Abstract
Background
Self-massage is a ubiquitous intervention similar to massage, but performed by the recipient him- or herself rather than by a therapist, most often using a tool (e.g., foam roller, roller massager). Self-massage has been found to have a wide range of effects. It is particularly known for increasing flexibility acutely, although not always. The variability of the results in previous studies may potentially be a function of the tool used. Recent findings also suggest that self-massage exerts global effects. Therefore, increased flexibility should be expected in the areas adjacent to the ones treated.
Purpose
To investigate the acute effects of foam rolling and rolling massage of anterior thigh on hip range-of-motion (ROM) – i.e., hip extension and hip flexion – in trained men.
Methods
Eighteen recreationally active, resistance trained males visited the lab on two occasions over a 4-day period separated by at least a day. Each session included two baseline ROM measures of passive hip flexion and extension taken in a randomized fashion. Recording of baseline measures was followed by the intervention of the day, which was either foam rolling or rolling massage of the anterior thigh as per randomization. Immediately post intervention, passive hip flexion and hip extension ROM were reassessed. In order to assess the time course of improvements in ROM, hip flexion and hip extension ROM were reevaluated at 10, 20, and 30 minutes post-intervention.
Results
Hip flexion and hip extension ROM increased immediately following both interventions (foam rolling or roller massager) and remained increased for 30 minutes post intervention. Foam rolling was statistically superior in improving hip flexion and hip extension ROM immediately post intervention. However, immediately post-intervention was the only time point that measurements exceeded the minimum detectable change for both interventions.
Conclusion
Both foam rolling and rolling massage appear to be effective interventions for improving hip flexion and extension ROM when applied to the anterior thigh, but the observed effects are transient in nature.
Level of evidence
2b
Keywords: Flexibility, foam rolling, rolling massage, self-manual therapy, self-myofascial release
INTRODUCTION
Self-massage is a ubiquitous intervention similar to massage, but performed by the individual rather than by a therapist, most often using a tool. Self-massage has been found to have wide range of effects.1 It is particularly known for increasing flexibility acutely,2-5 although not always.6,7 Importantly, self-massage has been found to increase range of motion (ROM) without impeding neuromuscular performance,1 based on no attenuation of maximal voluntary contraction,2,4,5 muscle activation as assessed by interpolated twitch technique,2 rate of force development,2,5 twitch force2,4 and half relaxation time,2 and electromechanical delay.4 While not fully elucidated, many possible mechanisms have been proposed for the aforementioned effects, including both mechanical and neurophysiological ones. Mechanical mechanisms describe a number of sub-mechanisms, such as fascial adhesions, piezoelectricity, cellular responses, myofascial trigger points, and/or thixotropic and viscoelastic properties of the tissue.1 Neurophysiological mechanisms can be divided into two primary submechanisms,1 spinal – associated with mechanoreceptors within muscle and fascia1,8 – and supraspinal – which include central pain modulation and descending noxious inhibitory control – both of which have been asserted to mediate perception.6,9
While self-massage has been shown to increase ROM in the majority,1 but not all,6 of investigations, the degree of ROM increase has been variable.1 These differences in outcomes may not only be due to the muscle group treated, overall volume of treatment, and differences in the applied pressure, but also the type of the tool used,1 particularly since it has been suggested that even the type of foam roller can have an effect on pressure that is applied to the underlying area.10 The two most commonly-employed tools for self-massage are the foam roller2,6,11 and roller massager.3-5 Roller massagers are similar to foam rollers in that they consist of a solid plastic cylinder enclosed by a small layer of dense foam, but differ from foam rollers insofar as they have a central axle that is grasped by hands, and that way applied to different parts of the body.1 MacDonald et al.2 applied a foam roller to the quadriceps muscle group for 2 sets of 60 seconds and observed an increase in knee joint ROM by 10.6 ° post intervention. When a roller massager was applied to the same muscle group, albeit only for 60 seconds, and the same test was used to measure ROM, the ROM increased by 8.6 °.3 While the difference between the studies may be explained by different pressures applied, as the participants of the former were instructed to apply as much of their body mass as possible onto the foam roller2 and the pressure in the latter study was controlled by a custom-made device,3 the influence of the type of tool used on the observed effect cannot be discounted. Furthermore, while the differences between the aforementioned studies are small and it is unclear whether the outcomes are real or meaningful, the results cannot be extrapolated to other modalities or body parts. Thus, more work is needed to understand the effect of different self-massage tools in order to guide appropriate practice. Specifically, should the effects be dependent on the type of the tool applied, it is important that practitioners are aware of it as to make their treatment more time-efficient.
Recent findings suggest that self-massage elicits global effects; that is, when one area of the body is treated, the effects are extended to neighboring regions. For example, it has been recently shown that overhead deep squat performance improved regardless of the body part rolled (i.e., lateral thigh, plantar surface of the foot, and lateral side of the trunk).12 Furthermore, Aboodarda et al.13 showed that pain pressure tolerance increases both in the ipsilateral (treated) calf as well as the contralateral one, and the same research group also demonstrated contralateral reductions in acute pain with evoked tetanic contractions after roller massage.14 Similarly, Kelly & Beardsley15 demonstrated a cross-over effect, whereby foam rolling the calf increased both ipsilateral and contralateral ROM of the ankle. However, whether the effects of self-massage are extended to different directions of movement about the same joint remains unclear. These findings have important clinical implications, in that non-local effects may be beneficial in rehabilitative protocols when an individual's skin or muscle is hypersensitive; for example, following surgery. That is, non-local effects allow for treatment outcomes (increased ROM) without the potential harms associated with direct contact.
Therefore, the purpose of this study was to investigate the acute effects of foam rolling and rolling massage of the anterior thigh on hip ROM – i.e., hip extension and hip flexion – in trained men. If observed effects are ‘global’ rather than ‘local’, one can expect to see changes in both hip extension and hip flexion, while ‘local’ effects will only be reflected by changes in hip extension.
METHODS
Participants
Eighteen resistance-trained men from the local university (age: 26.5 ± 4.2 years, height: 180.0 ± 4.2 cm, body mass: 92.8 ± 22.9 kg, BMI: 28.7 ± 6.3 m2/kg), with no prior foam rolling (FR) or rolling massage (RM) experience were recruited for the study. As per the questionnaire, participants had to be free of musculoskeletal injury or pain and were without existing neurological conditions. If participants were found to be hypermobile during baseline testing, they were excluded from the study. An a priori sample size calculation (effect size = 1.0; 1−β = 0.95; α = 0.05) using G*Power16 found that 12 participants would be sufficient to investigate the question posed; however, in order to increase statistical power by 50%, 18 were recruited. Anthropometric data included height (Stadiometer ES 2030 Sanny, São Paulo, Brazil) and body mass. Before the start of the study, all participants read and signed an informed consent document and a Physical Activity Readiness Questionnaire. Subjects were instructed to refrain from any lower body exercise or strenuous activity throughout the duration of the study. All procedures were in accordance with Declaration of Helsinki and the study was approved by the Institutional Review Board of University Hospital Clementino Fraga Filho of the Federal University of Rio de Janeiro.
Experimental design
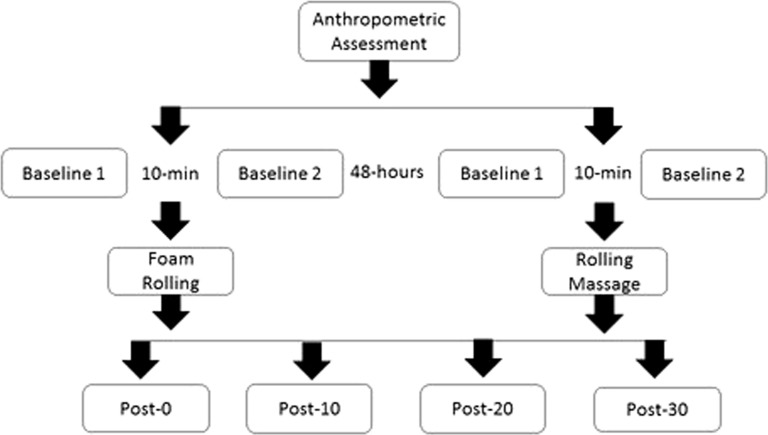
A single-blinded, randomized, crossover, within-subject design was used (Figure 1). Subjects visited the laboratory on two occasions over a four-day period with at least a day between each visit. Each session included two baseline ROM measures of passive hip flexion and extension, the order of which was randomized. The two measures were later averaged (average baseline). Recording of baseline measures was followed by the intervention of the day, which was either foam rolling or rolling massage as per randomization. Immediately following the intervention, passive hip flexion and extension ROM were measured again. In order to assess the time course of improvements in ROM, hip flexion and extension ROM were also measured at 10, 20, and 30 minutes post-intervention. These time points have been chosen to make the results more comparable to previous work.2,5,17 Only the dominant limb was tested as referenced to the limb that they would kick a ball with.11
Figure 1.
Study design – POST-0 = immediately post; POST-10 = 10-minutes post; POST-20 = 20-minutes post; POST-30 = 30-minutes post.
Procedures
Self-massage
Self-massage consisted of two protocols, depending on the tool used, both of which lasted for a single set of 120 seconds. This duration is similar to the study of MacDonald et al.,2 but different insofar as they split it into two sets.
The FR intervention was performed in a prone position with the anterior thigh of the test limb atop the foam roller (Foam Roller Brazil, Porto Alegre, RS, Brazil) as demonstrated previously (Figure 2).6 The foam roller used in this study consisted of a hard inner core enclosed in a layer of ethylene vinyl acetate foam, and has been shown to produce more pressure on the soft tissue.10 While keeping the knee of the dominant limb extended, participants were instructed to use their arms and the non-dominant limb to propel themselves backward and forward on the foam roller between the acetabulum and quadriceps tendon in fluid, dynamic motions. Subjects were encouraged to support their entire bodyweight with the foam roller and thus maximize pressure on the foam roller.
Figure 2.
The foam rolling procedure. A. starting point, B. end point.6
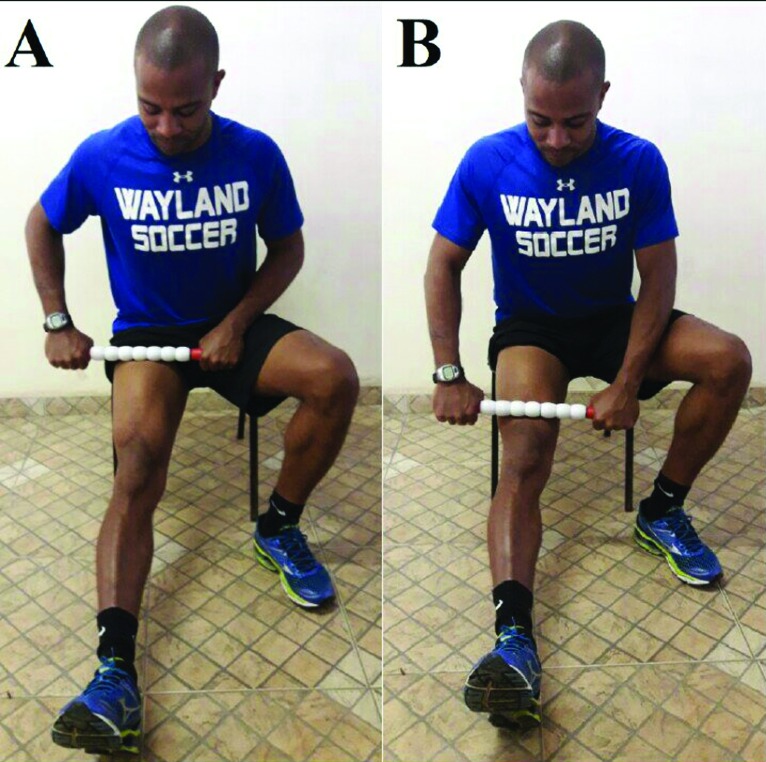
The RM intervention was performed with a self-massage stick (Stick Trigger Point Technologies, Austin, Texas, USA) up and down the anterior aspect of the thigh while in a seated position with the knee resting and extended. Subjects would then flex forward with their trunk to massage their anterior thigh. While it could be argued that this position placed the muscles of the thigh in an active state, the muscles are still thought to be relaxed as evidenced by electromyography recordings.18 Because the contact area during FR is likely greater, RM was applied with the self-massage stick at different angles in order to target all areas of the anterior thigh; i.e., medial (vastus medialis), lateral (vastus lateralis) and central (rectus femoris). Subjects were instructed to roll between the acetabulum and quadriceps tendon in fluid, dynamic motions. The pressure application was controlled by a pain level scale, in which a score of one represented no pain at all and a score of 10 represented the maximum pain that can be tolerated. Participants were instructed to apply pressure equivalent to between 6 and 8 on a pain level scale, similarly to instructions in previous work.5
Joint range of motion
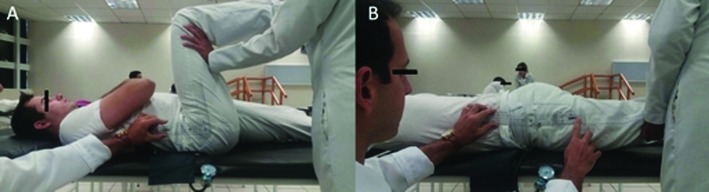
Passive hip flexion and extension ROM of the dominant limb were measured with a manual goniometer (Carci, São Paulo, BRA) using the standardized procedures outlined by Norkin and White.19 Hip flexion ROM was assessed in a supine position with the test knee flexed and the opposite knee extended (Figure 4A). A blood pressure cuff was placed under the lumbar spine and inflated to 60 mmHg, at which it was maintained for the duration of the measurement to ensure a stable lumbar spine.20 The test hip was flexed passively to the point of discomfort or anatomical limitation. The researcher aligned the axis of the goniometer with the greater trochanter and the arms of the goniometer with the lateral condyle of the femur and the mid-axillary line. When the trunk and thigh were collinear, hip flexion ROM was defined as 0 ° (positive ROM was defined by flexion of the hip). Hip extension ROM was assessed in a prone position with the knees extended (Figure 4B). The test hip was extended passively to the point of discomfort or anatomical limitation without the anterior thigh losing contact with the ground. To measure hip extension ROM, the experimenter aligned the axis of the goniometer with the greater trochanter, and the arms of the goniometer with the lateral epicondyle of the femur and the mid axillary line. When the trunk and thigh were collinear, hip extension ROM was defined as 0 ° (positive ROM was defined by extension of the hip). The arms were relaxed beside the body throughout ROM testing. The same experimenter collected all ROM data and was always blinded as to the intervention to which the participants had been subjected.
Figure 4.
Passive hip range of motion measurements. A = passive hip flexion; B = passive hip extension.
Figure 3.
The rolling massage procedure. A. starting point, B. end point.
Statistical methods
In order to identify differences between different time points, 95% confidence intervals (CI) of the change scores from the greatest baseline measure were calculated. 95% CI of the difference between these change scores were then calculated in order to identify between-intervention differences.21 Normality of the differences was ensured using the Shapiro-Francia test. Rather than traditional null hypothesis statistical testing, 95% CI were used in order to prevent the dichotomous interpretation of the results,22,23 to increase the likelihood of correct interpretation,22 and to allow for a more nuanced and qualitative interpretation of the data.24 For differences with a 95% CI that includes zero, it cannot be concluded that the observed differences are not due to chance alone; in other words, the observation are statistically different from one another when the 95% CI of differences does not equal zero. Additionally, Cohen's d effect-sizes were calculated using the formula , where Md is the mean difference and sd is the standard deviation of differences. This calculation differs slightly from traditional Cohen's d calculations, in that it better represents within-subject differences, whereas the traditional Cohen's d formula is better fit for between-subject comparisons.25-27 Cohen's d effect-sizes were defined as small, medium, and large for 0.2, 0.5, and 0.8, respectively.28 The combination of effect-sizes and 95% CI will therefore allow for a more nuanced and less polarizing interpretation of the results of the study.
In order to ensure that measures were greater than measurement error, minimum detectable change (MDC) scores were calculated at the 95% level. In order to calculate MDC, standard error of measurement (SEM) was calculated first, using the formula , where SDtest 1 is the standard deviation of scores from the first test and ICC is the test-retest intraclass correlation coefficient. Then, MDC at the 95% level was calculated using the formula . MDC is distinctly different from testing to see if the difference between pre and post intervention measurements differs from zero, as MDC strictly pertains to measurement error calculated from the reliability of measurement, while testing to see if changes differ from zero pertains to the change score and its variance relative to zero. For example, a change score can differ from zero, but still be within the MDC, or vice versa.
RESULTS
ICCs for baseline ROM measures and MDCs are presented in Table 1.
Table 1.
Intraclass correlation coefficients between the two baseline measures of range of motion and minimal detectable change for each measure of range of motion to ascertain reliability of baseline measures and assess whether the changes were greater than measurement error, respectively.
| ICC baseline flexion FR | 0.712 (95% CI = 0.376–0.882) |
| ICC baseline extension FR | 0.609 (95% CI = 0.206–0.834) |
| ICC baseline flexion RM | 0.535 (95% CI = 0.129–0.793) |
| ICC baseline extension RM | 0.583 (95% CI = 0.194–0.818) |
| MDC flexion FR | 10.31 º |
| MDC extension FR | 6.57 º |
| MDC flexion RM | 13.77 º |
| MDC extension RM | 4.02 º |
ICC = Intraclass Correlation Coefficient; MDC = Minimal Detectable Change; FR = foam rolling, RM = rolling massage.
The means and standard deviations of ROMs for each condition and time point are presented in Table 2.
Table 2.
Means and standard deviation for hip range-of-motion across conditions and time points. All results are expressed in degrees.
| Baseline mean | Post 0 | Post 10 | Post 20 | Post 30 | |
|---|---|---|---|---|---|
| FR flexion | 90.11 ± 6.91 | 112.00 ± 9.15 | 107.11 ± 11.52 | 101.00 ± 7.58 | 95.89 ± 6.63 |
| FR extension | 7.11 ± 3.77 | 15.89 ± 3.39 | 12.22 ± 2.73 | 10.56 ± 2.97 | 8.67 ± 3.00 |
| RM flexion | 92.56 ± 7.12 | 108.44 ± 9.27 | 103.44 ± 9.91 | 98.56 ± 8.91 | 91.89 ± 7.69 |
| RM extension | 7.22 ± 2.18 | 12.78 ± 2.92 | 11.33 ± 2.91 | 9.33 ± 2.91 | 7.78 ± 1.80 |
FR = foam rolling, RM = rolling massage; ‘Baseline mean’ = average of the two baseline scores, ‘post 0’ = immediately after intervention, ‘post 10’ = 10 minutes after intervention, ‘post 20’ = 20 minutes after intervention, ‘post 30’ = 30 minutes after intervention.
Mean within- and between-condition differences with accompanying 95% CIs and effect sizes are presented in Table 3. Hip flexion ROM statistically increased immediately after intervention with FR as compared to the baseline (Table 3). Furthermore, it remained statistically increased for 10-, 20-, and 30-minutes post intervention, respectively, with large effect sizes, but did not exceed MDC at 30-minutes post intervention. Similarly, hip extension ROM was statistically greater after the FR treatment and remained statistically increased for 10-, 20-, and 30-minutes post intervention, respectively, with medium to large effect sizes (Table 3). However, it only exceeded MDC immediately following treatment.
Table 3.
Mean within- and between-condition differences in hip range-of-motion, 95% confidence intervals and effect sizes.
| Post 0 - baseline | Post 10 - baseline | Post 20 - baseline | Post 30 – baseline | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean difference | 95% CI | d | Mean difference | 95% CI | d | Mean difference | 95% CI | d | Mean difference | 95% CI | d | |
| FR flexion | 21.89 | 18.72, 25.06* | 3.4 | 17.00 | 13.03, 20.97* | 2.1 | 10.89 | 7.81, 13.96* | 1.8 | 5.78† | 2.75, 8.81* | 0.9 |
| FR extension | 8.78 | 6.81, 10.74* | 2.2 | 5.11† | 2.97, 7.25* | 1.2 | 3.44† | 1.29, 5.60* | 0.8 | 1.56† | -0.27, 3.38 | 0.4 |
| RM flexion | 15.89 | 11.98, 19.80* | 2.0 | 10.88† | 6.05, 15.73* | 1.1 | 6.00† | 2.37, 9.63* | 0.8 | -0.67† | -3.37, 2.04 | 0.1 |
| RM extension | 5.56 | 4.45, 6.66* | 2.5 | 4.11 | 2.46, 5.76* | 1.2 | 2.11† | 0.77, 3.45* | 0.8 | 0.56† | -0.62, 1.73 | 0.2 |
| FR vs. RM flexion† | 6.00 | 0.91, 11.09* | 0.6 | 6.11 | 0.00, 12.22* | 0.5 | 4.89 | -0.05, 9.82 | 0.5 | 6.44 | 1.66, 11.23* | 0.7 |
| FR vs. RM extension† | 3.22 | 1.17, 5.27* | 0.8 | 1.00 | -1.82, 3.82 | 0.2 | 1.33 | -1.31, 3.98 | 0.3 | 1.00 | -0.91, 2.91 | 0.2 |
(*) illustrates statistically different as CI does not include 0; (†) illustrates values that did not exceed Minimum Detectable Change; FR = foam rolling, RM = rolling massage; ‘d’ = Cohen's d; ‘baseline’ = average of the two baseline scores, ‘post 0’ = immediately after intervention, ‘post 10’ = 10 minutes after intervention, ‘post 20’ = 20 minutes after intervention, ‘post 30’ = 30 minutes after intervention
Intervention with RM produced statistical increases in hip flexion and extension ROM when compared to the baseline (Table 3). Moreover, it remained statistically increased for 10- and 20-minutes post intervention, for both hip flexion and extension, respectively, with large effect sizes. However, for both hip flexion and extension, it only exceeded MDC immediately post and 10-minutes after intervention.
FR was statistically superior in improving hip extension ROM as compared to RM immediately post intervention relative to the baseline values with large effect size, as well as 30-minutes post with medium effect size (Table 3). Greater statistical increases in hip flexion ROM were also achieved in the FR condition as opposed to RM immediately post intervention and at 10- and 30-minutes post intervention (Table 3) with medium effect sizes. No other differences were found between interventions, and none of the observed differences exceeded the MDC.
DISCUSSION
The purpose of this study was to investigate the acute effects of foam rolling and rolling massage of anterior thigh on hip range-of-motion in trained men. The main findings of this study were: 1) FR and RM resulted in increased hip flexion and hip extension ROM immediately post intervention as compared to the baseline average, but these effects started to fall below the MDC in as little as 10 minutes; 2) FR was superior for improving hip flexion and hip extension ROM as compared to RM immediately post intervention, but this difference was not greater than the MDC; 3) FR was superior at improving hip flexion ROM as compared to RM 30-minutes post intervention, but these differences did not exceed the MDC.
To the authors' knowledge, this is the first study to have directly compared the acute effects of foam rolling to that of roller massage, and it appears that, for both hip flexion and extension, neither intervention is necessarily superior, because the differences between the two interventions did not exceed the MDC (Table 3). Although these interventions are similar, some differences do exist. For one, there are likely pressure differentials between foam rolling and roller massage, which were not measured. Specifically, participants were instructed to support their whole bodyweight in the FR condition, thereby maximizing the pressure, while they were told to apply a pressure equivalent to between 6 and 8 on a 10-level pain scale. Moreover, the efforts required by the participant in order to achieve greater pressures in each condition cannot be discounted, as foam rolling may be more passive than roller massage, in which the pressure is directly proportional to the force output of the participant. At present, the effects of pressure and effort alone, in addition to their interaction, in improving ROM, to the authors' knowledge, have yet to be fully elucidated; however, recent work by Gabrow et al.29 suggests that pressure differences result in more pain, but do not have implications for yielding differential active and passive ROM outcomes. Therefore, despite the fact that interventions in the present study likely resulted in different pressures, this should not have influenced the results.
Both interventions resulted in statistically increased ROM for 30-minutes post intervention. Findings from previous studies investigating the time course of acute effects of self-massage on increases in ROM are unclear, as some have found ROM to be increased only immediately post intervention,11 while others have found increases for at least 10 minutes,2,5,17 but not 30 minutes following the intervention.17 The discrepancy between studies may be a function of many parameters, including muscle group treated, volume of the intervention, level of pressure, and method of testing ROM. Considering the MDC in our study, hip extension ROM following FR and flexion following RM increased ROM only immediately post intervention, while hip extension ROM following RM remained increased 10 minutes post intervention. The former results are in line with Škarabot et al.,11 while the latter are in agreement with other studies.2,5,17
Interestingly, it was found that self-massage applied to the anterior thigh not only affects hip extension – as has been shown previously4,6,30,31 – but also affects hip flexion. This is a novel and important finding, as it suggests that the ROM effects of self-massage likely have a central component. Such a finding is in line with previous work by Aboodarda et al.,13 who found that self-massage applied to the calves not only increases pain pressure tolerance in the ipsilateral calf, but also the contralateral calf, suggesting central pain modulation may be at play. More recently, Kelly & Beardsley15 demonstrated a crossover effect, whereby foam rolling the ipsilateral calf not only increased ipsilateral dorsiflexion ROM, but also contralateral dorsiflexion ROM. These effects are similar to the non-local effects observed in stretching.32,33 Furthermore, it has been suggested that self-massage of the agonist can impede muscle activation of the antagonist,34 but it should be noted that it cannot be said for certain that the observed difference was real, since it did not exceed the MDC.35 Therefore, it appears that the effects of self-massage are not specific to the region(s) treated.
The ability for one to experience treatment effects in regions to where the treatment was not applied has important clinical applications. For example, if one has a wound to which pressure cannot be applied, but increased ROM is desired, such as following a proximal hamstrings repair,36 then self-massage applied to the quadriceps may be a viable option for increasing hip flexion ROM. The findings of this investigation and others13,15,32,33 evidence that non-local changes do indeed occur, which can allow for practitioners to improve their patients’ ROM without endangering the potentially-sensitive tissue surrounding the muscle of interest. Lastly, the choice of modality (i.e., FR or RM) may not be as important for maximal effectiveness.
In addition to the ROM findings, the results of this present study are also consistent with previous work by the authors of the present experiment.37,38 More specifically, it was found that self-massage applied to the agonist or antagonist musculature affected agonist performance during multiple sets of knee extensions. These effects were hypothesized to be attributable to a central opioidergic response, which could also account for the improvements in ROM observed in this present study.9 Specifically, in more noxious variations of massage therapy, such as self-massage, a descending inhibitory response is elicited via endogenous opioids and other neuropeptides acting on the periaqueductal grey and rostral ventromedial medulla.9 On a psychological level, such effects may be modulated by expectations,39 which have been shown to affect force inhibition/facilitation responses to stretching interventions.40 Furthermore, analgesia induced by techniques such as self-massage could have been mediated by autonomic nervous system (ANS) activity;41 that is, a shift from sympathetic to parasympathetic tone. The mechanism behind this ANS shift remains unclear, but it can be hypothesized that certain hormones and neuropeptides may be at play given that massage has been associated with changes in stress hormones42 (e.g., cortisol) and neuropeptides9 (e.g., endogenous opioids, oxytocin and endocannabinoids), and that the aforementioned hormones and neuropeptides that are associated with a sympathetic shift also play a role in descending modulatory pathways,43,44 which could account for changes in ROM. In essence, descending inhibition may have a role in stretch tolerance and, due to its diffuse nature, may explain the non-local effects observed in this study and others.13,15,32,33 However, despite the logical basis for the aforementioned neurophysiological mechanisms, the present investigation did not investigate them, and direct research into the mechanisms of self-massage are needed to further elucidate such mechanisms.
There are a number of limitations that should be taken into account when interpreting the findings in this study. Firstly, although the investigator was blinded as to which intervention was performed, the investigator was not blinded as to whether or not the participant performed an intervention. It is therefore possible that both the investigator and participant expected, and thus saw, improvements in ROM following each intervention. Moreover, goniometry was used to measure hip ROM, which is less objective than motion capture; however, because the changes exceeded the MDC, at least some of the observed changes are likely real. Secondly, the pace of rolling was not controlled for in both conditions, thereby reducing internal validity of the results due to the possibility of pace-dependent outcomes.6 However, not controlling for pace enhances ecological validity of the findings, as it is a better representative of the scenario in practice. Thirdly, participants in this study were males, and different results may be observed in females. Lastly, passive ROM was measured and improvements in passive ROM may not necessarily transfer to mobility in functional movement patterns.45 However, from a perspective of central mechanisms, the results are still relevant. Future studies in the area should try to expand these findings onto functional movement patterns. Notwithstanding these limitations, this work has important clinical and mechanistic implications, as it demonstrates that self-massage applied to the anterior thigh will not only increase hip extension ROM, but also hip flexion ROM.
Conclusions
The results of the present study indicate that FR and RM of the anterior thigh are equally effective at increasing hip flexion as well as hip extension ROM. These findings strongly suggest that the mechanisms for changes in ROM are at least partially central in nature, and further suggest that self-massage has a global effect. More data are needed to investigate the effects of foam rolling and roller massage on other joints and in other populations (e.g., rehabilitative).
REFERENCES
- 1.Beardsley C Škarabot J. Effects of self-myofascial release: a systematic review. J Bodyw Mov Ther. 2015;19:747-758. [DOI] [PubMed] [Google Scholar]
- 2.MacDonald GZ Penney MD Mullaley ME, et al. An acute bout of self-myofascial release increases range of motion without a subsequent decrease in muscle activation or force. J Strength Cond Res. 2013;27(3):812-821. [DOI] [PubMed] [Google Scholar]
- 3.Bradbury-Squires DJ Noftall JC Sullivan KM Behm DG Power KE Button DC. Roller-massager application to the quadriceps and knee-joint range of motion and neuromuscular efficiency during a lunge. J Athl Train. 2015;50(2):133-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sullivan KM Silvey DBJ Button DC Behm DG. Roller-massager application to the hamstrings increases sit-and-reach range of motion within five to ten seconds without performance impairments. Int J Sports Phys Ther. 2013;8(3):228-236. [PMC free article] [PubMed] [Google Scholar]
- 5.Halperin I Aboodarda SJ Button DC Andersen LL Behm DG. Roller massager improves range of motion of plantar flexor muscles without subsequent decreases in force parameters. Int J Sports Phys Ther. 2014;9(1):92-102. [PMC free article] [PubMed] [Google Scholar]
- 6.Vigotsky AD Lehman GJ Contreras B Beardsley C Chung B Feser EH. Acute effects of anterior thigh foam rolling on hip angle, knee angle, and rectus femoris length in the modified Thomas test. Peer J. 2015;3:e1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mikesky AE Bahamonde RE Stanton K Alvey T Fitton T. Acute effects of The Stick on strength, power, and flexibility. J Strength Cond Res. 2002;16(3):446-450. [PubMed] [Google Scholar]
- 8.Behm DG Peach A Maddigan M, et al. Massage and stretching reduce spinal reflex excitability without affecting twitch contractile properties. J Electromyogr Kinesiol. 2013;23(5):1215-1221. [DOI] [PubMed] [Google Scholar]
- 9.Vigotsky A Bruhns R. The role of descending modulation in manual therapy and its analgesic implications: a narrative review. Pain Res Treat. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Curran PF Fiore RD Crisco JJ. A comparison of the pressure exerted on soft tissue by 2 myofascial rollers. J Sport Rehabil. 2008;17(4):432-442. [DOI] [PubMed] [Google Scholar]
- 11.Škarabot J Beardsley C Štirn I. Comparing the effects of self-myofascial release with static stretching on ankle range-of-motion in adolescent athletes. Int J Sports Phys Ther. 2015;10(2):203-212. [PMC free article] [PubMed] [Google Scholar]
- 12.Monteiro ER Škarabot J Vigotsky AD Brown AF Gomes TM Novaes J da S. Acute effects of different self-massage volumes on the FMSTM overhead deep squat performance. Int J Sports Phys Ther. 2017;12(1):94-104. [PMC free article] [PubMed] [Google Scholar]
- 13.Aboodarda S Spence A Button D. Pain pressure threshold of a muscle tender spot increases following local and non-local rolling massage. BMC Musculoskelet Disord. 2015;16(1):265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cavanaugh MT Döweling A Young JD, et al. An acute session of roller massage prolongs voluntary torque development and diminishes evoked pain. Eur J Appl Physiol. 2017;117(1):109-117. [DOI] [PubMed] [Google Scholar]
- 15.Kelly S Beardsley C. Specific and cross-over effects of foam rolling on ankle dorsiflexion range of motion. Int J Sport Phys Ther. 2016;11(4):544-551. [PMC free article] [PubMed] [Google Scholar]
- 16.Faul F Erdfelder E Lang A-G Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175-191. [DOI] [PubMed] [Google Scholar]
- 17.Jay K Sundstrup E Søndergaard SD, et al. Specific and cross over effects of massage for muscle soreness: randomized controlled trial. Int J Sports Phys Ther. 2014;9(1):82-91. [PMC free article] [PubMed] [Google Scholar]
- 18.He H Kiguchi K Horikawa E. A study on lower-limb muscle activities during daily lower-limb motions. Int J Bioelectromagn. 2007;9(2):79-84. [Google Scholar]
- 19.Norkin C White J. Measurement of Joint Motion: A Guide to Goniometry. F.A: Davis Company; 2009. [Google Scholar]
- 20.Moreside J McGill S. Quantifying normal 3D hip ROM in healthy young adult males with clinical and laboratory tools: hip mobility restrictions appear to be plane-specific. Clin Biomech (Bristol, Avon). 2011;26(8):824-829. [DOI] [PubMed] [Google Scholar]
- 21.Gardner MJ Altman DG. Confidence intervals rather than P values: estimation rather than hypothesis testing. Br Med J (Clin Res Ed). 1986;292(6522):746-750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cumming G. The new statistics: why and how. Psychol Sci. 2014;25(1):7-29. [DOI] [PubMed] [Google Scholar]
- 23.Kline R. Beyond Significance Testing: Reforming Data Analysis Methods in Behavioral Research. Washington, D.C: American Psychological Association; 2004. [Google Scholar]
- 24.Dragicevic P. HCI Statistics without p-values. Inria. 2015:32. [Google Scholar]
- 25.Becker B. Synthesizing standardized mean-change measures. Br J Math Stat Psychol. 1988;41:257-278. [Google Scholar]
- 26.Morris SB. Estimating Effect Sizes From Pretest-Posttest-Control Group Designs. Organ Res Methods. 2007;11(2):364-386. [Google Scholar]
- 27.Smith L Beretvas S. Estimation of the Standardized Mean Difference for Repeated Measures Designs. J Mod Appl Stat Methods. 2009;8(2). [Google Scholar]
- 28.Cohen J. Statistical Power Analysis for Behavioral Sciences. Routledge Academic; 1988. [Google Scholar]
- 29.Gabrow L Young J Alcock L, et al. Higher Quadriceps Roller Massage Forces Do Not Amplify Range-of-Motion Increases. J Strength Cond Res. 2017;In press. [DOI] [PubMed] [Google Scholar]
- 30.Mohr A Long B Goad C. Effect of foam rolling and static stretching on passive hip-flexion range of motion. J Sport Rehabil. 2014;23(4):296-299. [DOI] [PubMed] [Google Scholar]
- 31.Couture G Karlik D Glass SC Hatzel BM. The effect of foam rolling duration on hamstring range of motion. Open Orthop J. 2015;9:450-455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Behm DG Cavanaugh T Quigley P Reid JC Nardi PSM Marchetti PH. Acute bouts of upper and lower body static and dynamic stretching increase non-local joint range of motion. Eur J Appl Physiol. 2016;116(1):241-249. [DOI] [PubMed] [Google Scholar]
- 33.Chaouachi A Padulo J Kasmi S Othmen A Ben Chatra M Behm DG. Unilateral static and dynamic hamstrings stretching increases contralateral hip flexion range of motion. Clin Physiol Funct Imaging. 2017;37(1):23-29. [DOI] [PubMed] [Google Scholar]
- 34.Cavanaugh MT Aboodarda SJ Hodgson D Behm DG. Foam Rolling of Quadriceps Decreases Biceps Femoris Activation. J strength Cond Res. September 2016:1. [DOI] [PubMed] [Google Scholar]
- 35.Cavanaugh MT Aboodarda SJ Behm DG. Intrasession and Intersession Reliability of Quadriceps' and Hamstrings' Electromyography During a Standardized Hurdle Jump Test With Single Leg Landing. J Strength Cond Res. 2017;31(6):1601-1609. [DOI] [PubMed] [Google Scholar]
- 36.Pombo M Bradley JP. Proximal hamstring avulsion injuries: a technique note on surgical repairs. Sports Health. 2009;1(3):261-264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Monteiro ER Škarabot J Vigotsky AD Brown AF Gomes TM Novaes J da S. Maximum repetition performance after different antagonist foam rolling volumes in the inter-set rest period. Int J Sports Phys Ther. 2017;12(1):76-84. [PMC free article] [PubMed] [Google Scholar]
- 38.Monteiro E Vigotsky A Škarabot J, et al. Acute effects of different foam rolling volumes in the inter-set rest period on maximum repetition performance. Hong Kong Physiother J. 2017;36: 57-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bjørkedal E Flaten MA. Expectations of increased and decreased pain explain the effect of conditioned pain modulation in females. J Pain Res. 2012;5:289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Janes WCI Snow BBG Watkins CE Noseworthy EAL Reid JC Behm DG. Effect of participants' static stretching knowledge or deception on the responses to prolonged stretching. Appl Physiol Nutr Metab. 2016;41(10):1052-1056. [DOI] [PubMed] [Google Scholar]
- 41.Bialosky JE Bishop MD Price DD Robinson ME George SZ. The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Man Ther. 2009;14(5):531-538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Field T Hernandez-Reif M Diego M Schanberg S Kuhn C. Cortisol decreases and serotonin and dopamine increase following massage therapy. Int J Neurosci. 2005;115(10):1397-1413. [DOI] [PubMed] [Google Scholar]
- 43.Carter CS. Oxytocin pathways and the evolution of human behavior. Annu Rev Psychol. 2014;65:17-39. [DOI] [PubMed] [Google Scholar]
- 44.Fields HL Heinricher MM Mason P. Neurotransmitters in nociceptive modulatory circuits. Annu Rev Neurosci. 1991;14:219-245. [DOI] [PubMed] [Google Scholar]
- 45.Moreside JM McGill SM. Improvements in Hip Flexibility Do Not Transfer to Mobility in Functional Movement Patterns. J Strength Cond Res. 2013;27(10):2635-2643. [DOI] [PubMed] [Google Scholar]