Abstract
Introduction
When darunavir (DRV) 800 mg is boosted with 150 mg cobicistat (DRV cobi), DRV trough concentration (Ctrough) is about 30% lower as compared to 100 mg ritonavir (DRV rtv). DRV cobi shows similar virological efficacy as DRV rtv when combined with two nucleos(t)ide analogue reverse‐transcriptase inhibitors, but it is unknown whether a lower DRV Ctrough would undermine the effectiveness of DRV cobi when given as monotherapy (mtDRV cobi).
Methods
Prospective observational study on virologically suppressed HIV‐infected subjects who switched to mtDRV cobi. Virological failure was defined as two consecutive HIV‐RNA >200 copies/mL. Efficacy was evaluated by intention‐to‐treat (ITT) and on‐treatment (OT) analyses, and compared with data from a previous cohort of subjects on mtDRV rtv conducted at our centre. Plasma DRV Ctrough was measured using LC–MS/MS.
Results
A total of 234 subjects were enrolled. At week 96, the efficacy rates were 67.8% (CI 95, 61.8 to 73.7) by ITT and 86.9% (CI 95, 78.0 to 87.7) by OT analyses. The corresponding rates in our historical DRV rtv controls were 67.6% (CI 95, 60.0 to 75.2) and 83.6% (CI 95: 77.2 to 90.0). A total of 135 DRV determinations were performed in 83 subjects throughout the follow‐up period, with a median plasma DRV Ctrough of 1305 ng/mL (range, 150 to 5895) compared with 1710 ng/mL (range, 200 to 3838) in subjects on monotherapy with DRV rtv (p = 0.05).
Conclusions
DRV Ctrough was lower in HIV‐infected subjects receiving DRV cobi than with DRV rtv. However, this did not appear to influence the efficacy of DRV cobi, when administered as monotherapy.
Keywords: Darunavir, cobicistat, ritonavir, monotherapy, pharmacokinetic, Ctrough
1. Introduction
Cobicistat is a potent and selective human CYP3A inhibitor without anti‐HIV activity showing a lower potential for undesirable drug‐drug interactions when compared to ritonavir (rtv) 1. When darunavir (DRV) 800 mg was boosted with cobicistat 150 mg (DRVcobi) once daily in healthy volunteers, DRV exposure was within the limits of bioequivalence for C max and AUC24h compared to DRVrtv, but DRV Ctrough were about 30% lower 2. This difference may not be clinically relevant for combined antiretroviral therapy (cART) since DRVcobi has shown similar virological efficacy as DRVrtv when administered in combination with two nucleos(t)ide analogue reverse‐transcriptase inhibitors (NRTIs) 3, 4. However, it remains unclear whether this is also true for DRVcobi when given as monotherapy (mtDRVcobi).
Data derived from both clinical trials and real‐life practice suggest that most subjects with long‐lasting virological suppression maintain undetectable viraemia 48 to 96 weeks after switching to DRVrtv monotherapy (mtDRVrtv). However, mtDRVrtv is less effective than cART, as transient detectable viral loads (blips) are more frequent 5, 6, 7, 8. Since 2009, protease inhibitor (PI)‐based monotherapy is considered as a simplification option in both the Spanish and European guidelines for the use of antiretroviral agents in HIV‐1‐infected adults without history of failure on prior PI‐based therapy and who have had viral load <50 copies/mL for more than 6 months 9, 10. In the clinical practice, DRVrtv is currently being replaced by DRVcobi, but there are no data about the effectiveness of mtDRVcobi and whether a lower DRV Ctrough could impacts on efficacy or an increase in the numbers of blips. The aim of this study was to evaluate the efficacy of mtDRVcobi in the daily clinical practice, to analyse the relationship between pharmacokinetic parameters and virological failure, and to compare it with historical data on mtDRVrtv.
2. Materials and methods
This prospective observational study was carried out at the Virgen del Rocío University Hospitals in Spain. All subjects who maintained virological suppression ≥6 months and who switched to mtDRVcobi once daily from January 2015 to January 2016 were included. Subjects with previous virological failure (VF) while on a PI‐containing regimen were included if the genotypic resistance tests showed no major (I47V, I50V, I54M/L, L76V and I84V) or ≤3 minor resistance mutations associated with reduced susceptibility to DRV according to the 2014 International AIDS Society criteria 11. The prescription of mtDRVcobi was based on the criteria of the attending physicians as part of their daily clinical practice based on the encouraging results of several clinical trials 12, 13, 14, 15, 16, 17 and personal experience on boosted‐PI monotherapy 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, with the objective of avoiding toxicity associated with nucleoside analogues, increasing adherence, and to augment the cost‐effectiveness of therapy 29. Inclusion was not dependent on CD4+ T cell counts, hepatitis C virus (HCV) coinfection, laboratory parameters or the presence of viral blips during the previous 12 months.
In our hospital, mtDRVcobi was not prescribed in case of pregnancy, hepatitis B coinfection or for concomitant use with drugs having potential adverse interactions with DRVcobi pharmacokinetics 30. This study was conducted according to the principles of the Declaration of Helsinki and was approved by the Ethics Committee for Clinical Research of the Virgen del Rocío University Hospital. All subjects provided written informed consent to use their anonymized data and to perform plasma drug monitoring.
2.1. Endpoints, follow‐up and assessments
The primary clinical endpoint was treatment effectiveness, assessed as the percentage of subjects with virological suppression after 48 and 96 weeks according to intention‐to‐treat (ITT) analysis (non‐complete/missing = failure). Virological failure (VF) was defined as two consecutive confirmed plasma HIV‐RNA >200 copies/mL, or a single HIV‐RNA level >200 copies/mL if followed by a loss to follow‐up. A cut‐off level of 200 copies/mL was chosen as a more accurate measurement of VF since values <200 copies/mL suffer high variability and the risk of emerging resistance is believed to be relatively low 31, 32. An additional estimation of virological failure rates using 50 copies/mL as criteria for VF was made to compare with other studies. As a secondary outcome, virological efficacy was assessed using on‐treatment (OT) analysis, where subjects who discontinue therapy for any reason, as well as those who are lost to follow‐up, are not considered. In addition, a pharmacological sub‐study was performed in which the association between plasma levels and treatment outcome was analysed. As reference, efficacy data and pharmacological results were compared with those of a historical cohort of 150 subjects who started mtDRVrtv at our centre 8.
Subject assessments were performed at baseline and every 3 months thereafter, including adherence (subject self‐report and pharmacy records), adverse events (AEs), biochemical and haematological profiles, flow cytometric counts of CD4+ T cells and plasma HIV‐RNA levels (COBAS AmpliPrep/COBAS TaqMan HIV‐1 test, version 2.0). AEs and abnormal laboratory findings were evaluated according to a standardized toxicity grade scale (AIDS Clinical Trials Group) 33. Genotypic resistance tests were performed on subjects with VF when viral load levels were sufficient. Subjects who missed two consecutive scheduled visits were considered lost to follow‐up.
2.2. Blood sampling and determination of DRV concentrations
Blood samples were drawn 24 h (±30 min) after the previous DRVcobi dose taken after standard breakfast and processed within an hour after collection. Plasma was separated and stored at −80°C until assayed. Separation was performed on a Phenomenex Luna C18 (5 μm, 150 × 2.0 mm) analytical column. The mobile phase was composed of 2 mM ammonium acetate 0.1% formic acid and acetonitrile 0.1% formic acid. DRV was extracted from the plasma by protein precipitation, using acetonitrile containing a deuterated internal standard. Plasma DRV concentrations were determined using LC–MS/MS based on an adapted method 34 with standard curves that were highly linear over the range of 50 to 10,000 ng/mL and an intra‐ and inter‐assay precision and accuracy of <15%.
2.3. Statistical analysis
Categorical and quantitative variables were compared using the χ2 test, Student's t‐test or Mann‐Whitney nonparametric test, according to their distribution. Time‐to‐event analyses were performed by Kaplan‐Meier survival curves. Both the intra‐ and inter‐subject variability in drug concentrations was measured using the coefficients of variation (CV) of the available values from each subject. Pharmacokinetic data were compared with those of the historical DRVrtv cohort 8, where 587 samples from 119 subjects were analysed. Statistical analyses were performed using the IBM software (SPSS v. 23.0, Chicago, USA), and p‐values <0.05 were considered significant.
3. Results and discussion
A total of 234 subjects were included in the study with a median follow‐up of 96 weeks (IQR, 58 to 96; range, 24 to 96). Baseline characteristics are described in Table 1. Before switching to mtDRVcobi, 175 (74.8%) subjects were on monotherapy as maintenance regimen (144 on DRVrtv, and 31 on LPVrtv), while 48 (20.5%) and 11 (4.7%) subjects were on triple and dual therapy, respectively.
Table 1.
Baseline characteristics of the study population (n = 234)
| Parameter | Value |
|---|---|
| Male, no. (%) | 178 (76.1) |
| Age (years), M (IQR) | 49.5 (43 to 54) |
| Weight (kg), M (IQR) | 71.5 (62.5 to 83) |
| BMI kg/m2, M (IQR) | 25 (22 to 27) |
| Nadir CD4+/μL, M (IQR) | 150 (52 to 248) |
| CD4+ T cells/μL, M (IQR) | 662 (512 to 837) |
| Zenith HIV‐RNA log10 copies/mL, M (IQR) | 4.8 (4.1 to 5.3) |
| Previous CDC C stage, no (%) | 66 (28.2) |
| Risk factor for HIV, no. (%) | |
| Previous intravenous drug use | 96 (41) |
| Homosexual contact | 62 (26.5) |
| Heterosexual contact | 66 (28.2) |
| Other | 10 (4.3) |
| Chronic hepatitis C, no. (%) | 40 (17.1) |
| Cirrhosis no. (%) | 8 (3.4) |
| Months on treatment, M (IQR) | 141 (92 to 195) |
| Months with undetectable HIV‐RNA, M (IQR) | 85 (50 to 119) |
| Presence of blips in the previous 12 months, no. (%) | 22 (9.4) |
| Previous failure on protease inhibitors, n (%) | 154 (65.8) |
| Previous ART regimens | |
| Monotherapy regimens | 175 (74.8) |
| DRVrtv monotherapy | 144 (61.5) |
| LPVrtv monotherapy | 31 (13.2) |
| Dual therapy regimens | 11 (4.7) |
| ATV + 3 TC | 7 (2.9) |
| DRVrtv + 3TC | 1 (0.42) |
| Others | 3 (1.28) |
| Triple therapy regimens | 48 (20.5) |
| CKD‐EPI mL/min/1.73 m2, M (IQR) | 99.1 (83.2 to 105.8) |
| CKD‐EPI < 60 mL/min/1.73 m2, no. (%) | 3 (1.2) |
M (IQR), Median (interquartile range), CDC, Centers of Disease Control; HCV, hepatitis C virus; ART, antiretroviral therapy; DRVrtv, ritonavir‐boosted darunavir; LPVrtv, ritonavir‐boosted lopinavir; ATV, atazanavir; 3TC, lamivudine; CKD‐EPI, Chronic Kidney Disease Epidemiology Collaboration.
One hundred and fifty‐four (65.8%) subjects had an earlier VF while receiving non‐boosted PI, including 30 (12.8%) subjects who had experienced a previous VF on a DRVrtv‐based regimen caused by treatment withdrawal. Genotypic resistance tests before switching to mtDRVcobi was available for 127 subjects who had shown VF, including all 30 subjects who had failed to DRVrtv, showing no major resistance mutations to DRV in any case.
3.1. Efficacy and safety
The Kaplan‐Meier estimations of treatment effectiveness by ITT analysis were 82.5% (CI95, 77.6 to 87.3) and 67.8% (CI95, 61.8 to 73.7) at week 48 and 96, respectively, while the historical control data with mtDRVrtv were 82.7% (CI95, 76.7 to 88.7) and 67.6% (CI95, 60.0 to 75.2) respectively. In an OT analysis, the values in the present cohort were 94.4% (CI95, 91.4 to 97.3) and 86.9% (CI95, 78.0 to 87.7), respectively, and 94.4% (CI95, 91.4 to 97.3) and 83.6% (CI95: 77.2 to 90.0) in the historical cohort (Figure 1). The estimations of virological failure rates using 50 copies/mL as criteria for virological failure are displayed in Table 2.
Figure 1.
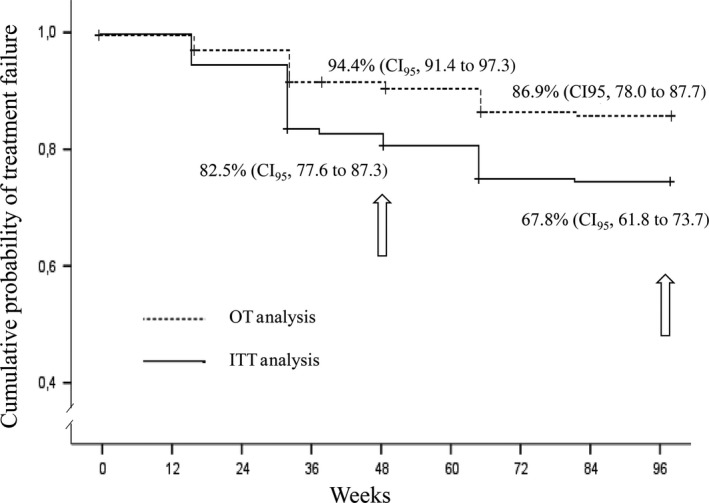
Kaplan‐Meier estimations of efficacy by on‐treatment (OT) and by intention‐to‐treat (ITT) at 48 and 96 weeks.
Table 2.
Kaplan‐Meier estimations of the efficacy of mtDRVcobi using HIV‐RNA >50 copies/mL x2 or >50 x1 followed by loss to follow‐up as definition for virological failure
| Virological failure definition | Virological efficacy | |
|---|---|---|
| Week 48 | Week 96 | |
|
HIV‐RNA >200 copies/mL x2 or >200 x1 followed by loss to follow‐up |
94.4% (CI95, 91.4 to 97.3) |
86.2% (81.7 to 90.6) |
|
HIV‐RNA >50 copies/mL x2 or >50 x1 followed by loss to follow‐up |
88.9% (CI95: 84.8 to 92.9 |
81.4% (CI95: 76.4 to 86.3) |
Twenty‐seven subjects (11.5%) had VF as defined by the protocol with a median plasma HIV‐RNA at failure of 1450 copies/mL (IQR, 244 to 5707). Eleven of these subjects were on cART before switching to monotherapy, 14 subjects were on monotherapy regimens and two on dual therapy.
There was no significant difference in the VF rates among those subjects with and without an earlier VF while on a PI‐based regimen (9.7% vs. 15.0% respectively; p = 0.263). Furthermore, 60 (25.6%) subjects had a blip episode while on mtDRVcobi, whereas this figure was 27.6% in the historical cohort on mtDRVrtv (p = 0.713). After 6 months, 26 out of 27 subjects who experienced a VF regained virological control either by adding one (n = 11) or two (n = 8) NRTIs to mtDRVcobi or switching to another triple therapy (n = 8). Other treatment failures were due to AEs (n = 7; grade 2 hypercholesterolaemia, 1; grades 1 and 3 hypertriglyceridaemia, 2; and grade 1 gastrointestinal disorder, 4), loss to follow‐up or treatment dropout (n = 10), switching to another regimen by physician decision without VF criteria (n = 6), death unrelated to treatment (n = 1),and other reasons not related to the treatment, such as imprisonment, pregnancy, drug interactions or relocation (n = 22). All these subjects had an undetectable viral load at the time of the last available HIV‐RNA assessment.
Regarding the CD4+ T cell counts, the mean increase from baseline to week 96 was 75 cells/mL (CI95, 25 to 125). Aminotransferase level elevations throughout the follow‐up occurred in 6/40 (15%) subjects with chronic hepatitis (grades 1, 5; grades 2, 1) and in 17/194 (8.8%) subjects without chronic hepatitis (grades 1, 12; grades 2, 2; grades 3, 1). All aminotransferase elevations were transient and improved without treatment modification. No significant changes were found in the lipid profiles. Overall, the mean changes in fasting total cholesterol and triglycerides in the subjects who completed 96 weeks were 5 mg/dl (CI95,−3 to 13) and −17 mg/dL (CI95, −42 to 7) (p‐values >0.1).
3.2. Pharmacokinetics of DRV
A total of 135 DRV determinations were performed in plasma samples derived from 83 subjects throughout the follow‐up period. The median of the plasma samples per subject was 2 (range, 1 to 2). Plasma DRV Ctrough was lower for mtDRVcobi (median, 1305 ng/mL; IQR, 652 to 2058; range, 150 to 5895) as compared to data of subjects on DRVrtv, (median, 1710 ng/mL; IQR, 1160 to 2210; range, 200 to 3838) (p = 0.05). We did not observe relationships between plasma DRV concentrations and weight (r 2 = 0.106; p = 0.340) or body mass index (r 2 = 0.127; p = 0.282), nor differences in plasma DRV Ctrough according to gender, the presence of chronic hepatitis, cirrhosis or renal dysfunction. The median intra‐subject variability was 27.4% (IQR, 18.5 to 54.0; range, 12.8 to 130.5) for subjects on mtDRVcobi, and 38.8% (IQR, 25.4 to 59.1; range, 3.7 to 213.1) for subjects on mtDRVrtv. Inter‐subject variability for subjects with more than one DRV Ctrough determination (n = 57) was 92.1% for those on mtDRVcobi and 43.6% for those on mtDRVrtv, respectively. We did not find any statistically significant difference between DRV plasma concentration and subjects with and without VF, median; 738 ng/mL (IQR; 467 to 2037) and 1378 ng/mL (IQR; 705 to 2185) (p = 0.710) respectively.
Although somewhat less effective than triple therapy, more than 90% of virologically suppressed subjects switching to mtDRVrtv maintained virological control in the clinical practice, even in subjects with previous VF‐ on PI‐based regimens when no major resistance mutations for DRV were present 7, 8. As it has been reported from various studies, monotherapy has a higher frequency of blips, although this has not been related to a higher frequency of VF. Moreover, in patients who failure on monotherapy with boosted PI, no resistance mutations have been found, and the introduction of analogues has been enough to control the infection again 35, 36, 37. These results, the benefits of regimens lacking the toxicity of nucleoside analogues, the low incidences and grades of the AEs, and to save up in antiretroviral drug costs 29 support the use of mtDRVrtv in clinical practice.
Recently, Ciaffi et al. reported a rate of virological failure as high as 21% at week 48 with DRV‐ or lopinavir‐based monotherapy as second‐line maintenance treatment for HIV‐1‐infected patients in sub‐Saharan Africa 38. Almost certainly these results were due to the fact that only 80% of the patients had a viral load <50 copies/mL at baseline.
Currently, DRVrtv is being replaced by DRVcobi in spite of an about 30% lower DRV Ctrough as observed in healthy volunteers. To the best of our knowledge, this is the first study addressing the effectiveness of mtDRVcobi. Our results show that the DRV Ctrough is about 22% lower for DRVcobi than the concentrations observed from our historical data with mtDRVrtv. However, these concentrations remain above sixfold the protein binding‐adjusted EC90 for wild‐type HIV‐1 (200 ng/mL) and above threefold the protein binding‐adjusted EC50 for resistant HIV‐1 (550 ng/mL) 39 in most subjects. Two and 13 subjects had a Ctrough below of 200 and 550 ng/mL, respectively, of whom only two subjects had VF, presenting a DRV Ctrough of 463.82 and 353.83 ng/mL. While the intra‐subject variability in DRV Ctrough, was similar for both regimens, the inter‐subject variability appeared to be higher in the case of DRVcobi, although the number of subjects is insufficient to draw conclusions on this issue. Nonetheless, the effectiveness was similar to that observed previously with mtDRVrtv 7, 8. The frequency of AEs in the present study was below 2%, which can in part be explained by the large proportion of subjects who were on a DRVrtv‐based regimen before switching to mtDRVcobi.
Our study has some limitations. First, blood samples for drug monitoring in the present study was not as frequent as in the earlier study, as in the last years the blood samples for the control of the HIV infection can be collected in primary health centres from where the samples are transferred in the same morning to our hospital. However, the analysis of pharmacokinetics was not the primary aim of the present work and still a considerably high proportion of patients representing the overall population could be analysed. Furthermore, although the number of subjects with VF are low, the data obtained from those subjects who were virologically suppressed show that the lower DRV concentrations observed when boosting with cobicistat appear not to impact on treatment outcome. Second, data from a previous cohort on mtDRVrtv was used as reference, since the present study is a prospective observational study that does not include controls. Still, both data sets were obtained from one single cohort including subjects seen at one single centre and by the same physicians, following a unique protocol. Therefore, the data can be regarded as comparable.
4. Conclusion
According to the data obtained in our study, it seems that the change ritonavir to cobicistat does not affect the efficacy of monotherapy with DRV, regardless of the lower plasma Ctrough achieved.
Competing interests
L. F. Lopez‐Cortes, P. Viciana and N. Espinosa have received unrestricted research funding, consultancy fees, and lecture fees from and have served on the advisory boards of Abbott, Bristol‐Myers Squibb, Gilead Sciences, Janssen‐Cilag, Merck Sharp & Dohme, and ViiV Healthcare. The other authors have no conflicts of interest to disclose.
Authors’ contributions
LFLC, AGV and MTR conceptualized and designed the study.
LFLC obtaining funding for the study.
LFLC, PV and NE contributed to provision of study materials or subjects.
AGV and TFM collected darunavir plasma levels.
AGV and MTR collected, assembled the data and managed the database.
AGV, MTR and LFLC analysed and interpreted the data.
AGV, MTR and LFLC drafted the article.
NE and PV critically reviewed the article for important intellectual content.
All authors approved the final version of the article:.
Acknowledgments
The authors are indebted to the subjects for their involvement in this study.
Gutierrez‐Valencia, A. , Trujillo‐Rodriguez, M. , Fernandez‐Magdaleno, T. , Espinosa, N. , Viciana, P. and López‐Cortés, L. F. Darunavir/cobicistat showing similar effectiveness as darunavir/ritonavir monotherapy despite lower trough concentrations. J Int AIDS Soc. 2018; 21(2):e25072
References
- 1. Deeks ED. Cobicistat: a review of its use as a pharmacokinetic enhancer of atazanavir and darunavir in patients with HIV‐1 infection. Drugs. 2014;74(2):195–206. [DOI] [PubMed] [Google Scholar]
- 2. Kakuda TN, Opsomer M, Timmers M, Iterbeke K, Van De Casteele T, Hillewaert V, et al. Pharmacokinetics of darunavir in fixed‐dose combination with cobicistat compared with coadministration of darunavir and ritonavir as single agents in healthy volunteers. J Clin Pharmacol. 2014;54(8):949–57. [DOI] [PubMed] [Google Scholar]
- 3. Tashima K, Crofoot G, Tomaka FL, Kakuda TN, Brochot A, Van de Casteele T, et al. Cobicistat‐boosted darunavir in HIV‐1‐infected adults: week 48 results of a Phase IIIb, open‐label single‐arm trial. AIDS Res Ther. 2014;1(11):39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mills A, Crofoot G Jr, McDonald C, Shalit P, Flamm JA, Gathe J Jr, et al. Tenofovir alafenamide versus tenofovir disoproxil fumarate in the first protease inhibitor‐based single‐tablet regimen for initial HIV‐1 therapy: a randomized phase 2 study. J Acquir Immune Defic Syndr. 2015;69(4):439–45. [DOI] [PubMed] [Google Scholar]
- 5. Valantin MA, Lambert‐Niclot S, Flandre P, Morand‐Joubert L, Cabiè A, Meynard JL, et al. Long‐term efficacy of darunavir/ritonavir monotherapy in patients with HIV‐1 viral suppression: week 96 results from the MONOI ANRS 136 study. J Antimicrob Chemother. 2012;67(3):691–5. [DOI] [PubMed] [Google Scholar]
- 6. Clumeck N, Rieger A, Banhegyi D, Schmidt W, Hill A, Van Delft Y, et al. 96 week results from the MONET trial: a randomized comparison of darunavir/ritonavir with versus without nucleoside analogues, for subjects with HIV RNA <50 copies/mL at baseline. J Antimicrob Chemother. 2011;66(8):1878–85. [DOI] [PubMed] [Google Scholar]
- 7. Lopez‐Cortes LF, Castano MA, Lopez‐Ruz MA, Rios‐Villegas MJ, Hernández‐Quero J, Merino D, et al. Effectiveness of ritonavir‐boosted protease inhibitor monotherapy in clinical practice even with previous virological failures to protease inhibitor‐based regimens. PLoS ONE. 2016;11(2):e0148924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gutierrez‐Valencia A, Torres‐Cornejo A, BenMarzouk‐Hidalgo OJ, Ruiz‐Valderas R, Lluch A, Viciana P, et al. Darunavir minimum plasma concentration and ritonavir‐boosted darunavir monotherapy outcome in HIV‐infected patients. Antivir Ther. 2014;19(5):443–7. [DOI] [PubMed] [Google Scholar]
- 9. European AIDS Clinical Society . European Guidelines for treatment of HIV infected adults in Europe. Version 9. 2017. [cited 2017 Nov 1]. Available from http://www.eacsociety.org/files/guidelines_9.0-english.pdf.
- 10. Panel de expertos de GeSIDA y Plan Nacional sobre el Sida . Documento de consenso de GeSIDA/Plan Nacional sobre el Sida respecto al tratamiento antirretroviral en adultos infectados por el virus de la inmunodeficiencia humana. 2017. [cited Oct 1 2017]. Available from: http://gesida-seimc.org/wp-content/uploads/2017/02/gesida-guiasclinicas-2017-TAR.pdf.
- 11. Wensing AM, Calvez V, Günthard HF, Johnson VA, Paredes R, Pillay D, et al. 2017 Update of the drug resistance mutations in HIV‐1. Top Antivir Med. 2017;24(4):132–3. [PMC free article] [PubMed] [Google Scholar]
- 12. Arribas JR, Pulido F, Delgado R, Lorenzo A, Miralles P, Arranz A, et al. Lopinavir/ritonavir as single drug therapy for maintenance of HIV‐1 viral suppression: 48‐week results of a randomized, controlled, open‐label, proof‐of‐concept pilot clinical trial (OK Study). J Acquir Immune Defic Syndr. 2005;40(3):280–7. [DOI] [PubMed] [Google Scholar]
- 13. Pulido F, Delgado R, Pérez‐Valero I, González‐García J, Miralles P, Arranz A, et al. Long‐term (4 years) efficacy of lopinavir/ritonavir monotherapy for maintenance of HIV suppression. J Antimicrob Chemother. 2008;61(6):1359–61. [DOI] [PubMed] [Google Scholar]
- 14. Arribas JR, Delgado R, Arranz A, Muñoz R, Portilla J, Pasquau J, et al. Lopinavir‐ritonavir monotherapy versus lopinavir‐ritonavir and 2 nucleosides for maintenance therapy of HIV: 96‐week analysis. J Acquir Immune Defic Syndr. 2009;51(2):147–52. [DOI] [PubMed] [Google Scholar]
- 15. Meynard JL, Bouteloup V, Landman R, Bonnard P, Baillat V, Cabie A, et al. Lopinavir/ritonavir monotherapy versus current treatment continuation for maintenance therapy of HIV‐1 infection: the KALESOLO trial. J Antimicrob Chemother. 2010;65(11):2436–44. [DOI] [PubMed] [Google Scholar]
- 16. Mathis S, Khanlari B, Pulido F, Schechter M, Negredo E, Nelson M, et al. Effectiveness of protease inhibitor monotherapy versus combination antiretroviral maintenance therapy: a meta‐analysis. PLoS ONE. 2011;6:e22003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Arribas JR, Doroana M, Turner D, Vandekerckhove L, Streinu‐Cercel A. Boosted protease inhibitor monotherapy in HIV‐infected adults: outputs from a pan‐European expert panel meeting. AIDS Res Ther. 2013;10(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Neth O, Falcon‐Neyra L, Ruiz‐Valderas R, León Leal JA, Obando I, Benito C. A., et al. Simplified human immunodeficiency virus maintenance therapy in virologically suppressed children with Ritonavir‐boosted protease inhibitor monotherapy. Pediatr Infect Dis J. 2011;30(10):917. [DOI] [PubMed] [Google Scholar]
- 19. Lopez‐Cortes LF, Ruiz‐Valderas R, Sánchez‐Rivas E, Lluch A, Gutierrez‐Valencia A, Torres‐Cornejo A, et al. Lopinavir plasma concentrations and virological outcome with lopinavir‐ritonavir monotherapy in HIV‐1‐infected patients. Antimicrob Agents Chemother. 2013;57(8):3746–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Torres‐Cornejo A, Benmarzouk‐Hidalgo OJ, Gutiérrez‐Valencia A, Pérez‐Romero P, Martín‐Peña R, Ruiz‐Valderas R, et al. Cellular HIV reservoir replenishment is not affected by blip or intermittent viremia episodes during darunavir/ritonavir monotherapy. AIDS. 2014;28(2):201–8. [DOI] [PubMed] [Google Scholar]
- 21. Pasquau J, López‐Cortés L, Mayorga MI, Viciana P, Del Mar Arenas M, Ríos MJ, et al. Monotherapy with darunavir/ritonavir is effective and safe in clinical practice. J Int AIDS Soc. 2014;17(4 Suppl 3):19813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. BenMarzouk‐Hidalgo OJ, Torres‐Cornejo A, Gutiérrez‐Valencia A, Ruiz‐Valderas R, Viciana P, López‐Cortés LF. Immune activation throughout a boosted darunavir monotherapy simplification strategy. Clin Microbiol Infect. 2014;20(12):1297–303. [DOI] [PubMed] [Google Scholar]
- 23. Torres‐Cornejo A, Benmarzouk‐Hidalgo OJ, Gutierrez‐Valencia A, Ruiz‐Valderas R, Viciana P, López‐Cortés LF. Low concordance and resistance mutation emergence in the HIV protease gene among circulating and cell‐associated viruses at viral replication episodes during darunavir/ritonavir monotherapy. HIV Med. 2015;16(1):57–61. [DOI] [PubMed] [Google Scholar]
- 24. Falcon‐Neyra L, Benmarzouk‐Hidalgo OJ, Madrid L, Noguera‐Julian A, Fortuny C, Neth O, et al. No differences of immune activation and microbial translocation among HIV‐infected children receiving combined antiretroviral therapy or protease inhibitor monotherapy. Medicine (Baltimore). 2015;94(11):e521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. BenMarzouk‐Hidalgo OJ, Torres‐Cornejo A, Gutiérrez‐Valencia A, Ruiz‐Valderas R, Viciana P, López‐Cortés LF. Differential effects of viremia and microbial translocation on immune activation in HIV‐infected patients throughout ritonavir‐boosted darunavir monotherapy. Medicine (Baltimore). 2015;94(17):e781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Torres‐Cornejo A, BenMarzouk‐Hidalgo OJ, Viciana P, Sánchez B, López‐Ruz MA, López‐Cortés LF, et al. Protease inhibitor monotherapy is effective in controlling human immunodeficiency virus 1 shedding in the male genital tract. Clin Microbiol Infect. 2016;22(1):98.e7–10. [DOI] [PubMed] [Google Scholar]
- 27. BenMarzouk‐Hidalgo OJ, Torres‐Cornejo A, Gutierrez‐Valencia A, Ruiz‐Valderas R, Viciana P, López‐Cortés LF. Higher activation in CD4(+) T cells but similar viral control among HIV/Hepatitis C virus‐coinfected patients on a simplification monotherapy. AIDS Res Hum Retroviruses. 2016;32(1):6–11. [DOI] [PubMed] [Google Scholar]
- 28. Benmarzouk‐Hidalgo OJ, Torres‐Cornejo A, Gutierrez‐Valencia A, Viciana P, López‐Cortés LF. HIV‐1 p24 and CD4+ T cell count during boosted protease‐inhibitor monotherapy in HIV‐infected patients. Enferm Infect Microbiol Clin. 2017;35(3):174–8. [DOI] [PubMed] [Google Scholar]
- 29. Pasquau J, Gostkorzewicz J, Ledesma F, Anceau A, Hill A, Moecklinghoff C. Budget impact analysis of switching to darunavir/ritonavir monotherapy for HIV‐infected people in Spain. Appl Health Econ Health Policy. 2012;10(2):139–41. [DOI] [PubMed] [Google Scholar]
- 30. Rezolsta (darunavir/cobicistat). Full prescribing information. Janssen‐Cilag SpA. European Medicine Agency. [Updated 12/12/2014. cited 2014 Dec 30]. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_Product_Information/human/002819/WC500178953.pdf
- 31. Panel on Antiretroviral Guidelines for Adults and Adolescents . Guidelines for the use of antiretroviral agents in HIV‐1‐infected adults and adolescents. Department of Health and Human Services. 2016. [cited 2016 Jul 16]. Available from: https://aidsinfo.nih.gov/contentfiles/adultandadolescentgl.pdf.
- 32. Ruelle J, Debaisieux L, Vancutsem E, De Bel A, Delforge ML, Piérard D, et al. HIV‐1 low‐level viremia assessed with 3 commercial real‐time PCR assays show high variability. BMC Infect Dis. 2012;24(12):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. U.S. Department of Health and Human Services, National Institutes of Health, National Institute of Allergy and Infectious Diseases, Division of AIDS . Division of AIDS (DAIDS) Table for Grading the Severity of Adult and Paediatric Adverse Events, Version 2.0. 2014. [cited 2017 July 16]. Available from: http://rsc.tech-res.com/docs/default-source/safety/daids_ae_grading_table_v2_nov2014.pdf
- 34. Fayet A, Béguin A, Zanolari B, Cruchon S, Guignard N, Telenti A, et al. A LC‐tandem MS assay for the simultaneous measurement of new antiretroviral agents: raltegravir, maraviroc, darunavir, and etravirine. J Chromatogr B Analyt Technol Biomed Life Sci. 2009;877:1057–69. [DOI] [PubMed] [Google Scholar]
- 35. Arribas JR, Girard PM, Paton N, Winston A, Marcelin AG, Elbirt D, et al. Efficacy of protease inhibitor monotherapy vs. triple therapy: meta‐analysis of data from 2303 patients in 13 randomized trials. HIV Med. 2016;17(5):358–67. [DOI] [PubMed] [Google Scholar]
- 36. Gazzard B, Hill A, Anceau A. Cost‐efficacy analysis of the MONET trial using UK antiretroviral drug prices. Appl Health Econ Health Policy. 2011;9(4):217–23. [DOI] [PubMed] [Google Scholar]
- 37. Oddershede L, Walker S, Stöhr W, Dunn DT, Arenas‐Pinto A, Paton NI, et al. Cost effectiveness of protease inhibitor monotherapy versus standard triple therapy in the long‐term management of HIV patients: analysis using evidence from the PIVOT trial. Pharmacoeconomics. 2016;34(8):795–804. [DOI] [PubMed] [Google Scholar]
- 38. Ciaffi L, Koulla‐Shiro S, Sawadogo AB, Ndour CT, Eymard‐Duvernay S, Mbouyap PR, et al. Boosted protease inhibitor monotherapy versus boosted protease inhibitor plus lamivudine dual therapy as second‐line maintenance treatment for HIV‐1‐infected patients in sub‐Saharan Africa (ANRS12 286/MOBIDIP): a multicentre, randomised, parallel, open‐label, superiority trial. Lancet HIV. 2017;4:e384–92. [DOI] [PubMed] [Google Scholar]
- 39. PREZISTA™ (Tibotec, Inc.) (Darunavir). Full prescribing information. Food and drug administration. 2008. [cited 2016 Oct 31]. Available from: http://accessdata.fda.gov/drugsatfda_docs/label/2008/021976s003s004lbl.pdf.


