Abstract
We evaluated electrocardiografie and echocardiografic changes of 40 patients with pulmonary tromboemboloism proved by perfusion scintigrams. ECG-changes included sinus tachycardia or apsolute tachyarrhythmia de nuovo, changes type Q1S3T3 and changes in right precordial leads. Analyses of echocardiography included hyperkinesis and then dilatation and apical hypokinesis of right ventricule and tricuspid regurgitation with maximal transvalvular gradients. We emphasize such a sensibility of echocardiographic changes in early estimation of pulmonary tromboembolism severity and necessity for echocardiography as early as possible in suspected patients
Keywords: pulmonary thromboembolism, deep vein thrombosis, echocardiogram, electrocardiogram
INTRODUCTION
Overall mortality in patients with acute pulmonary embolism remains high despite modern diagnostic and reperfusion strategies. In the largest international registry of 2454 patients, 3-month mortality was 17 % whereby 45 % of deaths were attributed to pulmonary embolism (1). Right ventricular dysfunction is present in about 30 % of patients with acute pulmonary embolism and normal blood pressure (2). Therefore, transthoracic echo-cardiography has emerged as important diagnostic tool for assessing the degree of right ventricular dilatation and the severity of right ventricular systolic dysfunction. In the international registry, echocardiographic right ventricular dysfunction was identified as the single most important prognostic factor for in-hospital death, and 75% deaths in patients with pulmonary embolism and right ventricular dysfunction occurred in the first days after diagnosis. In these patients overall mortality at 3 months was twice as high as in pastients with preserved right ventricular function in the baseline echocardio-gram. Nevertheless, none of the available reperfusion strategies has ever shown a mortality benefit for patients with acute pulmonary embolism. A mortality benefit for thrombolysis has not been shown(3). Thrombolysis is indicated in patients with pulmonary embolism-related shock. Therefore, there is a need for a simple management strategy for patients with acute pulmonary embolism, which provides a rapid and reliable diagnosis and which identifies high risk patients who need treatment without delay. This strategy is based on the initial haemodynamic presentation of the patients and allowed definition of the correct diagnostic and therapeutic algorithm to be defined. The proposed management strategy takes recent data on Doppler echocardiography and spiral CT, but ECG-changes are available and suitable for work-diagnosis. Our goals were to analyze retrospectively ECG-changes in patients with lung scin-tigram-proved pulmonary embolism and echocardiog-raphy-changes in these patients. Patients were divided into two-groups: patients with massive and patients with non-massive pulmonary embolism. Massive embolism involves more than half of pulmonary fields in lung scintigram and is presented with shock-index > 1.
MATERIALS AND METHODS
Clinical Internal department of General Hospital in Sarajevo had treated patients with acute pulmonary embolism. This study is retrospective and involved all patients with diagnosis of acute, first pulmonary embolism treated in a few last years. Final diagnosis was proved on lung scintigrams or rarely on spiral computer tomography. A total number of 40 consecutive patients with this diagnosis were admitted to the Intensive care of Internal departement and they were stratified according to the clinical probability pretest and shock index into two groups: massive (17 patients) and non-massive (23 patients) pulmonary embolism. ECG and transthoracic echocardiography was performed for each patients in order to asses changes typical for acute pulmonary obstruction. Typical ECG changes included sinus-tachycardia over 120/min, changes type S1Q3T3, new complete right bundle branch block and repolarisation changes in right precordial leads. Trans-thoracic echocardiography may identify right ventricular dysfunction and substantial pulmonary hypertension, In patient group with non-massive pulmonary embolism we registrated dilatation of right ventricul over 28 mm with apical hypokinesia and transtricuspidal max PG and consecutive pulmonary hypertension. Patients with massive pulmonary embolism were examined related to the right ventricular dilatation and max tricuspidal PG and consecutive pulmonary hypertension. We analysed predictory value and specificity of ECG-changes including sinus tachycardia, changed S1Q3T3, new complete right bundle branch block and repolarisation changes in right precordial leads in patients with lung-scintigram-proved diagnosis of pulmonary embolism. According to literature, similar nonspecific electrocardiographic findings were seen in about 70 % patients;classic but nonspecific S1Q3T3 patterns were seen in only 10 %. Left axis deviation was more common that right axis deviation (4). Transthoracic echocardiography in first group revealed hyperkinetic right ventricul or nonspecific changes and dilatation of right ventricule with low gradient on transtricuspidal flow. In group with massive embolism we examined dilatation of right ventricul and we measured transtricuspidal max pressure gradient. Our results are presented in folowing tables (Table 1 and 2) and figures (Figure 1, 2 and 3).
TABLE 1.
Electrocardiographic changes
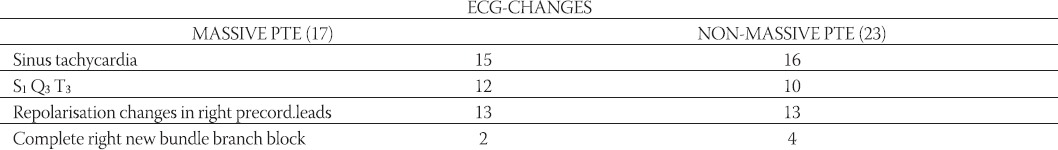
TABLE 2.
Echocardiographic changes
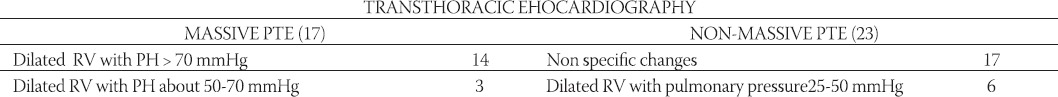
FIGURE 1.
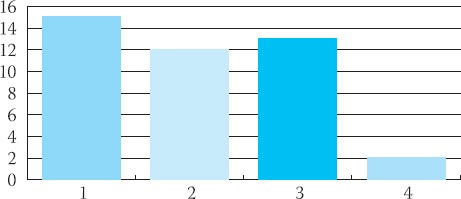
Massive PTE and ECG-changes
l-patients presenting sinus-tachycardia
2-S1Q3T3 changes on ECG
3-repolarisation changes in right praecoidial leads
4-new right bundle branch block
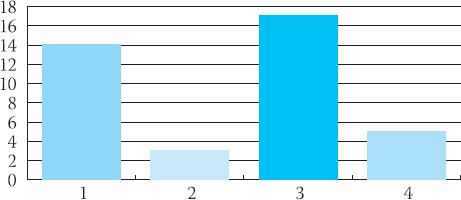
FIGURE 2.
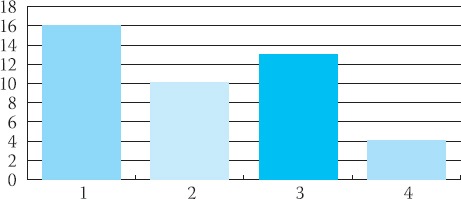
Non massive PTE and ECG-changes
l-patients presenting sinus-tachycaidia
2-S1Q3T3 changes on ECG
3-repolarisation changes in right praecoidial leads
4-new right bundle branch block
FIGURE 3.
Echocardiography changes in pulmonary embolism
1-Dilated RV with PH > 70 mmHg
2-Düated RV with PH about 50-70 mmHg
3-Non specific changes
4-Dilated RV with pulmonary pressure25-50 mmHg
RESULTS AND DISCUSSION
We analyzed 40 patients with diagnosis of first acute pulmonary embolism proved by lung scintigram and occasionally by spiral computered tomography(CT). Patients are divided into group with massive- and non-massive pulmonary embolism with goal to easy elaborate these results. In ECG-analyses, patients with massive embolism have presented with sinus-tachycardia in 15/17=88 %; S1Q3T3 changes were presented in 12/17=70 %; repolarisation changes in right precordial leads in 13/17=76 % and new right bundle branch block in 2/17=11,7 % cases. Patients with non massive embolism have presented with sinus-tachycardia in 16/23=69,5 %; S1Q3T3 changes were presented in 10/23=43 %; repolarisation changes in right precordial leads in 13/23=56,5% and new right bundle branch block in 2/23=8,6 % cases. Transthoracic echocardiogra-phy showed another changes: in massive pulmonary embolism we have seen dilated right ventricul and PH> 70 mmHg in 14/17=82%. Ten patients from this group died in first three days(58,5 %). Dilated right ventricular with PG 50-70 mmHg was found in 3/17=17,6 % and one patient from this group died in first three days(11/17=64,7 %-overall mortality of this group). In patients presented non-massive pulmonary embolism 17/23 =73,8 % non specific changes on echocardiography were revealed and 6/23=26 % patients presented low dilated right ventricul and max PG on transtricuspid flow 25-50 mmHg.
CONCLUSION
In our study we showed moderate predictive value of ECG-changes in acute non-massive pulmonary embolism (sinus-tachycardia in 69,5 %, SlQ3T3 changes in 43 %, repolarisation changes in right precordial leads in 56,5 % and new RBBB in 8,6 % of these patients). In patient gruop with massive PT this predictive value is higher (sinus-tachycardia in 88 %, SlQ3T3 changes in 70 %, repolarisation changes in right precordial leads in 76% and new RBBB in 11,7% of these patients). Transthoracic echocardiography is advocated by some as a useful diagnostic test for patients with pulmonary embolism. It’s sensitivity in massive PE is very high in our study with comment that patients with pulmonary pressure over 70 mmHg have high 3-days mortality (58,5 %). To sumarize, echocardiography proved to be a simple and realistic test. Our conclusion is that echocardiography is important and prognostically valuable test for every patient with suspected pulmonary embolism and should be done (in hospital environment) as soon as possible.
REFERENCES
- 1.Goldhaber SZ, Visani L, De Rosa M. Acute pulmonary embolism: clinical aotcomes in the international Cooperative Pulmonary Embolism Registry(ICOPER) Lancet. 1999;353:1386–1389. doi: 10.1016/s0140-6736(98)07534-5. [DOI] [PubMed] [Google Scholar]
- 2.Grifoni S, Olivotto I, Cecchini P, et al. Short-term clinical outcome of patients with acute pulmonary embolism, normal blood pressure and echocardioghraphic right ventricular dysfunction. Circulation. 2000;101:2817–2822. doi: 10.1161/01.cir.101.24.2817. [DOI] [PubMed] [Google Scholar]
- 3.Jerjes-Sanchez C, Ramirez-Rivera A, de Lourdes Gascia M, et al. Streptokinaze and heparin versus heparin alone in massive pulmonary embolism;a randomised controlled trial. J Thromb Thrombolysis. 1995;2:227–229. doi: 10.1007/BF01062714. [DOI] [PubMed] [Google Scholar]
- 4.Eagle K, Baliga R, et al. Practical Cardiology. Vol. 34. Lipincott Williams and Wilkins; 2003. pp. 510–521. [Google Scholar]


