Introduction
Coronary artery disease (CAD) is one of the leading causes of death and disability in Europe and worldwide. For patients with multi-vessel CAD, coronary artery bypass graft (CABG) surgery is a common approach for coronary revascularization, and is of proven symptomatic and prognostic benefit. Due to an aging population, higher prevalence of co-morbidities (such as diabetes mellitus, heart failure, hypertension, and renal failure), and a growing requirement for concomitant surgical procedures (such as valve and aortic surgery), higher risk patients are undergoing surgery.1–3 This has resulted in an increased risk of peri-operative myocardial injury (PMI)4 and Type 5 myocardial infarction (MI), both of which are associated with worsened clinical outcomes following CABG surgery. The aetiology and determinants of PMI and Type 5 MI are multi-factorial (see Tables 1 and 2 for summary). Although diagnostic criteria have been proposed for Type 5 MI (based on an elevation in cardiac biomarkers in the 48-h post-operative period and electrocardiogram/angiography/imaging evidence of MI5,13), there is currently no clear definition for prognostically significant PMI, in terms of the level of post-operative cardiac biomarker elevation, which is associated with worsened clinical outcomes following CABG surgery.
Table 1.
Causes of peri-operative myocardial injury in patients undergoing coronary artery bypass graft surgery
|
Adapted from reference 6.
Table 2.
Predictors of peri-operative myocardial infarction/graft-failure
|
Therefore, the aim of this European Society of Cardiology (ESC) Joint Working Groups (WG) Position Paper is to provide a set of recommendations to better define the level of cardiac biomarker elevation following CABG surgery at which PMI should be considered prognostically significant, and therefore prompt further clinical evaluation. We also provide guidance on how to manage patients with PMI and Type 5 MI.
Defining type 5 myocardial infarction
Type 5 MI has been defined in the Third Universal Definition of MI (2012) as an elevation of cardiac troponin (cTn) values >10× 99th percentile upper reference limit (URL) during the first 48 h following CABG surgery, in patients with normal baseline cardiac cTn values (<99th percentile URL) together with either: (a) new pathological Q waves or new left bundle branch block (LBBB), or (b) angiographic documented new graft or new native coronary artery occlusion, or (c) imaging evidence of new loss of viable myocardium or new regional wall motion abnormality (RWMA).13 In general, Type 5 MI is mainly due to an ischaemic event arising from either a failure in graft function, an acute coronary event involving the native coronary arteries, or inadequate cardioprotection. The incidence of Type 5 MI following CABG surgery varies depending on the diagnostic criteria which are used to define it. When assessed by elevations in cardiac biomarkers and new electrocardiogram (ECG) evidence of Q waves or LBBB, the incidence has been reported to range from 5 to 14%,4 whereas it ranges from 20 to 30% when using cardiac magnetic resonance (CMR) to detect new loss of viable myocardium.14–16
The current definition of Type 5 MI does have several limitations:
The selection of a cTn elevation of 10× URL as a threshold for diagnosing Type 5 MI was arbitrarily chosen. Elevated cTn of 10× URL occurs in over 90% of all patients undergoing CABG surgery.8,12
Type 5 MI requires the presence of ECG/angiography/imaging evidence of MI, and ignores post-surgical isolated elevations in cardiac biomarkers which may still be prognostically significant (i.e. biomarker elevations in the absence of ECG/angiographic or other imaging evidence of MI).
The diagnostic criteria for Type 5 MI can also be quite challenging in the setting of CABG surgery for several reasons: (i) In a substantial number of patients, the ECG may not be interpretable and many of the ECG changes following CABG surgery may be non-specific for MI.15–17 (ii) Coronary angiography is rarely performed post-surgery to diagnose very early graft failure; and (iii) Echocardiography is the most practical imaging modality for detecting new loss of viable myocardium or new RWMA following CABG surgery, but it may not be diagnostic in many cases.
As such, the diagnosis of Type 5 MI in the 48 h post-operative period may be quite challenging, unless it presents with obvious graft failure or a significant ischaemic event. Therefore, in many cases, patients may sustain prognostically significant PMI, but this may be overlooked. The Society for Cardiovascular Angiography and Interventions (SCAI) has proposed a new definition for clinically relevant MI, which takes into account isolated elevations in either creatine kinase-MB fraction (CK-MB) or cTn within 48 h of CABG surgery.18 With respect to CK-MB, these recommendations propose a peak elevation ≥10× URL in isolation or ≥5× URL with new pathologic Q-waves in ≥2 contiguous ECG leads or new persistent LBBB. A substantially higher cut-off for cTn elevation of ≥70× URL in isolation or ≥35× URL with new pathologic Q-waves in ≥2 contiguous ECG leads or new persistent LBBB is also proposed in that paper.18 Again, these threshold levels were arbitrarily chosen, and further studies are required to validate their new definition of clinically relevant MI, and explore their relationship to clinical outcomes post-surgery. In addition, these recommendations do not take into consideration isolated elevations of cardiac biomarkers below these thresholds, which may still be clinically relevant and prognostically significant.
Defining peri-operative myocardial injury
Peri-operative myocardial injury is defined as an isolated elevation in cardiac biomarkers (CK-MB and/or cTn) greater than the upper limit of normal, in the 48-h post-operative period. However, this level of cardiac biomarker elevation occurs in virtually all patients undergoing CABG surgery, and there is no clear consensus on the level of cardiac biomarker elevation above which, it is either clinically relevant or prognostically significant. A recent publication has proposed defining PMI as an isolated elevation in cTn <10× the URL within 48 h of CABG surgery,5 but this definition does not include those patients who have isolated cTn elevations >10× URL in the absence of ECG/angiographic or other imaging evidence of MI. Therefore, in this ESC Joint WG Position Paper we provide recommendations for defining prognostically significant PMI following CABG surgery, which should prompt further clinical evaluation to exclude Type 5 MI. In this paper, we mainly focus on those patients undergoing elective isolated on-pump or off-pump CABG surgery, as the presence of prognostically significant PMI is more challenging to define in patients presenting with an acute coronary syndrome (with elevated pre-operative cardiac biomarkers), and those having concomitant valve or aortic surgery. However, patients presenting with an acute coronary syndrome are become increasingly rare since many undergo primarily percutaneous intervention.
Isolated elevations in creatine kinase-MB fraction and mortality post-coronary artery bypass graft surgery
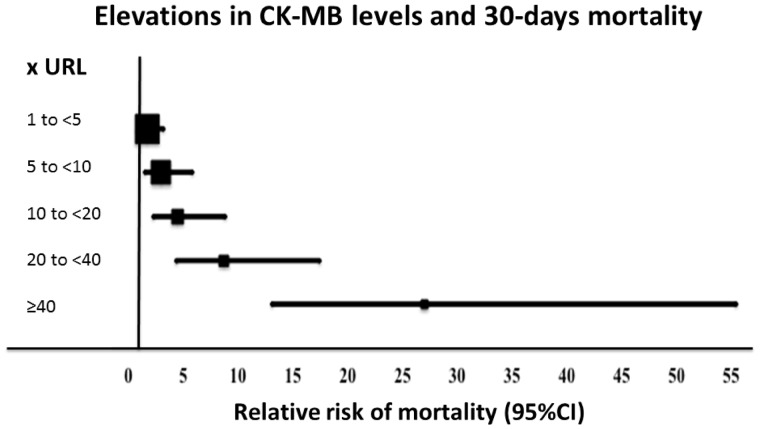
A large number of early studies have assessed the prognostic significance of isolated elevations in CK-MB following CABG surgery in the absence of ECG/angiographic or other imaging evidence of MI (Table 3 and Figure 1). These studies have demonstrated a graded increase in short, medium, and long-term mortality beginning with an isolated CK-MB elevation ≥3× URL within 24 h of CABG surgery. Above isolated 10× URL elevations, there appears to be a progressive increase in short-term (30 days) and longer-term mortality (1 year and over), which is independent of other evidence of MI.20,23,29 In most centres, CK-MB has now been replaced by the use of cardiac troponins, as the latter are more sensitive and specific for detecting PMI and Type 5 MI following CABG surgery.32,33 Hence, we have elected to not use isolated CK-MB elevations post-surgery to define prognostically significant PMI.
Table 3.
Major recent studies showing elevations in creatine kinase-MB fraction to be associated with mortality post-coronary artery bypass grafting surgery
| Study | Type of study and surgery | Number of patients | Cardiac biomarker (time) | Time from CABG when biomarker level taken | Major findings |
|---|---|---|---|---|---|
|
|
496 | CK-MB | 6,12,18 h |
|
|
|
2394 |
|
8, 12, 16, 24 h |
|
|
|
4911 | CK-MB | 24 h | >61 ug/L Relative Hazard 1.3 to 1.4 for late mortality (up to 6 years) |
| Brener et al.12 |
|
3812 | CK-MB | 24 h |
|
| Marso et al.22 |
|
3667 | CK-MB | Single measurement mean 15.2 h |
|
| Ramsay et al.23 |
|
800 | CK-MB |
|
|
| Engoren et al.24 |
|
1161 | CK-MB | 10–18 h | >8× URL HR 1.3 increased 1 yr mortality |
| Newall et al.7 |
|
2860 | CK-MB | Single value up to 24 h |
|
| Mahaffey et al.25 |
|
1406 | CK-MB | Single value up to 24 h |
|
| Muehlschlegel et al.26 |
|
545 | CK-MB | Daily from day 1 to 5 |
|
| Petaja et al.27 |
|
21 657 | CK-MB | Variable (peak or absolute value at various time points post-op) | CK-MB ≥5× URL –RR of short term mortality 3.69% (CI 2.17–6.26); RR of long term (6–60 m) mortality 2.66% (CI 1.95–3.63) |
| Vikenes et al.28 |
|
205 | CK-MB | 1–3, 4–8, 24, 48 and 72 h | CK-MB elevation ≥ 5× URL was associated with worst long term event free survival (median follow-up 92 mths). |
| Domanski et al.29 |
|
18 908 |
|
Single value < 24 h |
|
| Søraas et al.30 |
|
1350 |
|
7,20, 44 h |
|
| Farooq et al.31 SYNTAX trial substudy |
|
474 | CK-MB |
|
|
AUC, area under the curve; CABG, coronary artery bypass grafting; CMR, cardiac MRI; CK-MB, creatine kinase-MB fraction; d, day; ECG, electrocardiogram; ECHO, echocardiocardiogram; HR, hazards ratio; h, hour; LGE, late gadolinium enhancement; LV, left ventricle; MACE, major adverse cardiac events; MI, myocardial infarction; mth, month; ng, nanogram; ONBEAT, on-pump beating heart; CABG ONSTOP, on-pump CABG; OR, odds ratio; post-op, post-operative; PMI, perioperative myocardial injury; RR, relative risk; TEE, transoesophageal echocardiogram; cTnI, Troponin I; cTnT, Troponin T; UA, unstable angina; URL, upper reference limit; yr, year.
Figure 1.
Relationship between creatine kinase-MB fraction elevation post-coronary artery bypass graft surgery with relative risk of mortality at 30 days (adapted from meta-analysis by Domanski et al.29).
Isolated elevations in cTnT and cTnI and mortality post-coronary artery bypass graft surgery
Cardiac troponins have greater sensitivity and specificity for myocardial necrosis, when compared to CK-MB, and have been found to be superior to CK-MB in predicting mortality post-CABG surgery.30,34–37 However, the interpretation of isolated changes in cTn levels in the post-operative period, in the absence of ECG/angiographic or other imaging evidence of MI, can be quite challenging given the different cTn assays used, the introduction of high-sensitive assays for cTn, and the presence of renal dysfunction.
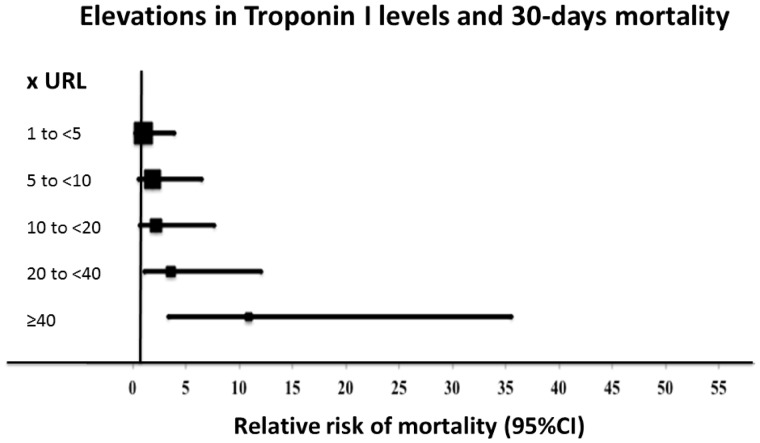
As with CK-MB, there appears to be a graded increase in short-term and long-term mortality following CABG surgery, based on the magnitude of post-operative cTnI or cTnT levels (Tables 4and5). Overall, there is a clear association between isolated elevations of cTnT ≥7× URL41 and cTnI levels ≥20× URL29,41 with significant increases in short-term (30 days) and long-term (one year and over) mortality after CABG surgery (Tables 4, 5 and Figure 2). Importantly, these findings were shown to be independent of ECG/angiography/imaging evidence of MI, confirming that isolated elevations of cTn following CABG surgery can predict mortality. The studies that have been used to define these thresholds used various generations of ‘standard’ cTnT and cTnI assays, and currently there is lack of sufficient data to accurately determine these thresholds for the high sensitivity-cTnT or cTnI assays. Hence, the above threshold for cTnT does not apply to the high-sensitive cTnT assay, and so for this assay, additional ECG and/or imaging evidence of MI appears to be required to identify those CABG patients at a higher risk of mortality when ≥10× URL hs-cTnT elevation is measured.8 The majority of studies have reported isolated elevations between 24 and 48 h post-surgery as being the most discriminatory for predicting clinical outcomes.27,30,36–38,42 Whether it is necessary to measure the AUC cTn elevation or whether a single time-point measurement of cTn is sufficient to predict post-surgical outcomes, is not clear. Recent evidence suggests that the AUC of high-sensitive cTnT may be a good surrogate for MI size.54
Table 4.
Major recent studies showing elevations in Troponin T to be associated with mortality post-coronary artery bypass grafting surgery
| Study | Type of study and surgery | Number of patients | Cardiac biomarker (time) | Time from CABG when biomarker level taken | Major findings |
|---|---|---|---|---|---|
| Januzzi et al.36 |
|
224 |
|
Immediately post-op, 6–8 h and 18–24 h |
|
| Lehrke et al.38 |
|
204 | cTnT | 4, 8 h then every day for 7 days |
|
| Kathiresan et al.37 |
|
136 |
|
Immediately post-op, 6–8 h and 18–24 h post-op |
|
| Nesher et al.39 |
|
1918 | cTnT | Single sample <24 h |
|
| Muehlschlegel et al.26 |
|
1013 | cTnT | Daily from day 1 to 5 |
|
| Mohammed et al.40 |
|
847 | cTnT | 6–8 and 18–24 h | A cTnT of < 1.60 (<160× URL) had good negative predictive value for poor 30 day outcomes (death or heart failure) |
| Petaja et al.41 |
|
2,547 | cTnT | <48 h post op | ≥7–16× URL: Short term mortality 3.2% vs. 0.5% for <7–16× URL elevation (RR 4.68–6.4); Long term mortality (12–28 mth) 16.1% vs. 2.3% (RR 5.7–10.09). (Pooled RR of mortality could not be calculated) |
| Søraas et al.30 |
|
1,350 |
|
7,20, 44 h post op |
|
| Wang et al.8 |
|
560 |
|
12–24 h after CABG | In a multivariate model >10× URL rise in hs-TNT + ECG/ECHO evidence of recent MI or regional ischaemia predicted 30 day (HR 4.9) and long-term mortality (median follow-up 1.8 years) (HR 3.4). > 10× URL rise in hs-cTnT was seen in 90% patients. |
| Gober et al.42 |
|
290 |
|
8,16 h post op | cTnT > 0.8 ng/mL (>80× URL) at 6–8 h was predictive of in hospital adverse outcomes and long term (4yr) mortality (OR 4.0). However, cTnT measured at 6–8 h was inferior to cTnT taken at 20 h in its prognostic ability. |
AUC, area under the curve; CABG, coronary artery bypass grafting; CMR, cardiac MRI; CK-MB, creatine kinase-MB fraction; d, day; ECG, electrocardiogram; ECHO, echocardiocardiogram; HR, hazards ratio; h, hour; LGE, late gadolinium enhancement; LV, left ventricle; MACE, major adverse cardiac events; MI, myocardial infarction; mth, month; ng, nanogram; ONBEAT, on-pump beating heart; CABG ONSTOP, on-pump CABG; OR, odds ratio; post-op, post-operative; PMI, perioperative myocardial injury; RR, relative risk; TEE, transoesophageal echocardiogram; cTnI, Troponin I; cTnT, Troponin T; UA, unstable angina; URL, upper reference limit; yr, year.
Table 5.
Major recent studies showing elevations in Troponin I to be associated with mortality post-coronary artery bypass grafting surgery
| Study | Type of study and surgery | Number of patients | Cardiac biomarker (time) | Other features | Major findings |
|---|---|---|---|---|---|
| Greenson et al.43 | Single centre prospective study; CABG or Aortic valve replacement | 100 |
|
Pre-op, 24 h and 48 h, then daily until discharge or 1 week | Peak cTnI > 60 ng/mL (> 120× URL) predictive of cardiac events up to 30 days post op |
| Holmvang et al.35 | Single centre prospective study, CABG only | 103 |
|
Every 2 h in first 20 h, 24, 30, 36 and 48 h, 72 and 98 h |
|
| Eigel et al.44 | Prospective single centre study; CABG only (Excluded MI within 7 days) | 540 | cTnI | Prior to induction of anaesthesia and at termination of CPB | cTnI level > 0.495 ng/L (> 9.9× URL for assay) measured at the end of CPB was predictive of in-hospital adverse outcomes (MI/death) |
| Lasocki et al.45 | Single centre prospective study; CABG or valve surgery (Acute MI < 7 days were excluded) | 502 |
|
20 h post-op |
|
| Thielmann et al.46 | Single centre prospective study: CABG only | 2,078 | cTnI | 1, 6, 12,24 h post op |
|
| Paparella et al.47 | Prospective Single centre study; CABG only (Patients with UA/MI < 7 days included) | 230 | cTnI | Pre-op, 1,6,12,24 and 36 h post-op, daily from day 2 to 7 |
|
| Onorati et al.9 | Prospective single centre study; CABG only | 776 |
|
Pre-op and 12, 24, 48 and 72 h post-op | cTnI >3.1 μg/L (> 310× URL) at 12 h predicted increased in-hospital and 12 month mortality; Additional ECG and ECHO criteria of MI predicted worst outcome |
| Thielmann et al.31,48 |
|
94 |
|
Pre-op, 1, 6, 12, 24, 36 and 48 h post-op | cTnI was the best discriminator between PMI ′in general′ and ′inherent′ release of cTnI after CABG with a cut-off value of 10.5 ng/mL (> 21× URL) and between graft-related and non-graft-related PMI with a cut-off value of 35.5 ng/mL (>71× URL). CK-MB level and ECG changes/TEE could not differentiate between those with or without graft failure. |
| Croal et al.49 |
|
1365 |
|
2 and 24 h |
|
| Provenchère et al.50 |
|
92 | cTnI | 20 h post op | cTnI levels were not predictive of 1 year mortality in a multivariate model. |
| Fellahi et al.51 |
|
202 | cTnI | Per-op and 24 h post-op |
|
| Adabag et al.34 |
|
1186 |
|
Ever 8 h for 24 h post-op, longer if no peak in 24 h | cTnI level independently associated with operative (30 day) mortality; CK-MB had a weaker association with operative mortality |
| Muehlschlegel et al.26 |
|
1013 | cTnI | Daily from day 1 to 5 |
|
| Petaja et al.41 |
|
2348–3271 | cTnI | Up to 7 days post op |
|
| Hashemzadeh et al.52 |
|
320 | cTnI | Immediately and 20 h post-op | 20 h post-op cTnI had better prognostic value than immediate post-op levels. 20 h cTnI level was an independent predictor of in-hospital mortality above a value of 14 ng/mL (>10× URL) |
| Van Geene et al.53 | Registry retrospective analysis;CABG and/or valve surgery | 938 (Separate validation subset, n = 579) | cTnI | 1 h post-op | 1 h post-op cTn values correlated with hospital mortality with the best cut-off value of 4.25 μ/L (Type of assay and URL for assay not known) |
| Domanski et al.29 |
|
18,908 | cTnI | <24 h post op |
|
| Ranasinghe et al.27 | Retrospective analysis of 2 prospective randomized controlled clinical trials | 440 | cTnI | 6, 12, 24, 48, 72 h post-op |
|
AUC, area under the curve; CABG, coronary artery bypass grafting; CMR, cardiac MRI; CK-MB, creatine kinase-MB fraction; d, day; ECG, electrocardiogram; ECHO, echocardiocardiogram; HR, hazards ratio; h, hour; LGE, late gadolinium enhancement; LV, left ventricle; MACE, major adverse cardiac events; MI, myocardial infarction; mth, month; ng, nanogram; ONBEAT, on-pump beating heart; CABG ONSTOP, on-pump CABG; OR, odds ratio; post-op, post-operative; PMI, perioperative myocardial injury; RR, relative risk; TEE, transoesophageal echocardiogram; cTnI, Troponin I; cTnT, Troponin T; UA, unstable angina; URL, upper reference limit; yr, year.
Figure 2.
Relationship between Troponin I elevation post-coronary artery bypass graft surgery with relative risk of mortality at 30 days (adapted from meta-analysis by Domanski et al.29).
In summary, we recommend, that for patients with a pre-operative cTn <1× URL, isolated elevations of ‘standard’ cTn assays (cTnT ≥7× URL and cTnI ≥20× URL) within the 48 h post-operative period (in the absence of ECG/angiographic or other imaging evidence of MI), may be indicative of prognostically significant PMI, and require further clinical evaluation to determine whether there is evidence for Type 5 MI. This is particularly so if there is additional clinical evidence for MI such as disproportionate chest pain, unusual ECG changes or new regional wall motion abnormalities on echocardiography in a territory that is dependent on a graft, or dependent on a major ungrafted vessel. However, these threshold values for cTnT and cTnI in defining prognostically significant PMI, may vary from site to site and the actual cTn assay used, and should be established for individual sites. Also, it is important to note that isolated elevations in cTn below these thresholds may still be clinically significant, but their impact on post-CABG mortality appears to be small. For patients with additional ECG/angiography/imaging evidence of MI, an elevation of cTnT or cTnI ≥10× URL should be used to define Type 5 MI, as per the 3rd Universal Definition of MI. For the newest generation of high-sensitive cTn assays, the threshold level above which clinical outcomes post-surgery can be predicted remains to be determined.
Other biomarkers for quantifying peri-operative myocardial injury
As mentioned above, cTn elevations between 24 and 48 h have been most clearly shown to correlate with mortality post-CABG surgery. However, this may be too late to identify prognostically significant PMI or Type 5 MI, as interventions at this stage may fail to salvage a substantial volume of myocardium at risk. Also, cTn elevation in this early time period (<24 h) may be due to non-ischaemic causes, making it a less reliable marker of regional ischaemia in the first 24 h.
Newer cardiac biomarkers are therefore needed to improve the diagnosis of PMI following CABG surgery with respect to earlier diagnosis, and improving specificity for regional ischaemia, thereby allowing prompt implementation of medical or surgical treatment and to maximise myocardial salvage. Myoglobin, heart-type fatty acid–binding protein,55,56 copeptin,57 microRNAs (miR-499 and miR-1),58,59 and cardiac myosin-binding protein C60 have been shown to be associated with PMI following CABG surgery. Some of these are not specific for myocardial necrosis, but they seem to provide additional power in combination with conventional cardiac biomarkers for detecting PMI following CABG surgery. Interestingly, new peptides have been identified via a phage display peptide library screen that might be useful in the future to predict PMI after CABG surgery.49 Although these new biomarkers seem to be extremely sensitive for detecting PMI, technological improvements for early detection, and large validation cohorts are needed to speed-up their clinical application.
Role of electrocardiogram for detecting type 5 myocardial infarction following coronary artery bypass graft surgery
The appearance of new Q waves or LBBB on ECG following CABG surgery remain part of the diagnostic criteria for Type 5 MI.5 Using ECG, the incidence of Type 5 MI is in the range of 5 to 14%. New ST-segment elevation or depression may indicate ongoing regional ischaemia, and warrant further diagnostic work-up. However, in many post-surgical patients the ECG may not be interpretable, and ECG changes may be non-specific or transient. A number of clinical studies have found that ECG changes alone are not always predictive of poorer outcomes following CABG surgery,23,26,49 although the additional presence of ECG evidence of PMI with an elevation in cTn appears to be associated with significantly worse outcomes.8,9 Interestingly, a number of studies have shown that many cases of Type 5 MI detected by CMR occur in the absence of new ECG changes (Q waves or LBBB), illustrating the difficulties in relying on ECG changes to detect Type 5 MI.15,61
Role of cardiac imaging for detecting type 5 MI following coronary artery bypass graft surgery
Although several cardiac imaging modalities exist for detecting new loss of viable myocardium or new regional wall motion abnormalities following CABG surgery, only coronary angiography allows for immediate final decision making (conservative, vs. redo CABG vs. percutaneous coronary intervention).
Echocardiography to detect type 5 myocardial infarction following coronary artery bypass graft surgery
Echocardiography is the most practical imaging modality for detecting new RWMA following surgery.13 However, image quality can be reduced after CABG surgery, due to the presence of pleural or pericardial effusions, inflammation or assisted ventilation, and in these cases transoesophageal echocardiography may be preferable.62 Endocardial visualisation might also be enhanced by the use of contrast agents, especially when 2 or more myocardial segments are not visualised by standard echocardiography.63 Moreover, detection of RWMA might be improved by more advanced echocardiography imaging modalities such as tissue Doppler imaging or speckle tracking.64 However, a large retrospective analysis found that RWMA detected by TEE were not able to predict those patients with graft failure as documented by coronary angiography.65 One major limitation of echocardiography is that new RWMA may reflect conditions not necessarily associated with Type 5 MI and include acute ischaemia (without infarction), stunning or hibernation, and non-ischaemic conditions, such as inflammation.
Myocardial nuclear imaging and cardiac computed tomography to detect type 5 myocardial infarction following coronary artery bypass graft surgery
Radionuclide single-photon emission computed tomography (SPECT) and positron emission tomography (PET) imaging can allow the direct assessment and quantification of myocardial viability before and after CABG surgery,66,67 although given the relatively low spatial resolution of this imaging technique, small areas of non-viable myocardium (especially subendocardial MI), which are commonly found with Type 5 MI, may be missed. Other radionuclide imaging approaches are currently under intense investigation, and will likely be tested in the next few years.68
New loss of viable myocardium may be also visualised by cardiac CT.69 Multi-slice CT coronary angiography is another useful non-invasive imaging modality that can be utilized to evaluate graft patency following CABG surgery.10,11,70,71 However, the radiation dose and the risks of cumulative ionising radiation need to be weighed against the obvious advantages of an early and accurate diagnosis.72
Cardiac magnetic resonance to detect type 5 myocardial infarction following coronary artery bypass graft surgery
Cardiovascular magnetic resonance (CMR) imaging is a well validated imaging technique with high spatial resolution, for the accurate assessment of both myocardial function and viability, which has proven to be an excellent tool in the diagnosis of Type 5 MI.73 The presence of new areas of late gadolinium enhancement (LGE), on CMR performed in the first couple of weeks following CABG surgery can detect the presence of new non-viable myocardial tissue required for diagnosing Type 5 MI (see Table 6). These clinical studies suggest that Type 5 MI occurs in 20–30% of all patients undergoing elective CABG surgery. Interestingly, the pattern of LGE observed on CMR post-CABG surgery reflects the multi-factorial aetiology of Type 5 MI with examples of transmural infarction (suggesting native artery or graft failure), subendocardial infarction (suggesting inadequate cardioprotection), and patchy areas of infarction (suggesting coronary microembolisation or non-ischaemic myocardial necrosis).16,17,77
Table 6.
Major studies using cardiac magnetic resonance to assess Type 5 myocardial infarction following coronary artery bypass graft surgery
| Study | Number of patients | Type of surgery | Cardiac biomarkers | Incidence of MI (LGE on CMR) | Major findings |
|---|---|---|---|---|---|
| Steuer et al.17 | 23 | CABG |
|
|
|
| Selvanayagam et al.15 | 53 |
|
|
|
|
| Pegg et al.16,74 | 40 |
|
|
|
|
| Lim et al.61 | 28 | CABG |
|
9/28 (32%) CMR day 7 (4–10) | cTnI > 83.3× URL at 1 h and peak cTnI/CK-MB at 24 h correlated with new LGEcTnI better than CK-MB in predicting new LGE at both 1 and 24 hNone of the 9 patients with new LGE had Q waves on ECGPre-op CMR performed |
| van Gaal et al.75 | 32 | CABG |
|
|
|
| Alam et al.76 | 69 |
|
|
|
|
| Hueb et al.14 | 136 |
|
|
|
|
AUC, area under the curve; CABG coronary artery bypass grafting; CMR, cardiac MRI; CK-MB, creatine kinase-MB fraction; d, day; ECG, electrocardiogram; ECHO, echocardiocardiogram; HR, hazards ratio; h, hour; LGE, late gadolinium enhancement; LV, left ventricle; MACE, major adverse cardiac events; MI, myocardial infarction; mth, month; ng, nanogram; ONBEAT, on-pump beating heart; CABG ONSTOP, on-pump CABG; OR, odds ratio; post-op, post-operative; PMI, perioperative myocardial injury; RR, relative risk; TEE, transoesophageal echocardiogram; cTnI, Troponin I; cTnT, Troponin T; UA, unstable angina; URL, upper reference limit; yr, year.
Overall, there is a good correlation between elevations in cardiac biomarkers post-surgery and new LGE mass quantified by CMR (see Table 6). However, in some patients with absence of LGE on CMR, there was still a significant elevation in AUC cTnI, suggesting that not all post-operative cTnI release represents irreversible myocardial injury,15 or that the tissue loss was too small to be detected by CMR.78 Therefore, the prognostic significance of post-surgical elevations in cardiac biomarkers in the absence of MI on LGE-CMR remains to be determined. One study has demonstrated that a single cTnI value at 1 h post-surgery accurately predicted new LGE on CMR, increasing the clinical utility of measuring cardiac biomarkers and implementing a change in management to avoid future complications.61
In most patients with LGE on CMR, in-hospital patient management was not changed. In one study, a rise in both CK-MB and cTnI to >5× URL in patients with new LGE on CMR had an inverse linear relation with lack of improvement in global left LV function post-CABG surgery, and a pooled analysis of percutaneous coronary intervention (PCI) and CABG patients suggested that new LGE on CMR increased by three-fold the risk of MACE- death, non-fatal MI, admission to hospital for unstable angina or worsening heart failure, or occurrence of ventricular arrhythmia (defined as ventricular fibrillation or sustained ventricular tachycardia).79 At least one clinical study76 has used the mass of LGE on CMR as a surrogate endpoint to assess the cardioprotective efficacy of a novel therapy during CABG surgery, although in this particular study the anti-inflammatory agent, Elafin, failed to reduce the mass of LGE (Table 6).
In summary, LGE-CMR post-CABG surgery has provided important insights into the pathophysiology of Type 5 MI. From a clinical perspective however, its utility for diagnosing Type 5 MI is limited given that it is not widely available, and may be impractical in the early post-operative phase.
Managing the patient with peri-operative myocardial injury and type 5 myocardial infarction
There is limited evidence from clinical studies comparing strategies on how best to manage either prognostically significant PMI or Type 5 MI following CABG surgery. The key issue in the immediate post-operative period is to identify patients with regional ischaemia due to graft-failure or an acute coronary event in the native coronaries, as this group of patients may benefit from urgent revascularisation.80 Graft failure post-CABG surgery is associated with higher mortality (∼15%),81 and is potentially amenable to intervention (PCI or redo-CABG).80 Early intervention in these patients may reduce the extent of Type 5 MI, thereby improving clinical outcomes.81 For non-graft-related PMI, there is currently no specific therapy available, only general supportive measures.
General management of peri-operative myocardial injury and type 5 myocardial infarction
General supportive measures apply both to graft-related as well as non-graft-related PMI and Type 5 MI. It is important to note that while there are several risk-stratification models to determine the risk of mortality in the patients undergoing CABG surgery based on pre-operative risk factors, such as EuroSCORE, EuroSCORE II, and STS score, there are currently no validated prediction models to determine which patients are at high-risk of PMI or Type 5 MI following CABG surgery. If patients at high risk of PMI or Type 5 MI can be identified, customised management pathways comprising more aggressive monitoring, investigations and/or treatment approaches may result in improved clinical outcomes. The ultimate treatment would be urgent coronary revascularisation, either interventional or surgical.80
Non-graft-related PMI is most often related to inappropriate myocardial protection, excessive surgical manipulation, inflammation, and air or plaque embolisation.82 Treatment of anaemia, pain and tachycardia can increase coronary blood flow and/or decrease myocardial oxygen consumption, thereby limiting Type 2 MI. Observational studies have shown an association between transfusion and worse outcome, including infections, ischaemic complications, and mortality.83,84 In contrast, a recent multi-centre randomised trial comparing a liberal (haemoglobin, Hb <9 g/dL) vs. a restrictive (Hb <7.5 g/dL) transfusion threshold in CABG surgery patients, showed a lower 30-day mortality in the liberal group, although it was not the primary outcome of the study.85 The incidence of PMI was similar in the two groups, but peak values of cardiac biomarkers were not reported. Two recent large multicentre randomised controlled trials showed no benefit of routine intra-operative high dose dexamethasone or methylprednisolone on major adverse events, and its use did not reduce the incidence of Type 5 MI.86,87 Beta-blockers can be used to treat tachycardia, diminish myocardial oxygen consumption and prevent arrhythmias, and are recommended prior to and early after CABG surgery in practice guidelines,88 however, hypotension due to systolic dysfunction or PMI may limit their use.
In cases of overt heart failure, pharmacological haemodynamic optimisation and/or mechanical support may be indicated. Due to safety concerns, inotropes are reserved for patients with inadequate peripheral tissue perfusion or hypotension. The β-agonist dobutamine, phosphodiesterase inhibitors like milrinone or enoximone, and the calcium sensitiser levosimendan can all be used to treat postoperative refractory low cardiac output syndrome and decompensated heart failure.
In patients with insufficient coronary perfusion (before surgery or insufficient graft perfusion), the intra-aortic balloon pump (IABP) may provide improvement of haemodynamics while underlying cause(s) of instability can be addressed and is still being used in high risk patients or in patients with difficulties weaning off cardiopulmonary bypass.89 A recent meta-analysis showed benefit of a pre-operative intra-aortic balloon pump insertion in patients undergoing CABG surgery on 30-day mortality, and this may be considered in selected unstable high-risk patient preoperatively.90 Advanced mechanical support may be indicated in severe cardiac failure, where inotropes, vasopressors and IABP fail to restore adequate output. Extracorporeal Life Support (ECLS or ECMO) may be a bridge to recovery of cardiac function, or bridge to decisions about further long-term mechanical support (LVAD) and future transplantation. Unfortunately, survival in ECLS treated patients is only 20–40%.91
Managing the patient with suspected graft-related failure
The incidence of early graft failure is ∼3%,92 and the rate of graft occlusion before discharge varies from 3 to 12% for vein grafts (3 to 4% for radial arteries and 1 to 2.5% for internal mammary arteries48). It is often difficult to distinguish graft-related from non-graft-related PMI and Type 5 MI, and surgeons rely on elevations in cardiac biomarkers, unexplained low cardiac output syndrome (LCOS), persistent ischaemic ECG changes, recurrent ventricular tachycardia and fibrillation, and new echocardiographic RWMAs to detect graft failure following CABG surgery. A variety of patient symptoms and objective findings should raise suspicion of regional ischaemia due to early graft failure, and trigger prompt evaluation with an ECG, measurement of cardiac biomarkers, coronary angiography or other appropriate cardiac imaging. These include the presence of typical or atypical chest pain, unexplained shortness of breath, haemodynamic instability as well as difficulty in weaning off cardiopulmonary bypass, refractory arrhythmia or persistent circulatory failure. Unfortunately, all of the above can be present following CABG surgery, even in the absence of regional ischaemia, hence none of these findings are sensitive or specific enough in isolation to accurately identify the presence of regional ischaemia, and so the appropriate diagnostic or management pathway should be determined in each patient taking the whole clinical picture in consideration. Equally, regional ischaemia may be present even in the absence of the above findings. The assessment of regional ischaemia following CABG surgery remains a considerable challenge for managing PMI and Type 5 MI.
The main cause of early graft failure post CABG surgery is graft occlusion but other causes include graft kinking and anastomotic stenosis.46 A graft-related cause is identified in 60–80% of coronary angiograms performed for this indication, and consecutive re-revascularisation is performed in 50–70% of graft-related Type 5 MI.81,92–95 However, in one study, 24–35% of patients undergoing coronary angiography after CABG for early graft dysfunction had patent grafts.93 One retrospective series found that an urgent post-CABG coronary angiogram was required in 1.8% patients, and more than half of these patients needed re-intervention, and, in spite of this, had high mortality.96 In multi-variate analysis, younger patients, female patients, smaller patients, and patients receiving a combined arterial and venous revascularisation were at a higher risk for an unplanned post-surgical coronary angiogram.96
When detected, potentially correctable abnormalities included early graft thrombosis, anastomotic stenosis, bypass kinks, overstretching or tension, significant spasm or incomplete revascularization. Compared with native coronary PCI, bypass graft PCI has been shown to be independently associated with higher in-hospital mortality.97 In the CathPCI registry, patients undergoing bypass graft PCI more frequently required intra-aortic balloon pump counter pulsation, longer fluoroscopy time, and larger amount of contrast medium; and less frequently achieved TIMI flow grade 3 post-stenting, were more likely to receive blood transfusions, and had higher rates of post-procedural complications and in-hospital mortality.97 In one of the few studies that investigated the appropriate treatment for patients with early graft failure following CABG surgery, the major findings were that: (i) patients with prompt re-intervention for early graft failure after CABG surgery had a higher number of graft/patient failure than in patients managed conservatively; (ii) even with more graft failure per patient, there was a trend towards smaller size of MI in the early aggressive re-intervention group than in the conservative group; and (iii) coronary angiography was a good tool to discriminate the aetiology of postoperative infarction (graft-related or non-graft-related).81
Early graft failure has been shown to be associated with a higher elevations in cTnI (about >45× URL at 12 h and >70× URL elevation at 24 h for cTnI).35,46,48 However, it is important to appreciate that there may be a significant overlap between patients with or without graft failure even at this level of biomarker elevation.35,46,48 Another important finding from these studies is that ECG and/or imaging evidence of MI did not appear to reliably identify those with early graft failure following surgery. Therefore, high cTnI elevations in the post-surgical period (>45× URL at 12 h and >70× URL elevation at 24 h), even in the absence of ECG and/or imaging evidence of MI, should raise the suspicion of early graft failure. However, it is important to have earlier markers of graft failure to allow the implementation of a change in management in order to limit PMI and improve clinical outcomes post-CABG surgery. In this regard, some studies have shown that post-operative cTn levels at 1 h post-surgery may be used to predict Type 5 MI on CMR, but the role of this measurement in detecting early graft failure has not been investigated.61 The detection of graft dysfunction by intraoperative transit time flow measurement (TTFM) within the graft may allow early detection of graft failure and thereby provide a potential strategy for limiting PMI and Type 5 MI.98,99 In addition, this approach has been shown to predict graft failure at 1 month100 and 6 months post-CABG surgery.101
In summary, strategies aimed at earlier identification of patients with significant on-going regional ischaemia could salvage viable myocardium. Anaesthesiologists and intensivists should be involved in this process. Early coronary angiography and on-site consultation of an interventional cardiologist and cardiac surgeon should result in a decision on the management of the individual patient, taking into account the extent of ischaemia, coronary anatomy, and comorbidities.
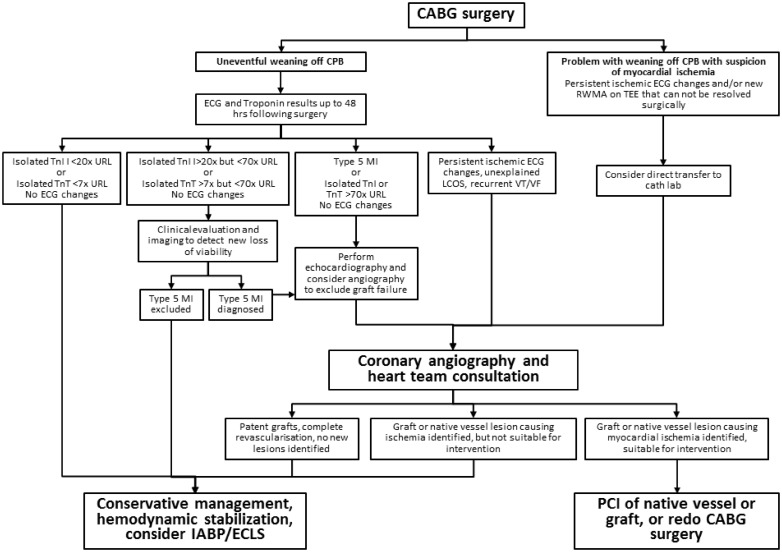
We present a management algorithm (Figure 3) providing guidance on when to perform coronary angiography for suspected PMI or Type 5 MI. It proposes emergent coronary angiography in case of clear signs of acute myocardial ischaemia or unexplained haemodynamic compromise immediately post-surgery, and urgent coronary angiography in case of recurrent ventricular arrhythmias, unexplained LCOS or persistent ischaemic ECG changes. Furthermore, high cTn elevations in the post-surgical period (such as cTnI >45× URL at 12 h and >70× URL elevation at 24 h) even in the absence of ECG and/or imaging evidence of MI, should raise the suspicion of early graft failure. This proposed algorithm aligns well with the current ESC/EACTS guidelines on myocardial revascularization (2014), which support emergency PCI in early post-operative graft failure to limit the extent of myocardial injury.80 Additionally, the current ESC/EACTS guidelines favour PCI to the body of the native vessel or IMA graft while avoiding PCI to an occluded vein graft or graft anastomosis site and reserve re-do surgery to patients with coronary anatomy unsuitable for PCI.80 Future studies aiming at earlier and more precise identification of patients with suspected graft-related ischaemia should allow one to refine this algorithm further.
Figure 3.
Proposed algorithm for managing patients with possible peri-operative myocardial injury and Type 5 myocardial infarction following coronary artery bypass graft surgery. CPB, cardiopulmonary bypass; RWMA, regional wall motion abnormality; TEE, transeophageal echocardiography; LCOS, low-cardiac output syndrome; VT, ventricular tachycardia; VF, ventricular fibrillation; IABP, intra-aortic balloon pulsation; ECLS, Extracorporeal Life Support; URL, upper reference limit.
Decision making following coronary angiography post-surgery
Once coronary angiography following CABG in cases of suspected graft failure, the treatment strategy (conservative vs. revascularisation) depends on many factors, and the decision needs to be made in close consultation with the Heart Team (intensivists, surgeons and cardiologists). These factors include the coronary anatomy, graft occlusion vs. native vessel occlusion, extent of myocardial ischaemia, extent of viable myocardium, clinical symptoms, haemodynamic status and inotrope support, and age and co-morbidities.
A conservative strategy should be considered if:
All grafts are patent.
There are no lesions in native coronary arteries potentially involved in post-operative myocardial ischaemia.
The graft or native coronary artery occlusion was identified late, in which case consider viability assessment first.
In cases of venous graft occlusion anastomosed on non-major left anterior descending (LAD) coronary artery with no lesion suitable for PCI on the related native coronary artery.
Revascularisation by PCI should be considered if:
There is early graft dysfunction.
There are suitable lesions in native coronary arteries involved in the post-operative myocardial ischaemia.
In the presence of severe cardiogenic shock emergency PCI or ECLS should be considered.
If PCI is chosen there are certain risks and technical challenges. PCI should be performed on lesions in the native vessels supplying the ischaemic region, and should be avoided in the occluded vein graft or graft anastomosis site, except when lesions on the native vessels are not suitable for PCI.
Revascularization by redo CABG surgery should be considered if:
The coronary anatomy is unsuitable for PCI
There is involvement of a large extent of ischaemia (e.g. LAD territory).
There is failure of LIMA or a Y-graft to the left system.
If redo CABG is being considered there are certain risk and technical challenges. Recurring cardiopulmonary bypass (CPB) with cardioplegic arrest may intensify acute myocardial ischaemia-reperfusion injury, already sustained, and a period of recovery using ECLS, may be beneficial in the initial 24–48 h after treatment. Redo CABG surgery may also be considered using ‘beating heart surgery’ (without cardiac arrest and cardioplegia) under cardiopulmonary bypass support, in order to limit additional acute myocardial ischaemia-reperfusion injury.
Using peri-operative myocardial injury and type 5 myocardial infarction to assess the cardioprotective efficacy of novel therapies in the setting of coronary artery bypass graft surgery
Cardioprotective strategies such as ischaemic preconditioning (IPC), ischaemic post-conditioning (IPost), remote ischaemic preconditioning (RIPC), and a number of drugs including volatile anesthetics which recruit the signal transduction pathways underlying conditioning, have been shown to attenuate myocardial injury following acute ischaemia-reperfusion injury.102–108 Ischaemic cardioplegic arrest on cardiopulmonary bypass with subsequent reperfusion was therefore considered an ideal and well controlled clinical setting to translate findings from animal experiments to humans. In fact, a number of smaller studies have reported reduced MI size with IPC, IPost, and RIPC (for review see reference 102), and cyclosporine A.109,110 These studies used biomarker release (CK, CK-MB, and cTn) to quantify PMI. It is important to note that the majority of studies have measured the magnitude of PMI to assess the cardioprotective efficacy of novel therapies, and did not investigate whether the new intervention was able to reduce the incidence of Type 5 MI or mortality. Two moderately sized trials also reported improved clinical outcomes with RIPC at short-111 or more long-term112 as a secondary endpoints.
In contrast to these encouraging phase II a studies, two recent larger phase III trials assessing RIPC neither confirmed reduced biomarker (cTnT or cTnI) release nor improved clinical outcomes during hospitalization113 or at one year follow-up.114 In both these neutral trials, less than 50% of patients had only CABG surgery, and the others had either additional or only valvular surgery. Valvular surgery causes greater traumatic injury than CABG, and the contribution of trauma to total biomarker release may have diluted a potential cardioprotective effect of remote ischaemic preconditioning. In contrast to these larger trials, the original positive phase II trials had only recruited patients undergoing CABG surgery.112,115 There are also other causes of biomarker release such as bypass graft failure48 or microembolization of atherothrombotic debris,77 which are not associated with subsequent reperfusion injury and from which, therefore, no protection by conditioning or drugs is expected. More disconcerting than the lack of reduction in biomarker release is the lack of improved clinical outcomes, which retrospectively also confirms the lack of reduced biomarker release in the two recent phase III trials.116 Therefore, the search for novel biomarkers specific to cardioprotection by ischaemic conditioning such as protectomiRs117 is of particular interest.
Recommendations for defining and managing prognostically significant peri-operative myocardial injury
In this ESC Joint WGs Position paper, we have provided recommendations for defining prognostically significant PMI (Table 7). In summary, we would recommend that isolated elevations in cTnT ≥7× URL and/or cTnI ≥20× URL in the 48-h post-operative period may indicate the presence of prognostically significant PMI, and should prompt clinical evaluation to exclude Type 5 MI. Where ECG/angiography/imaging evidence of MI is available, lower levels of biomarker elevation (cTn x10 URL) should be considered for diagnosing prognostically significant PMI, as per the Universal MI definition.
Table 7.
Overview of definitions for peri-operative myocardial injury and Type 5 myocardial infarction
| Diagnostic criteria | Cardiac biomarker | Threshold for isolated elevation in cardiac biomarker (with no ECG or imaging changes of MI) | Threshold for elevation in cardiac biomarker with ECG and imaging changes of MI |
|---|---|---|---|
|
Troponins only | N/A | ≥10× URL |
|
Troponins only | <10× URL | N/A |
|
CK-MB and Troponins |
|
|
|
Troponins only |
|
≥10× URL |
URL, upper reference limit.
We have also proposed an algorithm for managing CABG patients with or without suspected graft failure based on elevations in cardiac biomarkers (Figure 3). Isolated elevations in cTn (>70× URL in the 48 h post-operative period), even in the absence of any other feature of MI, may be indicative of graft failure and warrant further investigation with coronary angiography and re-revascularization by PCI or CABG surgery if indicated. More studies are needed to establish thresholds, especially for hs-cTnT elevations, which can be used in conjunction with clinical features and imaging findings, to predict those patients with regional ischaemia or graft failure. Furthermore, studies are required to better define the role of coronary angiography post-CABG surgery to detect early graft failure.
Funding
European Cooperation in Science and Technology (COST EU-ROS) and Hungarian Scientific Research Fund (OTKA K 109737 and ANN 107803) to P.F; British Heart Foundation (grant number FS/10/039/28270), the Rosetrees Trust, and National Institute for Health Research University College London Hospitals Biomedical Research Centre to D.J.H.; Italian Ministry of Health (GR-2009-1596220) and the Italian Ministry of University (RBFR124FEN) to C.P.; Netherlands Organization for Health Research and Development (ZonMW Veni 91612147) and Netherlands Heart Foundation (Dekker 2013T056) to L.V.L.; German Research Foundation (He 1320/18-3; SFB 1116 B8 to G.H.).
Conflict of interest: D.H., M.T., V.S., J.B., G.K., R.M., J.S., F.P., P.K., P.M., N.A., S.L., C.P., G.B., J.O., U.F., M.C., U.F., J.F.O., C.M., L.V.L., M.S.N. have no disclosures. G.H. served as consultant for Servier. P.F. is an owner of Pharmahungary Group, a group of R&D companies.
References
- 1. Cornwell LD, Omer S, Rosengart T, Holman WL, Bakaeen FG.. Changes over time in risk profiles of patients who undergo coronary artery bypass graft surgery: the Veterans Affairs Surgical Quality Improvement Program (VASQIP). JAMA Surg 2015;150:308–315. [DOI] [PubMed] [Google Scholar]
- 2. ElBardissi AW, Aranki SF, Sheng S, O'brien SM, Greenberg CC, Gammie JS.. Trends in isolated coronary artery bypass grafting: an analysis of the Society of Thoracic Surgeons adult cardiac surgery database. J Thorac Cardiovasc Surg 2012;143:273–281. [DOI] [PubMed] [Google Scholar]
- 3. Thorsteinsson K, Fonager K, Merie C, Gislason G, Kober L, Torp-Pedersen C, Mortensen RN, Andreasen JJ.. Age-dependent trends in postoperative mortality and preoperative comorbidity in isolated coronary artery bypass surgery: a nationwide studydagger. Eur J Cardiothorac Surg 2016;49:391–397. [DOI] [PubMed] [Google Scholar]
- 4. Hirsch WS, Ledley GS, Kotler MN.. Acute ischemic syndromes following coronary artery bypass graft surgery. Clin Cardiol 1998;21:625–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. White H, Thygesen K, Alpert JS, Jaffe A.. Universal MI definition update for cardiovascular disease. Curr Cardiol Rep 2014;16:492.. [DOI] [PubMed] [Google Scholar]
- 6. Yau JM, Alexander JH, Hafley G, Mahaffey KW, Mack MJ, Kouchoukos N, Goyal A, Peterson ED, Gibson CM, Califf RM, Harrington RA, Ferguson TB, Investigators PI.. Impact of perioperative myocardial infarction on angiographic and clinical outcomes following coronary artery bypass grafting (from PRoject of Ex-vivo Vein graft ENgineering via Transfection [PREVENT] IV). Am J Cardiol 2008;102:546–551. [DOI] [PubMed] [Google Scholar]
- 7. Newall N, Oo AY, Palmer ND, Grayson AD, Hine TJ, Stables RH, Fabri BM, Ramsdale DR.. Intermediate and high peri-operative cardiac enzyme release following isolated coronary artery bypass surgery are independently associated with higher one-year mortality. J Cardiothorac Surg 2006;1:20.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wang TK, Stewart RA, Ramanathan T, Kang N, Gamble G, White HD.. Diagnosis of MI after CABG with high-sensitivity troponin T and new ECG or echocardiogram changes: relationship with mortality and validation of the Universal Definition of MI. Eur Heart J Acute Cardiovasc Care 2013;2:323–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Onorati F, De Feo M, Mastroroberto P, Cristodoro L, Pezzo F, Renzulli A, Cotrufo M.. Determinants and prognosis of myocardial damage after coronary artery bypass grafting. Ann Thorac Surg 2005;79:837–845. [DOI] [PubMed] [Google Scholar]
- 10. Bassiri H, Nematollahi A, Noohi F, Hashemi J, Motevali M, Givtaj N, Raissi K, Haghjoo M.. Coronary graft patency after perioperative myocardial infarction: a study with multislice computed tomography. Interact Cardiovasc Thorac Surg 2011;12:596–599. [DOI] [PubMed] [Google Scholar]
- 11. Bassiri HA, Salari F, Noohi F, Motevali M, Abdi S, Givtaj N, Raissi K, Haghjoo M.. Predictors of early graft patency following coronary artery bypass surgery. Cardiol J 2010;17:344–348. [PubMed] [Google Scholar]
- 12. Brener SJ, Lytle BW, Schneider JP, Ellis SG, Topol EJ.. Association between CK-MB elevation after percutaneous or surgical revascularization and three-year mortality. J Am Coll Cardiol 2002;40:1961–1967. [DOI] [PubMed] [Google Scholar]
- 13. Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, Writing Group on the Joint ESCAAHAWHFTFftUDoMI, Thygesen K, Alpert JS, White HD, Jaffe AS, Katus HA, Apple FS, Lindahl B, Morrow DA, Chaitman BA, Clemmensen PM, Johanson P, Hod H, Underwood R, Bax JJ, Bonow RO, Pinto F, Gibbons RJ, Fox KA, Atar D, Newby LK, Galvani M, Hamm CW, Uretsky BF, Steg PG, Wijns W, Bassand JP, Menasche P, Ravkilde J, Ohman EM, Antman EM, Wallentin LC, Armstrong PW, Simoons ML, Januzzi JL, Nieminen MS, Gheorghiade M, Filippatos G, Luepker RV, Fortmann SP, Rosamond WD, Levy D, Wood D, Smith SC, Hu D, Lopez-Sendon JL, Robertson RM, Weaver D, Tendera M, Bove AA, Parkhomenko AN, Vasilieva EJ, Mendis S, Guidelines ESCCfP.. Third universal definition of myocardial infarction. Eur Heart J 2012;33:2551–2567. [DOI] [PubMed] [Google Scholar]
- 14. Hueb W, Gersh BJ, Alves da Costa LM, Costa Oikawa FT, Vieira de Melo RM, Rezende PC, Garzillo CL, Lima EG, Nomura CH, Villa AV, Hueb AC, Cassaro Strunz CM, Favarato D, Takiuti ME, de Albuquerque CP, Ribeiro da Silva EE, Franchini Ramires JA, Kalil Filho R.. Accuracy of myocardial biomarkers in the diagnosis of myocardial infarction after revascularization as assessed by cardiac resonance: the Medicine, Angioplasty, Surgery Study V (MASS-V) Trial. Ann Thorac Surg 2016;101:2202–2208. [DOI] [PubMed] [Google Scholar]
- 15. Selvanayagam JB, Kardos A, Francis JM, Wiesmann F, Petersen SE, Taggart DP, Neubauer S.. Value of delayed-enhancement cardiovascular magnetic resonance imaging in predicting myocardial viability after surgical revascularization. Circulation 2004;110:1535–1541. [DOI] [PubMed] [Google Scholar]
- 16. Pegg TJ, Selvanayagam JB, Francis JM, Karamitsos TD, Maunsell Z, Yu LM, Neubauer S, Taggart DP.. A randomized trial of on-pump beating heart and conventional cardioplegic arrest in coronary artery bypass surgery patients with impaired left ventricular function using cardiac magnetic resonance imaging and biochemical markers. Circulation 2008;118:2130–2138. [DOI] [PubMed] [Google Scholar]
- 17. Steuer J, Bjerner T, Duvernoy O, Jideus L, Johansson L, Ahlstrom H, Stahle E, Lindahl B.. Visualisation and quantification of peri-operative myocardial infarction after coronary artery bypass surgery with contrast-enhanced magnetic resonance imaging. Eur Heart J 2004;25:1293–1299. [DOI] [PubMed] [Google Scholar]
- 18. Moussa ID, Klein LW, Shah B, Mehran R, Mack MJ, Brilakis ES, Reilly JP, Zoghbi G, Holper E, Stone GW.. Consideration of a new definition of clinically relevant myocardial infarction after coronary revascularization: an expert consensus document from the Society for Cardiovascular Angiography and Interventions (SCAI). J Am Coll Cardiol 2013;62:1563–1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Costa MA, Carere RG, Lichtenstein SV, Foley DP, de Valk V, Lindenboom W, Roose PC, van Geldorp TR, Macaya C, Castanon JL, Fernandez-Avilez F, Gonzales JH, Heyer G, Unger F, Serruys PW.. Incidence, predictors, and significance of abnormal cardiac enzyme rise in patients treated with bypass surgery in the arterial revascularization therapies study (ARTS). Circulation 2001;104:2689–2693. [DOI] [PubMed] [Google Scholar]
- 20. Klatte K, Chaitman BR, Theroux P, Gavard JA, Stocke K, Boyce S, Bartels C, Keller B, Jessel A, Investigators G.. Increased mortality after coronary artery bypass graft surgery is associated with increased levels of postoperative creatine kinase-myocardial band isoenzyme release: results from the GUARDIAN Trial. J Am Coll Cardiol 2001;38:1070–1077. [DOI] [PubMed] [Google Scholar]
- 21. Steuer J, Horte LG, Lindahl B, Stahle E.. Impact of perioperative myocardial injury on early and long-term outcome after coronary artery bypass grafting. Eur Heart J 2002;23:1219–1227. [DOI] [PubMed] [Google Scholar]
- 22. Marso SP, Bliven BD, House JA, Muehlebach GF, Borkon AM.. Myonecrosis following isolated coronary artery bypass grafting is common and associated with an increased risk of long-term mortality. Eur Heart J 2003;24:1323–1328. [DOI] [PubMed] [Google Scholar]
- 23. Ramsay J, Shernan S, Fitch J, Finnegan P, Todaro T, Filloon T, Nussmeier NA.. Increased creatine kinase MB level predicts postoperative mortality after cardiac surgery independent of new Q waves. J Thorac Cardiovasc Surg 2005;129:300–306. [DOI] [PubMed] [Google Scholar]
- 24. Engoren MC, Habib RH, Zacharias A, Schwann TA, Riordan CJ, Durham SJ, Shah A.. The association of elevated creatine kinase-myocardial band on mortality after coronary artery bypass grafting surgery is time and magnitude limited. Eur J Cardio-Thorac Surg 2005;28:114–119. [DOI] [PubMed] [Google Scholar]
- 25. Mahaffey KW, Roe MT, Kilaru R, Alexander JH, Van de Werf F, Califf RM, Simoons ML, Topol EJ, Harrington RA.. Creatine kinase-MB elevation after coronary artery bypass grafting surgery in patients with non-ST-segment elevation acute coronary syndromes predict worse outcomes: results from four large clinical trials. Eur Heart J 2007;28:425–432. [DOI] [PubMed] [Google Scholar]
- 26. Muehlschlegel JD, Perry TE, Liu KY, Nascimben L, Fox AA, Collard CD, Avery EG, Aranki SF, D'ambra MN, Shernan SK, Body SC, Investigators CG.. Troponin is superior to electrocardiogram and creatinine kinase MB for predicting clinically significant myocardial injury after coronary artery bypass grafting. Eur Heart J 2009;30:1574–1583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ranasinghe AM, Quinn DW, Richardson M, Freemantle N, Graham TR, Mascaro J, Rooney SJ, Wilson IC, Pagano D, Bonser RS.. Which troponometric best predicts midterm outcome after coronary artery bypass graft surgery? Ann Thorac Surg 2011;91:1860–1867. [DOI] [PubMed] [Google Scholar]
- 28. Vikenes K, Andersen KS, Melberg T, Farstad M, Nordrehaug JE.. Long-term prognostic value of cardiac troponin I and T versus creatine kinase-MB mass after cardiac surgery in low-risk patients with stable symptoms. Am J Cardiol 2010;106:780–786. [DOI] [PubMed] [Google Scholar]
- 29. Domanski MJ, Mahaffey K, Hasselblad V, Brener SJ, Smith PK, Hillis G, Engoren M, Alexander JH, Levy JH, Chaitman BR, Broderick S, Mack MJ, Pieper KS, Farkouh ME.. Association of myocardial enzyme elevation and survival following coronary artery bypass graft surgery. JAMA: J Am Med Assoc 2011;305:585–591. [DOI] [PubMed] [Google Scholar]
- 30. Soraas CL, Friis C, Engebretsen KV, Sandvik L, Kjeldsen SE, Tonnessen T.. Troponin T is a better predictor than creatine kinase-MB of long-term mortality after coronary artery bypass graft surgery. Am Heart J 2012;164:779–785. [DOI] [PubMed] [Google Scholar]
- 31. Farooq V, Serruys PW, Vranckx P, Bourantas CV, Girasis C, Holmes DR, Kappetein AP, Mack M, Feldman T, Morice MC, Colombo A, Morel MA, de Vries T, Dawkins KD, Mohr FW, James S, Stahle E.. Incidence, correlates, and significance of abnormal cardiac enzyme rises in patients treated with surgical or percutaneous based revascularisation: a substudy from the Synergy between Percutaneous Coronary Interventions with Taxus and Cardiac Surgery (SYNTAX) Trial. Int J Cardiol 2013;168:5287–5292. [DOI] [PubMed] [Google Scholar]
- 32. Kemp M, Donovan J, Higham H, Hooper J.. Biochemical markers of myocardial injury. Br J Anaesth 2004;93:63–73. [DOI] [PubMed] [Google Scholar]
- 33. Babuin L, Jaffe AS.. Troponin: the biomarker of choice for the detection of cardiac injury. CMAJ 2005;173:1191–1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Adabag AS, Rector T, Mithani S, Harmala J, Ward HB, Kelly RF, Nguyen JT, McFalls EO, Bloomfield HE.. Prognostic significance of elevated cardiac troponin I after heart surgery. Ann Thorac Surg 2007;83:1744–1750. [DOI] [PubMed] [Google Scholar]
- 35. Holmvang L, Jurlander B, Rasmussen C, Thiis JJ, Grande P, Clemmensen P.. Use of biochemical markers of infarction for diagnosing perioperative myocardial infarction and early graft occlusion after coronary artery bypass surgery. Chest 2002;121:103–111. [DOI] [PubMed] [Google Scholar]
- 36. Januzzi JL, Lewandrowski K, MacGillivray TE, Newell JB, Kathiresan S, Servoss SJ, Lee-Lewandrowski E.. A comparison of cardiac troponin T and creatine kinase-MB for patient evaluation after cardiac surgery. J Am Coll Cardiol 2002;39:1518–1523. [DOI] [PubMed] [Google Scholar]
- 37. Kathiresan S, Servoss SJ, Newell JB, Trani D, MacGillivray TE, Lewandrowski K, Lee-Lewandrowski E, Januzzi JL Jr.. Cardiac troponin T elevation after coronary artery bypass grafting is associated with increased one-year mortality. Am J Cardiol 2004;94:879–881. [DOI] [PubMed] [Google Scholar]
- 38. Lehrke S, Steen H, Sievers HH, Peters H, Opitz A, Muller-Bardorff M, Wiegand UK, Katus HA, Giannitsis E.. Cardiac troponin T for prediction of short- and long-term morbidity and mortality after elective open heart surgery. Clin Chem 2004;50:1560–1567. [DOI] [PubMed] [Google Scholar]
- 39. Nesher N, Alghamdi AA, Singh SK, Sever JY, Christakis GT, Goldman BS, Cohen GN, Moussa F, Fremes SE.. Troponin after cardiac surgery: a predictor or a phenomenon? Ann Thorac Surg 2008;85:1348–1354. [DOI] [PubMed] [Google Scholar]
- 40. Mohammed AA, Agnihotri AK, van Kimmenade RR, Martinez-Rumayor A, Green SM, Quiroz R, Januzzi JL Jr.. Prospective, comprehensive assessment of cardiac troponin T testing after coronary artery bypass graft surgery. Circulation 2009;120:843–850. [DOI] [PubMed] [Google Scholar]
- 41. Petaja L, Salmenpera M, Pulkki K, Pettila V.. Biochemical injury markers and mortality after coronary artery bypass grafting: a systematic review. Ann Thorac Surg 2009;87:1981–1992. [DOI] [PubMed] [Google Scholar]
- 42. Gober V, Hohl A, Gahl B, Dick F, Eigenmann V, Carrel TP, Tevaearai HT.. Early troponin T and prediction of potentially correctable in-hospital complications after coronary artery bypass grafting surgery. PLoS One 2013;8:e74241.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Greenson N, Macoviak J, Krishnaswamy P, Morrisey R, James C, Clopton P, Fitzgerald R, Maisel AS.. Usefulness of cardiac troponin I in patients undergoing open heart surgery. Am Heart J 2001;141:447–455. [DOI] [PubMed] [Google Scholar]
- 44. Eigel P, van Ingen G, Wagenpfeil S.. Predictive value of perioperative cardiac troponin I for adverse outcome in coronary artery bypass surgery. Eur J Cardio-Thorac Surg 2001;20:544–549. [DOI] [PubMed] [Google Scholar]
- 45. Lasocki S, Provenchere S, Benessiano J, Vicaut E, Lecharny JB, Desmonts JM, Dehoux M, Philip I.. Cardiac troponin I is an independent predictor of in-hospital death after adult cardiac surgery. Anesthesiology 2002;97:405–411. [DOI] [PubMed] [Google Scholar]
- 46. Thielmann M, Massoudy P, Marggraf G, Knipp S, Schmermund A, Piotrowski J, Erbel R, Jakob H.. Role of troponin I, myoglobin, and creatine kinase for the detection of early graft failure following coronary artery bypass grafting. Eur J Cardio-Thorac Surg 2004;26:102–109. [DOI] [PubMed] [Google Scholar]
- 47. Paparella D, Cappabianca G, Visicchio G, Galeone A, Marzovillo A, Gallo N, Memmola C, Schinosa Lde L.. Cardiac troponin I release after coronary artery bypass grafting operation: effects on operative and midterm survival. Ann Thorac Surg 2005;80:1758–1764. [DOI] [PubMed] [Google Scholar]
- 48. Thielmann M, Massoudy P, Schmermund A, Neuhauser M, Marggraf G, Kamler M, Herold U, Aleksic I, Mann K, Haude M, Heusch G, Erbel R, Jakob H.. Diagnostic discrimination between graft-related and non-graft-related perioperative myocardial infarction with cardiac troponin I after coronary artery bypass surgery. Eur Heart J 2005;26:2440–2447. [DOI] [PubMed] [Google Scholar]
- 49. Croal BL, Hillis GS, Gibson PH, Fazal MT, El-Shafei H, Gibson G, Jeffrey RR, Buchan KG, West D, Cuthbertson BH.. Relationship between postoperative cardiac troponin I levels and outcome of cardiac surgery. Circulation 2006;114:1468–1475. [DOI] [PubMed] [Google Scholar]
- 50. Provenchere S, Berroeta C, Reynaud C, Baron G, Poirier I, Desmonts JM, Iung B, Dehoux M, Philip I, Benessiano J.. Plasma brain natriuretic peptide and cardiac troponin I concentrations after adult cardiac surgery: association with postoperative cardiac dysfunction and 1-year mortality. Crit Care Med 2006;34:995–1000. [DOI] [PubMed] [Google Scholar]
- 51. Fellahi JL, Hedoire F, Le Manach Y, Monier E, Guillou L, Riou B.. Determination of the threshold of cardiac troponin I associated with an adverse postoperative outcome after cardiac surgery: a comparative study between coronary artery bypass graft, valve surgery, and combined cardiac surgery. Crit Care 2007;11:R106.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Hashemzadeh K, Dehdilani M.. Postoperative cardiac troponin I is an independent predictor of in-hospital death after coronary artery bypass grafting. J Cardiovasc Surg 2009;50:403–409. [PubMed] [Google Scholar]
- 53. van Geene Y, van Swieten HA, Noyez L.. Cardiac troponin I levels after cardiac surgery as predictor for in-hospital mortality. Interact Cardiovasc Thorac Surg 2010;10:413–416. [DOI] [PubMed] [Google Scholar]
- 54. Erlinge D, Gotberg M, Lang I, Holzer M, Noc M, Clemmensen P, Jensen U, Metzler B, James S, Botker HE, Omerovic E, Engblom H, Carlsson M, Arheden H, Ostlund O, Wallentin L, Harnek J, Olivecrona GK.. Rapid endovascular catheter core cooling combined with cold saline as an adjunct to percutaneous coronary intervention for the treatment of acute myocardial infarction. The CHILL-MI trial: a randomized controlled study of the use of central venous catheter core cooling combined with cold saline as an adjunct to percutaneous coronary intervention for the treatment of acute myocardial infarction. J Am Coll Cardiol 2014;63:1857–1865. [DOI] [PubMed] [Google Scholar]
- 55. Petzold T, Feindt P, Sunderdiek U, Boeken U, Fischer Y, Gams E.. Heart-type fatty acid binding protein (hFABP) in the diagnosis of myocardial damage in coronary artery bypass grafting. Eur J Cardio-Thorac Surg 2001;19:859–864. [DOI] [PubMed] [Google Scholar]
- 56. Thielmann M, Pasa S, Holst T, Wendt D, Daniel-Sebastian D, Demircioglu E, Sharma V, Jakob H.. Heart-type FABP and ischemia modified albumin for detection of myocardial infarction after CABG. Ann Thorac Surg 2017;104:130–137. [DOI] [PubMed] [Google Scholar]
- 57. Jayasinghe R, Narasimhan S, Tran TH, Paskaranandavadivel A.. Rapid rule out of myocardial infarction with the use of copeptin as a biomarker for cardiac injury. Intern Med J 2014;44:921–924. [DOI] [PubMed] [Google Scholar]
- 58. Yao Y, Du J, Cao X, Wang Y, Huang Y, Hu S, Zheng Z.. Plasma levels of microRNA-499 provide an early indication of perioperative myocardial infarction in coronary artery bypass graft patients. PLoS One 2014;9:e104618.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Zhou X, Mao A, Wang X, Duan X, Yao Y, Zhang C.. Urine and serum microRNA-1 as novel biomarkers for myocardial injury in open-heart surgeries with cardiopulmonary bypass. PLoS One 2013;8:e62245.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Baker JO, Tyther R, Liebetrau C, Clark J, Howarth R, Patterson T, Mollmann H, Nef H, Sicard P, Kailey B, Devaraj R, Redwood SR, Kunst G, Weber E, Marber MS.. Cardiac myosin-binding protein C: a potential early biomarker of myocardial injury. Basic Res Cardiol 2015;110:23.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Lim CC, Cuculi F, van Gaal WJ, Testa L, Arnold JR, Karamitsos T, Francis JM, Digby JE, Antoniades C, Kharbanda RK, Neubauer S, Westaby S, Banning AP.. Early diagnosis of perioperative myocardial infarction after coronary bypass grafting: a study using biomarkers and cardiac magnetic resonance imaging. Ann Thorac Surg 2011;92:2046–2053. [DOI] [PubMed] [Google Scholar]
- 62. Smith JS, Cahalan MK, Benefiel DJ, Byrd BF, Lurz FW, Shapiro WA, Roizen MF, Bouchard A, Schiller NB.. Intraoperative detection of myocardial ischemia in high-risk patients: electrocardiography versus two-dimensional transesophageal echocardiography. Circulation 1985;72:1015–1021. [DOI] [PubMed] [Google Scholar]
- 63. Senior R, Becher H, Monaghan M, Agati L, Zamorano J, Vanoverschelde JL, Nihoyannopoulos P.. Contrast echocardiography: evidence-based recommendations by European Association of Echocardiography. Eur J Echocardiogr 2009;10:194–212. [DOI] [PubMed] [Google Scholar]
- 64. Flachskampf FA, Schmid M, Rost C, Achenbach S, DeMaria AN, Daniel WG.. Cardiac imaging after myocardial infarction. Eur Heart J 2011;32:272–283. [DOI] [PubMed] [Google Scholar]
- 65. De Mey N, Couture P, Laflamme M, Denault AY, Perrault LP, Deschamps A, Rochon AG.. Intraoperative changes in regional wall motion: can postoperative coronary artery bypass graft failure be predicted? J Cardiothorac Vasc Anesth 2012;26:371–375. [DOI] [PubMed] [Google Scholar]
- 66. Dakik HA, Howell JF, Lawrie GM, Espada R, Weilbaecher DG, He ZX, Mahmarian JJ, Verani MS.. Assessment of myocardial viability with 99mTc-sestamibi tomography before coronary bypass graft surgery: correlation with histopathology and postoperative improvement in cardiac function. Circulation 1997;96:2892–2898. [DOI] [PubMed] [Google Scholar]
- 67. Taqueti VR, Hachamovitch R, Murthy VL, Naya M, Foster CR, Hainer J, Dorbala S, Blankstein R, Di Carli MF.. Global coronary flow reserve is associated with adverse cardiovascular events independently of luminal angiographic severity and modifies the effect of early revascularization. Circulation 2015;131:19–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Katsikis A, Ekonomopoulos G, Papaioannou S, Kouzoumi A, Koutelou M.. Reversible reduction of cardiac sympathetic innervation after coronary artery bypass graft surgery: an observational study using serial iodine 123-labeled meta-iodobenzyl-guanidine (MIBG) imaging. J Thorac Cardiovasc Surg 2012;144:210–216. [DOI] [PubMed] [Google Scholar]
- 69. Schuleri KH, George RT, Lardo AC.. Assessment of coronary blood flow with computed tomography and magnetic resonance imaging. J Nucl Cardiol 2010;17:582–590. [DOI] [PubMed] [Google Scholar]
- 70. Yoo KJ, Choi D, Choi BW, Lim SH, Chang BC.. The comparison of the graft patency after coronary artery bypass grafting using coronary angiography and multi-slice computed tomography. Eur J Cardio-Thorac Surg 2003;24:86–91; discussion 91. [DOI] [PubMed] [Google Scholar]
- 71. Weustink AC, Nieman K, Pugliese F, Mollet NR, Meijboom WB, van Mieghem C, ten Kate GJ, Cademartiri F, Krestin GP, de Feyter PJ.. Diagnostic accuracy of computed tomography angiography in patients after bypass grafting: comparison with invasive coronary angiography. JACC Cardiovasc Imaging 2009;2:816–824. [DOI] [PubMed] [Google Scholar]
- 72. Knuuti J, Bengel F, Bax JJ, Kaufmann PA, Le Guludec D, Perrone Filardi P, Marcassa C, Ajmone Marsan N, Achenbach S, Kitsiou A, Flotats A, Eeckhout E, Minn H, Hesse B.. Risks and benefits of cardiac imaging: an analysis of risks related to imaging for coronary artery disease. Eur Heart J 2014;35:633–638. [DOI] [PubMed] [Google Scholar]
- 73. Klem I, Shah DJ, White RD, Pennell DJ, van Rossum AC, Regenfus M, Sechtem U, Schvartzman PR, Hunold P, Croisille P, Parker M, Judd RM, Kim RJ.. Prognostic value of routine cardiac magnetic resonance assessment of left ventricular ejection fraction and myocardial damage: an international, multicenter study. Circ Cardiovasc Imaging 2011;4:610–619. [DOI] [PubMed] [Google Scholar]
- 74. Pegg TJ, Maunsell Z, Karamitsos TD, Taylor RP, James T, Francis JM, Taggart DP, White H, Neubauer S, Selvanayagam JB.. Utility of cardiac biomarkers for the diagnosis of type V myocardial infarction after coronary artery bypass grafting: insights from serial cardiac MRI. Heart 2011;97:810–816. [DOI] [PubMed] [Google Scholar]
- 75. van Gaal WJ, Arnold JR, Testa L, Karamitsos T, Lim CC, Ponnuthurai FA, Petersen S, Francis JM, Selvanayagam J, Sayeed R, West N, Westaby S, Neubauer S, Banning AP.. Myocardial injury following coronary artery surgery versus angioplasty (MICASA): a randomised trial using biochemical markers and cardiac magnetic resonance imaging. EuroIntervention 2011;6:703–710. [DOI] [PubMed] [Google Scholar]
- 76. Alam SR, Lewis SC, Zamvar V, Pessotto R, Dweck MR, Krishan A, Goodman K, Oatey K, Harkess R, Milne L, Thomas S, Mills NM, Moore C, Semple S, Wiedow O, Stirrat C, Mirsadraee S, Newby DE, Henriksen PA.. Perioperative elafin for ischaemia-reperfusion injury during coronary artery bypass graft surgery: a randomised-controlled trial. Heart 2015;101:1639–1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Heusch G, Kleinbongard P, Bose D, Levkau B, Haude M, Schulz R, Erbel R.. Coronary microembolization: from bedside to bench and back to bedside. Circulation 2009;120:1822–1836. [DOI] [PubMed] [Google Scholar]
- 78. Nassenstein K, Breuckmann F, Bucher C, Kaiser G, Konorza T, Schafer L, Konietzka I, de Greiff A, Heusch G, Erbel R, Barkhausen J.. How much myocardial damage is necessary to enable detection of focal late gadolinium enhancement at cardiac MR imaging? Radiology 2008;249:829–835. [DOI] [PubMed] [Google Scholar]
- 79. Rahimi K, Banning AP, Cheng AS, Pegg TJ, Karamitsos TD, Channon KM, Darby S, Taggart DP, Neubauer S, Selvanayagam JB.. Prognostic value of coronary revascularisation-related myocardial injury: a cardiac magnetic resonance imaging study. Heart 2009;95:1937–1943. [DOI] [PubMed] [Google Scholar]
- 80. Kolh P, Windecker S.. ESC/EACTS myocardial revascularization guidelines 2014. Eur Heart J 2014;35:3235–3236. [DOI] [PubMed] [Google Scholar]
- 81. Laflamme M, DeMey N, Bouchard D, Carrier M, Demers P, Pellerin M, Couture P, Perrault LP.. Management of early postoperative coronary artery bypass graft failure. Interact Cardiovasc Thorac Surg 2012;14:452–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Raabe DS Jr., Morise A, Sbarbaro JA, Gundel WD.. Diagnostic criteria for acute myocardial infarction in patients undergoing coronary artery bypass surgery. Circulation 1980;62:869–878. [DOI] [PubMed] [Google Scholar]
- 83. Murphy GJ, Reeves BC, Rogers CA, Rizvi SI, Culliford L, Angelini GD.. Increased mortality, postoperative morbidity, and cost after red blood cell transfusion in patients having cardiac surgery. Circulation 2007;116:2544–2552. [DOI] [PubMed] [Google Scholar]
- 84. Koch CG, Li L, Duncan AI, Mihaljevic T, Cosgrove DM, Loop FD, Starr NJ, Blackstone EH.. Morbidity and mortality risk associated with red blood cell and blood-component transfusion in isolated coronary artery bypass grafting. Crit Care Med 2006;34:1608–1616. [DOI] [PubMed] [Google Scholar]
- 85. Murphy GJ, Pike K, Rogers CA, Wordsworth S, Stokes EA, Angelini GD, Reeves BC, Investigators TI.. Liberal or restrictive transfusion after cardiac surgery. N Engl J Med 2015;372:997–1008. [DOI] [PubMed] [Google Scholar]
- 86. Dieleman JM, Nierich AP, Rosseel PM, van der Maaten JM, Hofland J, Diephuis JC, Schepp RM, Boer C, Moons KG, van Herwerden LA, Tijssen JG, Numan SC, Kalkman CJ, van Dijk D.. Dexamethasone for Cardiac Surgery Study Group. Intraoperative high-dose dexamethasone for cardiac surgery: a randomized controlled trial. JAMA: J Am Med Assoc 2012;308:1761–1767. [DOI] [PubMed] [Google Scholar]
- 87. Whitlock RP, Devereaux PJ, Teoh KH, Lamy A, Vincent J, Pogue J, Paparella D, Sessler DI, Karthikeyan G, Villar JC, Zuo Y, Avezum A, Quantz M, Tagarakis GI, Shah PJ, Abbasi SH, Zheng H, Pettit S, Chrolavicius S, Yusuf S, Investigators S.. Methylprednisolone in patients undergoing cardiopulmonary bypass (SIRS): a randomised, double-blind, placebo-controlled trial. Lancet 2015;386:1243–1253. [DOI] [PubMed] [Google Scholar]
- 88. Hillis LD, Smith PK, Anderson JL, Bittl JA, Bridges CR, Byrne JG, Cigarroa JE, Disesa VJ, Hiratzka LF, Hutter AM Jr, Jessen ME, Keeley EC, Lahey SJ, Lange RA, London MJ, Mack MJ, Patel MR, Puskas JD, Sabik JF, Selnes O, Shahian DM, Trost JC, Winniford MD.. 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2011;124:e652–e735. [DOI] [PubMed] [Google Scholar]
- 89. Santa-Cruz RA, Cohen MG, Ohman EM.. Aortic counterpulsation: a review of the hemodynamic effects and indications for use. Catheter Cardiovasc Interv 2006;67:68–77. [DOI] [PubMed] [Google Scholar]
- 90. Zangrillo A, Pappalardo F, Dossi R, Di Prima AL, Sassone ME, Greco T, Monaco F, Musu M, Finco G, Landoni G.. Preoperative intra-aortic balloon pump to reduce mortality in coronary artery bypass graft: a meta-analysis of randomized controlled trials. Crit Care 2015;19:10.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Pellegrino V, Hockings LE, Davies A.. Veno-arterial extracorporeal membrane oxygenation for adult cardiovascular failure. Curr Opin Crit Care 2014;20:484–492. [DOI] [PubMed] [Google Scholar]
- 92. Thielmann M, Massoudy P, Jaeger BR, Neuhauser M, Marggraf G, Sack S, Erbel R, Jakob H.. Emergency re-revascularization with percutaneous coronary intervention, reoperation, or conservative treatment in patients with acute perioperative graft failure following coronary artery bypass surgery. Eur J Cardio-Thorac Surg 2006;30:117–125. [DOI] [PubMed] [Google Scholar]
- 93. Rasmussen C, Thiis JJ, Clemmensen P, Efsen F, Arendrup HC, Saunamaki K, Madsen JK, Pettersson G.. Significance and management of early graft failure after coronary artery bypass grafting: feasibility and results of acute angiography and re-re-vascularization. Eur J Cardio-Thorac Surg 1997;12:847–852. [DOI] [PubMed] [Google Scholar]
- 94. Fabricius AM, Gerber W, Hanke M, Garbade J, Autschbach R, Mohr FW.. Early angiographic control of perioperative ischemia after coronary artery bypass grafting. Eur J Cardio-Thorac Surg 2001;19:853–858. [DOI] [PubMed] [Google Scholar]
- 95. Davierwala PM, Verevkin A, Leontyev S, Misfeld M, Borger MA, Mohr FW.. Impact of expeditious management of perioperative myocardial ischemia in patients undergoing isolated coronary artery bypass surgery. Circulation 2013;128(11 Suppl 1):S226–S234. [DOI] [PubMed] [Google Scholar]
- 96. Fleissner F, Issam I, Martens A, Cebotari S, Haverich A, Shrestha ML.. The unplanned postoperative coronary angiogram after CABG: identifying the patients at risk. Thorac Cardiovasc Surg 2017;65:292–295. [DOI] [PubMed] [Google Scholar]
- 97. Brilakis ES, Rao SV, Banerjee S, Goldman S, Shunk KA, Holmes DR Jr., Honeycutt E, Roe MT.. Percutaneous coronary intervention in native arteries versus bypass grafts in prior coronary artery bypass grafting patients: a report from the National Cardiovascular Data Registry. JACC Cardiovasc Interv 2011;4:844–850. [DOI] [PubMed] [Google Scholar]
- 98. Becit N, Erkut B, Ceviz M, Unlu Y, Colak A, Kocak H.. The impact of intraoperative transit time flow measurement on the results of on-pump coronary surgery. Eur J Cardio-Thorac Surg 2007;32:313–318. [DOI] [PubMed] [Google Scholar]
- 99. Di Giammarco G, Pano M, Cirmeni S, Pelini P, Vitolla G, Di Mauro M.. Predictive value of intraoperative transit-time flow measurement for short-term graft patency in coronary surgery. J Thorac Cardiovasc Surg 2006;132:468–474. [DOI] [PubMed] [Google Scholar]
- 100. Oshima H, Tokuda Y, Araki Y, Ishii H, Murohara T, Ozaki Y, Usui A.. Predictors of early graft failure after coronary artery bypass grafting for chronic total occlusion. Interact Cardiovasc Thorac Surg 2016;23:142–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Jokinen JJ, Werkkala K, Vainikka T, Perakyla T, Simpanen J, Ihlberg L.. Clinical value of intra-operative transit-time flow measurement for coronary artery bypass grafting: a prospective angiography-controlled study. Eur J Cardio-Thorac Surg 2011;39:918–923. [DOI] [PubMed] [Google Scholar]
- 102. Heusch G. Cardioprotection: chances and challenges of its translation to the clinic. Lancet 2013;381:166–175. [DOI] [PubMed] [Google Scholar]
- 103. Ibanez B, Heusch G, Ovize M, Van de Werf F.. Evolving therapies for myocardial ischemia/reperfusion injury. J Am Coll Cardiol 2015;65:1454–1471. [DOI] [PubMed] [Google Scholar]
- 104. Heusch G. Molecular basis of cardioprotection: signal transduction in ischemic pre-, post- and remote conditioning. Circ Res 2015;116:674–699. [DOI] [PubMed] [Google Scholar]
- 105. Hausenloy DJ, Bøtker HE, Condorelli G, Ferdinandy P, Garcia-Dorado D, Heusch G, Lecour S, van Laake LW, Madonna R, Ruiz-Meana M, Schulz R, Sluijter JP, Yellon DM, Ovize M.. Translating cardioprotection for patient benefit: position paper from the Working Group of Cellular Biology of the Heart of the European Society of Cardiology. Cardiovasc Res 2013;98:7–27. [DOI] [PubMed] [Google Scholar]
- 106. Lecour S, Botker HE, Condorelli G, Davidson SM, Garcia-Dorado D, Engel FB, Ferdinandy P, Heusch G, Madonna R, Ovize M, Ruiz-Meana M, Schulz R, Sluijter JP, Van Laake LW, Yellon DM, Hausenloy DJ.. ESC working group cellular biology of the heart: position paper: improving the preclinical assessment of novel cardioprotective therapies. Cardiovasc Res 2014;104:399–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Heusch G. The coronary circulation as a target of cardioprotection. Circ Res 2016;118:1643–1658. [DOI] [PubMed] [Google Scholar]
- 108. Kunst G, Klein AA.. Peri-operative anaesthetic myocardial preconditioning and protection - cellular mechanisms and clinical relevance in cardiac anaesthesia. Anaesthesia 2015;70:467–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Hausenloy D, Kunst G, Boston-Griffiths E, Kolvekar S, Chaubey S, John L, Desai J, Yellon D.. The effect of cyclosporin-A on peri-operative myocardial injury in adult patients undergoing coronary artery bypass graft surgery: a randomised controlled clinical trial. Heart 2014;100:544–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Chiari P, Angoulvant D, Mewton N, Desebbe O, Obadia JF, Robin J, Farhat F, Jegaden O, Bastien O, Lehot JJ, Ovize M.. Cyclosporine protects the heart during aortic valve surgery. Anesthesiology 2014;121:232–238. [DOI] [PubMed] [Google Scholar]
- 111. Candilio L, Malik A, Ariti C, Barnard M, Di SC, Lawrence D, Hayward M, Yap J, Roberts N, Sheikh A, Kolvekar S, Hausenloy DJ, Yellon DM.. Effect of remote ischaemic preconditioning on clinical outcomes in patients undergoing cardiac bypass surgery: a randomised controlled clinical trial. Heart 2015;10:185–192. [DOI] [PubMed] [Google Scholar]
- 112. Thielmann M, Kottenberg E, Kleinbongard P, Wendt D, Gedik N, Pasa S, Price V, Tsagakis K, Neuhäuser M, Peters J, Jakob H, Heusch G.. Cardioprotective and prognostic effects of remote ischaemic preconditioning in patients undergoing coronary artery bypass surgery: a single-centre randomised, double-blind, controlled trial. Lancet 2013;382:597–604. [DOI] [PubMed] [Google Scholar]
- 113. Meybohm P, Bein B, Brosteanu O, Cremer J, Gruenewald M, Stoppe C, Coburn M, Schaelte G, Boning A, Niemann B, Roesner J, Kletzin F, Strouhal U, Reyher C, Laufenberg-Feldmann R, Ferner M, Brandes IF, Bauer M, Stehr SN, Kortgen A, Wittmann M, Baumgarten G, Meyer-Treschan T, Kienbaum P, Heringlake M, Schon J, Sander M, Treskatsch S, Smul T, Wolwender E, Schilling T, Fuernau G, Hasenclever D, Zacharowski K, Collaborators RIS.. A multicenter trial of remote ischemic preconditioning for heart surgery. N Engl J Med 2015;373:1397–1407. [DOI] [PubMed] [Google Scholar]
- 114. Hausenloy DJ, Candilio L, Evans R, Ariti C, Jenkins DP, Kolvekar S, Knight R, Kunst G, Laing C, Nicholas J, Pepper J, Robertson S, Xenou M, Clayton T, Yellon DM, Investigators ET.. Remote ischemic preconditioning and outcomes of cardiac surgery. N Engl J Med 2015;373:1408–1417. [DOI] [PubMed] [Google Scholar]
- 115. Hausenloy DJ, Mwamure PK, Venugopal V, Harris J, Barnard M, Grundy E, Ashley E, Vichare S, Di Salvo C, Kolvekar S, Hayward M, Keogh B, MacAllister RJ, Yellon DM.. Effect of remote ischaemic preconditioning on myocardial injury in patients undergoing coronary artery bypass graft surgery: a randomized controlled trial. Lancet 2007;370:575–579. [DOI] [PubMed] [Google Scholar]
- 116. Heusch G, Gersh BJ.. ERICCA and RIPHeart: two nails in the coffin for cardioprotection by remote ischemic conditioning? Probably not! Eur Heart J 2015;37:200–201. [DOI] [PubMed] [Google Scholar]
- 117. Varga ZV, Zvara A, Farago N, Kocsis GF, Pipicz M, Gaspar R, Bencsik P, Gorbe A, Csonka C, Puskas LG, Thum T, Csont T, Ferdinandy P.. MicroRNAs associated with ischemia-reperfusion injury and cardioprotection by ischemic pre- and postconditioning: protectomiRs. Am J Physiol Heart Circ Physiol 2014;307:H216–H227. [DOI] [PubMed] [Google Scholar]