Abstract
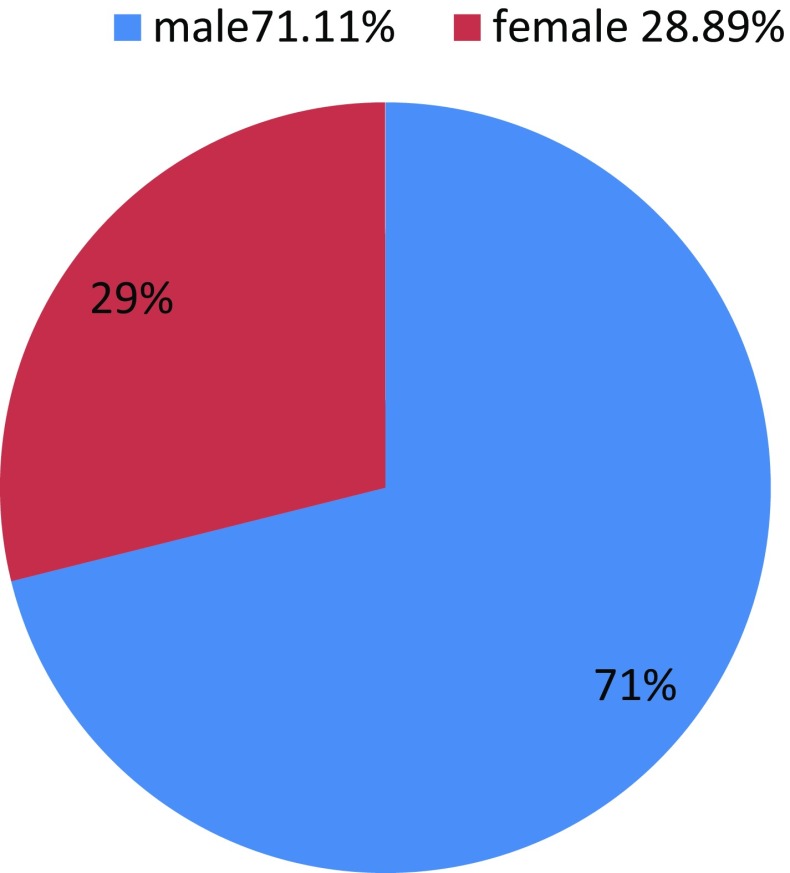
This study is intended to analyze the clinical profile and outcomes of deep neck space infection in diabetic patients in our tertiary care centre. A prospective study of 1 year duration from 30th September 2015 to 30th September 2016 at department of Otorhinolaryngology, Gauhati Medical College and Hospital, Guwahati. A total of 45 diabetic patients who presented with DNSI are included in this study. Their demographic profile, etiology, bacteriology, treatment, duration of hospital stay, complications and outcomes have been analyzed. 45 patients were recorded; 32 (71.11%) were men, and 13 (45%) were women, with a mean age of 63.27 ± 7.55 years. There were 30 patients (66.67%) who had associated systemic diseases apart from diabetes mellitus. The parapharyngeal space in 13 patients (28.89%) was the most commonly involved space. Odontogenic infections in 18 patients (40%) and upper airway infections 9 patients (20%) were the two most common causes. Klebsiella pneumonia in 29 patients (64.44%), was the commonest organism isolated through pus cultures. All the patients except one (97.78%) came with abscess and underwent surgical drainage. One patient (2.22%) with carbuncle underwent regular dressing. Six patients (13.33%) had major complications. Those patients with other underlying systemic diseases or complications tended to have a longer hospital stay and were older. No cases of death has been reported. (mortality rate, 0%). DNSI patients with diabetes have a more severe clinical course. They are likely to have complications more frequently and a longer duration of hospital stay. In clinical practices while dealing with these patients more vigilance is required. On admission empirical antibiotics should cover K. pneumonia. Early surgical drainage remains the main method of treatment. Primary prevention can be achieved by orodental hygiene, regular dental check ups and in this part of the country by avoidance of substance abuse like tobacco chewing.
Keywords: Diabetes, Neck spaces, Klebsiella, Parapharyngeal, Odontogenic
Introduction
In the past deep neck space infections were fairly common with considerable morbidity and mortality. The advent of better diagnostic tools, availability of broad spectrum antibiotics and decision for early surgical intervention has drastically reduced the incidence. However deep neck space infections still occur relatively frequently in older patients with systemic diseases like diabetes mellitus, with a definite potential for significant morbidity and even mortality with improper or delayed treatment.
Anatomy
Neck infections can be classified as superficial and deep infections. Superficial neck infections include the skin, subcutaneous tissues and superficial fascia. Deep neck space infections (DNSI) includes the deeper neck tissues, which are surrounded by multiple layers of deep cervical fascia with potential spaces between them. According to their relationship with the hyoid bone, 11 deep spaces has been described [1].
Pathophysiology and Spread of Infection
Lymphatic spread of infection from oral cavity., face and superficial neck compartment to deep neck spaces; resulting in cervical lymphadenopathy, which may lead to suppuration and abscess formation; and penetrating injury, which can introduce the infection to the deeper neck spaces. This infection can spread through the fascial planes, and the pus accumulated can expand the potential spaces between the different layers of the deep cervical fascia. The surgical drainage to these potential spaces is complex due to proximity to Neurovascular structures and their communication to each other and other parts of body (mediastinum and coccyx) [2].
Clinical Presentation
The clinical features of DNSI are due to the mass effect of the inflamed tissues or abscess cavity on the surrounding structures and because of the direct involvement of the surrounding structures. DNSI occur in any age group but are more commonly associated with the patients with poor oral hygiene and lack of dental care. The factors responsible for complications such as mediastinal extension are older age, involvement of two or more spaces, presence of cardiovascular and pulmonary comorbidities [3].
Aetiology
Before the advent of antibiotics, tonsillar and peritonsillar infections were the commonest (70%) source of infection in cases of DNSI [4]; but now the most common cause is considered to be odontogenic [5]. Another study shows tonsillitis as the most common aetiology of DNSI in children, whereas odontogenic origin is the most common aetiology of DNSI in adults [6].
Microbiology
The pus culture reports of the deep neck space abscess is polymicrobial, mostly reflecting the oral flora; aerobic as well as anerobic organisms are isolated, and both gram positive and gram negative organisms are cultured [7, 8]. Wang et al. [7] isolated klebsiella pneumoniae in patients with DM.
Investigations
Precise localization of DNSI on clinical ground is challenging, due to the complex anatomy of neck and deep seated nature of DNSI. Thus investigations are helpful in this situation. Laboratory tests are done to confirm raised markers of infection, and blood cultures are required in septic patients. Radiological investigations include a lateral neck radiograph, ultrasound scan and computed tomography (CT). A CT scan with contrast can show the presence of air indicating abscess. It can also be helpful in differentiating the retropharyngeal adenitis from abscess, hence avoiding unnecessary surgical intervention. After the surgical drainage biopsy of the tissue should be sent for histopathological examination. The MRI scan can yield better soft tissue delineation. Arteriography is done if there is suspected involvement of major neck vascularity in the infectious process. The ultrasound scan is very useful for guided fine needle aspiration for microscopy, culture and sensitivities [9].
Surgical Drainage
Early surgical incision and drainage with antibiotics as per culture and sensitivity reports has been the mainstay of treatment. Incision and exploration sometimes risks the patient to potential injury to neurovascular bundle. Therefore before performing incision and drainage one should have thorough anatomical knowledge of the deep neck spaces of head and neck [10].
Comorbidities
DNSI are associated with other comorbid illness. The most common being Diabetes Mellitus as reported by LEE et al. in his study. According to his study the complication are more with diabetes if more than two neck spaces were involved [11]. In another study by HUANG et al. it is confirmed that patient with DNSI associated with Diabetes had longer duration of hospital stay and required intubations and tracheostomy than without DM [8].
Results
Demography
Of 45 patients, 71.11% (32 of 45) were men and 28.89% (13 of 45) were women. Their ages ranged from 37 to 70 years, with a mean age of 63.27 ± 7.55 years. The age distribution curve peaked in the sixth decade. With respect to demographic distribution, (36 of 45) patients 80% were from a rural background and (9 of 45) 20% were from an urban background. All the patients 100% were tobacco chewer (45 of 45) and 40% were tobacco smokers (18 of 45).
Types of Deep Neck Infections (Space and Character)
Abscess formation was noted in all the patients except one (97.78%) and carbuncle in nape of neck in only 1 patient (2.22%). The parapharyngeal space was the most commonly involved space of deep neck infections 28.89% (13 of 45), posterior cervical space 17.78% (8 of 45) and extended space that is involvement of more than two spaces 17.78% (8 of 45), submandibular space 13.33% (6 of 45), masticator space 6.67% (3 of 45), carotid space 6.67% (3 of 45) and nape of neck 6.67% (3 of 45). Cases were confirmed by proper clinical examination and needle aspiration.
Distribution according to space involved
| S. no. | Space involved | No of patient (out of 45) | % Percentage |
|---|---|---|---|
| 1. | Parapharyngeal space | 13 | 28.89 |
| 2. | Posterior cervical space | 8 | 17.78 |
| 3. | Extended space | 8 | 17.78 |
| 4. | Submandibular space | 6 | 13.33 |
| 5. | Masticator space | 3 | 6.67 |
| 6. | Carotid space | 3 | 6.67 |
| 7. | Nape of neck | 3 | 6.67 |
Etiology
The causes of deep neck infections were identified in 36 of 45 patients (80%). Odontogenic infections were the most common cause 18 of 45 patients (40%), which accounted for submandibular space infections, and masticator space infections. Upper airway infection was the second most common cause 20% (9 of 45). They were usually related to parapharyngeal space infections, and extended space infections.
Etiology of DNSI
| S. no. | Source of infection | No of patients (out of 45) | % Percentage |
|---|---|---|---|
| 1. | Odontogenic | 18 | 40 |
| 2. | Upper airway infection | 9 | 20 |
| 3. | Skin infection | 8 | 17.78 |
| 4. | Unknown | 10 | 22.22 |
Underlying Systemic Diseases
30 patients (66.67%) had underlying systemic diseases apart from diabetes mellitus. 25 were men, and 5 were women. There were 15 patients with hypertension, 10 patients with nutritional anemia and 5 patients with diabetic nephropathy. The most commonly involved space in these patients was the parapharyngeal space 28.89% (13 of 45); second was the extended space 17.78% (8 of 45) followed by 6.67% (3 of 45) patient each of masticator space, posterior cervical space and nape of neck. It is notable that all the patients with parapharyngeal space and extended space abscess had associated systemic diseases. The patients with underlying systemic diseases tended to have a higher mean age and longer duration of hospital stay, complications occurred more frequently.
Comparision of patients with and without systemic diseases
| No. of patients | Mean age ± SD, years | Mean duration of stay ± SD, days | |
|---|---|---|---|
| Systemic diseases (+) | 10 | 56 ± 5.4 | 62.8 ± 3.2 |
| Systemic diseases (−) | 5 | 47 ± 7.8 | 41 ± 19.5 |
Bacteriology
Results of pus cultures from either incision and drainage or needle aspiration were available for all the patients. Blood culture was performed for those patients whose first presentation was only cellulitis and subsequently developed an abscess. All the patients had positive culture results. The most common organisms was Klebsiella 64.44% (29 of 45), followed by Streptococcus viridians 22.22% (10 of 45), Staphylococcus aureus 6.67% (3 of 45), MRSA (methicillin resistance staphylococcus aurues) 4.44% (2 of 45) and Burkholderia pseudomallei 2.22% (1 of 45).
Bacteriology of DNSI
| S. no. | Organism | No. of patients (out of 45) | % Percentage |
|---|---|---|---|
| 1, | Klebsiella | 29 | 64.44 |
| 2. | Streptococcus viridans | 10 | 22.22 |
| 3. | Staphylococcus aureus | 3 | 6.67 |
| 4. | MRSA | 2 | 4.44 |
| 5. | Burkholderia pseudomallei | 1 | 2.22 |
Treatment
All patients received empirical antimicrobial broad spectrum intravenous antibiotics, which were later updated based on culture and sensitivity report. Of the abscess group 97.78% (44 of 45) patients required an external approach for incision and drainage, 2.22% (1 of 45) patients with carbuncle nape of neck required only routine debridement and antiseptic dressing, Extended space infection group with skin necrosis 17.78% (8 of 45) received split skin grafting after appearance of granulation tissues. All the patients with odontogenic infection 40% (18 of 45) were adviced for caries teeth extraction. All patients were discharged in stable condition.
Different modalities of treatment
| S. no. | Treatment | No of patients (out of 45) | % Percentage |
|---|---|---|---|
| 1. | Incision and drainage | 44 | 97.78 |
| 2. | Debridement only | 1 | 2.22 |
| 3. | Caries teeth extraction | 18 | 40 |
| 4. | Split skin grafting | 8 | 17.78 |
Complications
Four patients (8.89%) had complications. 3 of 5 patients with diabetic nephropathy required dialysis due to severe electrolyte imbalance. Mediastinitis was noted in one patient with extended space infection.
Complications
| S. no. | Complications | No of patients (out of 45) | % Percentage |
|---|---|---|---|
| 1. | Diabetic nephropathy requiring dialysis | 3 | 6.67 |
| 2. | Mediatinitis | 1 | 2.22 |
Hospital Stay
The duration of hospital stay ranged from 7 to 68 days, with a mean stay of 55.53 ± 15.12 days. The patients with other systemc manifestions (62.8 ± 3.2 days), tended to have a longer hospital stay and belong to older age group.
Discussion
In the past deep neck space infections were fairly common and were a source of considerable morbidity and mortality. The advent of better laboratory testing, radiological investigations, availability of broad spectrum antibiotics and early surgical intervention has drastically reduced its incidence.
In our study, the majority of patients were seen in their sixth decade and hence it is evident from this study that old age patients are more susceptible to DNSI. This can be attributed to older age group associated with systemic illness, lower defence mechanism and lower recovery rate. However the age distribution is inconsistent with the studies by Parischar et al. and Meher et al. in which 50 and 60% patients were in the third and fourth decade of life, respectively [5, 12]. This can be due to better medical facilities with time. Another factor can be absence of intravenous drug abusers and blunt trauma cases in our study which usually occurs in younger age groups.
A male predominance was noted in our study which is comparable with studies by Sethi et al. Meher et al. and Parischar et al. all of which showed male preponderance [5, 12, 13]. Presumably this male preponderance can be attributed to high incidence of substance abuse among males.
In this part of the North eastern region of India, there is wide spread tobacco abuse as compared to the rest of the country. In our series we have found all of our patients were tobacco chewers. This results in poor oral hygiene and is reported to affect the host’s vulnerability to systemic diseases by the formation of subgingival biofilms acting as reservoirs of Gram-negative bacteria, and through the periodontium acting as a reservoir of inflammatory mediators [14].
Odontogenic infections are among the most common diseases in the oral and maxillofacial region, especially in developing countries [15]. In a study by Tschiassny et al. 70% of cases of DNSI were odontogenic in origin [16]. In a retrospective study by Parhiscar et al. and Sethi et al. odontogenic infections were declared as the most common cause of DNSI [5, 15]. Thus, our study results 40% odontogenic infection to be commonest source are consistent with these previous studies.
The most common presentation of DNSI in our study was Parapharyngeal space (26.67%) which is consistent with the studies by Khode et al. [17]. Odontogenic infections usually spread from the mandible or maxilla into the sublingual, submandibular or masticatory spaces which further can directly spread into the parapharyngeal space [18]. These factors explain why parapharyngeal space was most frequently involved in our study.
Further, in our study, only diabetic patients with DNSI were taken into account which agrees with the study of Huang et al. [8] showing high prevalence of deep neck space infection among diabetic population (30.3%). Higher incidence of DM as comorbidities in DNSI is evident in the study by LEE et al. According to his study the complications are more with Diabetes if more than two neck spaces were involved [3]. Huang et al. in his study confirmed that patient with DNIS associated with Diabetes had longer duration of hospital stay than without DM [8]. In patients with DM there is a defect in the host’s immune function such as cellular immunity complement activation and polymorphonuclear neutrophill function, which increase the risk of vascular complication and the episodes of infections [19]. Hence while dealing with DNSI special attention should be given to patients with DM.
Kleibsiella pneumoniea was the most common organism isolated, which agrees with the literature reviews of Wang [7], which show predominance of klebsiella in diabetic population. In our study streptococcus viridians was also one of the most commonly isolated organisms [5, 20], consistent with previous reports and can be explained by high rate of odotogenic infections.
The predisposition factors for complications such as mediastinal extension are older age, involvement of two or more spaces, presence of cardiovascular and pulmonary comorbidities [3], which is well evident from our study.
Worldwide, management of DNSI usually involves early surgical drainage of purulent abscesses via an external incision [7]. In our study, all patients were initiated on empirical intravenous broad spectrum antibiotic which was later modified according to the culture and sensitivity report. Followed by incision and drainage. As all our patients were diabetic, they received oral hypoglycemic agents or insulin to keep their blood sugar strictly <200 mg/dl. All the patients were discharged in good condition.
The management and diagnosis of DNSI is still a challenge for otorhinolaryngologists for several reasons: complex anatomy of neck, proximity to important neurovascular structure, deep seated nature, difficult to palpate and visualize externally and communication to other parts of body (mediastium and coccyx). Evaluation of variables relating to life-threatening diseases is very important as complications can even result in death.
Conclusion
We should pay more attention when dealing with deep neck space infections in patients with diabetes mellitus because these patients belong to older age group, have associated other systemic diseases and prone to have multiple neck spaces involvement. Frequent complications in these patients require longer duration of hospital stay. Appropriate management continues to favour a combination of early surgical drainage and systemic antibiotics covering Klebseilla pneumonia. In our study, odontogenic infections were the most common etiology for deep neck space infection in diabetic population. Therefore, primary prevention in diabetic patients must include awareness about dental and oral hygiene, avoidance of substance abuse like tobacco chewing and secondary prevention by encouraging regular check-ups for dental infections.
Abbreviations
- DNSI
Deep neck space infections
- DM
Diabetes mellitus
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Vieira F, Allen SM, Stocks RSM, Thompson JW. Deep neck infections. Otolaryngol Clin N Am. 2008;12:459–483. doi: 10.1016/j.otc.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 2.Poeschl PW, Spusta L, Russ Mueller G, Seemann R, Hirschl A, Poeschl E, et al. Antibiotic susceptibility and resistance of the odontogenic microbiological spectrum and its clinical impact on severe deep space head and neck infections. Oral Surge Oral Med, Oral Pathol, Oral Radiol Endod. 2010;110(2):151–156. doi: 10.1016/j.tripleo.2009.12.039. [DOI] [PubMed] [Google Scholar]
- 3.Kang SK, Lee S, Oh HK, Kang MW, Na MH, Yu JH, Koo BS, Lim SP. Clinical features of deep neck infections and predisposition factorsfor mediastinal extension. Korean J Thorac Cardiovasc Surg. 2012;45(3):171–176. doi: 10.5090/kjtcs.2012.45.3.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weed H, Forest L. Deep neck infection. J Otolaryngol Head Neck Surg. 1998;3:2515–2524. [Google Scholar]
- 5.Parhiscar A, Harel G. Deep neck abscess: a retrospective review of 210 cases. Ann Otolo Rhinol Laryngol. 2011;110(11):1051–1054. doi: 10.1177/000348940111001111. [DOI] [PubMed] [Google Scholar]
- 6.Murray AD Deep neck space infections. http://emedicine.medscape.com/article/837048-overview [PubMed]
- 7.Wang LF, Kuo WR, Tsai SM, Huang KJ. Characterizations of life threatening deep cervical space infections: a review of one hundred ninety six cases. Am J Otolaryngol. 2003;24(2):111–117. doi: 10.1053/ajot.2003.31. [DOI] [PubMed] [Google Scholar]
- 8.Huang TT, Liu TC, Chen PR, et al. Deep neck infection: analysis of 185 cases. Head Neck. 2004;26:854–860. doi: 10.1002/hed.20014. [DOI] [PubMed] [Google Scholar]
- 9.Logan turner’s diseases of the nose, throat and ear and head and neck surgery; neck space infections. 11th edn., p 277
- 10.Cummings otolaryngology, deep neck space infections and head and neck surgery, 5th edn
- 11.Lee JK, Kim HD, Lim SC. Predisposing factors of complicated deep neck infection: an analysis of 158 cases. Yonsei Med J. 2007;48(1):55–62. doi: 10.3349/ymj.2007.48.1.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meher R, Jain A, Sabharwal A, Gupta B, Singh I, Agarwal I. Deep neck abscess: a prospective study of 54 cases. J Laryngol Otol. 2005;119(04):299–302. doi: 10.1258/0022215054020395. [DOI] [PubMed] [Google Scholar]
- 13.Sethi DS, Stanley RE. Deep neck abscesses-changing trends. J Laryngol Otol. 1994;108:138–143. doi: 10.1017/S0022215100126106. [DOI] [PubMed] [Google Scholar]
- 14.Anil S, Al-Ghamdi HS. The impact of periodontal infections on systemic diseases. AN update for medical practitioners. Saudi Med J. 2006;27(6):767–776. [PubMed] [Google Scholar]
- 15.Wong TY. A nationwide survey of deaths from oral and maxillofacial infections: the Taiwanese experience. J Oral Maxillofac Surg. 1999;57:1297–1299. doi: 10.1016/S0278-2391(99)90863-7. [DOI] [PubMed] [Google Scholar]
- 16.Tschiassny K. Ludwig’s angina: an anatomic study of the role of the lower molar teeth in its pathogenesis. Arch Otolaryngol. 1943;38(5):485–496. doi: 10.1001/archotol.1943.00670040504010. [DOI] [Google Scholar]
- 17.Khode SR, Bhat P, Rane S, Dasguota KS. Retrospective analysis of 298 cases of deep neck infections: its diagnosis and management. Sci J Med Clin Trials. 2013;103:1–3. [Google Scholar]
- 18.Yonetsu K, Izumi M, Nakamura T. Deep facial infections of odontogenic origin: CT assessment of pathways of space involvement. AJNR Am J Neuroradiol. 1998;19:123–128. [PMC free article] [PubMed] [Google Scholar]
- 19.Delamaire M, Maugendre D, Moreno M, et al. Impaired leukocyte functions in diabetic patients. Diabetic Med. 1997;14:29–34. doi: 10.1002/(SICI)1096-9136(199701)14:1<29::AID-DIA300>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 20.Har-El G, Aroesty JH, Shaha A, Lucente FE. Changing trends in deep neck abscess. A retrospective study of 110 patients. Oral Surg OralMed Oral Pathol. 1994;77:446–450. doi: 10.1016/0030-4220(94)90221-6. [DOI] [PubMed] [Google Scholar]