Abstract
This article presents findings of a pilot test of a Motivational Interviewing social network intervention (MI-SNI) to enhance motivation to reduce high risk alcohol and other drug (AOD) use among formerly homeless individuals transitioning to housing. Delivered in-person by a facilitator trained in MI, this four-session computer-assisted intervention provides personalized social network visualization feedback to help participants understand the people in their network who trigger their alcohol and other drug (AOD) use and those who support abstinence. If ready, participants are encouraged to make changes to their social network to help reduce their own high-risk behavior. Participants were 41 individuals (33 male, 7 female, 1 other; 23 African-American, 5 non-Latino White, 6 Latino, 7 other, mean age 48) who were transitioning from homelessness to permanent supportive housing. They were randomly assigned to either the MI-SNI condition or usual care. Readiness to change AOD use, AOD abstinence self-efficacy, and AOD use were assessed at baseline and shortly after the final intervention session for the MI-SNI arm and around 3-months after baseline for the control arm. Acceptability of the intervention was also evaluated. MI-SNI participants reported increased readiness to change AOD use compared to control participants. We also conducted a subsample analysis for participants at one housing program and found a significant intervention effect on readiness to change AOD use, AOD abstinence self-efficacy, and alcohol use compared to control participants. Participants rated the intervention as highly acceptable. We conclude that a brief computer-assisted Motivational Interviewing social network intervention has potential to efficaciously impact readiness to change AOD use, AOD abstinence self-efficacy, and AOD use among formerly homeless individuals transitioning to permanent supportive housing, and warrants future study in larger clinical trials.
Keywords: Housing First, substance use, social networks, motivational interviewing, EgoWeb
1. Introduction
Homelessness has a significant negative impact on a variety of health-related consequences (Fazel, Khosla, Doll, & Geddes, 2008; Geddes & Fazel, 2011; Wolitski, Kidder, & Fenton, 2007), including harmful alcohol and other drug (AOD) use (Booth, Sullivan, Koegel, & Burnam, 2002; Rhoades et al., 2011). AOD use is both a cause and consequence of homelessness (Booth et al., 2002), in part due to continued exposure to AOD use in the social networks of homeless people (Rhoades et al., 2011; Tucker et al., 2009; Wenzel et al., 2009). Interrupting the cycle of homelessness through the provision of stable housing is often seen as the most effective homeless health intervention (Kidder et al., 2007). “Housing First” (HF) approaches (Kertesz, Crouch, Milby, Cusimano, & Schumacher, 2009; Padgett, 2007; Padgett, Stanhope, Henwood, & Stefancic, 2011) aim to meet the homelessness health challenge by providing housing without the requirement to participate in AOD treatment. There is evidence that residents of HF programs have similar (Padgett, Gulcur, & Tsemberis, 2006) or improved (Padgett et al., 2011; Tsemberis, Kent, & Respress, 2012) AOD outcomes compared to programs that require abstinence and treatment (Milby et al., 2008; Milby, Schumacher, Wallace, Freedman, & Vuchinich, 2005; Milby et al., 2010).
The current study describes the results of a pilot test of a novel intervention to reduce AOD use among new housing first residents. The intervention supplements usual HF case management with additional sessions that provide HF residents with personalized, visual information about their social networks. One challenge in the implementation of HF programs is that residents attempting to abstain from AOD use are inadvertently exposed to high-risk behavior through their HF-based social networks (Kertesz et al., 2009). Studies have shown that HF programs by themselves do not reduce substance use compared to treatment as usual (Somers, Moniruzzaman, & Palepu, 2015) but they provide an improved platform for recovery that can be enhanced with specific interventions targeting substance use (Henwood, 2015; Padgett, 2007). HF residents may require support to face the challenge of their changing social environments that include an evolving mixture of AOD users and non-users (Henwood et al., 2015). A large and growing body of research demonstrates both the positive and negative influences of social networks on the lives of homeless individuals (Reitzes, Crimmins, Yarbrough, & Parker, 2011; Stablein, 2011; Wolch, Rahimian, & Koegel, 1993), as well as the benefits of targeting social networks in health interventions (Valente, 2012). Therefore, providing support to HF residents to motivate them to make positive changes in their AOD use and social networks may enhance HF program benefits.
There is a need to develop social network based AOD interventions customized for HF resident populations because most existing network-based AOD interventions may not be appropriate for HF residents. Many network-based interventions are based on abstinence and/or focus on limiting social network contacts to abstaining network members (Bond, Kaskutas, & Weisner, 2003; Copello et al., 2002; Groh, Jason, & Keys, 2008; Kaskutas, Bond, & Humphreys, 2002; Kelly, Stout, Magill, & Tonigan, 2011; Litt, Kadden, Kabela-Cormier, & Petry, 2007; Litt, Kadden, Kabela-Cormier, & Petry, 2009), which may not be desirable or possible for many HF residents. Also, most network based health interventions target defined social groups rather than the personal networks of individuals who are transitioning from one social environment to another (Valente, 2012). Personal networks refer to the network of contacts most closely tied to a focal individual (Chung et al., 2015; Domínguez & Hollstein, 2014; McCarty, 2002) and can be visualized with intuitive diagrams (Eddens, Fagan, & Collins, 2017; Kennedy, Green, McCarty, & Tucker, 2011; Kennedy et al., 2016; Osilla, Kennedy, Hunter, & Maksabedian, 2016; Tubaro, Ryan, & D’Angelo, 2016). Personal network visualizations can be presented in different ways to highlight different network characteristics. Network visualizations based on responses to a personal network interview can provide individualized feedback to HF residents as they transition from homelessness to living in HF settings. HF residents who have been shown visualizations of their personal networks found them easy to understand, relevant for better understanding their social environments, and potentially useful for making changes in their AOD use and network interactions that influence AOD use (Osilla et al., 2016).
The intervention tested in this study combines visual information about HF residents’ social networks with Motivational Interviewing (MI), which is an evidence-based intervention style (Miller & Rose, 2009) that can enhance motivation to change AOD behavior (Lundahl, Kunz, Brownell, Tollefson, & Burke, 2010; Miller, Benefield, & Tonigan, 1993; Miller, Zweben, DiClemente, & Rychtarik, 1994). MI facilitators lead conversational sessions that are collaborative, nonjudgmental, and focus on strengthening clients’ own motivation and commitment to change. MI emphasizes client engagement (establishing a helpful relationship, understanding barriers and reasons to change), focusing (identifying change area, and setting an agenda), evocation (eliciting the client’s motivation to change and building their self-efficacy), and planning (developing a commitment to change and formulating an action plan). MI has been successfully coupled with a focus on social networks (Mason, Pate, Drapkin, & Sozinho, 2011) but without the use of network visualizations and with non-homeless populations. Addressing motivation to change among HF residents is important because there is evidence that motivation to change is a strong predictor of AOD use outcomes among HF residents (Collins et al., 2012). Combining MI with a focus on social networks for new HF residents is also important because of the well-known social influence on AOD use, the challenging social environmental changes that new HF residents experience, and the likelihood of exposure to AOD use among other HF residents who are not abstaining from drugs and alcohol because it is not a requirement for housing. This combination of factors suggests that the transition into HF programs is a critical time for providing support to new residents to address these social challenges and avoid future risk.
Beta tests that coupled network visualizations with MI for HF residents provided evidence that this intervention approach was feasible and acceptable by residents and staff (Osilla et al., 2016). Residents who tested the intervention reacted positively to the experience, reporting that the intervention helped them understand and discuss their social networks better than just having a conversation with a case manager. They also commented that seeing the visualization was powerful because it was based on answers they provided. They also reported that the intervention prompted them to think about how their social networks were influencing their AOD use and made them think about changing their social networks in order to change their AOD use.
The purpose of this study is to test if personalized, visual social network feedback delivered with MI to new HF residents receiving usual case management impacts their AOD use and motivation to change. We present findings of a Stage 1b pilot study (Rounsaville, Carroll, & Onken, 2001) of a MI social network intervention (MI-SNI) to enhance motivation to reduce high risk alcohol and other drug (AOD) use among formerly homeless individuals transitioning to permanent supportive housing. The goal of this Stage 1b pilot was to determine promise of this novel intervention approach for use in a larger Stage 2 RCT. We hypothesized that MI-SNI participants would show increased readiness to change AOD use and AOD abstinence self-efficacy and more positive changes in their AOD use between baseline and 3-months after baseline compared to control participants.
2. Material and Methods
2.1 Setting and Participants
Participants were new residents of either Skid Row Housing Trust (SRHT) or Single Room Occupancy Housing Corporation (SRO), two providers of permanent supportive housing (PSH) in Los Angeles County. Our initial design was to conduct the entire pilot test with SRHT residents. We designed the pilot test collaboratively with SRHT staff to meet the needs of their program (Kennedy et al., 2016) and conducted beta tests with SRHT residents (Osilla et al., 2016). SRHT residents were recruited between May 2015 and August 2016, with data collection completed in Fall 2016. In February 2016, after eight months of recruiting exclusively with SRHT residents, we began recruiting a smaller number of SRO residents as a supplement to the SRHT participants. This additional recruitment was in response to slower than expected monthly recruitment rates from SRHT and a projected shortfall in our targeted recruitment sample size. Like SRHT, SRO Housing provides rapid housing with minimal preconditions to many of their residents.
Recruitment was done through SRHT and SRO leasing office staff, who introduced the study to residents who had just received a housing unit assignment. Staff asked the resident’s permission to be contacted via phone by the research team to complete a short screening interview. Eligible participants were: (a) housed within 1 month; (b) English speaking; (c) aged 18 or older; and (d) screened positive for past-year harmful alcohol use (Alcohol Use Disorders Identification Test (AUDIT-C) score > 4 for men and > 3 for women) (Bradley, McDonell, Kivlahan, Diehr, & Fihn, 1998) or drug use (Drug Abuse Screen Test (DAST) score greater than 2) (Cocco & Carey, 1998; Maisto, Carey, Carey, Gordon, & Gleason, 2000; Skinner, 1982).
Of the 126 residents who were screened, 49 met the eligibility criteria, provided consent to participate, completed a baseline interview and were paid $30. Participants were randomly assigned to the MI-SNI intervention (n=25) or usual care (n=24). All participants were given a second assessment interview and paid $40. This “follow-up” assessment was given roughly 3 months after baseline for all participants, which was shortly after the last intervention session for those who received the intervention. All procedures were approved by the authors’ Institutional Review Board. A Federal Certificate of Confidentiality was obtained for this study, which provided additional privacy protection from legal requests.
2.2 Intervention Procedures
Detailed descriptions of the design of the Stage 1a–1b study as well as the development and beta testing of the Stage 1a computer interface and the feasibility of the intervention are available elsewhere (Kennedy et al., 2016; Osilla et al., 2016). Briefly, intervention participants were offered four biweekly in-person sessions in which they met with a MI-trained facilitator. During this meeting, the participant and facilitator sat in a private area. The facilitator first conducted a structured social network interview (~15 minutes) asking the participant about their social network interactions over the past 2 weeks. To identify network members, participants were asked, “Let’s start off with naming 15 people you have had contact with in the past two weeks. Think about the people who you interacted with the most in the past two weeks. Please only name people who are at least 18 years old.” Participants were then presented with the list of names and asked a series of questions about them. Two questions assessed network AOD use and influence on participants’ own use: 1) “How likely do you think it is that these people will drink alcohol or use some type of drugs to get high in the next two weeks? Unlikely, somewhat likely, or very likely?”; and 2) “Over the past 2 weeks, did you ever drink more alcohol or do more drugs than you wanted to when you were with any of these people? (Yes or no?)”. Finally, participants were asked about the support they received from the list of network contacts with one question: “Think about emotional support, encouragement or advice you received over the past 2 weeks from each of these people. Who gave you any emotional support, encouragement or advice?” To assess the connections among network members, participants were asked to assess the relationship between each unique network contact pair: “Does (Person 1) know (Person 2)? (If yes): How often did they interact in the past two weeks? If you don’t know for sure, give your best guess. (Not at all, a few times, most days, or every day?)” The facilitator entered responses to these questions in real-time into the social network data collection and visualization software EgoWeb 2.0 (egoweb.info) installed on a laptop computer. These responses were immediately presented back to participants in a series of social network visualizations with circles representing the network contacts mentioned by the participant (nodes) and lines between nodes representing network contacts who interacted with each other in the past 2 weeks (edges). The placement of the nodes was generated by a “spring embedding” algorithm [45], which renders the array of connections in the network into two-dimensional space by placing connected nodes that share many similar ties to other network members close together and nodes that do not further apart.
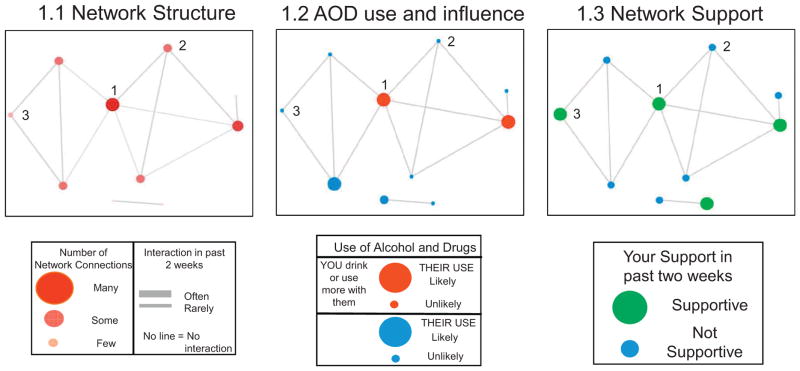
Fig. 1 provides an example of three visualizations shown to one participant during an initial session, including the visualization legends available to facilitators and participants during each session. Each of the three visualizations depict the same network structure (the same network members, connections, and node layout) with different network characteristics highlighted. The visualizations each show 10 network members (network size), with 8 network members connected in one large group (a component) and two connected network members disconnected from the main group (a dyad). Diagram 1.1 (left) highlights central network members with larger and darker color circles identifying those who had more connections to other people in the network (higher centrality). More frequent contact between network members was represented by thicker lines. Diagram (1.2) depicts the same network but highlights AOD use in the network, with larger nodes highlighting people who the participant thinks are likely to use AOD in the next 2 weeks and red nodes showing people with whom the participant recently used more AOD than usual. Diagram (1.3) depicts network contacts whom the respondent rated as supportive with larger, green nodes (vs. smaller, blue nodes). The original diagrams included the names of the network members provided by the participant, which enabled the facilitator to discuss the characteristics of individual network members in different contexts. Fig. 1 identifies three network members with different structural, AOD risk, and support profiles. The node labeled “1” is highly central, uses AOD and triggers the respondent’s use, but is also supportive. The node labeled “2” is slightly less central (has one fewer network connection), does not use or trigger AOD use, and does not provide support. Node “3” has only 2 connections, does not use AOD or trigger the participants use, and is supportive.
Fig. 1.
Example figures from an MI-SNI session 1 for 1 participant. Network contacts are represented by circles (graph “nodes”) and lines between nodes represent network contacts who interacted with each other in the past 2 weeks. The layout of the nodes, generated with the Fruchterman–Reingold force-directed placement algorithm highlights structural characteristics of the network, such as isolates (completely disconnected nodes) and components (a set of nodes tied together but disconnected from other nodes). The structural layout is consistent across the 3 diagrams. The left-side figure (1.1) uses node color and size, and line thickness to highlight other characteristics of the network structure, including the centrality of network actors (depicted by larger and darker nodes) and stronger relationship ties between actors (highlighted with thicker lines). The other figures use node size and color to highlight network composition. The middle figure (1.2) highlights the likelihood of AOD use by network members with size (larger = likely, smaller = unlikely) and increased resident use when with network member by color (red drink or use more drugs with, and blue typical use). The right-side figure (1.3) depicts supportive network members with size and color (large and green supportive, small and blue not supportive).
As these diagrams were displayed and discussed, the intervention facilitators explored the pros and cons of participants’ current social network composition and structure and discussed the impact their current network configuration had on their AOD use. Facilitators replicated the network interview and visualization discussion process with participants at sessions 2–4 and compared the current session visualizations with those generated during previous sessions. Within the context of these network discussions, facilitators discussed the participants’ readiness, willingness and confidence to change their own AOD use and risky aspects about their networks as well as strategies for positive behavior change in the future. At the end of sessions 1–3, participants were asked to identify goals to target and discuss during the next session. The second author, a clinical psychologist affiliated with the motivational interviewing network of trainers (MINT), monitored MI fidelity throughout the pilot by reviewing the recordings of each session, providing feedback about implementation of MI techniques to MI facilitators in regular meetings, and occasionally conducting re-training sessions as necessary. During the pilot period, participants assigned to both the intervention and control conditions received housing and usual support available to them as PSH residents, such as ongoing case management, support groups, referrals to mental health or substance use services, etc.
2.3 Measures
Baseline and follow-up assessments were conducted through one-on-one, in-person interviews by independent data collectors who were blind to study condition. Baseline interviews were administered after screening and follow-up interviews were administered about three months after baseline (i.e., within 2 weeks after final MI-SNI session for intervention participants).
2.3.1 Background variables
These variables included age, gender, race/ethnicity, education, number of children, marital status, and income.
2.3.2 Outcome variables
Readiness to change AOD use, AOD abstinence self-efficacy, and AOD use outcomes were measured at baseline and follow-up. We measured readiness to change AOD use using the Readiness to Change Questionnaire for Substance Use (Heather, Gold, & Rollnick, 1991; Heather, Rollnick, & Bell, 1993; Rollnick, Heather, Gold, & Hall, 1992), which consists of 12 items. Each item was scored as −1 (disagree with readiness to change AOD use), 0 (don’t know), or 1 (agree with readiness to change AOD use); α = .90. Each Readiness to Change AOD Use Questionnaire question was asked about the substance that participants identified as their biggest current problem. To measure AOD abstinence self-efficacy, we used an abbreviated version of an Abstinence Self-Efficacy Scale (DiClemente, Carbonari, Montgomery, & Hughes, 1994), modified for substance use in general, which consists of five items indicating how confident participants feel in their ability to abstain from substance use (1 = Not at all tempted, 2 = Not very tempted, 3 = Moderately tempted, 4 = Very tempted, 5 = Extremely tempted; α = .92). In analysis, items were reverse coded so that higher scores indicate higher efficacy to abstain.
To measure distal intervention outcomes, we asked respondents to self-report their past 4 week AOD use (typical drinking quantity; frequency of binge drinking; frequency of marijuana use; frequency of other drug use). Quantity of alcohol use was assessed with a Quantity Frequency Index (QFI) constructed from responses to two questions: 1) number of days (0–28) of any alcohol use and 2) the number of drinks typically consumed per drinking day. QFIs have a history of reliability and validity across various populations (O’Hare, 1997) and capture independent dimensions of AOD use behavior (Vamos et al., 2013). To calculate the QFI, we multiplied the response to the quantity of alcohol use question by the response to the typical frequency question to calculate a total number of drinks in the past 4 weeks. In a separate question, we assessed binge drinking by asking how often the respondent engaged in heavy drinking (defined as 5 or more drinks within 2 hours) over the past 4 weeks: Not at all, once, twice, three times, once a week, twice a week, 3 or 4 times a week, 5 or 6 times a week, or every day). Frequency of marijuana use was assessed as the number of days (0–28) of any use in the past 4 weeks, whereas frequency of other drug use was assessed as the sum of the number of days (0–28) that the participant used cocaine, crack, heroin, prescription medications (not prescribed by a doctor), amphetamines/methamphetamines, and/or any other type of drug in the past 4 weeks. Non-marijuana drugs were combined due to low overall frequency for any one type of drug for separate analysis. These measures have been used in other studies of substance use among homeless women (Kennedy et al., 2010), youth (Kennedy, Tucker, Green, Golinelli, & Ewing, 2012), and men (Kennedy, Brown, et al., 2013; Kennedy, Wenzel, Brown, Tucker, & Golinelli, 2013).
2.3.3 Acceptability of MI-SNI
To assess acceptability of the intervention, MI-SNI participants answered 23 questions about the quality of and their satisfaction with the sessions they attended on a 5-point Likert scale, with a higher score representing higher quality and satisfaction (D’Amico, Osilla, & Hunter, 2010; Marlatt et al., 1998; Osilla, Zellmer, Larimer, Neighbors, & Marlatt, 2008).
2.4 Analyses
The primary goal of the analysis was to assess the potential efficacy of the intervention with a small sample to determine promise for a larger clinical trial. Our approach is consistent with published guidelines for conducting Stage 1b pilot clinical trials which are developmental in scope, and exploratory in nature (Rounsaville et al., 2001). We compared demographic characteristics and outcomes at baseline by intervention group using t-tests and chi-square tests for continuous and categorical variables, respectively. To determine the effect of the intervention among eligible and consented participants, we used an intent-to-treat (Thomas et al., 2014) approach by offering follow-up to all participants and analyzing their data to reduce type I errors (Hewitt, Torgerson, & Miles, 2006).
To estimate the intervention effect we used linear regression for continuous outcomes and Poisson regression for count outcomes while controlling for the intervention group indicator and the baseline measure of the outcome. The models were fitted using the “survey” package in R version 3.3.1 to include non-response weights. These weights enabled computation of accurate standard errors and accounting for the potential bias caused by unit non-response missing data (Brick & Kalton, 1996) due to participants skipping the follow-up assessment or dropping out of the study. Of the 49 eligible study participants who completed a baseline assessment, 41 also completed 3 month follow-up assessments and responders differed from non-responders on a few characteristics, such as income and whether they were housed in SRHT or SRO. The nonresponse weights were estimated using a non-parametric regression technique, called boosting (McCaffrey, Ridgeway, & Morral, 2004), instead of logistic regression, as implemented in the TWANG R package (Ridgeway et al., 2016) and including baseline outcome and demographic variables in the model. We calculated effect sizes based on parameter estimates from the regressions and pooled standard deviation at baseline to calculate Cohen’s d (Cohen, 1992; Ferguson, 2009).
Because we designed the intervention for the SRHT program residents and only later supplemented participants with a small number of SRO residents, we conducted two stages of analysis: first, we analyzed the sample of 28 SRHT residents only and, second, we conducted the same analysis on the full sample of 41. Feedback from our facilitators suggested differences between programs and resident populations may have affected intervention impact. For example, facilitators noted that SRO Housing residents appeared more independent and did not have the same level of ongoing case management as the SRHT residents. An examination of the screening rates of participants from each program further justified this separate analysis: only 44% of the 62 SRO residents screened were eligible for the study based on previous year drug and/or alcohol use compared to 66% of the SRHT residents (chi-square 5.49, df = 1, p= 0.02).
3. Results
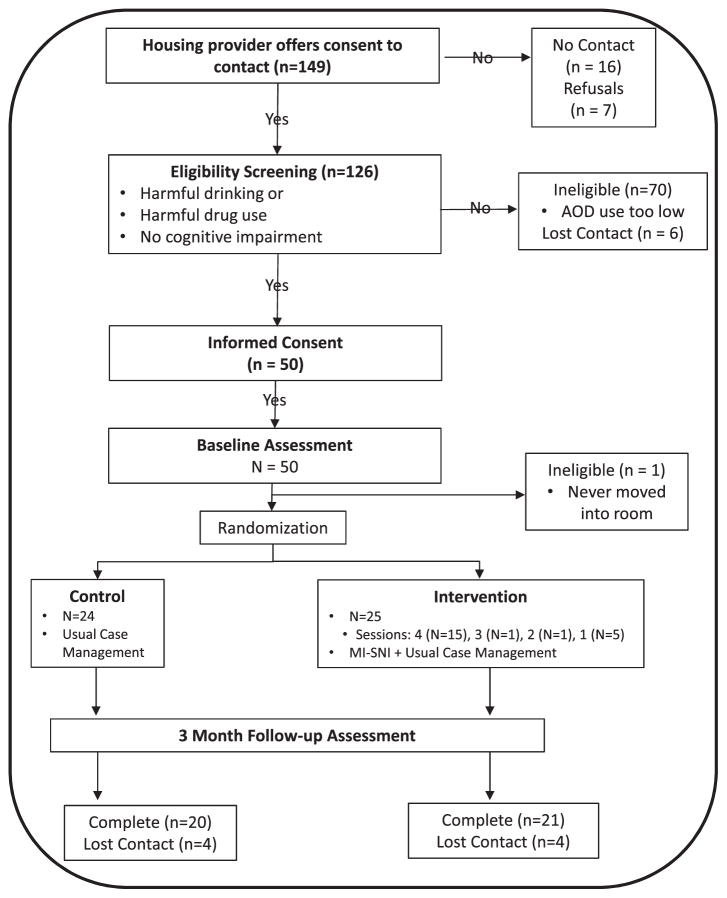
Participants’ demographic characteristics are presented in Table 1 for the entire sample, as well as by intervention arm. Participants randomly assigned to the intervention and control conditions did not significantly differ on baseline or screening characteristics. Retention in the study was excellent, with 84% (n=21 intervention, n=20 control) of participants completing the follow-up assessment three months later. See Fig. 2 for the study CONSORT flow diagram.
Table 1.
Baseline Demographic Characteristics and AOD Screening for the Final Analytic Sample
| Total (N = 41) | Control (N = 20) | Intervention (N = 21) | p1 | ||||
|---|---|---|---|---|---|---|---|
| Baseline characteristic | N | % | N | % | N | % | |
| Gender | .63 | ||||||
| Male | 33 | 80 | 15 | 75 | 18 | 86 | |
| Female/other | 8 | 20 | 5 | 5 | 3 | 14 | |
| Race-ethnicity | .94 | ||||||
| Non-Latino white | 5 | 12 | 3 | 15 | 2 | 10 | |
| African American | 23 | 56 | 11 | 55 | 12 | 57 | |
| Latino | 6 | 15 | 3 | 15 | 3 | 14 | |
| Other or multi-racial | 7 | 17 | 3 | 15 | 4 | 19 | |
| Education | .97 | ||||||
| Less than high school | 12 | 29 | 6 | 30 | 6 | 29 | |
| High school graduate | 16 | 39 | 8 | 40 | 8 | 38 | |
| Any college | 13 | 32 | 6 | 30 | 7 | 33 | |
| Relationship status | .69 | ||||||
| Married | 3 | 7 | 2 | 10 | 1 | 5 | |
| Formerly married | 11 | 27 | 6 | 30 | 5 | 24 | |
| Never married | 27 | 66 | 12 | 60 | 15 | 71 | |
| Have children | 24 | 59 | 14 | 70 | 10 | 48 | .25 |
| Mean age (SD) | 48±10 | 49±10 | 46±11 | .32 | |||
| Mean income ($), recent month (SD) | 471± 335 | 518±313 | 425±357 | .38 | |||
| Drug Abuse Screen Test (DAST)2 | 4.37±2.91 | 4.0±3.1 | 4.8±2.8 | .38 | |||
| Alcohol Use Disorders Identification Test (AUDIT-C)3 | 4.32±2.75 | 4.3±3.3 | 4.3±2.2 | .94 | |||
p-values for categorical variables are generated from chi-square tests and t-tests for continuous variables.
10 items with responses scored 0 or 1 each; summed items range from 0 to 10 with higher scores representing greater drug use problems; sum of >1 screened positive.
3 items with responses scored 0 to 4 each; summed items range from 0 to 12 with higher scores representing higher levels and more frequent drinking; Sum of >4 for men and >3 for women screened positive.
Fig. 2.
CONSORT diagram of pilot study recruitment.
Regarding intervention acceptability, we engaged 88% (22 out of 25) participants randomly assigned to the MI-SNI condition in the intervention. Of the 22 MI-SNI participants, 68% (n=15) completed all four sessions, 1 completed 3 sessions, 1 completed 2 sessions, and 5 completed 1 session. Overall, there was a high level of program satisfaction among MI-SNI participants, with a mean satisfaction rating of 4.68 (SD = 0.30) out of 5.
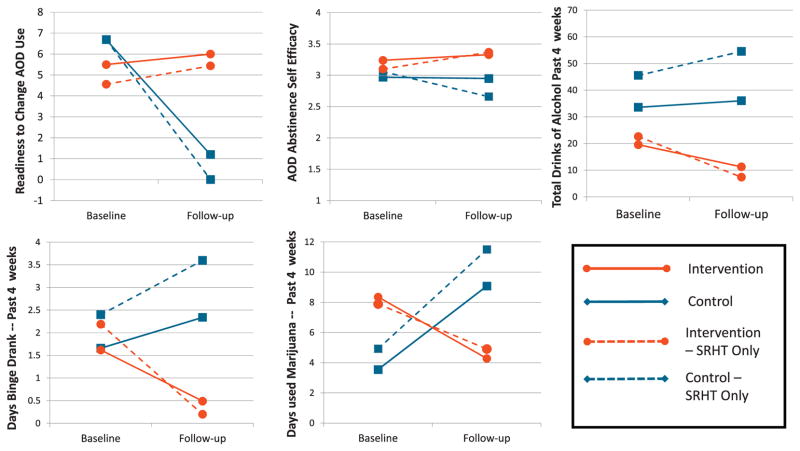
Baseline and follow-up measures and results of the regression models for the SRHT sample analysis are presented in Table 2. AOD use outcome model estimates and 95% CIs were converted to incident rate ratios (IRR) because model estimates can be easily interpreted as predicted % increase or decrease (Agresti, 1996). Intervention effects were significant and medium-large for Readiness to Change AOD Use (p=.02, d=.81) and AOD Abstinence Self-Efficacy (p=.04, d=.70), which both increased for MI-SNI participants and decreased among control participants. In addition, intervention effects were significant and small for drinking quantity (p=.02, d=.33) and binge drinking days (p=.02). While both indicators of alcohol use increased among control participants over time, they decreased among those in the MI-SNI condition. The IRR for the marijuana use model suggested a reduction in use for the intervention condition with a medium effect (43% fewer days on average, d=.60), but this model did not reach significance (p=.12). The non-marijuana drug use model was non-significant (p=.60). Fig. 3 illustrates the weighted mean estimates for each study condition at the baseline and follow-up time points on each outcome (except for non-marijuana drug use).
Table 2.
Regression model results for intervention effects on motivation to change and substance use behavior, SRHT only (N=28)
| Control (N=13) | Intervention (N=15) | |||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | |||||
| mean±SD1 | mean±SD | mean±SD | mean±SD | Est.2 | p | 95% CI2 | d3 | |
| Readiness to Change-AOD Use4 | 6.62±5.24 | .01±6.40 | 4.56±6.89 | 5.44±7.24 | 5.54 | .02 | 1.11–9.94 | .81 |
| AOD Abstinence Self Efficacy5 | 3.06±1.10 | 2.66±1.29 | 3.10±.94 | 3.37±.94 | .71 | .04 | .05–1.37 | .70 |
| AOD use outcomes, past 4 weeks | ||||||||
| Total number of drinks | 45.56.31±82.34 | 54.55.77±102.56 | 22.65±36.46 | 7.41±15.17 | .14 | .02 | .03–.67 | .33 |
| Total days binge drank | 2.40±7.48 | 3.60±8.40 | 2.19±5.59 | .20±.74 | .05 | .02 | .01–.52 | .37 |
| Total days marijuana use | 4.93±8.51 | 11.51±11.03 | 7.9±12.71 | 4.92±11.57 | .43 | .12 | .15–1.20 | .60 |
| Total days used other drugs | 12.01±11.28 | 13.86±14.64 | 12.72±14.22 | 11.10±17.13 | .80 | .60 | .35–1.82 | .15 |
Baseline and Follow-up means and SDs weighted from full intent-to-treat sample (N=49) to account for non-response at follow-up
Estimates and 95% CI reported for AOD use outcomes are converted to IRR to aid interpretation for non-linear models.
Cohen’s d effect sizes interpreted as small (.20), medium (.50), and large (.80).
12 items scored −1, 0 or 1 and summed; scale scores range from −12 to 12 with higher scores indicating higher readiness to change.
5 items averaged; scale scores range from 1 to 5 with higher scores representing higher efficacy to abstain.
Fig. 3.
Baseline and Follow-up weighted mean estimates for the intervention and control groups. Line graphs show change between baseline and follow-up on model estimated means for intervention (red with circle end-points) and control groups (blue with square end points) on five key outcomes: readiness to change AOD use, AOD abstinence self-efficacy, alcohol drinking, and marijuana use. Each figure depicts measures for both the overall sample (solid lines) and the sample restricted to SRHT residents only (dashed lines).
For the full sample (Table 3), the Readiness to Change AOD Use model predicted significantly higher scores for intervention condition controlling for baseline scores (p=.01) with a roughly large effect size (d=.72). There were no significant group differences for AOD Abstinence Self-Efficacy. The IRR values for models predicting AOD outcomes at follow-up controlling for baseline suggested reductions in alcohol use (31% fewer total drinks, d=.20; 21% fewer days binge drinking, d=.25) and marijuana use (47% fewer days using marijuana, d=.57) for intervention condition (vs. control); however, these models did not reach significance (p=.12 for each model). The model predicting use of drugs besides marijuana was also not significant (p=.60).
Table 3.
Regression model results for intervention effects on motivation to change and substance use behavior for full sample (N=41)
| Control (N=20) | Intervention (N=21) | |||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | |||||
| mean±SD1 | mean±SD | mean±SD | mean±SD | Est.2 | p | 95% CI2 | d3 | |
| Readiness to Change-AOD Use4 | 6.69±4.60 | 1.2±6.52 | 5.50±6.9 | 6.00±6.20 | 4.78 | .01 | 1.18–8.38 | .72 |
| AOD Abstinence Self Efficacy5 | 2.97±1.19 | 2.95±1.26 | 3.24±.99 | 3.33±1.03 | .38 | .23 | −.23–.99 | .22 |
| AOD use outcomes, past 4 weeks | ||||||||
| Total number of drinks (QFI) | 33.60±69.16 | 36.05±85.80 | 19.58±32.05 | 11.27±20.77 | .31 | .12 | .08–1.30 | .20 |
| Total days binge drank | 1.66±6.04 | 2.34±6.90 | 1.62±4.76 | .49±1.78 | .21 | .12 | .03–1.47 | .25 |
| Total days marijuana use | 3.55±7.08 | 9.08±9.76 | 8.36±11.10 | 4.29±11.16 | .47 | .12 | .19–1.19 | .57 |
| Total days used other drugs | 10.08±10.80 | 10.90±12.86 | 14.03±14.24 | 8.8±15.51 | .80 | .60 | .37–1.73 | .24 |
Baseline and Follow-up means and SDs weighted from full intent-to-treat sample (N=49) to account for non-response at follow-up
Estimates and 95% CI reported for AOD use outcomes are converted to IRR to aid interpretation for non-linear models.
Cohen’s d effect sizes interpreted as small (.20), medium (.50), and large (.80).
12 items scored −1, 0 or 1 and summed; scale scores range from −12 to 12 with higher scores indicating higher readiness to change.
5 items averaged; scale scores range from 1 to 5 with higher scores representing higher efficacy to abstain.
4. Discussion
We evaluated the efficacy of a MI-facilitated social network intervention among new HF residents. This study provides preliminary support for the intervention’s effect on increasing readiness to change AOD use in the full sample, as well as decreasing alcohol use and increasing AOD abstinence self-efficacy among SRHT intervention recipients compared to controls who received usual services. This pilot test also provided evidence of acceptability through high satisfaction ratings and excellent retention. The intervention’s effect on readiness to change AOD use in this at risk, non-treatment seeking population is important because higher motivation to change has been linked to AOD reductions in HF populations (Collins et al., 2012). Therefore, increasing readiness to change AOD use may lead to greater AOD use outcomes over time, suggesting the need for a larger trial and longer follow-up.
This small sample pilot study was designed to provide preliminary evidence of the intervention’s efficacy, acceptability and feasibility. The results justify continued efforts to understand the impact of an intervention aimed at changing social networks among those who are transitioning into PSH and to develop better techniques to support new HF residents as they make the social adjustments necessary to achieve targeted AOD behavior changes. The study also provides encouraging evidence that a social network-based intervention that focused on personal networks delivered in a non-judgmental MI style has promise for triggering behavior change and enhancing readiness to change AOD use.
This study has some limitations. While our sample size is appropriate for a small pilot study (Rounsaville et al., 2001), there were only a limited number of factors that we could explore and control in the analysis. The sample size was not powered for extended analysis, such as group comparisons, mediation, or examining the impact of the number of intervention sessions attended on outcomes. Also, our follow-up assessments only measured immediate outcomes. Another limitation is that our predominantly male sample drawn from only 2 HF providers limits generalizability. Finally, we also discussed HIV risk with participants in intervention sessions and collected measures of HIV-related sexual risk behaviors, as this was a target of the intervention (Kennedy et al., 2016), but we were unable to analyze this outcome because too few participants were sexually active. It is possible that this intervention approach would also successfully influence change in risky sexual behavior but we were unable to test for that effect with the current sample.
Interestingly, the subsample of residents from SRHT demonstrated stronger and significant differences between intervention and control recipients on several measures. Unfortunately, we can only speculate about why SRHT residents seemed to have benefitted from the intervention more than SRO residents. It is possible that differences in how the two programs implemented the HF model impacted the intervention effect on new residents. Different HF programs have different levels of fidelity to the HF model (Gilmer et al., 2014). Therefore, it is possible that the subsample results are due to differences in the HF program and residential population characteristics. SRHT residents may be more vulnerable to impacts of social changes that take place after moving into their apartments and this intervention that focuses on this factor may help to mitigate this vulnerability. However, the overall sample and the sample of SRO residents who screened into the study were too small for explicit group comparisons. Future studies should include sufficient sample size to test for HF program fidelity as a moderator of the intervention effect. Another unexpected finding that will require future studies to better understand is the sharp drop in readiness to change AOD use among controls between baseline and follow-up assessments. This drop was evident among SRHT residents as well as in the full sample. It is possible that the lack of a systematic focus on their social networks through usual case management contributed to a demoralization effect for those without the intervention treatment. It is also possible that all new HF residents have elevated readiness to change AOD use when first entering housing and the intervention maintains these high levels whereas control residents return to lower readiness to change AOD use levels. Future studies are necessary to better understand how the MI-SNI impacts readiness to change AOD use for new HF residents.
Future studies, with larger sample sizes, are also required to test for group differences based on characteristics such as gender, health status, primary drug of choice, and history of homelessness. This additional analysis would help to identify specific types of residents that are more likely to benefit from this intervention approach. Modifications to the intervention delivery should also be tested. For example, providing feedback to HF residents via case managers rather than external intervention facilitators may improve the support residents receive as part of PSH by making case managers more aware of the social challenges residents face as they transition to housing. Also, testing the impact of different approaches to visualizing social networks, such as having residents interactively build their networks rather than see the network after answering a series of questions, could also identify better ways to influence behavior change (Stark & Krosnick, 2017). Future studies can also test if this intervention approach has an impact on other populations (e.g., adolescents) and other health outcomes where social networks are influential (e.g., smoking).
5. Conclusions
The results of this pilot study indicate that presenting personal network based visualizations coupled with motivational interviewing could be a promising approach to increasing readiness to change AOD and decreasing substance use behavior among some HF residents. This provides sufficient evidence for further testing with a larger clinical trial. Additionally, more research is needed to determine under what circumstances this approach is most effective and what modifications to the intervention approach are necessary to increase the intervention impact on motivation and behavior change.
Highlights.
Intervention is innovative and was rated highly acceptable by participants
Readiness to change AOD use was higher for intervention recipients (d=.72)
A sub-sample had higher AOD abstinence self-efficacy and lower AOD use (d=.33–.70)
This small sample pilot’s findings warrant future study in a larger clinical trial
Acknowledgments
This work is supported by the National Institute on Drug Abuse (NIDA) grant R34 DA034855. Thank you to the participating staff and residents at Skid Row Housing Trust and Single Room Housing Corporation without whom this research would not be possible. The authors express appreciation to David Zhang for software development of EgoWeb 2.0, Gray Insight for assessment data collection, and Michael Bennett and Marylou Gilbert for intervention facilitation. The authors declare no conflicts of interests.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Agresti A. An introduction to categorical data analysis. New York: Wiley; 1996. [Google Scholar]
- Bond J, Kaskutas LA, Weisner C. The persistent influence of social networks and alcoholics anonymous on abstinence. Journal of Studies on Alcohol. 2003;64(4):579–588. doi: 10.15288/jsa.2003.64.579. [DOI] [PubMed] [Google Scholar]
- Booth BM, Sullivan G, Koegel P, Burnam A. Vulnerability factors for homelessness associated with substance dependence in a community sample of homeless adults. American Journal of Drug and Alcohol Abuse. 2002;28(3):429–452. doi: 10.1081/ada-120006735. [DOI] [PubMed] [Google Scholar]
- Bradley KA, McDonell MB, Kivlahan DR, Diehr P, Fihn SD. The AUDIT alcohol consumption questions: Reliability, validity and responsiveness to change in older male primary care patients. Alcoholism: Clinical and Experimental Research. 1998;22(8):1842–1849. doi: 10.1111/j.1530-0277.1998.tb03991.x. [DOI] [PubMed] [Google Scholar]
- Brick JM, Kalton G. Handling missing data in survey research. Statistical Methods in Medical Research. 1996;5(3):215–238. doi: 10.1177/096228029600500302. [DOI] [PubMed] [Google Scholar]
- Chung T, Sealy L, Abraham M, Ruglovsky C, Schall J, Maisto SA. Personal Network Characteristics of Youth in Substance Use Treatment: Motivation for and Perceived Difficulty of Positive Network Change. Substance Abuse. 2015;36(3):380–388. doi: 10.1080/08897077.2014.932319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cocco KM, Carey KB. Psychometric properties of the Drug Abuse Screening Test in psychiatric outpatients. Psychological Assessment. 1998;10(4):408–414. [Google Scholar]
- Cohen J. A power primer. Psychological Bulletin. 1992;112(1):155–159. doi: 10.1037/0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Collins SE, Clifasefi SL, Dana EA, Andrasik MP, Stahl N, Kirouac M, … Malone DK. Where harm reduction meets housing first: Exploring alcohol’s role in a project-based housing first setting. International Journal of Drug Policy. 2012;23(2):111–119. doi: 10.1016/j.drugpo.2011.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copello A, Orford J, Hodgson R, Tober G, Barrett C, Team UR. Social behaviour and network therapy - Basic principles and early experiences. Addictive behaviors. 2002;27(3):345–366. doi: 10.1016/s0306-4603(01)00176-9. [DOI] [PubMed] [Google Scholar]
- D’Amico EJ, Osilla KC, Hunter SB. Developing a group motivational interviewing intervention for adolescents at-risk for developing an alcohol or drug use disorder. Alcoholism Treatment Quarterly. 2010;28(4):417–436. doi: 10.1080/07347324.2010.511076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiClemente CC, Carbonari JP, Montgomery RP, Hughes SO. The Alcohol Abstinence Self-Efficacy scale. Journal of Studies on Alcohol and Drugs. 1994;55(2):141–148. doi: 10.15288/jsa.1994.55.141. [DOI] [PubMed] [Google Scholar]
- Domínguez S, Hollstein B. Mixed Methods Social Networks Research: Design and Applications. Vol. 36. Cambridge University Press; 2014. [Google Scholar]
- Eddens SK, Fagan MJ, Collins T. An Interactive, Mobile-Based Tool for Personal Social Network Data Collection and Visualization Among a Geographically Isolated and Socioeconomically Disadvantaged Population: Early-Stage Feasibility Study With Qualitative User Feedback. JMIR Res Protoc. 2017;6(6):e124. doi: 10.2196/resprot.6927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fazel S, Khosla V, Doll H, Geddes J. The Prevalence of Mental Disorders among the Homeless in Western Countries: Systematic Review and Meta-Regression Analysis. PLoS Med. 2008;5(12):e225. doi: 10.1371/journal.pmed.0050225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson CJ. An effect size primer: A guide for clinicians and researchers. Professional Psychology: Research and Practice. 2009;40(5):532–538. doi: 10.1037/a0015808. [DOI] [Google Scholar]
- Geddes JR, Fazel S. Extreme health inequalities: mortality in homeless people. Lancet. 2011;377(9784):2156–2157. doi: 10.1016/s0140-6736(11)60885-4. [DOI] [PubMed] [Google Scholar]
- Gilmer TP, Stefancic A, Katz ML, Sklar M, Tsemberis S, Palinkas LA. Fidelity to the Housing First Model and Effectiveness of Permanent Supported Housing Programs in California. Psychiatric Services. 2014;65(11):1311–1317. doi: 10.1176/appi.ps.201300447. [DOI] [PubMed] [Google Scholar]
- Groh DR, Jason LA, Keys CB. Social network variables in alcoholics anonymous: A literature review. Clinical Psychology Review. 2008;28(3):430–450. doi: 10.1016/i.cpr.2007.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heather N, Gold R, Rollnick S. Readiness to Change questionnaire: User’s manual. Kensington, Australia: National Drug and Alcohol Research Centre; 1991. [Google Scholar]
- Heather N, Rollnick S, Bell A. Predictive validity of the Readiness to Change Questionnaire. Addiction. 1993;88(12):1667–1677. doi: 10.1111/j.1360-0443.1993.tb02042.x. [DOI] [PubMed] [Google Scholar]
- Henwood BF. Commentary on Somers et al. (2015): Housing First — a platform for recovery? Addiction. 2015;110(10):1615–1616. doi: 10.1111/add.13045. [DOI] [PubMed] [Google Scholar]
- Henwood BF, Rhoades H, Hsu H-T, Couture J, Rice E, Wenzel SL. Changes in Social Networks and HIV Risk Behaviors Among Homeless Adults Transitioning Into Permanent Supportive Housing: A Mixed Methods Pilot Study. Journal of Mixed Methods Research. 2015 doi: 10.1177/1558689815607686. [DOI] [Google Scholar]
- Hewitt CE, Torgerson DJ, Miles JNV. Is there another way to take account of noncompliance in randomised trials? Canadian Medical Association Journal. 2006;175:347–348. doi: 10.1503/cmaj.051625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaskutas LA, Bond J, Humphreys K. Social networks as mediators of the effect of Alcoholics Anonymous. Addiction. 2002;97(7):891–900. doi: 10.1046/j.1360-0443.2002.00118.x. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Stout RL, Magill M, Tonigan JS. The role of Alcoholics Anonymous in mobilizing adaptive social network changes: A prospective lagged mediational analysis. Drug and Alcohol Dependence. 2011;114(2–3):119–126. doi: 10.1016/j.drugalcdep.2010.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy DP, Brown RA, Golinelli D, Wenzel SL, Tucker JS, Wertheimer S. Masculinity and HIV Risk among Homeless Men in Los Angeles. Psychology of Men & Masculinity. 2013;14(2):156–167. doi: 10.1037/a0027570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy DP, Green HD, McCarty C, Tucker JS. Nonexperts’ Recognition of Structure in Personal Network Data. Field Methods. 2011;23(3):287–306. doi: 10.1177/1525822x11399702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy DP, Hunter SB, Osilla KC, Maksabedian E, Golinelli D, Tucker JS. A computer-assisted motivational social network intervention to reduce alcohol, drug and HIV risk behaviors among Housing First residents. Addiction science & clinical practice. 2016;11(1):1–13. doi: 10.1186/s13722-016-0052-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy DP, Tucker JS, Green HD, Golinelli D, Ewing BA. Unprotected sex of homeless youth: Results from a multilevel analysis of individual, social network, and relationship factors. AIDS and Behavior. 2012;16(7):2015–2032. doi: 10.1007/s10461-012-0195-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy DP, Wenzel SL, Brown R, Tucker JS, Golinelli D. Unprotected Sex Among Heterosexually Active Homeless Men: Results from a Multi-level Dyadic Analysis. AIDS and Behavior. 2013;17(5):1655–1667. doi: 10.1007/s10461-012-0366-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy DP, Wenzel SL, Tucker JS, Green HD, Golinelli D, Ryan GW, … Zhou A. Unprotected Sex of Homeless Women Living in Los Angeles County: An Investigation of the Multiple Levels of Risk. AIDS and Behavior. 2010;14(4):960–973. doi: 10.1007/s10461-009-9621-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kertesz SG, Crouch K, Milby JB, Cusimano RE, Schumacher JE. Housing First for Homeless Persons with Active Addiction: Are We Overreaching? Milbank Quarterly. 2009;87(2):495–534. doi: 10.1111/j.1468-0009.2009.00565.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kidder DP, Wolitski RJ, Royal S, Aidala A, Courtenay-Quirk C, Holtgrave DR … Housing Hlth Study, T. Access to housing as a structural intervention for homeless and unstably housed people living with HIV: Rationale, methods, and implementation of the housing and health study. AIDS and Behavior. 2007;11(6):S149–S161. doi: 10.1007/s10461-007-9249-0. [DOI] [PubMed] [Google Scholar]
- Litt MD, Kadden RM, Kabela-Cormier E, Petry N. Changing network support for drinking: Initial findings from the network support project. Journal of Consulting and Clinical Psychology. 2007;75(4):542–555. doi: 10.1037/0022-006x.75.4.542. [DOI] [PubMed] [Google Scholar]
- Litt MD, Kadden RM, Kabela-Cormier E, Petry NM. Changing Network Support for Drinking: Network Support Project 2-Year Follow-Up. Journal of Consulting and Clinical Psychology. 2009;77(2):229–242. doi: 10.1037/a0015252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundahl BW, Kunz C, Brownell C, Tollefson D, Burke BL. A Meta-Analysis of Motivational Interviewing: Twenty-Five Years of Empirical Studies. Research on Social Work Practice. 2010;20(2):137–160. doi: 10.1177/1049731509347850. [DOI] [Google Scholar]
- Maisto SA, Carey MP, Carey KB, Gordon CM, Gleason JR. Use of the AUDIT and the DAST-10 to identify alcohol and drug use disorders among adults with a severe and persistent mental illness. Psychological Assessment. 2000;12(2):186–192. doi: 10.1037//1040-3590.12.2.186. [DOI] [PubMed] [Google Scholar]
- Marlatt GA, Baer JS, Kivlahan DR, Dimeff LA, Larimer ME, Quigley LA, … Williams E. Screening and brief intervention for high-risk college student drinkers: Results from a 2-year follow-up assessment. Journal of Consulting and Clinical Psychology. 1998;66:604–615. doi: 10.1037//0022-006x.66.4.604. [DOI] [PubMed] [Google Scholar]
- Mason M, Pate P, Drapkin M, Sozinho K. Motivational interviewing integrated with social network counseling for female adolescents: A randomized pilot study in urban primary care. Journal of Substance Abuse Treatment. 2011;41(2):148–155. doi: 10.1016/j.jsat.2011.02.009. [DOI] [PubMed] [Google Scholar]
- McCaffrey DF, Ridgeway G, Morral AR. Propensity Score Estimation With Boosted Regression for Evaluating Causal Effects in Observational Studies. Psychological Methods. 2004;9(4):403–425. doi: 10.1037/1082-989X.9.4.403. [DOI] [PubMed] [Google Scholar]
- McCarty C. Structure in personal networks. Journal of Social Structure. 2002;3(1) [Google Scholar]
- Milby JB, Schumacher JE, Vuchinich RE, Freedman MJ, Kertesz S, Wallace D. Toward cost-effective initial care for substance-abusing homeless. Journal of Substance Abuse Treatment. 2008;34(2):180–191. doi: 10.1016/j.jsat.2007.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milby JB, Schumacher JE, Wallace D, Freedman MJ, Vuchinich RE. To house or not to house: The effects of providing housing to homeless substance abusers in treatment. American Journal of Public Health. 2005;95(7):1259–1265. doi: 10.2105/ajph.2004.039743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milby JB, Schumacher JE, Wallace D, Vuchinich R, Mennemeyer ST, Kertesz SG. Effects of Sustained Abstinence Among Treated Substance-Abusing Homeless Persons on Housing and Employment. American Journal of Public Health. 2010;100(5):913–918. doi: 10.2105/ajph.2008.152975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Benefield RG, Tonigan JS. Enhancing motivation for change in problem drinking: a controlled comparison of two therapist styles. Journal of Consulting and Clinical Psychology. 1993;61(3):455–461. doi: 10.1037//0022-006x.61.3.455. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rose GS. Toward a Theory of Motivational Interviewing. American Psychologist. 2009;64(6):527–537. doi: 10.1037/a0016830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Zweben A, DiClemente CC, Rychtarik RG. Project MATCH Monograph Series: Motivational Enhancement Therapy Manual. Washington, DC: 1994. pp. 94–3723. [Google Scholar]
- O’Hare T. Measuring excessive alcohol use in college drinking contexts: The Drinking Context Scale. Addictive behaviors. 1997;22(4):469–477. doi: 10.1016/s0306-4603(96)00050-0. [DOI] [PubMed] [Google Scholar]
- Osilla KC, Kennedy DP, Hunter SB, Maksabedian E. Feasibility of a computer-assisted social network motivational interviewing intervention for substance use and HIV risk behaviors for housing first residents. Addiction science & clinical practice. 2016;11(14):1–11. doi: 10.1186/s13722-016-0061-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osilla KC, Zellmer SP, Larimer ME, Neighbors C, Marlatt GA. A brief intervention for at-risk drinking in an employee assistance program. Journal of Studies on Alcohol and Drugs. 2008;69(1):14–20. doi: 10.15288/jsad.2008.69.14. [DOI] [PubMed] [Google Scholar]
- Padgett DK. There’s no place like (a) home: Ontological security among persons with serious mental illness in the United States. Social Science and Medicine. 2007;64(9):1925–1936. doi: 10.1016/j.socscimed.2007.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padgett DK, Gulcur L, Tsemberis S. Housing first services for people who are homeless with co-occurring serious mental illness and substance abuse. Research on Social Work Practice. 2006;16(1):74–83. doi: 10.1177/1049731505282593. [DOI] [Google Scholar]
- Padgett DK, Stanhope V, Henwood BF, Stefancic A. Substance Use Outcomes Among Homeless Clients with Serious Mental Illness: Comparing Housing First with Treatment First Programs. Community Mental Health Journal. 2011;47(2):227–232. doi: 10.1007/s10597-009-9283-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reitzes DC, Crimmins TJ, Yarbrough J, Parker J. Social support and social network ties among the homeless in a downtown Atlanta park. Journal of Community Psychology. 2011;39(3):274–291. doi: 10.1002/jcop.20431. [DOI] [Google Scholar]
- Rhoades H, Wenzel SL, Golinelli D, Tucker JS, Kennedy DP, Green HD, Zhou A. The social context of homeless men’s substance use. Drug and Alcohol Dependence. 2011;118(2–3):320–325. doi: 10.1016/j.drugalcdep.2011.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridgeway G, McCaffrey D, Morral A, Griffin BA, Burgette L, Burgette ML, … Burgette M. Package ‘twang’. 2016 Retrieved from https://cran.r-project.org/web/packages/twang/twang.pdf.
- Rollnick S, Heather N, Gold R, Hall W. Development of a short readiness to change questionnaire for use in brief, opportunistic interventions among excessive drinkers. British Journal of Addiction. 1992;87(5):743–754. doi: 10.1111/j.1360-0443.1992.tb02720.x. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, Carroll KM, Onken LS. A Stage Model of Behavioral Therapies research: Getting started and moving on from stage I. Clinical Psychology-Science and Practice. 2001;8(2):133–142. doi: 10.1093/clipsy/8.2.133. [DOI] [Google Scholar]
- Skinner HA. The Drug Abuse Screening Test. Addictive behaviors. 1982;7(4):363–371. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- Somers JM, Moniruzzaman A, Palepu A. Changes in daily substance use among people experiencing homelessness and mental illness: 24-month outcomes following randomization to Housing First or usual care. Addiction. 2015;110(10):1605–1614. doi: 10.1111/add.13011. [DOI] [PubMed] [Google Scholar]
- Stablein T. Helping Friends and the Homeless Milieu: Social Capital and the Utility of Street Peers. Journal of Contemporary Ethnography. 2011;40(3):290–317. doi: 10.1177/0891241610390365. [DOI] [Google Scholar]
- Stark TH, Krosnick JA. GENSI: A new graphical tool to collect ego-centered network data. Social Networks. 2017;48:36–45. doi: 10.1016/j.socnet.2016.07.007. [DOI] [Google Scholar]
- Thomas CP, Fullerton CA, Kim M, Montejano L, Lyman DR, Dougherty RH, … Delphin-Rittmon ME. Medication-Assisted Treatment With Buprenorphine: Assessing the Evidence. Psychiatric Services. 2014;65(2):158–170. doi: 10.1176/appi.ps.201300256. [DOI] [PubMed] [Google Scholar]
- Tsemberis S, Kent D, Respress C. Housing Stability and Recovery Among Chronically Homeless Persons With Co-Occuring Disorders in Washington, DC. American Journal of Public Health. 2012;102(1):13–16. doi: 10.2105/ajph.2011.300320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tubaro P, Ryan L, D’Angelo A. The Visual Sociogram in Qualitative and Mixed-Methods Research. Sociological Research Online. 2016;21(2):1. [Google Scholar]
- Tucker JS, Kennedy DP, Ryan G, Wenzel SL, Golinelli D, Zazzali J, McCarty C. Homeless women’s personal networks: Implications for understanding risk behavior. Human Organization. 2009;68(2):129–140. doi: 10.17730/humo.68.2.m23375u1kn033518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valente TW. Network Interventions. Science. 2012;337(6090):49–53. doi: 10.1126/science.1217330. [DOI] [PubMed] [Google Scholar]
- Vamos S, Cook R, Chitalu N, Mumbi M, Weiss SM, Jones D. Quality of relationship and sexual risk behaviors among HIV couples in Lusaka, Zambia. AIDS care. 2013;25(9):1102–1108. doi: 10.1080/09540121.2012.749339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenzel SL, Green HD, Tucker JS, Golinelli D, Kennedy DP, Ryan G, Zhou AN. The social context of homeless women’s alcohol and drug use. Drug and Alcohol Dependence. 2009;105(1–2):16–23. doi: 10.1016/j.drugalcdep.2009.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolch JR, Rahimian A, Koegel P. Daily and periodic mobility patterns of the urban homeless. Professional Geographer. 1993;45(2):159–169. doi: 10.1111/j.0033-0124.1993.00159.x. [DOI] [Google Scholar]
- Wolitski RJ, Kidder DP, Fenton KA. HIV, homelessness, and public health: Critical issues and a call for increased action. AIDS and Behavior. 2007;11(6):S167–S171. doi: 10.1007/s10461-007-9277-9. [DOI] [PubMed] [Google Scholar]