Abstract
Although disparities in the burden of disease and illness experienced across major racial and ethnic groups in the United States (US), little is known about subgroups, including the Hmong population. This review sought to determine the current state of health disparities related to health promotion and disease prevention among Hmong adults from 1975 through 2015. Seventy-one descriptive (qualitative and quantitative) studies were reviewed. Most focused on two areas: (1) health status (mainly breast and cervical cancers) and (2) health-related behaviors. This literature review confirms the existence of health disparities related to health promotion and disease prevention in the Hmong adult population. Effective intervention relies on identifying these disparities. A possible explanation for these disparities is the lack of health data collected on subgroup populations, which includes the Hmong adult population. More research and more comprehensive health policies at the organizational level are needed to allow data to be collected on sub-group populations in order to better understand the social determinants that place the Hmong people at risk.
Keywords: Hmong, Disease Prevention, Health Promotion, Systematic Review, Health Disparities
INTRODUCTION
Despite the clear health goals set out in Healthy People 2020, disparities in the health status among racial and ethnic groups in the United States (US) remain substantial [1–5]. Research has improved our understanding of where health disparities come from, facilitating better planning for addressing the needs of various populations. However, much of the research has focused on large (umbrella) racial and ethnic minority categories. For example, US national studies, such as those conducted by the Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS) and Behavioral Risk Factor Surveillance System (BRFSS) defined the umbrella racial and ethnic minorities as “White, Black or African American, American Indian or Alaskan Native, and Asian [6],” making racial and ethnic minority subgroups invisible.
National health research has been conducted with Asian Americans as an aggregate group, or with the six larger Asian American subgroup populations (Asian Indian, Chinese, Filipino, Japanese, Korean, and Vietnamese) at a disaggregate level [7]. However, there are many other sizable Asian American groups in the US: Pakistani (409,000); Cambodian (276,000); Hmong (260,000); Thai (237,000); Laotian (232); Taiwanese (230,000); Bangladeshi (147,000); and Burmese (100,000) [8], who have not been disaggregated in national studies. These groups have different cultural backgrounds and vastly different histories, including differences in diet, cultural practices, health beliefs, education, socioeconomic status, and geographical origins. Thus, “determinants of health,” such as income and education, may vary considerably between and among each of these subgroups and could result in significant differences in health outcomes [9]. However, little is known about whether there are differences between the umbrella group and any of the subgroups or among the subgroups.
The few existing research studies of subgroups (Asian American) illustrate that aggregating data from multiple racial and ethnic minority subgroups can provide a misleading picture of individual subgroups [10–12]. For example, liver cancer has been shown to affect Asian and Pacific Islander subgroups [13] disproportionately, with mortality rates varying significantly across subgroups when examined separately. Liver cancer rates, for instance, are higher for the Vietnamese, Korean, and Filipino populations compared with other Asian subgroups and non-Hispanic whites [13]. This study’s findings underline the need for disaggregating data on subgroup populations. Thus, to fully understand the patterns of disease and to target prevention and intervention effectively, differences among subgroup populations must be clearly established.
One of the least studied Asian American subgroups is the Hmong. According to Bachrach, Pfister, Wallis, and Lipson (2014), almost 40% of health outcomes are closely linked to social factors [14]. The Hmong population differs significantly from other Asian American populations in many social factors, which may put them at risk for experiencing poorer health.
The Hmong
The Hmong people are an ethnic group that originated in southern China and later migrated to other parts of Asia. The Hmong in the US are primarily from Laos and were recruited by the US Central Intelligence Agency (CIA) to fight in the “Secret War” in Laos in 1965 [15]. The Secret War involved the US CIA and the Hmong people in Laos. The role of the Hmong people was to fight the communists in Laos, preventing the North Vietnamese from coming through Laos to South Vietnam. The Secret War ended in 1975, after the Vietnam War ended. Many Hmong fled to refugee camps in Thailand, and subsequently migrated to the US [15]. Currently, there are 260,073 Hmong living in the US [16]. The Hmong people in the US are concentrated in California, Minnesota, and Wisconsin [16]. Eighty-seven percent of Hmong in the US speak English “less than very well,” compared to 60% of all Asian Americans who speak English less than very well [17,18]. Hmong have a median household income of $45,776, compared to $66,201 of all Asian Americans [19]. Additionally, only 24.9% of Hmong people have a high school education, compared to 85% of all Asian Americans [20]. This demographic profile, which includes social determinants of health, suggests the Hmong population may bear a disproportionate burden of poor health.
A systematic literature review was conducted to fully understand the extent of the disproportionate burden of disease that the Hmong population experiences and to examine the current state of health of Hmong adults living in the US, focusing on health promotion and disease prevention. In particular, this systematic review summarized data on Hmong health in the US and critiqued the approaches used to understand health within the Hmong population. This review is the first step in addressing Executive Order 13515, signed by President Obama in 2009, to seek data on health disparities and improve the health of Asian Americans [21].
METHODS
This systematic review was prepared using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) recommendations [22,23]. This paper uses the National Institutes of Health (NIH) definition of health promotion and disease prevention to select the most appropriate articles for review. NIH defines health promotion and disease prevention research based on the following seven categories: (1) identifying modifiable risk and protective factors for diseases; (2) assessing risk (e.g., genetic susceptibility); (3) developing methods for screening and identifying markers for those at risk for onset or progression of asymptomatic diseases or high-risk behaviors; (4) developing and evaluating interventions to promote health for groups of individuals; (5) translating effective prevention strategies into practice; (6) conducting effectiveness studies related to the organization, management, financing, and adoption of prevention services and practices; and (7) conducting methodological and statistical procedures to assess risk and measure the effects of prevention strategies [24]. Using NIH’s definition is appropriate because it is one of the federal agencies that funds and prioritizes this area of research.
Data Sources and Search Strategies
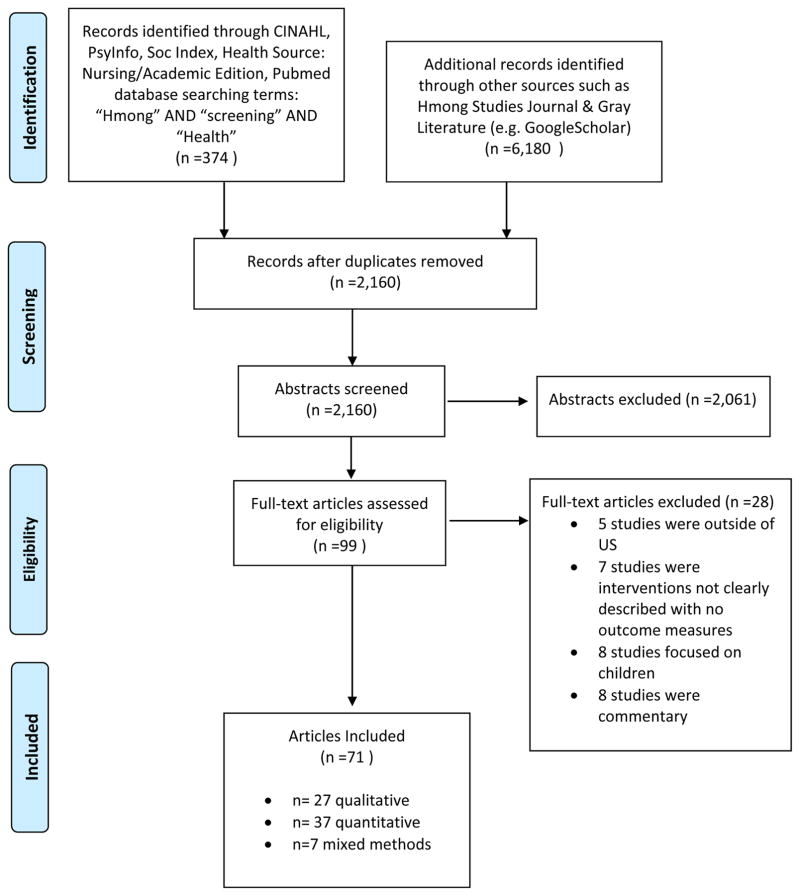
Articles were searched in the following databases: PubMed, Current Index to Nursing and Allied Health Literature (CINHAL), PsychInfo, SocINDEX, Medline, Health Source: Nursing/Academic Edition, Hmong Studies Journal, and gray literature, including Google Scholar, for articles published between 1975 and 2015. This time frame was selected because 1975 marks the beginning of the Hmong immigration to the US [25], and it allowed the researcher to gain a thorough historical understanding of research conducted on Hmong health since their arrival in the US. Broader search terms, including “Hmong,” “health,” “health promotion,” “prevention,” “screening,” OR “cancer screening,” OR “cardiovascular disease screening,” OR “diabetes screening,” OR “hypertension screening” were also used in the search databases. See Figure 1 for a flow diagram of the article selection process.
Figure 1.
PRISMA 2009 Flow Diagram
Informed Consent
Informed consent was not obtained for this paper because this is a review paper that collects and critically analyzes multiple research studies. However, informed consent was obtained from all individuals who participated in the studies that served as the primary sources of this review.
Study Selection and Data Extraction
Articles were included if they met the following criteria: (1) focused on Hmong adults defined as 18 years and older; (2) were peer-reviewed English-language publications; (3) described research that was conducted in the US; (4) were data-driven studies, including qualitative, quantitative, and mixed studies; and (6) focused on categories from the NIH’s definitions of health promotion and disease prevention. Articles were excluded if they: (1) focused on maternal/child health and mental health; (2) were review or commentary papers; (3) were from countries other than the US; and (4) did not focus on Hmong adults. Maternal/child health and mental health were not examined in this study because there has already been a large number of studies that focus on Hmong mental health and maternal/child health; there is no existing literature review on Hmong adults in the US. The author reviewed titles and abstracts using the inclusion criteria and the NIH definition of health promotion and disease prevention, as stated above[24].
The review of literature revealed that the current research on health promotion and disease prevention on the adult Hmong population focuses on two research categories within the NIH definition: (1) identifying modifiable risk and protective factors for diseases; and (2) assessing risk. The author independently read through the included articles and coded the articles deductively for: (a) author(s); (b) years; (c) study purpose; (d) design; (e) research area of focus; (f) sample size; (g) major findings; and (h) findings relevant to this review. All data were entered into a table to facilitate a cross article comparison. By comparing results from the articles, the author identified common themes across the articles. Two common themes were identified: (1) health status, which refers to research that describes differences in prevalence and mortality of diseases; and (2) health-related behavior, which refers to research that describes behaviors affecting an individual’s personal health and other people’s health, including health knowledge and attitudes. See Tables 1, 2, and 3 for findings of reviewed studies.
Table 1.
Qualitative Studies
| Authors | Study Purpose | Sample | Setting | Design | Analysis | Results |
|---|---|---|---|---|---|---|
| Baisch, Vang, & Peterman, 2008 | Explored the perspectives of Hmong women on cancer, using focus groups as the research method. | 10 | WI | Qualitative study | Inductive content analysis | There is no Hmong word for ‘cancer.’ Hmong participants have ‘fatalistic’ beliefs about cancer. Misunderstandings occur because of misunderstandings due to inadequate translations. Women are embarrassed to discuss about their body parts and male leaders controlled women’s health care decisions. |
| Barrett, Shadick, Schilling, Spencer, del Rosario, Moua, & Vang, 1998 | Examined interaction between Hmong patients and their health care providers and identified specific factors that either enable or obstruct health care delivery | 47 | WI | Complementary qualitative method including participant observation, focus groups, and literature review | Transcripts were analyzed by a multidisciplinary team | Hmong patients and their health care providers have different health beliefs systems. Translation was reported as a challenge, specifically for linguistic and cultural translation. The majority of Hmong patients identified kindness, caring, and a positive attitude as important provider characteristics. Providers reported that Hmong patients lack understanding of the following concepts: acute versus chronic diseases, illness prevention, and pain, both physical and psychological. |
| Burgess et al., 2008 | Explored beliefs and experiences related to smoking and cessation among the Hmong population in the United States | 18 | MN | Qualitative using focus groups | Used Patton (2002)’s qualitative analysis methods | Barriers to smoking cessation were different based on gender and acculturation. For example, women were concerned about having their smoking status revealed if they were to seek help, because of cultural prohibitions against female smokers. Less acculturated Hmong believed U.S. commercial tobacco to be more addictive than the homegrown tobacco they were used to. Participants were strongly influenced by smokers in their social networks. A powerful obstacle to quitting was addiction or “cravings”. |
| Burgess et al., 2014 | Examined how tobacco use patterns in Minnesota’s Southeast Asian communities (Minnesota’s Hmong, Khmer (Cambodian), Lao, and Vietnamese) have been shaped by culture, immigration, and adjustment to life in America. | 60 | MN | Qualitative | Used a standardized framework for ethnographic analysis called a face sheet comparison to look at each interview as a whole and to compare interviews to find similarities and differences | Among the Hmong participants, regular consumption of tobacco was unacceptable. Consumption of tobacco was rarely seen until the civil war in Laos when a number of Hmong soldiers became smokers. Social norms of smoking have begun to shift, with smoking becoming less acceptable. Although older male smokers felt social pressure to quit, they reported that smoking reduced their stress of social isolation, economic hardship, prior trauma, and the loss of power and status. |
| Culhane-Pera & Lee, 2006 | Explored Hmong patients and family members’ explanatory models, decision-making processes, and experiences with the health care system. | 34 | Not specify | Qualitative study | Analyzed major themes related to ideas of etiology, patho-physiology, signs/symptoms, course, and preferred treatment; reaction to health care system and medical decision | Hmong people’s concepts of kidney function and explanatory models of kidney stones are both from traditional and biomedical concepts. Hmong understood kidney stones as acute health problems caused by hard substances in water and food that stick to the kidney, which weak kidneys cannot excrete. People who had kidney stone did not know they had stones until they passed a stone or they saw stones on X-rays. They preferred medications, including herbal medicines, to invasive urological procedures. |
| Culhane-Pera, Her, & Her, 2007 | Increased understanding about Hmong cultural model of type 2 diabetes | 39 | MN | Qualitative | Hmong adults attribute their diabetes to their refugee experience. They also reported that feeling out of balance, defined as not fitting with the food, activity, weather, or community in the U.S., combined with emotional losses of being refugees, resulted in the development of diabetes. Hmong adults’ interpretation of diabetes was related to their traditional health model of balance and in the context of their loss place as refugees. | |
| Devlin, Roberts, Okaya & Xiong, 2006 | Explored health-related beliefs and experiences of African American, Hispanic/Latino, American Indian, and Hmong people with diabetes and engage community members in improving diabetes care. | 80 | MN | phenomenological approach using focus groups | Data were organized into similar or contrasting groups of themes using Krueger (1998) team-based analysis strategy approach | People reported a loss of health, healthy habits, and traditions through the exposure of American lifestyle, particularly with the lack of physical activity and poor diet resulted in the development of diabetes. Participants also reported a lack of confidence in the medical system. Participants also expressed the importance of spirituality, which shaped their experiences and self-care practices. |
| Fang & Baker, 2013 | Explored barriers and facilitators of cancer screening among women of Hmong origin | 44 | CA | Qualitative study using community-based participatory research approach | Krippendorff guidelines : used for reliability & reliability Social determinant of health framework used to guide probe and discussion during focus group and to capture key themes (analysis) |
Sociocultural barriers to screening included a lack of accurate knowledge about the causes of cervical cancer, language barriers, stigma, fear, lack of time and embarrassment. Structural barriers to screening included attitudes and practices of health care providers, lack of insurance (for college & professional women), and quality of service provision at clinics for the uninsured |
| Fu et al., 2007 | Explored minority smokers including Hmong’s experiences and beliefs about guideline-recommended smoking cessation treatments | 95 | MN | Qualitative using focus groups | Used Patton (2002)’s qualitative analysis method | Hmong participants reported that it was unlikely for the older Hmong generation to seek smoking cessation help from doctors due to the lack of awareness of the services. |
| Helsel, Mochel, & Bauer, 2004 | Examined Hmong Shaman respondents’ understanding and management of their illnesses. | 11 | CA | Exploratory qualitative | Grounded theory | Hmong shamans are influential individuals within the Hmong community and are often the resource persons to whom patients turn to for information on health. Hmong participants do not understand the concept of chronic illness, as a result, Hmong participants have sporadic medication and dietary regimens. They also lack awareness of potential complications, and persistently believed that chronic diseases could be cured rather than managed. |
| Johnson, 2002 | Determined Hmong perspectives and beliefs that influence the Hmong experience in Western medical situations. | 19 | CA | Ethnography study | No information on analysis | Hmong language lacked terminology of biomedical body physiology and anatomy. Medical terms and diagnoses lack direct translation and require extensive nondirect terms to approximate meaning. |
| Lor et al., 2013 | Described the beliefs, feelings, norms, and external conditions regarding breast and cervical cancer screening in a sample of Hmong women. | 16 | WI | Descriptive study, guided by the Theory of Care Seeking Behavior | Directed content analysis | Hmong women’s beliefs about breast and cervical cancer screening were based on their earlier experiences with breast and cervical symptoms. Many Hmong women felt embarrassed about breast and cervical cancer screening. They also fear about dealing with the results. Hmong women’s cultural norms about undressing for an exam and listening to authority figures were different from Western norms. Hmong women reported that difficulties in communicating with interpreters and clinicians were external conditions that influenced their screening behaviors. |
| De Castro, Krenz, & Neitzel, 2014 | Investigated agricultural-related safety and health issues among Hmong refugees working on family-operated farms. | 11 | WA | Photovoice methodology | Used a group analysis using Wang & Burris, 1997’s coding method | Hmong participants shared that their farm work put them at risk for musculoskeletal problems (e.g. chronic pain). Participants reported that handling and operating heavy machinery resulted in physical injuries. Participants also reported problems related to heat and cold stress and respiratory exposures. Pest management was reported as a challenge for Hmong farmers. Due to Hmong farmers’ socioeconomic status and language barriers, they reported difficulty in affording crops and communicating with supply stories and companies. |
| Nguyen & Seal, 2014 | Elicited the definitions of successful aging according to Chinese and Hmong elders living in Milwaukee, WI. | 44 | WI | Exploratory qualitative | Used Grounded Theory principles for analysis (Corbin & Strauss, 2990; Strauss & Corbin, 1994) | Hmong elders reported concerns about having good physical health, strength, and energy. They also reported having harmonious family relationships were important to them and feeling love is an important part of healthy aging. Hmong elders’ source of happiness included having children and having loving relationships with siblings and extended relatives. Elders expect to live with their children and for their children to provide tangible forms of support such as buying groceries, paying bills, and household chores. |
| Perez & Cha, 2007 | Investigated knowledge, beliefs, and treatment of diabetes in the Hmong community in Fresno County | 33 | No specificity | Qualitative using focus groups | Used Miles and Huberman (1984) and Patton (1990) for dealing with qualitative data | Findings from this survey revealed that the majority of study participants had no knowledge of the disease. Results from the survey also revealed misconceptions about the disease (e.g., believing a person can catch the disease by eating too many sweet foods). The study also revealed that the majority of study participants utilize traditional Hmong remedies such as herbs, including plants and tree roots for diabetes treatments |
| Perez & Thao, 2009 | Documented barriers to addressing diabetes in the Hmong community. | 10 | CA | Photovoice, a qualitative | Code for issues, themes, and theories in the documented stories | Barriers to diabetes prevention included 1) the environment, 2) personal choices, habits, and life style and, 3) lack of a safe environment to access physical activity as factors contributing to the potential for developing diabetes. |
| Perez, Moua, & Pinzon-Perez, 2006 | Identified risk factors for food-borne illness, knowledge of safe food handling practices, and understanding that transmission of food-borne diseases among Hmong. | 25 | CA | Qualitative | Data were coded into themes | Participants did not understand the direct relationship between bacteria and food borne illnesses. Participants were more likely to report reliance on traditional medicine to address foodborne illnesses. |
| Pham, Harrison, & Kagawa-Singer, 2007 | Explored Hmong parents’ and youths’ knowledge, attitudes, opinions, and behavior about health and healthy lifestyles. | 84 | CA | Qualitative | Data analyzed using inductive approach | Hmong valued physically active lifestyles and dietary patterns as well as fresh foods. Barriers to a healthy lifestyle included limited access to safe spaces, time for adequate physical activity, access to land to grow fresh produce, and time for home preparation of food. |
| Plotnikoff et al., 2002 | Increased understanding of the process and meanings of shamanic care from patient complaint through diagnosis, treatment, and outcome. | 36 | CA | Descriptive qualitative study | Grounded theory | Hmong patients sought shamanic help for different types of care including physical, emotional, and psychological complaints. |
| Thorburn, Kue, Keon, & Zukoski, 2013 | Explored family and clan influences on Hmong women’s breast and cervical cancer screening attitudes and behavior. | 83 | Oregon | Exploratory study | Content analysis | Hmong women make their own independent decisions about breast and cervical cancer screening. Half the women shared that their family encouraged/supported them in getting screened. However, some shared that elders discouraged screening. Hmong families do not discuss about breast and cervical cancer screening because they see it as a way for their family and clan to influence their attitudes. |
| Thorburn, Kue, Keon, & Lo, 2012 | Explored medical mistrust and trust of Western medicine and the health care system among Hmong women and men as well their experiences with discrimination in health care, and how these factors may influence Hmong women’s breast and cervical cancer screening behavior. | 83 | Oregon | Exploratory study | Did not specify type of data analysis method | Hmong distrust their doctors. Sources of mistrust included lack of understanding and negative impressions of Western medicine and the health care system. In addition, having a positive experience with providers created trust with some Hmong participants. However, participants reported that mistrust/trust did not have any effect on their decisions to get breast and cervical cancer screenings. A few Hmong participants reported being treated differently when they obtained their screening. This experience of discrimination affect Hmong participants’ behavior in willing to seek care. |
| Thorburn, Keon, et al., 2013 | Explored sources of information about breast and cervical cancer, including screening, and identify barriers to seeking such information fir Hmong women & men | 83 | Oregon | Qualitative descriptive study | Content analysis | Health care providers and the Internet were the most frequently cited sources for obtaining information about breast and cervical cancer for Hmong. Barriers to seeking information included fear of knowing they had the disease or of inviting it |
| Van Duyn et al., 2007 | Examined how best to adapt proven, evidence-based strategies to increase physical activity for use with underserved racial or ethnic groups. | 292 | CA | Qualitative study using focus groups | Did not specify | Media messages in the Hmong native language were important. Hmong families reported that community campaigns to increase physical activity could be done at Asian grocery stores, community organizations, churches, and festivals. Hmong gatekeepers reported they had little ability to change their environments (e.g. workplace, schools). Hmong reported safety concerns as a barrier to access their resources because they live in communities with high crime rates. |
| Vang, 2009 | Explored factors that influence Hmong women‘s willingness to be screened for breast cancer | 15 | WI | Qualitative | Used grounded theory to guide analysis | Breast health messages influenced Hmong women’s decisions about obtaining a mammogram. Hmong women only sought care when they were symptomatic (e.g. there is a visible sign or symptoms of illness). Instrumental barriers were reported to influence screening including lack of tangible aid and services, language barriers, and lack of insurance and transportation. Sociocultural influence such as family influences (e.g. husbands’ approval) on decisions to seek screening. |
| Vue, Wolff, & Goto, 2011 | Examined perspectives on food habits, acculturation, and health among Hmong women with young children in northern California. | 15 | CA | Qualitative | Data analysis done using principles of Grounded Theory | Participants reported that Hmong food culture is a healthful lifestyle and helps them maintain their self-identity. Hmong mothers encountered enormous challenges in bridging two extreme generations; the less acculturated immigrant adults and the highly acculturated, US-born children in their households. |
| Xiong & Westberg, 2012 | Determined perceptions of the Hmong population about Type 2 Diabetes | 9 | MN | Qualitative using focus group | Looked for common themes | Participants lacked knowledge about diabetes including different types of diabetes, risks of diabetes, causes, and treatment for diabetes. As a result, many participants were upset about taking the medication for the rest of their life and were reluctant to take their medications as prescribed. |
| Yang, Xiong, Vang, & Pharris, 2009 | Explored how to better care for Hmong women with diabetes using nursing theory praxis. | 5 | MN | Qualitative phenomenologic design | Data were analyzed using Newman’s (1994) hermeneutic-dialectic method | Hmong participants viewed causes of diabetes from culture change and hardships. Further, also described a direct connection between their loss, depression, deep grief, worry, stress, and diabetes. |
Table 2.
Quantitative Studies
| Authors | Study Purpose | Sample | Setting | Design | Results |
|---|---|---|---|---|---|
| Prevalence Studies | |||||
| Albright, 2010 1 No comparison to other groups |
Examined the prevalence of excess body mass (XBM), poor oral health (POH), and stress in a secluded population of aged (≥60 years) Hmong immigrants | 877 | CA | Survey study Had a PA who spoke Hmong to conduct the questionnaire |
The prevalence of diabetes among Hmong elders were 24% while the prevalence of POH was 41%. The prevalence of stress was 27% and prevalence of XBM was 87%. POH was related to the presence of diabetes. |
| Constantine et al., 2010 2 yes |
Measured the prevalence of smoking among the Hmong, Vietnamese, Lao, and Cambodian communities | 1,628 | MN | Cross-sectional survey study Telephone interview |
The Hmong have the lowest prevalence rate of smoking across all the SEA populations. The majority of Hmong smokers began smoking in the United States. Hmong women also started smoking at a much younger age (14 years) than males (21 years). |
| Gjerdingen & Lor, 1997 3 yes |
Determined hepatitis B status, by age, of Hmong patients | 1,585 | MN | Chart review | Hepatitis B infection is prevalent in the Hmong population. 18% of the Hmong patients had positive HBsAg test results. 85% tested positive for anti-HBs. People from age 15 to 19 have the highest frequency of acute or chronic hepatitis B infection (28%) compared to 18% of the entire sample. |
| Sheikh et al., 2011 4 yes |
Determined the prevalence of HBV among Hmong immigrants in the San Joaquin Valley of California. | 534 | CA | Cross-sectional study | Eighty-nine Hmong were tested positive for HBsAg; a prevalence of 16.7%. The majorities of HBsAg positive patients were ≥40 years (64.2%), married (66.7%), born in Laos (87.3%), and had lived in the United States ≥20 years (62.5%). Only 37.5% of the participants reported having a primary care physician. One out of every six Hmong immigrants was infected with HBV when they were screened. |
| Sheikh, Atla, Raoufi, Sadiq, & Sadler, 2012 5 yes |
Examined chronic hepatitis B virus (HBV) prevalence and its trends in Hmong donors in the Central Valley | 821 | CA | cross-sectional review study | The overall prevalence of HBV in Hmong donors was 3.41% compared to 0.06% in donors of all ethnicities from 2006 to 2010. |
| Sheikh, Atla, Ameer, Sadiq, & Sadler, 2013 6 yes |
Evaluated the prevalence of hepatitis B virus (HBV) and hepatitis C virus (HCV) in healthy blood donors in the Valley. | 217,738 | CA | Review of blood donor laboratory screening records from Central California Blood Center | Hmong had the highest HBV prevalence of 7.63% with a peak prevalence of 8.76% among the 16- to 35-year-old age group compared to other Asian subgroups. |
| Thao, Arndt, Tandis, & Hanrahan, 2015 7 yes |
Compared the prevalence of diabetes between Hmong and non-Hispanic white patients of the University of Wisconsin departments of family medicine, pediatrics, and internal medicine clinics | 964 | WI | Electronic health record data | The total prevalence of diabetes in the Hmong patient population was 11.3% compared to 6.0% in the non-Hispanic white patient population. The prevalence of diabetes in Hmong adult patients was 19.1% compared to 7.8% in white adult patients. |
| Rooney & Choudhary, 2009 8 no |
Examined correlates of tobacco use among Hmong people residing in Wisconsin. | 2,856 | WI | Survey study Survey was done in Hmong language but there was no information inclusion criteria of literacy |
The overall prevalence of daily tobacco use for adults was 25.3% for males and 12.4% for females. Males aged 51–83 had the highest rate of daily and ever use of tobacco. In contrast, females aged 18–35 reported the highest prevalence for daily and ever use of tobacco. People with no formal education were at the highest risk for using tobacco, with a decrease in the odds of smoking as the number of years of education increased. |
| Wahedduddin et al., 2010 yes |
Compared characteristics of gout in Hmong patients versus Caucasians and examined if Hmong ethnicity is associated with risk of tophaceous gout. | 89 | MN | A retrospective chart review | The Hmong who were diagnosed with gout was younger (58.3 years old), had an earlier onset of symptoms (37.4 years old) and higher mean serum uric acid levels during follow-up (9.1 mg/dl). There were higher rates of tophaceous gout (31.5%), including hand tophi (21.3%) among Hmong. Hmong ethnicity was significantly associated with risk of tophaceous gout after adjusted for age, sex, hypertension, diuretic use and kidney function, |
| Incidences | |||||
| Mills & Yang, 1997 1 |
Examine cancer incidence in the Hmong population | 183 | CA | Retrospective study using cancer registry | There were six elevated rates of cancer sites in the Hmong: nasopharynx, stomach, liver, pancreas, leukemia, and non-Hodgkin’s lymphoma. Hmong women have elevated cervical cancer incidence and invasive cervix cancer. Hmong also experienced advanced stage and grade of disease at diagnosis for many cancer sites in addition to cervical cancer. |
| Ross, Xie, Kiffmeyer, Bushhouse, & Robison, 2003 2 |
Examined cancer incidence in the Hmong population | 186 | MN | Cancer registry | The Hmong population had increased proportional incidence ratios for nasopharyngeal cancer, gastric cancer, and cervical cancer compared to all Minnesotans. |
| Mortality | |||||
| Kwong, Stewart, Aoki, & Chen, 2010 1 |
Analyzed the differences in survival of Californians of Asian ancestry with hepatocellular carcinoma (HCC) | 6,068 | CA | Use cancer registry | Laotian/Hmong had significantly higher cause-specific mortality HCC compared to all ethnic groups. Forty-three percent of Hmong patients had disease spread to remote sites, with only 3% receiving local surgical treatment, resection, or liver transplantation. |
| Yang, Mills, & Nasseri, 2010 2 |
Examined causes of death (COD) and compare age-adjusted mortality rates (AAMR) in the Hmong with those of non-Hispanic white (NHW) population in California | 2,744 | CA | Retrospective study using data from the California Center for Health Statistics | Hmong and NHW have the highest AAMR in neoplasm, circulatory and respiratory diseases. Hmong experienced 1.3–1.9 times higher mortality rates for certain COD, compared to NHW. Hmong have 1.3–1.9 times higher mortality rates for injuries and poisonings, digestive diseases, prenatal conditions, ENMID (endocrine, nutritional, metabolic, immunity disorders), infections and parasitic illnesses, and congenital anomalies when compared to NHW. Hmong men were observed to be at statistically significantly higher mortality risk for just infections and parasitic diseases when compared to NHW men. |
| Risk Factors | |||||
| Bates, Hill, & Barrett-Connor, 1989 | Screened for heart disease risk factors | 117 | CA | Cross-sectional study No information |
The Hmong, compared with other Indochinese, had a significantly lower mean cholesterol level, which remained after adjusting for age and body mass. High rates of cigarette smoking were found among Vietnamese men and young Indochinese men. |
| Her & Mundt, 2005 | Quantified the proportion that may be at risk for developing type 2 diabetes among of Hmong adults in Wisconsin | 144 | WI | cross sectional risk prevalence survey no information on addressing literacy issues |
Forty-one percent had positive blood glucose screens on survey. Waist-to-hip ratio was a stronger predictor of a positive screen than the ADA Risk Test. |
| Neitzel, Krenz, & de Castro, 2014 | Evaluated occupational health and safety hazards in agriculture, and pilot-tested this on several small-scale Hmong farming operations. | 66 | WA | Cross-sectional pilot test of hazard assessment tool | Observed a range of hazard types related to musculoskeletal activities including bending (about 56% of all observations, with the vast majority of these being bending at the back) and constant hand grip (about 42% of all observations). Other common hazards that we observed “frequently” were use of sharp blades and lifting <50 pounds (about 31% of observations each) and awkward postures (about 29% of observations). |
| COMBINATION OF PREVALENCE, RISK, AND MORTALITY | |||||
| Culhane-Pera DeFor, & Desai, 2009 1 |
Measured prevalence of CVD and CVD risk factors in Hmong refugees newly arriving from Wat Tham Krabok, Thailand 2004–2006 | 1,462 | MN | Cross-sectional study including screening exam | 48.7% of older people (ages 14–41) were overweight, obese, or morbidly obese by WHO categories. Hmong refugees had significant CVD risk factors on arrival. Specifically, men in the older group have a higher cardiovascular disease risk factor compared to women, particularly for hypertension, hyperlipidemia, and hyperuricemia. |
| Dodge, Mills, & Yang, 2005 2 |
Identified nasopharyngeal cancer in the California Hmong | 59 | CA | Case series design | Hmong had an incidence of 2–3 times greater of nasopharyngeal cancer compare to non-Hispanic whites. Nasopharyngeal cancer mortality rates were 10.4 for Hmong compared to 0.2 for Asian Pacific Islanders and 1.7/1,000 for non-respectively. Hmong were more likely to be diagnosed with later stages and less likely to receive treatment. |
| Mills, Yang, & Riordan, 2005 3 |
Examined cancer incidence rates in the Hmong in the state of California for the years 1988–2000 | 749 | CA | Cancer registry | A total of 749 Hmong in California were diagnosed with invasive cancer. There was 284 per 100,000 population age adjusted rate of cancer for the Hmong compared to 362.6 and 478 per 100,000 in the API and NHW populations, respectively. Specifically, there were elevated for hepatic, gastric, cervical, and nasopharyngeal cancers and for leukemia and non-Hodgkin lymphoma (NHL) among the Hmong. Cervical cancer incidence increased, rates of NHL declined, and rates for colorectal cancer remained steady between 1988 and 2000. The Hmong were diagnosed at later disease stage with poorer grade of disease diagnosis than other API. |
| Portis, Hermans, Culhane-Pera, & Curhan, 2004 4 |
Examined whether the Hmong have a high rate of uric acid stone disease was evaluated. | 204 | MN | A retrospective chart review was performed | Of the 204 patients, 94 Hmong (46%) and 23 non-Hmong (11%) patients had stone disease. Surgical treatments differed between Hmong and non-Hmong. Nine (43%) Hmong patients refused treatment for staghorn calculi. |
| Yang, Mills, & Riordan, 2004, 5 |
Examined cervical cancer incidence, mortality, and other tumor characteristics in the Hmong female population of California between 1988 and 2000. | 102 | CA | Cancer cases obtained from the population-based California Cancer Registry (CCR) | Hmong women experienced incidence and mortality rates of cancer three and four times higher than Asian/Pacific Islander and non-Hispanic white women, respectively. Fifty-one percent of Hmong women chose no treatment, compared to 5.8% for Asian/Pacific Islander women and 4.8% for non-Hispanic white women. Hmong women are more likely to be diagnosed with cervical cancer at later stages and poorer histologic grades, and had a lower survival rate than younger Hmong females. |
| Yang, Mills, & Riordan, 2005 6 |
Examined gastric adenocarcinoma incidence, mortality, and tumor characteristics in the Hmong population of California, 1988–2000. | 66 | CA | Data obtained from California Cancer Registry (CCR) | From 1988–2000, there were 66 gastric cancer cases diagnosed of Hmong living in CA. Over 97% of these cases were malignant tumors. Hmong have high incidence rate of stomach cancer (26.9,100000) compared to Asian Pacific Islanders (19.8/100000) and non-Hispanic Whites (8.4/100000). Hmong were more likely to be diagnosed with cancer at later stages. More than 97% of Hmong patients chose no treatment, compared to only 25.6% of API and 30.3% of Non-Hispanic Whites patients. |
| Factors Associated with Health Behavior | |||||
| Albright, Woo, Ji, Sun, Lang, & Albright, 2013 | Investigated associations between type 2 diabetes (DM) and several variables (e.g. poor oral health and overweight (OW)/obesity among a group of elderly Hmong | 495 | CA | Survey No info on translation; inclusion criteria of English or Hmong ability |
DM was correlated with poor oral health (POH). There was a strong correlation between concurrent POH and OW and the presence of DM: all subjects with both POH and OW had DM. There was a significant association between the presence of DM and concurrent OW and POH, controlling for OW, POH, age, years of residence in California, and stress level. |
| Baker, Dang, Ly, & Diaz, 2010 | Explored factors associated with perception of barriers to immunization among parents of Hmong | 417 | CA | Cross-sectional survey Inclusion criteria: reported being able to read and write in either Hmong or English. |
Socioeconomic position and use of traditional Hmong health care (i.e., consulting shamans and herbalists) significantly predicted higher perceived barriers to immunization. Nativity (e.g. years in the United States), age of arrival in the United States, and English language fluency, did not predict perceived barriers. |
| Fang, Lee, Stewart, Ly, & Chen, 2010 | Examined baseline data on the proportion of Hmong women who reported they had a Pap test for the early detection of cervical cancer | 402 | CA | Cross-sectional questionnaire Survey translated into Hmong; no information about how survey was taken |
Only 74% of Hmong women had ever had a Pap test. 61% of Hmong women had a Pap test in the previous three years. Women were more likely to have had a recent Pap test if they were younger (e.g. age 21–30 or 31–40). Hmong women who were single were or born in the U.S. were less likely going to have a Pap test. |
| Lee & Vang, 2013 | Examined how cultural factors were associated with breast cancer screening utilization, specifically clinical breast exam (CBE) | 164 | MN | Cross-sectional survey Participants were given the option of completing the survey on their own or in a face-to-face interview with a bilingual and bicultural research assistant who was intensively trained by the first author. English or Hmong |
73 % of Hmong American women reported ever having had a CBE. Hmong women’s modest views were the greatest barrier to ever having had a CBE. Age and language preference were also found to be significant predictors of past CBE use. |
| Lee, Yang, Lee, & Ghebre, 2015 | Investigated Hmong-American immigrant women’s utilization of cervical cancer screening | 164 | CA | A cross-sectional survey research design Either face to face interview or in persons surveys conducted by Hmong women |
About 67.1% had received a Pap test within the last 3 years. Fatalism, modesty, education, and marital status were significantly correlated with receiving a Pap test. |
| Maxwell et al 2012 | Examined relationships using Health Behavior Framework factors across four Asian American groups (Vietnamese-, Hmong-, Korean- and Cambodian-American) to advance the development of theory-based interventions for HBV testing in at-risk populations. | 1,735 | Washington, DC & Washington State | Survey No information about survey tailored for Hmong |
Only 45% of Hmong who had heard of hepatitis B. Perceived susceptibility was lowest among Hmong compared to ___?. |
| Nguyen & O’Connell, 2002 | Determined Asian and Asian-American college students’ knowledge of osteoporosis prevention, risk factors, and treatment. | 168 | MN | Cross-sectional survey No information on translation or language requirement of participants |
Thirty-eight percent of Hmong participants thought osteoporosis was attributed to fate, chance, or luck. In contrast, Vietnamese participants attribute osteoporosis to diet. Most participants (63%) did not know whether their culture objected to estrogen replacement therapy, and 42% said menopause was a natural occurrence for which pharmacologic treatment should not be administered. |
| Okunseri, Yang, Gonzalez, LeMay, & Iacopino, 2008 | (1) described the self-rated oral health (SROH), self-rated general health (SRGH), and use of dental/physician services; and (2) identified the factors associated with SROH among Hmong adults. | 118 | WI | A cross-sectional study No information on translation or language requirement of participants |
Of the 118 participants, 49% rated their oral health as poor/fair and 30% rated their general health as poor/fair. Thirty-nine percent of Hmong reported that they did not have a regular source of dental care, 46% rated their access to dental care as poor/fair, 43% visited a dentist and 66% visited a physician within the past 12 months. Access to dental care, past dental visits, age and SRGH were significantly associated with SROH. There was a strong association between access to dental care and good/excellent SROH. |
| Story & Harris, 1989 | Obtained information changes in food habits. | 60 | N/A | Survey study | Southeast Asian refugee families including the Hmong have maintained strong ties to their native foods and traditional diets. Rice remains the main food in their diet. Although most adults prefer eating their native foods, their children prefer both American and native foods. |
| Sugerman, Backman, Foerster, Ghirardelli, Linares, & Fong, 2011 | Gained opinions from low-income, limited-English-speaking Hispanic and Asian immigrants for formative research in a social marketing campaign. | 905 | CA | Descriptive study Telephone survey done in Hmong |
Hmong reported receiving most of their information from the radio. Hispanics, Koreans, and Vietnamese thought diabetes was the greatest health issue in California while Hmong thought high blood pressure was the greatest health issues. Among Hmong, 83% thought fruits and vegetables were too expensive, and 49% of Vietnamese thought good quality, affordable fresh FVs were too hard to find |
| Tanjasiri et al., 2001a | Examined Hmong women’s breast cancer screening behaviors—breast self-examination (BSE), clinical breast examination (CBE), and mammography | 201 | CA | Survey One-on-one survey interviews |
Over 50% of all respondents reported they had ever performed BSE. Among respondents aged 40 or older, 52% had ever had a CBE and only 30% had ever had mammography. |
| Vang & Pinzon-Perez, 2006 | Examined nasopharyngeal cancer (NPC) knowledge among a rural Hmong community in California | 145 | CA | Cross-sectional survey study Survey translated from English into Hmong No information about delivery of survey |
The participants’ knowledge of cancer varied with age and educational level. Middle-aged generations had the highest level of knowledge on nasopharyngeal cancer compared to older generations. Participants with no school were the least knowledgeable about nasopharyngeal cancer. Those participants with the highest formal education were most knowledgeable about the disease. There was no difference between Hmong males and females on knowledgeable of nasopharyngeal cancer. |
| Wong, Mouanoutoua, Chen, Gray, & Tseng, 2005 | Assessed contexts of adherence with hypertension care among Hmong Americans | 323 | CA | Cross-sectional survey study Face to face survey; no information about translation, delivery of survey |
Only 27% of Hmong reported having control over their blood pressure and over 50% reported non-adherence with hypertension care. Respondents who were 50 years of age or older, had no physical illness, did not know that hypertension was preventable, or believed that American medicine was too strong, were more likely to report non-adherence with proper medication consumption. |
| Wu, Hsieh, Wang, Yao, & Oakley, 2011 | Examined the role of ethnicity in explaining multiple cardiovascular disease risk factors after controlling for demographic and access to care variables | 388 | MI | Cross-sectional surveys and blood tests Survey was done in English and all other Asian languages and bilingual interpreters were available to assist participants to complete the study surveys if needed. |
Hmong participants had the highest risk of diabetes among the Hmong participants compared to four other Asian groups (e.g.. |
| Yang, Mills, & Dodge, 2006 | Examined patterns of cancer screening, reproductive history, and cancer health behaviors among the Hmong adults | 248 | CA | Cross-sectional survey Respondents literate in English or Hmong were given the option to respond to the questionnaire individually, and at their own pace. For all other respondents, the interviews were conducted in either group or one-on-one sessions. In the group sessions, the interviewer guided the participants through the questionnaire by reading each question and the response options out loud. Then, the respondents were asked to mark the answer that best described his/her opinion on the survey. In one-on-one interviews, the interviewer recorded the answers, as the respondent answered each question when asked. |
No one ever received colorectal exam. Only 30% have ever did a self-breast exam and only 15.8% received a mammogram. |
| Yang & Mills, 2008 | Examined Hmong dietary and lifestyle patterns | 248 | CA | Descriptive survey study The adapted survey was translated into Hmong, and pre-tested with a focus group of 12 Hmong adults. |
Over 63% of Hmong adults were either overweight or obese. Hmong identified rice, chicken, beef, and eggs as the most frequently eaten items. Fruits and vegetables were also identified. |
Table 3.
Mixed Methods Studies
| Author | Study Purpose | Sample | Setting | Design | Results |
|---|---|---|---|---|---|
| Franzen & Smith, 2010 | Investigate influences on shopping and eating behavior of Hmong adultsliving in St. Paul/Minneapolis, Minnesota | 69 | MN | Questionnaire, focus group, and community mapping | St. Paul, MN has the highest density of the Hmong population as well as Hmong/Asian grocery stories. The current consumer price index (CPI) was only available for a limited number of foods which means there were less ethnic food for Hmong. Those who were born outside of the US and lived less than 5 years in the US reported significant increase of some American food. In contrast, those who were born outside of the US and lived more than 5 years reported increased consumption of all foods after moving to the US. Moreover, those born in the US reported to eat less produce food, hunt food, and drink milk. |
| Goto, Vue, Xiong, & Wolffa, 2010 | Examine perspectives on food, culture, and health and nutrition education among Hmong mothers with middle school children | 40 | CA | Q methodology included sorting and ranking statements regarding food culture, acculturation, child obesity, and health and discussing in depth their choices | Mothers fell into three groups based on their perspectives: (1) traditional food culture preservers (n = 20), (2) financially struggling health-conscious mothers (n = 11), and (3) mothers concerned about a parent-child generational gap (n = 4). There was no significant difference between these three groups. Mothers in group 1 reported enjoying cooking and eating Hmong food. They disagree that Hmong food are cheaper than American food. Mothers in group 2 reported a lack of financial assistance to acquire fruits and vegetables. These mothers were concerned about excessive snacking that may led to future health problems and strongly agreed that it is important to encourage physical activities among their children. Mothers in group 3 shared that there is a different food preference between them and their children (Hmong food vs American food). |
| Grazier, Armenian, & Vohra, 2014 | Examined a case of life-threatening cinchonism from illicit purchase of chloroquine and survey local ethnic markets to determine what medications are sold without a prescription. | MN | Case report and survey | Ethnic markets sold discontinued FDA prescription medications. Five were identified as discontinued by the FDA: diphenidol, phenacetin, metamizole, phenylbutazone, and sibutramine. | |
| Ikeda et al., 1991 | Collected information necessary to design effective nutrition education programs that would meet the unique needs and interests of the Hmong. | 205 | CA | Used focus groups interviews and administered two questionnaires:1) Food and Habit Questionnaire; 2) the Adult EFNEP Family Record Form | Over 50% of Hmong reported consuming two meals per day. Hmong people’s meals consist of white rice, vegetables, and meat. Snacking was not common. Eighty-four percent of Hmong males reported that food was prepared by their wife. |
| Kue & Thorburn, 2013 | Explored Hmong women and men’s knowledge of hepatitis B, their screening, and vaccination behavior. | 83 | Oregon | Questionnaire and qualitative interviews Interview questions were guided by Kleinman’s explanatory models approach |
Ninety-six percent participants have heard Hepatitis B. Fifty-three percent have been screened for Hepatitis B. Fifty percent reported being vaccinated. There was low knowledge about transmission of Hepatitis B. Participants reported lack of word in their Hmong language about their illness. Participants reported fearing about the cost of treatment and the effects of cancer treatment on their bodies. |
| Neitzel, Krenz, & de Castro, 2014 | Developed an observation-based methodology to evaluate occupational health and safety hazards in agriculture, and pilot-tested this on several small-scale Hmong farming operations. | 9 | WA | Semi-quantitative observational tool | Observations revealed that the most common hazards Hmong farmers faced were bending at the back while lifting <50 pounds, using sharp tools without adequate guarding mechanisms (e.g. awkward posture), and lifting >50 pounds. |
| Schroepfer, Waltz, Noh, Matloub, & Kue, 2010 | Assessed the Hmong population’s stage of readiness to address cancer and understand what factors contribute to their stage of readiness. | 9 | WI | Scale and interviews | Hmong’s stage of readiness to address cancer was “vague awareness.” There were six themes that contributed to the Hmong’s stage of readiness including: (1) new home, illness, and healthcare system; (2) Hmong healthcare beliefs and practices; (3) newness impacts resources needed and their access; (4) community view of cancer; (5) issues of trust; and (6) reliance on Hmong medicine. |
After the tables and themes were created, the author worked with her research team, which comprised three doctoral students, a post-doctorate fellow, and her advisor, to review the tables and themes, specifically to determine whether the tables agree or disagree with the themes. Consensus was achieved when research group members agreed on the themes. When there was disagreement, the research team members discussed the rationale for their decisions and collaborated to create a new theme that was satisfactory to all members.
Quality Assessment
The author assessed the quality of each of the 71 articles included in this review. The quantitative studies were analyzed to determine quality of research methods, reliability and validity of measures, and relevance of findings to Hmong health promotion and disease prevention. The qualitative studies were reviewed using the consolidated criteria for reporting qualitative research (COREQ) checklist [26].
RESULTS
Study Characteristics
Of the 71 articles, 33 studies were conducted in California, 17 in Minnesota, 10 in Wisconsin, 1 in Michigan, 4 in Oregon, 3 in Washington, and 3 at an unspecified location. The study sample sizes were wide-ranging, from 4 to 217,738. The sample sizes across qualitative studies ranged from 5 to 292. In contrast, the sample sizes across quantitative studies ranged from 59 to 217,738.
Of the 71 articles, 37 were quantitative, 27 were qualitative, and 7 were mixed-method. Of the 37 quantitative studies, 19 used surveys/questionnaires, 3 used screening studies, 6 used chart review, and 7 used cancer registries.
Health Status
Health status research described differences in health risks, prevalence, and disease mortality. Twenty-two studies addressed disease prevalence, incidence, risks, and mortality rates. Of the 22 studies, eight studies focused on disease prevalence using electronic health records (n=6), four studies focused on disease incidence using mainly registries (n=4); two studies focused on mortality rates using a combination of registries, serologic tests, chart reviews, and surveys; two studies focused on risk factors using surveys; and six studies focused on two or more areas including incidence, prevalence, and/or mortality using survey, registry, and screening exams.
Prevalence
The nine studies of prevalence focused on: body mass, oral health, and stress (n=1;[27]); smoking (n=2; [28,29], hepatitis B virus (n=4; [30–32, 35]); gout (n=1; [34]; and diabetes studies (n=2; [33]). Of these nine studies, only seven compared disease prevalence in Hmong with other racial/ethnic groups.
From the comparative studies of Hmong with other racial/ethnic minority groups, there is some evidence that Hmong face worse health outcomes. For examples, Hmong have a high prevalence of hepatitis B virus, ranging from 3.41%–16.7%, compared to the 0.15%–1.27% documented for other Asians, Caucasians, African Americans, Hispanics, and Native Americans [30–32]. Researchers reported that diabetes prevalence among Hmong was 11.3% compared to 6% of the non-Hispanic white population [33]. In a 2010 study, Wahedduddin and colleagues reported that the Hmong had a 31.5 % incidence of tophaceous gout compared to 10.7% of Caucasians [34].
With no comparison groups, one study reported that Hmong people have a high occurrence of hepatitis B virus infection [35]. Specifically, 17% (47 of 77) of Hmong patients aged 20 years and older were infected with the hepatitis B virus, and 48% (130 of 183) had developed immunity to the hepatitis B virus [35]. Similarly, from a survey of Hmong people, 20% of Hmong adults reported daily use of tobacco and approximately 40% reported ever using tobacco [29]. Constantine and colleagues (2010) also reported that Hmong have the lowest rate of smoking compared to all Southeast Asian populations [28].
Incidence
Two studies examined disease incidences; both focused on cancer [36,37]. Only one study compared the disease incidence of the Hmong with other racial/ethnic minority groups [36]. Hmong in California have an age-adjusted incidence rate for cervical cancer of 50/100,000 compared to 30.1/100,000 for the Asian/Other group; leukemia, of 10.7/100,000 compared to 9.98/100,000 for all Asian groups combined (e.g., Vietnamese, Laotian, Cambodian, or Asian/Other); stomach cancer, of 40/100,000 compared to 14.3/100,000 for all Asian groups combined; non-Hodgkin’s lymphoma, of 17.6/100,000 compared to 9.8/100,000 for all Asian groups combined; nasopharyngeal cancer, of 15.6/100,000 compared to 0.72/100,000; and liver cancer, of 7.1/100,000 compared to 3.1/100,000 for all Asian groups combined [36]. Similarly, Ross and colleagues (2003) reported that there were significantly increased proportional incidence ratios (PIR) of nasopharyngeal (PIR 39.39), gastric (PIR 8.70), hepatic (PIR 8.08), and cervical (PIR 3.72) malignancies among Hmong in Minnesota [37].
Mortality Rates
Of the two mortality rate studies, one focused on cancer survival and the other focused solely on cancer mortality rates in comparison to Asian/Pacific Islander and non-Hispanic whites [38,39]. Kwong and colleagues (2010) reported that Hmong have the worse survival rates (e.g., an average of 2 months for case-specific cancer) among Asian American groups (e.g., Cambodian average of 6 months; Thai average of 4 months, and Korean and South Asian average of 7 months for cause-specific cancer) [38]. Hmong also experienced 1.3–1.9 times higher mortality rates for some causes of death compared to non-Hispanic whites [39].
Health Risks
Two studies examined the risk for developing heart disease [40] and diabetes [41]. Only one of these studies compared the risks to other racial/ethnic minority groups [40]. Bates and colleagues (1989) reported that the Hmongs’ heart disease risk is lower than that of other Southeast Asians because the Hmong have a lower mean cholesterol level compared to other Southeast Asians [40]. However, Her and Mundt (2005) reported that 41% of Hmong had abnormal blood glucose screening during their surveys, indicating an increased risk for developing diabetes [41].
Combination of Prevalence, Incidence, and/or Mortality
Six studies focused on either prevalence and incidence and/or mortality together [42–47]. These studies focused on cancer (n=4; [43–45], cardiovascular disease (n=1; [42]), and gout (n=1; [45]). All six studies compared the Hmong with other racial/ethnic minority groups.
Cancer mortality rates are high for the Hmong compared to non-Hispanic whites and Asians/Pacific Islanders. For example, nasopharyngeal cancer mortality rates are 10.4 for Hmong compared to 0.2 and 1.7/100,000 for non-Hispanic whites and Asians/Pacific Islanders, respectively [43]. Hmong women experience cervical cancer incidence and mortality rates three to four times higher than Asians/Pacific Islanders and non-Hispanic white women [44,46]. Furthermore, Hmong are more likely to be diagnosed with cancer at a later stage [43,46].
In addition, gout incidence rates are higher among the Hmong population compared to the non-Hmong population. Portis and colleagues (2004) reported that of the 204 patient chart reviews they performed, 46% of Hmong had uric acid stone disease compared to 11% of non-Hmong patients [45].
Health-Related Behavior
Health-related behavior refers to behaviors that affect an individual’s personal health and other people’s health, including health knowledge and attitudes. A total of 55 studies focused on health-related behaviors. Seven main content areas of health-related behaviors were studied among Hmong adults: (1) general health (n=2); (2) screening behavior (n=3); (3) disease treatment and management (n=5); (4) physical activity, safety, eating habits, and health (n=12); (5) structural factors (n=2); (6) socio-cultural factors (n=30); and (7) predictors of behaviors (n=1).
General Health Care Seeking
Two studies on general health care seeking behaviors focused on the Hmong people’s healthcare experiences and how these experiences influenced their healthcare seeking behaviors. Specifically, healthcare providers who were kind, caring, and had a positive attitude resulted in a positive experience for Hmong participants [48]. Some Hmong reported that when they felt they were treated differently by their provider during their health encounters, they were less willing to seek care [49].
Screening Behavior
Of the 17 studies, three examined self-reported cancer screening rates among Hmong adults. These three studies were done using surveys without any comparison groups to other racial/ethnic minorities. The Hmong self-reported low screening rates, specifically for breast and cervical cancer [50–52]. Two California-based studies found that the proportion of Hmong women who reported ever having had a clinical breast exam ranged from 50% [50] to 73% [51]. In addition, the proportion of Hmong women in this study who had had a Pap test in the last three years ranged from 61% [53] to 67% [54] in comparison to 86% of Californian women overall. Yang and colleagues revealed the Hmong in their study reported not ever receiving a colorectal exam [52]. Only 30% had ever performed a breast self-exam and only 15.8% had received a mammogram [52]. Fourteen additional studies of screening focused on socio-cultural factors related to screening behavior; this is reported in the below section.
Disease Treatment and Management
With regard to disease treatment, researchers have mainly focused on cancer treatment. Hmong adults were less likely to receive cancer treatment compared to Asians/Pacific Islanders and non-Hispanic whites [43]. For example, over 97% of Hmong patients in California chose no treatment for nasopharyngeal cancer compared to only 25.6% of Asians/Pacific Islanders and 30.3% of non-Hispanic whites [43]. Similarly, one study in California reported that only 3% of Hmong received local surgical treatment, resection, or liver transplantation for hepatocellular carcinoma compared with 22% of Asian Americans [38].
On the other hand, with regard to chronic disease management, researchers reported that medication compliance was an issue in managing chronic disease for Hmong adults. With no comparison group, one study conducted in California reported over 50% of the 323 Hmong adults were non-compliant with their prescribed hypertension medications [55]. Another study reported that the Hmong prefer traditional Hmong remedies such as herbs, including plants and tree roots, to treat diabetes [56]. Grazier, Armenian, & Vohra (2014) reported that Hmong markets in Minnesota sold medications that were not approved by the FDA [57].
Physical Activity, Safety, Eating Habits, and Health
Of the 12 studies, seven studies examined eating practices [58–62]; two examined physical activity [63,64]; and three safety and occupational health [65,66,66]. These studies investigated how different factors influence health. Specifically, the studies were concerned with how food habits, food culture, acculturation, health [62], and environmental factors influence eating habits and body mass index (BMI), and how all these factors affect health [67,68]. In addition, one study examined ways to promote physical activity [69].
Researchers found that acculturation and environmental factors limited the Hmong people’s ability to engage in healthy behavior, documenting that Hmong generally perceived Hmong food as healthy and American food as not healthy [62]. However, acculturation and environmental change affected Hmong adults’ eating habits [58,62,70,71]. Specifically, the Hmong have transitioned from a food-insecure environment to “a more food-secure, obesogenic environment” that has negatively affected their eating and purchasing habits [62,70].
Furthermore, food-borne illness was new to the Hmong. Perez and colleagues (2006) reported that Hmong participants did not understand the direct relationship between bacteria and food-borne illnesses [59].
In addition, one study of physical activity found that safety concerns and lack of public spaces for physical activities were significant barriers to maintaining good health for Hmong participants [69]. Furthermore, Hmong people reported a loss of health, healthy habits, and traditions through exposure to the American lifestyle, particularly the lack of physical activity and poor diet, resulting in the development of diabetes [60,63,72].
Neitzel and colleagues (2014) reported that many Hmong continue farming in the US [65]. Netizel and colleagues observed musculoskeletal hazards that may pose health problems for Hmong adults while doing farm work. These hazards included constant hand gripping and bending at the back and lifting <50 pounds.
Structural factors
Two of the 55 studies reported that structural factors prevented the Hmong from participating in health-related behaviors. For example, Okunseri and colleagues (2008) reported lack of access to dental health [73]. Sugerman and colleagues (2011) reported Hmong had poor access to information [74]. Hmong participants reported receiving most of their information from the radio.
Socio-cultural factors
Thirty of the 55 studies investigated factors that affected health-related behaviors of Hmong adults, including socio-cultural factors and predictors of behaviors. Because researchers reported similar findings across each content area with regard to socio-cultural factors, each factor was discussed separately.
Knowledge and Attitudes
With regard to screening, four studies reported that Hmong adults had never heard of cancer or the causes of cancer and, consequently, did not understand the importance of screening [75–78]. Furthermore, there was no word for “cancer” in the Hmong language [79].
Schroepfer and colleagues (2010) used a nine-stage scale to assess the Wisconsin Hmong community’s stages of readiness to address cancer. They reported that the Hmong people’s stage of readiness to address cancer was “vague awareness.” Many Hmong women expressed embarrassment about screening, as well as fear of dealing with the screening results [51,75,79,80]. Thorburn and colleagues (2013) reported that over 50% of their participants were able to seek information about breast and cervical cancer screening from their peers, healthcare professionals, and the internet [81]. Similarly, Maxwell and colleagues revealed that only 45% of Hmong reported having ever heard of hepatitis B [82].
With regard to chronic disease management, researchers reported that Hmong participants had no knowledge of diabetes [56,83,84] or hypertension [85], and when diagnosed, often believed they could be cured with traditional medicine and that chronic management was unnecessary. This often resulted in poor management [55]. One study reported that 38% of Hmong participants were unaware of the causes of osteoporosis, attributing it to fate, chance, or luck compared to 18% of Vietnamese participants with similar beliefs [86]. Similarly, the Hmong reported that they did not understand that kidney stone development was a chronic health problem [87].
With regard to smoking, the Hmong reported a low level of awareness of resources for smoking cessation [88]. Moreover, there are gender and acculturation differences in smoking cessation [89]; for example, women are more concerned about revealing their smoking status due to cultural prohibition. Smoking norms in the Hmong community also shifted after the war in Laos from being acceptable to being less acceptable [90].
Cultural Practices and Beliefs
Six studies reported that the Hmong participants’ cultural practices and beliefs were barriers to screening [51,79,91–95]. Cultural beliefs about the privacy of body parts and the common practice of women deferring to their husbands and children often prevented women from seeking breast and cervical cancer screening [95,96].
Cultural beliefs also influenced chronic disease management. Wong and colleagues reported that Hmong participants believed hypertension was caused by “bad blood” [55] and that diabetes was caused by a change in weather and environment, as well as stress [84,97].
Cultural practices also influenced Hmong adults’ treatment decisions and who they sought care from. For example, Burgess and colleagues (2014) reported that Hmong patients prefer to use their herbal medicines instead of invasive urological procedures for kidney stones. In addition, the Hmong continue to seek care from shamans for physical, emotional, and psychological complaints as well as health information before seeking care from a western care provider [98–100].
Furthermore, culture also played an important role in promoting healthy aging. One study reported that the Hmong people’s collectivist culture of positive family relationships, maintenance of group harmony, family interdependence, and filial piety played a role in promoting healthy aging for Hmong elders [101].
Language Barrier
Language was also a barrier identified in nine studies [50,73,79,91,94,98,102–104]. Regarding language, women reported three types of barriers: (1) a lack of specific language for discussing cancer (i.e., there is no literal translation of the word “cancer” in the Hmong language) and health screening; (2) hurtful experiences related to their status as English language learners; and (3) inaccessible or poor-quality interpreters.
Predictors of Behaviors
One study examined predictors of perceived barriers to immunizations among parents of Hmong children in California [105]. Predictors of perceived barriers included (1) access to immunization; (2) concerns about vaccines; and (3) belief that immunization is not important. Researchers reported that the socio-economic position and the use of traditional health care (e.g., consulting with shamans and herbalists) were significant barriers for Hmong parents to immunize their children [105].
DISCUSSION
This systematic review provides a context for understanding the health status of the Hmong adult population in the United States. The review revealed evidence indicating that the Hmong adult population in the US experiences significant and wide-ranging health disparities, specifically in the areas of cancer and hepatitis B compared to non-Hispanic whites and some Asian groups. This review also identified a variety of factors (e.g., no knowledge, cultural factors, and language barriers) that may contribute to health disparities among the Hmong adult population. This is the first systematic review to focus on Hmong health promotion and disease prevention in the United States.
The state with the largest Hmong population, California [16], contributed the most research on the Hmong population, including health data. Specifically, cancer disease data from cancer registries in California may have greatly raised awareness among healthcare providers of prevalent cancers among Hmong adults in the US. Perhaps this explains why there is a larger number studies focused on cancer.
Although health-related behavior received the most attention from researchers (55 of 71 studies), researchers have also focused on cancer prevention, in particular breast and cervical cancers, followed by diabetes. Again, this can be explained by the fact that the published studies on cancer incidence, prevalence, and mortality rates have lured researchers to focusing on cancer, including prevention and cancer screening behaviors, instead of other health outcomes such as hypertension management.
Cultural factors and language barriers were the most frequently mentioned barrier to seeking healthcare and managing chronic diseases in both the qualitative and the quantitative studies that were reviewed. These factors are consistent with the existing literature that cultural values, beliefs, and traditional health practices can influence health care utilization [106–109]. Furthermore, this literature review showed that the Hmong have limited knowledge about Western health conditions, including cancer, diabetes, and hypertension, affecting their health behaviors. This finding is consistent with other racial/ethnic minority groups [110–112] and those with limited education [113]. Thus, the current level of knowledge affords opportunities for interventions to address cultural and language issues as well as to improve knowledge about health conditions, thereby reducing health disparities among the Hmong adult population.
On the other hand, current methods and research questions studied among the Hmong adult populations are still at the descriptive level and use cross-sectional designs. Thus, there is insufficient knowledge about the patterns and interactions of health problems, socio-cultural, and structural factors that influence health behaviors among the Hmong population. In addition, additional studies are needed comparing the Hmong population with other groups of racial/ethnic minorities to understand the extent of disparities between and across groups.
Of the 21 survey studies reviewed, none of them addressed issues related to illiteracy in the Hmong population. Only 13 studies reported using surveys translated into the Hmong language, bilingual Hmong research assistants, or conducting the survey face to face with participants. One study excluded individuals who could read or write in English or Hmong [105]. While excluding those who cannot read or write in English is a common inclusion criterion in survey research, this current, traditional methodology for the collection of data may not be culturally appropriate for Hmong adults because they have an oral culture with no written language [114]. Thus, researchers may end up aggregating subgroup populations because participants are either low literate or illiterate, preventing them from participating in surveys. More research focused on testing culturally and linguistically appropriate data collection methods is needed to increase inclusion of this population.
Implications for Applied Practice
This systematic review revealed that health registries and charts from the state and within health organizations have allowed researchers to disaggregate data to understand Hmong people’s health. However, there is still an underlying problem of data collection—measures of race and ethnicity are not collected from all racial and ethnic groups, including subgroup populations, at all levels. This challenge has been recognized [11], yet not much has been done to address it. Thus, it is important to reiterate the critical needs of health care systems in making data collection on race and ethnicity, including subgroups, a standard of practice and priority. For example, health care systems, including hospitals and public health departments, could collect data on race and ethnicity during admission for hospitalization or during enrollment in health programs. This will become crucial as big data advances and progresses, emphasizing the need for data to be collected at the clinical level.
At the national level, clinicians, researchers, and policy makers could aim to work together to change how data are collected and shared. Specifically, a culture of data-sharing and common data collection standards between cancer registries, vital records, Medicare and Medicaid data, Behavioral Risk Factor Surveillance, and hospital discharge data is needed to understand the health disparities among and between racial and ethnic minorities, including subgroup populations.
Despite the data challenge, clinicians and researchers should make the effort to include illiterate (cannot read or write in their native language or English) populations in research, including survey research. In addition, care should also be tailored for such populations. Research has documented that individuals with low literacy have poor self-management skills and preventive behaviors [115–117]. They are therefore more likely to experience health disparities.
Limitations of this Literature Review
There are limitations to this research review. Because this paper only focused on the adult population, findings cannot be generalized to the entire Hmong population in the US. Because the research used broad search terms: “health,” “health promotion,” “health risks,” “disease prevalence,” “screening,” and “disease prevention,” some research related to health promotion and disease prevention may not have been included. In addition, because the NIH’s definition of health promotion and disease prevention did not provide a specific definition for each domain, other relevant studies that may not fall under the NIH’s definition may have been excluded. Furthermore, many of the quantitative studies, including the prevalence and incidence studies, came from the same data source (e.g., cancer registry). Thus, there may be a threat of validity to the review.
CONCLUSION
This systematic review confirms that the Hmong adult population experiences health disparities. Efforts are urgently needed to increase research and develop a deeper understanding of the health issues faced by the Hmong adult population and to develop culturally salient and linguistically responsive health interventions for them. Policies are also needed to allow data to be collected on subgroup populations. The inability to collect data and identify the Hmong population within large surveys will contribute to the widening gap of health disparities in subgroup racial and ethnic minority populations as they become invisible to policy makers, researchers, and funders.
Footnotes
COMPLIANCE WITH ETHICAL STANDARDS: This article does not contain any studies with human participants or animals performed by any of the authors.
CONFLICTS OF INTEREST: The author of this paper declares that there is no conflict of interest. This study was funded by the National Institute of Nursing Research (NINR), Grant # F31NR015966. This study was also partially supported by the Clinical and Translational Science Award (CTSA) program, through the National Institute of Health (NIH) National Center for Advancing Translational Sciences (NCATS), grant UL1TR000427.
References
- 1.Agency for Healthcare Research and Quality. 2014 National Healthcare Quality & Disparities Report [Internet] 2015 [cited 2016 Apr 8]. Available from: http://www.ahrq.gov/research/findings/nhqrdr/nhqdr14/index.html.
- 2.Anderson KM, editor. Institute of Medicine (U.S.), Institute of Medicine (U.S.), National Academies Press (U.S.), ebrary, Inc. How far have we come in reducing health disparities? progress since 2000: workshop summary [Internet] Washington, D.C: National Academies Press; 2012. [cited 2014 Nov 24]. Available from: http://site.ebrary.com/lib/uwriverfalls/Doc?id=10606356. [PubMed] [Google Scholar]
- 3.Care C on U and ER and ED in H, Policy B on HS, Medicine I of. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care (with CD) National Academies Press; 2009. [PubMed] [Google Scholar]
- 4.LaVeist T, Pollack K, Thorpe R, Fesahazion R, Gaskin D. Place, not race: disparities dissipate in southwest Baltimore when blacks and whites live under similar conditions. Health Aff (Millwood) 2011;30:1880–1887. doi: 10.1377/hlthaff.2011.0640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee H, Fitzpatrick JJ, Baik S-Y. Why isn’t evidence based practice improving health care for minorities in the United States? Appl Nurs Res. 2013;26:263–8. doi: 10.1016/j.apnr.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 6.National Center for Health Statistics. Health. United States, 2015 With Special Feature on Racial and Ethnic Health Disparities [Internet] 2016 Available from: https://www.cdc.gov/nchs/data/hus/hus15.pdf. [PubMed]
- 7.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System [Internet] 2016 [cited 2017 Jan 10]. Available from: https://www.cdc.gov/brfss/data_documentation/index.htm.
- 8.United States Census Bureau. Asian alone or in combination with one or more other races, and with one or more Asian categories for selected groups [Internet] 2011 [cited 2016 Dec 19]. Available from: https://en.wikipedia.org/wiki/Demographics_of_Asian_Americans.
- 9.Shi L, Stevens GD. Vulnerable Populations in the United States. 2. San Francisco: Jossey--Bass, A Wiley Imprint; 2010. [Google Scholar]
- 10.Hastings KG, Jose PO, Kapphahn KI, Frank ATH, Goldstein BA, Thompson CA, et al. Leading Causes of Death among Asian American Subgroups (2003–2011) PLoS ONE [Internet] 2015 doi: 10.1371/journal.pone.0124341. [cited 2016 Sep 22];10. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4411112/ [DOI] [PMC free article] [PubMed]
- 11.Islam NS, Khan S, Kwon S, Jang D, Ro M, Trinh-Shevrin C. Methodological Issues in the Collection, Analysis, and Reporting of Granular Data in Asian American Populations: Historical Challenges and Potential Solutions. J Health Care Poor Underserved. 2010;21:1354–81. doi: 10.1353/hpu.2010.0939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Srinivasan S, Guillermo T. Toward improved health: disaggregating Asian American and Native Hawaiian/Pacific Islander data. Am J Public Health. 2000;90:1731–4. doi: 10.2105/ajph.90.11.1731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chang ET, Keegan THM, Gomez SL, Le GM, Clarke CA, So SKS, et al. The burden of liver cancer in Asians and Pacific Islanders in the Greater San Francisco Bay Area, 1990 through 2004. Cancer. 2007;109:2100–8. doi: 10.1002/cncr.22642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bachrach D, Pfister H, Wallis K, Lipson M. Addressing Patients’ Social Needs An Emerging Business Care for Provider Investment [Internet] 2014 May; Available from: http://www.manatt.com/uploadedFiles/Content/5_News_and_Events/Newsletters/Medicaid_Update/Addressing-Patients-Social-Needs-An-Emerging-Business-Case-for-Provider-Investment.pdf.
- 15.Hamilton-Merritt J. Tragic Mountains: The Hmong, the Americans, and the Secret Wars for Laos, 1942–1992. Indiana University Press; 1993. [Google Scholar]
- 16.Hmong National Development Inc. The state of the Hmong American community 2013. 2010. [Google Scholar]
- 17.National Asian Pacific Center on Aging. National Asian Pacific Center on Aging Annual Report 2012–2013. 2014. [Google Scholar]
- 18.U.S. Census Bureau. 2013 American Community Survey 1-Year Estimates. 2013. [Google Scholar]
- 19.Southeast Asia Resource Action Center. Southeast Asian American At A Glance: Statistics on Southeast Asians adapated from the American Community Survey. 2011. [Google Scholar]
- 20.US Census Bureau Public Information. Facts for Features: Asian/Pacific American Heritage Month: May 2011 - Facts for Features & Special Editions - Newsroom. U.S. Census Bureau; 2011. [Google Scholar]
- 21.United States National Archives and Records Administration. Executive Order 13515--Increasing Participation of Asian Americans and Pacific Islanders in Federal Programs [Internet] 2009:1–6. Available from: https://www.gpo.gov/fdsys/pkg/FR-2009-10-19/pdf/E9-25268.pdf.
- 22.Moher D, Liberati A. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern …. 2009 [PMC free article] [PubMed] [Google Scholar]
- 23.Welch V, Petticrew M, Petkovic J, Moher D, Waters E, White H, et al. Extending the PRISMA statement to equity-focused systematic reviews (PRISMA-E 2012): explanation and elaboration. Int J Equity Health. 2015;14:92. doi: 10.1186/s12939-015-0219-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.National Institutes of Health Office of Disease Prevention. Prevention Research at the NIH [Internet] 2016 Available from: https://prevention.nih.gov/prevention-research.
- 25.Lee GY. Diaspora and the predicament of origins: Interrogating Hmong postcolonial history and identity. Hmong Stud J. 2007:8. [Google Scholar]
- 26.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–57. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 27.Albright JW. Interactions of overweight, poor oral health, and stress related to chronic disease in an aging population. Curr Gerontol Geriatr Res. 2010;2010:614814. doi: 10.1155/2010/614814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Constantine ML, Rockwood TH, Schillo BA, Alesci N, Foldes SS, Phan T, et al. Exploring the relationship between acculturation and smoking behavior within four Southeast Asian communities of Minnesota. Nicotine Tob Res Off J Soc Res Nicotine Tob. 2010;12:715–23. doi: 10.1093/ntr/ntq070. [DOI] [PubMed] [Google Scholar]
- 29.Rooney BL, Choudhary R. Social Determinants of Smoking among Hmong americans residing in Wisconsin. Wis Med J. 2009;28:439–46. [PubMed] [Google Scholar]
- 30.Sheikh M, Mouanoutoua M, Walvick M, Khang L, Singh J, Stoltz S, et al. Prevalence of Hepatitis B Virus (HBV) Infection Among Hmong Immigrants in the San Joaquin Valley. J Community Health. 2011;36:42–6. doi: 10.1007/s10900-010-9283-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sheikh MY, Atla PR, Ameer A, Sadiq H, Sadler PC. Seroprevalence of Hepatitis B and C Infections among Healthy Volunteer Blood Donors in the Central California Valley. Gut Liver. 2013;7:66–73. doi: 10.5009/gnl.2013.7.1.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sheikh M, Atla P, Raoufi R, Sadiq H, Sadler P. Prevalence of Hepatitis B Infection Among Young and Unsuspecting Hmong Blood Donors in the Central California Valley. J Community Health. 2012;37:181–1855p. doi: 10.1007/s10900-011-9434-y. [DOI] [PubMed] [Google Scholar]
- 33.Thao K, Arndt B, Tandis A, Hanrahan L. The Prevalence of Type 2 Diabetes Mellitus in a Wisconsin Hmong Patient Population. Wis Med J. 2015;114:190–5. [PubMed] [Google Scholar]
- 34.Wahedduddin S, Singh JA, Culhane-Pera KA, Gertner E. Gout in the Hmong in the United States. J Clin Rheumatol Pract Rep Rheum Musculoskelet Dis. 2010;16:262–6. doi: 10.1097/RHU.0b013e3181eeb487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gjerdingen DK, Lor V. Hepatitis B status of Hmong patients. J Am Board Fam Pract Am Board Fam Pract. 1997;10:322–8. [PubMed] [Google Scholar]
- 36.Mills PK, Yang R. Cancer incidence in the Hmong of Central California, United States, 1987–94. Cancer Causes Control CCC. 1997;8:705–12. doi: 10.1023/a:1018423219749. [DOI] [PubMed] [Google Scholar]
- 37.Ross JA, Xie Y, Kiffmeyer WR, Bushhouse S, Robison LL. Cancer in the Minnesota Hmong population. Cancer. 2003;97:3076–3079. doi: 10.1002/cncr.11443. [DOI] [PubMed] [Google Scholar]
- 38.Kwong SL, Stewart SL, Aoki CA, Chen MS. Disparities in hepatocellular carcinoma survival among Californians of Asian ancestry, 1988 to 2007. Cancer Epidemiol Biomark Prev Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol. 2010;19:2747–57. doi: 10.1158/1055-9965.EPI-10-0477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yang RC, Mills PK, Nasseri K. Patterns of Mortality in California Hmong, 1988–2002. J Immigr Minor Health. 2010;12:754–60. doi: 10.1007/s10903-009-9230-2. [DOI] [PubMed] [Google Scholar]
- 40.Bates SR, Hill L, Barrett-Connor E. Cardiovascular disease risk factors in an Indochinese population. Am J Prev Med. 1989;5:15–20. [PubMed] [Google Scholar]
- 41.Her C, Mundt M. Risk prevalence for type 2 diabetes mellitus in adult Hmong in Wisconsin: a pilot study. WMJ Off Publ State Med Soc Wis. 2005;104:70–7. [PubMed] [Google Scholar]
- 42.Culhane-Pera K, Moua M, DeFor T, Desai J. Cardiovascular disease risks in Hmong refugees from Wat Tham Krabok, Thailand. J Immigr Minor Health. 2009;11:372–379 8p. doi: 10.1007/s10903-008-9211-x. [DOI] [PubMed] [Google Scholar]
- 43.Dodge JL, Mills PK, Yang RC. Nasopharyngeal cancer in the California Hmong, 1988–2000. Oral Oncol. 2005;41:596–601. doi: 10.1016/j.oraloncology.2005.01.009. [DOI] [PubMed] [Google Scholar]
- 44.Mills PK, Yang RC, Riordan D. Cancer incidence in the Hmong in California, 1988–2000. Cancer. 2005;104:2969–74. doi: 10.1002/cncr.21525. [DOI] [PubMed] [Google Scholar]
- 45.Portis AJ, Hermans K, Culhane-Pera KA, Curhan GC. Rapid Communication: Stone Disease in the Hmong of Minnesota: Initial Description of a High-Risk Population. J Endourol. 2004;18:853–7. doi: 10.1089/end.2004.18.853. [DOI] [PubMed] [Google Scholar]
- 46.Yang RC, Mills PK, Riordan DG. Cervical cancer among Hmong women in California, 1988 to 2000. Am J Prev Med. 2004;27:132–8. doi: 10.1016/j.amepre.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 47.Yang RC, Mills PK, Riordan DG. Gastric adenocarcinoma among Hmong in California, USA, 1988–2000. Gastric Cancer. 2005;8:117–23. doi: 10.1007/s10120-005-0314-y. [DOI] [PubMed] [Google Scholar]
- 48.Barrett B, Shadick K, Schilling R, Spencer L, del Rosario S, Moua K, et al. Hmong/medicine interactions: improving cross-cultural health care. Fam Med. 1998;30:179–84. [PubMed] [Google Scholar]
- 49.Thorburn S, Kue J, Keon KL, Lo P. Medical mistrust and discrimination in health care: A qualitative study of Hmong women and men. J Community Health Publ Health Promot Dis Prev. 2012;37:822–9. doi: 10.1007/s10900-011-9516-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tanjasiri SP, Kagawa-Singer M, Foo MA, Chao M, Linayao-Putman I, Lor Y, et al. Breast cancer screening among Hmong women in California. J Cancer Educ. 2001;16:50–54 5p. doi: 10.1080/08858190109528725. [DOI] [PubMed] [Google Scholar]
- 51.Lee HY, Vang S. Cultural Beliefs and Clinical Breast Examination in Hmong American Women: The Crucial Role of Modesty. J. Immigr. Minor. Health Cent Minor Public Health. 2013 doi: 10.1007/s10903-013-9890-9. [DOI] [PubMed] [Google Scholar]
- 52.Yang RC, Mills PK, Dodge JL. Cancer screening, reproductive history, socioeconomic status, and anticipated cancer-related behavior among Hmong adults. Asian Pac J Cancer Prev APJCP. 2006;7:79–85. [PubMed] [Google Scholar]
- 53.Fang DM, Lee S, Stewart S, Ly MY, Chen MS. Factors associated with pap testing among Hmong women. J Health Care Poor Underserved. 2010;21:839–50. doi: 10.1353/hpu.0.0338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lee Hee Yun, Yang Pa Nhia, Lee Do Kyung, Ghebre Rahel. Cervical Cancer Screening Behavior among Hmong-American Immigrant Women. Am J Health Behav. 2015;39:301–307 7p. doi: 10.5993/AJHB.39.3.2. [DOI] [PubMed] [Google Scholar]
- 55.Wong CC, Mouanoutoua V, Chen MJ, Gray K, Tseng W. Adherence with hypertension care among Hmong Americans. J Community Health Nurs. 2005;22:143–56. doi: 10.1207/s15327655jchn2203_2. [DOI] [PubMed] [Google Scholar]
- 56.Perez MA, Cha K. Exploring diabetes knowledge, beliefs, and treatments of the Hmong Population: An exploratory study. Hmong Stud J. 2007;8:1–21. [Google Scholar]
- 57.Grazier MR, Armenian P, Vohra R. Illicit Distribution of Prescription Drugs: Report of Inadvertent Chloroquine Toxicity and a Market Survey of Businesses Serving Ethnic Minority Populations. Ann Pharmacother. 2014;48:1070–6. doi: 10.1177/1060028014535908. [DOI] [PubMed] [Google Scholar]
- 58.Ikeda JP, Ceja DR, Glass RS, Hardwood JO, Lucke KA, Sutherlin JM. Food habits of the Hmong living in central California. J Nutr Educ. 1991;23:168–175. [Google Scholar]
- 59.Perez MA, Moua LJ, Pinzon-Perez H. Food Preparation, Practices, and Safety In The Hmong Community. Hmong Stud J. 2006;7:1–24. [Google Scholar]
- 60.Pham KL, Harrison GG, Kagawa-Singer M. Perceptions of diet and physical activity among California Hmong adults and youths. Prev Chronic Dis. 2007;4:A93. [PMC free article] [PubMed] [Google Scholar]
- 61.Story M, Harris LJ. Food habits and dietary change of Southeast Asian refugee families living in the United States. J Am Diet Assoc. 1989;89:800–3. [PubMed] [Google Scholar]
- 62.Vue W, Wolff C, Goto K. Hmong Food Helps Us Remember Who We Are: Perspectives of Food Culture and Health among Hmong Women with Young Children. J Nutr Educ Behav. 2011;43:199–204. doi: 10.1016/j.jneb.2009.10.011. [DOI] [PubMed] [Google Scholar]
- 63.Devlin H, Roberts M, Okaya A, Xiong YM. Our Lives Were Healthier Before: Focus Groups With African American, American Indian, Hispanic/Latino, and Hmong People With Diabetes. Health Promot Pract. 2006;7:47–55. doi: 10.1177/1524839905275395. [DOI] [PubMed] [Google Scholar]
- 64.Van Duyn MAS, McCrae T, Wingrove BK, Henderson KM, Boyd JK, Kagawa-Singer M, et al. Adapting evidence-based strategies to increase physical activity among African Americans, Hispanics, Hmong, and Native Hawaiians: a social marketing approach. Prev Chronic Dis. 2007;4:A102. [PMC free article] [PubMed] [Google Scholar]
- 65.Neitzel RL, Krenz J, de Castro AB. Safety and Health Hazard Observations in Hmong Farming Operations. J Agromedicine. 2014;19:130–49. doi: 10.1080/1059924X.2014.886319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.De Castro AB, Krenz MJ, Neitzel RL. Assessing Hmong farmers’ safety and health. Workplace Health Saf. 2014;62:178. doi: 10.3928/21650799-20140422-02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Franzen L, Smith C. Acculturation and environmental change impacts dietary habits among adult Hmong. Appetite. 2009;52:173–83. doi: 10.1016/j.appet.2008.09.012. [DOI] [PubMed] [Google Scholar]
- 68.Franzen L, Smith C. Food system access, shopping behavior, and influences on purchasing groceries in adult Hmong living in Minnesota. Am J Health Promot AJHP. 2010;24:396–409. doi: 10.4278/ajhp.080710-QUAL-121. [DOI] [PubMed] [Google Scholar]
- 69.Van Duyn MAS, McCrae T, Wingrove BK, Henderson KM, Boyd JK, Kagawa-Singer M, et al. Adapting evidence-based strategies to increase physical activity among African Americans, Hispanics, Hmong, and Native Hawaiians: a social marketing approach. Prev Chronic Dis. 2007;4:A102. [PMC free article] [PubMed] [Google Scholar]
- 70.Franzen L, Smith C. Food System Access, Shopping Behavior, and Influences on Purchasing Groceries in Adult Hmong Living in Minnesota. Am J Health Promot. 2010;24:396–409. doi: 10.4278/ajhp.080710-QUAL-121. [DOI] [PubMed] [Google Scholar]
- 71.Franzen L, Smith C. Acculturation and environmental change impacts dietary habits among adult Hmong. Appetite. 2009;52:173–83. doi: 10.1016/j.appet.2008.09.012. [DOI] [PubMed] [Google Scholar]
- 72.Perez MA, Thao C. Understanding Barriers to prevention of ntshav qab zib / nsthaav qaab zib: A Hmong Perspective. Hmong Stud J. 2009;10:1–23. [Google Scholar]
- 73.Okunseri C, Yang M, Gonzalez C, LeMay W, Iacopino AM. Hmong adults self-rated oral health: a pilot study. J Immigr Minor Health Cent Minor Public Health. 2008;10:81–8. doi: 10.1007/s10903-007-9054-x. [DOI] [PubMed] [Google Scholar]
- 74.Sugerman S, Backman D, Foerster SB, Ghirardelli A, Linares A, Fong A. Using an opinion poll to build an obesity-prevention social marketing campaign for low-income Asian and Hispanic immigrants: report of findings. J Nutr Educ Behav. 2011;43:S53–66. doi: 10.1016/j.jneb.2011.02.007. [DOI] [PubMed] [Google Scholar]
- 75.Lor M, Khang PY, Xiong P, Moua KF, Lauver D. Understanding Hmong women’s beliefs, feelings, norms, and external conditions about breast and cervical cancer screening. Public Health Nurs. 2013;30:420–8. doi: 10.1111/phn.12043. [DOI] [PubMed] [Google Scholar]
- 76.Kue J, Zukoski A, Keon KL, Thorburn S. Breast and cervical cancer screening: exploring perceptions and barriers with Hmong women and men in Oregon. Ethn Health. 2014;19:311–27. doi: 10.1080/13557858.2013.776013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Vang T, Pinzon-Perez H. Knowledge of nasopharyngeal carcinoma among Hmong populations in central California. Hmong Stud J. 2006;7:1–24. [Google Scholar]
- 78.Schroepfer TA, Waltz A, Noh H, Matloub J, Kue V. Seeking to bridge two cultures: the Wisconsin Hmong cancer experience. J Cancer Educ Off J Am Assoc Cancer Educ. 2010;25:609–16. doi: 10.1007/s13187-010-0102-1. [DOI] [PubMed] [Google Scholar]
- 79.Baisch MJ, Vang PC, Peterman BR. An Exploration of Hmong Women’s Perspectives on Cancer. Asian Nurs Res. 2008;2:82–91. doi: 10.1016/S1976-1317(08)60032-8. [DOI] [PubMed] [Google Scholar]
- 80.Vang P. Using Mammography Screening: Hmong Women’s Perceptions and Beliefs. Hmong Stud J. 2009;10:1–29. [Google Scholar]
- 81.Thorburn S, Keon KL, Kue J. Sources of breast and cervical cancer information for hmong women and men. Women Health. 2013;53:468–78. doi: 10.1080/03630242.2013.796305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Maxwell AE, Stewart SL, Glenn BA, Wong WK, Yasui Y, Chang LC, et al. Theoretically informed correlates of hepatitis B knowledge among four Asian groups: the health behavior framework. Asian Pac J Cancer Prev APJCP. 2012;13:1687–92. doi: 10.7314/apjcp.2012.13.4.1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Helsel D, Mochel M, Bauer R. Chronic Illness and Hmong Shamans. J Transcult Nurs. 2005;16:150–4. doi: 10.1177/1043659604273553. [DOI] [PubMed] [Google Scholar]
- 84.Yang A, Xiong D, Vang E, Pharris MD. Hmong American Women Living With Diabetes. J Nurs Scholarsh. 2009;41:139–48. doi: 10.1111/j.1547-5069.2009.01265.x. [DOI] [PubMed] [Google Scholar]
- 85.Wong CC, Mouanoutoua V, Chen M-J, Gray K, Tseng W. Adherence with Hypertension Care among Hmong Americans. J Community Health Nurs. 2005;22:143–56. doi: 10.1207/s15327655jchn2203_2. [DOI] [PubMed] [Google Scholar]
- 86.Nguyen DN, O’Connell MB. Asian and Asian-American college students’ awareness of osteoporosis. Pharmacotherapy. 2002;22:1047–54. doi: 10.1592/phco.22.12.1047.33608. [DOI] [PubMed] [Google Scholar]
- 87.Culhane-Pera KA, Lee M. Die Another Day”: A qualitative analys is of Hmong experiences with kidney stones. Hmong Stud J. 2006;7:1–34. [Google Scholar]
- 88.Fu SS, Burgess D, van Ryn M, Hatsukami DK, Solomon J, Joseph AM. Views on smoking cessation methods in ethnic minority communities: A qualitative investigation. Prev Med. 2007;44:235–40. doi: 10.1016/j.ypmed.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 89.Burgess D, Fu SS, Joseph AM, Hatsukami DK, Solomon J, van Ryn M. Understanding smoking and cessation among Hmong smokers. J Health Care Poor Underserved. 2008;19:442–51. doi: 10.1353/hpu.0.0022. [DOI] [PubMed] [Google Scholar]
- 90.Burgess DJ, Mock J, Schillo BA, Saul JE, Phan T, Chhith Y, et al. Culture, acculturation and smoking use in Hmong, Khmer, Laotians, and Vietnamese communities in Minnesota. BMC Public Health. 2014;14:791. doi: 10.1186/1471-2458-14-791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Fang DM, Baker DL. Barriers and facilitators of cervical cancer screening among women of Hmong origin. J Health Care Poor Underserved. 2013;24:540–55. doi: 10.1353/hpu.2013.0067. [DOI] [PubMed] [Google Scholar]
- 92.Kue J, Zukoski A, Keon KL, Thorburn S. Breast and cervical cancer screening: exploring perceptions and barriers with Hmong women and men in Oregon. Ethn Health. 2014;19:311–27. doi: 10.1080/13557858.2013.776013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Lee HY, Vang S. Cultural Beliefs and Clinical Breast Examination in Hmong American Women: The Crucial Role of Modesty. J Immigr Minor Health Cent Minor Public Health. 2013 doi: 10.1007/s10903-013-9890-9. [DOI] [PubMed] [Google Scholar]
- 94.Lor M, Khang PY, Xiong P, Moua KF, Lauver D. Understanding Hmong Women’s Beliefs, Feelings, Norms, and External Conditions About Breast and Cervical Cancer Screening. Public Health Nurs. 2013 doi: 10.1111/phn.12043. n/a–n/a. [DOI] [PubMed] [Google Scholar]
- 95.Vang PC. Using Mammography Screening: Hmong Women’s Perceptions and Beliefs. Hmong Stud J. 2009;10:1–29. [Google Scholar]
- 96.Lor M, Khang PY, Xiong P, Moua KF, Lauver D. Understanding Hmong Women’s Beliefs, Feelings, Norms, and External Conditions About Breast and Cervical Cancer Screening. Public Health Nurs. 2013;30:420–428 9p. doi: 10.1111/phn.12043. [DOI] [PubMed] [Google Scholar]
- 97.Culhane-Pera KA, Her C, Her B. “We are out of balance here”: a Hmong cultural model of diabetes. J Immigr Minor Health Cent Minor” Public Health. 2007;9:179–90. doi: 10.1007/s10903-006-9029-3. [DOI] [PubMed] [Google Scholar]
- 98.Johnson SK. Hmong Health Beliefs and Experiences in the Western Health Care System. J Transcult Nurs. 2002;13:126–32. doi: 10.1177/104365960201300205. [DOI] [PubMed] [Google Scholar]
- 99.Plotnikoff GA, Numrich C, Wu C, Yang D, Xiong P. Hmong shamanism Animist spiritual healing in Minnesota. Minn Med. 2002;85:29–34. [PubMed] [Google Scholar]
- 100.Helsel DG, Mochel M, Bauer R. Shamans in a Hmong American Community. J Altern Complement Med. 2004;10:933–8. doi: 10.1089/acm.2004.10.933. [DOI] [PubMed] [Google Scholar]
- 101.Nguyen AL, Seal DW. Cross-cultural comparison of successful aging definitions between Chinese and Hmong elders in the United States. J Cross-Cult Gerontol. 2014;29:153–71. doi: 10.1007/s10823-014-9231-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Baker D, Dang M, Ly M, Diaz R. Perception of barriers to immunization among parents of Hmong origin in California. Am J Public Health. 2010;100:839–45. doi: 10.2105/AJPH.2009.175935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kagawa-Singer M, Tanjasiri SP, Valdez A, Yu H, Foo MA. Outcomes of a Breast Health Project for Hmong Women and Men in California. Am J Public Health. 2009;99:S467–73. doi: 10.2105/AJPH.2008.143974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Schroepfer TA, Waltz A, Noh H, Matloub J, Kue V. Seeking to Bridge Two Cultures: The Wisconsin Hmong Cancer Experience. J Cancer Educ. 2010;25:609–16. doi: 10.1007/s13187-010-0102-1. [DOI] [PubMed] [Google Scholar]
- 105.Baker DL, Dang MT, Ly MY, Diaz R. Perception of barriers to immunization among parents of Hmong origin in California. Am J Public Health. 2010;100:839–45. doi: 10.2105/AJPH.2009.175935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Chung VCH, Ma PHX, Lau CH, Wong SYS, Yeoh EK, Griffiths SM. Views on traditional Chinese medicine amongst Chinese population: a systematic review of qualitative and quantitative studies. Health Expect. 2014;17:622–36. doi: 10.1111/j.1369-7625.2012.00794.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kujawska M, Pardo-de-Santayana M. Management of medicinally useful plants by European migrants in South America. J Ethnopharmacol. 2015;172:347–55. doi: 10.1016/j.jep.2015.06.037. [DOI] [PubMed] [Google Scholar]
- 108.Lor M, Xiong P, Park L, Schwei RJ, Jacobs EA. Western or Traditional Healers? Understanding Decision Making in the Hmong Population. West J Nurs Res. 2016 doi: 10.1177/0193945916636484. 0193945916636484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Sackett K, Carter M, Stanton M. Elders’ Use of Folk Medicine and Complementary and Alternative Therapies: An Integrative Review With Implications for Case Managers. Prof Case Manag. 2014;19:113–23. doi: 10.1097/NCM.0000000000000025. [DOI] [PubMed] [Google Scholar]
- 110.Al-Maskari F, El-Sadig M, Al-Kaabi JM, Afandi B, Nagelkerke N, Yeatts KB. Knowledge, Attitude and Practices of Diabetic Patients in the United Arab Emirates. PLOS ONE. 2013;8:e52857. doi: 10.1371/journal.pone.0052857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Flynn SJ, Ameling JM, Hill-Briggs F, Wolff JL, Bone LR, Levine DM, et al. Facilitators and barriers to hypertension self-management in urban African Americans: perspectives of patients and family members. 2013 doi: 10.2147/PPA.S46517. [cited 2017 May 15]; Available from: https://dukespace.lib.duke.edu/dspace/handle/10161/8327. [DOI] [PMC free article] [PubMed]
- 112.Leung L. Diabetes mellitus and the Aboriginal diabetic initiative in Canada: An update review. J Fam Med Prim Care. 2016;5:259–65. doi: 10.4103/2249-4863.192362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Basu Knowledge of diabetes among diabetic patients in government hospitals of Delhi. 2017;2:8–10. [Google Scholar]
- 114.Yang D. Hmong at the turning point. In: Blake Point JL., editor. Hmong Turn. Minneapolis, MN: World Bridge Associate; 1993. pp. 230–40. [Google Scholar]
- 115.McNaughton CD, Jacobson TA, Kripalani S. Low literacy is associated with uncontrolled blood pressure in primary care patients with hypertension and heart disease. Patient Educ Couns. 2014;96:165–70. doi: 10.1016/j.pec.2014.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Zhang NJ, Terry A, McHorney CA. Impact of Health Literacy on Medication Adherence: A Systematic Review and Meta-analysis. Ann Pharmacother. 2014;48:741–51. doi: 10.1177/1060028014526562. [DOI] [PubMed] [Google Scholar]
- 117.Oldach BR, Katz ML. Health literacy and cancer screening: A systematic review. Patient Educ Couns. 2014;94:149–57. doi: 10.1016/j.pec.2013.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]