Abstract
Introduction:
The surgical treatment of proximal femoral fractures predominantly involves geriatric patients and is associated with high morbidity and mortality. However, analyses on postoperative infections or hematoma are rare.
Methods:
Patients requiring surgical revision due to infection (n = 90) or hematoma (n = 77) in the postoperative phase were identified from an electronic database of 2000 consecutive patients surgically treated for proximal femoral fractures between 2006 and 2014. Demographic and clinical data were retrieved, including information on the pathogens in patients with infection. A follow-up on morbidity and mortality was conducted via telephone for at least 2 years postsurgery.
Results:
The follow-up rate was 100%, and the mean age was 81.9 years. The incidence rate of infection was 4.1% (90/2000), and women were commonly affected. Staphylococcus aureus and Staphylococcus epidermidis were the most commonly detected pathogens (35.5% and 25.5%, respectively). Mixed infections were observed in 15 patients, and Methicillin-resistant Staphylococcus aureus infections were observed in only 4 patients. A total of 77 (85.6%) infections occurred within 30 days postsurgery. The implant was preserved in 76 (84.4%) patients, and resection arthroplasty was required in 14 patients. Dementia and pertrochanteric fractures were significantly more common in the infection than in the hematoma group. Although infections were associated with high mortality rates for up to 2 years postsurgery, the rates did not significantly differ from those in the hematoma control group.
Conclusion:
One of every 2 patients who developed an infection following the surgical treatment of a proximal femoral fracture died within 2 years postsurgery. In addition, infections were significantly associated with dementia. Avoiding postoperative infection should be a high priority in the surgical treatment of proximal femoral fractures.
Keywords: proximal femoral fractures, infection, hematoma, revision, mortality
Introduction
The surgical treatment of proximal femoral fractures is predominantly performed in geriatric patients; thus, it is associated with high morbidity and mortality.1–4 A variety of surgical techniques are available, including intramedullary nails, dynamic hip screws, and alloarthroplasty, the use of which depends on the patient’s age and fracture morphology.1–4 Studies involving a high numbers of cases or national registries have reported revision rates of 6% to 15% and a 1-year mortality of up to 30%.1,4–6 However, studies regarding infections as a postoperative complication are limited, which are characterized by small case numbers and considerable “lost to follow-up.”7 Furthermore, based on clinical experience, the reported incidence rates of 1% to 2% appear to be too low and must be challenged.5,7
Therefore, we conducted a retrospective study evaluating the incidence rate and pathogen spectrum of infections following the surgical treatment of proximal femoral fractures. In addition, we evaluated potential influencing variables using a control group of patients who underwent surgical revision due to hematoma. Finally, mortality rates were evaluated for up to 2 years postsurgery.
Methods
A retrospective study was conducted. Patients requiring surgical revision due to infection or hematoma in the postoperative phase were identified from an electronic database of 2000 consecutive patients surgically treated for proximal femoral fractures between 2006 and 2014. A total of 90 patients who underwent surgical revision at least once due to postoperative infections were identified. Definition of infection was from the workgroup of the Musculoskeletal Infection Society.8
In addition, 77 consecutive patients who underwent surgical revision due to hematoma were identified (control group). All patients with hematoma presented negative cultures at the time of revision, showed no sinus tract, and not fulfilled the criteria for an infection in any case.8
The database included 2 years of postoperative follow-up, covering any surgical revision and mortality. Missing data were retrieved by telephoning patients, relatives, or general practitioners. For the infection group, information regarding the pathogens was collected.
Statistics
Statistical analyses were performed using SPSS for Windows, version 24.0 (SPSS Inc., Chicago, Illinois, USA). Metric variables were presented as mean values, while the ranges were specified as standard deviations. Categorized and/or nominal data are specified as absolute and relative frequencies, respectively. Metric variables were assessed for normality using the Kolmogorov-Smirnov test. For non-normal variables (Kolmogorov-Smirnov test: P < .05), group differences were evaluated using the Mann-Whitney U test. Categorical data were analyzed using the χ2 test or Fisher exact test. A Kaplan-Meier survival analysis was conducted to evaluate group differences in mortality; the log-rank test was used to compare survival probabilities. For all analyses, a 2-sided P value of <.05 was considered statistically significant.
Results
Demographic and clinical data are shown in Table 1. The follow-up rate was 100%, and the incidence rate of infection was 4.1% (90/2000). The pathogen spectrum of the infection group was dominated by gram-positive cocci (n = 65; 72.2%; Table 2). Methicillin-resistant Staphylococcus aureus (MRSA) infections were observed in only 4 (4.4%) patients. Overall, significant group differences (infection vs hematoma) were observed in 3 of the 13 evaluated variables. Pertrochanteric fractures and dementia were significantly more common in the infection group than in the hematoma group. In addition, the first surgical revision was delayed by an average of 1 week in the infection group compared to that in the hematoma group. A total of 32 (35.6%) of 90 patients with infection required at least 2 (up to 6) surgical revisions (irrigation and debridement) and calculated antibiotic treatment to control the infection. In contrast, only 7 (9.1%) of 77 patients with hematoma required 2 or 3 revisions. A total of 77 (85.6%) infections were treated initially within 30 days postsurgery. Girdlestone resection was necessary in 14 (15.6%) of 90 patients in the infection group, but was not required in the hematoma group. Nevertheless, it was possible to preserve the implant in 76 (84.4%) of 90 patients with infection.
Table 1.
Demographic and Clinical Comparisons.
| Variables | Infection (n = 90) | Hematoma (n = 77) | P Value |
|---|---|---|---|
| Age, years, mean (SD) | 82.0 (10.5) | 81.6 (8.2) | .556 |
| Sex | |||
| Male | 23 | 19 | 1.000 |
| Female | 67 | 58 | |
| Side | |||
| Right | 41 | 44 | .163 |
| Left | 49 | 33 | |
| Diagnosis | |||
| Cervical hip fracture | 35 (38.9%) | 45 (58.4%) | .033 |
| Pertrochanteric fracture | 45 (50.0%) | 28 (36.4%) | |
| Subtrochanteric fracture | 10 (11.1%) | 4 (5.2%) | |
| Therapy | |||
| Osteosynthesis | 47 (52.2%) | 32 (41.6%) | .214 |
| Arthroplasty | 43 (47.8%) | 45 (58.4%) | |
| CRP value, mean (SD) | 19.3 (32.8) | 21.9 (41.8) | .280 |
| Hemoglobin value, mean (SD) | 12.0 (1.76) | 12.3 (1.8) | .156 |
| ASA | |||
| 2 | 4 (4.4%) | 1 (1.3%) | .445 |
| 3 | 80 (88.9%) | 72 (93.5%) | |
| 4 | 6 (6.7%) | 4 (5.2%) | |
| Dementia | |||
| Yes | 49 (54.4%) | 28 (36.4%) | .021 |
| No | 41 (45.6%) | 49 (63.6%) | |
| Presurgical time, hours | 37.8 (SD 49.0) | 35.1 (SD 40.0) | .851 |
| Duration of surgery, minutes | 89 (SD 39.5) | 77 (SD 25.7) | .086 |
| Hospitalization, days | 22 (SD 17) | 21 (SD 8) | .289 |
| First revision, days | 25.7 (SD 37.1) | 18.2 (SD 16.4) | .039 |
Abbreviation: CRP, 0-5 mg/l; Hemoglobin, 14-18 g/dl; SD, standard deviation.
Table 2.
Pathogen Spectrum (n = 90 Patients).
| Group | Organism | Number of Cases |
|---|---|---|
| Gram-positive cocci | MRSA | 4 |
| Staphylococcus aureus sensitive | 32 | |
| Staphylococcus epidermidis | 23 | |
| Enterococcus | 5 | |
| Streptococcus | 1 | |
| Gram-positive rods | Clostridium perfringens | 1 |
| Gram-negative | Escherichia coli | 3 |
| Enterobacter cloacae | 2 | |
| Klebsiella pneumonia | 2 | |
| Proteus mirabilis | 1 | |
| Pseudomonas aeruginosa | 1 | |
| Mixed infections | 15 |
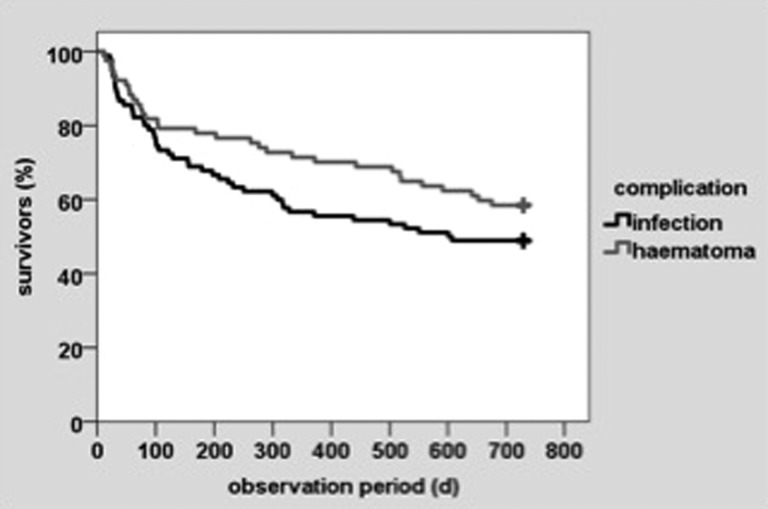
Mortality rates at 30 days, 6 months, 1 year, and 2 years postsurgery are shown in Table 3. The infection group had a considerable higher postoperative mortality rate compared to that in the hematoma group at each time point, with 1 of every 2 patients in the infection group dying within 2 years postsurgery. However, the group differences in survival were not statistically significant (Figure 1).
Table 3.
Postoperative Mortality.
| Mortality | Infection | Hematoma | P Value |
|---|---|---|---|
| 30 days | 8/90 (8.9%) | 5/77 (6.5%) | .773 |
| 6 months | 29/90 (32.2%) | 17/77 (22.1%) | .166 |
| 1 year | 39/90 (43.3%) | 22/77 (28.6%) | .054 |
| 2 years | 46/90 (51.1%) | 32/77 (41.6%) | .276 |
Figure 1.
Kaplan-Meier survival analysis of infection versus hematoma without significant differences.
Discussion
Geriatric patients undergoing surgical treatment of proximal femoral fractures are commonly multimorbid.9,10 A sufficient volume of scientific data exists with regard to surgical treatment, applicable methods, and mortality.3,9 In contrast, in-depth analyses regarding complications, particularly infections, are rare.5,11,12 Furthermore, a review of national arthroplasty registries showed that revisions due to hematoma do not have priority and are not reported in many publications.13
In the present study, we examined the incidence, mortality, and variables associated with infection and hematoma following the surgical treatment of proximal femoral fractures. Unlike previous studies, the present study used patients who underwent surgical revision for postoperative hematoma as a control group. From the authors’ point of view, this is clinically more appropriate compared to a control group without complications or any revision.
It must be clarified that all patients with revision for hematoma had also negative bacteriological findings. Another strength of the present study is that all patients in the total population (n = 2000) completed the 2-year follow-up; thus, we achieved a follow-up rate of 100% for any revision and mortality. In contrast, several previous studies on postoperative infections relied solely on existing registries without actual control mechanisms or follow-ups.5,12 Previous studies on infection following the surgical treatment of proximal femoral fractures with moderately large case numbers have reported infection rates of 0.7% up to 3.4%.5,11,12,14 In contrast, the present study had an infection rate of 4.1%. It must be mentioned that all patients received an intravenous single-shot antibiotic (cefuroxime 1.5 g) prior to surgery. Our higher infection rate may be related to the lack of any “lost to follow-up” in the analysis. In addition, no patients were excluded, including those with dementia. Furthermore, previous studies may have underestimated infection rates by including only “deep wound infections” with putrid secretions.11 From our point of view, the differences between superficial and deep wounds are unclear, and the transition is fluent. Therefore, infection was not differentiated in the present study. The demographic data (eg, age, gender) are generally consistent with that in similar previous studies.5,11,12
Surprisingly, for 10 of the 13 evaluated variables, there were no significant differences between the infection and hematoma groups. However, infections were significantly associated with dementia, with more than half of the patients affected. The impact of dementia has not been previously considered.
The pathogen spectrum was dominated by gram-positive cocci, and Staphylococcus aureus was identified as one of the major pathogens, consistent with previous studies.5,11 However, we observed only 4 cases of MRSA infections, which is clearly less than that observed in other studies. For example, a recent bicenter study (Leeds and Oxford) reported an MRSA rate of 47%.12 Although the mortality rate was clearly higher in the infection group compared to those for hematoma at all investigated time points, the differences failed to reach statistical significance. High mortality rates have been previously shown; however, the data were limited to a maximum period of 1 year postsurgery.5,11
The present study has several limitations. As this is a retrospective study, the evidence level (level 3) is low. In addition, the small number of patients with detected gram-negative bacterial pathogens precluded a statistical analysis of the pathogen spectrum. Furthermore, no additional clinical and radiological examinations regarding the outcomes were conducted. Given the multimorbid nature of the patient population, such additional examinations could not have been conducted in a representative manner.
Conclusion
One of every 2 patients who developed an infection following the surgical treatment of a proximal femoral fracture died within 2 years postsurgery. In addition, infections were significantly associated with dementia. Therefore, avoiding postoperative infection should be a high priority in the surgical treatment of proximal femoral fractures.
Footnotes
Authors’ Note: Each of the authors have participated in the research for this article. The manuscript has not been submitted elsewhere for publication. Institutional review board approval has been obtained.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Hu F, Jiang C, Shen J, Tang P, Wang Y. Preoperative predictors for mortality following hip fracture surgery: a systemic review and meta-analysis. Injury. 2012;43(6):676–685. [DOI] [PubMed] [Google Scholar]
- 2. Ma KL, Wang X, Luan FJ, et al. Proximal femoral nails antirotation, Gamma nails, and dynamic hip screws for fixation of intertrochanteric fractures of femur: a meta-analysis. Orthop Traumatol Surg Res. 2014;100(8):859–866. [DOI] [PubMed] [Google Scholar]
- 3. Metcalfe D, Gabbe B, Perry DC, et al. Quality of care for patients with a fracture of the hip in a major trauma centres: a national observational study. Bone Joint J. 2016;98-B(3):414–419. [DOI] [PubMed] [Google Scholar]
- 4. Mueller-Mai C, Schulze-Raestrup U, Kostui T, Dahlhoff G, Guenster C, Smektala R. One-year outcomes for proximal femoral fractures: posthospital analysis of mortality and care levels based on health insurance data. Unfallchirurg. 2015;118(9):780–794. [DOI] [PubMed] [Google Scholar]
- 5. Edwards C, Counsell A, Boulton C, Moran CG. Early infection after hip fracture surgery: risk factors, costs and outcome. J Bone Joint Surg Br. 2007;90(6):770–777. [DOI] [PubMed] [Google Scholar]
- 6. Muhm M, Hillenbrand H, Danko T, Weiss C, Ruffing T, Winkler H. Early complication rate of fractures close to the hip joint. Dependence on treatment in on-call services and comorbidities. Unfallchirurg. 2015;118(4):336–346. [DOI] [PubMed] [Google Scholar]
- 7. Harrison T, Robinson P, Cook A, Parker MJ. Factors affecting the incidence of deep wound infection after hip fracture surgery. J Bone Joint Surg Br. 2012;94(2):237–240. [DOI] [PubMed] [Google Scholar]
- 8. Parvizi J, Zmistowski B, Berbari EF, et al. New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop Relat Res. 2011;469(11):2992–2994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kostuj T, Smektala R, Schulze-Raestrup U, Müller-Mai C. The influence of timing of surgery on mortality and early complications in femoral neck fractures by surgical procedure: an analysis of 22,566 cases from the German External Quality Assurance Program. Unfallchirurg. 2013;116(2):131–137. [DOI] [PubMed] [Google Scholar]
- 10. Leonardsson O, Rolfson O, Hommel A, Garellick G, Akesson K, Rogmark C. Patient-reported outcome after displaced femoral neck fracture: a national survey of 4467 patients. J Bone Joint Surg Am. 2013;95(18):1693–1699. [DOI] [PubMed] [Google Scholar]
- 11. Partanen J, Syrjälä H, Vähänikkilä H, Jalovaara P. Impact of deep infection after hip fracture surgery on function and mortality. J Hosp Infect. 2006;62(1):44–49. [DOI] [PubMed] [Google Scholar]
- 12. Theodorides AA, Pollard TCB, Fishlock A, et al. Treatment of post-operative infections following proximal femoral fractures: our institutional experience. Injury. 2011;42(suppl 5):S28–S34. [DOI] [PubMed] [Google Scholar]
- 13. Liebs TR, Splietker F, Hassenpflug J. Is a revision a revision? An analysis of National Arthroplasty Registries’ definitions of revision. Clin Orthop Relat Res. 2015;473(11):3421–3430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Johnston P, Wynn-Jones H, Chakravarty D, Boyle A, Parker MJ. Is perioperative blood transfusion a risk factor for mortality or infection after hip fractures? J Orthop Trauma. 2006;20(10):675–679. [DOI] [PubMed] [Google Scholar]