Abstract
Background and aims
The Republic of Moldova is a small ex-soviet country in the Central Eastern European group of states, whose official language is Romanian. In countries with limited resources, quality improvement in healthcare and patient safety are very challenging. This study aims to identify which areas of the patient safety culture (PSC) need prompt intervention.
Methods
A cross-sectional study was conducted in three Moldovan healthcare settings, using the Romanian translation of the US Hospital Survey on Patient Safety Culture HSOPSC. Descriptive statistics were carried out, based on the responses from n. 929 staff. Percentages of positive responses (PPRs) by item (41 items) and composite (12 PSC areas) were computed.
Results
Most respondents were nurses (53%), followed by doctors (35%). The main work areas were: primary care (27%), medical specialties (20%), gynecology and obstetrics (16%), and general surgery (11%). The highest composite PPRs were for: teamwork within units (80%), feedback & communication about error, organizational learning-continuous improvement and supervisor/manager expectations & actions promoting patient safety (78%), and management support for patient safety (75%). The lowest composites were for: frequency of events reported (57%), non-punitive response to errors (53%), communication openness (51%) and staffing (37%).
Conclusion
Our results suggest that staffing issues should be tackled to provide safe care. Staff avoid to openly report adverse events and/or discuss errors, likely because a poor understanding of the potential of these events for learning and because of fear of blame or punitive actions. Future research should check psychometrics of the Romanian version of the HSOPSC applied to Moldovan staff.
Keywords: organizational culture, patient safety, survey, low-income country, Republic of Moldova
Background and aims
In recent years there has been a widely spread international interest in patient safety. Systematic evaluation of key outcome indicators and assessment of staff perceptions and attitudes toward patient safety help healthcare organizations identify priority areas for improving safety and quality of healthcare. In the Republic of Moldova patient safety data are not routinely collected and analyzed and there is no formal and reliable statistical evidence on patient safety at a national level. In the context of the actions taken at European and international level, this country assumed commitments for developing a public policy on patient safety, in compliance with the recommendations formulated by the European Union (EU), the Council of Europe and the World Health Organization (WHO) [1].
The Republic of Moldova is one of the Central and Eastern Europe former socialist states (CEE). Demographic, economic and healthcare key indicators in this country are illustrated in Box 1 [2]. It is the poorest country in Europe, with 41% of its 4 million inhabitants living below the poverty line (i.e. US $5 daily) in 2014 [3]. Precarious material context (obsolete physical infrastructure and equipment, and insufficient supplies) and inadequate healthcare staff and staffing (number and allocation, training and retention) are critical obstacles to the assurance of patient safety, as in most low-income countries. [4–6] Another obstacle is represented by the hierarchical dynamics, governance and accountability, which are still tributary to the ancient healthcare system, despite years of reforms since the independence of the country from the former Soviet Union (1991).
Box 1. Facts on the Republic of Moldova: demographic, economic and healthcare key indicators.
| DEMOGRAPHICS |
|
|
| Mid-year population (2015): 4,068,897 |
| -% of population aged 0–14 years (2014): 16 |
| -% of population aged 65+ years (2014): 10 |
| Crude death rate per 1000 population (2014): 11 |
| Infant deaths per 1000 live births (2014): 10 |
| Life expectancy at birth (years) 2014: 72 |
| -females (2014): 76 |
| -males (2014): 68 |
|
|
| ECONOMY |
|
|
| Gross domestic product per capita (2015) : 1,843 US $ |
|
|
| HEALTHCARE |
|
|
| Total health expenditure, PPP*$ per capita (2014): 514 US $ |
| Total health expenditure as % of GDP** (2014): 10 |
| Public-sector health expenditure as % of total health expenditure (2014): 51 |
| Hospital beds per 100,000 (2014): 566 |
| Average length of stay, all hospitals (2014): 9 |
| Doctors per 100,000 (2014): 291 |
| Nurses per 100,000 (2014): 608 |
purchasing power parity;
gross domestic product
Source: European Health for All database (HFA-DB) WHO/Europe July 2016 [2]
Independently of the resources of a country, improving patient safety requires attention to both culture and the organizational system [4]. Currently, the Republic of Moldova does not have in use any tool to assess patient safety culture. The US Agency for Healthcare Research and Quality (AHRQ).
Hospital Survey on Patient Safety Culture (HSOPSC) is a questionnaire released in 2004 that has been translated into 31 languages and experimented in 66 countries across the world [7]. The European Network for Patient Safety (EUNetPas) has been an important promoter of this tool in Europe. [8] Thus, after an initial wave of application in high-income European countries (UK, France, The Netherlands, Belgium, Germany, etc.) [9–13] several middle-low income CEE countries have tested it in their hospital sector in recent years (Slovenia, Croatia, Slovakia, Kosovo, Romania) [14–18].
Since the official language in the Republic of Moldova is that of Romania, in this study the Romanian version of the HSOPSC has been applied in three Moldovan healthcare facilities. The aims were to identify which areas of patient safety culture need further improvement and to compare patient safety perceptions among the main work areas and among doctors and nurses.
Material and methods
Participants and settings
The study was carried out in three healthcare settings in Chisinau (the capital of the Republic of Moldova), which voluntarily participated in the project. The settings in the study were: one public hospital with an inpatient capacity of 530 beds (A), one private clinic (B) and one territorial medical association (C) providing primary care and secondary healthcare services, mainly to outpatients. The sample study was based on the census of all clinical and non-clinical staff i.e. 976 staff: 410 in setting A; 113 in setting B; and 453 in setting C. We received 944 completed questionnaires, out of which 929 were valid for statistical analysis. Overall, this equates to an adjusted response rate of 95%, ranging from 93% (setting A) to 96% (setting C).
Questionnaire and key variables
The 42 items of the original US survey use a five-point scale to measure agreement (from strongly agree to strongly disagree) or frequency (from always to never). The items measure seven unit-level process dimensions (supervisor expectations and actions promoting patient safety, organizational learning - continuous improvement, teamwork within hospital units, communication openness, feedback and communication about error, non-punitive response to error and staffing); three hospital-level process dimensions (hospital management support for patient safety, teamwork across hospital units and hospital handoffs and transitions) and two outcome dimensions (overall perception of safety and frequency of event reporting). The survey also includes two single-item outcome variables: a global safety grade between poor and excellent (Please give your area/unit in this hospital an overall grade on patient safety) and the number of incidents reported in the past year (In the past 12 months, how many event reports have you filled out and submitted?). Some items are reverse worded: disagreement or low frequency indicate a positive response in terms of patient safety culture.
Methodology
Thanks to a collaborative international project (Progetto IRIDE: Italia - Romania - Repubblica Moldova in Rete: Imparando dagli errori verso una cultura della sicurezza dei pazienti/utenti) coordinated by Agenzia di Tutela della Salute of Bergamo (Italy) and involving the Republic of Moldova and Romania as well, the US HSOPSC was translated (with back translation) into Romanian, by a team of healthcare professionals fluent in English. Subsequently, the translated tool was pre-tested on a group of both Romanian and Moldovan doctors and nurses, to check that the language was familiar and culturally appropriate for the target population. In the final version, one item in the staffing dimension, concerning the use of temporary staff, was removed. It is not common in the Romanian or Moldovan healthcare system to hire temporary staff. The paper questionnaire was administered in the Republic of Moldova in 2014, in February (settings A and B) and October (setting C). In all settings, the data collection lasted one month. The questionnaire was anonymous and each questionnaire was numbered before distribution.
Data analysis
After the data input, we used the number marked on each questionnaire to check the accuracy of the paper information transcription in electronic records. We also used the AHRQ quality criteria for checking our data set. A total of 15 records were excluded from the final analyses as the respondents answered less than one entire section of the questionnaire, fewer than half of the items throughout the entire survey or scored all the items in the same way.
Descriptive analyses were computed to summarize respondents’ characteristics. For each item and dimension, percentages of positive responses (PPRs) were calculated, based on the respondents who answered “Strongly Agree/Agree” or “Always/Most of the time” to positively worded items or who disagreed with those negatively worded. Ninety-five % confidence intervals (95% CI) were used to determine statistical significance of the PPRs.
Results
Table I illustrates the respondents’ general characteristics, as well as their perception of the patient safety grade in their workplace and the number of the adverse events they reported in the last year (output indicators). Most respondents were nurses (53%), followed by doctors (35%). Primary care (27%), medical specialties (20%), gynecology and obstetrics (16%), and general surgery (11%) were the work areas with most respondents. About one third of the respondents had worked in the same facility (35%)/unit (30%) for more than 21 years. Most staff (90%) reported less than 60 working hours per week. Two thirds of the staff perceived the patient safety grade as “excellent” (20%)/”very good” (39%) and one third as “acceptable”. Most staff did not report any adverse event in the last 12 months (68%).
Table I.
General characteristics of the respondents (I) and output indicators (II).
| Variable | Frequency | % | |
|---|---|---|---|
| I. ACTUARIAL CHARACTERISTICS | |||
| Work Area | A. Primary care | 252 | 27 |
| B. Medical specialties | 186 | 20 | |
| C. Gynecology and obstetrics | 144 | 15 | |
| D. Surgery | 99 | 11 | |
| E. Laboratory | 72 | 8 | |
| F. Anesthesiology and intensive care | 67 | 7 | |
| G. Dentistry | 47 | 5 | |
| H. Other | 62 | 7 | |
| Work in the Facility (years) | <1 | 39 | 4 |
| 1–5 | 164 | 18 | |
| 6–10 | 134 | 14 | |
| 11–15 | 121 | 13 | |
| 16–20 | 146 | 16 | |
| 21 or more | 325 | 35 | |
| Work in the Unit (years) | <1 | 57 | 6 |
| 1–5 | 192 | 21 | |
| 6–10 | 142 | 15 | |
| 11–15 | 122 | 13 | |
| 16–20 | 137 | 15 | |
| 21 or more | 279 | 30 | |
| Working hours in the Unit per week | <20 | 25 | 3 |
| 20–39 | 468 | 50 | |
| 40–59 | 343 | 37 | |
| 60–79 | 71 | 8 | |
| 80–99 | 11 | 1 | |
| 100 or more | 11 | 1 | |
| Staff position in the Facility | Doctor | 329 | 35 |
| Nurse/midwife | 489 | 53 | |
| Unit assistant/clerk/secretary | 27 | 3 | |
| Other (Chemist, Dietician, etc) | 84 | 9 | |
| Direct interaction or contact with patients/users | Yes | 843 | 91 |
| No | 86 | 9 | |
| Experience in the profession (years) | <1 | 35 | 4 |
| 1–5 | 122 | 13 | |
| 6–10 | 116 | 13 | |
| 11–15 | 115 | 12 | |
| 16–20 | 150 | 16 | |
| 21 or more | 391 | 42 | |
| II. OUTPUT INDICATORS | |||
| Patient Safety Grade | Excellent | 183 | 20 |
| Very Good | 363 | 39 | |
| Acceptable | 339 | 37 | |
| Poor | 29 | 3 | |
| Failing | 2 | 0 | |
| No response | 13 | 1 | |
| Number of Events Reported | None | 630 | 68 |
| 1–2 | 188 | 20 | |
| 3–5 | 40 | 4 | |
| 6–10 | 25 | 3 | |
| 11–20 | 0 | 0 | |
| 21 or more | 5 | 1 | |
| No response | 41 | 4 |
Table II shows the overall staff percentage of positive responses for the patient safety culture (PPRs), by item and dimension. The item “We are actively doing things to improve patient safety” (89%) received the highest PPR, while the negatively worded item “Staff in this unit work longer hours than is best for patient care” received the lowest one (16%). The highest scored dimensions were teamwork within units (80%); feedback & communication about error, organizational learning-continuous improvement and supervisor/manager expectations & actions promoting patient safety (78%); and management support for patient safety (75%). The lowest scored dimensions were: frequency of events reported (57%), non-punitive response to errors (53%), communication openness (51%) and staffing (37%).
Table II.
Hospital SOPSC: response frequency (N) and percentage of positive responses (PPRs)1 by survey item and composite2, with 95% confidence intervals (CI).
| Composite and survey item (N= 929 respondents) | N | PPR | 95%CI |
|---|---|---|---|
| 1. Teamwork Within Units | 3686 | 80.1 | 78.8–81.4 |
| A1. People support one another in this Unit. | 925 | 88.1 | 86.0–90.2 |
| A3. When a lot of work needs to be done quickly, we work together as a team to get the work done. | 919 | 85.8 | 83.5–88.0 |
| A4. In this Unit people treat each other with respect. | 921 | 81,2 | 78.7–83.7 |
| A11. When one area in this Unit gets really busy, others help out. | 921 | 65.3 | 62.2–68.3 |
| 2. Supervisor/Manager Expectations & Actions Promoting Patient Safety | 3615 | 77.8 | 76.5–79.2 |
| B1. My supervisor/manager says a good word when he/she sees a job done according to established patient safety procedures. | 907 | 84.0 | 81.6–86.4 |
| B2. My supervisor/manager seriously considers staff suggestions for improving patient safety. | 902 | 85.3 | 82.9–87.6 |
| B3r. Whenever pressure builds up, my supervisor/manager wants us to work faster, even if it means taking shortcuts. | 901 | 58.2 | 54.9–61.4 |
| B4r. My supervisor/manager overlooks patient safety problems that happen over and over. | 905 | 83.9 | 81.5–86.3 |
| 3. Organizational Learning—Continuous Improvement | 2737 | 78.3 | 76.8–79.8 |
| A6. We are actively doing things to improve patient safety. | 923 | 89.1 | 87.0–91.1 |
| A9. Mistakes have led to positive changes here. | 904 | 59.2 | 56.0–62.4 |
| A13. After we make changes to improve patient safety, we evaluate their effectiveness. | 910 | 86.4 | 84.1–88.6 |
| 4. Management Support for Patient Safety | 2735 | 75.2 | 73.6–76.8 |
| F1. Facility management provides a work climate that promotes patient safety. | 922 | 82.9 | 80.4–85.3 |
| F8. The actions of facility management show that patient safety is a top priority. | 900 | 80.4 | 77.8–83.0 |
| F9r. Facility management seems interested in patient safety only after an adverse event happens. | 913 | 62.2 | 59.1–65.4 |
| 5. Overall Perceptions of Patient Safety | 3636 | 71.2 | 69.8–72.7 |
| A15. Patient safety is never sacrificed to get more work done. | 901 | 61.2 | 58.0–64.3 |
| A18. Our procedures and systems are good at preventing errors from happening. | 909 | 77.8 | 75.1–80.5 |
| A10r. It is just by chance that more serious mistakes don’t happen around here. | 909 | 70.7 | 67.8–73.7 |
| A17r. We have patient safety problems in this Unit. | 917 | 75.1 | 72.3–77.9 |
| 6. Feedback & Communication About Error | 2711 | 77.5 | 75.9–79.1 |
| C1. We are given feedback about changes put into place based on event reports. | 882 | 68.0 | 65.0–71.1 |
| C3. We are informed about errors that happen in this Unit. | 913 | 78.2 | 75.5–80.9 |
| C5. In this Unit we discuss ways to prevent errors from happening again. | 916 | 85.9 | 83.7–88.2 |
| 7. Communication Openness | 2735 | 50.5 | 48.6–52.4 |
| C2. Staff will freely speak up if they see something that may negatively affect patient care. | 914 | 55.1 | 51.9–58.4 |
| C4. Staff feel free to question the decisions or actions of those with more authority. | 909 | 44.1 | 40.9–47.3 |
| C6r. Staff are afraid to ask questions when something does not seem right. | 912 | 52.19 | 49.0–55.4 |
| 8. Frequency of Events Reported | 2738 | 57.3 | 55.4–59.1 |
| D1. When a mistake is made, but is caught and corrected before affecting the patient, how often is this reported? | 919 | 60.4 | 57.2–63.6 |
| D2. When a mistake is made, but has no potential to harm the patient, how often is this reported? | 913 | 51.9 | 48.7–55.2 |
| D3. When a mistake is made that could harm the patient, but does not, how often is this reported? | 906 | 59.5 | 56.3–62.7 |
| 9. Teamwork Across Units | 3672 | 69.9 | 68.4–71.3 |
| F4. There is good cooperation among facility Units that need to work together. | 919 | 73.8 | 70.9–76.6 |
| F10. Facility Units work well together to provide the best care for patients. | 914 | 81.5 | 79.0–84.0 |
| F2r. Facility Units do not coordinate well with each other. | 918 | 63.7 | 60.6–66.8 |
| F6r. It is often unpleasant to work with staff from other facility Units. | 921 | 60.5 | 57.3–63.6 |
| 10. Staffing3 | 2756 | 37.4 | 35.6–39.2 |
| A2. We have enough staff to handle the workload. | 922 | 54.7 | 51.5–57.9 |
| A5r. Staff in this Unit work longer hours than is best for patient care. | 919 | 16.3 | 13.9–18.7 |
| A14r. We work in “crisis mode” trying to do too much, too quickly. | 915 | 41.1 | 37.9–44.3 |
| 11. Handoffs & Transitions | 3660 | 70.8 | 69.4–72.3 |
| F3r. Things “fall between the cracks” when transferring patients from one Unit to another. | 914 | 74.3 | 71.5–77.1 |
| F5r. Important patient care information is often lost during shift changes. | 913 | 75.6 | 72.8–78.4 |
| F7r. Problems often occur in the exchange of information across facility Units. | 918 | 59.9 | 56.7–63.1 |
| F11r. Shift changes are problematic for patients in this facility. | 915 | 73.6 | 70.7–76.4 |
| 12. Non punitive Response to Errors | 2731 | 53.2 | 51.4–55.1 |
| A8r. Staff feel like their mistakes are held against them. | 914 | 57.2 | 54.0–60.4 |
| A12r. When an event is reported, it feels like the person is being written up, not the problem. | 909 | 50.1 | 46.8–53.3 |
| A16r. Staff worry that mistakes they make are kept in their personnel file. | 908 | 52.4 | 49.2–55.7 |
According to the scale used for each item, positive response means “Agree”/”Strongly Agree” or “Most of the time”/”Always”. For negatively worded (r) questions, positive response means “Strongly Disagree”/”Disagree” or “Never”/”Rarely”.
Composites are highlighted in Bold.
The composite staffing includes 3 items instead of the 4 of the original survey. The item “A7r. We use more agency/temporary staff than is best for patient care.” was excluded as use of agency/temporary staff is not applicable to the facilities in the study
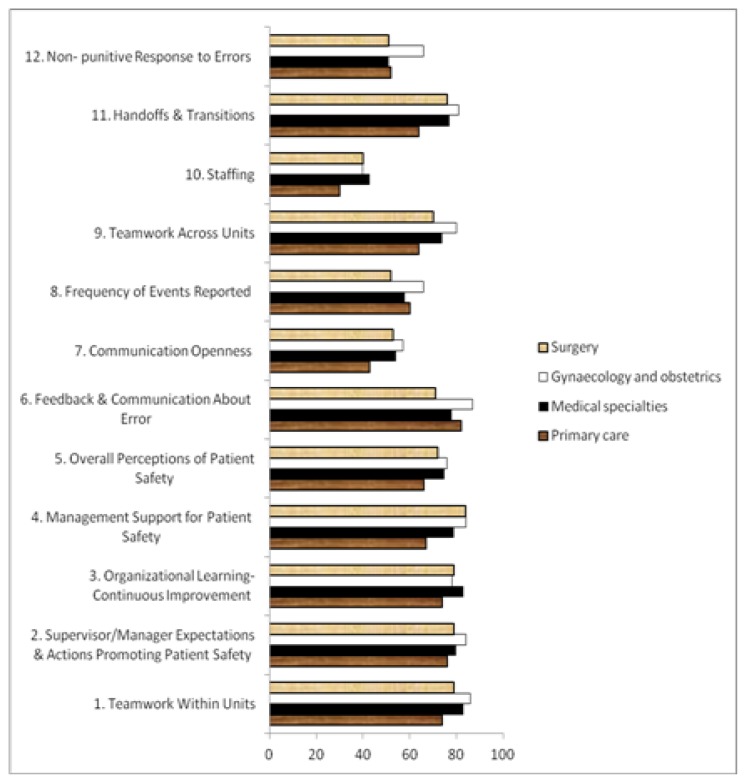
Figure 1 illustrates the composite PPRs in the Republic of Moldova, by main work area. The lowest PPR for each work area was for staffing. The highest PPR among primary care and gynecology and obstetrics staff (82% and 83% respectively) was for feedback and communication about error; among the medical specialties staff it was for organizational learning – continuous improvement (83%), and among surgery staff it was for Management support for patient safety (84%).
Figure 1.
Percentage of positive responses (PPRs) to HSOPSC composites in the Rep. of Moldova, by work area.
Generally, composite PPRs were significantly lower in primary care. Gynecology and obstetrics exhibited significantly higher PPRs than surgery for a series of composites. (i.e. teamwork within units: 86% versus 79%, feedback and communication about error: 87% versus 71%, frequency of events reported: 66% versus 53%, teamwork across units: 80% versus 70%, non-punitive response to errors: 66% versus 51%).
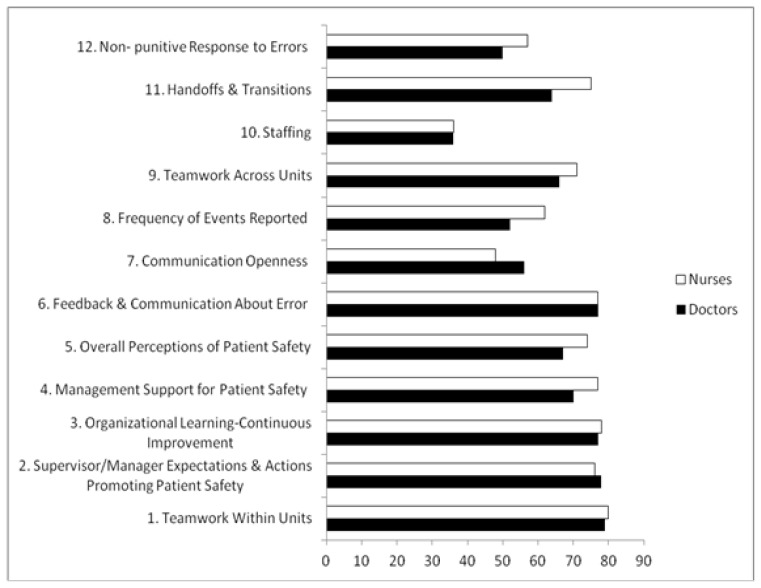
Figure 2 presents composite PPRs in the Republic of Moldova, by main professional groups. Nurses had significantly higher PPRs than doctors for: Management and support for patient safety (77% versus 60%), overall perception of patient safety (74% versus 67%), frequency of events reported (62% versus 52%), handoffs & transitions (75% versus 64%), non-punitive response to errors (57% versus 50%). Doctors had higher PPRs for communication openness (56% versus 48%). No statistically significant differences were found for the other dimensions of patient’s safety culture.
Figure 2.
Percentage of positive responses (PPRs) to HSOPSC composites in the Rep. of Moldova, by profession.
Discussion
In this pilot study, we applied for the first time in the Republic of Moldova the Romanian version of the US AHRQ questionnaire HSOPSC to explore staff perceptions about patient safety in three healthcare settings providing out- and in-patient primary and secondary care. Our results are based on 929 surveys returned (response rate: 95%). Respondents were mainly nurses and doctors, with more than 20 years of work experience.
Patient safety culture aspects such as teamwork, feedback and communication about error, organizational learning - continuous improvement and Management actions for promoting or supporting safety were highly positively scored by the participants.
The most critical aspect perceived by the Moldovan respondents participating in this study was staffing, in line with WHO evidence showing that the number of doctors and nurses is currently much lower in the Republic of Moldova than the European Region average (i.e. 291 versus 322 doctors per 100,000 inhabitants and 608 versus 740 per 100,000 inhabitants for nurses). This issue was present in setting A (public hospital) and C (territorial primary and secondary care association) respectively. In setting B, which was a small modern private clinic, respondents did not perceive staffing as critical. In all settings, the positive score to the Question A5 was extremely low (14%), so staff might have misunderstood this item. Bagnasco et al. [19] reached the same conclusion and suggested that it would be better to say ”Does the staff work more hours than necessary to provide optimal care to the patient?”.
Our study also pointed out the low frequency of reporting adverse events, along with low composite scores attributed by staff to non-punitive response to errors and to communication openness. Available data on the frequency of adverse events, e.g. healthcare-associate infections (HAIs), suggest that they are underestimated and underreported in the Republic of Moldova (e.g. 1.8 to 1,000 among postsurgical patients and 6.7 per 1,000 live births among newborns, which is much lower in comparison with the EU average) [1,20–22]. The main reasons for this are: lack of knowledge of the definition of an adverse event/HAI and the fear of being punished after reporting it [20–22]. Traditionally, HAIs were rarely reported in the communist bloc countries, and reported cases often resulted in administrative sanctions and penalties to healthcare service providers [21]. It is likely that in the healthcare facilities in our study, management style is still based on the ”authoritarian and hierarchical model”, as observed in other countries with different status of democracy with respect to the US (the country of origin of the HSOPSC) [23,24]. According to the type of organization, high scores for Supervisor/Manager expectations & actions promoting patient safety (78%) and Management support for patient safety (75%) might suggest true Management commitment in improving safety as well as respondents reticence in expressing negative opinions about the Management of their institution. This distinction is important. Therefore, qualitative research along with the examination of the psychometric properties of the Romanian translation of the HSOPSC are needed for a better understanding of the extent to which a quantitative tool such as the HSOPSC captures the real staff perceptions in the Republic of Moldova [25]. Resistance to open disclosure and communication represents an important barrier for progress in preventing harm caused by unintentional errors that might occur in complex systems (e.g. the healthcare system) through learning systems.
The overall scores for patient safety culture were lower in primary healthcare/medical specialties units than in general surgery/gynecology and obstetrics, likely because these units have a lower potential for life-threatening medical errors and procedures. As highlighted by other authors [26], we believe that patient safety culture in these settings needs to be further developed in order to avoid unexpected threats to patient care or staff health.
Nurses are the largest workforce in healthcare and spend more time with the patient than doctors. They are an important interface between patient safety and both the patient experience and suboptimal outcomes. Thus, they are likely to show strong awareness with respect to a multitude of patient safety aspects. In our study, nurses scored the majority of patient safety culture aspects higher than doctors, which is consistent with other studies [18,27]. Interestingly, some authors reported significantly less positive opinions in nurses than in doctors for specific composites (communication, reporting adverse events, hospital handoffs and transitions, perception of the patient safety grade and managerial actions promoting safety) but the overall score was still higher for nurses [16]. In line with Brborović and al. [15], we believe that increasing the response rate of doctors to the survey might be necessary for a more authentic comparison to be made between doctors and nurses.
Across the other CEE countries that applied the HSOPSC, the Republic of Moldova and Romania exhibited generally higher scores than Croatia, Slovenia and Slovakia, for most patient safety dimensions. Most of these countries shared a similar pattern, according to which staffing had a low score and teamwork within units had a high score [14–16,18]. It could be hypothesized that personnel shortage contributes to develop better teamwork. Communication openness, non-punitive response to errors and frequency of the reported events also received low scores with respect to other patient safety culture aspects in the CEE countries. Slovenia was an exception: it exhibited unexpectedly high score for the frequency of the reported events, likely because of major sensitivity to this issue by the staff. In recent years, Slovenia, Croatia and Slovakia have started implementing a new reporting system for incidents, each country using a different method: nationwide incident reporting system (Slovenia), full-scale operation at launch (Slovakia), step by step implementation (Croatia). In Slovenia and Slovakia, the reporting is voluntary for the healthcare professionals and mandatory for the healthcare organizations; it is not accessible to patients and it is not regulated by law. In Croatia, the reporting is mandatory for healthcare professionals and voluntary for patients and it is partially regulated by law [28]. We are not aware of similar initiatives in the Republic of Moldova or Romania. These two countries, which are similar linguistically and culturally, should start with a thorough revision of their existing mandatory reporting system of HAIs. The notable inefficiency of this system is mainly due to dominance of continuing reliance on a blame culture (focusing on complaints, negligence, liability and promotion of patient rights rather than safety culture, risk management or system improvement) [22,29]. According to the study of Maciek et al. [29], international cooperation is needed to develop and implement patient safety initiatives in CEE countries, along with the stakeholders’ engagement in establishing priorities for safe practices, which should be addressed through interdisciplinary teamwork with strong leadership and adequate financial resourcing [29].
Our study has several limitations. Firstly, it is based on a census sample from voluntary facilities and therefore results cannot be generalized. Secondly, this is a snapshot of staff perceptions obtained through a self assessment tool and therefore “socially desirable responses” cannot be excluded nor quantified. Thirdly, our findings cannot be supported by more objective data about patient safety, because systematic review of medical records (or other alternative reliable methodologies proposed for countries with limited resources) [30] nor spontaneous incident reporting are in place in the facilities participating in the study. Fourthly, the psychometric performance of the Romanian version of the HSOPSC has only been checked on Romanian staff [31].
However, since little is known about patient safety culture in countries with limited resources, and research in this area is lacking in the Republic of Moldova, we believe that this study is important. It is the first application in this country of the US HSOPSC, widely diffused at international level and strongly recommended by the EUNetPAS in Europe [8]. The participants in this pilot-study cover different typologies of institutions (public hospital, private clinic, territorial primary care organization) and consequently a wide variety of healthcare professionals, working with both inpatients and outpatients. The response rate was very high.
Conclusion
This baseline pilot study experimenting the Romanian version of the HSOPSC in the Republic of Moldova within 929 staff in three healthcare facilities indicates that there is room for improvement with respect to staffing, communication openness, non-punitive response to errors and frequency of the events reported. Future research should check if psychometrics of the Romanian version applied to Moldovan staff are acceptable. Poor validity would require additional qualitative approaches (e.g.: observation, focus groups, interviews) in order to define more accurately which are the aspects of patient safety culture in the Republic of Moldova and how to measure them. On the other hand, sufficiently sound psychometric properties would support the need to expand the application of the US HSOPSC to other facilities in the country. International comparisons are interesting, but they should be interpreted very cautiously.
This study has several implications for research. In the Republic of Moldova, it is a first insight in the staff views about patient safety using a multidimensional international assessment tool. The results could be used as a help to interpret results of research on patient outcomes, since differences in the effective patient safety between units/healthcare settings might be associated with differences in the perception, attitude, and behavior of the staff related to patient safety. Thanks to a series of internationally funded and guided projects constantly implemented in recent years in the Republic of Moldova, this country is making continuous progress in improving available standards of care (e.g. reduction of hospital vulnerability to natural disasters, reduction of surgical hazards/complications following sustained use of check-lists, etc.) [32–33]. The questionnaire might need further refinement, but after psychometric validation, it could be used to examine trends in patient safety culture change over time and to evaluate the cultural impact of patient safety interventions. Our study is certainly a crucial starting point for research in this field in this country and increases available data on the application of the HSOPSC in limited resource countries.
The study has also important implications for practice. It explores the current condition of patient safety culture, identifying strengths and areas for improvement. Therefore, it raises awareness about patient safety among staff and helps driving up targeted interventions aiming at improving safety culture in the participating settings. Subsequent inter-unit and inter-organizational nationwide comparisons could stimulate the exchange of evidence-based best practices for intervention to improve safety culture. The patient safety culture evaluation could also be envisaged as a requirement for the hospital accreditation process and/or as a basis to draw indicators for accountability and public diffusion [10].
Acknowledgments
The authors thank the Management of the three facilities participating in the study and all of the staff who responded to the questionnaire. The authors are grateful to the Latin Association for Analysis of Healthcare Systems (www.alass.org) for their patronage for the IRIS Project.
References
- 1.Institute of Health and Medical Social Assistance. Public Health Monitor Policies on Patient Safety 2011. (Electronic bulletin No. 4). [Google Scholar]
- 2.European health for all database (HFA-DB) WHO/Europe July 2016. Available from: http://data.euro.who.int/hfadb/
- 3.World Bank Group. Reducerea sărăciei şi prosperitatea partajată în Moldova: Progrese şi perspective. Report No. 105722-MD. Available from: http://documents.worldbank.org/curated/en/715861467989513808/pdf/105722-WP-P151472-PUBLIC-ROMANIAN-Moldova-Poverty-Assessment-2016.pdf.
- 4.Aveling EL, Kayonga Y, Nega A, Dixon-Woods M. Why is patient safety so hard in low-income countries? A qualitative study of healthcare workers’ views in two African hospitals. Global Health. 2015 Feb 25;11:6. doi: 10.1186/s12992-015-0096-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pîsla M, Domente S, Chetraru L, Ostaficiuc R. Evaluarea siguranţei spitalelor din Republica Moldova: Raport sumar. Chisinau. 2010 [Google Scholar]
- 6.Palese A, Cristea E, Mesaglio M, Stempovscaia E. Italian-Moldovan international nurse migration: rendering visible the loss of human capital. Int Nurs Rev. 2010;57(1):64–69. doi: 10.1111/j.1466-7657.2009.00785.x. [DOI] [PubMed] [Google Scholar]
- 7.Agency for Healthcare Research and Quality. Surveys on Patient Safety Culture. Available from: http://www.ahrq.gov/professionals/quality-patient-safety/patientsafetyculture/pscintusers.html.
- 8.European Network for Patient Safety – EUNetPaS. Use of Patient Safety Culture Instruments and Recommendations. Denmark: 2010. Available from: http://www.pasq.eu/DesktopModules/BlinkQuestionnaires/QFiles/448_WP4_REPORT%20%20Use%20of%20%20PSCI%20and%20recommandations%20-%20March%20%202010.pdf. [Google Scholar]
- 9.Waterson P, Griffiths P, Stride C, Murphy J, Hignett S. Psychometric properties of the Hospital Survey on Patient Safety Culture: findings from the UK. Qual Saf Health Care. 2010;19(5):e2. doi: 10.1136/qshc.2008.031625. [DOI] [PubMed] [Google Scholar]
- 10.Occelli P, Quenon JL, Kret M, Domecq S, Delaperche F, Claverie O, et al. Validation of the French version of the Hospital Survey on Patient Safety Culture questionnaire. Int J Qual Health Care. 2013;25(4):459–468. doi: 10.1093/intqhc/mzt047. [DOI] [PubMed] [Google Scholar]
- 11.Smits M, Christiaans-Dingelhoff I, Wagner C, Wal Gv, Groenewegen PP. The psychometric properties of the ‘Hospital Survey on Patient Safety Culture’ in Dutch hospitals. BMC Health Serv Res. 2008 Nov 7;8:230. doi: 10.1186/1472-6963-8-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vlayen A, Hellings J, Claes N, Abdou EA, Schrooten W. Measuring safety culture in belgian psychiatric hospitals: validation of the Dutch and French translations of the hospital survey on patient safety culture. J Psychiatr Pract. 2015;21(2):124–139. doi: 10.1097/01.pra.0000462605.17725.48. [DOI] [PubMed] [Google Scholar]
- 13.Hammer A, Ernstmann N, Ommen O, Wirtz M, Manser T, Pfeiffer Y, et al. Psychometric properties of the Hospital Survey on Patient Safety Culture for hospital management (HSOPS_M) BMC Health Serv Research. 2011 Jul 11;11:165. doi: 10.1186/1472-6963-11-165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Robida A. Hospital Survey on Patient Safety Culture in Slovenia: a psychometric evaluation. Int J Qual Health Care. 2013;25(4):469–475. doi: 10.1093/intqhc/mzt040. [DOI] [PubMed] [Google Scholar]
- 15.Brborović H, Šklebar I, Brborović O, Brumen V, Mustajbegović J. Development of a Croatian version of the US Hospital Survey on Patient Safety Culture questionnaire: dimensionality and psychometric properties. Postgrad Med J. 2014;90:125–132. doi: 10.1136/postgradmedj-2013-131814. [DOI] [PubMed] [Google Scholar]
- 16.Mikušová V, Rusnáková V, Naďová K, Boroňová J, Beťková M. Patient Safety Assessment in Slovak Hospitals. International Journal of Collaborative Research on Internal Medicine & Public Health. 2012;4(6):1236–1244. [Google Scholar]
- 17.Brajshori N, Behrens J. Translation, Cultural Adaptation and Validation of Hospital Survey on Patient Safety Culture in Kosovo. Open Journal of Nursing. 2016;6:483–490. [Google Scholar]
- 18.Tereanu C, Ghelase MS, Sampietro G, Furtunescu FL, Dragoescu A, Molnar A, et al. Measuring Patient Safety Culture in Romania Using the Hospital Survey on Patient Safety Culture (HSOPSC) Current Health Science Journal. 2017;43(1) doi: 10.12865/CHSJ.43.01.0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bagnasco A, Tibaldi L, Chirone P, Chiaranda C, Panzone MS, Tangolo D, et al. Patient safety culture: an Italian experience. J Clin Nurs. 2011;20:1188–1195. doi: 10.1111/j.1365-2702.2010.03377.x. [DOI] [PubMed] [Google Scholar]
- 20.Colegiul Ministerului Sanatatii. Notă informativă privind calitatea serviciilor medicale în contextul rezultatelor evaluării şi acreditării instituţiilor medico-sanitare [Ministry of Health College. Available from: http://www.ms.gov.md/sites/default/files/6811-nota20colegiu2020-2001.11.101_0.pdf.
- 21.Ider BE, Adams J, Morton A, Whitby M, Clements A. Infection control systems in transition: the challenges for post-Soviet Bloc countries. J Hosp Infect. 2012;80:277–287. doi: 10.1016/j.jhin.2012.01.012. [DOI] [PubMed] [Google Scholar]
- 22.Shaw CD. Quality and safety of health care in the Republic of Moldova. WHO Regional Office for Europe. Republic of Moldova. Health Policy 2015. (Paper Series No. 19). Available from: http://www.euro.who.int/__data/assets/pdf_file/0007/281869/Quality-safety-of-health-care-in-MDA.pdf?ua=1.
- 23.Šklebar I, Mustajbegović J, Šklebar D, Cesarik M, Milošević M, Brborović H, et al. How To Improve Patient Safety Culture In Croatian Hospitals? Acta Clin Croat. 2016;55:370–380. doi: 10.20471/acc.2016.55.03.04. [DOI] [PubMed] [Google Scholar]
- 24.Chen IC, Li HH. Measuring patient safety culture in Taiwan using the Hospital Survey on Patient Safety Culture (HSOPSC) BMC Health Serv Res. 2010 Jun 7;10:152. doi: 10.1186/1472-6963-10-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pumar-Méndez MJ, Attree M, Wakefield A. Methodological aspects in the assessment of safety culture in the hospital setting: a review of the literature. Nurse Educ Today. 2014;34:162–70. doi: 10.1016/j.nedt.2013.08.008. [DOI] [PubMed] [Google Scholar]
- 26.Bodur S, Filiz E. A survey on patient safety culture in primary healthcare services in Turkey. Int J Qual Health Care. 2009;21(5):348–355. doi: 10.1093/intqhc/mzp035. [DOI] [PubMed] [Google Scholar]
- 27.Pronovost PJ, Weast B, Holzmueller CG, Rosenstein BJ, Kidwell RP, Haller KB, et al. Evaluation of the culture of safety: survey of clinicians and managers in an academic medical center. Qual Saf Health Care. 2003;12:405–410. doi: 10.1136/qhc.12.6.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.European Commission. Patient Safety and Quality of Care working group Key findings and recommendations on Reporting and learning systems for patient safety incidents across Europe. 2014. Available from: http://ec.europa.eu/health/patient_safety/policy/index_en.htm.
- 29.Godycki-Cwirko M, Esmail A, Dovey S, Wensing M, Parker D, Kowalczyk A, et al. Patient safety initiatives in Central and Eastern Europe: A mixed methods approach by the LINNEAUS collaboration on patient safety in primary care. Eur J Gen Pract. 2015;21(Suppl):62–68. doi: 10.3109/13814788.2015.1043727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.World Health Organization. Assessing and tackling patient harm: a methodological guide for data-poor hospitals. WHO Press, World Health Organization; Geneva, Switzerland: 2010. [Google Scholar]
- 31.Tereanu C, Smith SA, Ghelase MS, Sampietro G, Molnar A, Furtunescu FL, et al. Proprietà psicometriche del Questionario statunitense sulla cultura della sicurezza dei pazienti HSOPSC applicato agli ospedali rumeni: risultati del progetto internazionale IRIDE, oral communication. Annual Congress of ALASS; 7–9th September 2017; Liège (Belgium). [Google Scholar]
- 32.WHO Europe. New assessment of all public hospitals in the Republic of Moldova shows improved hospital resilience to natural disasters. Available from: http://www.euro.who.int/en/countries/republic-of-moldova/news/news/2016/11/new-assessment-of-all-public-hospitals-in-the-republic-of-moldova-shows-improved-hospital-resilience-to-natural-disasters.
- 33.Kim RY, Kwakye G, Kwok AC, Baltaga R, Ciobanu G, Merry AF, et al. Sustainability and long-term effectiveness of the WHO surgical safety checklist combined with pulse oximetry in a resource-limited setting: two-year update from Moldova. JAMA Surg. 2015;150(5):473–479. doi: 10.1001/jamasurg.2014.3848. [DOI] [PubMed] [Google Scholar]