Abstract
Drug-eluting stent (DES) implantation using the ‘provisional’ approach is the gold standard for percutaneous treatment of patients with unselected bifurcated lesions. Nevertheless, many operators still consider the provisional approach unsuitable for coronary patients with complex bifurcation anatomies. Yet, the provisional approach may be so differently carried out that its procedural outcome is often unpredictable. Some technical refinements may help to anticipate or manage procedural difficulties, which may occur during the management of complex patients. We sought to overview the issues related with DES selection as well as some technical points, which may increase the effectiveness of provisional stenting. In particular, the DES characteristics influencing bifurcation interventions and the technical refinements, which may be considered during a provisional stenting procedure are discussed. Indeed, main vessel stent sizing, proximal optimisation, side branch protection modality, side branch rewiring, kissing balloon and side branch rescue techniques are all pivotal to increase the safety and efficacy of the provisional strategy especially in the setting of complex anatomies and patients.
Keywords: Percutaneous coronary interventions, bifurcated lesions, stent
Diseased coronary bifurcations are frequently treated by percutaneous coronary interventions (PCI), and in these complex lesions the adoption of the most suitable treatment technique and the selection of the most appropriate coronary stent are of primary importance. Clinical evidence suggests that drug-eluting stent (DES) implantation using a provisional approach is the gold standard for unselected bifurcated lesions.[1,2] In particular, an accumulated body of evidence shows that the systematic adoption of ‘complex’ techniques with intentional implantation of DES in both main vessel (MV) and side branch (SB) is associated with worse clinical results compared with the provisional approach.[3,4] Of note, the double stenting techniques do not appear to be beneficial even in the more challenging anatomies.[3] On the other hand, a series of technical issues (DES selection and sequence of procedural steps) may greatly influence the results of provisional stenting and its suitability for complex bifurcation anatomies. In this manuscript we sought to overview the tips and tricks useful to manage coronary bifurcated lesions by systematic ‘provisional’ stenting.
Approaching the Bifurcation – Branch Wiring and Lesion Preparation
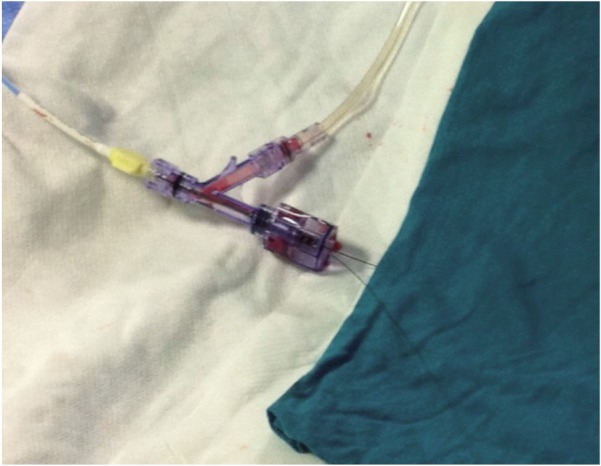
The provisional SB stenting approach is an ‘A technique’ (A for across the SB) of the Main, Across, Distal, Side (MADS) classification[5] adopted by the European Bifurcation Club (EBC) in 2007. A 6 French size (Fr) guide catheter is generally appropriate and this increases the overall safety of the procedure since the radial approach may liberally be practised and large sheaths may not be needed. As a first step in a bifurcation PCI, it is usually advisable to wire both branches, MV and SB, with two 0.014” coronary guidewires. Details regarding the wiring techniques for complex bifurcated lesions have been recently summarised by our group.[6] According to our experience, the practice of wiring the more complex branch first and keeping the two wires separated over the operative table by a simple sterile drape sheet minimises the risk of wire twisting (see Figure 1). After wiring, the MV is pre-dilated if required (according to operator’s preference or after the direct stenting failure).
Figure 1: Typical Set-up of the Operative Table in the Course of Bifurcation Intervention. The Two Guidewires (Main Vessel and Side Branch) are Kept Separated Over the Operative Table by a Simple Sterile Drape Sheet.
Regarding the SB preparation, there is a general consensus that SB dilation before MV stenting should be avoided in most of the cases since balloon dilation may cause SB dissections, which may cause an obstacle during subsequent rewiring. However, this concept has been recently challenged by the results of a randomised trial by Pan and colleagues[7] showing improved result after MV stenting in patients with SB ostial disease randomised to SB pre-dilation versus no pre-dilation. Thus, in case of true bifurcations with critical stenosis of a relevant SB, preventive SB dilation should probably be considered (with liberal use of non-compliant balloons). Some authors may recommend the use of scoring balloons or debulking devices in the case of (fibro)calcific SB ostial disease.
Issues Related with Stent Implantation in the Main Vessel
After wiring both branches and pre-dilation, when appropriate, the stent is deployed in the MV across the SB. As a first point, it must be emphasised that with the systematic provisional approach, careful evaluation of the ‘operative’ MV axis is mandatory. Indeed, when treating a bifurcated lesion with a single stent, it is pivotal to cover as much as possible the atherosclerotic disease with the stent. An example of provisional stenting with ‘inverted’ operative MV axis is shown in Figure 2. When adopting this strategy (i.e. use of distal SB for first stent implantation), it is advisable to carefully evaluate the bifurcation anatomy by invasive imaging (intravascular ultrasound or optical coherence tomography [OCT]) in order to ascertain the pre-intervention plaque distribution pattern and the result obtained.
Figure 2: (A) Dual Left Anterior Descending Artery with Tight, Long, Ostial Stenosis on the Diagonal Branch, (B) After Stenting (Using a Last Generation DES) from Left Anterior Descending Artery Toward the Diagonal Branch (Operative Main Vessel), the POT is Performed with a Short Balloon, (C) Pullback Rewiring Technique to Enter the Distal Part of Stent’s Side Cells, (D) Fluoro Appearance of Distal Rewiring – to Facilitate Visualisation of Distance Between Jailed Wire and Rewiring Wire, the Jailed Wire is Pulled Back Until the Radiopaque Segment is Located at the Bifurcation Level, (E) Post-PCI Result After Kissing Balloon with Non-compliant Balloons and (F) Angiographic Follow-up at Seven Months.
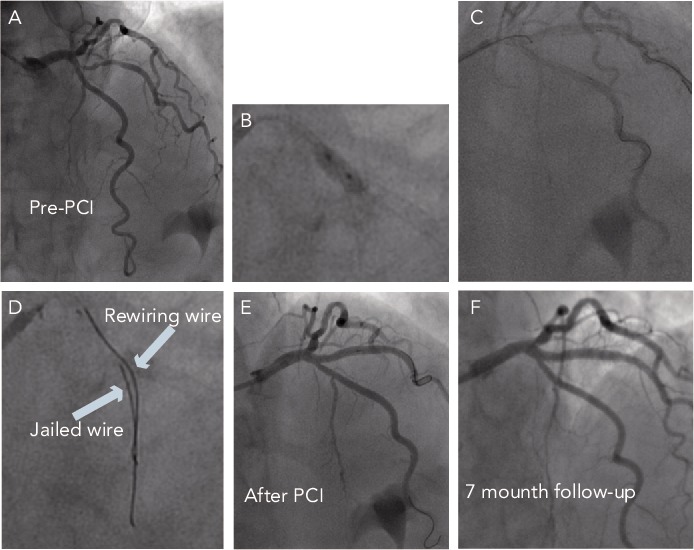
PCI = percutaneous coronary intervention.
Similarly, when dealing with diffuse disease in both MV and SB, the operative MV axis should take into account the easiness of SB rewiring. Accordingly, in case of prohibitive SB take-off with high probability of suboptimal result, it is advisable to accept the possibility to end up with double stenting and to facilitate this by implanting the first stent toward the SB.
For provisional stenting, it should be recognised that the MV stent selection is of crucial importance to guarantee a satisfactory final result. Indeed, MV stenting may induce a significant worsening at the level of jailed SB. Recent data have demonstrated that this phenomenon is mainly related to the so-called ‘carina shift’ (shift of the highly mobile ‘soft’ tissue located at the flow divider) rather than to plaque shift.[8,9] As a consequence, MV stent oversizing in the critical area of the carina (i.e. the segment of MV located immediately after the SB take-off) should be avoided, especially when dealing with acute angles. Accordingly, we use to select the MV stent diameter on the basis of the distal MV diameter. This causes a systematic malapposition of the stent at the level of proximal MV that must be promptly corrected by post-dilating the proximal part of MV stent with appropriately sized balloons according to the proximal optimisation technique (POT).[10] Regarding the POT, the technical characteristic of the different DES should be considered. Indeed, DES response to the POT has been recently recognised to be highly variable. In particular:
Pre-mounted stents differ among companies regarding sizings and crowns; this means that same diameter stents coming from different companies might have different behaviour in terms of stent oversizing and SB accessibility.[11]
The different DES have different potentiality to expand their diameter after the POT; as a consequence, when selecting a stent according to the distal MV, there is a different potentiality to expand the MV properly at the level of the proximal MV.[11,12]
The different DES have different distortion of the side cells after the POT; as a consequence, when performing the POT, some DES may have an higher side cell opening in front of the SB take-off.[12]
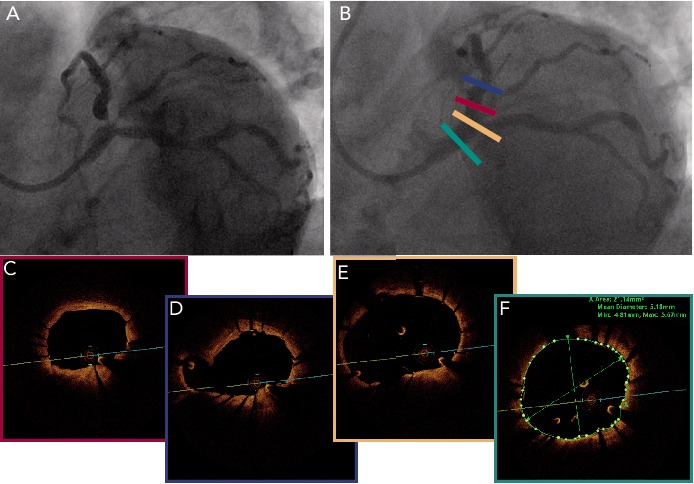
Careful attention is also mandatory when selecting the length of the MV stent as well as the length and position for post-dilating balloon. Indeed, it is important to cover at least 6–8 millimetres (mm) of the proximal MV segment with the stent. Such length is needed to accommodate the shorter available balloon for the POT in order to avoid any injury to the proximal stent edge. Regarding the balloon selection for the POT, it should be short enough to not exceed the proximal edge of the stent and to avoid touching the distal MV in order to avoid carina shift. Of note, while performing the POT, we select non-compliant balloons only when MV stent under-expansion is due to highly resistant fibrotic or calcified plaque. In the remaining cases, we choose semi-compliant balloons to take advantage of balloon compliance to fully appose the stent struts toward the vessel wall (see Figure 3 for OCT documentation of full apposition of a last generation DES in a large left main).
Figure 3: (A) Complex Lesion of the Ostial Left Anterior Descending Artery Involving the Left Main Trifurcation, (B) Final Result After Provisional Approach (Implantation of a Last Generation DES Followed by the POT and Trissing Balloon Inflation). At Post-PCI OCT, Good Apposition is Obtained Not Only at the Level of Ostial Left Anterior Descending, But Also at the Level of the Large Left Main (Panels C–F).
Beside carina and plaque shift, it should be recognised that the SB patency after MV stenting is dependent on a complex interplay between bifurcation geometry and its deformation induced by stent.[13] As a consequence, during bifurcation interventions with provisional approach, the risk of SB compromise should be strongly considered. Even if the jailed guidewire technique has been proven to be effective in facilitating bifurcation interventions,[14] in some situations the risk of SB occlusion may be predicted to be very high. In these conditions, the ‘protection’ of the SB may be further enhanced using the ‘jailed balloon protection’ technique.[15] According to this technique, an uninflated balloon is kept in the SB during MV stenting.[15] It is then removed uninflated in case of SB Thrombolysis In Myocardial Infarction (TIMI) grade 3 flow or it is inflated to restore SB flow in the case of its occlusion.[15] Such technique has been reported to allow treating safely patients with adverse bifurcation anatomies.[15,16]
Side Branch Interventions After Main Vessel Stent Implantation
Trials conducted in the setting of (selected) bifurcated lesions have used different protocols of the provisional technique (as testified by the highly variable rates of SB ballooning and stenting). The available clinical data suggest that routine kissing balloon inflation is not associated with improved clinical outcome.[17,18] However, kissing ballooning in patients undergoing provisional stenting has been recognised to:
acutely improve the SB fractional flow reserve in case of suboptimal result after MV stenting;[19]
improve the acute and long-term angiographic result at the level of SB ostium;[17,20] and
be associated with reduced post-procedural inducible ischaemia.[20]
Thus SB rewiring and kissing balloon dilation retains a relevant role in bifurcation interventions conducted according to the provisional approach, especially in the subgroup of patients with complex anatomies.
In the recent years, it has been recognised that the SB rewiring site impacts on MV stent distortion after SB dilation. Crossing of the MV stent struts in the most distal cell is associated with better SB ostium scaffolding. Accordingly, the operators should focus their attention not only on getting into the SB through the stent but also in doing this in the most distal part of the SB ostium. To this aim, the best way is to wire the SB with the ‘pullback’ technique (see Figure 2),[6] and check the rewiring site before performing kissing balloon inflation. To do this, some authors have recently proposed OCT assessment.[21] A simple alternative method consists of pulling back the jailed wire until the radiopaque segment is located at the bifurcation level to facilitate visualisation of the distance between jailed wire and rewiring wire, as shown in Figure 2.
Once the wire has re-crossed the stent struts, SB dilation is usually performed with the kissing balloon technique. Such attitude is supported by a series of experimental data documenting that isolated SB balloon dilation, without kissing balloon inflation, induces a stent deformation in the MV resulting in lumen reduction distal to the carina.[23–25] The choice of balloons for kissing inflation should consider diameters that match the two branches and have a length sufficiently short to avoid inflating them out of the stent. Recently, the use of non-compliant balloons has been proposed for final kissing inflation to have better opening of the stent struts and to reduce SB dissections.[26]
Concerning rewiring and kissing balloon procedural features, it must be underlined that the technical characteristics of the DES implanted in the MV may play a pivotal role. Indeed, the size and the shape of the MV stent cells to be re-crossed have major differences among available stents and this may translate into different easiness of SB management.[27]
How to Rescue a Failed Provisional Approach
The worst scenario in the setting of a bifurcation intervention with provisional technique is represented by comp lete loss of a relevant SB after MV stenting, with failure to rewire it. When SB occlusion is clinically relevant and any attempt to rewire it fails, operators should consider the possibility of a ‘rescue’ technique[28] based on the advancement of a small balloon over the jailed wire with the aim of reaching the SB under the stent struts. Gentle balloon dilation may restore SB flow thus facilitating rewiring. In such circumstances, jailed balloon-induced MV stent distortion should be corrected by the POT and final kissing balloon inflation.
References
- 1.Colombo A, Moses JW, Morice MC et al. Randomized study to evaluate sirolimus-eluting stents implanted at coronary bifurcation lesions. Circulation. 2004;109:1244–9. doi: 10.1161/01.CIR.0000118474.71662.E3. [DOI] [PubMed] [Google Scholar]
- 2.Stankovic G, Darremont O, Ferenc M et al. Percutaneous coronary interventions for bifurcation lesions: 2008 consensus document from the fourth meeting of the European Bifurcation Club. Eurointervention. 2009;5:39–49. doi: 10.4244/eijv5i1a8. [DOI] [PubMed] [Google Scholar]
- 3.Behan MW, Holm NR, Curzen NP et al. Simple or complex stenting for bifurcation coronary lesions: a patient-level pooled-analysis of the Nordic Bifurcation Study and the British Bifurcation Coronary Study. Circ Cardiovasc Interv. 2011;4(1):57–64. doi: 10.1161/CIRCINTERVENTIONS.110.958512. [DOI] [PubMed] [Google Scholar]
- 4.Zimarino M, Corazzini A, Ricci F et al. Late Thrombosis After Double Versus Single Drug-Eluting Stent in the Treatment of Coronary Bifurcations: A Meta-Analysis of Randomized and Observational Studies. JACC Cardiovasc Interv. 2013;6(7):687–95. doi: 10.1016/j.jcin.2013.03.012. [DOI] [PubMed] [Google Scholar]
- 5.Louvard Y, Thomas M, Dzavik V et al. Classification of coronary artery bifurcation lesions and treatments: time for a consensus! Catheter Cardiovasc Interv. 2008;71:175–83. doi: 10.1002/ccd.21314. [DOI] [PubMed] [Google Scholar]
- 6.Burzotta F, De Vita M, Sgueglia G et al. How to solve difficult side branch access? EuroIntervention. 2010;6(Suppl J:J):72–80. doi: 10.4244/EIJV6SUPJA12. [DOI] [PubMed] [Google Scholar]
- 7.Pan M. Oral communication. 2013. EuroPCR.com. EuroPCR.com Available at: website (accessed)
- 8.Suárez de Lezo J, Medina A, Martín P et al. Predictors of ostial side branch damage during provisional stenting of coronary bifurcation lesions not involving the side branch origin: an ultrasonographic study. EuroIntervention. 2012;7(10):1147–54. doi: 10.4244/EIJV7I10A185. [DOI] [PubMed] [Google Scholar]
- 9.Xu J, Hahn JY, Song YB et al. Carina shift versus plaque shift for aggravation of side branch ostial stenosis in bifurcation lesions: volumetric intravascular ultrasound analysis of both branches. Circ Cardiovasc Interv. 2012;5(5):657–62. doi: 10.1161/CIRCINTERVENTIONS.112.969089. [DOI] [PubMed] [Google Scholar]
- 10.Stankovic G, Darremont O, Ferenc M et al. Percutaneous coronary intervention for bifurcation lesions: 2008 consensus document from the fourth meeting of the European Bifurcation Club. EuroIntervention. 2009;5(1):39–49. doi: 10.4244/eijv5i1a8. [DOI] [PubMed] [Google Scholar]
- 11.Foin N, Sen S, Allegria E et al. Maximal expansion capacity with current DES platforms: a?critical factor for stent selection in the treatment of left main bifurcations? EuroIntervention. 2013;8(11):1315–25. doi: 10.4244/EIJV8I11A200. [DOI] [PubMed] [Google Scholar]
- 12.Basalus MW, van Houwelingen KG, Ankone MJ et al. Micro-computed tomographic assessment following extremely oversized partial postdilatation of drug-eluting stents. EuroIntervention. 2010;6:141–8. [PubMed] [Google Scholar]
- 13.Vassilev D, Gil RJ, Koo BK et al. The determinants of side branch compromise after main vessel stenting in coronary bifurcation lesions. Kardiol Pol. 2012;70(10):989–97. [PubMed] [Google Scholar]
- 14.Brunel P, Lefevre T, Darremont O, Louvard Y. Provisional T-stenting and kissing balloon in the treatment of coronary bifurcation lesions: results of the French multicenter “TULIPE” study. Catheter Cardiovasc Interv. 2006;68(1):67–73. doi: 10.1002/ccd.20800. [DOI] [PubMed] [Google Scholar]
- 15.Burzotta F, Trani C, Sianos G. Jailed balloon protection: a new technique to avoid acute side-branch occlusion during provisional stenting of bifurcated lesions. Bench test report and first clinical experience. EuroIntervention. 2010;5(7):809–13. doi: 10.4244/eijv5i7a135. [DOI] [PubMed] [Google Scholar]
- 16.Singh J, Patel Y, Depta JP et al. A modified provisional stenting approach to coronary bifurcation lesions: clinical application of the “jailed-balloon technique”. J Interv Cardiol. 2012;25(3):289–96. doi: 10.1111/j.1540-8183.2011.00716.x. [DOI] [PubMed] [Google Scholar]
- 17.Niemelä M, Kervinen K, Erglis A et al. Randomized comparison of final kissing balloon dilatation versus no final kissing balloon dilatation in patients with coronary bifurcation lesions treated with main vessel stenting: the Nordic-Baltic Bifurcation Study III. Circulation. 2011;123(1):79–86. doi: 10.1161/CIRCULATIONAHA.110.966879. [DOI] [PubMed] [Google Scholar]
- 18.Gwon HC, Hahn JY, Koo BK et al. Final kissing ballooning and long-term clinical outcomes in coronary bifurcation lesions treated with 1-stent technique: results from the COBIS registry. Heart. 2012;98(3):225–31. doi: 10.1136/heartjnl-2011-300322. [DOI] [PubMed] [Google Scholar]
- 19.Koo BK, Park KW, Kang HJ et al. Physiological evaluation of the provisional side-branch intervention strategy for bifurcation lesions using fractional flow reserve. Eur Heart J. 2008;29:726–32. doi: 10.1093/eurheartj/ehn045. [DOI] [PubMed] [Google Scholar]
- 20.Burzotta F, Trani C, Todaro D et al. Prospective evaluation of myocardial ischemia related to post-procedural side-branch stenosis in bifurcated lesions treated by provisional approach with drug-eluting stents. Catheter Cardiovasc Interv. 2012;79(3):351–9. doi: 10.1002/ccd.23218. [DOI] [PubMed] [Google Scholar]
- 21.Di Mario C, Iakovou I, van der Giessen WJ, Foin N, Adrianssens T, Tyczynski P, Ghilencea L, Viceconte N, Lindsay AC. Optical coherence tomography for guidance in bifurcation lesion treatment. EuroIntervention. 2010;6(Suppl J):J99–J106. doi: 10.4244/EIJV6SUPJA16. [DOI] [PubMed] [Google Scholar]
- 22.Alegría-Barrero E, Foin N, Chan PH et al. Optical coherence tomography for guidance of distal cell recrossing in bifurcation stenting: choosing the right cell matters. EuroIntervention. 2012;8(2):205–13. doi: 10.4244/EIJV8I2A34. [DOI] [PubMed] [Google Scholar]
- 23.Ormiston JA, Webster MW, Ruygrok PN et al. Stent deformation following simulated side-branch dilatation: a comparison of five stent designs. Catheter Cardiovasc Interv. 1999;47:258–64. doi: 10.1002/(SICI)1522-726X(199906)47:2<258::AID-CCD27>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 24.Kinoshita T, Kobayashi Y, De Gregorio J et al. Difference in security of stent jail between Palmaz-Schatz, NIR, and Multi-Link stents: the effect of balloon inflation through stent struts. Catheter Cardiovasc Interv. 1999;48:230–4. doi: 10.1002/(sici)1522-726x(199910)48:2<230::aid-ccd25>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 25.Mortier P, De Beule M, Van Loo D et al. Finite element analysis of side branch access during bifurcation stenting. Med Eng Phys. 2009;31:434–40. doi: 10.1016/j.medengphy.2008.11.013. [DOI] [PubMed] [Google Scholar]
- 26.Mylotte D, Hovasse T, Ziani A et al. Non-compliant balloons for final kissing inflation in coronary bifurcation lesions treated with provisional side branch stenting: a pilot study. EuroIntervention. 2012;7(10):1162–9. doi: 10.4244/EIJV7I10A187. [DOI] [PubMed] [Google Scholar]
- 27.Burzotta F, Trani C, Talarico GP et al. Resolute zotarolimus-eluting stent to treat bifurcated lesions according to the provisional technique: a procedural performance comparison with sirolimus- and everolimus-eluting stents. Cardiovasc Revasc Med. 2013;14(3):122–7. doi: 10.1016/j.carrev.2013.01.002. [DOI] [PubMed] [Google Scholar]
- 28.Aminian A, Dolatabadi D, Lalmand J. Small balloon inflation over a jailed wire as a bailout technique in a case of abrupt side branch occlusion during provisional stenting. J Invasive Cardiol. 2010;22(9):449–52. [PubMed] [Google Scholar]


