Defects in DNA repair genes are now understood to be common in patients with metastatic castration-resistant prostate cancer (mCRPC) according to studies sequencing tumor samples [1] and the germline [2]. In a proof-of-concept study to demonstrate that such defects could be exploited therapeutically, patients with mCRPC with mutations in DNA repair genes had responses when treated with olaparib [3]. The mechanism by which PARP inhibition leads to cell death, is in part via induction of DNA double-strand breaks, which go unrepaired in cells harboring defects in the homologous recombination repair pathway [4].
We have previously reported on the therapeutic potential of high-dose testosterone in men with mCRPC [5]. Preclinical studies demonstrated that rapid cycling between high and low levels of androgen, termed bipolar androgen therapy (BAT), could disrupt DNA relicensing and produce DNA double-strand breaks in CRPC cells. Given the emerging data on DNA repair defects in prostate cancer and the mechanism of BAT, we postulated that men with such defects may be particularly susceptible to BAT. Here we report a case of an exceptional responder to BAT and the underlying tumor mutations that possibly explain his susceptibility to the therapy.
The patient is a 70-yr-old man with mCRPC. He initially presented with Gleason 9 disease for which he underwent radical prostatectomy followed by salvage radiation therapy. He was initiated on hormonal therapy 2 yr later because of rising prostate-specific antigen (PSA). He received bicalutamide, nilutamide, ketoconazole, and enzalutamide sequentially over 3 yr (Fig. 1). At the time of progression on enzalutamide, computed tomography (CT) imaging showed enlarging node-only disease (target lesion was 3.3 cm in the iliac node). He was enrolled in a clinical trial and received testosterone cypionate 400 mg intramuscularly every 28 d and continuous luteinizing hormone–releasing hormone agonist therapy. After two cycles, his PSA became unmeasurable and has remained so for 20 cycles of ongoing BAT (Fig. 1). He achieved a radiographic complete response after six cycles. At this point, the patient continues to have no evidence of disease on bone scan or CT scan, nondetectable PSA, and testosterone in the non-castrate range.
Fig. 1.
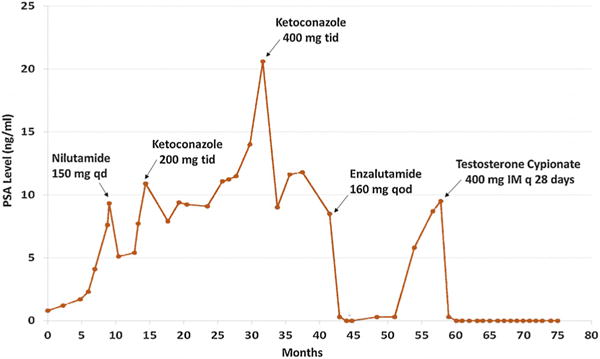
Prostate-specific antigen (PSA) levels over time in response to the hormonal therapies indicated.
To test whether this patient’s tumor had underlying DNA repair defects, we sequenced his archived primary prostate cancer tissue using a 203-gene panel (Personal Genome Diagnostics, Baltimore, MD, USA). The tumor was found to have an inactivating S1982Rfs*22 frame shift mutation in BRCA2 and an L2307F missense mutation in ATM. Both of these mutations were present in the germline.
The results for this patient, who is experiencing a durable complete response to BAT, support the hypothesis that patients harboring mutations in DNA repair pathway genes may be particularly sensitive to BAT. Further testing of BAT in patients with DNA repair deficits or testing of BAT in combination with agents targeting the DNA repair pathway is warranted.
Footnotes
Conflicts of interest: The authors have nothing to disclose.
References
- 1.Robinson D, Van Allen EM, Wu YM, et al. Integrative clinical genomics of advanced prostate cancer. Cell. 2015;161:1215–28. doi: 10.1016/j.cell.2015.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pritchard CC, Matteo J, Walsh MF, et al. Inherited DNA-repair gene mutations in men with metastatic prostate cancer. N Engl J Med. 2016;375:443–53. doi: 10.1056/NEJMoa1603144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mateo J, Carreira S, Sandhu S, et al. DNA-repair defects and olaparib in metastatic prostate cancer. N Engl J Med. 2015;373:1697–708. doi: 10.1056/NEJMoa1506859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Farmer H, McCabe N, Lord CJ, et al. Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature. 2005;434:917–21. doi: 10.1038/nature03445. [DOI] [PubMed] [Google Scholar]
- 5.Schweizer MT, Antonarakis ES, Wang H, et al. Effect of bipolar androgen therapy for asymptomatic men with castration-resistant prostate cancer: results from a pilot clinical study. Sci Transl Med. 2015;7:269ra2. doi: 10.1126/scitranslmed.3010563. [DOI] [PMC free article] [PubMed] [Google Scholar]


