Abstract
Background:
Almost 80% of people have low back pain at least once in their life. Clinical guidelines emphasize the use of conservative physiotherapy and the importance of staying active. While the psychological factors predicting poor recovery following surgical intervention are understood, the psychosocial factors associated with poor outcomes following physiotherapy have yet to be identified.
Methods:
Electronic searches of PubMed, Medline, CINAHL, PsycINFO and EBSCO were conducted using terms relating to psychosocial factors, chronic low back pain, disability and physiotherapy. Papers examining the relationship between psychosocial factors and pain and disability outcomes following physiotherapy were included. Two reviewers selected, appraised and extracted studies independently.
Results:
In total, 10 observational studies were identified that suggested an association between fear of movement, depression, self-efficacy and catastrophizing in modifying pain and disability outcomes following physiotherapy.
Discussion:
Although limited by methodological shortcomings of included studies, and heterogeneity of physiotherapy interventions and measures of disability and psychosocial outcomes, the findings are consistent with other research in the context of back pain and physiotherapy, which suggest an association between psychosocial factors, including fear of movement, catastrophizing and self-efficacy and pain and disability outcomes in chronic low back pain patients treated by physiotherapist. However, a direct relationship cannot be concluded from this study.
Conclusion:
Findings suggest an association between psychosocial factors, including fear of movement, catastrophizing and self-efficacy and pain and disability outcomes in chronic low back pain patients treated by physiotherapist, which warrants further study.
Keywords: Chronic low back pain, outcomes, physiotherapy, psychosocial
Introduction
Low back pain (LBP) is one of the most predominant musculoskeletal disorders in industrialized societies.1,2 Although the prevalence of LBP is high, with up to 80% of people reporting at least one episode during their lifetime,3 most people recover within 1 month.4 However, some 10%–40% of all LBP patients go on to develop chronic symptoms and suffer some form of disability.
While there are many different approaches used in the treatment of chronic low back pain (CLBP), there is consensus among clinical guidelines on the promotion of conservative rather than surgical intervention.5,6 Conservative treatment often equates to a physiotherapy-based intervention, which includes exercise and education.
The outcomes of physiotherapy intervention vary, with pain and disability the most frequently measured.7 Several factors could potentially moderate these outcomes. In a secondary analysis of data from a prospective cohort of a mixed group of patients with CLBP and acute LBP (n = 111) receiving outpatient physiotherapy for LBP, patients’ 6-month outcomes, assessed on a range of psychological, pain and disability measures, were compared between patients who had recovered (12.6%) and those who had not. At 6 months, non-recovered patients had higher fear avoidance, kinesiophobia and depressive symptoms (all p < 0.001) compared with recovered patients. From discriminant function analysis, fear avoidance, kinesiophobia and depressive symptoms were found to make significant unique contributions to the prediction of recovery status following physiotherapy.8 In addition, psychosocial factors have been reported to influence outcomes in primary care settings and after surgery.9,10
More recently, attention has turned towards identifying and examining the contribution of psychological factors such as fear of movement and catastrophizing to recovery in people with CLBP. In a review of 25 prospective cohort studies, Pincus et al.11 reported that fear avoidance, depression and catastrophizing were predictive of progression from acute LBP to CLBP. Likewise, in a systematic review, Wertli et al.12 highlighted the moderating effect of fear-avoidance beliefs on treatment efficacy in LBP patients and suggested that the presence of fear-avoidance beliefs is associated with poor recovery.
While there is evidence of multiple prognostic psychosocial factors associated with LBP recovery, this does not distinguish clearly between CLBP and acute LBP. Moreover, there has been no systematic review of the evidence exploring the association between psychosocial factors and pain and disability outcomes specifically following physiotherapy.13
Understanding more about the relationship between psychosocial factors and physiotherapy could inform a more stratified physiotherapy intervention targeting psychosocial impairments in CLBP patients.
Aim
The aim of this systematic review was to identify the psychosocial factors associated with pain and/or disability in CLBP patients treated by physiotherapist.
Methods/design
Protocol and registration
The systematic review protocol was registered on PROSPERO (registration number 2016: CRD42016034132) and conformed to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement.14
Eligibility criteria
Primary research studies published in the English language and that met the inclusion criteria were included in the review. There was no restriction on the study design or the methodological quality.
Inclusion criteria
Inclusion criteria were as follows:
Age between 18 and 65 years.
CLBP of duration ≥3 months.
Studies with mixed patient groups (acute and chronic) were included if separate analysis of chronic patients was reported.
No pathoanatomical diagnosis (e.g. stenosis, fracture).
Physiotherapy intervention, either alone or as part of a multidisciplinary team.
Reporting psychosocial outcome measure (fear, anxiety etc.) and correlation with pain and/or disability after physiotherapy intervention.
Primary outcome measures of the included studies had to include the following:
Pain (e.g. visual analogue scale (VAS), McGill Pain Questionnaire);
Disability (e.g. Roland Morris, Oswestry Disability index);
Psychosocial outcome measures (e.g. Fear-Avoidance Beliefs Questionnaire).
Information source
Reviewers searched academic databases from inception to 17 March 2016. In addition, the reference sections of the extracted articles were manually searched for any articles missed by the electronic search. Academic databases, including PubMed, Medline, CINAHL, PsycINFO and EBSCO, were used to extract relevant studies. Two independent reviewers (A.H. and M.A.) conducted the electronic search. Keywords facilitated the search process and included the following: chronic low back pain, low back pain, psychosocial predictors, disability, psychosocial, catastrophizing, depression, worry, fear avoidance and physiotherapy. These keywords were combined using the Boolean operators ‘AND’ and ‘OR’ (Appendix 1).
Study selection
Two reviewers (A.A. and M.A.) independently screened the titles and abstracts of all studies retrieved from the database search. Studies without psychosocial factors and physiotherapy or rehabilitation keywords in the title were excluded, and if the abstract clearly stated no physiotherapy was used or that only acute back pain patients were studied, the study was excluded. If there was uncertainty about whether a paper should be excluded based on the abstract, the full-text copy of the article was retrieved and reviewed. Any disagreements were resolved by discussing the study outcomes and other measures with a third reviewer (either K.R. or N.C.). Records of studies excluded from the review were kept and reasons for exclusion noted.
Data collection process
The included studies passed through a data extraction process in which two reviewers (A.A. and M.A.) independently extracted the following information: title and authors, objectives and study design, start and end dates, duration of study participation, description of the population from which the participants were drawn, study setting, inclusion and exclusion criteria, methods of recruiting the study participants, the number and demographic characteristics of participants, severity of CLBP, participant comorbidities and study outcomes, conclusions and limitations reported by authors.
Risk of bias in individual studies
Considering the aim was to identify prognostic psychosocial factors, the risk of bias in studies included in the review was assessed by two reviewers (A.A. and M.A.) independently using the Quality in Prognostic Studies (QUIPS) tool for reporting the risk of bias in prognostic systematic reviews. The tool has six domains covering study participation, attrition, prognostic factor measurement, outcome measurement, confounding, statistical analysis and reporting.
Quality assessment
The search strategy did not limit study design and all the included studies were either cross-sectional or prospective cohort studies. Thus, the quality of evidence and strength of recommendation was assessed using the Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies, developed by the National Institutes of Health.15 The tool consists of 14 criteria and reviewers decide whether the criteria exist or not. The assessment was carried out by two independent reviewers (A.A. and M.A.).
Summary of measures
The association between fear avoidance, catastrophizing, self-efficacy, depression and days off work and pain and/or disability outcomes was reported in accordance with the original study statistical analysis.
Results
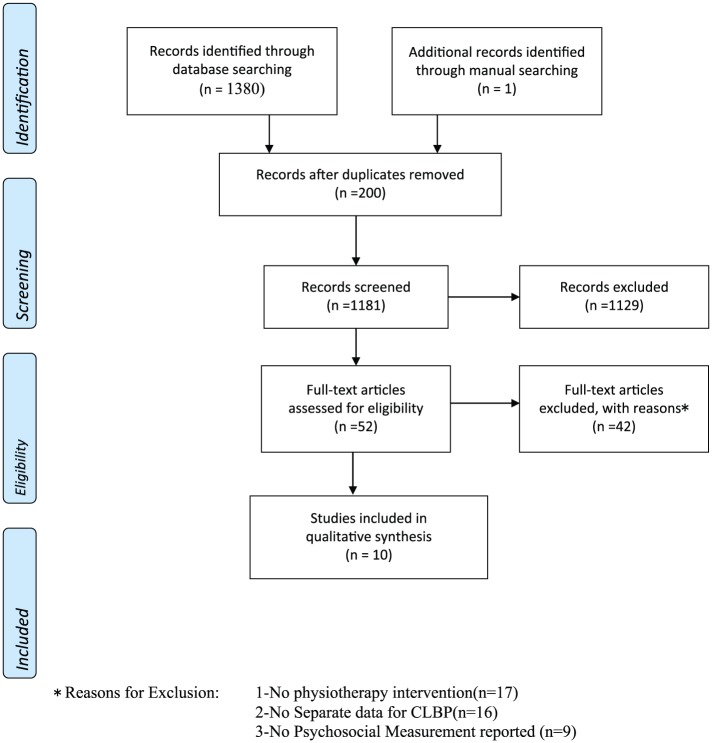
The PRISMA chart (Figure 1) shows the process of study selection. A total of 10 studies met the inclusion criteria after the full-text screening (see Table 1). The most common reasons for exclusion by abstract screening were a lack of a physiotherapy intervention or psychosocial outcome measure. The most frequent reason for excluding full-text studies was a lack of separate data for CLBP in studies involving mixed CLBP and acute LBP patients.
Figure 1.
Prisma flow chart.
Table 1.
Characteristics of the included studies.
| Study origin | Sample size (n) | Age, mean (SD) | Baseline pain severity, VAS | Follow-up (weeks) | |
|---|---|---|---|---|---|
| Ayre and Tyson16 | Australia | 121 | 39.42 (9.5) | 5.45 | 0 |
| Briggs et al.17 | Australia | 117 | 39.7 (12.4) | 4.25 | 0 |
| Cougot et al.18 | France | 217 | 41.33 (9.5) | 3.99 | 104 |
| Elfving et al.19 | Sweden | 149 | 48.56 (NA) | NA | 0 |
| Ferreira and Pereira20 | Portugal | 203 | 48.75 (NA) | NA | 5 |
| Thomas et al.21 | France | 50 | 50.2 (11.4) | 4.5 | 0 |
| Woby et al.22 | UK | 83 | 41 (10) | 4 | 8 |
| Woby et al.23 | UK | 102 | 43.9 (11.7) | 4.4 | 8 |
| Woby et al.24 | UK | 166 | 44.4 (11.4) | 4 | 8 |
| Rainville et al.25 | USA | 72 | 37 (NA) | 7 | 7 |
VAS: visual analogue scale; SD: standard deviation; NA: not applicable.
Most included studies (six) were prospective cohort designs and four were cross-sectional. The total number of participants was 1280. Mean age (standard deviation (SD)) across the studies was 44.0 ± 4.7 years with a marginally higher proportion of women (51%). Average pain intensity measured at the initial assessment before physiotherapy commences by VAS was 4.7 ± 1.0 from all included studies (Table 1). Average percentage dropout from all included studies was 12%. All of the prospective cohort studies reported measurements before and after physiotherapy intervention; only one study reported on follow-up beyond physiotherapy intervention.18
Methodological quality and risk of bias
On application of the QUIPS bias assessment tool for prognostic studies, the bias assessment of included studies showed low to moderate risk. The overall quality of the included studies was ‘fair’ using the Quality Assessment Tool for Observational and Cohort Studies, with 100% agreement between the two assessors.
The included studies were heterogeneous in terms of the nature of the physiotherapy intervention and utilized different outcome measures when reporting the relationship between the intervention and the outcomes. Therefore, comparison between studies was only possible in terms of the identified outcomes. An adapted cognitive behavioural therapy approach was reported in four studies, a multidisciplinary team approach to CLBP management was used in one study, while the five remaining studies did not describe the content of the physiotherapy intervention delivered.
Four psychosocial factors were found to correlate with pain and disability outcomes. The outcome measures used varied among the selected studies (Table 2).
Table 2.
Description of the included studies.
| Author Type of study Study objective |
Outcome measures | Results | Conclusions |
|---|---|---|---|
| Thomas et al.21
Cross-sectional To evaluate fear beliefs and catastrophizing before starting physiotherapy |
Correlation between Roland Morris Back Pain Disability Questionnaire and • DALLAS Pain Questionnaire – daily living • DALLAS Pain Questionnaire – social • Pain Catastrophizing Scale (PCS) • Tampa Scale for Kinesiophobia (TSK) • Hospital anxiety and depression scale |
R = 0.52; p = 0.0001 R = 0.43; p = 0.0001 R = 0.464; p = 0.0008 R = 0.060; p = 0.0001 R = 0.047; p = 0.0006 |
Psychosocial factors are strongly associated with disability and altered quality of life in chronic low back pain (CLBP) patients |
| Woby et al.24
Prospective cohort To investigate whether CLBP patients display changes in cognitive level after a physiotherapy programme |
Change in disability as an outcome and changes in below outcomes as predictors: • Tampa Scale for Kinesiophobia (TSK) • Functional subscale of the Chronic Pain Self-Efficacy Scale • Catastrophizing subscale of Coping Strategy Questionnaire (CSQ) |
t = 2.33; p < 0.001 t = −3.08 (p < 0.001) t = 0.97 (p < 0.001) |
Education in fear of movement and catastrophizing and increases in functional self-efficacy are predictors of function |
| Cougot et al.18
Prospective cohort To study the prognostic factors influencing return to work in CLBP receiving rehabilitation |
The positive prognostic factors for return to work are as follows: • DALLAS Pain Questionnaire – anxiety and depression • DALLAS Pain Questionnaire – daily activities • DALLAS Pain Questionnaire – social • Number of days missed |
OR 0.97; 95% CI OR 0.96; 95% CI OR 0.98; 95% CI OR 1.00; 95% CI |
Failure to return to work after 2 years follow-up is associated with high depression level, low quality of life and more than 112 sick leave days |
| Ferreira and Pereira20
Cross-sectional To study the mediating role of psychological variables that discriminate low and high disability |
Correlation between quality of life and functional ability: • Short-form general health survey with Roland Morris Back Pain Disability Questionnaire (RMDQ) Correlation between quality of life and anxiety: • Short-form general health survey with Hospital Anxiety and Depression Scale (HADS) |
t = −8.013; p < 0.01 t = −9.99; p < 0.01 |
The quality of life of CLBP patients is associated with high disability and high depression |
| Briggs et al.17
Prospective cohort To explore the role of health literacy in relation to disability and beliefs |
High disability scores correlated with • Catastrophizing subscale of Coping Strategy Questionnaire (CSQ) • Fear-Avoidance Beliefs Questionnaire – work • Fear-Avoidance Beliefs Questionnaire – activities |
r2 = 0.15; p = 0.003 r2 = 0.07; p = 0.06 r2 = 0.30; p < 0.001 |
LBP-related beliefs and behaviours, rather than pain intensity and health literacy skills, were found to be important correlates of disability related to LBP |
| Elfving et al.19
Cross-sectional To study the relationship between physical activity level and fear-avoidance beliefs and catastrophizing |
Odd ration of High Roland Morris Disability Questionnaire (RMDQ) is associated with • Pain Catastrophizing Scale (PCS) • Tampa Scale for Kinesiophobia (TSK) |
OR 6.5 and 5.8 compared with 1.1 in low disability; 95% CI OR 7.4 and 4.4 compared with 1.1 in low disability; 95% CI |
This study indicates the importance of physiotherapists measuring levels of fear-avoidance and pain catastrophizing |
| Woby et al.23
Prospective cohort To study the predictive role of self-efficacy in pain and pain-related fear |
Correlation between pain intensity measured by visual analogue scale (VAS) and a subscale of the Chronic Pain Self-Efficacy Scale Correlation between pain-related fear measured by Fear-Avoidance Beliefs Questionnaire (FABQ) and a subscale of the Chronic Pain Self-Efficacy Scale |
Standardized β = 0.23; p < 0.05 Standardized β = 0.38; p < 0.01 |
When self-efficacy is high, elevated pain-related fear might not lead to greater pain and disability. However, in instances where self-efficacy is low, elevated pain-related fear is likely to lead to greater pain and disability |
| Woby et al.22
Prospective cohort To study the role of patient adjustment to CLBP in relation to their fear avoidance, catastrophizing and appraisal of control |
Change in pain intensity in relation to • Pain Catastrophizing Scale (PCS) • Fear-Avoidance Beliefs Questionnaire (FABQ) • Coping Strategy Questionnaire (CSQ) Change in disability score in relation to: • Pain Catastrophizing Scale (PCS) • Fear-Avoidance Beliefs Questionnaire (FABQ) • Coping Strategy Questionnaire (CSQ) |
t = 1.46; p < 0.05 t = 0.22; p < 0.01 t = −1.26; p < 0.05 t = 1.05; p < 0.05 t = 3.46; p < 0.01 t = −1.96; p < 0.05 |
Reductions in fear-avoidance beliefs about work and physical activity, as well as increased perceptions of control over pain were uniquely related to reductions in disability |
| Ayre and Tyson16
Cross-sectional To study the role of self-efficacy and fear in disability outcomes |
Disability measured by Quebec Low Back Pain Disability Scale: Pain Self-Efficacy Questionnaire Fear-Avoidance Beliefs Questionnaire – work Fear-Avoidance Beliefs Questionnaire – activity |
β = 0.57; p < 0.05 β = 0.21; p < 0.01 β = −0.07; p < 0.01 |
Self-efficacy explained 24% of the variance in disability scores, and fear avoidance only a further 3.1% |
| Rainville et al.25
Prospective cohort To investigate the alteration of pain and impairments beliefs in functional-oriented treatment of CLBP |
Correlation between Pain and Impairment Relationship Scale (PARIS) and • Pain intensity score • Beck Depression Inventory |
0.47; p < 0.01 0.46; p < 0.001 |
PARIS score was not strongly correlated with depression and pain intensity measures |
Fear avoidance
Fear-avoidance factors were reported to influence disability scores in eight studies.16,17,19,21–24,25 The outcome measures used were the Tampa Scale for Kinesiophobia and the Fear-Avoidance Beliefs Questionnaire. Higher fear-avoidance scale scores did not predict pain levels in one study.23
Catastrophizing
Pain catastrophizing as measured by the Pain Catastrophizing Scale (PCS) correlated with disability levels in four studies.17,19,21,24
Self-efficacy
Self-efficacy, as measured by the functional subscale of the Chronic Pain Self-Efficacy Scale, was reported to predict levels of pain-related disability and pain in three studies.17,23,24
Depression and anxiety
An association between pain-related disability levels and depression was reported in two studies,18,20 and in one study high depression and anxiety scores were found predictive of poor quality of life and failure to return to work.20
Anxiety, measured using the Hospital Anxiety and Depression Scale, was reported in three studies18,20,21 and found to be associated with high levels of disability and pain.
Working days missed due to LBP
Correlations between the number of working days missed due to LBP and disability levels and work outcomes, that is, return to work, were reported in two studies.17,18
Discussion
The aim of this systematic review was to identify psychosocial factors associated with changes in pain and/or disability in CLBP patients treated by physiotherapist.
Although the results suggesting a clear correlation between these variables are inconclusive due to the broad scope of physiotherapy and heterogeneity of included studies, the findings support an association between disability and levels of pain following physiotherapist treatment and baseline psychosocial factors; the greater the level of disability and pain reported, the higher the scores in fear avoidance and catastrophizing.
These associations may have direct implications for managing CLBP patients, especially those with low scores on functional outcome measures. These results support the findings of George and Beneciuk8 in a retrospective cohort study of CLBP patients, in which pain intensity was found to be predictive of treatment outcome.
They are also consistent with the findings of the systematic review by Wertli et al.,12 who found that participants’ fear-avoidance beliefs had a moderating effect on treatment efficacy. The most frequently reported association in this review was that between fear avoidance and physical disability.
These findings strengthen the legitimacy of the fear-avoidance model,26,27 which suggests that the presence of psychological factors, such as fear of pain, catastrophization and depression after experiencing pain, leads to fear of movement, resulting in disuse and further disability. Fear-avoidance model elements were associated with improvements in pain and disability outcomes in people with CLBP treated by physiotherapist. Quality of life was also associated with both higher disability and higher anxiety levels in people with CLBP.
Although the findings of this study highlight a positive association between low levels of disability and pain intensity at baseline and improvement following physiotherapist treatment, a single-centre prospective study of 101 LBP patients27 found that baseline disability scores were not predictive of recovery. However, this was a sub-acute patient with CLBP. Clearly more research is needed to clarify the relationship between initial disability scores and physiotherapy outcomes in people with CLBP.
Several quality assessment tools have been used to evaluate observational studies.25 However, these tools lack validity and reliability.28 Therefore, further research is needed to develop a standardized and validated quality assessment tool for use in observational studies.
Limitations
The term ‘physiotherapy’ was generic and not limited to specific treatments. The interventions in included studies were poorly described but ranged from individual exercise-based interventions delivered by a single therapist, to physiotherapy as a component of a multidisciplinary team intervention, to cognitive behavioural therapy.
Therefore, it remains unclear which, if any, type of physiotherapy intervention or mode of delivery influenced the outcomes of interest positively or negatively. Improved reporting of physiotherapy interventions in research, for example, using the TiDieR Checklist,29 would assist in the selection of studies for review and in interpretation. This would also help to identify which physiotherapy interventions might positively influence pain and disability outcomes following treatment30 and expedite the translation of research into better outcomes for people with CLBP.
None of the included studies set out to examine the outcome of interest. Therefore, the findings cannot conclude that a direct relationship between psychosocial factors and pain and disability outcomes exists but suggest that further research to explore this is warranted.
Conclusion
Although somewhat broad in its scope, this review points to an association between psychosocial factors, including fear of movement, catastrophizing and self-efficacy, and pain and disability outcomes in CLBP treatment. This suggests that such factors may need to be addressed in future physiotherapy interventions. Future studies should investigate the effectiveness of physiotherapy interventions that address psychosocial factors, in addition to more conventional exercise and education-based interventions.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethical approval: Ethical approval is not applicable since this is a systematic review study.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
Informed consent: Informed consent is not applicable since this is a systematic review study.
Trial registration: The systematic review protocol was registered on PROSPERO (registration number 2016: CRD42016034132).
References
- 1. Kelsey JL, White AA, Pastides H, et al. The impact of musculoskeletal disorders on the population of the United States. J Bone Joint Surg Am 1979; 61: 959–964. [PubMed] [Google Scholar]
- 2. Haddad GH. Analysis of 2932 workers’ compensation back injury cases. The impact on the cost to the system. Spine 1987; 12: 765–769. [DOI] [PubMed] [Google Scholar]
- 3. Leboeuf-Yde C, Lauritsen JM, Lauritzen T. Why has the search for causes of low back pain largely been nonconclusive? Spine 1997; 22: 877–881. [DOI] [PubMed] [Google Scholar]
- 4. Jarvik JG, Deyo RA. Diagnostic evaluation of low back pain with emphasis on imaging. Ann Intern Med 2002; 137: 586–597. [DOI] [PubMed] [Google Scholar]
- 5. Koes BW, Van Tulder M, Lin CW, et al. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J 2010; 19: 2075–2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Airaksinen O, Brox JI, Cedraschi C, et al. Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J 2006; 15(Suppl. 2): S192–S300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kamper SJ, Stanton TR, Williams CM, et al. How is recovery from low back pain measured? A systematic review of the literature. Eur Spine J 2011; 20(1): 9–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. George SZ, Beneciuk JM. Psychological predictors of recovery from low back pain: a prospective study. BMC Musculoskelet Disord 2015; 16: 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Foster NE, Thomas E, Bishop A, et al. Distinctiveness of psychological obstacles to recovery in low back pain patients in primary care. Pain 2010; 148(3): 398–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Alodaibi FA, Minick KI, Fritz JM. Do preoperative fear avoidance model factors predict outcomes after lumbar disc herniation surgery? A systematic review. Chiropr Man Therap 2013; 21(1): 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Pincus T, Burton AK, Vogel S, et al. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine 2002; 27: E109–E120. [DOI] [PubMed] [Google Scholar]
- 12. Wertli MM, Rasmussen-Barr E, Held U, et al. Fear-avoidance beliefs – a moderator of treatment efficacy in patients with low back pain: a systematic review. Spine J 2014; 14(11): 2658–2678. [DOI] [PubMed] [Google Scholar]
- 13. Hill JC, Fritz JM. Psychosocial influences on low back pain, disability, and response to treatment. Phys Ther 2011; 91(5): 712–721. [DOI] [PubMed] [Google Scholar]
- 14. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009; 151(4): 264–269. [DOI] [PubMed] [Google Scholar]
- 15. National Institutes of Health. Quality assessment tool for observational cohort and cross-sectional studies. Bethesda, MD: NHLBI, National Institutes of Health (NIH), 2016, https://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/cohort (accessed 31 October 2016). [Google Scholar]
- 16. Ayre M, Tyson GA. The role of self-efficacy and fear-avoidance beliefs in the prediction of disability. Aust Psychol 2001; 36: 250–253. [Google Scholar]
- 17. Briggs AM, Jordan JE, Buchbinder R, et al. Health literacy and beliefs among a community cohort with and without chronic low back pain. Pain 2010; 150: 275–283. [DOI] [PubMed] [Google Scholar]
- 18. Cougot B, Petit A, Paget C, et al. Chronic low back pain among French healthcare workers and prognostic factors of return to work (RTW): a non-randomized controlled trial. J Occup Med Toxicol 2015; 10: 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Elfving B, Andersson T, Grooten WJ. Low levels of physical activity in back pain patients are associated with high levels of fear-avoidance beliefs and pain catastrophizing. Physiother Res Int 2007; 12: 14–24. [DOI] [PubMed] [Google Scholar]
- 20. Ferreira MS, Pereira MG. The mediator role of psychological morbidity in patients with chronic low back pain in differentiated treatments. J Health Psychol 2014; 19: 1197–1207. [DOI] [PubMed] [Google Scholar]
- 21. Thomas EN, Pers YM, Mercier G, et al. The importance of fear, beliefs, catastrophizing and kinesiophobia in chronic low back pain rehabilitation. Ann Phys Rehabil Med 2010; 53: 3–14. [DOI] [PubMed] [Google Scholar]
- 22. Woby SR, Watson PJ, Roach NK, et al. Are changes in fear-avoidance beliefs, catastrophizing, and appraisals of control, predictive of changes in chronic low back pain and disability? Eur J Pain 2004; 8: 201–210. [DOI] [PubMed] [Google Scholar]
- 23. Woby SR, Urmston M, Watson PJ. Self-efficacy mediates the relation between pain-related fear and outcome in chronic low back pain patients. Eur J Pain 2007; 11: 711–718. [DOI] [PubMed] [Google Scholar]
- 24. Woby SR, Roach NK, Urmston M, et al. Outcome following a physiotherapist-led intervention for chronic low back pain: the important role of cognitive processes. Physiotherapy 2008; 94: 115–124. [Google Scholar]
- 25. Rainville J, Ahern DK, Phalen L. Altering beliefs about pain and impairment in a functionally oriented treatment program for chronic low back pain. Clin J Pain 1993; 9: 196–201. [DOI] [PubMed] [Google Scholar]
- 26. Vlaeyen JW, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain 2000; 85: 317–332. [DOI] [PubMed] [Google Scholar]
- 27. Hendrick P, Milosavljevic S, Hale L, et al. Does a patient’s physical activity predict recovery from an episode of acute low back pain? A prospective cohort study. BMC Musculoskelet Disord 2013; 14: 126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Shamliyan T, Kane RL, Dickinson S. A systematic review of tools used to assess the quality of observational studies that examine incidence or prevalence and risk factors for diseases. J Clin Epidemiol 2010; 63(10): 1061–1070. [DOI] [PubMed] [Google Scholar]
- 29. Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014; 348: g1687. [DOI] [PubMed] [Google Scholar]
- 30. Yamato T, Maher C, Saragiotto B, et al. The TIDieR checklist will benefit the physical therapy profession. Braz J Phys Ther 2016; 20: 191–193. [DOI] [PMC free article] [PubMed] [Google Scholar]