Abstract
Background:
Various operative strategies have been introduced to restore the integrity of articular cartilage when injured. The frequency of revision surgery after cartilage regenerative surgery remains incompletely understood.
Purpose/Hypothesis:
The purpose of this study was to identify the reasons for revision surgery after cartilage regenerative surgery of the knee. We hypothesized that in a large patient cohort, revision rates would differ from those in the current literature.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
A total of 2659 complete data sets from the German Cartilage Registry were available for analyses. In brief, baseline data were provided by the attending physician at the time of index surgery. Follow-up data were collected using a web-based questionnaire inquiring whether patients had needed revision surgery during follow-up, which was defined as the endpoint of the present analysis.
Results:
A total of 88 patients (3.3%) reported the need for revision surgery as early as 12 months postoperatively. Among the most common causes were arthrofibrosis (n = 27) and infection (n = 10). Female patients showed a significantly greater complication rate (4.5%) when compared with male patients (2.6%; P = .0071). The majority of cartilage lesions were located at the medial femoral condyle (40.2%), with a mean defect size of 3.5 ± 2.1 cm2. Neither the location nor defect size appeared to lead to an increased revision rate, which was greatest after osteochondral autografts (5.2%) and autologous chondrocyte implantation (4.6%). Revision rates did not differ significantly among surgical techniques. Chi-square analysis revealed significant correlations between the number of previous joint surgeries and the need for revision surgery (P = .0203). Multivariate regression analysis further confirmed sex and the number of previous surgeries as variables predicting the need for early revision surgery.
Conclusion:
The low early revision rates found in this study underline that today’s cartilage repair surgeries are mostly safe. Although invasiveness and techniques differ greatly among the procedures, no differences in revision rates were observed. Specific factors such as sex and the number of previous surgeries seem to influence overall revision rates and were identified as relevant risk factors with regard to patient safety.
Keywords: revision surgery, cartilage, German Cartilage Registry, knee
The treatment of articular cartilage defects is still a challenging task in orthopaedic surgery because of the poor regenerative potential of cartilage and its limited ability to recover spontaneously.20 The progression of defects can lead to osteoarthritis, which significantly impairs quality of life.8 Patients suitable for regenerative cartilage surgery have high expectations toward final outcomes.17 For most patients, a speedy recovery and return to sports represent important parameters to measure success or failure after surgery.10,24 This has led to the introduction of various arthroscopic and open-surgery treatment strategies. Arthroscopic microfracture, for example, is commonly used for small cartilage defects.29,31,32 A more complex 1-step procedure is the transplantation of osteochondral autograft cylinders. Despite its satisfactory clinical results, this method is applied less frequently because of harvest site morbidity and its technically challenging nature.1,13 Also, it is generally not recommended for larger lesions, which are commonly treated by 2-step autologous chondrocyte implantation (ACI).7,15,28 ACI has become an established method that has been studied in depth over the past 2 decades. Long-term follow-up analyses have reported failure rates of up to 20%.18,21,25 These studies helped to identify various patient-specific factors influencing outcomes, such as defect location, age, and sex, which remain controversially discussed.6,12
The reasons for revision surgery are not thoroughly investigated. Most studies are hampered by small patient numbers and low methodological quality, requiring caution when interpreting results after surgical cartilage repair.9
Recently, the German Cartilage Registry (KnorpelRegister DGOU) was introduced.14 This patient registry uses a nationwide multicenter approach and is a scientifically motivated project, independent of the interests of industrial partners, observing patients for a minimum of 5 years. It systematically describes the current medical care situation of patients undergoing surgical treatment of their cartilage defects, and it allows researchers to evaluate the efficiency and safety of surgically treated cartilage defects in a patient cohort only minimally influenced by inclusion and exclusion criteria.
The aim of this study was to assess the incidence of revision surgery after articular cartilage surgery. With this information, we were further interested in understanding the most frequent reasons leading to revision surgery. By comparing the variety of cartilage therapies included in the registry, we aimed to identify procedure-specific needs for revision surgery.
Methods
Data were evaluated and obtained from the German Cartilage Registry (KnorpelRegister DGOU), a nationwide and longitudinal multicenter registry of patients undergoing surgical treatment for cartilage defects.14,15 Since the initiation of the registry in October 2013, a total of 2691 data sets for patients undergoing cartilage regenerative surgery for cartilage lesions of the knee joint have been entered by the treating physicians of the 136 participating centers. All participating centers performed each of the cartilage regenerative procedures analyzed in this study. A minority of 32 patients (1.2%) failed to respond to the inquiry regarding the need for revision surgery, thus 2659 full data sets were available for analysis. Data were collected by means of a web-based remote data entry system, which was paperless and accessible directly via an internet browser. Patients needed to be in possession of a personal email address, aged ≥18 years, and eligible to take part in the German Cartilage Registry if surgical treatment of cartilage defects of the knee, ankle, or hip joint took place.
If signed, written informed consent was available, patient- and defect-specific parameters were reported by the treating physician at the time of surgery. These included age, sex, smoking behavior (defined as currently smoking at the time of inclusion into the registry), weight, and height as well as varus or valgus malalignment, preliminary operative procedures, all surgical procedures performed on the injured joint, and therapy characteristics. Table 1 gives a detailed overview of patient-specific parameters. The day after initial data entry by the physician, patients automatically received an email inviting them to fill in a questionnaire for baseline data. The patients then received an email at follow-up intervals of 6, 12, 24, 36, 60, and 120 months after surgery to complete the questionnaire. If the patient did not complete the form within a given time limit, an email reminder was sent automatically.14 Patient satisfaction as well as joint-specific measures such as the International Cartilage Repair Society score were reported. Patients gave information if revision surgery was required.
TABLE 1.
Patient Characteristicsa
| General Study Population (N = 2659) | Patients Requiring Revision Surgery (n = 88) | P Value | |
|---|---|---|---|
| Sex, male/female, n (%) | 1623/996 (61.04/37.46) | 43/45 (2.65/4.52) | .0071 |
| Age at cartilage surgery, y | 37.4 ± 12.2 (18.0-78.0) | 37.9 ± 10.3 (18.0-58.0) | .9760 |
| Body mass index, kg/m2 | 26.3 ± 4.0 (15.0-35.0) | 26.2 ± 4.5 (19.0-34.0) | .4211 |
| Smoker, n (%) | 608 (22.87) | 17 (0.64) | .6510 |
| Duration of symptoms before surgery, mo | 23.63 ± 38.6 (0-240) | 24.92 ± 26.2 (0-240) | .3802 |
aData are shown as mean ± SD (range) unless otherwise indicated.
Only the need for revision surgery was assessed in this study. Planned surgical procedures (eg, secondary correction of axis deviation or implant removal after high tibial osteotomy) were not considered revision surgery. Failure to improve postoperative scores compared with preoperatively or subjective absence of improvement was not assessed in this study. The need for revision surgery, together with relevant reasons, was assessed 12 months after index cartilage surgery.
For all statistical analyses, SPSS Statistics version 24 (IBM) was used. Descriptive statistics were calculated as mean ± SD for all numeric parameters. For all group comparisons, 2-way analysis of variance with a subsequent post hoc Tukey test was applied after normal distribution was verified to detect significant differences between groups. Chi-square analyses were used to evaluate significant relationships between different groups and subgroups. Multivariate regression analysis was performed to predict the need for revision surgery from patient-specific parameters such as sex, age, and weight; defect-specific parameters such as defect size and location; and treatment-specific parameters such as number of previous surgeries and type of surgery. All parameters were tested for independence. P values ≤.05 were considered statistically significant.
Results
Patient-Specific Parameters
Twelve months after initial surgery, a total of 88 patients (3.3%) reported undergoing unplanned revision surgery. With regard to the entire cohort, the majority of patients analyzed were male (n = 1623; 61.0%); however, among the patients requiring revision surgery, a nearly even distribution between the sexes was found. When these patients were set in relation to male and female patients of the entire cohort, female patients showed a significantly higher rate (4.5%) for revision surgery when compared with male patients (2.6%; P = .0071). Multivariate regression analysis identified sex as a parameter significantly predicting the need for revision surgery (P = .0481, R 2 = 0.577).
With regard to age distribution, revision surgery was required for patients aged <20 years in 2.2%, while 3.2% of patients between 20 and 40 years of age underwent revision surgery. A total of 43 patients (3.7%) aged >40 years reported undergoing revision surgery. No significant differences between age groups were found.
Defect-Specific Parameters
A detailed overview of defect-specific parameters is given in Table 2. Seventy patients (79.5%) who required revision surgery had 1 cartilage defect of the knee joint. This observation was comparable with the entire cohort, in which 79.9% of patients were treated for a single defect of the knee joint. Cartilage defects of a degenerative nature requiring revision surgery were found in 3.1%, while traumatic and posttraumatic defects made revision surgery necessary in 3.3% and 4.3%, respectively. The chi-square test revealed no significant correlation between the cause of the defect and the need for revision surgery. Also, neither defect size or location nor the number of defects or their cause appeared to be significantly associated with an increased risk for revision surgery.
TABLE 2.
Defect Characteristicsa
| General Study Population | Patients Requiring Revision Surgery | P Value | |
|---|---|---|---|
| Defect location | .6090 | ||
| 1 location | 2077 (78.11) | 70 (3.37) | |
| 2 locations | 434 (16.32) | 12 (2.76) | |
| >2 locations | 148 (5.67) | 5 (3.38) | |
| Defect size, mean ± SD (range), cm2 | 3.5 ± 2.1 (1.0-10.0) | 3.7 ± 2.1 (1.0-10.0) | .1781 |
| <2 cm2 | 770 (28.96) | 20 (2.60) | |
| 2-4 cm2 | 987 (37.12) | 40 (4.05) | |
| >4 cm2 | 714 (26.85) | 28 (3.92) | |
| Not reported | 188 (7.07) | ||
| Defect location | .8891 | ||
| Medial femoral condyle | 1070 (40.24) | 35 (3.27) | |
| Lateral femoral condyle | 305 (11.47) | 7 (2.30) | |
| Patella | 733 (27.57) | 25 (3.41) | |
| Trochlea | 344 (12.94) | 13 (3.78) | |
| Tibia | 109 (4.10) | 4 (3.67) | |
| Multiple | 98 (3.69) | 4 (4.08) | |
| Cause of defect | .8124 | ||
| Traumatic | 480 (18.05) | 15 (3.13) | |
| Degenerative | 1451 (54.57) | 48 (3.31) | |
| Posttraumatic | 376 (14.14) | 16 (4.26) | |
| Not reported | 352 (13.24) | 9 (2.56) |
aData are shown as n (%) unless otherwise indicated.
Treatment-Specific Parameters
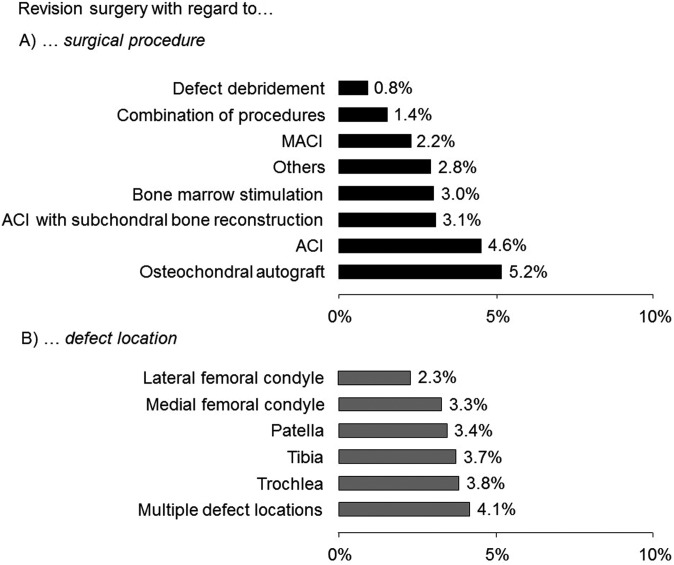
Detailed information regarding treatment-specific parameters is given in Table 3. The majority (41.4%) of cartilage lesions were treated by ACI. Third-generation ACI techniques included Chondrosphere (38.9%; co.don), Novocart 3D (32.2%; Tetec), Novocart Inject (15.2%; Tetec), and others (13.7%). A total of 50 patients reported that after ACI, unexpected revision surgery became necessary. With regard to all patients treated with ACI, this resulted in a revision rate of 4.6%. When set in relation to the entire cohort of 2659 patients, the revision rate was 1.9%. A detailed illustration of revision rates with regard to surgical procedure is given in Figure 1.
TABLE 3.
Treatment Characteristicsa
| General Study Population | Patients Requiring Revision Surgery | % of Revision Surgery With Regard to Entire Cohort | P Value | |
|---|---|---|---|---|
| Type of surgery | .2914 | |||
| ACI | 1100 (41.37) | 50 (4.54) | 1.88 | |
| Bone marrow stimulation | 497 (18.69) | 15 (3.02) | 0.56 | |
| ACI with subchondral bone reconstruction | 195 (7.33) | 6 (3.08) | 0.23 | |
| Osteochondral autograft | 58 (2.18) | 3 (5.17) | 0.11 | |
| MACI | 92 (3.46) | 2 (2.17) | 0.08 | |
| Defect debridement | 127 (4.78) | 1 (0.79) | 0.04 | |
| Multiple | 211 (7.94) | 3 (1.42) | 0.11 | |
| Other | 291 (10.94) | 8 (2.75) | 0.30 | |
| No. of previous knee operative procedures | .0203 | |||
| None | 1275 (47.95) | 29 (2.27) | 1.09 | |
| 1 procedure | 759 (28.54) | 29 (3.82) | 1.09 | |
| 2 procedures | 299 (11.24) | 17 (5.69) | 0.64 | |
| >2 procedures | 203 (7.63) | 12 (5.91) | 0.45 | |
| Not reported | 35 (1.32) | 1 (2.86) | 0.04 | |
| No. of surgeries for cartilage defect | .0749 | |||
| None | 1998 (75.14) | 59 (2.95) | 2.22 | |
| 1 surgery | 416 (15.64) | 20 (4.81) | 0.75 | |
| 2 surgeries | 83 (3.12) | 6 (7.23) | 0.23 | |
| >2 surgeries | 30 (1.13) | 2 (6.67) | 0.08 | |
| Not reported | 44 (1.65) | 1 (2.27) | 0.04 |
aData are shown as n (%) unless otherwise indicated. ACI, autologous chondrocyte implantation; MACI, matrix-induced autologous chondrocyte implantation.
Figure 1.
Revision rates were calculated with regard to (A) the surgical procedure and (B) the defect location. Patients requiring revision surgery per group were set in relation to the entire cohort. Neither the type of surgical procedure nor defect location led to a significant increase in revision rates. ACI, autologous chondrocyte implantation; MACI, matrix-induced autologous chondrocyte implantation.
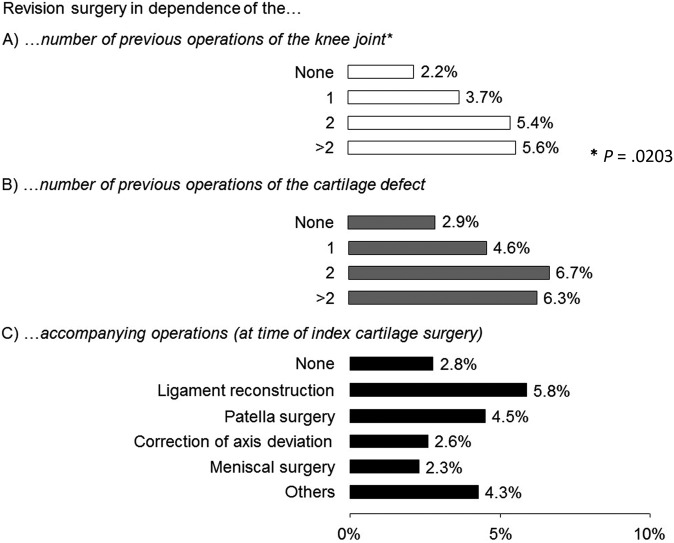
For almost half of the entire cohort (n = 1275; 47.95%), no surgery of the knee had been necessary before initial cartilage regenerative surgery. This was different among the 88 patients undergoing revision surgery. Here, a minority of 29 patients had not undergone surgery on their knee joint before cartilage surgery, while a majority of 59 patients had undergone ≥1 operative procedures on their knee joint. Chi-square analysis revealed significant associations between the number of previous joint surgeries performed and the need for revision surgery (P = .0203) (Figure 2). Multivariate regression analysis confirmed this finding, as it identified previous joint surgeries as a parameter significantly predicting the need for revision surgery (P = .0373, R 2 = 0.504).
Figure 2.
Revision rates were calculated based on (A) the number of previous operative procedures on the knee joint, (B) the number of previous operative procedures on the cartilage defect, and (C) the number of accompanying operative procedures. Previous operative procedures on the knee joint appeared to be a risk factor for revision surgery after cartilage regenerative surgery, as significantly more revision surgeries were found for patients having undergone previous surgery of the knee joint (P = .0203). Cartilage surgery other than the index surgical procedure or other accompanying operative procedures such as meniscal surgery or correction of axis deviation did not appear to increase the risk for revision surgery.
In 52.3% (n = 1391) of all cases found in the registry, cartilage regenerative surgery was performed alone without the need for concomitant procedures. A revision rate of 2.8% was found for these patients. The most common accompanying surgical procedures performed were bony corrections of axis deformations of the lower extremity. These included high tibial and femoral osteotomy as well as derotational femoral osteotomy. Simultaneous correction of axis deviation at the time of cartilage surgery resulted in a revision rate of 2.6%. The second most common accompanying treatment was bony and soft tissue rebalancing of the patella, which accounted for 19.1% of cases, followed by additional meniscus surgery with partial meniscal resection (14.6%), meniscus sutures (1.7%), and implantation of a meniscal transplant (1.6%). Here, a revision rate of 2.3% was observed. In 125 cases, anterior cruciate ligament reconstruction was performed at the same time as cartilage regenerative surgery. In summary, none of the revision rates for concomitant surgery described above and shown in Figure 2 were significantly different from the rates of patients without concomitant surgery.
Reasons for Revision Surgery
As early as 6 months postoperatively, 48 patients (1.8% of the entire cohort) had undergone revision surgery for movement restrictions (n = 15); postoperative hematomas, persistent joint swelling, or infections (n = 9); and secondary meniscus abnormalities (n = 4). At 12 months, another 40 patients had undergone revision surgery. The most common indications were again arthrofibrosis and painful restriction of joint movement (1.0%), secondary meniscus abnormalities (0.4%), and additional cartilage lesions in the same knee joint but at another location (0.19%). A total of 5 patients reported that secondary anterior cruciate ligament reconstruction became necessary because of knee trauma or persistent knee instability. Revision surgery for insufficiency of the cartilage transplant was reported in 4 patients (4.5%). For 5 patients (5.7%), arthroplasty became necessary at a mean age of 50.8 years because of failed reconstructive joint surgery. Detailed information of the most relevant reasons for revision surgery is given in Table 4.
TABLE 4.
Indications for Revision Surgery After 12 Months
| n (%) | |
|---|---|
| Arthrofibrosis | 27 (1.01) |
| Infection | 10 (0.38) |
| Secondary meniscus abnormality | 10 (0.38) |
| Secondary cruciate ligament repair | 10 (0.38) |
| Other | 10 (0.38) |
| Secondary realignment procedure | 5 (0.19) |
| Secondary joint replacement | 5 (0.19) |
| Cartilage defect at different location | 5 (0.19) |
| Secondary cartilage treatment at identical location | 5 (0.19) |
| Incomplete healing of osteotomy | 1 (0.03) |
| Total | 88 (3.31) |
Discussion
Despite intensive research efforts in the field of regenerative cartilage surgery, prognostic factors leading to revision surgery in the first year are incompletely investigated and understood. Most studies focus on the average improvement offered by the surgical technique through the use of specific questionnaires and analysis of their scores at different follow-up times.3,27 Even though relevant data regarding long-term failure after cartilage surgery can be found in the current literature, little is known about the early need for revision surgery related to patient-, defect-, or treatment-specific parameters.16,19,21,25 Furthermore, an internal review of the literature showed that in a surprisingly high number of 35% of all studies published, information regarding failure rates after cartilage regenerative surgery is missing (unpublished data). One possible explanation for this circumstance might be the lack of a commonly accepted definition of failure. In 2004, Dindo et al4 proposed a general classification of surgical complications. It was adapted in 2012 for application in orthopaedic surgery by Sink et al,30 and it defined 5 grades of complications beginning with clinically irrelevant to severely life-threatening and deadly complications. Despite its well and thoroughly performed adaptation for orthopaedic surgery, this classification system is not commonly used in the field of regenerative cartilage surgery. According to the Sink classification, the need for revision surgery corresponds to a severe complication, which is defined as “a complication that is treatable but requires surgical, endoscopic, or radiographic interventions or an unplanned hospital admission.”30 Following this definition, all cases requiring revision surgery reported in the current study would have to be classified as severe complications. Infections or graft failure with the need for revision surgery surely are severe complications. In some cases, however, persistent complaints after surgery can make diagnostic arthroscopic surgery necessary, especially when clinical or radiological findings are inconclusive. Following the definition described above, this would have to be classified as a severe complication, which may not be justified.
Also, an incomplete assessment of revision rates might, in some cases, be explained by low patient numbers. Conclusions regarding the need for revision surgery and more specifically of uncommon complications are difficult to make. Heterogeneity in patient- and defect-specific factors such as the cause and anatomic locations of cartilage lesions may lead to incomparability between different study groups.5 Randomized controlled trials (RCTs) are therefore perceived as the “gold standard” for evaluating treatment options. It has been reported that as few as 4% of all patients undergoing cartilage regenerative surgery are suitable for RCT studies.5 This implies that they may not always represent “everyday” cartilage patients. It must be kept in mind that with a mean age of 37.4 ± 12.2 years (range, 18.0-78.0 years) at the time of index surgery and almost half of all patients aged >40 years, patients in the current study were older than in most RCTs, although cartilage regenerative surgery in patients between 20 and 40 years of age did not appear to lead to greater revision rates when compared with patients aged >40 years. The exclusion of patients in controlled studies is necessary to achieve high internal validity because of the study design of RCTs but may naturally interfere with external validity and clinical applicability. Strict inclusion criteria ensure homogeneity within patient cohorts. In prospective studies, these criteria generally limit patient inclusion, leading to low case numbers and possibly artificial patient cohorts.
With the assessment of the cohort presented in this study, we eliminated some of the problems and limitations described above. The great majority (98.8%) of patients undergoing cartilage surgery of the knee joint at one of the 136 centers affiliated with the registry were included in this study. Inclusion criteria were wide, while few exclusion criteria were defined. The result is an extensive heterogeneous study population that includes a great variety of cartilage regenerative techniques applied on patients that greatly differ with regard to patient-, defect-, and technique-associated factors.
When the incidence for self-reported need for revision surgery in this study was correlated with the different techniques of cartilage regenerative surgery, no statistically significant correlations were found. This is particularly interesting, as it could be expected that 2-step procedures such as ACI might be associated with a greater revision rate than single-step techniques such as arthroscopic microfracture. Although not statistically significant, a moderate tendency toward a greater revision rate was observed in the group of osteochondral autografts (5.2%) when compared with ACI (4.6%) and microfracture (3.0%). In comparison with the current literature, this is interesting, as osteochondral autografts are generally associated with higher complication and failure rates.1 Also, accompanying surgical procedures during index cartilage surgery did not result in an increased number of revision surgeries. While cartilage repair techniques alone have evolved over several decades, little information is found on their utilization concurrently with surgery such as correction of axis deviation, ligament reconstruction, or meniscus surgery. The findings in this cohort, however, support previous reports that joint abnormalities treated simultaneously with cartilage repair surgery lead to satisfactory outcomes when compared with cartilage therapy alone.2,26
One of the most important findings of this study was the sex-dependent occurrence of revision surgeries. A previous study found inferior results for female patients after ACI.12 In that study, male patients achieved significantly better results in the Lysholm score at all time intervals and in the International Knee Documentation Committee (IKDC) score at 6 and 12 months after surgery. Patellar defects were described as a prognostic factor leading to inferior results among female patients undergoing ACI.12 Subgroup analyses of our cohort partially confirmed this finding, as female patients showed a significantly higher rate of revision surgery.
Another important finding of this study was that surgery of the knee joint before index cartilage surgery was associated with a higher incidence of revision surgery. However, previous treatment of the cartilage defect did not appear to result in a higher revision rate. This is a surprising finding, as in cases of ACI after failed microfracture, a significantly higher failure rate and inferior clinical outcomes have been observed when compared with ACI as a first-line treatment.23
Interestingly, no signs of age dependency with regard to revision surgery were found in this study. The mean age of all 88 patients requiring revision surgery was 37.9 years, with a range of 18 to 58 years, while the mean age at which cartilage surgery was performed was 37.4 years in the entire cohort. Because of the large number of patients included in this study and the fact that all kinds of cartilage regenerative surgery techniques were included, we found a broad age distribution among patients (18 to 78 years for the entire cohort). While ACI is generally not recommended for patients aged >50 years, to our knowledge, no obligatory age limitations exist for microfracture or autologous osteochondral grafts.11 However, the absence of patients aged >60 years who required revision surgery could be explained by the decreasing requirements of an aging joint. Treatment options between the ages of 50 and 60 years are limited. On one hand, cartilage regenerative surgery with ACI is generally not recommended. On the other hand, indications for arthroplasty for patients aged <60 years need to be carefully evaluated. In this predicament, conservative treatment options could be favored by the treating orthopaedic surgeon.
Our analyses found 5 patients (0.2% of the study cohort) reporting the need for arthroplasty as early as 6 (n = 3) and 12 (n = 2) months postoperatively. This change in the treatment course does not generally represent our philosophy, as previous studies showed that as early as 6 months after cartilage regenerative surgery, no final judgments toward success or failure of the procedure should be made.22 As patients were asked to complete an online questionnaire to be returned to the registry, we cannot exclude the fact that patients with unsatisfactory results after cartilage regenerative surgery did not return the questionnaire. However, the rate of nonrepliers was low, at 1.2%. Those patients lost to follow-up might be a bias influencing this study’s results. Also, the great majority of the reasons leading to revision surgery were not graft associated but were because of unexpected adverse events such as arthrofibrosis, infections, and concomitant meniscal or ligament surgery.
The evaluation of self-reported complications, which were assessed through patient-reported information and examined by a web-based remote data entry system, is a limitation of this study. As described above, initial data regarding patient-, defect-, and technique-specific characteristics were recorded by the treating physician. All follow-up data were based on patient replies. Minor complications without the need for revision surgery were generally not reported and are therefore missing in this study. Also, inaccurate answers and incomplete data have surely influenced our results. Each questionnaire completed by the patient included the inquiry of whether revision surgery became necessary. Initially, this question was affirmed by more than the 88 patients presented in this study. Follow-up surgery such as implant removal after axis correction, for example, was judged as revision surgery by several patients. Also, the need for surgery of the other knee was regarded as a complication by some patients. These false-positive patient answers made further inquiries necessary. In a number of cases, the treating center had to be contacted to collect detailed information.
Another limitation of this study is the absence of clinical follow-up data as well as imaging data such as magnetic resonance imaging results, which could have been collected at scheduled follow-up visits at the centers. Even though the majority of patients were seen at the centers for routine clinical check-ups after surgery, magnetic resonance imaging examinations were scheduled only in those patients with complaints or postoperative complications. The inclusion of these radiological and clinical follow-up data would clearly have gone beyond the scope of the registry.
The absence of a long-term follow-up is clearly another limitation of our study, and it needs to be part of subsequent analyses. We cannot exclude the fact that follow-up analyses will reveal different findings favoring one or another treatment technique or possibly identifying additional factors influencing revision rates. Future follow-up analyses of this cohort will therefore be necessary, and an assessment of long-term results after cartilage surgery will be crucial for understanding the need for revision surgery after those procedures.
Conclusion
Taken together, revision surgery within 12 months after cartilage regenerative surgery was necessary for 88 patients (3.3%). With the help of the German Cartilage Registry, it was possible to confirm previously identified risk factors for revision surgery, such as patient sex and knee surgery before index cartilage surgery. Interestingly, neither the type of surgery nor defect location appeared to be associated with an increased risk for revision surgery.
Acknowledgment
The article-processing charge for this study was provided by the German Research Foundation and Albert Ludwigs University of Freiburg through the funding program Open Access Publishing. The German Cartilage Registry (KnorpelRegister DGOU) is supported by the Deutsche Arthrose-Hilfe and Stiftung Oskar-Helene-Heim.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
Ethical approval for this study was obtained from the Albert Ludwigs University of Freiburg.
References
- 1. Bentley G, Biant LC, Carrington RWJ, et al. A prospective, randomised comparison of autologous chondrocyte implantation versus mosaicplasty for osteochondral defects in the knee. J Bone Joint Surg Br. 2003;85(2):223–230. [DOI] [PubMed] [Google Scholar]
- 2. Bode G, Ogon P, Pestka J, et al. Clinical outcome and return to work following single-stage combined autologous chondrocyte implantation and high tibial osteotomy. Int Orthop. 2015;39(4):689–696. [DOI] [PubMed] [Google Scholar]
- 3. Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM. Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care Res (Hoboken). 2011;63(11):S208–S228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dindo D, Demartines N, Clavien P-A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Engen CN, Engebretsen L, Årøen A. Knee cartilage defect patients enrolled in randomized controlled trials are not representative of patients in orthopedic practice. Cartilage. 2010;1(4):312–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Filardo G, Andriolo L, Sessa A, et al. Age is not a contraindication for cartilage surgery: a critical analysis of standardized outcomes at long-term follow-up. Am J Sports Med. 2017;45(8):1822–1828. [DOI] [PubMed] [Google Scholar]
- 7. Harris JD, Brophy RH, Siston RA, Flanigan DC. Treatment of chondral defects in the athlete’s knee. Arthroscopy. 2010;26(6):841–852. [DOI] [PubMed] [Google Scholar]
- 8. Heir S, Nerhus TK, Røtterud JH, et al. Focal cartilage defects in the knee impair quality of life as much as severe osteoarthritis: a comparison of knee injury and osteoarthritis outcome score in 4 patient categories scheduled for knee surgery. Am J Sports Med. 2010;38(2):231–237. [DOI] [PubMed] [Google Scholar]
- 9. Jakobsen RB, Engebretsen L, Slauterbeck JR. An analysis of the quality of cartilage repair studies. J Bone Joint Surg Am. 2005;87(10):2232–2239. [DOI] [PubMed] [Google Scholar]
- 10. Jungmann PM, Salzmann GM, Schmal H, Pestka JM, Südkamp NP, Niemeyer P. Autologous chondrocyte implantation for treatment of cartilage defects of the knee: what predicts the need for reintervention? Am J Sports Med. 2012;40(1):58–67. [DOI] [PubMed] [Google Scholar]
- 11. Kreuz PC, Erggelet C, Steinwachs MR, et al. Is microfracture of chondral defects in the knee associated with different results in patients aged 40 years or younger? Arthroscopy. 2006;22(11):1180–1186. [DOI] [PubMed] [Google Scholar]
- 12. Kreuz PC, Müller S, von Keudell A, et al. Influence of sex on the outcome of autologous chondrocyte implantation in chondral defects of the knee. Am J Sports Med. 2013;41(7):1541–1548. [DOI] [PubMed] [Google Scholar]
- 13. Marcacci M, Kon E, Zaffagnini S, et al. Multiple osteochondral arthroscopic grafting (mosaicplasty) for cartilage defects of the knee: prospective study results at 2-year follow-up. Arthroscopy. 2005;21(4):462–470. [DOI] [PubMed] [Google Scholar]
- 14. Maurer J, Grotejohann B, Jenkner C, et al. A registry for evaluation of efficiency and safety of surgical treatment of cartilage defects: the German Cartilage Registry (KnorpelRegister DGOU). JMIR Res Protoc. 2016;5(2):e122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Niemeyer P, Feucht MJ, Fritz J, Albrecht D, Spahn G, Angele P. Cartilage repair surgery for full-thickness defects of the knee in Germany: indications and epidemiological data from the German Cartilage Registry (KnorpelRegister DGOU). Arch Orthop Trauma Surg. 2016;136(7):891–897. [DOI] [PubMed] [Google Scholar]
- 16. Niemeyer P, Pestka JM, Kreuz PC, et al. Characteristic complications after autologous chondrocyte implantation for cartilage defects of the knee joint. Am J Sports Med. 2008;36(11):2091–2099. [DOI] [PubMed] [Google Scholar]
- 17. Niemeyer P, Porichis S, Salzmann G, Sudkamp NP. What patients expect about autologous chondrocyte implantation (ACI) for treatment of cartilage defects at the knee joint. Cartilage. 2012;3(1):13–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Niemeyer P, Porichis S, Steinwachs M, et al. Long-term outcomes after first-generation autologous chondrocyte implantation for cartilage defects of the knee. Am J Sports Med. 2014;42(1):150–157. [DOI] [PubMed] [Google Scholar]
- 19. Niemeyer P, Salzmann G, Feucht M, et al. First-generation versus second-generation autologous chondrocyte implantation for treatment of cartilage defects of the knee: a matched-pair analysis on long-term clinical outcome. Int Orthop. 2014;38(10):2065–2070. [DOI] [PubMed] [Google Scholar]
- 20. Ochi M, Adachi N, Nobuto H, Yanada S, Ito Y, Agung M. Articular cartilage repair using tissue engineering technique: novel approach with minimally invasive procedure. Artif Organs. 2004;28(1):28–32. [DOI] [PubMed] [Google Scholar]
- 21. Pareek A, Carey JL, Reardon PJ, Peterson L, Stuart MJ, Krych AJ. Long-term outcomes after autologous chondrocyte implantation: a systematic review at mean follow-up of 11.4 years. Cartilage. 2016;7(4):298–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Pestka JM, Bode G, Salzmann G, et al. Clinical outcomes after cell-seeded autologous chondrocyte implantation of the knee: when can success or failure be predicted? Am J Sports Med. 2014;42(1):208–215. [DOI] [PubMed] [Google Scholar]
- 23. Pestka JM, Bode G, Salzmann G, Südkamp NP, Niemeyer P. Clinical outcome of autologous chondrocyte implantation for failed microfracture treatment of full-thickness cartilage defects of the knee joint. Am J Sports Med. 2012;40(2):325–331. [DOI] [PubMed] [Google Scholar]
- 24. Pestka JM, Feucht MJ, Porichis S, Bode G, Südkamp NP, Niemeyer P. Return to sports activity and work after autologous chondrocyte implantation of the knee. Am J Sports Med. 2016;44(2):370–377. [DOI] [PubMed] [Google Scholar]
- 25. Peterson L, Vasiliadis HS, Brittberg M, Lindahl A. Autologous chondrocyte implantation: a long-term follow-up. Am J Sports Med. 2010;38(6):1117–1124. [DOI] [PubMed] [Google Scholar]
- 26. Pike AN, Bryant T, Ogura T, Minas T. Intermediate- to long-term results of combined anterior cruciate ligament reconstruction and autologous chondrocyte implantation. Orthop J Sports Med. 2017;5(2):2325967117693591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS): development of a self-administered outcome measure. J Orthop Sport Phys Ther. 1998;28(2):88–96. [DOI] [PubMed] [Google Scholar]
- 28. Samsudin EZ, Kamarul T. The comparison between the different generations of autologous chondrocyte implantation with other treatment modalities: a systematic review of clinical trials. Knee Surg Sports Traumatol Arthrosc. 2016;24(12):3912–3926. [DOI] [PubMed] [Google Scholar]
- 29. Saris D, Price A, Widuchowski W, et al. Matrix-applied characterized autologous cultured chondrocytes versus microfracture: two-year follow-up of a prospective randomized trial. Am J Sports Med. 2014;42(6):1384–1394. [DOI] [PubMed] [Google Scholar]
- 30. Sink EL, Leunig M, Zaltz I, Gilbert JC, Clohisy J; Academic Network for Conservational Hip Outcomes Research Group. Reliability of a complication classification system for orthopaedic surgery. Clin Orthop Relat Res. 2012;470(8):2220–2226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Steadman JR, Miller BS, Karas SG, Schlegel TF, Briggs KK, Hawkins RJ. The microfracture technique in the treatment of full-thickness chondral lesions of the knee in National Football League players. J Knee Surg. 2003;16(2):83–86. [PubMed] [Google Scholar]
- 32. Steinwachs MR, Engebretsen L, Brophy RH. Scientific evidence base for cartilage injury and repair in the athlete. Cartilage. 2011;3(suppl 1):11S–17S. [DOI] [PMC free article] [PubMed] [Google Scholar]