Abstract
Atherosclerosis is the leading cause of cardiovascular mortality and morbidity in the developed world. Intravascular ultrasound (IVUS) is a widely used imaging modality providing complementary diagnostic information to angiography regarding the vessel wall of the coronary arteries. IVUS has been used for assessment of ambiguous angiographic lesions, evaluation of new interventional devices and in atherosclerosis progression-regression trials. However, the standard gray-scale IVUS has limited value for the accurate identification of specific plaque components. This limitation has been partially over- come by introduction of new IVUS-based imaging methods such as: virtual histology IVUS, iMAP-IVUS and Integrated Backscatter IVUS. These methods utilise the ultrasound backscatter signal to enable a more detailed characterization of plaque morphology or tissue characterization and to provide insight on the features of vulnerable plaque.
Keywords: Atherosclerosis, Imaging, Ultrasonics, Radiofrequency data analysis, Tissue characterization
Intravascular ultrasound (IVUS) is the first catheter-based imaging modality that has been widely used in interventional cardiology.[1] It creates cross-sectional images of the vessel lumen and the arterial wall and provides valuable diagnostic information to angiography regarding lumen and vessel measurements and plaque morphology. This information helps clinical decision-making in ambiguous angiographic lesions. IVUS has also been used to evaluate new interventional devices and for atherosclerosis progression-regression trials. Recently, IVUS has been used to detect vulnerable plaques. In this review, we will focus on the potential clinical and research utility of IVUS-based imaging modalities for tissue characterisation.
Greyscale Ivus and Ivus Radiofrequency Analysis
IVUS uses a miniaturised piezoelectric transducer mounted on the tip of a catheter where it produces ultrasound signals. The imaging is based on the emission, attenuation and backscattering of ultrasonic waves that are converted to electrical signals and then processed as an image. Standard greyscale IVUS allows quantitative measurements of lumen and vessel and qualitative assessment of atherosclerotic plaque. Calcified tissues are highly echogenic and thus appear as bright echoes with acoustic shadowing. Regions of low echogenicity are usually labelled as “soft” plaque. Soft plaque has high lipid content or it may also be attributable to a necrotic zone within the plaque, an intramural haemorrhage or a thrombus. Fibrous plaques have an intermediate echogenicity between soft and calcific plaques.[2] Recent IVUS studies have described attenuated plaque defined as hypoechoic plaque with deep ultraouns attenuation without calcification or very dense fibrous plaque.[3] The grey-scale IVUS image is formed using the envelope (amplitude) of the radiofrequency (RF) signal. However, the frequency and power of the signal differ between tissues, regardless of similarities in the amplitude. Therefore, grey-scale IVUS has limited value for the accurate identification of specific plaque components. This limitation has been partially overcome by introduction of several IVUS-based post-processing methods. Analysis of IVUS radiofrequency backscatter enables a more detailed characterisation of plaque morphology or tissue characterisation and provides insight on the features of vulnerable plaque.[4] Three different mathematical methods that have been applied to IVUS RF data analysis are virtual histology IVUS, Volcano Therapeutics (Rancho Cordova, CA, USA), iMAP-IVUS, Boston Scientific Corp (Santa Clara, CA, USA), Integrated Backscatter IVUS (YD, Nara, Japan) (See Figure 1, Table 1).
Figure 1: Grey-scale Intravascular Ultrasound and Intravascular Ultrasound Radiofrequency Analysis.
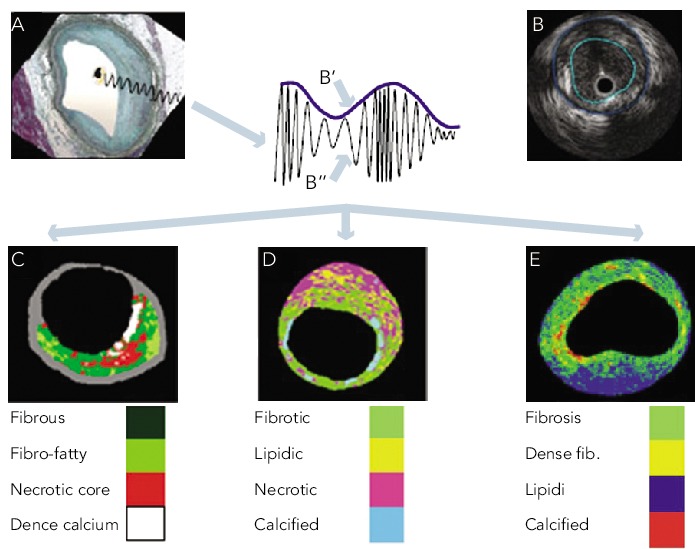
A. An IVUS is obtained from the vessel wall within an histology image. B. The greyscale IVUS image is formed by the envelope (amplitude) of the radiofrequency signal. C. From the backscatter radiofrequency data different types of tissue information can be retrieved: virtual histology; iMAP (D) and integrated backscattered IVUS (E). Adapted from Garcìa-Garcìa HM et al.[4]
Table 1: Similarities and differences IVUS-based imaging modalities.
| VH | IMAP | Integrated backscatter | |
|---|---|---|---|
| Backscatter radiofrequency signal analysis | Autoregressive model | Fast Fourier transformation | Fast Fourier transformation |
| Colour code |
Fibrous: green Fibrofatty: light green Necrotic core: red Dense calcium: white |
Fibrotic: light green Lipidic: yellow Necrotic: pink Calcified: blue |
Fibrosis: light green Dense fibrosis: yellow Lipid: blue Calcified: red |
| Ex vivo Validation against histology | The overall predictive accuracies were 93.5 % for fibrous, 94.1 % for fibro-fatty, 95.8 % for necrotic core, and 96.7 % for dense calcium regions with sensitivities and specificities ranging from 72 % to 99 %[36] | The accuracies at the highest level of confidence (75-100%) were 95 % for fibrotic, 98 % for lipidic, 97 % for necrotic, and 98 % for calcified regions[25] | The sensitivity was 100 % for calcification, 94 % for fibrosis, and 84 % for lipid pool. The specificity was 99 % for calcification, 93 % for fibrosis, and 67 % for lipid pool[37] |
| In vivo validation of vulnerable plaque | The diagnostic accuracy to detect TCFA as determined by optical coherence tomography was 86 % with sensitivity 89 %, specificity 86 %[38] | ||
| Limitations |
|
|
|
Virtual Histology IVUS
Virtual histology (VH) IVUS is based on the spectral analysis of the raw backscattered IVUS RF data. It utilises a mathematical autoregressive model and constructs tissue maps that classify plaque into four major tissue types (fibrous, fibro-fatty, necrotic core, and dense calcium).[5] VH-IVUS clinical utility ranges from predicting high-risk plaques for patients undergoing coronary angiography to predicting adverse events post percutaneous coronary intervention (PCI).[6–9]
Detection of High-risk Plaques
Rupture of an atherosclerotic plaque is the most common pathological substrate of acute myocardial infarction (AMI). Thin fibrous cap atheroma is a precursor to plaque rupture and is associated with sudden cardiac death.[10] Although the axial resolution of VH-IVUS is too low to visualise thin fibrous cap <65 μm, it can potentially identify virtual histology thin cap fibroatheroma (VH-TFCA) that is defined as >10 % confluent necrotic core on three consecutive frames and arc of necrotic core in contact with the lumen for 36 degrees along lumen circumference.[11] The prevalence of VF-TFCA is higher in acute coronary syndrome than in stable angina patients.[12] In the Providing regional observations to study predictors of events in the coronary tree (PROSPECT) study, 697 patients presenting with acute coronary syndrome (ACS) underwent three-vessel grey-scale and VH-IVUS after successful PCI. The three-year cumulative rate of major adverse cardiovascular events (death from cardiac causes, cardiac arrest, myocardial infarction or rehospitalisation due to unstable or progressive angina) was 20.4 percent. Most events were rehospitalisation for unstable or progressive angina. Nearly half of these events (11.6 %) were related to non-culprit lesions.
The PROSPECT study demonstrated that non-culprit lesions associated with recurrent events were frequently angiographically mild, most were VH-TFCA or were characterised by a minimal luminal area ≤ 4.0 mm2 or a plaque burden ≥ 70 %. Adverse events related to non-culprit lesions rarely developed from non-fibroatheromas, regardless of the minimal luminal area or plaque burden.[6] Non-culprit lesions that had the non-fibroatheroma phenotype were associated with lower rate of future cardiovascular events than lesions with a fibroatheroma phenotype. We can speculate that VH-IVUS can predict lesion stability and defer intervention.[7]
In the Virtual Histology in Vulnerable Atherosclerosis (VIVA) study of 170 patients with stable angina or troponin positive ACS referred for PCI, VH-TCFA was associated with major adverse events defined as death, myocardial infarction and unplanned revascularisation.[8] In line with previous studies, the European Collaborative Project on Inflammation and Vascular Wall Remodeling in Atherosclerosis – Intravascular Ultrasound (ATHEROREMO-IVUS) study found that the presence of a VH-TFCA in a non-culprit coronary artery was independently predictive for the occurrence of major adverse cardiac events in stable and acute patients undergoing coronary angiography. VH-TFCA lesions were also independently associated with the composite of death or ACS only (present 7.5 % vs absent 3.0 %; adjusted hazard ratio (HR): 2.51, 95 % CI: 1.15–5.49; P = 0.021).[9] Although VH-IVUS has been shown to predict major adverse cardiac events, it is unclear what treatment options might be effective in mitigating the risk associated with high-risk lesion features.
Use in Percutaneous Coronary Intervention
Grey-scale IVUS has been used to plan and guide PCI. Recently, few studies have tested clinical utility of VH-IVUS for guidance of PCI. The Bifurcation lesion analysis and stenting (BLAST) study investigated VH-IVUS guidance for drug-eluting stent deployment in bifurcation lesions compared to angiographic guidance alone enrolled 195 patients. Initial results showed that 30 days major adverse event rate was similar in both VH-IVUS unblinded and VH-IVUS blinded groups. Higher volumes of dense calcium and necrotic core at the side branch preintervention were contributing factors for major adverse events at 30 days.[13] The long-term results have not been published yet. The Vascular evaluation for revascularisation: defining the indications for coronary therapy (VERDICT) study and Fractional flow reserve and intravascular ultrasound relationship study (FIRST) evaluated the prognostic utility of fractional flow reserve (FFR) and VH IVUS–derived parameters of atherosclerosis in intermediate coronary lesions (40–80 % angiographic diameter stenosis). There was only a modest correlation between IVUS minimum lumen area and FFR, but plaque morphology characteristics did not correlate with FFR.[14,15]
VH-IVUS can identify lesions that are at high-risk for causing distal embolisation or myocardial necrosis. Distal embolisation occurs in 15–70 % of patients and is associated with a poor prognosis after PCI. In a recent meta-analysis the association between plaque composition and distal embolisation after PCI was evaluated in 16 greyscale IVUS or VH-IVUS studies of 1697 patients. Pooled analysis showed that the absolute necrotic core volume, absolute and relative necrotic core areas at the minimum lumen sites were significantly greater in the embolisation group than in the no embolisation group. The other plaque components were similar in both groups.[16] A previously published systematic review reported similar findings. In 9 of the 11 reviewed studies the necrotic core by itself or as a component of VH-TFCA was associated with distal embolisation.[17] Two studies by Nakamura et al. and Bae et al. failed to demonstrate the association between necrotic core and distal embolisation, but a “marble”-like image, consisting of fibro-fatty and fibrous plaque, was associated with the angiographic no-reflow phenomenon during primary PCI.[18,19] This can be explained by the fact that thrombus by VH-IVUS has appearance of fibrotic or fibrofatty tissue and the percentage of necrotic core could be compromised by the presence of thrombus. In a study by Hong et al. in cohort of 80 patients with stable and unstable angina necrotic core volumes and areas were significantly greater in patients with post-PCI cardiac troponin I elevation.[20] The use of statins and embolic protection devices could be particularly beneficial for patients with lesions with a large necrotic core. However no trial examining embolic protection devices in high embolic risk patients has yet been published. We also cannot conclude that VH-IVUS should be used routinely in all patients undergoing PCI.
VH-IVUS has not been validated to assess plaque behind stents, but it has been used to evaluate the development of neoatherosclerosis within neointimal tissues after stent implantation (See Figure 3). VH-IVUS was performed in 36 lesions more than three years after stent implantation. In-stent VH-TFCA was identified in 45.5 % of bare metal stent-treated lesions and in 18.2 % after drug eluting stent implantation (p = 0.361). There was no statistically significant difference with regard to the in-stent tissue composition, including necrotic core and dense calcium.[21]
Figure 3: Corresponding Greyscale and Virtual Histology-Intravascular Ultrasound Images One Year After Bare Metal Stent Implantation.
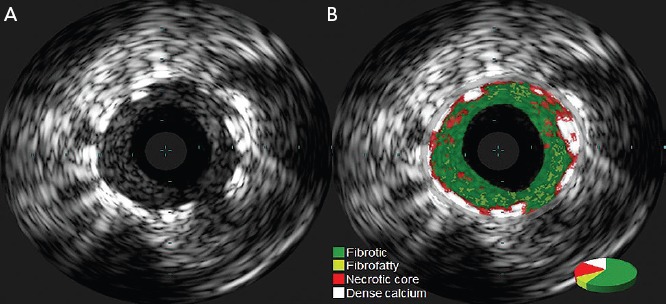
A. Greyscale image shows neointimal hyperplasia inside bare metal stent. B. Metallic stent struts appear as dense calcium surrounded by necrotic core.
Effect of Pharmacological Intervention on Plaque Composition
VH-IVUS has also been used in several studies reporting serial changes of plaque composition in patients treated with lipid lowering therapies. However IVUS-VH acquisition is electrocardiogram-gated which makes accurate co-registration of serial studies difficult.
Recently, in a substudy of the Study of coronary atheroma by intravascular ultrasound: the effect of rosuvastatin vs. Atorvastatin (SATURN) study serial VH-IVUS imaging was performed in 71 patients treated with rosuvastatin 40 mg or atorvastatin 80 mg daily for 24 months.[22] This study showed a decrease in fibro-fatty tissue (P<0.001), while dense calcium increased (P=0.002). There were no changes in fibrous or necrotic core tissue volumes. However, these data are inconsistent with other studies. In meta-analysis by Tian et al. 17 studies involving 2171 patients receiving statin therapy were analysed, a regressive trend was reported for necrotic core volume (mean difference: –2.1 mm3; 95 % CI: –4.7–0.5 mm3, P = 0.11) while statin therapy did not induce a significant change for fibrotic, fibro-fatty, or dense calcium compositions.[23] The Synergistic effect of combination therapy with cilostazol and probucol on plaque stabilization and lesion regression (SECURE) study compared the effects of nine months of treatment with probucol and cilostazol combination therapy or cilostazol monotherapy. This study failed to demonstrate significant differences in changes in plaque volume or composition between two groups despite different impacts on lipid biomarkers.[24] However, there is no clear proof of a direct connection between changes in plaque composition and clinical events.
IMAP IVUS
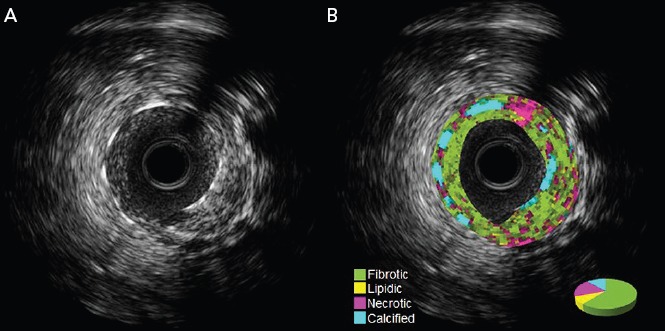
Another IVUS RF data analysis system is the iMAP software.[25] Unlike VH-IVUS, iMap uses a 40 MHz single rotational transducer and can acquire RF data continuously, while VH-IVUS data are collected with a 20 MHz electronic catheter that acquires only electrocardiogram-gated data. VH-IVUS uses autoregressive modelling to analyse the IVUS RF spectrum, while iMap uses a pattern recognition algorithm on the spectra that were obtained from a fast Fourier transformation and a histology-derived database. iMAP-IVUS classifies coronary plaque into four components (fibrotic, lipidic, necrotic, and calcified). Like VH-IVUS, iMAP could be used to detect high risk plaques and predict adverse events following PCI, for example, slow flow. However it is noteworthy that in vivo comparison of iMAP and VH-IVUS tissue characterisation has reported a significant and systematic variability in plaque composition estimates (See Figure 2). iMap expressed plaque as necrotic core in poor signal areas, such as guidewire artefact or acoustic shadowing of the calcium. VH-IVUS classified acoustic shadowing as fibrous or fibrofatty tissue. VH-IVUS showed metallic stent struts as dense calcium and necrotic core, while iMap showed thinner stent thickness without necrotic core around the stent (See Figures 3 and 4).[26]
Figure 2: Corresponding Cross-sections of iMap and Virtual Histology Images.
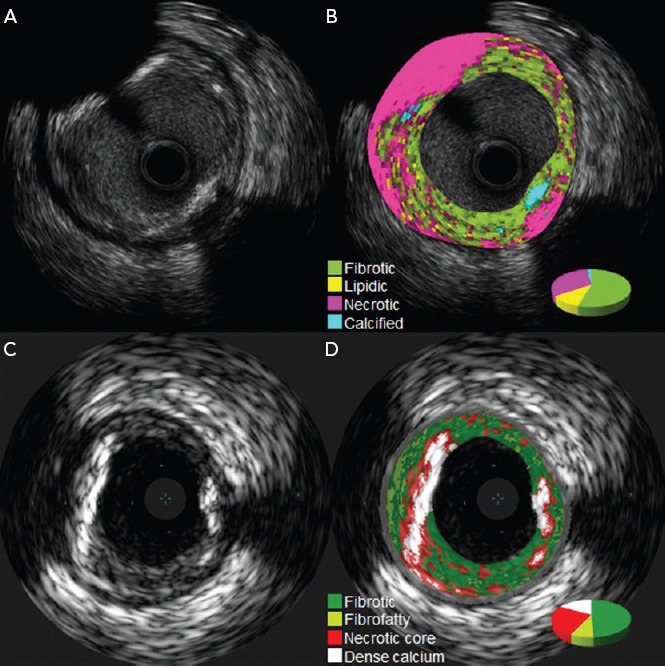
Standard Intravascular ultrasound (IVUS) image using a 40-MHz mechanical rotating catheter (A) and a 20-MHz phased-array catheter (C). iMap shows large amounts of necrotic tissue (B), while with VH the same area is reported as fibrous or fibrofatty tissue (D).
Figure 4: Corresponding greyscale and iMAP-Intravascular Ultrasound Images One Year after Bare Metal Stent Implantation.
A. Greyscale image shows neointimal hyperplasia inside bare metal stent. B. Metallic stent struts appear as dense calcium without necrotic core around them.
iMAP can be used for the in vivo identification of vulnerable plaque and prediction of adverse events of PCI. In a study of 87 patients, iMAP analysis revealed that the culprit plaques in patients with ACS contained larger lipidic and necrotic components with a smaller fibrous component compared to non-ACS group.[27] In a study of 63 ST elevation MI patients, iMAP-IVUS imaging was performed in the culprit segment and the segment immediately proximal to the culprit lesion (non-culprit). At index procedure the culprit lesion had a higher percentage of necrotic tissue compared to the non-culprit lesions. At 10 months follow-up the proportion of necrotic tissue in the non-culprit lesion remained stable, but the percentage of lipidic tissue decreased.[28] Like in studies with VH-IVUS, the necrotic plaque volume and necrotic plaque ratio by iMAP are predictors of slow flow during PCI.[29]
iMAP-IVUS has been used to evaluate neointimal tissue components after stent implantation. In a series of 61 lesions, iMAP-IVUS showed that neointima after drug eluting stent implantation consisted of statistically significant smaller fibrotic component, larger necrotic and calcified components compared with bare metal stent.[30]
Integrated Backscatter IVUS
Integrated backscatter IVUS (IB-IVUS) also uses a 40 MHz single rotational transducer.[31] It analyses the RF signals by applying a fast Fourier transformation. It has been used for assessment of vulnerable plaques. IB-IVUS studies have demonstrated that culprit lesions as well as non-culprit lesions of acute coronary syndrome are significantly associated with the increase in lipid component and decrease in fibrous component compared to those with stable angina pectoris.[32] The percentage of coronary lipid volume is independent predictor of no-reflow during PCI.[33] In a study of 260 patients, large lipid volume (odds ratio 1.95, 95 % confidence interval 1.14-3.33, P = 0.02) was significantly and independently associated with major adverse events defined as death, nonfatal myocardial infarction, and any repeat revascularisation during median follow-up of 1285 days after drug eluting stent implantation.[34] Serial IB-IVUS studies have demonstrated that statin therapy in patients with ACS reduces plaque volume and lipid components and increases in fibrous tissue content suggesting that statin therapy is able to induce plaque morphologic changes.[35]
Conclusion
IVUS-based imaging modalities allow us to improve our understanding of atherosclerotic disease and vulnerable plaque. Radiofrequency IVUS analysis enables identification of patients at high risk for future cardiovascular events and adverse outcomes following PCI. It can also be used to evaluate the effect of pharmacological treatment on coronary plaque morphology. Although IVUS radiofrequency analysis is a promising tool for identification of vulnerable plaque, the limitations are unproven clinical benefit and overall cost effectiveness. More research and randomised trials are needed to answer whether or not routine IVUS radiofrequency imaging is clinically relevant.
References
- 1.Yock PG, Linker DT, Angelsen BA. Two-dimensional intravascular ultrasound:technical development and initial clinical experience. J Am Soc Echocardiogr. 1989 Jul-Aug;2:296–304. doi: 10.1016/s0894-7317(89)80090-2. [DOI] [PubMed] [Google Scholar]
- 2.Mintz GS, Nissen SE, Anderson WD, Bailey SR, Erbel R, Fitzgerald PJ, Pinto FJ, Rosenfield K et al. American College of Cardiology clinical expert consensus document on standards for acquisition, measurement and reporting of intravascular ultrasound studies (IVUS). A report of the American College of Cardiology task force on clinical expert consensus documents. J Am Coll Cardiol. 2001 Apr;37:1478–92. doi: 10.1016/s0735-1097(01)01175-5. [DOI] [PubMed] [Google Scholar]
- 3.Lee SY, Mintz GS, Kim SY et al. Attenuated plaque detected by intravascular ultrasound: clinical, angiographic, and morphologic features and post-percutaneous coronary intervention complications in patients with acute coronary syndromes. JACC Cardiovasc Interv. 2009 Jan;2:65–72. doi: 10.1016/j.jcin.2008.08.022. [DOI] [PubMed] [Google Scholar]
- 4.Garcìa-Garcìa HM, Gogas BD, Serruys PW, Bruining N. IVUS-based imaging modalities for tissue characterization: similarities and differences. Int J Cardiovasc Imaging. 2011 Feb;27:215–24. doi: 10.1007/s10554-010-9789-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nair A, Kuban BD, Tuzcu EM et al. Coronary plaque classification with intravascular ultrasound radiofrequency data analysis. Circulation. 2002 Oct 22;106:2200–6. doi: 10.1161/01.cir.0000035654.18341.5e. [DOI] [PubMed] [Google Scholar]
- 6.Stone GW, Maehara A, Lansky AJ, de Bruyne B, Cristea E, Mintz GS, Mehran R, McPherson J et al. PROSPECT Investigators. A prospective natural-history study of coronary atherosclerosis. N Engl J Med. 2011 Jan 20;364:226–35. doi: 10.1056/NEJMoa1002358. [DOI] [PubMed] [Google Scholar]
- 7.Dohi T, Mintz GS, McPherson JA et al. Non-fibroatheroma lesion phenotype and long-term clinical outcomes: a substudy analysis from the PROSPECT study. JACC Cardiovasc Imaging. 2013 Aug;6:908–16. doi: 10.1016/j.jcmg.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 8.Calvert PA, Obaid DR, O’Sullivan M et al. Association between IVUS findings and adverse outcomes in patients with coronary artery disease: the VIVA (VH-IVUS in Vulnerable Atherosclerosis) Study. JACC Cardiovasc Imaging. 2011 Aug;4:894–901. doi: 10.1016/j.jcmg.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 9.Cheng JM, Garcia-Garcia HM, de Boer SP et al. In vivo detection of high-risk coronary plaques by radiofrequency intravascular ultrasound and cardiovascular outcome: results of the ATHEROREMO-IVUS study. Eur Heart J. 2014 Mar;35:639–47. doi: 10.1093/eurheartj/eht484. [DOI] [PubMed] [Google Scholar]
- 10.Virmani R, Kolodgie FD, Burke AP et al. Lessons from sudden coronary death: a comprehensive morphological classification scheme for atherosclerotic lesions. Arterioscler Thromb Vasc Biol. 2000 May;20:1262–75. doi: 10.1161/01.atv.20.5.1262. [DOI] [PubMed] [Google Scholar]
- 11.García-García HM, Mintz GS, Lerman A et al. Tissue characterization using intravascular radiofrequency data analysis: recommendations for acquisition, analysis, interpretation and reporting. EuroIntervention. 2009 Jun;5:177–89. doi: 10.4244/eijv5i2a29. [DOI] [PubMed] [Google Scholar]
- 12.Rodriguez-Granillo GA, García-García HM, Mc Fadden EP et al. In vivo intravascular ultrasound-derived thin-cap fibroatheroma detection using ultrasound radiofrequency data analysis. J Am Coll Cardiol. 2005 Dec 6;46:2038–42. doi: 10.1016/j.jacc.2005.07.064. [DOI] [PubMed] [Google Scholar]
- 13.Lefevre T, Erglis A, Gil R et al. Initial results of BLAST: bifurcation lesion analysis and stenting of thin cap fibroatheroma (TCFA/FA) as measured by VH-intravascular ultrasound – a global multicentre, prospective, randomised study. Eurointervention. 2011;790(Supplement M)(abstract) [Google Scholar]
- 14.Stone GW. VERDICT/FIRST: prospective, multi- center study examining the correlation between IVUS and FFR parameters in intermediate lesions. http://www.tctmd.com/show.aspx?id=114442 http://www.tctmd.com/show.aspx?id=114442 Available at:
- 15.Waksman R, Legutko J, Singh J et al. FIRST: Fractional Flow Reserve and Intravascular Ultrasound Relationship Study. J Am Coll Cardiol. 2013 Mar 5;61:917–23. doi: 10.1016/j.jacc.2012.12.012. [DOI] [PubMed] [Google Scholar]
- 16.Jang JS, Jin HY, Seo JS et al. Meta-analysis of plaque composition by intravascular ultrasound and its relation to distal embolization after percutaneous coronary intervention. Am J Cardiol. 2013 Apr 1;111:968–72. doi: 10.1016/j.amjcard.2012.12.016. [DOI] [PubMed] [Google Scholar]
- 17.Claessen BE, Maehara A, Fahy M et al. Plaque composition by intravascular ultrasound and distal embolization after percutaneous coronary intervention. JACC Cardiovasc Imaging. 2012 Mar;5(3 Suppl):S111–8. doi: 10.1016/j.jcmg.2011.11.018. [DOI] [PubMed] [Google Scholar]
- 18.Nakamura T, Kubo N, Ako J, Momomura S. Angiographic no-reflow phenomenon and plaque characteristics by virtual histology intravascular ultrasound in patients with acute myocardial infarction. J Interv Cardiol. 2007 Oct;20:335–9. doi: 10.1111/j.1540-8183.2007.00282.x. [DOI] [PubMed] [Google Scholar]
- 19.Bae JH, Kwon TG, Hyun DW et al. Predictors of slow flow during primary percutaneous coronary intervention: an intravascular ultrasound-virtual histology study. Heart. 2008 Dec;94:1559–64. doi: 10.1136/hrt.2007.135822. [DOI] [PubMed] [Google Scholar]
- 20.Hong YJ, Mintz GS, Kim SW et al. Impact of plaque composition on cardiac troponin elevation after percutaneous coronary intervention: an ultrasound analysis. JACC Cardiovasc Imaging. 2009 Apr;2:458–68. doi: 10.1016/j.jcmg.2008.12.020. [DOI] [PubMed] [Google Scholar]
- 21.Kitabata H, Loh JP, Pendyala LK et al. Intra-stent tissue evaluation within bare metal and drug-eluting stents >3 years since implantation in patients with mild to moderate neointimal proliferation using optical coherence tomography and virtual histology intravascular ultrasound. Cardiovasc Revasc Med. 2014 Apr;15:149–55. doi: 10.1016/j.carrev.2014.01.009. [DOI] [PubMed] [Google Scholar]
- 22.Puri R, Libby P, Nissen SE et al. Long-term effects of maximally intensive statin therapy on changes in coronary atheroma composition: insights from SATURN. Eur Heart J Cardiovasc Imaging. 2014 Apr;15:380–8. doi: 10.1093/ehjci/jet251. [DOI] [PubMed] [Google Scholar]
- 23.Tian J, Gu X, Sun Y et al. Effect of statin therapy on the progression of coronary atherosclerosis. BMC Cardiovasc Disord. 2012 Sep 1;12:70. doi: 10.1186/1471-2261-12-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ko YG, Choi SH, Chol Kang W Effects of Combination Therapy with Cilostazol and Probucol versus Monotherapy with Cilostazol on Coronary Plaque, Lipid and Biomarkers: SECURE Study, a Double-Blind Randomized Controlled Clinical Trial. J Atheroscler Thromb. 2014. Apr 4, [Epub ahead of print] [DOI] [PubMed]
- 25.Sathyanarayana S, Carlier S, Li W, Thomas L. Characterisation of atherosclerotic plaque by spectral similarity of radiofrequency intravascular ultrasound signals. EuroIntervention. 2009 May;5:133–9. doi: 10.4244/eijv5i1a21. [DOI] [PubMed] [Google Scholar]
- 26.Shin ES, Garcia-Garcia HM, Ligthart JM et al. In vivo findings of tissue characteristics using iMap™ IVUS and Virtual Histology™ IVUS. EuroIntervention. 2011 Mar;6:101–79. doi: 10.4244/EIJV6I8A175. [DOI] [PubMed] [Google Scholar]
- 27.Kozuki A, Shinke T, Otake H et al. Feasibility of a novel radiofrequency signal analysis for in-vivo plaque characterization in humans: comparison of plaque components between patients with and without acute coronary syndrome. Int J Cardiol. 2013 Aug 20;167:1591–6. doi: 10.1016/j.ijcard.2012.04.102. [DOI] [PubMed] [Google Scholar]
- 28.Trusinskis K, Juhnevica D, Strenge K, Erglis A. iMap intravascular ultrasound evaluation of culprit and non-culprit lesions in patients with ST-elevation myocardial infarction. Cardiovasc Revasc Med. 2013. Mar-Apr. pp. 71–5. [DOI] [PubMed]
- 29.Utsunomiya M, Hara H, Sugi K, Nakamura M. Relationship between tissue characterisations with 40 MHz intravascular ultrasound imaging and slow flow during coronary intervention. EuroIntervention. 2011 Jul;7:340–6. doi: 10.4244/EIJV7I3A58. [DOI] [PubMed] [Google Scholar]
- 30.Tsujita K, Takaoka N, Kaikita K et al. Neointimal tissue component assessed by tissue characterization with 40 MHz intravascular ultrasound imaging: comparison of drug-eluting stents and bare-metal stents. Catheter Cardiovasc Interv. 2013 Dec 1;82:1068–74. doi: 10.1002/ccd.24907. [DOI] [PubMed] [Google Scholar]
- 31.Kawasaki M, Takatsu H, Noda T et al. Noninvasive quantitative tissue characterization and two-dimensional color-coded map of human atherosclerotic lesions using ultrasound integrated backscatter: comparison between histology and integrated backscatter images. J Am Coll Cardiol. 2001 Aug;38:486–92. doi: 10.1016/s0735-1097(01)01393-6. [DOI] [PubMed] [Google Scholar]
- 32.Ando H, Amano T, Matsubara T et al. Comparison of tissue characteristics between acute coronary syndrome and stable angina pectoris. An integrated backscatter intravascular ultrasound analysis of culprit and non-culprit lesions. Circ J. 2011;75:383–90. doi: 10.1253/circj.cj-10-0815. [DOI] [PubMed] [Google Scholar]
- 33.Daidoji H, Takahashi H, Otaki Y A combination of plaque components analyzed by integrated backscatter intravascular ultrasound (IB-IVUS) and serum pregnancy-associated plasma protein A (PAPP-A) levels predict the no-reflow phenomenon during percutaneous coronary intervention (PCI). Catheter Cardiovasc Interv. 2013. Nov 13, [DOI] [PubMed]
- 34.Kumagai S, Takashima H, Waseda K Prognostic impact of lipid contents on the target lesion in patients with drug eluting stent implantation. Heart Vessels. 2013. Oct 20, [Epub ahead of print] [DOI] [PubMed]
- 35.Otagiri K, Tsutsui H, Kumazaki S et al. Early intervention with rosuvastatin decreases the lipid components of the plaque in acute coronary syndrome: analysis using integrated backscatter IVUS (ELAN study). Circ J. 2011;75(3):633–41. doi: 10.1253/circj.cj-10-0600. [DOI] [PubMed] [Google Scholar]
- 36.Nair A, Margolis MP, Kuban BD, Vince DG. Automated coronary plaque characterisation with intravascular ultrasound backscatter: ex vivo validation. EuroIntervention. 2007 May;3(1):113–20. [PubMed] [Google Scholar]
- 37.Kawasaki M, Bouma BE, Bressner J et al. Diagnostic accuracy of optical coherence tomography and integrated backscatter intravascular ultrasound images for tissue characterization of human coronary plaques. J Am Coll Cardiol. 2006 Jul 4;48:81–8. doi: 10.1016/j.jacc.2006.02.062. [DOI] [PubMed] [Google Scholar]
- 38.Kubo T, Nakamura N, Matsuo Y et al. Virtual histology intravascular ultrasound compared with optical coherence tomography for identification of thin-cap fibroatheroma. Int Heart J. 2011;52(3):175–9. doi: 10.1536/ihj.52.175. PubMed PMID: [DOI] [PubMed] [Google Scholar]


