Abstract
An ongoing obstacle in dealing with minority health disparities is discriminatory behavior from healthcare practitioners, also known as medical discrimination. It is not clear, however, if the effects of medical discriminations onto health are constant across space. For example, there is evidence to suspect minorities in racially segregated neighborhoods suffer less from discrimination compared to those living elsewhere. To determine the presence of spatial heterogeneity underlying medical discrimination, we implement logistic geographically weighted regression (GWR) using individual data in the city of Philadelphia from the 2006 and 2008 Public Health Management Corporation's Southeastern Pennsylvania Household Health Surveys. Evaluating the potential role residential segregation has in offsetting medical discrimination, we compare the GWR results to tract data from the 2005-2009 American Community Survey. Through this comparison, we find that the effects of medical discrimination on self-rated health are weaker in magnitude in areas that are mostly minority. However, evidence of direct health benefits for minorities in segregated communities is inconclusive. Thus, while we cannot say living in segregated neighborhoods leads to better minority health, the sting of medical discrimination can be weaker in these places. These results emphasize the importance of local variation, even within a city like Philadelphia, challenging the aspatial one-model-fits-all approach normally found in population studies.
1. Introduction
Racial discrimination against minorities by medical practitioners towards their patients is a serious thorn in the side of efforts to reduce medical disparities based on race in the United States. Such discrimination, also known as medical discrimination,includes actions such as condescending behavior towards nonwhite patients compared to White patients1 (Cooper et al., 2012; Johnson, 2004), prescribing these patients weaker medications (Goyal et al., 2015), and avoiding taking them on as patients (Greene et al., 2006). These factors can lead to less patient-centered care for minorities (Blair et al., 2013; Cooper et al., 2012), contributing to the reduced trust of the healthcare system among nonwhite populations (Boulware et al., 2003), increased patient stress (Kessler et al., 1999), and avoidance of care outright (Gaskin et al., 2009; Johnson, 2004). Thus, medical discrimination exacerbates poor health for minorities while effectively blocking access to the care needed to deal with it. Though the implications of medical discrimination are clear, much remains in disentangling both how the perception of medical discrimination unfolds across space, as well as how serious its implications are for one's self-rated health (SRH) from one place to another.
While connecting something as singular as the discrimination one experiences from their healthcare providers to urban processes may initially appear unexpected, doing so plays into gaps in the population literature, especially in the area of racial/ethnic neighborhoods in segregated regions. Even if segregation has been strongly argued to harm minority health, esepcially for non-Hispanic Blacks2 (Acevedo-Garcia et al., 2003; Gibbons and Yang, 2014; Kramer and Hogue, 2009; Sampson, 2012; Subramanian, 2005; Williams and Collins, 2001), it is not clear if it affects medical discrimination for Blacks. In addition, nonblack minority groups may not experience the same discrimination effects from segregation.
Some scholars postulate that residence in segregated places, in fact,reduces the harm of discrimination for minority health. This phenomenon is known as the ‘ethnic density effect’ and has been documented across the world, including New Zealand (Bécares et al., 2013), the United Kingdom (Bécares et al., 2009), and United States (Gibbons and Yang, 2014; Hunt et al., 2007; Pickett and Wilkinson, 2008; Shaw and Pickett, 2011). Putting these various strands of research together indicates that medical discrimination, or, at least, the perception that it exists, varies between non-Hispanic white and nonwhite communities in segregated regions. Thus, could it be that medical discrimination is weaker in nonwhite areas? If this proves the case, does this suggest health benefits of segregation on minorities' health? Finally, are these benefits consistent between black and nonblack minorities, or do they vary?
To determine how medical discrimination would vary across a segregated place requires a nuanced examination of individual perspectives across space. To aid in this effort, we utilize Geographically Weighted Regression (GWR) and a novel method of coordinate randomization for individual responses from the Public Health Management Corporations (PHMC) 2008 survey to evaluate the spatial heterogeneity of perceived medical discrimination in the city of Philadelphia. This city is an ideal site for this study given its long history of racial discrimination, segregation, and health disparities (Du Bois 1899). Past studies have shown that GWR is an effective way to not only document local variations in health (Black, 2014), but also in attitudes pertaining to local institutions (Bagheri et al., 2009; Comber et al., 2012). With GWR, we can compare the local variation in our predictors against the distribution of racial/ethnic neighborhoods drawn from 2005-2009 American Community Survey (ACS)data. Through this comparison, we can explore segregation's spatial influence on individual perceived medical discrimination. While multi-level modeling strategies, commonly used in urban health research (Acevedo-Garcia et al., 2003; Gibbons and Yang, 2014; Kramer and Hogue, 2009; Subramanian, 2005), can examine the interrelation between individual and neighborhood characteristics, they are limited in that local effects are assumed to be discrete, separated by neighborhood boundaries,and mutually independent across space (Yang and Matthews, 2012). More recent criticisms of this approach can be found elsewhere (Owen et al., 2016). Multi-level strategies overlook the underlying spatial structures influencing perceived medical discrimination within and between neighborhood boundaries. While this study is focused on one specific city, the findings have implications globally, as the spatial heterogeneity of racial discrimination is likely to manifest in a variety of places even if its precise character may be subject to local context.
2. Literature Review
Medical discrimination has been identified both through qualitative research and observational studies including focus groups and recording doctor/patient interactions (Cooper et al., 2012; Gee, 2002; Kessler et al., 1999) and by the self-reporting of nonwhite patients (Blair et al., 2013). The effects of medical discrimination for a person of color can be big or small. On the one hand are ‘everyday’ acts of discrimination which consist of small routine behaviors. For example, doctors have been found to be more domineering and condescending to their nonwhite patients, especially Black, when compared to White patients (Cooper et al., 2012; Johnson, 2004). The harm from these microaggressions are cumulative in nature, gradually building over time - such as distrust of healthcare practitioners among nonwhites (Boulware et al., 2003; Shoff and Yang, 2012; Yang and Matthews, 2012). On the other hand are more substantial ‘lifetime’ events, which carry lasting impacts on one's life (Hunt et al., 2007; Kessler et al., 1999). Notable examples of lifetime discriminatory acts from healthcare practitioners include the forced sterilization of women, which disproportionately targets Black women (Davis, 1983).
While the existence of medical discrimination has been demonstrated empirically, the perception of medical discrimination is highly subjective, influenced by a number of factors which require further consideration. First, medical discrimination has been found to fluctuate across different racial/ethnic groups (Blair et al., 2013; Boulware et al., 2003). While very terse interactions have been identified between doctors and Black patients (Cooper et al., 2012), Latino patients have been found in some studies more likely to feel disconnected from their doctors than their Black peers (Collins and Fund, 2002).
Second, the perception that one is being discriminated is influenced the local environment within which they reside. Local racial/ethnic concentration, which contributes towards segregation, has long been associated with the strength of racist attitudes that both motivate discriminatory behavior as well as its perceived existence. Oliver and Wong (2003) found that racist attitudes from Whites to Blacks are strongest where Whites constitute the demographic majority, itself a product of regional segregation separating Whites from Blacks. Turning to the potential health influence associated with the relation between segregation and discrimination, Gibbons and Yang (2014) found that Blacks report worse SRH when living in mostly White areas than in racially mixed areas. The poorer health Blacks experience in mostly White communities may be due to the potentially higher Whites' discrimination against nonwhites in such places, but this has not been confirmed in research.
Some support for this notion comes from Hunt (et al., 2007), who found that perceptions of discrimination were weaker in segregated nonwhite places than in any other local setting. Indeed, it has been suggested that reduced discrimination identified in mostly nonwhite communities can improve a person of color's mental health (Brown, 2001), as well as lead to other positive health effects. In the epidemiological literature, this local protective effect is known as ‘ethnic density effect’, and one explanation for this positive effect is to avoid discrimination from the racial/ethnic majority (Bécares et al., 2013; Pickett and Wilkinson, 2008; Shaw and Pickett, 2011).
At present, empirical tests of the ethnic density effect have been inconclusive (Bécares et al., 2013). For example, Gibbons and Yang (2014) could not find intrinsic health benefits for a Black person living in a mostly Black area. The ethnic density literature has suggested that segregated nonblack minorities experience more of this protective effect compared to Blacks (Shaw and Pickett, 2011). Indeed, nonblack minorities are argued to be more likely to self-select into such places for ethnic benefits compared to Blacks (Zhou, 1992). Others contest that African Americans specifically also carry such ‘in-group’ preferences that they would self-select into neighborhoods, however the empirical proof of this argument is limited (Patterson, 1997). Another limitation in this past discrimination research is how well it reflects medical discrimination, which carries some potentially confounding attributes.
As medical discrimination takes place in a professional setting, it may be more a product of institutional discrimination as opposed to the interpersonal discrimination the previous studies emphasize. In other words, local variation's role in perceived discrimination may be related more to the kind of place one goes for care than local racial composition. For example, It is generally agreed that a small private practice with a primary caregiver is the best source of regular care (Gaskin et al., 2007). It is thought that these practitioners are more likely to become familiar with their patients given the relatively low amount of clients that they have (Radecki and Bernstein, 1989). This increased familiarity with nonwhite clients may reduce the chances such practitioners would act discriminatorily against them, reflecting an argument known as the ‘contact hypothesis’ (Allport, 1954). In comparison, hospital outpatient clinics are seen as less effective with building close ties with patients to care providers. These clinics present the problems such as long wait times and large volumes of patients, leading to more impersonal care (Doescher et al., 2001). Not clear from this work though is if these practitioners are more discriminatory in nature. Meanwhile, small nonprofit clinics, or community health centers (CHCs), are recognized as key sites of health access for minorities (Forrest and Whelan, 2000). CHCs, like most American nonprofits, are run through public-private partnerships. This sets CHCs apart from other healthcare providers as they tend to be privately managed. This difference may lead to a greater community attachment among these from CHC's. Indeed, research has found that CHC staff can build close social ties with their clientele (Watkins-Hayes, 2009), assumedly reducing discriminatory attitudes. However, the efforts of these CHCs are often piecemeal due to funding and mission limitations, inhibiting their effectiveness (Allard, 2009; Radecki and Bernstein, 1989). If a person of color has his/her choice of healthcare provider, does this offset whatever medical discrimination they perceive from one location to the next? If this is the case, are their health outcomes better?
In sum, there is a strong consensus in the literature as to the existence and implications of medical discrimination. However, there is a lack of understanding as to how local context matters in this dynamic. Foremost, there is no conclusive agreement if the influence of medical discrimination on SRH varies by location. Following on the ethnic density theory, do minorities living in segregated areas perceive less medical discrimination? If so, does this protective effect offset minority health disparities? What is more, how do perceptions of medical discrimination vary across racial/ethnic groups? Finally, does one's choice of healthcare practitioner confound the effects of local context and perceived medical discrimination on SRH?
3. Hypothesis
This study examines the spatial heterogeneity underlying perceived medical discrimination's relation to SRH. We have the following four hypotheses to frame this inquiry: First, we include (H1) Individual perceptions of medical discrimination from healthcare practitioners consistently perpetuate poor SRH. In other words, the harm of perceived medical discrimination will be consistent regardless of where one resides. Second, we explore the existence of segregation's effect onto perceived discrimination for minorities by directly looking at race's local impact onto SRH. This leads us to include (H2) the impact of individual minority status onto SRH is consistent across space. Third, to distinguish the impact of medical discrimination felt by nonblack minorities compared to Blacks, we add (H3) individual nonblack minority status has a stronger impact on poor SRH in segregated areas than nonblack minority status. Finally, we investigate how different types of health providers confound the relationship of perceived medical discrimination to SRH. To this end, we include (H4) going to community health center, or an outpatient clinic consistently undermines SRH.
4. Data and Methods
4.1 Data Source
To empirically examine the hypotheses above, we used a pooled sample of the 2006 and 2008 PHMC's Southeastern Pennsylvania Household Surveys to explore the spatial heterogeneity of perceived healthcare discrimination. The PHMC surveys have been administered biennially since 1983, and the goal is to collect the information on individual's health status, behaviors, attitudes, and access to healthcare in the Philadelphia metropolitan area (PHMC 2008). We focused on the 8,577 adult respondents from the city of Philadelphia alone for the following reasons. Most of the medical resources, such as clinics and healthcare centers, are concentrated in the city. Focusing on the city residents helps control for the potential bias caused by the transportation barrier to healthcare. What is more, the population density is the highest in Philadelphia within the survey area, which allows us to obtain a more reliable and robust assessment of spatial variations than in other areas surveyed, particularly in the areas where few, if any, respondents were included in the PHMC surveys. The high population density in the city also helps us to obtain consistent results based on the randomization approach.
In addition to the PHMC, we also draw census tract data from the 2005-2009 wave of the ACS to serve as a reference to help interpret our findings. Census tracts provide local demographic information including the racial/ethnic compositions. Identified by the federal government, census tracts serve as a proxy of neighborhoods, their size varying based on population density. The average population size of the tracts in Philadelphia (i.e., 4,077 residents) is close to the optimal size defined by the Census Bureau and the average tract area is 0.30 square miles (S.D.=0.24). As of the year 2000, the city of Philadelphia has 383 tracts.
The PHMC surveys provide the information on participants' residential census tracts. While it is a common practice to use the geographic centroids of the tracts to implement GWR at the individual level, this approach has been criticized for underestimating the spatial variation across research area (Yang and Matthews, 2012). To address this issue, we randomly generated a set of coordinates that fall within one's residential tract for each individual using ArcGIS. This approach has been found to be a useful method to preserve spatial variation (Yang and Matthews, 2012). The details of how to generate coordinates within a specific tract are available upon request. The low variation in area size makes the randomization approach reliable as the observations within a bandwidth rarely differ. Note that we implemented several GWR models with different sets of coordinates as sensitivity analyses but the results and conclusions are not altered.
With respect to the reliability and validity of the PHMC surveys, a recent study (Gibbons and Yang, 2015) reported that several health and socioeconomic indicators (e.g., obesity rate and poverty) drawn from the pooled PHMC data were comparable with those estimated by the Centers for Diseases Control and Preventions. That is, while the PHMC surveys are cross-sectional, the data quality is not affected by pooling two waves of data together. More importantly, PHMC calculates the balancing weights that adjust for sampling bias and non-responses and advises users to use them when implementing statistical tests of significance (PHMC 2006PHMC 2008). Following this suggestion, we applied the balancing weights to our multivariate analyses to yield more accurate results and conclusions.3
4.2 Measurements
The dependent variable is self-rated health (SRH), a powerful predictor of mortality and other physical and mental health outcomes (Idler and Benyamini, 1997; Jylhä, 2009). Also, SRH allows the reporting of poor well-being in ways that cannot easily be categorized, making it a useful indicator of well-being (Wu et al., 2013). As such, SRH offers a useful benchmark for the study of other perspective-based measures, like feelings of medical discrimination. The participants were asked to rate their overall health into one of the following four categories: excellent, good, fair, and poor. Following the common practice in demography, we dichotomized the answers into excellent/good (coded 0, reference group) and fair/poor (coded 1) (Gibbons and Yang, 2014).
The key independent variable is the perceived medical discrimination. Specifically, the respondents were asked “Have you ever experienced discrimination, been prevented from doing something or been hassled or made to feel inferior in [getting medical care] because of your race, ethnicity or color?” Those who answered yes were coded 1, otherwise 0. It should be noted that while this discrimination measure is relatively crude, similar approaches have been used in other surveys or studies administered by federal agencies, which was discussed by a recent study (Paradies, 2006).
With respect to other independent variables, we categorized them into three groups: demographics, socioeconomic status, and access to healthcare. Gender, race/ethnicity, and marital status were included in the demographics group. The second group comprises of poverty, educational attainment, and employment status. We measure access to health care with insurance status and regular sources of health care. We include the definitions of these variables in Table 1 and compare these variables between those who perceived medical discrimination and those who did not.
Table 1. Descriptive statistics of the variables used in this study.
| Definitions | Overall Samples (N=8,577) | Samples with Discrimination (N=729) | Samples without Discrimination (N=7,848) | Testing Resultsa | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | S.D. | Mean | S.D. | Mean | S.D. | |||
| Self-rated health (SRH) | Poor/fair coded 1; excellent/good coded 0 | 0.297 | 0.457 | 0.426 | 0.495 | 0.281 | 0.450 | *** |
| Perceived Medical discrimination | 1 when answering yes to the question of whether one experiencing discrimination; otherwise 0 | 0.085 | 0.279 | N.A. | N.A. | N.A. | N.A. | |
| Demographics | ||||||||
| Gender | Males coded 1, females 0. | 0.305 | 0.461 | 0.308 | 0.462 | 0.303 | 0.459 | |
| Race/ethnicity | Non-Hispanic white are the reference group and three dummy variables were created; non-Hispanic black; Hispanics, and non-Hispanic other races | |||||||
| Non-Hispanic black | 0.433 | 0.496 | 0.607 | 0.489 | 0.418 | 0.493 | *** | |
| Hispanics | 0.136 | 0.342 | 0.165 | 0.372 | 0.132 | 0.339 | * | |
| Others | 0.011 | 0.106 | 0.007 | 0.084 | 0.011 | 0.106 | ||
| Marital status | Married or living with a partner coded 1; other marital status, such as widowed or single, coded 0. | 0.407 | 0.491 | 0.344 | 0.475 | 0.413 | 0.492 | *** |
| Socioeconomic status | ||||||||
| Poverty | Family income below the federal poverty line coded 1; otherwise 0 | 0.160 | 0.366 | 0.240 | 0.427 | 0.153 | 0.360 | *** |
| Educational attainment | Less than high school is the reference group; three dummy variables were created: high school graduate or equivalent, some college education, college or post-college degree. | |||||||
| High school graduate or equivalent | 0.384 | 0.486 | 0.381 | 0.486 | 0.383 | 0.486 | ||
| Some college education | 0.211 | 0.408 | 0.263 | 0.440 | 0.207 | 0.405 | *** | |
| College or post-college graduate | 0.264 | 0.441 | 0.237 | 0.426 | 0.268 | 0.443 | ||
| Employment status | Employed coded 1; other status (e.g., student and retired) coded 0. | 0.539 | 0.499 | 0.483 | 0.500 | 0.547 | 0.498 | *** |
| Access to health care | ||||||||
| Insurance status | Having insurance is coded 1; otherwise 0 | 0.900 | 0.300 | 0.823 | 0.382 | 0.908 | 0.289 | *** |
| Regular sources of health care | “Other places” are the reference group; three dummy variables were created: private doctor's office, community health center/public cline; and outpatient clinic. | |||||||
| Private doctor's office | 0.782 | 0.413 | 0.657 | 0.475 | 0.795 | 0.404 | *** | |
| Community health center/public Clinic | 0.099 | 0.299 | 0.173 | 0.379 | 0.092 | 0.290 | *** | |
| Outpatient clinic | 0.077 | 0.267 | 0.098 | 0.297 | 0.075 | 0.264 | * | |
p<0.05;
p<0.001
Mann-Whitney U-tests were used to examine whether the proportion of a given category is the same between the samples with and those without perceived discrimination. We also used Chi-square test to understand if the distribution between two categorical variables follows expectation.
Drawing on the ACS data at the census tract level,4 we also create a racial typology of different neighborhood racial/ethnic compositions which articulate regional segregation locally to be used as a reference to interpret the GWR findings. Typologies of segregation using racial/ethnic compositions have been found to be a useful way to identify and directly compare different ethnic communities within segregated places (Johnston et al., 2014). This typology is influenced by the extant literature (Friedman, 2008; Gibbons and Yang, 2014, 2015) and compares different compositions of Whites, Blacks, and ‘nonblack minorities’ including Hispanics and non-Hispanic Asians, and other racially mixed people. This measure is essentially a proxy of ‘evenness’ measure of segregation, commonly used as a measure of segregation (Massey and Denton, 1993). Racial/ethnic communities include Predominantly White neighborhoods, defined as tracts where there is at least 60 percent of Whites, and no minority group represents more than 20 percent. Next, Predominantly Black neighborhoods have at least 50 percent non-Blacks and no more than 20 percent of another racial/ethnic group. Predominantly nonblack minority neighborhoods consist of at least 50 percent of a certain non-black minority and no more than 20 percent of Blacks, Hispanics and Asians. Also, we identify Mixed neighborhoods are the tracts that cannot be classified into any of the typologies above.
4.3 Analytic Methods and Strategy
To explore the spatial variation between SRH and other covariates across Philadelphia, we employed logistic GWR to handle properly the binary dependent variable (Fotheringham et al., 2003). As we randomly created the coordinates for each individual, the model below can be applied to our data:
where yi is the probability of reporting fair/poor SRH for an individual i, (ui, vi) denotes the coordinates of individual i, xni represents the explanatory variables (n=1,…,k) discussed above for individual i, and βni represents the estimated association of variable n with SRH for individual i. We used the software program developed by Fotheringham and colleagues (et al., 2003) to implement the analysis. The estimation method is the iteratively reweighted least squares and the kernel density function is the bi-square weighting function, which is a commonly used weighting scheme (Fotheringham et al., 2003). To be specific, GWR will identify a bandwidth for each observation and the local model will be estimated using the data within this bandwidth. The local likelihood methodology is employed to estimate the parameters at each location. The estimation process will be applied to all observations and the distributions of the local estimates can be obtained. When the data points are dense in a study area (like this study), the choice of kernel density function may not affect the results greatly.
One advantage of GWR is that it is an extension of generalized regression models, and thus the interpretations of regression coefficients remain unchanged (Brunsdon et al., 2008; Brunsdon et al., 1998; Chen and Yang, 2012). Explicitly, the regression coefficient of a specific variable at a specific location, (ui, vi), in the model above indicates the change in the log-odds of reporting fair/poor SRH given a one-unit change in this variable. Similar to the conventional logistic regression, exponentiating the coefficient yields the odds ratio associated with this variable at a particular location. As the model above generates results for each individual in our data, it is ineffective to show all local estimates. Following previous studies (Brunsdon et al., 1998; Shoff and Yang, 2012; Yang and Matthews, 2012), we reported the estimates of conventional logistic results, presented the five-number summary (i.e., minimum, three quartiles, and maximum) of local estimates, and visualized the GWR results with thematic maps using a recently developed method (Matthews and Yang, 2012).
While the logistic GWR model above played an important role in exploring spatial variations, we conducted descriptive analysis to understand better our data before implementing the logistic GWR analysis. When the GWR analysis was performed, we first included the perceived medical discrimination only to understand if this variable was associated with SRH. We then included all other covariates to examine if the relationship between perceived medical discrimination and SRH remained. The corrected Akaike Information Criterion (AIC) was used to understand whether the logistic GWR fits the data better than the conventional logistic model (Fotheringham et al., 2003). As a rule of thumb, when the difference in AICs between two models is larger than 4, the model with the smaller AIC is strongly preferred (Burnham and Anderson, 2002).
5. Results
The descriptive statistics of the variables used in this study are presented in Table 1. Several important findings are notable. First, 8.5 percent of the respondents reported discriminatory medical experience and 29.7 percent of the overall samples had fair/poor SRH. When comparing SRH by perceived medical discrimination, we found that more than 40 percent of those with perceived medical discrimination reported fair/poor SRH, in contrast to 28 percent among the respondents without perceived medical discrimination. This discrepancy in SRH was found statistically significant, which provides cursory evidence that perceived medical discrimination is associated with SRH.
Second, more than 60 percent of the samples with perceived medical discrimination were Black, which is roughly 19 percent higher than the proportion of Black in the samples without discrimination experience. Third, compared with those who did not experience medical discrimination, those who reported medical discrimination were featured with lower rates of marriage/cohabiting, employment, and health insurance, as well as higher prevalence of poverty. Finally, with respect to the regular sources of healthcare, almost 80 percent of the respondent without perceived medical discrimination went to private doctor's offices for regular healthcare, in contrast to approximately 66 percent among those experiencing medical discrimination. Also, the proportion of those using CHCs as a regular source of healthcare among those who perceived medical discrimination (17 percent) doubled that of the samples without medical discrimination (9 percent). The differences in the regular source of healthcare seemed to imply that going to a private doctor's office was associated with the lower chance of reporting medical discrimination, which may ultimately improve SRH.
We make a series of descriptive maps to unpack the local spatial characters of our key variables, presented in Figures 1 and 2. To aid in the interpretation of these data, we use Planning Districts developed by the Philadelphia City Planning Commission to identify collections of neighborhoods and the racial typology based on tract-level ACS data, presented in Figure 1. As Figure 1 shows, Philadelphia is a deeply segregated city, with clearly defined Black, nonblack minority and White areas. More subtext at the individual-level is offered in Figure 2, which consists of spatially smoothed kernel density maps of population distributions based on race, SRH, and perceived discrimination. The distribution of Black and Hispanic respondents is largely consistent with the neighborhood-level data presented in the typology, notable exceptions being the strong distributions of Blacks in Upper and Lower Northwest Districts and Hispanics in River Wards District which are not seen in the typology. This difference suggests that even if these populations do not constitute majorities in these respective areas, they still have a strong presence. Turning to health and discrimination, Comparing maps, the perception of medical discrimination is disproportionately stronger in the mostly minority areas of the city, suggesting that segregation is encouraging discrimination. Poor SRH is similarly strong in the minority areas, indicating that it is related to discrimination. To examine these patterns further, we turn to our multivariate results.
Figure 1. Map of Racial Composition of Philaldelphia Neighborhoods.
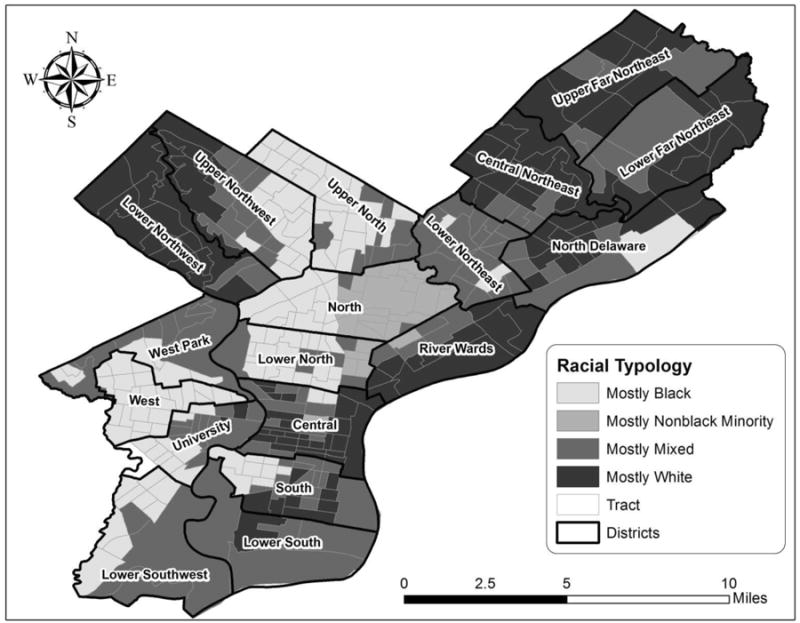
Figure 2. Descriptive Maps.
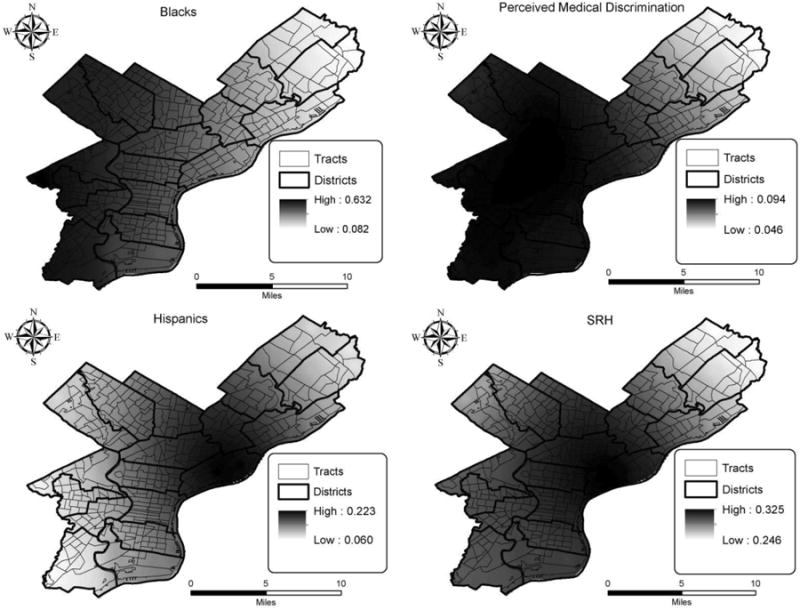
Table 2 showed the results of the conventional, or ‘global’ (i.e., non-spatial), logistic regression. As the goal of this study is to explore the spatial variation across the study area, we briefly summarized the key findings in Table 2. First, perceived medical discrimination was adversely related to SRH. After controlling for other covariates, those who reported medical discrimination when getting medical care were 76 percent (odds ratio [OR] =1.761) more likely to report fair/poor SRH than their counterparts without a discriminatory medical experience. Furthermore, Blacks and Hispanics were between 27 and 29 percent (OR=1.269 and 1.291, respectively) more likely to report fair/poor SRH than Whites, while we did not find any significant difference for other minority groups. Third, echoing the literature (Jylhä, 2009), the socioeconomic status variables were significant factors and their associations with SRH followed the expectations. For example, in contrast to those without a high school diploma, the protective effect of educational attainment on SRH increased with the level of education. The odds ratio of reporting fair/poor SRH dropped from 0.633 (high school graduate or equivalent) to 0.304 (college or post-college degree). Finally, those who used CHCs or outpatient clinics were found to be more likely to report fair/poor SRH than those used other healthcare sources.
Table 2. Global/conventional logistic regression results of SRH (1=fair/poor, 0=good/excellent)a.
| Variables | Coefficient | S.E. | Odds Ratio | Significance |
|---|---|---|---|---|
| Perceived Medical Discrimination (1=yes, 0=no) | 0.566 | 0.088 | 1.761 | *** |
| Demographics | ||||
| Gender (1=Male, 0=Female) | 0.067 | 0.057 | 1.069 | |
| Race/ethnicity (ref.=non-Hispanic White) | ||||
| Non-Hispanic black | 0.238 | 0.058 | 1.269 | *** |
| Hispanics | 0.255 | 0.081 | 1.291 | *** |
| Others | -0.426 | 0.327 | 0.653 | |
| Marital status (Married or cohabiting =1, others=0) | -0.231 | 0.055 | 0.794 | *** |
| Socioeconomic status | ||||
| Poverty (1=poor, 0=non-poor) | 0.344 | 0.068 | 1.411 | *** |
| Educational attainment | ||||
| High school graduate or equivalent | -0.458 | 0.073 | 0.633 | *** |
| Some college education | -0.908 | 0.086 | 0.404 | *** |
| College or post-college graduate | -1.190 | 0.091 | 0.304 | *** |
| Employment status (1=employed, others=0) | -1.123 | 0.055 | 0.325 | *** |
| Access to health care | ||||
| Insurance status (1=having health insurance, 0=no health insurance) | 0.049 | 0.089 | 1.050 | |
| Regular sources of health care | ||||
| Private doctor's office | 0.068 | 0.079 | 1.070 | |
| Community health center/public Clinic | 0.222 | 0.106 | 1.248 | * |
| Outpatient clinic | 0.519 | 0.114 | 1.680 | *** |
|
| ||||
| Corrected AIC=9108.607 | ||||
| Log-likelihood= -4538.272 | ||||
p<0.05;
p<0.001.
We also used Wald tests to examine if the coefficients are significant. The results did not change.
As discussed in the previous section, the GWR logistic regression generated a set of coefficient estimates for each individual, which makes it difficult, if not impossible, to present all results. Following Fotheringham and colleagues (2003), we reported the five-number summary in Table 3 and visualized the GWR findings into thematic maps. We would like to emphasize that while several methods have been proposed to examine spatial non-stationarity (Brunsdon et al., 1998; Leung et al., 2000), these methods are not applicable to the logistic GWR model and visualization remains an appropriate way to explore spatial non-stationarity.
Table 3.
Five-number summary of the GWR logistic regression results.a
| Variables | Min. | Q1 | Median | Q3 | Max. |
|---|---|---|---|---|---|
| Perceived Medical Discrimination (1=yes, 0=no) | 0.431 | 0.469 | 0.578 | 0.632 | 0.820 |
| Demographics | |||||
| Gender (1=Male, 0=Female) | -0.078 | 0.061 | 0.076 | 0.093 | 0.159 |
| Race/ethnicity (ref.=non-Hispanic White) | |||||
| Non-Hispanic black | -0.063 | 0.171 | 0.272 | 0.310 | 0.410 |
| Hispanics | 0.111 | 0.185 | 0.272 | 0.306 | 0.464 |
| Others | -1.002 | -0.713 | -0.339 | -0.134 | 0.177 |
| Marital status (Married or cohabiting =1, others=0) | -0.369 | -0.261 | -0.212 | -0.174 | -0.151 |
| Socioeconomic status | |||||
| Poverty (1=poor, 0=non-poor) | 0.244 | 0.271 | 0.293 | 0.354 | 0.593 |
| Educational attainment | |||||
| High school graduate or equivalent | -0.563 | -0.509 | -0.477 | -0.432 | -0.330 |
| Some college education | -1.049 | -1.016 | -0.966 | -0.873 | -0.543 |
| College or post-college graduate | -1.420 | -1.288 | -1.218 | -1.139 | -0.837 |
| Employment status (1=employed, others=0) | -1.185 | -1.175 | -1.160 | -1.117 | -0.966 |
| Access to health care | |||||
| Insurance status (1=having health insurance, 0=no health insurance) | -0.082 | 0.000 | 0.033 | 0.098 | 0.184 |
| Regular sources of health care | |||||
| Private doctor's office | -0.213 | 0.027 | 0.101 | 0.184 | 0.273 |
| Community health center/public Clinic | -0.600 | 0.185 | 0.290 | 0.379 | 0.433 |
| Outpatient clinic | 0.151 | 0.479 | 0.635 | 0.694 | 0.838 |
|
| |||||
| Corrected AIC=9102.437 | |||||
| Log-likelihood= -4507.077 | |||||
Min=minimum, Q1=first quartile, Q3=third quartile, max=maximum.
The five-number summary aims to show the distributions of local estimates and the estimates were obtained after controlling for other covariates.
On the question of whether the GWR logistic model fit our data better than the global logistic model, we compared the corrected AICs in Tables 2 and 3. Because the difference in AICs is 6.17, which is larger than 4, the model with a smaller AIC should be strongly preferred. That being said, the GWR logistic model (AIC=9102.437) fit our data better5, and the results should provide more robust results to our research questions and hypotheses.
As Table 3 shows, the GWR estimates range quite dramatically. For example, the maximum of the perceived medical discrimination is almost twice as large as the minimum. This means that the impact of perceived medical discrimination onto SRH is not consistent across the city. Several variables even had GWR estimates whose slopes changed in direction, such as Black and using a private doctor's practice. These are noteworthy results, indicating that the relationships between our independent variables and SRH may depend on where an individual resides. Being Black, for example, would appear to carry more harm health-wise in some places than others. Where then is being minority causing more harm for SRH?
To better contextualize our GWR estimates, we created the spatially smoothed local estimates and local t-values of the coefficients for our dependent variable and focal predictors (Matthews and Yang, 2012). We then overlaid local estimates with t-values in the geographic information systems and showed the local estimates with a t-value that is greater than 1.96 (p-value < 0.05). That is, the areas with shading were estimated to have statistically significant associations of covariates with SRH. We used the light to dark gradient scheme to show different magnitudes of the local estimates, dark grey being strong effects and light grey indicating weak associations. We find in keeping with Table 3, notable variations with the perception of medical discrimination across the city. While the coefficient remains statistically significant across the entire study area, its magnitude is lower in the southwestern portion of the city than in the Northeastern portion.
Comparing these results to the racial typology and kernel estimates, the areas with low magnitudes appear to correspond to areas of the city which are mostly Black or mixed, especially for tracts in the West District and Lower Southwest District. Meanwhile, the areas with the strongest effects, the Upper and Lower Far Northeast regions, are characterized by mixed neighborhoods were surrounded by predominately white neighborhoods. This suggests that in spite of the higher overall rates of perceived discrimination in nonwhite areas, people in these areas suffer less from perceived medical discrimination than their peers in other sections. Conversely, the negative effects of medical discrimination could be enhanced in the northeastern minority areas being bordered by predominately white neighborhoods. It is important to note that there is no place in the city where the statistical significance of perceived medical discrimination on poor SRH goes away completely. Additionally, the coefficients appear to have more intermediate magnitudes in the minority tracts within the North and Upper North Districts, demonstrating limits of this effect.
The GWR results for the other variables are ambiguous as to the existence of a protective health effect for minorities residing in Black and Hispanic areas. The positive relation of being Black or Hispanic to poor/fair SRH, while significant in the global model, is found in Figure 3 respectively only to be significant in parts of the city. What is more, the magnitude of these coefficients varies from one area to another. This figure reveals the magnitudes for the positive effect of being Black or Hispanic onto poor/fair SRH are the strongest in the predominately white tracts of the Lower Northwest District, which is notable given the overall lower levels of poor SRH in this area identified in Figure 2. However, save for parts of the Central District and South District, most of the remaining areas where significant coefficients can be found correspond to either mostly predominately black, nonblack minority, or racially mixed tracts. Meanwhile, the predominately white Upper and Lower Far Northeast Districts of the city had no significant local coefficients. In other words, save for some notable exceptions, poor SRH for nonwhites is mostly clustering in mostly nonwhite communities. This is noteworthy because these minority areas are where the negative health effects of perceiving medical discrimination were weaker.
Figure 3. Maps of GWR Local Estimates of Selected Variablesa.
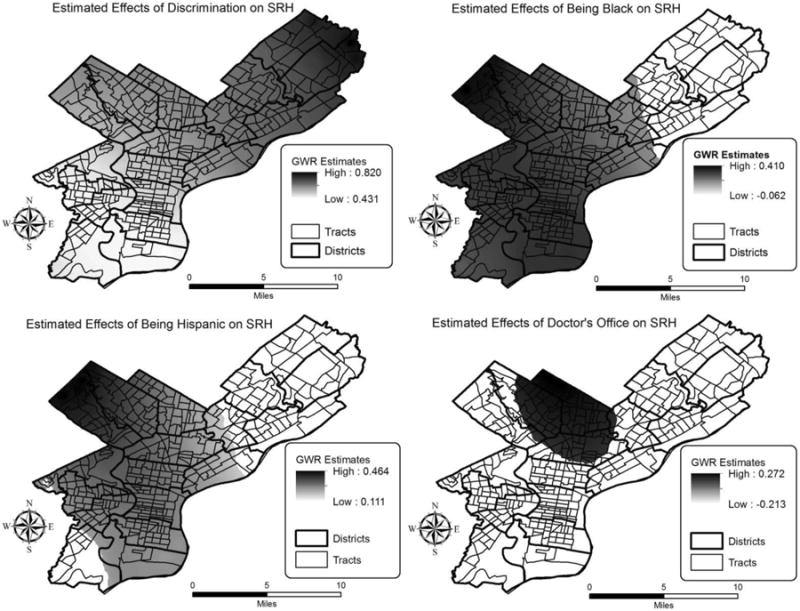
a. The space in white indicates the areas where the local estimates are not statistically significant
Another important finding from our GWR estimates worth exploring further was the change in direction of the coefficient for going to a private doctor's office on SRH. While going to private practices did not have a significant relation to SRH in the global model, the GWR maps in Figure 3 reveal that in the mostly black Upper North District choosing to go to a private practice had a significant positive effect on poor/fair SRH. This trend is surprising not only for its lack of significance in the global model but also because it contradicts the common assumption that private practices should lead to better health outcomes. It should be notedthat this area is mostly nonwhite and has intermediate effect of perceived medical discrimination on SRH.
6. Discussion and Conclusions
Using the GWR approach, the goal of this study was to evaluate the spatial heterogeneity underlying perceived medical discrimination as it related to poor/fair SRH. We explored this first through a hypothesis (H1) stating that perceived medical discrimination from healthcare practitioners adversely affects SRH consistently across space, even after controlling for other covariates. While the global results show that, ceteris paribus, individuals reporting perceived medical discrimination were almost 80 percent more likely to have fair/poor SRH, we found with our GWR results that the effect of perceived medical discrimination on poor/fair SRH varies spatially in our study area. Comparing these results to the racial typology, the magnitude of this detrimental effect was stronger in the areas where most neighborhoods were predominantly White, or surrounded by predominantly White areas, rather than the areas where most neighborhoods were predominately Black or racially mixed. This is an important advance in our understanding of communities in segregated cities, pointing to a relative weaker effect of perceived medical discrimination which offsets the otherwise poor health outcomes of people in these areas.
We evaluate ethnic density's impact on minority SRH with our second (H2) and third hypotheses (H3), which stated that minority status and nonblack minority status respectively should have less impact on poor/fair SRH in mostly nonwhite areas. Our GWR results offer some support for these hypotheses, as the magnitudes of the effect of being Black or Hispanic were the strongest in the mostly White Lower Northwest District of the city. This suggests for Black or Hispanic respondents, living in mostly White areas is associated with the greatest risk of reporting poor/fair SRH. These results echo the findings of previous multi-level modeling research that found Blacks were more likely to report poor SRH when residing in predominately white neighborhoods (Gibbons and Yang, 2014). As for the unique experience of Blacks compared to non-black minorities, while the exact spatial distributions of coefficients for Blacks and Hispanics are different, both groups have weaker coefficients in minority areas. Along with the spatial variations in perceived medical discrimination, this challenges the established research on segregation and health which paints segregation as unilaterally detrimental for minority well-being (Acevedo-Garcia et al., 2003; Subramanian, 2005; Williams and Collins, 2001).
In spite of this strong evidence for the ethnic density effect, our other results were more ambiguous. For one, there were no significant coefficients for being Black or Hispanic in the mostly White Upper and Lower Far Northeast Districts. Furthermore, most of the remaining areas where the coefficient for being Black or Hispanic was significant were either mostly Black, mostly nonblack minority, or racially mixed. This demonstrates health disadvantages still exist for nonwhites living in segregated minority communities. Why then is the strongly positive and significant magnitude observed for the mostly White Lower Northwest rather than other mostly White areas in the city? It may be that minorities in the Lower Northwest are experiencing other forms of subtle discrimination due to that area's proximity to racially mixed and mostly Black areas. Past work has shown White communities in close proximity nonwhite communities exhibit strong discriminatory attitudes towards nonwhite community members (Reider, 1987). It may also be related to the large underlying black population found in this area identified through the PHMC data, depicted in Figure 2. However, we do not have sufficient data to verify either possibility. At the very least, these results allow us to reconcile somewhat the protective health effects of segregation we found to the previous research on this subject which consistently identified negative health effects in these places. We do so by demonstrating that both the detrimental and protective effects of segregation vary spatially, due in no small part to local factors.
Finally, we did not find support for our fourth hypothesis (H4) that going to CHCs or outpatient clinics confounds the relation of medical discrimination to SRH. The spatial variation we found for the impact of medical discrimination and race on SRH holds even when accounting for the choice of provider. This suggests that even if medical discrimination is at least partially routed in institutional discrimination, there is a varying local character influencing it as well. This is not to say there are no health disparities based on the practitioner one uses. For example, respondents whose regular source of healthcare was outpatient clinics were 70 percent more likely to report fair/poor SRH than those who seek healthcare from other sources of care. An interesting revelation from our GWR findings is the SRH of the individuals living in the mostly Black Upper North District were adversely affected if private doctor's offices were their regular source of healthcare. This goes against the common wisdom that private practices have a unilaterally positive influence on health. Also, compared other minority areas in the city, the GWR coefficients for perceived medical discrimination in this area were stronger. These corresponding trends may be pointing to a latent localized effect which is putting the nonwhite community at a disadvantage. In sum, these findings are a prime example of the importance of GWR in unpacking spatial trends that cannot be seen in aspatial models.
Our findings make important contributions to the population literature. By decompiling our results spatially with GWR, we demonstrate that the adverse health effects of medical discrimination are subject to local context, stemming in no small part from racial segregation. Building on this first contribution, we can also say that the health effects of segregation for minorities are multifaceted. Living in a racially homogenous neighborhood offers some protective effects to minorities, slightly relieving the detrimental influence of perceived medical discrimination on SRH. However, this protective effect has its limitations. Save for some notable exceptions, minority SRH is more likely to be poor in segregated areas. Put simply, the reduced the sting of medical discrimination does not change the other health problems minorities may experience in segregated minority communities - not limited to the absence of resources needed to be healthy (Doescher et al., 2001; Story et al., 2008; Williams and Collins, 2001). This is a stark reminder that racial segregation harms health for people of color, even if they are not directly experiencing medical discrimination.
Despite the contributions above, this study is subject to several limitations. First, we cannot account for the race of the healthcare practitioner and how that might impact perceptions of discrimination. In addition, while the measure of perceived medical discrimination directly captures the discriminatory experience when seeking healthcare services, the actual location of where an individual experienced medical discrimination is unavailable. Similarly, our discrimination measure is limited in distinguishing interpersonal discrimination from institutional discrimination. That is, our GWR analysis is confined to one's residential location and one's overall experience in the process of seeking healthcare. Future research may consider the contextualized GWR approach (Harris et al., 2013) to take neighborhood covariates into account or adopt the suggestions by Owen and colleagues (2016) to explore the spatial dimension of neighborhood effect by including the local spatial association measures (Anselin, 1995). Next, though the typology approach to proxy racial segregation has been commonly used in the literature (Friedman, 2008; Gibbons and Yang, 2014; Johnston et al., 2014), there is no agreement on the cut-off thresholds. In addition, the low population counts of non-black minorities make it difficult to account separately for Asian and Hispanic populations whose experiences with segregation may vary greatly. One should be cautious when generalizing our findings and conclusions to other areas or metropolitans where the race/ethnicity composition is different from Philadelphia. Finally, our data are cross-sectional, and the causality between SRH and other independent covariates cannot be derived. In spite of these limitations, our core finding that discrimination's effect on minority health is not constant across space demonstrates the importance of location. This insight should be applicable across a variety of contexts globally.
Several policy implications can be drawn from our findings. There are protective elements found in neighborhoods in segregated regions that can be applied to reduce the impact of medical discrimination, including efforts to foster strong social support among nonwhites (Noh and Kaspar, 2003). Also, cultural competency should be further promoted in the health care system (Brach and Fraserirector, 2000) to minimize, if not eliminate, the discriminatory experience for minorities. Once medical practitioners understand the cultural or attitudinal differences across race/ethnicity groups, they are more likely to treat every patient with respect. However, while these solutions present promising starts, they do get to the deepest problem perpetuating minority health disparities-- residential segregation itself. Until more aggressive desegregation efforts are pursued, gaps in health will remain an ongoing fact of urban life, to which there are no true silver linings.
Footnotes
Henceforth, White
Henceforth, Black
The balancing weights are also known as survey weights because applying the balancing weights to analysis does not change the total sample size and will not lead to the large sample size bias.
Census tracts are derived by the Office of Management and Budget and are a commonly used proxy for neighborhoods.
According to Fotheringham et al (2002) and the common practice in model selection (Burnham and Anderson, 2002), when the difference in AIC is greater than 4, the model with a smaller AIC is preferred.
Contributor Information
Joseph Gibbons, Department of Sociology, 5500 Campanile Drive, San Diego State University.
Tse-Chuan Yang, Department of Sociology, 1400 Washington Ave, University at Albany.
References
- Acevedo-Garcia D, Lochner KA, Osypuk TL, Subramanian SV. Future directions in residential segregation and health research: a multilevel approach. Am J Public Health. 2003;93:215–221. doi: 10.2105/ajph.93.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allard SW. Out of Place: The New Geography of Welfare Policy. University of Chicago Press; Chicago, Illinos: 2009. [Google Scholar]
- Allport G. The nature of prejudice. Perseus Books; Cambridge, MA: 1954. [Google Scholar]
- Bagheri N, Holt A, Benwell GL. Using Geographically Weighted Regression to Validate Approaches for Modelling Accessibility to Primary Health Care. Appl Spat Anal Policy. 2009;2:177. doi: 10.1007/s12061-009-9021-0. [DOI] [Google Scholar]
- Bécares L, Cormack D, Harris R. Ethnic density and area deprivation: Neighbourhood effects on Māori health and racial discrimination in Aotearoa/New Zealand. Soc Sci Med. 2013;88:76–82. doi: 10.1016/j.socscimed.2013.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bécares L, Nazroo J, Stafford M. The buffering effects of ethnic density on experienced racism and health. Health Place. 2009;15:700–708. doi: 10.1016/j.healthplace.2008.10.008. [DOI] [PubMed] [Google Scholar]
- Black NC. An Ecological Approach to Understanding Adult Obesity Prevalence in the United States: A County-level Analysis using Geographically Weighted Regression. Appl Spat Anal Policy. 2014;7:283–299. doi: 10.1007/s12061-014-9108-0. [DOI] [Google Scholar]
- Blair IV, Steiner JF, Fairclough DL, Hanratty R, Price DW, Hirsh HK, Wright LA, Bronsert M, Karimkhani E, Magid DJ, Havranek EP. Clinicians' Implicit Ethnic/Racial Bias and Perceptions of Care Among Black and Latino Patients. Ann Fam Med. 2013;11:43–52. doi: 10.1370/afm.1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boulware LE, Cooper LA, Ratner LE, LaVeist TA, Powe NR. Race and trust in the health care system. Public Health Rep. 2003;118:358. doi: 10.1016/S0033-3549(04)50262-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brach C, Fraserirector I. Can cultural competency reduce racial and ethnic health disparities? A review and conceptual model. Med Care Res Rev. 2000;57:181–217. doi: 10.1177/1077558700057001S09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TN. Exposure to All Black Contexts and Pyschological Well-Being: The Benefits of Racial Concentration. Afr Am Res Perspect. 2001;7:157–172. [Google Scholar]
- Brunsdon C, Fotheringham AS, Charlton M. Spatial nonstationarity and autoregressive models. Environ Plan A. 1998;30:957–973. doi: 10.1068/a300957. [DOI] [Google Scholar]
- Brunsdon C, Fotheringham S, Charlton M. Geographically weighted regression: a method for exploring spatial nonstationarity. Encycl Geogr Inf Sci. 2008:558. [Google Scholar]
- Brunsdon C, Fotheringham S, Charlton M. Geographically weighted regression. J R Stat Soc Ser Stat. 1998;47:431–443. doi: 10.1002/sim.2129. [DOI] [PubMed] [Google Scholar]
- Burnham K, Anderson D. Model selection and multimodel inference: a practical information-theoretic approach. Springer Science & Business Media; New York, NY: 2002. [Google Scholar]
- Chen VYJ, Yang TC. SAS macro programs for geographically weighted generalized linear modeling with spatial point data: Applications to health research. Comput Methods Programs Biomed. 2012;107:262–273. doi: 10.1016/j.cmpb.2011.10.006. [DOI] [PubMed] [Google Scholar]
- Collins KS, Fund C. Diverse communities, common concerns: assessing health care quality for minority Americans. Commonwealth Fund; New York: 2002. [Google Scholar]
- Comber AJ, Brunsdon C, Phillips M. The Varying Impact of Geographic Distance as a Predictor of Dissatisfaction Over Facility Access. Appl Spat Anal Policy. 2012;5:333–352. doi: 10.1007/s12061-011-9074-8. [DOI] [Google Scholar]
- Cooper LA, Roter DL, Carson KA, Beach MC, Sabin JA, Greenwald AG, Inui TS. The associations of clinicians' implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. Am J Public Health. 2012;102:979–987. doi: 10.2105/AJPH.2011.300558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis A. Women, Race and Class. Vintage; New York, NY: 1983. [Google Scholar]
- Doescher MP, Saver BG, Fiscella S, Franks P. Racial/Ethnic Inequities in Continuity and Site of Care: Location, Location, Location. HSR Health Serv Res. 2001;36:78–89. [PMC free article] [PubMed] [Google Scholar]
- Du Bois WEB. The Philadelphia Negro: A Social Study. University of Pennsilvania Press; Pennsylvania, PA: 1899. [Google Scholar]
- Forrest CB, Whelan EM. Primary Care Safety-Net Delivery Sites in the United States A Comparison of Community Health Centers, Hospital Outpatient Departments, and Physicians' Offices. J Am Med Assoc. 2000;284:2077–2083. doi: 10.1001/jama.284.16.2077. [DOI] [PubMed] [Google Scholar]
- Fotheringham S, Brunsdon C, Charlton M. Geographically weighted regression: the analysis of spatially varying relationships. John Wiley & Sons; New York, NY: 2003. [Google Scholar]
- Friedman S. Do declines in residential segregation mean stable neighborhood racial integration in metropolitan America? A research note. Soc Sci Res. 2008;37:920–933. doi: 10.1016/j.ssresearch.2007.06.010. [DOI] [Google Scholar]
- Gaskin DJ, Arbelaez JJ, Brown JR, Petras H, Wagner FA, Cooper LA. Examining racial and ethnic disparities in site of usual source of care. J Natl Med Assoc. 2007;99:22. [PMC free article] [PubMed] [Google Scholar]
- Gaskin DJ, Price A, Brandon DT, LaVeist TA. Segregation and Disparities in Health Services Use. Med Care Res Rev. 2009;66:578–589. doi: 10.1177/1077558709336445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee GC. A multilevel analysis of the relationship between institutional and individual racial discrimination and health status. Am J Public Health. 2002;92:615–623. doi: 10.2105/ajph.92.4.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons J, Yang TC. Connecting Across the Divides of Race/Ethnicity: How Does Segregation Matter? Urban Aff Rev Online First. 2015:1–28. doi: 10.1177/1078087415589193. [DOI] [Google Scholar]
- Gibbons J, Yang TC. Self-Rated Health and Residential Segregation: How Does Race/Ethnicity Matter? J Urban Health. 2014;91:648–660. doi: 10.1007/s11524-013-9863-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goyal MK, Kuppermann N, Cleary SD, Teach SJ, Chamberlain JM. Racial Disparities in Pain Management of Children With Appendicitis in Emergency Department. JAMA Pediatr Online First. 2015 doi: 10.1001/jamapediatrics.2015.1915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene J, Blustein JAN, Weitzman BC. Race, segregation, and physicians' participation in Medicaid. Milbank Q. 2006;84:239–272. doi: 10.1111/j.1468-0009.2006.00447.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris R, Dong G, Zhang W. Using Contextualized Geographically Weighted Regression to Model the Spatial Heterogeneity of Land Prices in Beijing, China: Using GWR to Model the Spatial Heterogeneity of Land Prices. Trans GIS. 2013;17:901–919. doi: 10.1111/tgis.12020. [DOI] [Google Scholar]
- Hunt MO, Wise LA, Jipguep MC, Cozier YC, Rosenberg L. Neighborhood racial composition and perceptions of racial discrimination: evidence from the Black Women's Health Study. Soc Psychol Q. 2007;70:272–289. [Google Scholar]
- Idler EL, Benyamini Y. Self-Rated Health and Mortality: A Review of Twenty-Seven Community Studies. J Health Soc Behav. 1997;38:21. doi: 10.2307/2955359. [DOI] [PubMed] [Google Scholar]
- Johnson RL(Ed) Patient Race/Ethnicity and Quality of Patient–Physician Communication During Medical Visits. Am J Public Health. 2004;94:2084–2090. doi: 10.2105/ajph.94.12.2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston R, Poulsen M, Forrest J. Social-Spatial Segregation: Concepts, Processes and Outcomes. Policy Press at the University of Bristol; Bristol: 2014. Segregation Matters, Measurment Matters; pp. 13–44. [Google Scholar]
- Jylhä M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc Sci Med. 2009;69:307–316. doi: 10.1016/j.socscimed.2009.05.013. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Mickelson KD, Williams DR. The Prevalence, Distribution, and Mental Health Correlates of Perceived Discrimination in the United States. J Health Soc Behav. 1999;40:208–230. [PubMed] [Google Scholar]
- Kramer MR, Hogue CR. Is Segregation Bad for Your Health? Epidemiol Rev. 2009;31:178–194. doi: 10.1093/epirev/mxp001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung Y, Mei CL, Zhang WX. Statistical tests for spatial nonstationarity based on the geographically weighted regression model. Environ Plan A. 2000;32:9–32. doi: 10.1068/a3162. [DOI] [Google Scholar]
- Massey DS, Denton NA. American Apartheid: Segregation and the Making of the Underclass. Harvard University Press; Cambridge, MA: 1993. [Google Scholar]
- Matthews SA, Yang TC. Mapping the results of local statistics: Using geographically weighted regression. Demogr Res. 2012;26:151–166. doi: 10.4054/DemRes.2012.26.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noh S, Kaspar V. Perceived discrimination and depression: Moderating effects of coping, acculturation, and ethnic support. Am J Public Health. 2003;93:232–238. doi: 10.2105/ajph.93.2.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliver JE, Wong J. Intergroup Prejudice in Multiethnic Settings. Am J Polit Sci. 2003;47:567. doi: 10.2307/3186119. [DOI] [Google Scholar]
- Owen G, Harris R, Jones K. Under examination: Multilevel models, geography and health research. Prog Hum Geogr. 2016;40:394–412. doi: 10.1177/0309132515580814. [DOI] [Google Scholar]
- Paradies Y. A systematic review of empirical research on self-reported racism and health. Int J Epidemiol. 2006;35:888–901. doi: 10.1093/ije/dyl056. [DOI] [PubMed] [Google Scholar]
- Patterson O. The Ordeal of Integration: Progress and Resentment in America's Racial Crisis. Civitas; Washington, DC; 1997. [Google Scholar]
- Pickett KE, Wilkinson RG. People like us: ethnic group density effects on health. Ethn Health. 2008;13:321–334. doi: 10.1080/13557850701882928. [DOI] [PubMed] [Google Scholar]
- Radecki SE, Bernstein GS. Use of clinic versus private family planning care by low-income women: access, cost, and patient satisfaction. Am J Public Health. 1989;79:692–697. doi: 10.2105/ajph.79.6.692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reider J. Canarsie: The Jews and Italians of Brooklyn Against Liberalism. Harvard University Press; Cambridge, MA: 1987. Reprint ed. [Google Scholar]
- Sampson RJ. Great American City: Chicago and the Enduring Neighborhood Effect. 1st. University of Chicago Press; Chicago, Illinos: 2012. [Google Scholar]
- Shaw RJ, Pickett KE. The association between ethnic density and poor self-rated health among US Black and Hispanic people. Ethn Health. 2011;16:225–244. doi: 10.1080/13557858.2011.561428. [DOI] [PubMed] [Google Scholar]
- Shoff C, Yang TC. Untangling the associations among distrust, race, and neighborhood social environment: A social disorganization perspective. Soc Sci Med. 2012;74:1342–1352. doi: 10.1016/j.socscimed.2012.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Story M, Kaphingst KM, Robinson-O'Brien R, Glanz K. Creating Healthy Food and Eating Environments: Policy and Environmental Approaches. Annu Rev Public Health. 2008;29:253–272. doi: 10.1146/annurev.publhealth.29.020907.090926. [DOI] [PubMed] [Google Scholar]
- Subramanian SV. Racial residential segregation and geographic heterogeneity in black/white disparity in poor self-rated health in the US: a multilevel statistical analysis. Soc Sci Med. 2005;60:1667–1679. doi: 10.1016/j.socscimed.2004.08.040. [DOI] [PubMed] [Google Scholar]
- Watkins-Hayes C. The New Welfare Bureaucrats: Entaglements of Race, Class, and Policy Reform. University of Chicago Press; Chicago, Illinos: 2009. [Google Scholar]
- Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116:404. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu S, Wang R, Zhao Y, Ma X, Wu M, Yan X, He J. The relationship between self-rated health and objective health status: a population-based study. BMC Public Health. 2013;13:320. doi: 10.1186/1471-2458-13-320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang TC, Matthews SA. Understanding the non-stationary associations between distrust of the health care system, health conditions, and self-rated health in the elderly: A geographically weighted regression approach. Health Place. 2012;18:576–585. doi: 10.1016/j.healthplace.2012.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou M. Chinatown: The Socioeconomic Potential of an Urban Enclave. Temple University Press; Philadelphia, PA: 1992. [Google Scholar]


