Abstract
Despite progress within the past 15 years, improving patient safety in healthcare remains an important public health issue. History of safety policies, research, and development has revealed that this issue is more complex than initially perceived and is pertinent to all healthcare settings. Solutions, therefore, must be approached at the systems level and supplemented with a change in safety culture, especially in higher risk fields such as surgery. To do so, healthcare agents at all levels have started to prioritize the improvement of non-technical skills such as teamwork, communication, and accountability, as reflected by the development of various checklists and safety campaigns. This progress may be sustained by adopting teamwork training programs that have proven successful in other high-risk industries, such as crew resource management (CRM) in aviation. These techniques can be readily implemented among surgical teams; however successful application depends heavily on the strong leadership and vigilance of individual surgeons.
Keywords: Error, patient safety, safety culture, surgery, teamwork
Introduction
Patient safety did not garner national attention until the late 1990’s, upon the publication of the Institute of Medicine (IOM) report, “To Err is Human.” This report estimated that nearly 44,000–98,000 patients die from preventable errors in American hospitals each year,1 a statistic that galvanized patient safety into the public eye and sparked activity among various healthcare stakeholders at both national and institutional levels. Since this landmark publication, substantial efforts have been made to identify sources of error, develop safety metrics, and create impactful policy initiatives to improve safety in hospitals nationwide.
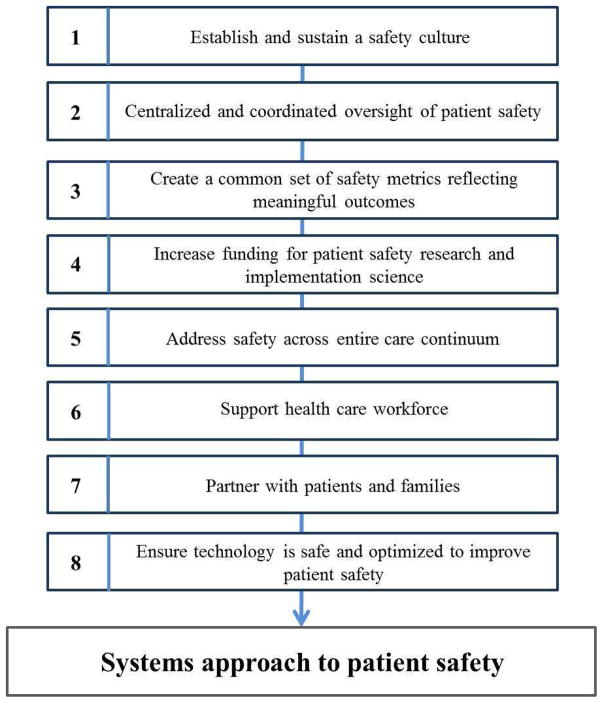
Although awareness has increased, patient safety endeavors have yielded mixed results in the reduction of preventable harms, errors, and adverse events. Recently, the National Patient Safety Foundation (NPSF) summarized the 15-year progress since “To Err is Human” and concluded that improvements have occurred at a much slower rate than initially expected.2 They stated that initiatives targeting specific and individualized harms, such as central line infection and venous thromboembolism, have demonstrated clear improvements; however proposals aimed at broader spectrums of harm have not achieved similar success.3–5 Recent patient safety research revealed that defining and measuring ‘preventable harm’ extends beyond mortality, and should also include metrics such as morbidity, diagnostic errors, decreased quality of life, and loss of dignity. This paradigm shift has broadened the scope of patient safety, classifying it as an issue pertinent not only to hospitals, but rather to all settings within the healthcare continuum. Solutions, therefore, must be approached holistically and implemented at the systems level, as indicated by NPSF recommendations (Figure 1). Creating sustainable change relies on the leadership of physicians and administrators to establish cultures of safety amongst medical teams, which requires a high degree of accountability at both institutional and individual levels. For these reasons, it is imperative that current solutions for improving patient safety are well-understood and that the ideals of widespread initiatives are translated into the actions of individuals, especially for leaders in high-risk fields of healthcare such as surgery.
Figure 1.
National Patient Safety Foundation (NPSF) Recommendations for a Total Systems Approach to Safety
A Problem of Many Hands
A common barrier to developing solutions for widespread issues is the ‘problem of many hands’, or the inability to hold an individual agent or group accountable for outcomes at the systems level.6 First applied to politics, this historical concept describes the absence of responsibility occurring in large systems that thrive on the interaction of many different agents. In these cases, structural weaknesses are more likely to go unnoticed and accumulate over time, which can eventually lead to a widespread crisis with an unidentifiable cause. This problem is particularly salient in addressing and strategizing change in the healthcare system as a whole and may further explain the inability to improve broader issues of patient safety.7
The healthcare system is a unique example of a large network of intensely specialized, yet discordant, actors who have different goals, priorities, and problems. The ability of these various actors to coordinate medical efforts as a team is a key focus of patient safety literature; improvement in communication is the primary aim for current patient safety solutions. A report of sentinel events conducted by the Joint Commission found that 70% of unexpected events causing either death or serious injury in healthcare originate from communication failures.8 The effects of communication errors in operative settings are especially well-described in surgical literature, as teamwork deficiencies in surgery can lead to complications or adverse events that can immediately endanger patients or unnecessarily stress surgical teams.9
Although the operating room resembles the problem of many hands on a smaller scale, applying systems-based solutions can benefit surgical teams and help alleviate common structural and procedural errors. An observational study carried out by Lingard et al monitored 48 surgical procedures and found that observed communication failures could be categorized into four different types: timing errors, inaccurate information, unresolved issues, and exclusion of team members.9 Furthermore, these errors are linked to observable effects on the intraoperative process such as procedure inefficiency, tension within the surgical team, delay, and wasted resources. Improving upon these patterns of error requires a formal culture change, as well as uncomfortable levels of transparency, disclosure, and dialogue to facilitate accountability at all levels of the surgical team.
Solutions and Future Directions
Many techniques have been utilized in surgery to formally change how safety values are applied in the operating room. For example, the World Health Organization (WHO) created a “Safe Surgery Saves Lives” checklist that features checkpoints of certain safety verifications that should be performed at different times in all perioperative processes to protect against universal safety hazards.10 An important component of this checklist is marking of the surgical site by the surgeon while the patient is awake, a process that has also been advocated for by the American Academy of Orthopaedic Surgeons (AAOS) “Sign Your Site” campaign, which was first introduced in 1998.11 Additionally, the Joint Commission developed a preoperative safety initiative called “Speak UP”, which emphasizes similar checkpoints in the preoperative time period to reduce wrong site and wrong patient surgical errors. A critical aspect of this protocol is having a ‘time-out’ in the preoperative period that is led by a designated team leader to ensure that the medical team addresses any communication issues or questions. The importance of allowing team members to voice concerns is similarly highlighted by the Agency for Healthcare Research and Quality (AHRQ) training program called TeamSTEPPS, which empowers any team member to speak up and “stop the line” if necessary.12 These initiatives have continued to highlight the widespread importance of non-technical skills, such as communication and teamwork, in prioritizing patient safety in the operative setting.
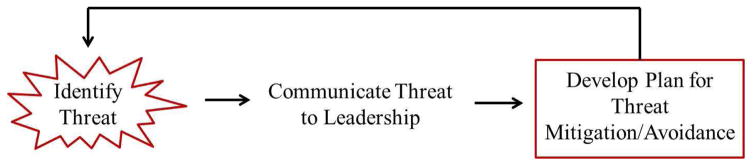
In addition to checklists and time-outs, healthcare stakeholders have explored the utility of safety management tools that have been successful for other large, high-risk industries. One of the most widely investigated sector-level policies is Crew Resource Management (CRM), a concept developed nearly three decades ago by the commercial aviation industry in response to data suggesting that human error was a major contributor to aviation incidents and accidents. The principles of CRM are founded upon a system of resource utilization that promotes both efficiency and safety by establishing clear communication pathways to report, mitigate, and avoid threats (Figure 2). To help aviation teams incorporate these principles into daily routine, CRM training is aimed at teaching effective leadership, interpersonal communication, and decision-making amongst all crew members.13 Similarities in both structure and need for safety improvement between healthcare and commercial aviation industries have prompted hospitals to bring aviation experts to train medical employees in CRM. In a recent study of CRM effectiveness in healthcare, the Hospital Survey on Patient Safety Culture (HSOPS) was administered before and two years after institution-wide implementation of CRM training and found a statistically significant improvement in composite scores for 10 out of 12 HSOPS domains.14 Of the 10 domains that improved in scores, those with the most consistent improvement were Organizational Learning-Continuous Improvement, Overall Perceptions of Patient Safety, Feedback and Communication about Error, and Communication Openness. Although these results indicate that widespread safety culture improvement may be feasible through CRM training, applying these concepts to specific medical departments may require adjustments.
Figure 2.
Crew Resource Management (CRM) conceptual framework of safety management
Military CRM
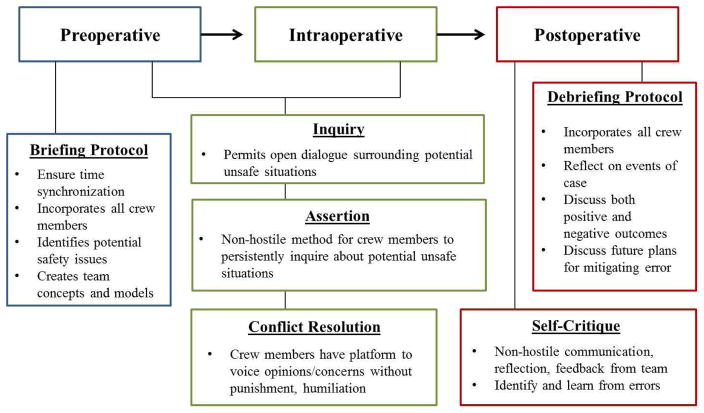
In applying an aviation framework to the healthcare system, surgeons are the fighter pilots of medicine. The many similarities between the personalities and job requirements of fighter pilots and surgeons are not limited to quick cognitive processing and the ability to handle high-risk scenarios, constant unpredictability, and responsibility for the lives of others. For these reasons, surgical teams may benefit from incorporating military, rather than commercial, aviation strategies to improve patient safety in surgery. Military CRM embodies the same concepts as commercial CRM, yet places a greater emphasis on briefing and debriefing processes in order to reflect on performance and spur continuous educational growth. For example, prior to a mission, fighter pilot teams engage in a structured and formal briefing process with the entire flight crew to define clear objectives for the mission and ensure that each member of the team has a detailed understanding of his/her role.15 Likewise, after the mission, the entire team convenes in a debriefing session to reflect on the mission proceedings and discuss how smoothly the desired objectives were met. Each briefing and debriefing session is led by the pilot of the mission and can take anywhere from 30 minutes to 2 hours (briefing) and 2 to 4 hours (debriefing).15 Surgeons certainly do not have time to conduct 4 hour debriefing sessions after each case; however, researchers have described the merits of designating small portions of time for surgical teams to utilize several key components of military CRM in daily practice (Figure 3).16
Figure 3.
Concepts of CRM and their utilization in the perioperative process
Although military CRM is time- and resource-intensive for fighter pilots, the communicative techniques of military CRM training can be readily adapted by individual surgeons without great investments of time or money. A recent report by McGreevy and Otten compiled suggestions from fighter pilots about how surgeons can replicate the essence of military CRM in the operating room.15 The authors suggest that for the preoperative briefing process, behaviors that can be adapted without formal training include both time synchronization, in which entire surgical team is punctual to establish a professional and purposeful tone; and the clear dictation of operative goals, in which the surgeon ensures that each member of the operative team understands the main objective. Additionally, after a few dedicated hours of studying military CRM techniques, the authors suggest that surgeons can create “mission objectives” for the preoperative briefing, in which surgeons dictate a dry run of the operation to the team and specify important steps that need to be achieved, roles that specific individuals need to have, and errors that need to be avoided. For residents and trainees, the authors suggest that surgeons create a desired learning objective (DLO), or a predefined benchmark for the individual student to achieve by the end of the procedure. By incorporating these practices into preoperative routine and communicating them to the entire team, the surgeon constructs a “shared mental model” for the team to work within.16 In this way, the surgeon sets a tone for collaboration and shapes a team culture that will be more resilient to common surgical stressors and able to withstand procedural unpredictability.
Briefing protocols are important to ensure avoidance of error; however, debriefing protocols are equally important for reflecting upon error and devising a plan to mitigate future sources of error. In their report of military CRM implementation, McGreevy and Otten suggest that the immediate postoperative period is an opportune time for surgeons to practice reflection with the surgical team present.15 During this time, surgeons can readily adapt fighter pilot practices of discussing both positive and negative outcomes of the operation, while also creating future plans to avoid any negative outcomes that were experienced. Although the surgeon leads postoperative discussion, it is important to note that it is the surgeon’s duty to create a platform for all team members to feel comfortable to provide input. With continual use over time, these principles may become important habits that have powerful implications for both improving team cohesion and perception of safety culture as a system value. Eliminating patient harm is a difficult task. As the scope of patient safety continues to expand alongside an increasingly specialized network of healthcare agents, endeavors aimed at reducing harm and prioritizing safety have never been more vital. Increased attention to the topic of safety has exposed the interdependency of patient harms, which must be met with interdisciplinary and integrative solutions that prompt culture change and new avenues for teamwork. However, putting these solutions into action is complex and may entail uncomfortable disclosure, dialogue, and changes in patterns of workflow. Therefore, moving towards a total-systems approach to patient safety relies on individual leaders in healthcare to recognize the importance, value, and utility of current solutions and integrate them into daily practice.
Footnotes
Disclosure: Research reported in this publication was supported by a Midcareer Investigator Award in Patient-Oriented Research (2K24 AR053120-06) to Dr. Kevin C. Chung. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors do not have a conflict of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.To Err Is Human: Building a Safer Health System. Washington, DC: Institute of Medicine; 1999. [press release] [Google Scholar]
- 2.Foundation NPS. Free From Harm: Accelerating Patient Safety Improvement Fifteen Years After “To Err is Human”. Boston, MA: National Patient Safety Foundation; 2015. [Google Scholar]
- 3.Baines RJ, Langelaan M, de Bruijne MC, et al. Changes in adverse event rates in hospitals over time: a longitudinal retrospective patient record review study. BMJ Qual Saf. 2013;22(4):290–298. doi: 10.1136/bmjqs-2012-001126. [DOI] [PubMed] [Google Scholar]
- 4.Landrigan CP, Parry GJ, Bones CB, Hackbarth AD, Goldmann DA, Sharek PJ. Temporal trends in rates of patient harm resulting from medical care. N Engl J Med. 2010;363(22):2124–2134. doi: 10.1056/NEJMsa1004404. [DOI] [PubMed] [Google Scholar]
- 5.Pronovost P, Needham D, Berenholtz S, et al. An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med. 2006;355(26):2725–2732. doi: 10.1056/NEJMoa061115. [DOI] [PubMed] [Google Scholar]
- 6.Thompson D. Moral responsibility of public officials: the problem of many hands. Am Polit Sci Rev. 1980;74:905–916. [Google Scholar]
- 7.Dixon-Woods M, Pronovost PJ. Patient safety and the problem of many hands. BMJ Qual Saf. 2016;25(7):485–488. doi: 10.1136/bmjqs-2016-005232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sentinel events statistics. The Joint Commission; [Google Scholar]
- 9.Lingard L, Espin S, Whyte S, et al. Communication failures in the operating room: an observational classification of recurrent types and effects. Qual Saf Health Care. 2004;13(5):330–334. doi: 10.1136/qshc.2003.008425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haynes AB, Weiser TG, Berry WR, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360(5):491–499. doi: 10.1056/NEJMsa0810119. [DOI] [PubMed] [Google Scholar]
- 11.Canale STDJ, Edmonson A, Fountain SS, Weiland AJ, Bartholomew L, Thomason J, Olds Glavin K, Wieting MW, Heckman JD, Gelberman RH. The American Academy of Orthopaedic Surgeons report of the task force on wrong-site surgery, 1998. American Academy of Orthopaedic Surgeons. 1998 [Google Scholar]
- 12.Clancy CM. TeamSTEPPS: optimizing teamwork in the perioperative setting. AORN J. 2007;86(1):18–22. doi: 10.1016/j.aorn.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 13.Helmreich RL, Merritt AC, Wilhelm JA. The evolution of Crew Resource Management training in commercial aviation. Int J Aviat Psychol. 1999;9(1):19–32. doi: 10.1207/s15327108ijap0901_2. [DOI] [PubMed] [Google Scholar]
- 14.Hefner JL, Hilligoss B, Knupp A, et al. Cultural Transformation After Implementation of Crew Resource Management: Is It Really Possible? Am J Med Qual. 2016 doi: 10.1177/1062860616655424. [DOI] [PubMed] [Google Scholar]
- 15.McGreevy JM, Otten TD. Briefing and debriefing in the operating room using fighter pilot crew resource management. J Am Coll Surg. 2007;205(1):169–176. doi: 10.1016/j.jamcollsurg.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 16.McGreevy J, Otten T, Poggi M, Robinson C, Castaneda D, Wade P. The challenge of changing roles and improving surgical care now: Crew Resource Management approach. Am Surg. 2006;72(11):1082–1087. doi: 10.1177/000313480607201117. discussion 1126–1048. [DOI] [PubMed] [Google Scholar]