Abstract
Yttria-stabilized polycrystalline zirconia ceramics have greatly advanced over the past few years. High-translucent zirconia is a newly introduced ceramic which enables high strength and aesthetics, and has significantly increased the clinical indications of monolithic zirconia restorations. Thus, the purpose of this case report was to evaluate the performance of ultra-thin monolithic zirconia veneers adhesively luted to enamel surfaces after minimally invasive preparations, in addition to presenting a clinical protocol of zirconia surface treatment in order to promote bonding effectiveness to resin cement. This type of restoration presented very acceptable aesthetic results and decreased the risk of fracturing the veneer during try-in and clinical use. The results were still satisfactory after one-year follow-up. However, randomized prospective controlled clinical trials are required to determine the long-term clinical durability of this treatment.
Keywords: Zirconia, CAD/CAM, translucency, surface treatment, bond strength
Introduction
Porcelain veneers are a conservative and highly aesthetic treatment, that also presents high predictability and good clinical performance in the long term1. With technological improvement and the evolution of dental restorative materials, it is currently possible to develop/produce ultra-thin veneers with thicknesses of 0.1–0.3mm, adhesively cemented on the tooth surface with minimal or no preparation, to modify color, shape and/or positioning of the teeth2,3.
Several ceramic materials are currently indicated for veneers: lithium disilicate, feldspathic ceramic, feldspathic reinforced with leucite, fluorapatite and lithium silicate reinforced with zirconia4,5,6,7. All these ceramics exhibit high translucency characteristics due to the high content of glassy matrix in their composition, thus providing highly satisfactory aesthetics, in addition to excellent adhesion to resin cement through the conditioning with hydrofluoric acid (4–10%) followed by silanization5. For these reasons, these ceramics have also been chosen for manufacturing ultra-thin veneers 8.
On the other hand, high crystalline content ceramics, such as tetragonal zirconia partially stabilized by yttria (Y-TZP), were originally considered only for the manufacturing of frameworks of crowns and fixed prostheses due to their high fracture resistance and ability to mask the dark substrate9. However, in recent years, zirconia ceramics have undergone many changes in its microstructure and composition10 to increase their translucency without significantly losing their fracture resistance11, thereby expanding their clinical indication. Thus, translucent zirconia has been considered as an aesthetic material, being indications for manufacturing crowns and anterior and posterior monolithic fixed prostheses, including veneers and ultra-thin veneers 12. Its main difficulty are in situations of little mechanical retention of preparation since polycrystalline zirconia is chemically inert and cannot be etched by hydrofluoric acid (4–10%), which implies a less effective adhesion when compared to silica-based ceramics (acid-sensitive)13.
Few clinical studies using monolithic zirconia prostheses have been reported in the literature. Rinke et al.14 evaluated the clinical performance of posterior monolithic crowns and concluded that good aesthetic results in the posterior region were achieved, even in cases of minimal occlusal space. Stober at al.15, in evaluating the wear of the enamel caused by monolithic translucent zirconia crowns in molars during six months of follow-up, concluded that the enamel wear of the antagonist tooth was equal to that caused by other ceramics.
In vitro studies on veneers have reported a higher resistance to fracture of zirconia compared to lithium disilicate and feldspathic veneers16, which can be regarded as a great advantage of this material, as the proof and cementation stages of ultra-thin veneers become much less critical compared to conventional glass-ceramics. However, the same authors also found that there is a possibility of zirconia veneers debonding due to less effective adhesion to resin cement16.
In order to optimize the adhesion between zirconia and cement, various surface treatments have been proposed: sandblasting with aluminum oxide17, tribochemical silica coating followed by silanization18, nanostructured alumina coating 19, resin cement containing 10-methacryloxydecyl dihydrogen phosphate monomer (MDP)20, universal primers also containing methacrylate monomers21, plasma processing, silica infiltration by sol-gel method22, feldspathic glass infiltration23, selective infiltration-etching technique24, glaze-on technique25, and heating silanes26, among others. Therefore, the treatment of zirconia surfaces has been the subject of much scientific research27,28,29,30,17. Depending on the type of treatment of the zirconia surface, it is possible to significantly improve their adherence to resin cement16,17,21,23. However, clinical studies with zirconia veneers and ultra-thin zirconia veneers have not yet been published.
Thus, based on the promising results of surface treatments in zirconia and on the aesthetic evolution of this material, the aim of this case report was to describe, through a clinical case, the manufacturing of ultra-thin veneers using translucent zirconia, as well as to discuss relevant aspects for success in this type of treatment and report a one-year follow-up of this clinical rehabilitation.
Case Report
A female patient, A.T.T.S., 25 years of age, sought specialized dental care reporting small, yellowing upper front teeth with diastema as her main complaint. Upon clinical examination, the presence of a disharmonious smile with proclined lateral incisors, unfavorable dental proportions, diastema between lateral incisors and upper central, in addition to inadequate gingival contouring and zenith (Figures 1a–b and 2). The occlusal contacts and the eccentric movements were evaluated by mounting of study models using the facial arch in a semi-adjustable articulator. After digitally planning the smile, it was observed the need for correcting the contouring and gingival zenith, increasing the incisal edges of the lateral incisors and vertically increasing her central incisors towards the cervical direction, setting a tooth ratio of 80% (the final width to length ratio of the centrals was 9/11.2 millimeters, approximately 80%). Surgery was then recommended for crown enlargement of teeth 7 to 10 (universal numbering system) (Figure 3). After 60 days, whitening therapy was initiated with the use of 16% carbamide peroxide (Whiteness Perfect/FGM, Joinville, SC, Brazil) for 4 weeks.
Figures 1a–b.
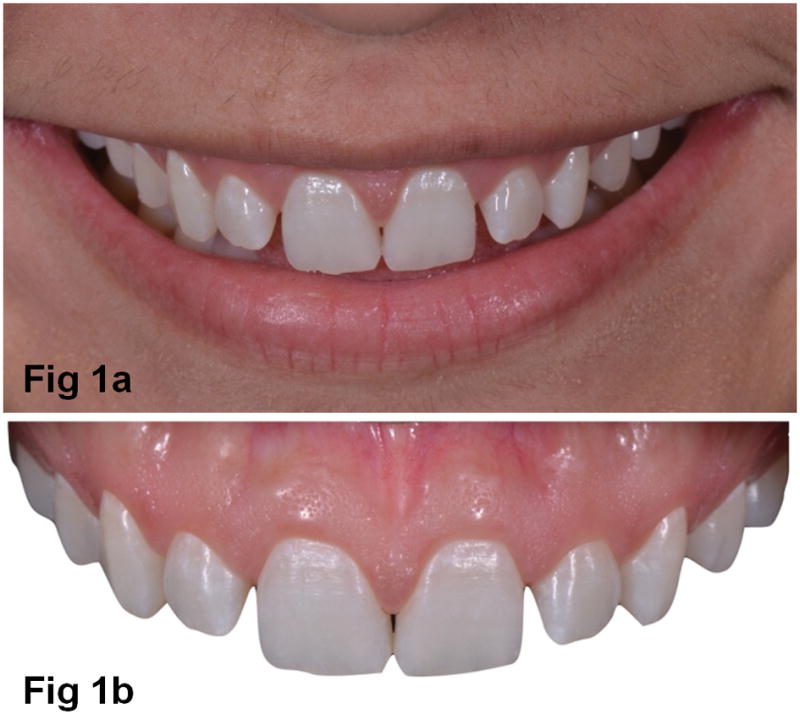
a) Initial apearance of patient smile and with b) unfavorable dental proportions and diastema between lateral incisors and upper central.
Figure 2.

Intraoral view of teeth in occlusion. Patient with stable occlusion.
Figure 3.
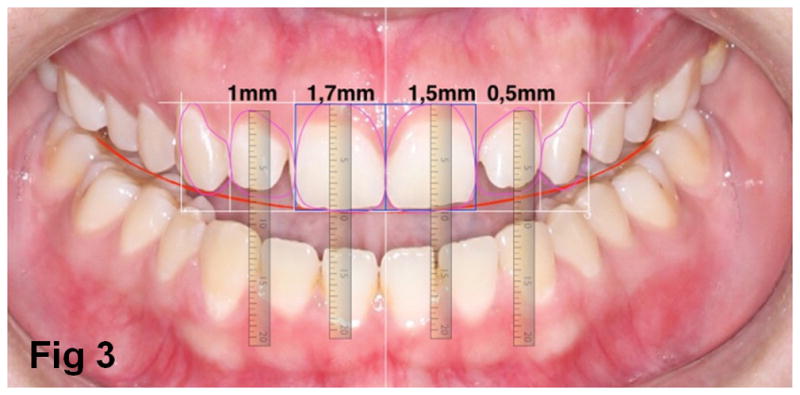
Digital smile analysis and planning for periodontal surgery before restorative procedures.
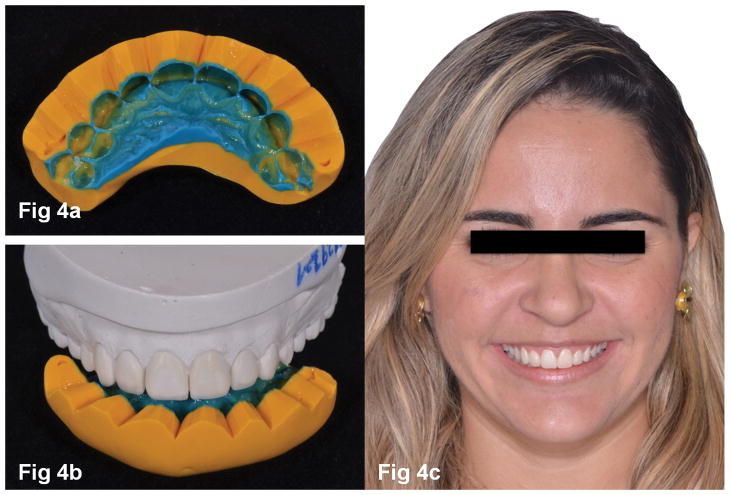
In the next session, an impression with vinyl polysiloxane/silicone was made (Express XT [commercially available in the United States as Express VPS] 3M ESPE, St Paul/MN, USA) to prepare stone models, a diagnostic wax-up, and mock-up (Systemp/Ivoclar Vivadent, Schaan, Liechtenstein) of teeth 6 to 11, according to the digital smile design (Figures 4a–c). In this stage, the occlusal contacts and the eccentric movements were evaluated again, clinically in the patient’s mouth, with the assistance of articulating metallic film (Arti-fol/12 microns/Bausch, Germany). There was no need for any mock-up adjustment. Next, minimally invasive preparations were performed in teeth 6 to 11. A medium grit diamond bur with rounded edge was used on the buccal surface of the teeth to remove a uniform thickness of 0.3 mm. Approximately 0.6mm of the buccal surface of teeth 7 and 10 was removed because they were slightly proclined.
Figures 4a–c.
a) Silicone index for mock-up, b) wax model and c) aspect of the patient after mock-up.
In order to guide all steps of teeth preparation, an index was made with a condensation silicon (Zetaplus/Zhermack, São Paulo, São Paulo, Brazil) (Figures 5a–b). All angles were rounded and the cervical finish line in tilted chamfer was continuous, defined, and clear. The preparations were finished and polished with fine diamond burs, followed by multilaminated burs (Komet, Lemgo, Germany) and an Arkansas polisher (Komet, Lemgo, Germany) with the aid of a multiplier contra-angle (Sirona, Bensheim, Germany). In the same session, an impression of the prepared veneers was taken with addition silicone (Express XT [commercially available in the United States as Express VPS] 3M ESPE, St Paul/MN, USA) and sent to a dental technician to manufacture the restorations in a prosthetic laboratory. Because the preparations were minimally invasive, there was no need to manufacture temporary veneers (Figure 6).
Figures 5a–b.
Index positioned on the teeth before preparations: a) buccal and b) incisal view.
Figure 6.

Clinical aspect after final preparation of the anterior teeth.
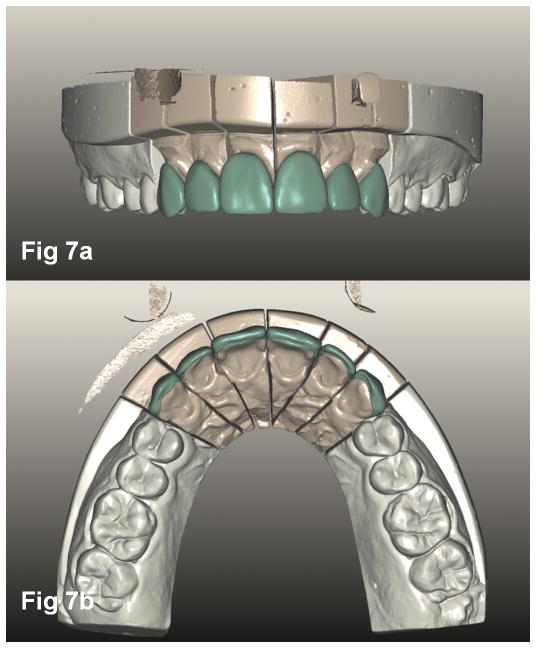
The stone models were scanned and the ultra-thin veneers were fabricated with monolithic translucent zirconia (Prettau Anterior, Zirkonzahn, Gais, Switzerland) (Figures 7a–b) and milled in a Zirkonzahn CAD/CAM system (Gais, Switzerland). The veneers were characterized in the following way: before sintering, polishing with rubber tips followed by stained and after sintering, new polishing and glaze. No veneering ceramics were applied.
Figures 7a–b.
3D images of the veneers from 13 to 23 on the scanned model of the prepared teeth: a) buccal and b) incisal view
After dry testing to check the marginal fit, the resin cement shade was selected using try-in pastes (Variolink Veneer Try-In, Ivoclar Vivadent, Schaan, Liechtenstein). It was possible to observe that the color was significantly affected by the shade of the try-in paste (Figure 8). Next, the veneers were washed, thoroughly dried, and the intaglio surfaces of the zirconia veneers and the tooth surfaces were treated as described below.
Figure 8.

Resin cement color test of ceramic veneers with Try-in pastes (Variolink Veneer, Ivoclar vivadent) of medium value 0 (left) and low value −3 (right). The cement of medium value 0 was selected.
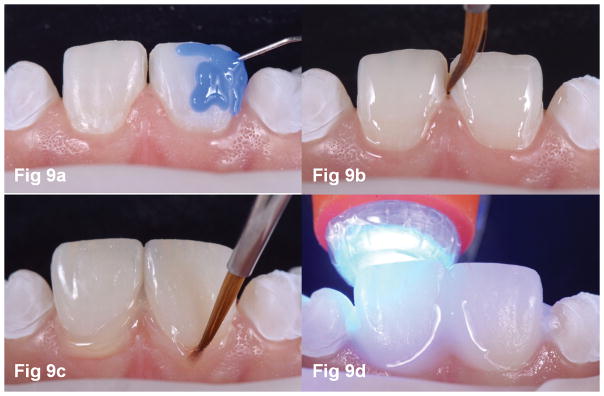
Prophylaxis was performed on the tooth surfaces with pumice and water, and then they were washed and thoroughly dried. These surfaces were then etched with 35% phosphoric acid (Ultra-Etch/Ultradent) for 20 seconds, rinsed in running water, thoroughly dried and treated with an adhesive system (Excite F/Ivoclar Vivadent). The intaglio surfaces of the veneers were abraded with particles of aluminum oxide coated with silica (CoJet, 3M ESPE, Seefeld, Germany) for 20s (2.8bar, 10mm standoff distance), and dried. Silane was then applied (Monobond Plus/Ivoclar Vivadent), and left to dry for 2 min before the application of an adhesive system (Excite F/Ivoclar Vivadent) without curing.
Light-cure resin cement Variolink Veneer of “0” medium value (Ivoclar Vivadent, Schaan, Liechtenstein) was inserted into the ceramic veneers, which were placed in their respective abutments. The excess resin cement was removed with a brush and floss, followed by light-curing for 40 seconds on each veneer surface (Radii Cal, SDI Limited, Victoria, Australia; 1000 mW/cm2). The Radii light intensity was confirmed by a radiometer (Kondortech-Kondentech, São Paulo, Brazil). Next, glycerin gel (Liquid strip, Ivoclar Vivadent, Schaan, Liechtenstein) was applied to the cervical and incisal regions of veneers and another curing cycle was performed on each face (Figures 9a–d). Additional excess cement after curing was removed with a #12-scalpel blade. The clinical appearance of the veneers after luting and one year follow-up can be seen in Figures 10a–b and Figures 11a–b, respectively. There was no need for any occlusal adjustment in the ultra-thin zirconia veneers. Moreover, no protective splint was needed since the patient had no clinical signs and symptoms of bruxism.
Figures 9a–d.
Teeth surface treatment - a) Etchingwith 35% phosphoric acid/15s; b) Application the adhesive on the the tooth surface; c) Removal of excess cement with a thin brush and dental floss; d) Cement photopolymerization with glycerine gel application on the adhesive interface.
Figures 10a–b.

a) Final intraoral view in oclusion; b) Close-up view of the central incisor characterization.
Figures 11a–b.

Final a) smile and b) facial aspect after one year follow-up.
Discussion
In the present clinical study, ultra-thin veneers of monolithic cubic ultra-translucent zirconia were manufactured (Prettau Anterior, Zirkonzahn). This type of zirconia has recently been developed to provide adequate aesthetic and mechanical properties for all-ceramic restorations for both anterior and posterior teeth31.
Several types of zirconia have been most often used in clinical dentistry, such as: traditional tetragonal (opaque) zirconia, with a strength range from 900 to 1200 MPa; high-translucent (HT) zirconia (900 to 1200 MPa) and cubic ultra-translucent (UT) zirconia (500 to 800 MPa)31. This last generation of zirconia has excellent optical features compared to the other two types of zirconia described previously, and therefore we chose it for this clinical study.
In order to achieve adequate translucency, the microstructure of zirconia was modified. It is known that zirconia can exist in three crystallographic forms depending on the temperature at ambient pressure: monoclinic, tetragonal and cubic phases32. In conventional zirconia, 0.5–1.0% of its weight is alumina and 3–6% is yttrium oxide. On the other hand, translucent zirconia has 0.11 to 0.26% of alumina33 and a yttria concentration close to 12%34. Alumina acts as light scattering centers in zirconia due to its different refractive index, reducing the translucency of zirconia33. Furthermore, the amount of zirconia in the tetragonal phase was reduced and a larger amount of cubic zirconia was incorporated, thus enabling a more uniform transmission of light through zirconia9. Factors such as porosity35 and grain size36 also affect the translucency of zirconia. It is evident that zirconia is less translucent than glass ceramics and the translucency decreased more slowly with material thickness37. However, high translucency can be observed for thinner translucent zirconia, specifically about 0.3mm38, which can be confirmed by the pleasant appearance achieved in this clinical case where 0.3mm of translucent zirconia veneers were used.
Few studies on zirconia veneers have been reported15,39, and none of them used translucent zirconia. Alghazzawi et al.39 evaluated the influence of cement color on the final color of ceramic veneers and observed that conventional zirconia was neither influenced by the color of the resin cement nor by the color of the substrate, even at a minimum thickness. Currently, it is possible to manufacture veneers/ultra-thin veneers made entirely from translucent zirconia.40 According to our observations and contrary to what was found for conventional zirconia, there was an influence of cement shade on the final color of the veneers, during the selection of cement with the try-in test pastes.
Regarding the mechanical properties of translucent zirconia, the zirconia used in this clinical case exhibits a flexural strength of 670 MPa, according to the manufacturer’s data sheet. This high-strength ultra-translucent zirconia offers great advantages over feldspathic ceramics or lithium disilicate ultra-thin veneers, considering that these restorations are difficult to manipulate before cementation due to their brittleness, which may lead to fracture during the try-in stage.
Unarguably, the greatest difficulty in performing a treatment with zirconia veneers lies in its low adherence to resin cement compared to the ceramics that can be conditioned by hydrofluoric acid (4–10%) followed by silanization12. The loss of retention (debonding) of zirconia restorations has been reported by clinical studies41. For this reason, many surface treatments have been proposed to modify the surface of zirconia and optimize adhesion to resin cements 16,17,21,23,42,26. Among these treatments, silica coating has presented some of the best bonding results.
Tribochemical silica coating process (Cojet and Rocatec, 3M ESPE, Seefeld, Germany) consists of air-abrasion of the zirconia surface with alumina particles coated by silica, which promotes adhesion between the 3-methacryloxypropyltrimethoxysilane (MPS) silane coupling agent and the silica adhered on the zirconia surface due to the impact16. The silicatization associated with a 10-MDP primer seems to be the most common form of surface treatment to provide long-lasting bonding to zirconia17,26. The phosphate ester groups in this silane bond directly to the surface oxides of zirconia and the methacrylate group makes covalent bonds with the resin matrix of the cement43. Therefore, in the present clinical case, the monolithic zirconia veneers were air-abraded with 30 μm alumina coated by silica (Rocatec Soft, 3M ESPE, Seefeld, Germany), followed by 10-MDP silane agent. We know that the one-year follow-up is not enough time to validate this type of treatment, but up until the writing of this article, none of the veneers had debonded.
However, further in vitro and long-term clinical trials should be conducted to predict the clinical performance of high-translucent monolithic zirconia veneers.
Conclusion
Based on the clinical case presented herein and scientific evidence, we can conclude that the use of translucent zirconia ultra-thin veneers provides satisfactory aesthetics; however, further longitudinal studies are necessary to consolidate this type of treatment.
Clinical Relevance.
Tetragonal zirconia stabilized by yttria has indications limited to prosthetic frameworks due to its low translucency. However, the development of translucent zirconia has enabled this material to become aesthetic, presenting itself as a viable alternative for the manufacturing of ultra thin veneers, along with the benefit of its high strength, thereby reducing the risk of fracture in the stages of try-in and cementation.
Acknowledgments
The authors are grateful to Vagner Laboratory (São Paulo, Brazil) for manufacturing the monolithic zirconia ultra-thin veneers. YZ would like to thank the United States National Institutes of Health, National Institute of Dental and Craniofacial Research (Grant No. R01DE026772 and Grant No. R01DE026279) for their support.
Footnotes
Conflict of Interest
The authors of this manuscript certify that they have no proprietary, financial, or other personal interest of any nature or kind in any product, service, and/or company that is presented in this article.
References
- 1.Peumans M, Meerbeek BV, Lambrechts P, Vanherke G. Porcelain veneers: a review of the literature. Journal of Dentistry. 2000;28(3):163–177. doi: 10.1016/s0300-5712(99)00066-4. [DOI] [PubMed] [Google Scholar]
- 2.Strassler HE. Minimally invasive porcelain veneers: Indications for a conservative esthetic dentistry treatment modality. General Dentistry. 2007;55(7):686–694. [PubMed] [Google Scholar]
- 3.Carpena G, Ballarin A, Aguiar JA. New Ceramics Approach for Contact Lens. Odovtos International Journal of Dental Sciences. 2015;17(1):12–18. [Google Scholar]
- 4.Soares PV, Spini PH, Carvalho VF, Souza PG, Gonzaga RC, Tolentino AB, Machado AC. Esthetic rehabilitation with laminated ceramic veneers reinforced by lithium disilicate. Quintessence International. 2014;45(2):129–133. doi: 10.3290/j.qi.a31009. [DOI] [PubMed] [Google Scholar]
- 5.Conrad HJ, Seong W-J, Pesun IJ. Current ceramic materials and systems with clinical recommendations: A systematic review. The Journal of Prosthetic Dentistry. 2007;98(5):389–404. doi: 10.1016/S0022-3913(07)60124-3. [DOI] [PubMed] [Google Scholar]
- 6.Trinkner TF, Roberts M. Fluorapatite-leucite glass ceramic veneers for aesthetic anterior restorations. Practical Procedures & Aesthetic Dentistry. 2001;13(1):37–41. [PubMed] [Google Scholar]
- 7.Manicone PF, Lammetti RP, Raffaelli L. An overview of zircônia ceramics: Basic properties and clinical appications. Journal of Dentistry. 2007;35(11):819–826. doi: 10.1016/j.jdent.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 8.Spear F, Holloway J. Which all-ceramic system is optimal for anterior esthetics? The Journal of the American Dental Association. 2008;139(9):19S–24S. doi: 10.14219/jada.archive.2008.0358. [DOI] [PubMed] [Google Scholar]
- 9.Zhang Y. Making yttria-stabilized tetragonal zircônia. Dental Material. 2014;30(10):1195–1203. doi: 10.1016/j.dental.2014.08.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Matsuzaki F, Sekine H, Honma S, Takanashi T, Furuya K, Yajima Y, Yoshinari M. Translucency and flexural strength of monolithic translucent zirconia and porcelain-layered zircônia. Dental Materials Journal. 2015;34(6):910–917. doi: 10.4012/dmj.2015-107. [DOI] [PubMed] [Google Scholar]
- 11.Koutayas SO, Vagkopoulou T, Pelekanos S, Koidis P, Strub JR. Zirconia in Dentistry: Part 2. Evidence-based clinical breakthrough. The European Journal of Esthetic Dentistry. 2009;4(4):348–380. [PubMed] [Google Scholar]
- 12.Thompson JY, Stoner BR, Piascik JR, Smith R. Adhesion/cementation to zircônia and other non-silicate ceramics: Where are we now? Dental Material. 2011;27(1):71–82. doi: 10.1016/j.dental.2010.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rinke S, Fischer C. Range of indications for translucent zirconia modifications: Clinical and technical aspects. Quintessence International. 2013;44(8):557–566. doi: 10.3290/j.qi.a29937. [DOI] [PubMed] [Google Scholar]
- 14.Stober T, Bermejo JL, Rammelsberg P, Schmitter M. Enamel wear caused by monolithic zirconia crowns after 6 months of clinical use. Journal of Oral Rehabilitation. 2014;41(4):314–322. doi: 10.1111/joor.12139. [DOI] [PubMed] [Google Scholar]
- 15.Alghazzawi TF, Lemons J, Liu P-R, Essig ME, Janowski GM. The failure load of CAD/CAM generated zirconia and glass-ceramic laminate veneers with different preparation designs. The Journal Prosthetic Dentistry. 2012;108(6):386–393. doi: 10.1016/S0022-3913(12)60198-X. [DOI] [PubMed] [Google Scholar]
- 16.Sarmento HR, Campos F, Sousa RS, Machado JPB, Souza ROA, Bottino MA, Özcan M. Influence of air-particle deposition protocols on the surface topography and adhesion of resin cement to zirconia. Acta Odontologica Scandinavica. 2013;72(5):346–353. doi: 10.3109/00016357.2013.837958. [DOI] [PubMed] [Google Scholar]
- 17.Alves MLL, Campos F, Bergoli CD, Botino MA, Özcan M, Souza ROA. Effect of adhesive cementation strategies on the bonding of Y-TZP to human dentin. Operative Dentistry. 2016;41(1):1–8. doi: 10.2341/15-052-L. [DOI] [PubMed] [Google Scholar]
- 18.May LG, Passos SP, Capelli DB, Özcan M, Bottino MA, Valandro LF. Effect of silica coating combined to a MDP-based primer on the resin bond to Y-TZP ceramic. Journal of Biomedical Materials Research Part B: Applied Biomaterials. 2010;95(1):69–74. doi: 10.1002/jbm.b.31684. [DOI] [PubMed] [Google Scholar]
- 19.Srikanth R, Kosmac T, Della Bona A, Yin L, Zhang Y. Effects of Cementation Surface Modifications on Fracture Resistance of Zirconia. Dental Materials. 2015;31(4):435–442. doi: 10.1016/j.dental.2015.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Queiroz JRC, Duarte DA, Souza ROA, Fissmer SF, Massi M, Bottino MA. Deposition of SiOx thin films on Y-TZP by reactive magnetron sputtering: Inluence of plasma parameters on the adhesion properties between Y-TZP and resin cement for application in dental prosthesis. Materials Research. 2011;14(2):212–216. [Google Scholar]
- 21.Pereira LL, Campos F, Dal Piva AM, Gondim LD, Souza RO, Özcan M. Can application of universal primers alone be a substitute for airborne-particle abrasion to improve adhesion of resin cement to zirconia? The Journal of Adhesive Dentistry. 2015;17(2):169–74. doi: 10.3290/j.jad.a33974. [DOI] [PubMed] [Google Scholar]
- 22.Campos TMB, Ramos NC, Machado JPB, Bottino MA, Souza ROA, Melo RM. A new sílica-infiltrated Y-TZP obtainded by the sol-gel method. Journal of Dentistry. 2016;48:55–61. doi: 10.1016/j.jdent.2016.03.004. [DOI] [PubMed] [Google Scholar]
- 23.Chai H, Kaizer M, Chughtai A, Tong H, Tanaka C, Zhang Y. On the Interfacial Fracture Resistance of Resin-Bonded Zirconia and Glass-Infiltrated Graded Zirconia. Dental Materials. 2015;31(11):1304–1311. doi: 10.1016/j.dental.2015.08.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aboushelib MN1, Kleverlaan CJ, Feilzer AJ. Selective infiltration-etching technique for a strong and durable bond of resin cements to zirconia-based materials. Journal Prosthetic Dentistry. 2007;98(5):379–88. doi: 10.1016/S0022-3913(07)60123-1. [DOI] [PubMed] [Google Scholar]
- 25.Ha JY, Son JS, Kim YK, Kim KH, Kwon TY. Effect of heat treatment of dental zirconia ceramic treated with three different primers on the bonding of resin cement. Macromolecular Research. 2013;21(1):71–7. [Google Scholar]
- 26.Melo RM, Souza RO, Dursun E, Monteiro EB, Valandro LF, Bottino MA. Surface Treatments of Zirconia to Enhance Bonding Durability. Operative Dentistry. 2015;40(6):636–643. doi: 10.2341/14-144-L. [DOI] [PubMed] [Google Scholar]
- 27.Queiroza JRC, Duarteb DA, Souza ROA, Fissmerb SF, Massib M, Bottinoa MA. Deposition of SiOx Thin Films on Y-TZP by Reactive Magnetron Sputtering: Influence of plasma parameters on the adhesion Ppoperties between Y-TZP and resin cement for application in dental prosthesis. Materials Research. 2011;14(2):212–216. [Google Scholar]
- 28.Lung CY, Botelho MG, Heinonen M, Matinlinna JP. Resin zircônia bonding promotion with some novel coupling agentes. Dental Materials. 2012;28(8):863–872. doi: 10.1016/j.dental.2012.04.023. [DOI] [PubMed] [Google Scholar]
- 29.Castro HL, Corazza PH, Paes-Júnior TA. Influence of Y-TZP ceramic treatment and different resin cements on bond strength to dentin. Dental Materials. 2012;28(11):1191–1197. doi: 10.1016/j.dental.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 30.Ikoshi M, Kameyama A, Munck JD, Minakuchi, Meerbeek Durable bonding to mechanically and/or chemically pre-treated dental zircônia. Journal of Dentistry. 2013;41(2):170–179. doi: 10.1016/j.jdent.2012.10.017. [DOI] [PubMed] [Google Scholar]
- 31.Rondoni D. Zirconia: some practical aspects from the technologist’s point of view. The International Journal of Esthetic Dentistry. 2016;11(2):2–6. [PubMed] [Google Scholar]
- 32.Harada K, Raigrodski AJ, Chung KH, Flinn BD, Dogan S, Mancl LA. A comparative evaluation of the translucency of zirconias and lithium disilicate for monolithic restorations. The Journal of Prosthetic Dentistry. 2016;116(2):257–263. doi: 10.1016/j.prosdent.2015.11.019. [DOI] [PubMed] [Google Scholar]
- 33.Sulaiman TA, Abdulmajeed AA, Donovan TE, Ritter AV, Lassila LV, Vallittu PK, Närhi TO. Degree of conversion of dual-polymerizing cements light polymerized through monolithic zirconia of different thicknesses and types. The Journal of Prosthetic Dentistry. 2015;114(1):103–108. doi: 10.1016/j.prosdent.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 34.Vichi A, Louca C, Corciolani G, Ferrari M. Color related to ceramic and zirconia restorations: a review. Dental Materials. 2011;27(1):97–108. doi: 10.1016/j.dental.2010.10.018. [DOI] [PubMed] [Google Scholar]
- 35.Klimke J, Trunec M, Krell A. Transparent tetragonal yttria-stabilized zirconia ceramics: influence of scattering caused by birefringence. Jounal of the American Ceramic Society. 2011;94(6):1850–1858. [Google Scholar]
- 36.Jiang L, Liao YM, Wan QB, Li W. Effects of sintering temperature and particle size on the translucency of zirconium dioxide dental ceramic. Journal of Materials Science: Materials in Medicine. 2011;22(11):2429–2435. doi: 10.1007/s10856-011-4438-9. [DOI] [PubMed] [Google Scholar]
- 37.Tong H, Tanaka CB, Kaizer MR, Zhang Y. Characterization of three commercial Y-TZP ceramics produced for their high-translucency, high-strength and high-surface area. Ceramics International. 2016;42(1):1077–1085. doi: 10.1016/j.ceramint.2015.09.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Alghazzawi TF, Lemons J, Liu P-R, Essig ME, Janowski GM. Evaluation of the optical properties of CAD-CAM generated yttria-stabilized zirconia and glass-ceramic laminate veneers. The Journal of Prosthetic Dentistry. 2012;107(5):300–308. doi: 10.1016/S0022-3913(12)60079-1. [DOI] [PubMed] [Google Scholar]
- 39.Kelly JR, Nishimura I, Campbell SD. Ceramics in dentistry: historical roots and current perspectives. The Journal of Prosthetic Dentistry. 1996;75(1):18–32. doi: 10.1016/s0022-3913(96)90413-8. [DOI] [PubMed] [Google Scholar]
- 40.Al-Amleh B, Lyons K, Swain M. Clinical trials in zirconia: A systematic review. Journal of Oral Rehabilitation. 2010;37(8):641–652. doi: 10.1111/j.1365-2842.2010.02094.x. [DOI] [PubMed] [Google Scholar]
- 41.Vanderlei AD, Queiroz JR, Bottino MA, Valandro LF. Improved adhesion of Y-TZP ceramics: a novel approach for surface modification. General Dentistry. 2014;62(1):22–27. [PubMed] [Google Scholar]
- 42.Ha JY, Son JS, Kim YK, Kim KH, Kwon TY. Effect of heat treatment of dental zirconia ceramic treated with three different primers on the bonding of resin cement. Macromolecular Research. 2013;21(1):71–7. [Google Scholar]
- 43.Kern M. Resin bonding to oxide ceramics for dental restorations. Journal Adhesion Science and Technology. 2009;23(7–8):1097–111. [Google Scholar]