Abstract
Objective
To evaluate the temperature distribution among moderately preterm (MPT, 29–33 weeks) and extremely preterm (EPT, <29 weeks) infants upon neonatal intensive care unit (NICU) admission in 2012–2013, the change in admission temperature distribution for EPT infants between 2002–2003 and 2012–2013, and associations between admission temperature and mortality and morbidity for both MPT and EPT infants.
Study design
Prospectively collected data from 18 centers in the Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network were used to examine NICU admission temperature of inborn MPT and EPT infants. Associations between admission temperature and mortality and morbidity were determined by multivariable logistic regression. EPT infants from 2002–2003 and 2012–2013 were compared.
Results
MPT and EPT cohorts consisted of 5818 and 3213 infants, respectively. The distribution of admission temperatures differed between the MPT vs EPT (P < .01), including the percentage <36.5°C (38.6% vs 40.9%), 36.5°C–37.5°C (57.3% vs 52.9%), and >37.5°C (4.2% vs 6.2%). For EPT infants in 2012–2013 compared with 2002–2003, the percentage of temperatures between 36.5°C and 37.5°C more than doubled and the percentage of temperatures >37.5°C more than tripled. Admission temperature was inversely associated with in-hospital mortality.
Conclusions
Low and high admission temperatures are more frequent among EPT than MPT infants. Compared with a decade earlier, fewer EPT infants experience low admission temperatures but more have elevated temperatures. In spite of a change in distribution of NICU admission temperature, an inverse association between temperature and mortality risk persists.
The National Institute of Child Health and Human Development Neonatal Research Network (NRN) reported admission temperatures of inborn infants with birth weights 401–1499 g born in 2002 and 2003.1 Low admission temperatures were common (46.9% were <36.0°C) and were inversely associated with the risks of mortality and late-onset sepsis. Multiple randomized trials, primarily in extremely preterm (EPT) neonates, have tested interventions to reduce the proportion of infants admitted to neonatal intensive care units (NICUs) with low temperatures. Interventions tested included polyethylene wraps,2 exothermic mattresses,3,4 polyethylene caps,5 active warming during cesarean delivery,6 increased delivery room temperature,7 and humidified and heated air during stabilization.8 Evidence-based interventions to prevent low temperatures at birth are now part of neonatal resuscitation.9 Quality improvement initiatives demonstrated a reduced proportion of preterm infants with low temperatures upon NICU admission,10–12 but elevated admission temperatures also have been reported among preterm infants who received interventions to prevent low temperatures.13–16
In view of the efforts to prevent hypothermia at birth, it is likely that the distribution of admission temperatures has changed compared with our earlier report.1 A recent time-limited observational study of moderately preterm (MPT) infants (290–336 weeks of gestation) conducted by the NRN combined with a standing registry of mortality and morbidity for EPT infants, <29 weeks) facilitated examination of admission temperature over a broad gestational age range. The objectives of this report were to determine the frequency of low and high admission temperature among a recent cohort of MPT and EPT infants born in 2012 and 2013, the change in distribution of admission temperature among EPT infants compared with those born in 2002 and 2003, and associations between admission temperature and mortality and morbidity in both the MPT and EPT infant cohorts.
Methods
This study analyzed prospectively collected maternal and infant data abstracted from the medical record by trained research nurses at 18 centers of the Eunice Kennedy Shriver National Institute of Child Health and Human Development’s NRN. Data were entered into a computerized database approved by the institutional review board at each participating site. Inclusion criteria were infants who were born at an NRN center and admitted directly to the NICU from a delivery or operating room with a gestational age between 220 and 336 weeks. Data were collected from March 1, 2012 through October 31, 2013 for MPT infants with gestational ages of 290 through 336 weeks (MPT) and throughout 2012 and 2013 for EPT infants with gestational ages of 220 through 286 weeks (EPT). Exclusion criteria included congenital brain malformations, malformations resulting in an open lesion (eg, myelomeningocele, abdominal wall defects), noninitiation of medical therapy for infants who died within 12 hours, a prenatal diagnosis with a decision to withdraw or limit intensive care, missing admission temperature measurements, and first temperature recorded at >2 hours of age.
The first temperature after NICU admission from Labor and Delivery was recorded as the admission temperature. For centers that admit infants to a holding area or delivery room stabilization area, the first temperature recorded in this area was recorded as the admission temperature. The date and time of the admission temperature and the site of temperature measurement (axilla, rectal, or skin) were recorded. Temperatures recorded in the delivery room or during transport to the NICU were not recorded. Use of a thermal wrap (NeoWrap [Fisher-Paykel Healthcare, Auckland, New Zealand], or thin plastic food wrap) was collected if this information was available. The database does not contain information on any other intervention to maintain temperature at birth (eg, exothermic mattress, hat, etc).
Data for 2012–2013 included (1) maternal variables including maternal hypertension, multiple births, antenatal steroids, antibiotics; (2) intrapartum variables including chorioamnionitis (clinical and histologic), duration of rupture of membranes, and delivery mode; (3) infant characteristics including birth weight, gestational age (obstetric estimate), sex, race, and ethnicity; (4) delivery room events including intubation, chest compressions, medications, and Apgar scores; and (5) Network center. Neonatal outcomes included death before discharge, highest mode of respiratory support at day 28 (high-frequency or conventional ventilation, continuous positive airway pressure, nasal cannula/oxygen, or no support), grade III or IV (severe) intracranial hemorrhage (ICH), early or late-onset sepsis (positive blood culture before or after 72 hours, respectively), and necrotizing enterocolitis (NEC, modified Bell’s stage II or above treated medically or surgically17). Neonatal outcomes were collected until hospital discharge, 120 days or death, whichever came first.
For comparison of 2012–2013 and 2002–2003, data were used only from centers participating in the NRN during both epochs. Infants with admission temperatures and born in 2002–2003 were included if they had gestational ages of 220–286 weeks.
A temperature of 36.5°C–37.5°C was considered normothermia as suggested by the World Health Organization.18 Descriptive statistics characterized the distribution of admission temperatures among MPT and EPT infants. Statistical significance was calculated using χ2 tests and logistic regressions. Associations between admission temperature and neonatal outcomes were initially explored with bivariate analyses. Variables significant at the 0.10 level were entered into logistic regression models to adjust for covariates using admission temperature as a continuous variable. Variables included in the models were antenatal steroid exposure, sex, race, birth weight, intubation, Apgar at 5 minutes, center, prematurity level (MPT or EPT), and the interaction between admission temperature and type of infant (MPT/EPT) if present. Results were expressed using ORs and 95% CIs. The results prompted 2 post-hoc analyses. Short-term outcomes of EPT infants with admission temperatures >37.5°C were explored with adjusted logistic regression for differences with infants whose admission temperature was 36.5°C–37.5°C or <36.5°C. The sample size was determined by the number of infants available in the database registries. With the available MPT and EPT infants in 2012–2013, the power was greater than 90% among both cohorts to detect a 10% reduction in the frequency of admission temperature less than 36.0°C based on 2002–2003 data.
In a sensitivity analysis, associations were evaluated between missing temperatures and mortality. Two logistic regression models adjusting for the above listed covariates were run: the first comparing mortality among MPT and EPT infants between those missing vs those not missing admission temperatures and a second model comparing mortality between the 4 categories of admission temperature (<36.5°C, 36.5°C–37.5°C, >37.5°C, and missing).
Results
During 2012–2013, a total of 10 965 infants were entered into the Moderate Preterm Database (7051 MPT) and Generic Database (3914 EPT) with gestational ages from 220 to 336 weeks. The final cohort included 9031 infants (5818 MPT and 3213 EPT) after excluding 705 (6.4%) outborn infants (637 MPT and 68 EPT), 405 (3.7%) infants with anomalies or limited care, and 824 (7.5%) infants with missing or late admission temperature recordings. Exclusions because of missing temperature or time of temperature recordings were similar for MPT and EPT infants (7.1% and 9.6% of eligible infants, respectively).
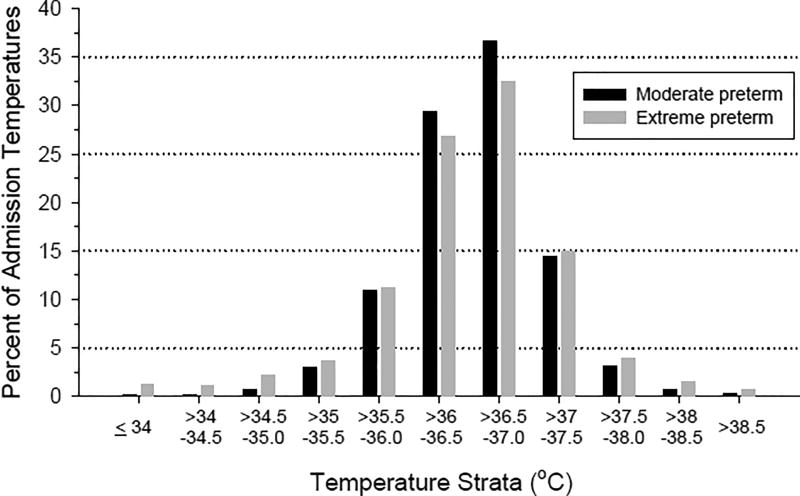
Table I shows characteristics of the MPT and EPT cohorts and their associated admission temperatures. The age of the admission temperature was earlier for MPT compared with EPT infants. The distribution of the temperature site (axillary, rectal, skin) used for admission temperature differed slightly; MPT had more rectal and fewer skin temperatures compared with EPT. Median and range of admission temperatures for MPT and EPT were similar, but the distribution differed. More MPT infants than EPT infants had admission temperatures 36.5°C–37.5°C, but fewer MPT infants had admission temperatures <36.5°C or >37.5°C. MPT infants with missing admission temperatures were similar with respect to the variables in Table I except for less use of maternal antibiotics (63.6%, P < .0001), more frequent 5-minute Apgar score <7 (15.9%, P < .001) and more frequent cardiopulmonary resuscitation (3.9%, P < .001). Deaths among MPT infants with admission temperatures (1.9%) did not differ from infants without an admission temperature (3.1%, P = .09). EPT infants with missing admission temperatures differed from those who had admission temperatures with less use of maternal antibiotics (68.9%, P = .0017) and antenatal steroids (86.6%, P = .003), lower birth weight (780 ± 240 g, P < .0001) and gestational age (25.3 ± 1.7, P < .0001), more frequent 5-minute Apgar scores <7 (59.8%, P < .0001), and more frequent cardiopulmonary resuscitation (24.5%, P < .0001). Deaths among EPT infants with admission temperatures (14.3%) differed from infants without an admission temperature (39.5%, P < .0001). Admission temperatures by 0.5°C strata are plotted in Figure 1 (available at www.jpeds.com). The relationship between gestational age and admission temperatures for MPT and EPT is shown in Table II. Excessive missing data for thermal wraps prevented analysis of their use for thermal protection.
Table I.
Descriptive characteristics and admission temperatures of the study cohort
| EPT n = 3213 |
MPT n = 5818 |
P value | |
|---|---|---|---|
| Maternal* | |||
| Medications received | |||
| Antibiotics | 2448 (76.3) | 4315 (74.2) | .03 |
| Antenatal steroids | 2932 (91.3) | 5144 (88.6) | <.01 |
| Hypertension | 908 (28.3) | 2075 (35.7) | <.01 |
| Intrapartum | |||
| Multiple births | 916 (28.5) | 1756 (30.2) | .10 |
| PROM, >18 h | 831 (26.0) | 1127 (20.4) | <.01 |
| Cesarean delivery | 2194 (68.3) | 3674 (63.2) | <.01 |
| Chorioamnionitis | 1454 (49.3) | 1443 (27.7) | <.01 |
| Infant characteristics | |||
| Birth weight | 868 ± 244 | 1698 ± 421 | <.01 |
| Gestational age | 26.0 ± 1.7 | 31.5 ± 1.4 | <.01 |
| Male | 1642 (51.2) | 3003 (51.6) | .66 |
| Race | <.01 | ||
| Black | 1290 (41.5) | 1937 (34.9) | |
| White | 1600 (51.5) | 3225 (58.1) | |
| Other | 216 (6.9) | 389 (7.0) | |
| Hispanic | 439 (13.8) | 874 (15.3) | .05 |
| Delivery room | |||
| Apgar at 1 min <7 | 2539 (79.3) | 2440 (42.0) | <.01 |
| Apgar at 5 min <7 | 1343 (41.9) | 684 (11.8) | <.01 |
| Intubation | 2139 (66.6) | 850 (14.6) | <.01 |
| Bag/mask vent | 2487 (77.5) | 2287 (39.3) | <.01 |
| Compression ± epinephrine | 230 (7.2) | 95 (1.6) | <.01 |
| CPAP | 707 (22.0) | 195 (3.3) | <.01 |
| Admission temperature | |||
| Postnatal age (min) | 24.4 ± 13.0 | 22.0 ± 12.5 | <.01 |
| Site of temperature recording (%) | <.01 | ||
| Axilla | 84.5 | 84.9 | |
| Rectal | 11.7 | 13.7 | |
| Skin | 3.8 | 1.4 | |
| Temperature (°C) | 36.6 (30.7–40.5) | 36.6 (30.3–39.6) | |
| % temperatures 36.5–37.5 | 52.9 | 57.3 | <.01 |
| % temperatures <36.5 | 40.9 | 38.6 | |
| % temperatures >37.5 | 6.2 | 4.2 |
CPAP, continuous positive airflow pressure; PROM, prolong rupture of membranes.
MPT infants 290– 336 weeks born March 1, 2012–October 31, 2013.
EPT infants 220 – 286 weeks born January 2012–December 2013.
Categorical data are presented as n (%) where percentages are calculated based on non-missing data. Continuous data are presented as mean ± SD or median and range (admission temperature). P values for categorical data were calculated using chi-square and continuous data using the Wilcoxon test.
Fig 1.
The distribution of admission temperatures among preterm infants
Table II.
Admission temperature by gestational age
| Admission temperature (%) | |||||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Gestational age (wk) | n | Birth weight ± SD (g) | <35°C | 35.0°C–36.4°C | 36.5°C–37.5°C | 37.6°C–38.0°C | >38°C |
| MPT infants | |||||||
| 33 | 1868 | 1996 ± 369 | 0.7 | 36.1 | 59.8 | 2.7 | 0.8 |
| 32 | 1387 | 1784 ± 338 | 0.7 | 33.3 | 61.6 | 3.3 | 1.1 |
| 31 | 1027 | 1585 ± 319 | 1.7 | 38.7 | 55.6 | 3.5 | 0.6 |
| 30 | 881 | 1392 ± 281 | 1.3 | 44.2 | 50.4 | 2.8 | 1.4 |
| 29 | 655 | 1251 ± 250 | 0.5 | 41.1 | 52.7 | 4.0 | 1.8 |
| EPT infants | |||||||
| 28 | 808 | 1091 ± 213 | 1.2 | 34.2 | 58.7 | 4.1 | 1.9 |
| 27 | 654 | 966 ± 198 | 1.4 | 32.0 | 59.5 | 5.1 | 2.1 |
| 26 | 569 | 841 ± 169 | 2.5 | 33.4 | 56.6 | 4.9 | 2.6 |
| 25 | 508 | 745 ± 140 | 3.4 | 41.3 | 49.4 | 2.8 | 3.2 |
| 24 | 410 | 653 ± 111 | 8.8 | 43.9 | 42.0 | 3.4 | 2.0 |
| 23 | 210 | 590 ± 92 | 9.1 | 50.5 | 36.7 | 1.9 | 1.9 |
| 22 | 54 | 520 ± 64 | 31.5 | 39.0 | 29.6 | 0.0 | 0.0 |
MPT infants 290–336 weeks born March 1, 2012–October 31, 2013.
EPT infants 220–286 weeks born January 2012–December 2013.
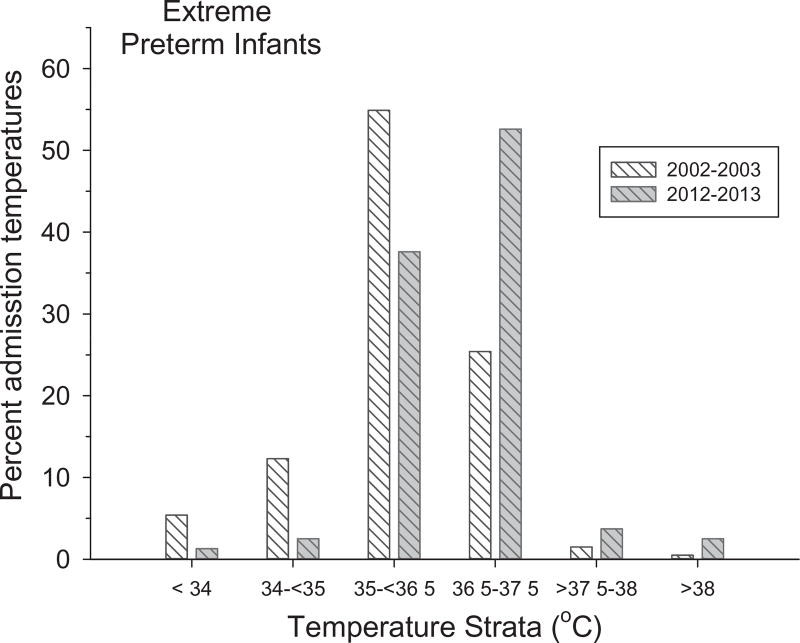
For comparison of EPT infants between 2002–2003 and 2012–2013, there were a total of 4353 admission temperatures (2270 and 2083, respectively). Compared with 2002–2003 (Figure 2), the percentage of admission temperatures between 36.5°C and 37.5°C more than doubled in 2012–2013 and was mirrored by reductions in admission temperatures <36.5°C. In contrast, admission temperatures >37.5°C increased 3-fold (2.0%–6.1%). EPT infants evaluated in 2002–2003 were similar to those evaluated in 2012–2013 in birth weight (872 ± 233 g vs 858 ± 234 g), gestational age (26.0 ± 1.6 weeks vs 26.0 ± 1.6 weeks) and sex (53.8% vs 51.8% male) but had less frequent 5-minute Apgar <7 (39.0% vs 43.7%, P = .0015), and more frequent intubation at birth (73.8% vs 60.2%, P < .0001). Post-hoc analysis of EPT infants in 2012–2013 with admission temperatures >37.5°C compared with infants with admission temperatures of <36.5°C or 36.5°C–37.5°C indicated no differences in 1- and 5-minute Apgar score, frequency of cardiopulmonary resuscitation, mortality, severe ICH, highest respiratory support, early or late-onset sepsis, or NEC. EPT infants with an admission temperature <36.5°C or 36.5°C–37.5°C had lower odds of intubation (OR 0.54, 95% CI 0.36–0.82 and OR 0.65, 95% CI 0.44–0.96, respectively) compared with infants with an admission temperature >37.5°C adjusted for antenatal steroids, sex, race, and gestational age.
Figure 2.
The distribution of admission temperature is plotted among 6 strata of temperature for EPT infants for 2002–2003 (white cross hatch) and 2012–2013 (gray cross hatch).
EPT infants had higher rates of mortality, respiratory support, severe ICH, early onset sepsis, late onset sepsis, and NEC than MPT infants (P < .01, Table III). The acquisition of cranial ultrasounds differed between cohorts (56.4% MPT, 96% EPT). Adjusted associations between admission temperature and mortality and morbidities are summarized in Table III. Significant interactions between prematurity level (MPT/EPT) and admission temperature indicate that the association of admission temperature and a specific outcome varied for EPT and MPT infants; ORs are listed for each prematurity level. Over the range of admission temperatures in this study, the odds of mortality decreased for each 1°C increase in admission temperature (OR 0.81, CI 0.71–.91). The absence of an interaction with prematurity level indicated that this association extended across gestational ages of 220–336 weeks. Associations between admission temperature and respiratory support at 28 days, severe ICH, and early-onset sepsis were present only among MPT infants; the odds of each outcome increased for each 1°C increase in admission temperature. There was no association between admission temperature and either late-onset sepsis or NEC.
Table III.
Frequency of mortality and morbidity among MPT and EPT cohorts and adjusted association between admission temperatures and mortality/morbidity
| Outcomes | MPT n = 5818 |
EPT n = 3213 |
OR* (95% CI) |
P value |
|---|---|---|---|---|
| Mortality | 1.9% | 14.3% | 0.81 (0.71–0.91) | <.001 |
| Respiratory support† | 4.9% | 62.3% | MPT: 1.61 (1.12–2. 13) | .019 |
| EPT: 0.93 (0.75–1.16) | ||||
| Severe ICH‡ | 1.3% | 12.7% | MPT: 1.88 (1.14–3.11) | .003 |
| EPT: 0.87 (0.75–1.00) | ||||
| Early onset sepsis§ | 0.6% | 2.1% | MPT: 2.25 (1.26–4.00) | .013 |
| EPT: 0.99 (0.73–1.35) | ||||
| Late onset sepsis | 3.1% | 20.1% | 0.92 (0.82–1.02) | .122 |
| NEC¶ | 2.4% | 8.7% | 0.97 (0.83–1.12) | .640 |
Adjusted association represents the odds of mortality or morbidity for each 1°C increase in admission temperature. Regressions were adjusted for antenatal steroids, sex, race, birth weight, intubation, Apgar at 5 minutes, center, type of infant (MPT or EPT), and interactions if present. If the interaction between the prematurity level (MPT/EPT) and admission temperature was significant, it indicated that the association of admission temperature and a specific outcome varied across the 2 cohorts and ORs are listed for each prematurity level.
Adjusted for an interaction between admission temperature and type of infant. Respiratory support was the use of ventilation (conventional, high frequency) relative to no support.
Adjusted for an interaction between admission temperature and type of infant.
Adjusted for an interaction between admission temperature and type of infant.
NEC treated medically or surgically.
In a sensitivity analysis, mortality was higher among infants with missing admission temperatures compared with those with documented admission temperatures (P = .029). This association was present for EPT (OR 2.25, CI 1.69–2.99) but not MPT infants (OR 1.04, CI .55–1.97). For EPT infants with documented admission temperatures, the odds of mortality were lower within each category of admission temperature (<36.5°C, 36.5°C–37.5°C, >37.5°C) compared with infants with missing admission temperatures (P = .57, P = .33, P = .44, respectively).
Discussion
The principal findings of this study were that the distribution of admission temperatures differed between MPT and EPT infants born at 18 centers of the NRN in 2012–2013, the distribution of admission temperatures in EPT infants differed markedly compared with 10 years earlier in a subset of NRN centers, and that admission temperature was associated with the odds of important outcomes, most notably in-hospital mortality.
Although MPT and EPT infants had similar median admission temperatures, the distribution differed and EPT infants had fewer temperatures between 36.5°C and 37.5°C and more temperatures less than 36.5°C. This presumably reflects the higher ratio of body surface area to weight and other thermal disadvantages of EPT compared with MPT infants. A limitation of our study is the absence of data on interventions used at NRN sites to minimize heat loss. It is unclear if differences in temperature distribution between MPT and EPT reflect solely heat loss, measures to avoid heat loss or a combination of both. However, differences in temperature distribution among MPT and EPT are not striking, and both gestational age cohorts have a large percent of infants with admission temperatures <36.5°C. The distribution of admission temperatures is similar to data reported by the Canadian Neonatal Network for 9833 infants born at <33 weeks gestation between 2010 and 2012.19
EPT infants in the current report had a higher frequency of elevated admission temperatures compared with MPT infants. This has been noted with implementation of placing EPT infants in plastic bags at birth13–16 and use of plastic bags combined with exothermic mattresses,4 but has not been universally reported. For example, a multidisciplinary practice plan (occlusive wrap, exothermic mattress, caps, and increased room temperature) decreased low admission temperatures in preterm infants without an increase in temperatures >37.5°C.20 We cannot distinguish whether the elevated temperatures among NRN EPT infants reflected interventions to avoid hypothermia or maternal conditions (eg, fever associated with chorioamnionitis or epidural analgesia).21
In our prior report, 46.9% of infants with a birth weight <1500 g had an admission temperature <36.0°C.1 Compared with EPT infants born in 2002–2003, EPT infants born in 2012–2013 had a dramatic shift in the distribution of their admission temperatures; fewer infants had lower temperatures but more had elevated temperatures. These changes presumably reflect a greater focus on avoiding low temperatures after birth by adopting strategies to attenuate heat loss. Term infants exposed to peripartum maternal pyrexia have higher rates of respiratory depression at birth, seizures, encephalopathy and cerebral palsy.22–25 Our post-hoc analyses suggest that elevated temperatures at birth among EPT infants are not associated with more frequent short-term morbidities, but the odds of intubation were higher among hyperthermic infants.
In the current study, an inverse relationship between admission temperature and in-hospital mortality was found, as previously reported.1 Of note, the distribution of admission temperatures differed from infants born in 2002–2003. Multiple publications have reported a similar association. These include the EPICure study (infants <27 weeks’ gestation),26 the California Perinatal Quality Care Collaborative (infants with a birth weight <1500 g),27 the Brazilian Network of Neonatal Research (23–33 weeks),28 and the Canadian Neonatal Network.19 Consistent with these observations is a systematic review of prediction models for mortality among preterm infants.29 Among 59 studies (1998–2010), 8 variables predicted survival, including a normal temperature on admission. The association between admission temperature and mortality prompted a randomized trial of polyethylene wraps at birth to improve survival. Among infants 240–276 weeks, wraps did not change mortality (aOR 0.9, 95% CI 0.6–1.3) between groups despite different baseline admission temperature (36.3°C vs 35.7°C, wrap vs no wrap, P < .0001).16 Similar mortality between groups with different admission temperatures may reflect a relatively small, albeit significant difference of admission temperatures between groups. Whether a bundle of interventions to prevent hypothermia at birth would result in wider separation of admission temperatures between groups and alter mortality is unclear. Although mortality was similar between intervention groups, mortality rose with lower baseline temperatures and was most prominent at the extremes of temperature (<35.5°C).16 The available data from Reilly et al as well as the results of our current and prior publication1 do not distinguish whether temperature is causally linked with mortality or if temperature is simply a marker of mortality risk.16
An association between admission temperature and late-onset sepsis was not found in the current study, in contrast to our prior findings.1 Reductions in late-onset sepsis have been documented in the NRN as recently reported in an analysis of care practices, morbidity, and mortality over 20 years.30 These results mirror quality initiatives to reduce nosocomial infection.31,32 For MPT infants, increasing admission temperature was associated with higher odds of respiratory support at 28 days, severe ICH, and early onset sepsis. We did not investigate bronchopulmonary dysplasia because of limitations in applying the same diagnostic criteria to MPT and EPT. Caution is needed when considering these findings given the low frequency of morbidities among MPT infants and that cranial ultrasound examinations were not routinely performed among MPT infants. These results differ from the Canadian Neonatal Network, which demonstrated a U-shaped relationship between admission temperature and individual morbidities for infants <33 weeks including severe neurologic injury, severe retinopathy of prematurity, NEC, bronchopulmonary dysplasia, nosocomial infection, and duration of ventilation.19
There are limitations to this study. Data were not available on interventions to reduce heat loss at birth, maternal and delivery room temperatures, and use of epidural anesthesia. Data were missing for the admission temperature or the time of the temperature for both MPT and EPT infants, and some infants with missing admission temperatures differed in selected characteristics from those with available temperatures. The magnitude of the association between admission temperature and mortality may be underestimated given the higher mortality among infants with missing temperatures. Strengths of this study include a large sample size from a contemporary cohort of preterm infants, prospective data collection, and predefined morbidities.
Over the past 10 years, there has been a dramatic shift in the distribution of admission temperatures among EPT infants. There are more admission temperatures in the desired range, and fewer lower temperatures at a small cost of more frequent higher temperatures. In spite of the change in temperature distribution, approximately 40% of both EPT and MPT infants had admission temperatures <36.5°C, and lower admission temperatures were associated with in-hospital mortality. These data support ongoing surveillance of admission temperatures and quality improvement efforts to avoid hypothermia balanced with the potential for elevated temperatures upon NICU admission.
Acknowledgments
Funded by the National Institutes of Health (M01 RR80), the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) (U10 HD21364, U10 HD21373, U10 HD21385, U10 HD27851, U10 HD27853, U10 HD27856, U10 HD27880, U10 HD27904, U10 HD34216, U10 HD36790, U10 HD40492, U10 HD40689, U10 HD53089, U10 HD53109, U10 HD68244, U10 HD68263, U10 HD68270, U10 HD68278, U10 HD68284), and the National Center for Advancing Translational Sciences (UL1 TR6, UL1 TR41, UL1 TR42, UL1 TR77, UL1 TR93, UL1 TR442, UL1 TR454, UL1 TR1117, UL1 TR1111). The National Institutes of Health, NICHD, and the National Center for Advancing Translational Sciences provided grant support for the Neonatal Research Network’s (NRN) Generic Database and Moderate Preterm Registry through cooperative agreements. Participating NRN sites collected data and transmitted it to RTI International, the data coordinating center for the network, which stored, managed, and analyzed the data for this study. Although NICHD staff did have input into the study design, conduct, analysis, and manuscript drafting, the content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Glossary
- EPT
Extremely preterm
- ICH
Intracranial hemorrhage
- MPT
Moderately preterm
- NEC
Necrotizing enterocolitis
- NICU
Neonatal intensive care unit
- NRN
Neonatal Research Network
Footnotes
The authors declare no conflicts of interest.
We are indebted to our medical and nursing colleagues and the infants and their parents who agreed to take part in this study.
References
- 1.Laptook AR, Salhab W, Bhaskar B, Neonatal Research Network Admission temperature of low birth weight infants: predictors and associated morbidities. Pediatrics. 2007;119:e643–9. doi: 10.1542/peds.2006-0943. [DOI] [PubMed] [Google Scholar]
- 2.Vohra S, Roberts RS, Zhang B, Janes M, Schmidt B. Heat Loss Prevention (HeLP) in the delivery room: a randomized controlled trial of polyethylene occlusive skin wrapping in very preterm infants. J Pediatr. 2004;145:750–3. doi: 10.1016/j.jpeds.2004.07.036. [DOI] [PubMed] [Google Scholar]
- 3.Simon P, Dannaway D, Bright B, Krous L, Wlodaver A, Burks B, et al. Thermal defense of extremely low gestational age newborns during resuscitation: exothermic mattresses vs polyethylene wrap. J Perinatol. 2011;31:33–7. doi: 10.1038/jp.2010.56. [DOI] [PubMed] [Google Scholar]
- 4.McCarthy LK, Molloy EJ, Twomey AR, Murphy JF, O’Donnell CP. A randomized trial of exothermic mattresses for preterm newborns in polyethylene bags. Pediatrics. 2013;132:e135–41. doi: 10.1542/peds.2013-0279. [DOI] [PubMed] [Google Scholar]
- 5.Trevisanuto D, Doglioni N, Cavallin F, Parotto M, Micaglio M, Zanardo V. Heat loss prevention in very preterm infants in delivery rooms: a prospective, randomized, controlled trial of polyethylene caps. J Pediatr. 2010;156:914–7. e1. doi: 10.1016/j.jpeds.2009.12.021. [DOI] [PubMed] [Google Scholar]
- 6.Horn EP, Schroeder F, Gottschalk A, Sessler DI, Hiltmeyer N, Standl T, et al. Active warming during cesarean delivery. Anesth Analg. 2002;94:409–14. doi: 10.1097/00000539-200202000-00034. table of contents. [DOI] [PubMed] [Google Scholar]
- 7.Jia YS, Lin ZL, Lv H, Li YM, Green R, Lin J. Effect of delivery room temperature on the admission temperature of premature infants: a randomized controlled trial. J Perinatol. 2013;33:264–7. doi: 10.1038/jp.2012.100. [DOI] [PubMed] [Google Scholar]
- 8.Meyer MP, Hou D, Ishrar NN, Dito I, te Pas AB. Initial respiratory support with cold, dry gas versus heated humidified gas and admission temperature of preterm infants. J Pediatr. 2015;166:245–50. e1. doi: 10.1016/j.jpeds.2014.09.049. [DOI] [PubMed] [Google Scholar]
- 9.Wyckoff MH, Aziz K, Escobedo MB, Kapadia VS, Kattwinkel J, Perlman JM, et al. Part 13: neonatal resuscitation: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132:S543–60. doi: 10.1161/CIR.0000000000000267. [DOI] [PubMed] [Google Scholar]
- 10.Ibrahim CP, Yoxall CW. Use of plastic bags to prevent hypothermia at birth in preterm infants–do they work at lower gestations? Acta Paediatr. 2009;98:256–60. doi: 10.1111/j.1651-2227.2008.01076.x. [DOI] [PubMed] [Google Scholar]
- 11.DeMauro SB, Douglas E, Karp K, Schmidt B, Patel J, Kronberger A, et al. Improving delivery room management for very preterm infants. Pediatrics. 2013;132:e1018–25. doi: 10.1542/peds.2013-0686. [DOI] [PubMed] [Google Scholar]
- 12.Pinheiro JM, Furdon SA, Boynton S, Dugan R, Reu-Donlon C, Jensen S. Decreasing hypothermia during delivery room stabilization of preterm neonates. Pediatrics. 2014;133:e218–26. doi: 10.1542/peds.2013-1293. [DOI] [PubMed] [Google Scholar]
- 13.Newton T, Watkinson M. Preventing hypothermia at birth in preterm babies: at a cost of overheating some? Arch Dis Child Fetal Neonatal Ed. 2003;88:F256. doi: 10.1136/fn.88.3.F256-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lyon AJ, Stenson B. Cold comfort for babies. Arch Dis Child Fetal Neonatal Ed. 2004;89:F93–4. doi: 10.1136/fn.89.1.F93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Singh A, Duckett J, Newton T, Watkinson M. Improving neonatal unit admission temperatures in preterm babies: exothermic mattresses, polythene bags or a traditional approach? J Perinatol. 2010;30:45–9. doi: 10.1038/jp.2009.94. [DOI] [PubMed] [Google Scholar]
- 16.Reilly MC, Vohra S, Rac VE, Dunn M, Ferrelli K, Kiss A, et al. Randomized trial of occlusive wrap for heat loss prevention in preterm infants. J Pediatr. 2015;166:262–8. e2. doi: 10.1016/j.jpeds.2014.09.068. [DOI] [PubMed] [Google Scholar]
- 17.Walsh MC, Kliegman RM. Necrotizing enterocolitis: treatment based on staging criteria. Pediatr Clin North Am. 1986;33:179–201. doi: 10.1016/S0031-3955(16)34975-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization. Thermal control of the newborn: a practical guide. Geneva, Switzerland: World Health Organization; 1993. [Google Scholar]
- 19.Lyu Y, Shah PS, Ye XY, Warre R, Piedboeuf B, Deshpandey A, et al. Association between admission temperature and mortality and major morbidity in preterm infants born at fewer than 33 weeks’ gestation. JAMA Pediatr. 2015;169:e150277. doi: 10.1001/jamapediatrics.2015.0277. [DOI] [PubMed] [Google Scholar]
- 20.Russo A, McCready M, Torres L, Theuriere C, Venturini S, Spaight M, et al. Reducing hypothermia in preterm infants following delivery. Pediatrics. 2014;133:e1055–62. doi: 10.1542/peds.2013-2544. [DOI] [PubMed] [Google Scholar]
- 21.Laptook AR, Watkinson M. Temperature management in the delivery room. Semin Fetal Neonatal Med. 2008;13:383–91. doi: 10.1016/j.siny.2008.04.003. [DOI] [PubMed] [Google Scholar]
- 22.Lieberman E, Lang J, Richardson DK, Frigoletto FD, Heffner LJ, Cohen A. Intrapartum maternal fever and neonatal outcome. Pediatrics. 2000;105:8–13. doi: 10.1542/peds.105.1.8. [DOI] [PubMed] [Google Scholar]
- 23.Impey L, Greenwood C, MacQuillan K, Reynolds M, Sheil O. Fever in labour and neonatal encephalopathy: a prospective cohort study. BJOG. 2001;108:594–7. doi: 10.1111/j.1471-0528.2001.00145.x. [DOI] [PubMed] [Google Scholar]
- 24.Blume HK, Li CI, Loch CM, Koepsell TD. Intrapartum fever and chorioamnionitis as risks for encephalopathy in term newborns: a case-control study. Dev Med Child Neurol. 2008;50:19–24. doi: 10.1111/j.1469-8749.2007.02007.x. [DOI] [PubMed] [Google Scholar]
- 25.Grether JK, Nelson KB. Maternal infection and cerebral palsy in infants of normal birth weight. JAMA. 1997;278:207–11. [PubMed] [Google Scholar]
- 26.Costeloe K, Hennessy E, Gibson AT, Marlow N, Wilkinson AR. The EPICure study: outcomes to discharge from hospital for infants born at the threshold of viability. Pediatrics. 2000;106:659–71. doi: 10.1542/peds.106.4.659. [DOI] [PubMed] [Google Scholar]
- 27.Miller SS, Lee HC, Gould JB. Hypothermia in very low birth weight infants: distribution, risk factors and outcomes. J Perinatol. 2011;31(Suppl 1):S49–56. doi: 10.1038/jp.2010.177. [DOI] [PubMed] [Google Scholar]
- 28.de Almeida MF, Guinsburg R, Sancho GA, Rosa IR, Lamy ZC, Martinez FE, et al. Hypothermia and early neonatal mortality in preterm infants. J Pediatr. 2014;164:271–5. e1. doi: 10.1016/j.jpeds.2013.09.049. [DOI] [PubMed] [Google Scholar]
- 29.Medlock S, Ravelli AC, Tamminga P, Mol BW, Abu-Hanna A. Prediction of mortality in very premature infants: a systematic review of prediction models. PLoS ONE. 2011;6:e23441. doi: 10.1371/journal.pone.0023441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993–2012. JAMA. 2015;314:1039–51. doi: 10.1001/jama.2015.10244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kaplan HC, Lannon C, Walsh MC, Donovan EF, Ohio Perinatal Quality Collaborative Ohio statewide quality-improvement collaborative to reduce late-onset sepsis in preterm infants. Pediatrics. 2011;127:427–35. doi: 10.1542/peds.2010-2141. [DOI] [PubMed] [Google Scholar]
- 32.Schulman J, Stricof R, Stevens TP, Horgan M, Gase K, Holzman IR, et al. Statewide NICU central-line-associated bloodstream infection rates decline after bundles and checklists. Pediatrics. 2011;127:436–44. doi: 10.1542/peds.2010-2873. [DOI] [PubMed] [Google Scholar]