00 | . | . | . | . | . | . | . |
| Primary care doctors per 100,000 pop in | .19 | .42 | .22 | -.26 | -.33 | .29 | -.21 | 1.00 | . | . | . | . | . | . | |
| V8 | 2011 | ||||||||||||||
| V9 | Medicare reimbursement/enrollee | .07 | .01 | -.08 | .43 | .43 | -.22 | .34 | -.16 | 1.00 | . | . | . | . | . |
| V10 | % With exercise opportunities | .32 | .55 | .24 | -.29 | -.34 | .44 | -.34 | .41 | -.17 | 1.00 | . | . | . | . |
| V11 | Poor air quality 2006 | .35 | .43 | .13 | -.10 | -.19 | .46 | -.26 | .22 | .02 | .35 | 1.00 | . | . | . |
| V12 | % Long commute | .11 | -.21 | .05 | .27 | .15 | .21 | -.07 | -.29 | .24 | -.14 | .17 | 1.00 | . | . |
| V13 | Food availability index | .05 | .08 | .05 | -.45 | -.41 | .54 | -.67 | .18 | -.13 | .27 | .16 | .13 | 1.00 | . |
| V14 | Diabetes incidence per 100000, 2013 (age-adjusted) | -.06 | -.08 | -.09 | .62 | .55 | -.43 | .58 | -.22 | .48 | -.30 | -.07 | .22 | -.41 | 1.00 |
Table A2.
Variance inflation factors
| Coefficient | Standard Error | p-value | Variance inflation factor | |
|---|---|---|---|---|
| Intercept | 416.498 | 43.2369 | <.0001 | 0 |
| Population (1000) | -0.0459 | 0.01052 | <.0001 | 1.31395 |
| % Urban | 1.239 | 0.1407 | <.0001 | 2.28818 |
| Service-dependent economy | -30.218 | 6.42768 | <.0001 | 1.20694 |
| % Unemployed 2006-2010 | 6.45214 | 0.59452 | <.0001 | 2.92603 |
| % Without high school education | 0.93828 | 0.66809 | 0.1603 | 2.81326 |
| Median income 2006 ($1000) | -2.6791 | 0.56803 | <.0001 | 4.16719 |
| % in poverty 2006 | 7.46733 | 1.10691 | <.0001 | 5.52504 |
| Primary care doctors per 100,000 pop in 2011 | 0.07352 | 0.10155 | 0.4691 | 1.47305 |
| Medicare reimbursement/enrollee | 0.0296 | 0.00215 | <.0001 | 1.4067 |
| % With exercise opportunities | -0.8272 | 0.15758 | <.0001 | 1.73726 |
| Poor air quality 2006 | 17.5894 | 9.45539 | 0.0629 | 1.50411 |
| % Long commute | 3.61049 | 0.33512 | <.0001 | 1.87556 |
| Food availability index | -15.033 | 3.3019 | <.0001 | 1.97456 |
Table A3.
Random effects from multilevel models
| State | Random Intercept | Lower 95% CI | Upper 95% CI | p-value |
|---|---|---|---|---|
| Alabama | 341.51 | 293.69 | 389.34 | <.0001 |
| Alaska | -144.41 | -208.10 | -80.7192 | <.0001 |
| Arizona | -57.8656 | -128.78 | 13.0478 | 0.1095 |
| Arkansas | 159.63 | 113.01 | 206.24 | <.0001 |
| California | -134.05 | -183.77 | -84.3248 | <.0001 |
| Colorado | -283.05 | -330.80 | -235.30 | <.0001 |
| Connecticut | -138.36 | -226.65 | -50.0601 | 0.0022 |
| Delaware | 101.63 | -24.5236 | 227.78 | 0.1141 |
| District of Columbia | -25.6621 | -203.89 | 152.57 | 0.7767 |
| Florida | 34.6857 | -13.9178 | 83.2892 | 0.1605 |
| Georgia | 132.06 | 89.4854 | 174.63 | <.0001 |
| Hawaii | -88.3530 | -202.26 | 25.5517 | 0.1282 |
| Idaho | -160.07 | -211.66 | -108.47 | <.0001 |
| Illinois | -5.6496 | -49.9622 | 38.6631 | 0.8008 |
| Indiana | 131.37 | 86.2810 | 176.46 | <.0001 |
| Iowa | 38.2127 | -6.9427 | 83.3682 | 0.0963 |
| Kansas | 60.3727 | 15.4386 | 105.31 | 0.0089 |
| Kentucky | 123.08 | 78.7154 | 167.45 | <.0001 |
| Louisiana | 171.81 | 122.03 | 221.60 | <.0001 |
| Maine | -7.6467 | -76.7772 | 61.4838 | 0.8280 |
| Maryland | 105.78 | 44.8517 | 166.70 | 0.0007 |
| Massachusetts | -24.2942 | -96.6387 | 48.0502 | 0.5097 |
| Michigan | 0.07066 | -45.8291 | 45.9704 | 0.9976 |
| Minnesota | -165.38 | -211.26 | -119.50 | <.0001 |
| Mississippi | 302.26 | 255.06 | 349.46 | <.0001 |
| Missouri | 21.6550 | -22.0307 | 65.3407 | 0.3275 |
| Montana | -147.21 | -197.02 | -97.4069 | <.0001 |
| Nebraska | -104.46 | -150.58 | -58.3350 | <.0001 |
| Nevada | -164.04 | -232.00 | -96.0783 | <.0001 |
| New Hampshire | 1.7348 | -79.3516 | 82.8212 | 0.9665 |
| New Jersey | -35.0146 | -99.0976 | 29.0684 | 0.2833 |
| New Mexico | -142.77 | -198.61 | -86.9231 | <.0001 |
| New York | -56.5532 | -104.81 | -8.2934 | 0.0220 |
| North Carolina | 68.6554 | 24.2592 | 113.05 | 0.0028 |
| North Dakota | -66.4579 | -117.02 | -15.8943 | 0.0103 |
| Ohio | 151.81 | 106.35 | 197.27 | <.0001 |
| Oklahoma | 86.7101 | 39.7920 | 133.63 | 0.0004 |
| Oregon | -52.0336 | -106.47 | 2.4028 | 0.0609 |
| Pennsylvania | 30.3445 | -17.3631 | 78.0521 | 0.2106 |
| Rhode Island | -41.9560 | -146.85 | 62.9350 | 0.4325 |
| South Carolina | 252.64 | 201.37 | 303.92 | <.0001 |
| South Dakota | -23.7744 | -72.6877 | 25.1389 | 0.3383 |
| Tennessee | 126.45 | 80.9611 | 171.93 | <.0001 |
| Texas | -63.8850 | -105.45 | -22.3212 | 0.0030 |
| Utah | -139.89 | -197.44 | -82.3291 | <.0001 |
| Vermont | -88.3800 | -160.73 | -16.0285 | 0.0168 |
| Virginia | 61.7240 | 18.4691 | 104.98 | 0.0057 |
| Washington | -117.63 | -170.78 | -64.4818 | <.0001 |
| West Virginia | 103.22 | 53.3274 | 153.10 | <.0001 |
| Wisconsin | -64.1618 | -111.12 | -17.2057 | 0.0078 |
| Wyoming | -64.4225 | -126.01 | -2.8354 | 0.0404 |
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Centers for Disease Control and Prevention. Centers for Disease Control and Prevention, ed. U.S Department of Health and Human Services; Atlanta, GA: 2014. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States, 2014. [Google Scholar]
- 2.Rowley WR, Bezold C, Arikan Y, Byrne E, Krohe S. Diabetes 2030 Insights from Yesterday, Today, and Future Trends. Popul Health Manag. 2016 doi: 10.1089/pop.2015.0181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barker L, Crespo R, Gerzoff RB, Denham S, Shrewsberry M, Cornelius-Averhart D. Residence in a distressed county in Appalachia as a risk factor for diabetes, Behavioral Risk Factor Surveillance System, 2006-2007. Prev Chronic Dis. 2010;7(5):A104. [PMC free article] [PubMed] [Google Scholar]
- 4.Barker LE, Kirtland KA, Gregg EW, Geiss LS, Thompson TJ. Geographic distribution of diagnosed diabetes in the U.S.: a diabetes belt. Am J Prev Med. 2011;40(4):434–9. doi: 10.1016/j.amepre.2010.12.019. [DOI] [PubMed] [Google Scholar]
- 5.Dwyer-Lindgren L, Mackenbach JP, Lenthe FJv, Flaxman AD, Mokdad AH. Diagnosed and Undiagnosed Diabetes Prevalence by County in the U.S., 1999–2012. Diabetes Care. 2016;39:1556–62. doi: 10.2337/dc16-0678. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Diabetes Data and Statistics - County Data. Atlanta, GA: 2014. [Google Scholar]
- 7.Castro FG, Shaibi GQ, Boehm-Smith E. Ecodevelopmental contexts for preventing type 2 diabetes in Latino and other racial/ethnic minority populations. Journal of behavioral medicine. 2009;32(1):89–105. doi: 10.1007/s10865-008-9194-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Laraia BA, Karter AJ, Warton EM, Schillinger D, Moffet HH, Adler N. Place matters: neighborhood deprivation and cardiometabolic risk factors in the Diabetes Study of Northern California (DISTANCE) Soc Sci Med. 2012;74(7):1082–90. doi: 10.1016/j.socscimed.2011.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Portrait F, Teeuwiszen E, Deeg D. Early life undernutrition and chronic diseases at older ages: the effects of the Dutch famine on cardiovascular diseases and diabetes. Soc Sci Med. 2011;73(5):711–8. doi: 10.1016/j.socscimed.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 10.Basu S, Stuckler D, McKee M, Galea G. Nutritional determinants of worldwide diabetes: an econometric study of food markets and diabetes prevalence in 173 countries. Public Health Nutr. 2013;16(1):179–86. doi: 10.1017/S1368980012002881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Christine PJ, Auchincloss AH, Bertoni AG, Carnethon MR, Sanchez BN, Moore K, et al. Longitudinal Associations Between Neighborhood Physical and Social Environments and Incident Type 2 Diabetes Mellitus: The Multi-Ethnic Study of Atherosclerosis (MESA) JAMA Intern Med. 2015;175(8):1311–20. doi: 10.1001/jamainternmed.2015.2691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.L PM, H JS, L JM, W DR, M RP, C J. Socioeconomic factors, health behaviors, and mortality: Results from a nationally representative prospective study of us adults. JAMA. 1998(279):1703–8. doi: 10.1001/jama.279.21.1703. [DOI] [PubMed] [Google Scholar]
- 13.Lantz PM, Golberstein E, House JS, Morenoff J. Socioeconomic and behavioral risk factors for mortality in a national 19-year prospective study of U.S. adults. Social Science & Medicine. 2010;70:1558–66. doi: 10.1016/j.socscimed.2010.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Murray CJL, Kulkarni SC, Michaud C, Tomijima N, Bulzacchelli MT, Iandiorio TJ, et al. Eight Americas: Investigating Mortality Disparities across Races, Counties, and Race-Counties in the United States. PlosMed. 2006;3:e260. doi: 10.1371/journal.pmed.0030260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.U.S. Department of Health and Human Services OoDPaHP. Healthy People 2020. Washington, DC: 2010. https://www.healthypeople.gov/sites/default/files/HP2020_brochure_with_LHI_508_FNL.pdf. [Google Scholar]
- 16.Barker L, Thompson T, Kirtland K, Boyle J, Geiss L, McCauley M, et al. Bayesian small areaestimates of diabetes incidence by United States county, 2009. J Data Sci. 2013;11:249–69. [PMC free article] [PubMed] [Google Scholar]
- 17.US Census Bureau. 2014 Pages on November 19, 2015. [Google Scholar]
- 18.U.S. Department of Health and Human Services Health Resources and Services Administration Bureau of Health Professions and National Center for Health Workforce Analysis. User Documentation for the Area Health Resource File (AHRF) 2012-2013 Release. 2013 [Google Scholar]
- 19.US Census Bureau. 2011 Pages on November 19, 2015. [Google Scholar]
- 20.US Census Bureau DID. 2009 Pages on November 14, 2015. [Google Scholar]
- 21.University of Wisconsin Population Health Institute. County Health Rankings & Roadmaps, 2010. 2014 [Google Scholar]
- 22.U.S. Department of Health and Human Services Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System 2006 BRFSS Supplement: County Level Variables. Atlanta, GA: 2007. [Google Scholar]
- 23.Shrestha SS, Kirtland KA, Thompson TJ, Barker L, Gregg EW, Geiss L. Spatial Clusters of County-Level Diagnosed Diabetes and Associated Risk Factors in the United States. The Open Diabetes Journal. 2012;5:29–37. [Google Scholar]
- 24.Hipp JA, Chalise N. Spatial analysis and correlates of county-level diabetes prevalence, 2009-2010. Prev Chronic Dis. 2015;12:E08. doi: 10.5888/pcd12.140404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ludwig Jea. Neighborhoods, obesity, and diabetes—a randomized social experiment. N Engl J Med. 2011;365(18):1509–19. doi: 10.1056/NEJMsa1103216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kennedy BP, Kawachi I, Glass R, Prothrow-Stith D. Income distribution, socioeconomic status, and self rated health in the United States: multilevel analysis. BMJ. 1998;317(7163):917–21. doi: 10.1136/bmj.317.7163.917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mehta NK, Chang VW. Weight status and restaurant availability a multilevel analysis. Am J Prev Med. 2008;34(2):127–33. doi: 10.1016/j.amepre.2007.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sullivan PS, Peterson J, Rosenberg ES, Kelley CF, Cooper H, Vaughan A, et al. Understanding Racial HIV/STI Disparities in Black and White Men Who Have Sex with Men: A Multilevel Approach. PLoS ONE. 2014;9(3):e90514. doi: 10.1371/journal.pone.0090514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Singh GK, Kogan MD. Widening Socioeconomic Disparities in US Childhood Mortality, 1969–2000. American Journal of Public Health. 2007;97(9):1658–65. doi: 10.2105/AJPH.2006.087320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gebreab SY, Davis SK, Symanzik J, Mensah GA, Gibbons GH, Diez-Roux AV. Geographic Variations in Cardiovascular Health in the United States: Contributions of State- and Individual-Level Factors. Journal of the American Heart Association. 2015;4(6) doi: 10.1161/JAHA.114.001673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Molloy R, Smith CL, Wozniak A. Finance and Economics Discussion Series: Divisions of Research & Statistics and Monetary Affairs, Federal Reserve Board. Washington, D.C: 2011. Internal Migration in the United States. [Google Scholar]
- 32.Ali MK, Bullard KM, Gregg EW, Del Rio C. A cascade of care for diabetes in the United States: visualizing the gaps. Ann Intern Med. 2014;161(10):681–9. doi: 10.7326/M14-0019. [DOI] [PubMed] [Google Scholar]


