Hypertension, a major contributor to cardiovascular disease (CVD) including heart disease and stroke, is one of the leading contributors of global burden of disease and a growing public health problem worldwide.1 In the U.S., about 75.2 million adults (one in every three) had hypertension during 2013–2014.2 In 2014, hypertension was listed as a primary or contributing cause of 427,631 American deaths, and heart disease and stroke were the first-and fifth-leading causes of death respectively.3 Economically, hypertension cost the nation about $51.2 billion per year, and total CVD cost the nation about $316.1 billion per year during 2012–2013.4 Reducing the health and economic burden of hypertension and CVD is a public health priority.
Substantial knowledge regarding the epidemiology, pharmacologic and non-pharmacologic treatments, and genetics of hypertension is available; however, many people with hypertension remain undiagnosed or undertreated because health systems cannot efficiently identify or treat them, often because of poor access to health care.5 Hypertension control remains a major public health challenge.6 To promote effective hypertension prevention and control, a better understanding of the economic aspects of hypertension is important. The Division for Heart Disease and Stroke Prevention (DHDSP), Centers for Disease Control and Prevention, routinely conducts applied research that evaluates program cost, cost of illness, and cost effectiveness to address this need. This commentary highlights some challenges in quantifying the economic impact, recent research, and future research opportunities of hypertension based on the applied research from DHDSP.
DEFINING AND QUANTIFYING ECONOMIC COSTS OF HYPERTENSION
Hypertension is (1) a serious health condition requiring timely and sustained treatment; (2) an independent risk factor for many costly chronic diseases including heart disease, stroke, and chronic renal disease; and (3) a general health indicator that might be associated with other diseases and conditions unrelated to hypertension. Because of these facts, quantifying the economic costs of hypertension is particularly challenging.
Economic costs of hypertension include both direct medical costs and indirect costs such as productivity loss. Direct medical costs are the costs incurred for medical products and services used to prevent, detect, or treat a disease and its complications.7 These costs include the costs of inpatient stays, emergency room visits, physician visits, laboratory and imaging tests, home health care, and prescription medications. Although such costs are relatively straightforward to estimate because of readily available data and standardized methods, differences in study perspectives and scope of the costs, such as “charges” versus “payments,” can still present challenges to standardization. Nevertheless, cost estimates are easily understood and accepted by most decision makers and other stakeholders. Direct medical costs of hypertension include costs for hypertension treatment (i.e., hypertension treatment costs) and costs of comorbidities attributable to hypertension (i.e., hypertension-attributable costs). Hypertension-associated costs, which includes treatment and comorbidity-attributable costs, together approximate the economic burden of hypertension.
Limiting the economic cost estimates to hypertension treatment cost alone can substantially underestimate the economic burden of hypertension because it ignores the fact that hypertension is a major risk factor for many other costly diseases. One study suggested that hypertension treatment costs accounted for only 12.1% of hypertension-associated cost.8 Another study estimated that hypertension treatment costs accounted for about 21% of hypertension-associated cost, cardiovascular complications accounted for 27%, and other diagnoses for 52%.9 The former study also showed that the composition of the treatment cost was substantially different from the composition of hypertension-associated costs (Figure 1).8
Figure 1. Composition of direct medical expenditures of hypertension by service type.
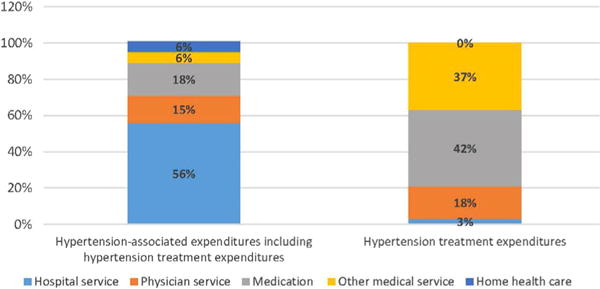
Source: Based on findings from “National Estimate of Cost of Illness for Hypertension and Non-persistence With Drug Therapy Using the Medical Expenditure Panel Survey” by SE Graden, PhD dissertation, Ohio State University, 2003.
Indirect costs are incurred from productivity loss because of morbidity and disease-related premature mortality.7 Although indirect costs are a significant public health burden, few studies on the indirect cost of hypertension exist. One study estimated the indirect cost of hypertension to U.S. employers in 2004 at $392 per eligible employee per year, which includes presenteeism, work absence, and short-term disability.10 The cost of hypertension was found to be highest among ten studied health conditions including heart disease, mental disorders, and arthritis. Furthermore, the costs were generally higher than direct medical costs. Another study projected the indirect costs of hypertension at $27.2 billion in 2015, accounting for about 23% of total costs, with direct medical costs of $91.4 billion.11
People with hypertension-related complications, such as heart disease and stroke, may require a substantial amount of informal care, including assistance with activities of daily living. This is especially true for older adults. Thus, calculating the economic burden of hypertension should also include the costs of informal caregiving. Studies have estimated the costs of informal caregiving associated with stroke in the elderly and the cost associated with heart failure in people aged >50 years.12,13 Some of these costs could be attributed to hypertension.
RECENT DEVELOPMENT IN RESEARCH ON ECONOMICS OF HYPERTENSION
Recent research on the economics of hypertension in the DHDSP has started to address the priority areas of hypertension as a secondary diagnosis, informal caregiving, and evaluation of program cost and cost effectiveness. Almost all previous cost-of-illness literature has relied on data that have only included the costs for hypertension when it was listed as a primary diagnosis on medical records.9 Recent research in DHDSP addressed hospitalization costs associated with hypertension as a secondary diagnosis.14 Medical costs by primary and secondary diagnosis status for heart failure, acute myocardial infarction, ischemic heart disease, and stroke have also been investigated. Methods employed by and findings from these studies can be used as a foundation for further cost-effectiveness evaluations and investigation of comorbidity and aging issues related to many chronic conditions.
Another major contribution to the field is estimating informal caregiving costs for patients with heart failure and stroke.12,13 Using a difference-in-difference approach, propensity score matching technique, and two-part models, incremental informal caregiving hours and costs associated with stroke and heart failure were examined. Some of these costs should be attributed to hypertension. These studies provided much needed information for further investigating the economic burden associated with hypertension and other chronic conditions.
Finally, much needed research in the evaluation of program cost and effectiveness has been conducted. A cost analysis of a community health worker program in rural Vermont provided a framework for cost evaluations using data from administrative records and personal interviews.15 An effectiveness evaluation of full coverage for antihypertension drugs in China’s rural communities suggested it was a viable means of enhancing medication adherence while reducing total medical costs.16 The cost effectiveness of a hypertension control intervention in community health centers in China was also examined.17 These research methods and findings could be used to support community-based interventions for hypertension control.
FUTURE RESEARCH ON THE ECONOMICS OF HYPERTENSION
The substantial health and economic burden associated with hypertension suggests that hypertension prevention is a growing public health priority. Expanding the literature on the economics of hypertension can support such a priority. Several specific areas for future economic research may be particularly relevant to expand and improve efforts for promoting cardiovascular health:
The economics of health disparities: Addressing health disparities is a public health imperative in the U.S. Researchers have examined health disparity issues in chronic conditions including hypertension. However, little research has documented the economic aspects of disparities, such as the impact of health disparities on medical costs or the cost effectiveness of reducing health disparities. Such economic information can support community- and local-level interventions promoting cardiovascular health in disparate population groups.
Indirect costs and costs of informal caregiving associated with hypertension: More research is needed to better estimate indirect costs. Furthermore, the burden of chronic diseases and an aging population may increase the demand for formal and informal caregiving, especially for the elderly. Information on productivity loss as well as formal and informal caregiving can be used to more fully estimate the economic burden and help identify the necessary resources to support healthy aging.
Economic analyses of comorbidities: Multiple chronic conditions are common among people with hypertension. For example, more than 66% of people with hypertension have three or more other chronic conditions among Medicare fee-for-service beneficiaries.18 However, more needs to be done to accurately estimate comorbidity costs and avoid counting the same costs for multiple conditions (i.e., double counting).
These and other priorities are addressed in research from DHDSP. The articles presented in this supplement highlight some of the economic research in these areas. Ongoing and future research will continue to advance our knowledge and generate improved methods regarding the economics of hypertension. This supplement and other economic research can be used to develop, improve, and assess public health interventions for better cardiovascular health.
Acknowledgments
Publication of this article was supported by the U.S. Centers for Disease Control and Prevention (CDC), an Agency of the U.S. Department of Health and Human Services, and the Association for Prevention Teaching and Research (APTR) Cooperative Agreement No. 1U36 OE000005.
The findings and conclusions in this publication are those of the authors and do not necessarily represent the official position of the CDC.
Footnotes
No financial disclosures were reported by the authors of this paper.
This article is part of a supplement issue titled The Economics of Hypertension and Cardiovascular Disease.
References
- 1.Constant AF, Geladari EV, Geladari CV. The economic burden of hypertension. Chapter 21. In: Andreadis EA, editor. Hypertension and Cardiovascular Disease. Switzerland: Springer International Publishing; 2016. https://doi.org/10.1007/978-3-319-39599-9_21. [Google Scholar]
- 2.Merai R, Siegel C, Rakotz M, et al. CDC grand rounds: a public health approach to detect and control hypertension. MMWR Morb Mortal Wkly Rep. 2016;65(45):1261–1264. doi: 10.15585/mmwr.mm6545a3. https://doi.org/10.15585/mmwr.mm6545a3. [DOI] [PubMed] [Google Scholar]
- 3.CDC, National Center for Health Statistics. Multiple Cause of Death 1999–2015. CDC WONDER online database. http://wonder.cdc.gov/mcd-icd10.html. December 2016. Accessed June 10, 2017.
- 4.Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics—2017 updates: a report from the American Heart Association. Circulation. 2017;135(10):e146–e603. doi: 10.1161/CIR.0000000000000485. https://doi.org/10.1161/CIR.0000000000000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goyal A, Bornstein WA. Health system-wide quality programs to improve blood pressure control. JAMA. 2013;310(7):695–696. doi: 10.1001/jama.2013.108776. https://doi.org/10.1001/jama.2013.108776. [DOI] [PubMed] [Google Scholar]
- 6.Jaffe MG, Lee GA, Young JD, Sidney S, Go AS. Improved blood pressure control associated with a large-scale hypertension program. JAMA. 2013;310(7):699–705. doi: 10.1001/jama.2013.108769. https://doi.org/10.1001/jama.2013.108769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eisenberg JM. Clinical economics: a guide to economic analysis of clinical practice. JAMA. 1989;262(20):2879–2886. doi: 10.1001/jama.262.20.2879. https://doi.org/10.1001/jama.1989.03430200123038. [DOI] [PubMed] [Google Scholar]
- 8.Graden SE. National Estimate of Cost of Illness for Hypertension and Non-persistence With Drug Therapy Using the Medical Expenditure Panel Survey [dissertation] Columbus, OH: Ohio State University; 2003. [Google Scholar]
- 9.Hodgson TA, Cai L. Medical care expenditures for hypertension, its complications, and its comorbidities. Med Care. 2001;39(6):599–615. doi: 10.1097/00005650-200106000-00008. https://doi.org/10.1097/00005650-200106000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Goetzel RZ, Long SR, Ozminkowski RJ, et al. Health, absence, disability, and presenteeism cost estimates of certain physical and mental health conditions affecting U.S. employers. J Occup Environ Med. 2004;46(4):398–412. doi: 10.1097/01.jom.0000121151.40413.bd. https://doi.org/10.1097/01.jom.0000121151.40413.bd. [DOI] [PubMed] [Google Scholar]
- 11.Heidenreich PA, Trogdon JG, Khavjou OA, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123(8):933–944. doi: 10.1161/CIR.0b013e31820a55f5. https://doi.org/10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- 12.Joo H, Dunet DO, Fang J, Wang G. Cost of informal caregiving associated with stroke among the elderly in the United States. Neurology. 2014;83(20):1831–1837. doi: 10.1212/WNL.0000000000000986. https://doi.org/10.1212/WNL.0000000000000986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Joo H, Fang J, Losby JL, Wang G. Cost of informal caregiving for patients with heart failure. Am Heart J. 2015;169(1):142–148. doi: 10.1016/j.ahj.2014.10.010. https://doi.org/10.1016/j.ahj.2014.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang G, Zhang Z, Ayala C. Hospitalization costs associated with hypertension as a secondary diagnosis among insured patients aged 18-64 years. Am J Hypertens. 2010;23(3):275–281. doi: 10.1038/ajh.2009.241. https://doi.org/10.1038/ajh.2009.241. [DOI] [PubMed] [Google Scholar]
- 15.Mirambeau AM, Wang G, Ruggles L, Diane DO. A cost analysis of a community health worker program in rural Vermont. J Community Health. 2013;38(6):1050–1057. doi: 10.1007/s10900-013-9713-x. https://doi.org/10.1007/s10900-013-9713-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yu B, Zhang X, Wang G. Full coverage for hypertension drugs in rural communities in China. Am J Manag Care. 2013;19(1):e22–e29. [PMC free article] [PubMed] [Google Scholar]
- 17.Bai YM, Zhao YF, Wang G, Wang H, Liu K, Zhao WH. Cost-effectiveness of a hypertension control intervention in three community health centers in China. J Prim Care Community Health. 2013;4(3):194–201. doi: 10.1177/2150131912470459. https://doi.org/10.1177/2150131912470459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bell SP, Saraf AA. Epidemiology of multimorbidity in older adults with cardiovascular disease. Clin Geriatr Med. 2016;32(2):215–226. doi: 10.1016/j.cger.2016.01.013. https://doi.org/10.1016/j.cger.2016.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]


