Abstract
Background and Purpose
Early sport specialization (ESS) refers to intense training year round in a specific sport starting at a young age with no or limited participation in other sports. This approach to training is highly controversial; recent literature suggests that this type of specialized training could be a contributing source to overuse injuries in youth athletes. The purpose of this case report was to describe a patellofemoral articular cartilage defect of the knee in a preadolescent skier due to overuse and repetitive microtrauma as a result of ESS.
Study Design
Case Report
Case Description
A healthy 11-year-old male competitive alpine skier presented with recurrent swelling of his right knee and persistent anterior knee pain while skiing without evidence of any specific history of injury or traumatic event. The patient failed a conservative treatment regimen including rest and formal physical therapy focused on generalized knee strengthening. Magnetic resonance imaging was ordered and revealed an articular cartilage defect of the medial patellar facet. The patient was treated with an arthroscopic debridement of his articular cartilage defect.
Outcome
At 12 weeks postoperatively, the patient presented with a normalized gait pattern, no evidence of knee effusion, full knee range of motion and patellar mobility symmetric to his contralateral limb, and no patellar crepitation or painful palpation on physical exam. The patient was released to begin return to sport progression at 12 weeks, and was cleared for full activities/returned to competitive skiing at 15 weeks postoperatively. At 16 weeks postoperatively, he won an international alpine ski race in Europe for his age group.
Discussion
Cartilage injuries and osteochondral defects are very common in adolescent athletes and often go undiagnosed. Allied healthcare professionals must be educated on the known causes of recurrent knee effusions and how early sport specialization may result in overuse injuries to knee joint cartilage.
Level of Evidence
4
Keywords: Anterior knee pain, early sport specialization, overtraining, overuse injuries
INTRODUCTION
It is estimated that 27 million U.S. youths participate in team sports, and approximately 60 million participate in some type of organized athletics.1 Most adolescents have taken to specializing in one sport as opposed to participation in multiple sport disciplines. Early sport specialization (ESS) refers to intense training year-round in a specific sport starting at a young age. This approach to training is highly controversial; recent literature suggests that this type of specialized training may increase the rate of acute injuries, overuse injuries, and ultimately lead to decreased sports participation.2-4 Sports which require high velocity movement and change of direction demands, for example alpine skiing, can lead to lower extremity overuse injuries.5,6
Anterior knee pain (AKP) is a common complaint in youth athletes.7 This complaint is usually diagnosed as patellofemoral pain and treatment commonly consists of nonoperative physical therapy, with a rehabilitation emphasis placed on strengthening quadriceps and generalized hip musculature. However, many conditions can cause AKP and swelling, especially after physical activity. AKP commonly results from irritation of the medial suprapatellar plica.8 Many youth athletes in repetitive jump/landing sports will develop patellar tendinopathy, Osgood-Schlatter disease, or Sinding-Larsen-Johansson disease—which often can mimic or even coincide with cartilage injuries. Osteochondritis dissecans (OCD) of the knee can also cause idiopathic AKP and swelling with activity.9 Osteochondritis dissecans of the knee is an injury to the subchondral bone and articular cartilage that usually develops in young athletes from overuse or acute trauma.9,10 Patients with an OCD lesion may present with no prior history of injury and often times a benign physical exam. While rest is indicated, most of the time OCD lesions continue to cause recurrent knee swelling (due to the intraarticular nature of this lesion, and altered mechanics resulting in intra articular effusion) which may differ from other extraarticular knee pathology (i.e. patellar tendinopathy, Osgood-Schlatter's disease). Unfortunately, OCD lesions are often unrecognized on diagnostic imaging, such as plain radiographs and magnetic resonance imaging. This presents a major challenge for clinicians when diagnosing and treating potential cartilage injuries of the knee. With recurrent knee effusions and AKP that does not respond to rest or conservative treatment, clinician's must rule out cartilage injuries as the source of pathology. The purpose of this case report was to describe a patellofemoral articular cartilage defect of the knee in a preadolescent skier due to overuse and repetitive microtrauma as a result of ESS.
SUBJECT PRESENTATION AND EXAMINATION
Verbal informed consent from both the subject and parents were obtained prior to publication. A healthy 11-year-old male (height: 160.0 cm; weight: 40.8 kg) competitive alpine skier presented with recurrent swelling of his right knee and persistent AKP while skiing without evidence of any specific history of injury or traumatic event. Of note, the athlete was a competitive skier who competed six days per week during the season and trained year-round, specializing in downhill ski racing. The athlete first disclosed his pain presentation to his parents and coaching staff after skiing practice. The parents subsequently referred the athlete to physical therapy and was prescribed a 2-week rest period with no skiing. After four weeks of generalized knee strengthening, the athlete (and his parents) presented for further orthopaedic evaluation due to recurrent knee effusions despite conservative rehabilitation. The patient presented with a history of recurrent knee effusions over a period of six weeks. While interviewing the patient, he denied any specific injury or fall that he could attribute to his knee pain and swelling. The patient presented with a slight limp causing an asymmetrical gait pattern that was non-painful. On physical exam, the patient had full knee range of motion with 2 + moderate effusion and tenderness to palpation over the medial aspect of the patella. His patellar mobility was equal bilaterally with no crepitation noted and his knee was stable during all ligamentous testing of the tibiofemoral joint.
INTERVENTIONS
Radiographs were obtained and revealed an anatomic variant, a bipartite patella, but no other acute bone abnormalities (Figure 1). Magnetic resonance imaging (MRI) was ordered and revealed an articular cartilage defect of the medial patellar facet (Figure 2A). The patient then underwent a diagnostic injection of a local, short-acting anesthetic to confirm or deny the source of intraarticular pathology as indicated on MRI. The patient had a positive diagnostic response, as the majority of his pain diminished soon after the injection.
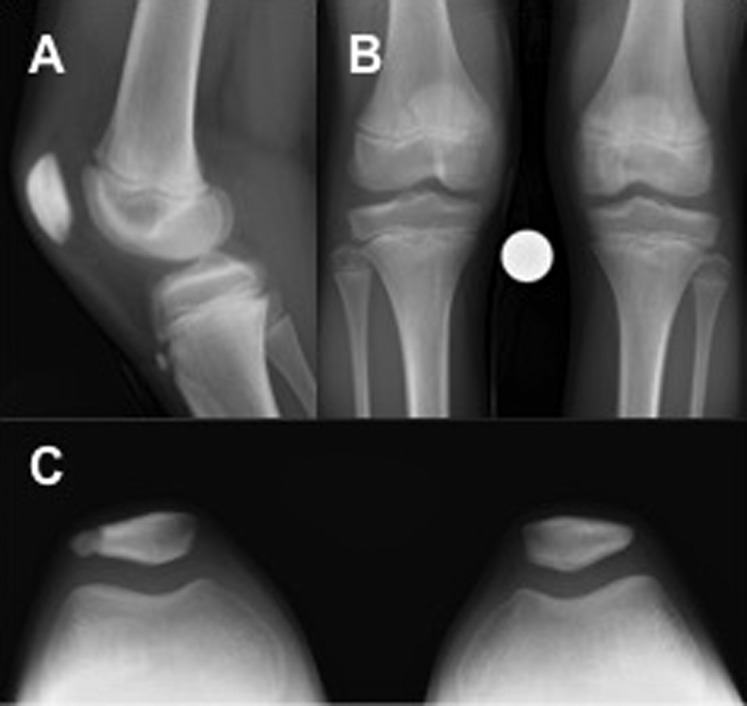
Figure 1.
Initial radiographs of patients injured right knee. Three view lateral (A), anteroposterior (B), and sunrise (C) radiographs with no acute bony abnormalities or OCD lesions present. It is noted that the patient did have the presence of an anatomic variant, a bipartite patella, noted on both the anteroposterior and sunrise views.
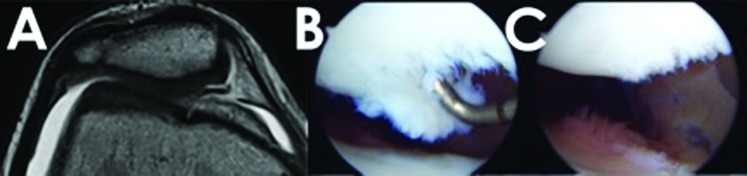
Figure 2.
Patellar chondral defect in an 11-year-old skier with no history of trauma or acute injury. A) Axial view of T1 weighted MRI, showing articular cartilage defect of medial patellar facet. B) Intraoperative view showcasing 10 mm wide Outerbridge grade IV focal chondral defect with delamination on the medial patellar facet. C) Chondral defect trimmed to stable border.
The patient underwent diagnostic arthroscopy the next day, which showed a 10 mm wide Outerbridge grade IV focal cartilage defect with delamination on the medial facet of his patella (Figure 2B). The chondral defect was treated with an arthroscopic chondroplasty to ensure that the cartilage defect did not continue to delaminate and cause recurrent effusions and pain with activity (Figure 2C). A chondroplasty was performed because the size, depth, and location of the lesion were not suitable for a cartilage resurfacing procedure (i.e. Osteoarticular Autograft Transplantation) or cellular based repair (i.e. Autologous Chondrocyte Implantation). No other intraarticular pathology was noted during the arthroscopic evaluation. The patient started formal physical therapy 24 hours after the procedure.
Postoperatively, the patient was allowed to weight bear as tolerated with the use of crutches for two weeks. Physical therapy initially focused on edema control, range of motion, and quadriceps activation exercises with a generalized progression from muscular endurance to strength and hypertrophy. A major emphasis was placed on rest from skiing and sports activities and allowing the patient's knee pain and swelling to subside before increasing activity. The focus of this case report is on diagnosis and relationship of ESS to AKP, not intervention, therefore, interventions are presented generally. At 12 weeks postoperatively, the patient presented with a normalized gait, no knee effusion, full knee range of motion, patellar mobility symmetric to his contralateral limb, and no patellar crepitation or painful palpation on physical exam. The patient was released to begin return to sport progression at 12 weeks, and was cleared for full activities with a return to competitive skiing at 15 weeks postoperatively. At 16 weeks postoperatively, he won an international alpine ski race in Europe for his age group.
DISCUSSION
Early sports specialization is common in the United States due to the theoretical consensus that early specialization in one sport is the recipe for creating superior athletes.11-13 However, not only has this theory been contradicted in terms of athlete and individual success,12,14 but there is growing evidence that this focus on one sport with excessive repetition of set movements and stressors can lead to unique pathology through overuse, even in the absence of acute trauma (Table 1).10,15-17
Table 1.
Categorization of risk factors for overuse injury. Adapted from DiFiori et al.6 Reprinted with permission.
|
Growth-related factors
Susceptibility of growth cartilage to repetitive stress Adolescent growth spurt |
|
Other intrinsic factors
Previous injury Previous level of conditioning Anatomic factors Menstrual dysfunction Psychological and developmental factors (athlete-specific) |
|
Extrinsic factors
Training workload (rate, intensity) Training progression Training and competition schedules Equipment/footwear Sport technique Psychological factors (adult and peer influences) |
Jayanthi et al17 performed a case controlled study on 1,190 athletes 7 to 18 years of age who were separated into two groups: injury and no injury. They found that those with injuries had a significantly greater number of hours training for their chosen sport, and furthermore they found sports specialization was an independent risk factor for injury. This theory of increased training hours and subsequent increased exposure has been correlated with increased injury risk in a young preadolescent cohort (9-12 years of age) of Japanese basketball players.18 Kuzuhara et al.18 attributed this increase injury incidence to the Japanese culture, in which most young athletes participate in one sport all year round. Furthermore, authors speculated that the higher injury rate in practice might be the direct result of sport specialization at a young age.18 Similarly, Hall et al.7 evaluated 546 middle and high school female multi-sport athletes with AKP and compared them to a group of female athletes who specialized in a single sport. The authors found that there was a significant increase in patellofemoral pain in athletes who specialized in a specific sport earlier compared to those who specialized later.19
Specific sports have been correlated with specific overuse injury patterns.18,20-23 Due to the biomechanics involved with throwing a baseball, and the tendency for ESS in the baseball culture, there have been studies that discuss the correlation between ESS in baseball with elbow and shoulder injuries.16,24 To date, there have not been any cases reported on the correlation between alpine skiing and patellofemoral chondral injuries. The relationship of skiing and injury to the patellofemoral joint is explained by the repetitive forces on the knee during sustained knee flexion, which brings the patella and trochlea into tight articulation. As the skier maneuvers over bumps and around course gates, repetitive microtrauma in the patellofemoral joint can lead to chondral injuries, especially in young athletes.25 This case report is an example of this potential relationship between patellofemoral chondral damage and ESS in alpine skiing. However, the assumption of this cause and effect relationship cannot be validated.
Youth injuries due to overuse in all sports range from 46% to 54%, with recent data suggesting that these numbers are increasing.4,10,13,21,26 Concerns for the rise in overuse injuries in young athletes are the increasingly popular trend of early single-sport specialization.11,12 However, some believe that overuse injuries are often under-reported in the current literature because most of the injury definitions have focused on time loss from sport.10,18,20 The American Orthopaedic Society for Sports Medicine (AOSSM) consensus statement14 defined early sports specialization according to 3 criteria: 1) participation in intensive training and/or competition in organized sports greater than eight months per year; 2) participation in one sport to the exclusion of participation in other sports; and 3) involving prepubertal children (grade 7 or roughly age 12 years old). In this case report, the athlete satisfies the criteria of ESS because of his single sport specialization, prepubertal age, and intensive ski competition > eight months per year. This is possible due to his unique ski academy in which he participates in on-snow training and competition in the United States (late October to April) and internationally (June to August). A recent position statement from the American Medical Society for Sports Medicine describes the importance of recognizing specific risk factors for overuse injury among youth athletes in order to deploy prevention strategies (Table 1).10 In order to decrease the risk of overuse injuries in young athletes associated with early sport specialization, the AOSSM consensus statement recommends the following: A) children who participate in more hours per week than their age, or more than 16 hours per week in intense training, and who are specialized in sport activities should be closely monitored for indicators of burnout, overuse injury, or potential decrements in performance due to overtraining; B) all youth (including inactive youth) can benefit from periodized strength and conditioning (e.g., Integrative Neuromuscular Training [INT]) to help them prepare for the demands of competitive sport participation; and C) youth who specialize in a single sport should plan periods of isolated and focused INT to enhance diverse motor skill development and reduce injury risk factors.14 In order to decrease the risk of future knee problems associated with ESS and skiing in this athlete, both the parents and the athlete were educated on the detrimental effects of single sport specialization at a young age. In addition, both the physical therapist and school athletic trainer were contacted and a team approach was implemented regarding a safe but efficient return to sport progression.
LIMITATIONS
The findings in this case report appear to be educational and representative of ESS; however, there are inherent limitations. While this overuse injury pattern may be representative of a larger group of individuals, it is still only a single case and therefore results cannot be directly extrapolated. It is also possible that the lesion could have developed from a source other than skiing. Furthermore, because the aim of this study was to describe the epidemiology of an injury presentation, and not evaluate the details or outcomes of treatment, there is not long-term follow-up to report.
CONCLUSIONS
With the presentation in this case report and the increasing incidence of ESS in youth athletes, allied health care professionals should consider patellofemoral chondral injury in the competitive skier with persistent AKP and recurrent effusions. This case report may provide insight to the detrimental consequences of overuse and skeletal immaturity associated with ESS in young skiers. However, future studies are needed to further identify injury risk factors and long-term outcomes within a larger group of similar patients.
REFERENCES
- 1.Feeley BT Agel J LaPrade RF. When is it too early for single sport specialization? Am J Sports Med. 2016;44(1):234-241. [DOI] [PubMed] [Google Scholar]
- 2.Post EG Bell DR Trigsted SM, et al. Association of competition volume, club sports, and sport specialization with sex and lower extremity injury history in high school athletes. Sports Health. 2017; 9(6):518-523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Post EG Trigsted SM Riekena JW, et al. The association of sport specialization and training volume with injury history in youth athletes. Am J Sports Med. 2017;45(6):1405-1412. [DOI] [PubMed] [Google Scholar]
- 4.Bell DR Post EG Trigsted SM Hetzel S McGuine TA Brooks MA. Prevalence of sport specialization in high school athletics: a 1-year observational study. Am J Sports Med. 2016;44(6):1469-1474. [DOI] [PubMed] [Google Scholar]
- 5.Steadman JR Swanson KR Atkins JW Hagerman GR. Training for alpine skiing. Clin Ortho Rel Res. 1987(216):34-38. [PubMed] [Google Scholar]
- 6.Sulheim S Holme I Rodven A Ekeland A Bahr R. Risk factors for injuries in alpine skiing, telemark skiing and snowboarding--case-control study. Br J Sports Med. 2011;45(16):1303-1309. [DOI] [PubMed] [Google Scholar]
- 7.Hall R Barber Foss K Hewett TE Myer GD. Sport specialization's association with an increased risk of developing anterior knee pain in adolescent female athletes. J Sport Rehab. 2015;24(1):31-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Griffith CJ LaPrade RF. Medial plica irritation: diagnosis and treatment. Cur Rev Musculo Med. 2008;1(1):53-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bruns J Werner M Habermann C. Osteochondritis dissecans: etiology, pathology, and imaging with a special focus on the knee joint. Cartilage. 2017; 8(3):211-228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.DiFiori JP Benjamin HJ Brenner JS, et al. Overuse injuries and burnout in youth sports: a position statement from the American Medical Society for Sports Medicine. Br J Sports Med. 2014;48(4):287-288. [DOI] [PubMed] [Google Scholar]
- 11.Myer GD Jayanthi N Difiori JP, et al. Sport specialization, part I: does early sports specialization increase negative outcomes and reduce the opportunity for success in young athletes? Sports Health. 2015;7(5):437-442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Myer GD Jayanthi N DiFiori JP, et al. Sports specialization, part II: alternative solutions to early sport specialization in youth athletes. Sports health. 2016;8(1):65-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cheatham SA Little BA. Early sports specialization: helpful or harmful? Orthopedics. 2015;38(12):724-725. [DOI] [PubMed] [Google Scholar]
- 14.LaPrade RF Agel J Baker J, et al. AOSSM early sport specialization consensus statement. Ortho J Sports Med. 2016;4(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nyland J. Coming to terms with early sports specialization and athletic injuries. J Orthop Sports Phys Ther. 2014;44(6):389-390. [DOI] [PubMed] [Google Scholar]
- 16.Ferguson B Stern PJ. A case of early sports specialization in an adolescent athlete. J Canad Chiro Assoc. 2014;58(4):377-383. [PMC free article] [PubMed] [Google Scholar]
- 17.Jayanthi NA LaBella CR Fischer D Pasulka J Dugas LR. Sports-specialized intensive training and the risk of injury in young athletes: a clinical case-control study. Am J Sports Med. 2015;43(4):794-801. [DOI] [PubMed] [Google Scholar]
- 18.Kuzuhara K Shibata M Uchida R. Injuries in japanese mini-basketball players during practices and games. J Athl Train. 2016;51(12):1022-1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hall R Foss KB Hewett TE Myer GD. Sports specialization is associated with an increased risk of developing anterior knee pain in adolescent female athletes. J Sport Rehabil. 2015;24(1):31-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dompier TP Powell JW Barron MJ Moore MT. Time-loss and non-time-loss injuries in youth football players. J Athl Train. 2007;42(3):395-402. [PMC free article] [PubMed] [Google Scholar]
- 21.Fabricant PD Lakomkin N Sugimoto D Tepolt FA Stracciolini A Kocher MS. Youth sports specialization and musculoskeletal injury: a systematic review of the literature. Physic Sports Med. 2016;44(3):257-262. [DOI] [PubMed] [Google Scholar]
- 22.Post EG Thein-Nissenbaum JM Stiffler MR, et al. High school sport specialization patterns of current division I athletes. Sports Health. 2017;9(2):148-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Smith J DePhillipo N Kimura I Kocher M Hetzler R. Prospective functional performance testing and relationship to lower extremity injury incidence in adolescent sports participants. Int J Sports Phys Ther. 2017;12(2):206-218. [PMC free article] [PubMed] [Google Scholar]
- 24.Tisano BK Estes AR. Overuse injuries of the pediatric and adolescent throwing athlete. Med Sci Sports Exerc. 2016;48(10):1898-1905. [DOI] [PubMed] [Google Scholar]
- 25.Steadman JR Hanson CM Briggs KK Matheny LM James EW Guillet A. Outcomes after knee microfracture of chondral defects in alpine ski racers. J Knee Surg. 2014;27(5):407-410. [DOI] [PubMed] [Google Scholar]
- 26.Brenner JS, Council On Sports M, Fitness. Sports specialization and intensive training in young athletes. Pediatrics. 2016;138(3). [DOI] [PubMed] [Google Scholar]