Abstract
Cervical dysplasia, a premalignant lesion that can progress to cervical cancer, is caused primarily by a sexually transmitted infection with an oncogenic strain of the human papillomavirus (HPV). The HPV infections are treated through destroying the clinical lesions: laser, cryotherapy, podophylline… The hope is that by causing local tissue inflammation that the body will be stimulated to mount an antibody response and thereby prevent recurrence. In contrast to other prevention approaches, vaccines can reduce susceptibility in uninfected partners by stimulating the immune system. Aloa vera has also been reported to retard tumour growth and stimulate the immune response to viruses. A list of possible actions of propolis includes: antibacterial, antifungal, antiviral, antioxidant, anticarcinogenic, antithrombotic and immunomodulatory. Research on the possible role of some B vitamins in preventing cancer began in the last few decades, but however this complex have an influence on immune status. The aim of our study is to try to treat the HPV infection as confirmed cause of neoplastic transformation with some herbal therapy and interferon and to try define the guidelines in the management of the HPV positive patients. Goal of this paper is to search for evidence of efficacy of any treatment for HPV infection of the cervix mostly in woman with no concomitant CIN. Fifty five woman affected by HPV genital infection were enrolled in the study from September 2005 to April 2006. Patients were classified according to the results of the HPV testing prior and after the therapy. Patients were randomized into two groups: the first group was HPV positive woman treated with other than recommanded therapy (n=20), (control group); the second group was pharmacologically treated with intravaginal administration of an interferon and aloa vera – propolis in recommended scheme (n=35) with treatment of the possible fungal or bacterial genital infection prior to the specific therapy. The almost same therapy was recommended to the male partner. Patients from the second group used B complex during the therapy. Patients were retested for the HPV presence after three or six month from therapy depend of the presence bacterial or fungal genital coinfection. Three months after applied therapy HPV infection was still present in more than 90% of the patients in the first group. In the second group treated according to the recommended therapy scheme HPV infection disappeared in 71,42% of the patients after three months and in 100% of patients after six months. Samples of the cervical smear for the HPV analysis were being taken during routine gineacological examinations, by using sticks with cotton, taken from the Digene Specimen Collection Kit, from the whole surface of a portion, and by mild rotating moves from the outer cervical entrance. Our results suggest that the combination of interferon and herbal therapy with B complex is effective, atraumatic and simple non-surgical treatment of HPV infection. Since prospective efficacy trials will take several years to complete, considering alternative approaches is also worthwhile.
Keywords: human papilloma virus, cervical lesion, herbal therapy
INTRODUCTION
Cervical dysplasia, a premalignant lesion that can progress to cervical cancer, is caused primarily by a sexually transmitted infection with an oncogenic strain of the human papillomavirus (HPV) (1, 2, 3). Women less than 30 years old display a high rate of HPV positivity with normal cytologic findings. HPV is most usually detected in women, but it has been shown that up to 85% of the male partners of women diagnosed with HPV test positive for the virus. The HPV infections are treated through destroying the clinical lesions: laser, cryothera-py, podophylline…(4, 5). The hope is that by causing local tissue inflammation that the body will be stimulated to mount an antibody response and thereby prevent recurrence. In contrast to other prevention approaches, vaccines can reduce susceptibility in uninfected partners by stimulating the immune system. The vaccine protects against some of the cancer-causing strains of HPV, but not all. In 1500 B.C. Egyptians recorded use of the herbal plant in treating burns, infections and parasites. Aloe, native to Africa, is also known as “lily of the desert”, the “plant of immortality”, and the “medicine plant”. The name was derived from the Arabic alloeh meaning “bitter” because of the bitter liquid found in the leaves. Aloe vera has also been reported to retard tumor growth and stimulate the immune response to viruses (6). Propolis, also known as bee glue and bee propolis, is a brownish resinous substance collected by bees. It is said that propolis is the most natural antibiotic that man has ever discovered. The remarkable thing about this statement is the fact that this discovery took place some 2000 years ago. A list of possible actions of propolis includes: antibacterial, antifungal, antiviral (including anti HIV-1 activity), antioxidant, anticarcinogenic, antithrombotic and immunomodulatory. Research on the possible role of some B vitamins in preventing cancer began in the last few decades, but however this complex has an influence on immune status. B vitamins are essential nutrients for growth, development, and a variety of other bodily functions. They play a major role in the activities of enzymes (proteins) that regulate chemical reactions in the body. This is especially important in turning food into energy and other needed substances. B vitamins are found in a variety of plant and animal food sources. Because of the public health importance of cervical cancer and its precursor lesion, this report focuses on the possible treatment of genital HPV infection and its sequelae in both sexual partners with mostly natural, herbal therapy. The aim of our study is to try to treat the HPV infection as confirmed cause of neoplastic transformation with some herbal therapy and interferon and to try defining the guidelines in the management of the HPV positive patients. Goal of this paper is to search for evidence of efficacy of any treatment for HPV infection of the cervix mostly in woman with no concomitant CIN.
MATERIALS AND METHODS
STUDY DESIGN
Fifty-five women affected by HPV genital infection were enrolled in the study from September 2005 to April 2006. Patients were classified according to the results of the HPV testing prior and after the therapy. Patients were randomized into two groups: the first group was HPV positive women treated with other than recommended therapy (n=20), (control group); the second group was pharmacologically treated with intravaginal administration of an interferon and aloe vera – propolis in recommended scheme (n=35) with treatment of the possible fungal or bacterial genital infection prior to the specific therapy. The almost same therapy was recommended to the male partner. Patients from the second group used B complex during the therapy. Patients were retested for the HPV presence after three or six month from therapy depends of the presence bacterial or fungal genital co-infection. The study was conducted under University Clinical Center Tuzla and proved by Ethical committee.
DETECTION OF HPV DNA AND PAP RESULTS
Samples of the cervical smear for the HPV analysis were being taken during routine gynecological examinations, by using sticks with cotton, taken from the Digene Specimen Collection Kit, from the whole surface of a portion, and by mild rotating moves from the outer cervical entrance. Detection of the presence of HPV in the cervical smear was done by the Digene HPV Test-Hybrid Capture II. The cytomorphological changes found by using light-microscope method were classified according to the Bethesda classification of cervical lesion.
STATISTICAL ANALYSIS
Categorical variables were analyzed by χ2 test and Fisher’s exact test to prove the better therapeutic effects of recommended therapy compared with other therapeutic modality. Value of less than 0.0001 was considered to indicate statistical significance. Odds ratios (OR), as maximum likelihood estimates of success of the treatment were computed with 95% confidence intervals (CI).
RESULTS
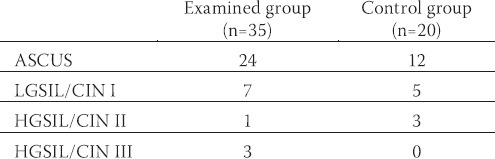
Overall, 55 HPV positive women with different cytology results were enrolled in the study: 35 women in the examined group (II group), and 20 women in the control group (I group). Cytology evaluation of the smears was presented in the Table 1.
TABLE 1.
Cytomorphological changes verified in HPV positive woman
Recommended therapy:
Treat the possible infection of vaginal flora (bacterial, fungal, mixed)
Interferon vagitorie or cream (7x1vag in the evening, two months for women; 1 tube to spread for man).
Aloe vera/propolis vag (7x1 vag in the evening, three months for women, 1 tube of gel to spread for man).
B-complex vitamin
Scheme:
First treat the possible infection of vaginal flora than start with specific therapy; 7x1 vag in the evening followed by 7x1 vag aloe vera/propolis, repeat during next two months).
ACTIVE INGREDIENTS OF ALOE VERA/PROPOLIS VAGITORIE AND BASIC MECHANISM OF ACTION
Vagitories: Propolis, Aloe vera, Echinacea (sx3gr)
Extract of propolis (5%), filtered juice of aloe (Aloe barbadensis) with certified organic quality, Extract of over ground part of Echinacea (Echinacea purpurea); extract of marigold flower, (Calendula officinalis). The additional ingredients: white wax (Cera alba); Witespol H15- hydrogenised herbal glicerids (Adeps solidus), propylene glycol, alfa tokoferol. The pharmacy contains the extract of propolis (5%) with more than 180 identified ingredients, mostly biologically active. Propolis as natural antibiotic, works actively against different bacteria, fungi, and viruses and with enhanced action in combination with antracinons from aloe, and ingredients from Echinacea and marigold. Anti-inflammatory action is result of effectivity of few different active ingredients with point on CAPE (cafeic acid of phenitil ester) from propolis, which also has an antitumor effect.
BIOLOGIC CHARACTERISTICS OF THE HERBS AND VITAMIN B
Aloe vera: Aloe is derived from the A. vera plant, a green, succulent, cactus-like plant belonging to the lily family. The substance, A. vera, is derived from thin-walled mucilaginous cells of the inner central zone of the leaf. This gel is thought to have emollient and moisturizing effects and therapeutic properties. A. vera is a complex plant that contains many biologically active substances. Davis, Parker, Samson et al., (1991) (6) reported that one tablespoon of A. vera contains over 75 different chemicals that have biological activity. Therefore it has proved difficult to isolate a single active ingredient, and it has been suggested that there is a synergistic relationship between the constituents. Mannose-6-phosphate is a major structural constituent of A. vera. Research conducted by Davis, Di Donato, Hartman et al, suggested that mannose-6-phosphate is an active ingredient in A. vera which demonstrates wound healing and anti-inflammatory activity in a dose response fashion. Current theory suggests that mannose-6-phosphate needs to be protein linked to yield its therapeutic activity. The authors speculate that the binding of fibroblast receptors with mannose-6-phosphate is capable of activating fibroblast proliferation.
Propolis: The use of Propolis in popular medicine goes back all the way to ancient times. Egyptians, Greeks and Romans reported the use of Propolis for its general healing qualities and for the cure of some lesions of the skin. Propolis has a long history of use in folk medicine and was even used as an official drug in London in the 1600s. The composition of propolis is variable, depending on the locale and variety of trees and other plant species used for the collection. For example, unique constituents have been identified in propolis collected in Cuba and Brazil. The main chemical classes found in propolis are flavonoids, phenolics and terpenes. The flavonoids include quercetin, apegenin, galangin, kaempferol, lu-teolin, pinocembrin, pinostrobin and pinobanksin. The phenolic ester (caffeic acid phenethyl ester or CAPE) present in propolis is receiving much attention in the medical research community because of its potential for the treatment in the number of disorders, including spinal cord injury. Most of the substances in propolis are poorly soluble in water. Caffeic acid phenethyl ester (CAPE) inhibits the lipoxygenase pathway of arachidonic acid, resulting in anti-inflammatory activity. CAPE is also known to have anticarcinogenic, antimitogenic and immunomodulatory properties. CAPE has been found to completely inhibit the activation of the nuclear transcription factor NF-Kappa B by tumor necrosis factor (TNF), as well as by other pro-inflammatory agents. The inhibition of NF-Kappa B activation may provide the molecular basis for its immunomodulatory, anticarci-nogenic, anti-inflammatory and antiviral activities. It is possible that CAPE exerts its effects by inhibiting reactive oxygen species (ROS) production. ROS are known to play a major role in the activation of NF-Kappa B (7).
B complex vitamins: All vitamin B-Complex group are water soluble, and are linked together in several chemical ways. They are formed from bacteria, yeast’s, fungi, or moulds. They are responsible for providing energy to the body during the conversion of glucose, from carbohydrates. They are also critically required for the metabolism of both, fats and proteins, as well as the health and maintenance of the body’s nervous system (8).
Interferon: Belong to the group of the regulatory glico-proteins of low molecular mass. Besides the antiviral and antiproliferative effects, they have also effect in the treatment of malignant disease, and act protectively against the radiation. Interferon beta posses’ only one protein molecule the product of fibroblast as well as the epithelial cells resistant to the low pH as well as alfa is antiviral and antiproliferative effect. Application of exogenous IFN has the significant effect in initiative phase’s virus infection by stoppage of viral replication.
EFFECTS OF THE THERAPY
Three months after applied therapy HPV infection was still present in more than 90% of the patients in the first group. In the second group treated according to the recommended therapy scheme HPV infection disappeared in 71,42% of the patients after three months and in 100% of patients after six months (Figure 1). After adjustment for the therapy, there was a significant trend of increasing success to cure the HRHPV infection with recommended therapy scheme (χ2 =16,84; P< 0,0001). Compared with other applied therapy for HRHPV infection, the success of the recommended therapy scheme was significantly higher OR= 22,5 (95% CI: 3,95-219,85). In the first group (control group, n=20) vaginal flora analyses showed persistent mixed bacterial/fungal infection in 80% of women during the therapy, while in the second (examined group, n=35) group treatment of the possible infection and inflammation was a precondition to start the specific recommended HRHPV therapy. 28,57%(10) of the women from the second group was still HPV positive after three months of applied therapy. 4 women out of 10 had persistent mixed vaginal infection, while in 6 patients; the male partner was not adequately treated. In this group of patients the whole recommended therapy procedure was repeated, with point on the treatment of vaginal infection and male partner. Therapeutic options used in the patients of the first (control) group with HRHPV infection included laser, cryotherapy, podo-phylline but without treatment of the male partner and without prior treatment of possible vaginal infection.
FIGURE 1.
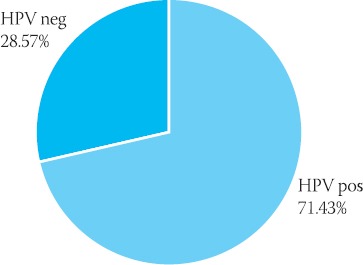
The ratio between HRHPV negative and HRHPV positive women in the examined group after three months of therapy
DISCUSSION
Genital infection with human papillomavirus (HPV) is very common in sexually active man and woman and can sometimes have serious health consequences. The virus can infect the genital skin and the linings of the vagina, cervix, rectum, and urethra. Although the majority of infections cause no symptoms, they are self-limited, and go away on their own without clinical consequences, genital HPV is of public health concern because persistent infection with certain high-risk types can cause cervical cancer in women (2). The results conducted in Bosnia and Herzegovina by E. Iljazović and co-workers, as well as the results of numerous studies conducted world-wide point to the central role of the HPV in the pathogenesis of cervical lesions with an etiologically important co-action with other mutually independent factors, primarily factors related to sexual habits/behavior (9). All those facts underline the necessity for active treatment of HPV infection. The HPV specific vaccine has been designed solely for the prevention of cancer. Cervical Cancer is the second most frequent cancer in women worldwide, 80% of the cases occur in developing countries where screening programs for early detection do not exist. Prevention of cervical cancer can be achieved by prophylactic vaccination preventing disease or therapeutic vaccination (immune therapy) curing disease. Over the two and a half years of follow-up after vaccination, quadrivalent human papillomavirus (HPV) (types 6, 11, 16, and 18) recombinant vaccine, reduced the combined incidence of persistent infection from HPV 6, 11, 16, or 18 and related genital disease including new cervical pre-cancers and genital warts by 90 percent compared with placebo among women who were naïve to the relevant HPV types at baseline (p<0,001) (10). The results of our study showed that low risk cervical lesion are very often associated with HRHPV (56,6% in the examined group and 30,9% in the control group). According to the data of the National Cancer Institute HRHPV is present in 83% of patients with ASCUS/LGSIL, and in 26,92% of women with ASCUS/LGSIL in Bosnia and Herzegovina (11). The combination of smears with detection of high-risk HPV types increases the triage sensitivity especially at patients with mild changes, and therapeutic procedure is more simple (12). The incorporation of HPV testing into primary screening will result in informing millions of women with normal cytology that they are at increased risk of cervical cancer. Medical treatment of cervical lesion is usually painful, invasive, and generally traumatic. The most common methods are cauterization (burning off) and cryosurgery (freezing off). There are also topical medications (podophyllin, bichloroacetic acid, and trichloroacetic acid), which are applied weekly until the lesion goes away (13, 14). In any case it has been shown that treatment or not the recurrence level is the same. There are no enough references in the literature about possible different approach to the treatment of HRHPV and cervical lesion (15). Unfortunately, effective therapy is currently not available. Therapeutic options are limited, expensive and often ineffective (16). Immunotherapy seems to be one of the more promising options. Persistent mixed bacterial/fungal infection was verified in 80% of women in the first, control group during the therapy and in only 11,42% of women in the second, examined group. Three months after applied therapy HPV infection was still present in more than 95% of the patients in the first group. In the second group treated according to the recommended therapy scheme HPV infection disappeared in 71,42% of the patients. We concluded that coexistence of other different infection compromise the local and systemic immune status of the patients. Treatment of the possible mixed vaginal infection should be the first step in the therapeutic approach to HRHPV infection. Since treatment options are limited and typically not very satisfactory, the development of safe and effective antiviral drugs for HPV could have substantial clinical impact. Interferon combined with propolis, aloe vera and B Complex vitamins with their basic antibacterial, an-tifungal, antiviral, antioxidant, anticarcinogenic, anti-thrombotic and immunomodulatory action can cure HPV infection and prevent recurrence of disease. A substantial medical need exists for the development of antiviral medicines for the treatment of diseases associated with infection by human papillomaviruses (HPVs) (17). Our results suggest that HRHPV infection associated with different cervical lesion could be cured with: a) treatment of the possible fungal or bacterial genital infection, b) treatment of the both sexual partners should be the rule, c) local application of aloe vera and propolis could improve local immune status and help to HPV go away, d) B complex vitamins may have an influence on systemic immune status.
CONCLUSION
Papillomaviruses have proved to be the most complex group of human pathogenic viruses. Specific types, most notably human papillomavirus (HPV) types 16, 18, and a few others, have been shown to cause the majority of cervical cancers and their high-grade precursor lesions (18). Our results suggest that the combination of interferon and herbal therapy with B complex is effective, atraumatic and simple non-surgical treatment of HPV infection. Clinical trials are being conducted to test the preventive and therapeutic efficacy of HPV vaccines and in the meantime a different therapeutic option should be considered in order to prevent development of possible high-grade cervical lesion.
REFERENCES
- 1.Marshall K. Cervical dysplasia: early intervention. Altern Med Rev. 2003;8(2):156–170. [PubMed] [Google Scholar]
- 2.Duarte-Franco E, Franco EL. Cancer of the uterine cervix. BMC Women’s Health. 2004;4(Suppl 1):S13. doi: 10.1186/1472-6874-4-S1-S13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bosch FX, Munoz N, de Sanjose Human papillomavirus and other risk factors for cervical cancer. Biomed. Pharmacother. 1997;51(6-7):268–275. doi: 10.1016/s0753-3322(97)83542-1. [DOI] [PubMed] [Google Scholar]
- 4.Wierrani F, Kubin A, Jindra R, et al. 5-Aminolevulinic acid-mediated photodynamic therapy of intraepithelial neoplasia and human papillomavirus of the uterine cervix – A new experimental approach. Cancer Detection & Prevention. 1999;23(4):351–355. doi: 10.1046/j.1525-1500.1999.99036.x. [DOI] [PubMed] [Google Scholar]
- 5.Parent D, Binet H. Viral sexually transmitted diseases and their treatments. Rev. Med. Brux. 1998;19(4):A 185–190. [PubMed] [Google Scholar]
- 6.Davis RH, Parker WL, Samson RT, Murdoch DP. Isolation of a stimulatory system in an aloe extract. J. Am. Ped. Med. Assoc. 1991;81(9):473–478. doi: 10.7547/87507315-81-9-473. [DOI] [PubMed] [Google Scholar]
- 7.Natarajan K, Singh S, Burke TR, Jr, et al. Caffeic acid phenethyl ester is a potent and specific inhibitor of activation of nuclear transcription factor NF-Kappa B. Proc. Natl. Acad. Sci. 1996;93:9090–9095. doi: 10.1073/pnas.93.17.9090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Laurence DR, Bennett PN. Vitamin, Calcium, Pharmacotherapy of the bone. In: Vrhovec B, editor. Clinical Pharmacology, for Yugoslavian edition. Zagreb: Jumena; 1984. pp. 694–696. [Google Scholar]
- 9.Iljazović E, Poljak M, Čičkušić E, et al. Identifikacija i tipizacija humanog virusa papiloma i udruženost sa lezijama grlića materice. Acta Medica Saliniana. 2003;32(2):153–157. [Google Scholar]
- 10.Villa L Study Group. Gardasil™HPV vaccine reduced infection and disease in new clinical study. [date of access: 10.09.2006];Medical New Today 2005. Cancer/Oncology New – Google Search. [Google Scholar]
- 11.Iljazović E, Čičkušić E, Mustedanagić-Mujanović J, et al. Presence of high-risk human papilomaviruses (HPV) in the low-grade cervical lesion. Med. Arh. 2006;60(1):30–32. [PubMed] [Google Scholar]
- 12.Baldauf JJ, Cuenin C, Ritter J. Long term progress of low-grade intraepithelial lesions after a smear and colposcopy, directed biopsies and/or normal endocervical curettage. Contracept. Fertil. Sex. 1999;27(11):774–779. [PubMed] [Google Scholar]
- 13.Okamoto A, Woodworth CD, Yen K, et al. Combination therapy with podophyllin and vidarabine for human papilloma-virus positive cervical intraepithelial neoplasia. Oncol. Rep. 1999;6(2):269–276. doi: 10.3892/or.6.2.269. [DOI] [PubMed] [Google Scholar]
- 14.Mancino P, Cocola M, Roma B, Di Roberto R. Management of female genital HPV infections by the LEEP method. Minerva Ginecol. 1998;50(7-8):333–336. [PubMed] [Google Scholar]
- 15.Fox PA, Tung YM. Human papillomavirus: burden of illness and treatment cost consideration. Curr. Opin. Infect. Dis. 2006;19:62–66. [Google Scholar]
- 16.Gross G. Therapy of human papillomavirus infection and associated epithelial tumors. Intervirology. 1997;40(5-6):368–377. doi: 10.1159/000150569. [DOI] [PubMed] [Google Scholar]
- 17.Phelps WC, Barnes JA, Lobe DC. Molecular targets for human papillomaviruses: prospects for antiviral therapy. Antivir. Chem. Chemother. 1998;9(5):359–377. doi: 10.1177/095632029800900501. [DOI] [PubMed] [Google Scholar]
- 18.zur Hausen H. Papillomaviruses in human cancers. Proc. Assoc. Am. Physicians. 1999;111(6):581–587. doi: 10.1046/j.1525-1381.1999.99723.x. [DOI] [PubMed] [Google Scholar]


