Abstract
Individuals’ behaviors are influenced by those of others in their social environment (i.e., descriptive norms), as well as by how individuals perceive they should behave in that environment (e.g., injunctive norms). Although social norms are thought to play an important role in hepatitis B virus (HBV) screening, limited theoretical or empirical guidance exists on how the underlying process works. In addition, norms are social phenomena that are spread through family discussion about the importance of getting HBV screening. Using the theory of normative social behavior (TNSB), this study examined the roles of injunctive norms (IN), descriptive norms (DN), and family discussion in HBV screening behavior among Asian Americans. Data from a survey of Asian Americans in the Baltimore Washington metropolitan area (N = 877) were used to test underlying theoretical propositions. DN and family discussion emerged as key factors in HBV screening behavior among all Asian Americans. IN were associated with HBV screening among Chinese and Korean Americans, but not for Vietnamese Americans. Family discussion moderated the influence of DN on behavior among Chinese and Vietnamese Americans. However, the main effect of DN on screening behavior was not modified by IN (no interactions between DN and IN). The results indicate that family discussion and social norms are integral in enabling Asian Americans to undergo HBV screening and warrant sensitivity in the design and implementation of a liver cancer prevention program in this high-risk group of Asian Americans.
Hepatocellular carcinoma (HCC) is the major form of primary liver cancer. Asian Americans experience the highest liver cancer incidence and mortality rates of all ethnic groups in the United States (ACS, 2017). In a recent summary of cancer incidence trends among Asian American populations (Gomez et al., 2013), Vietnamese had the highest incidence of liver cancer of all racial/ethnic groups (58.5 per 100,000 for men; 20.9 for women). Incidence among Korean males (34.9) and Chinese males (24.1) was much higher than among white males (8.9) (Gomez et al., 2013; Siegel, Miller, & Jemal, 2015). Chronic hepatitis B virus (HBV) infection is the most common cause of liver cancer, accounting for 80% of all cases. While HBV shows up rarely among Whites in the United States (0.1%), as many as 1 in 10 Asian Americans carry the virus, accounting for more than half of the cases in the U.S. A quarter of hepatitis B patients will eventually die of liver cancer or liver failure. Chronic HBV infection and liver cancer in Asian Americans is a source of one of the most serious—but frequently neglected—racial and ethnic disparities in the United States (Office of Minority Health, 2011).
Because of the asymptomatic nature of chronic HBV, about 65% of infected adults are unaware of their condition (Institute of Medicine, 2010). In combination with cultural, linguistic, and financial barriers, this knowledge gap can drive HBV infection rates even higher—particularly for high-risk groups, such as foreign-born Asian American immigrants. With insufficient knowledge of liver cancer prevention and treatment and low rates of HBV screening among adults, Asian Americans (AAs) are often diagnosed with late-stage cancer, resulting in high mortality rates.
AAs only constituted 6.3% of the total U.S. population in 2014, but they are the fastest-growing racial/ethnic group in the United States (Colby & Ortman, 2015; Hoeffel, Rastogi, Kim, & Shahid, 2012). In contrast to other rapidly growing ethnic groups, such as Hispanic-Americans, population growth among AAs is driven primarily by immigration rather than by U.S. births. Because HBV infection is highly endemic in their countries of birth and a high proportion of immigrants are unaware of their HBV status, AAs experience disproportionately higher incidence and mortality from diseases such as liver cancer (Torre et al., 2016). Several surveys have shown that AAs have a low HBV screening rate, ranging from 7.5% to 54% for self-reported screening rates by region and various Asian ethnic groups (Choe et al., 2006; Ma et al., 2011, 2007; Strong, Lee, Tanaka, & Juon, 2012; Taylor, Jackson, Chan, Kuniyuki, & Yasui, 2002; Thompson et al., 2002). In a self-reported survey of 1,312 AAs in the Delaware Valley region, Ma and her colleagues (2011) reported significant ethnic differences in HBV screening: Chinese (37.8%) had the highest screening rate, followed by Koreans (32.2%) and Vietnamese (20.3%). Therefore, it is important to develop educational programs to increase early detection of HBV infection through screening activities in high risk AAs.
HBV screening behavior is the first step in liver cancer prevention and hence its psychosocial determinants might be important to study. Like other important health behaviors, it is likely that determinants of HBV screening behaviors may be driven by social influences (although this has not been explicitly studied before, to our knowledge). Whether to get screened may be the result of knowing the importance of screening, but it may also be guided by the extent to which individuals believe others in their social network engage in the behavior (descriptive norms) and pressures they perceive to do the same (injunctive norms) (see Cialdini, Reno, & Kallgren, 1990).
In broader terms, this is one of the central ideas behind the theory of normative social behavior (TNSB; Rimal & Real, 2005). The literature provides strong evidence for the impact of social norms on a variety of behaviors, including alcohol consumption (Padon, Rimal, Jernigan, Siegel, & DeJong, 2016; Pedersen et al., 2017; Rimal, 2008; Rimal & Mollen, 2013), tobacco use (Ali & Dwyer, 2009; Mead, Rimal, Ferrence, & Cohen, 2014; Mereish, Goldbach, Burgess, & DiBello, 2017), cannabis use (Ecker & Buckner, 2014; Mereish et al., 2017), healthy food consumption (Mollen, Rimal, Ruiter, & Kok, 2013), contraceptive use (Rimal & Lapinski, 2015), and HIV testing (Batona, Gagnon, Simonyan, Guedou, & Alary, 2015). Findings on the role of norms do vary, however. For example, Smith-McLallen and Fishbein (2008) examined the roles of injunctive norms (IN) and descriptive norms (DN) in predicting intentions to engage in cancer screening, including mammography, colonoscopy, and PSA testing. They found that IN were important predictors of intention for all three cancer screening tests, while DN were not associated with cancer screening intention. In contrast, in a study of 2426 German men, DN were associated with prostate and colon cancer screening intention and DN interacted significantly with IN (Sieverding, Matterne, & Ciccarello, 2010). To date, the roles of IN and DN in predicting in HBV screening behavior have not been tested.
The TNSB posits not only that descriptive and injunctive norms independently influence behavior but also that these two factors operate interactively, such that the influence of descriptive norms on behaviors is heightened when injunctive norms are also strong. In other words, individuals are more likely to engage in a popular behavior if they also believe they are under pressure from their peers to do so (Rimal, 2008; Rimal & Lapinski, 2015). This particular hypothesis has been tested in number of health behaviors including alcohol consumption (Rimal, 2008), contraceptive behavior (Rimal & Lapinski, 2015), and cancer screening intention (Sieverding et al., 2010). So far, this has not been tested on HBV screening behavior. Our hypothesis tests this proposition.
Furthermore, because interpersonal discussion in a social network is often the vehicle through which normative information is shared (Calhoun et al., 2013; Real & Rimal, 2007), the influence of descriptive norms is also heightened when interpersonal communication is present. In Asian American societies, family discussion about HBV infection is important – not only because of the family orientation of many Asian Americans but also because 90% of HBV transmission among AAs comes from mother to child (vertical transmission). Moreover, because of the stigma attached to HBV infection, AAs may restrict their HBV-related discussions only to family members, severely limiting such discussions with peers, coworkers, and others. In this paper, family discussion was used as a measure of interpersonal communication about HBV screening behavior. So far, it is not known what role family discussion plays in normative influences on HBV screening behavior. In this paper, we seek to understand the underlying process and also test the hypothesis how the interaction between DN and family discussion affects on HBV screening behaviors.
The effects on health and health behavior of navigating these varied and potentially conflicting norms and expectations are often discussed in the context of acculturation (Elder, Broyles, Brennan, Zuniga De Nuncio, & Nader, 2005). As proxy measures of acculturation, studies of Asian Americans have used duration of U.S. residence, proportion of life spent in the United States, and spoken English proficiency to predict cancer screening behaviors (e.g., mammogram, Pap test, and colonoscopy) and health examination (e.g., physical, dental, and eye exam): A higher level of acculturation has been found to be associated with a number of better preventive health behaviors among Asian immigrants (Jung et al., 2017; Lee, Chae, Jung, Chen, & Juon, 2016; Lee, Chen, Jung, Baezconde-Garbanati, & Juon, 2014). In contrast, greater length of residence in the U.S. is associated with decreased HBV screening (Strong et al., 2012; Tanaka, Gehan, Chen, & Wang, 2014; Tanaka, Strong, Lee, & Juon, 2013). In this paper, we will explore the role of acculturation on HBV screening.
Application of the TNSB to liver cancer prevention leads to the prediction that the relationship between DN and HBV screening behavior among AAs may be enhanced by IN and family discussion. However, there have been no empirical studies to explore these potential influences on HBV screening and vaccination behaviors in high-risk AAs. Overall, we hypothesized that the influence of descriptive norms on screening behavior is strengthened when (a) IN are strong and (b) interpersonal communication is high. In addition, we explored potential differences in TNSB constructs between three ethnic subpopulations (i.e., Chinese, Korean, and Vietnamese Americans) and how these differences predicted their HBV screening behavior. Also, in the special context of immigrants, we hypothesized that less acculturated Asian Americans are more likely to have HBV screening. This study fills a significant gap in the health communication literature by extending TNSB to the study of HBV screening behavior among AAs and by providing evidence to leverage its potential in designing effective interventions.
Methods
We used the baseline survey data collected for the Maryland Asian American Liver Cancer Education Program (hereafter “the Program”) for this analysis. The Program was a cluster randomized control design that tested the hepatitis B/liver cancer educational program. The Program received approval for Human Subject Research from the Institutional Review Board of Johns Hopkins Bloomberg School of Public Health.
Recruitment Strategy
The Program recruited 877 participants (294 Korean, 303 Chinese, and 280 Vietnamese immigrants) living in the Baltimore–Washington metropolitan area. Between November 2009 and June 2010, self-identified Asian American adults (18 years of age and older) at various Chinese, Korean, and Vietnamese community-based organizations (CBOs) completed a self-reported questionnaire. The sampling frame for these organizations was created from ethnic yellow-pages, industry membership directories, and suggestions from community leaders in the targeted region. We contacted the leaders or pastors of these CBOs to seek their consents. A total of 32 organizations agreed to participate in the Program. Then, participants were recruited from faith-based organizations (churches and temples) and CBOs (e.g., language schools and college cultural group organizations). Asian grocery stores, restaurants, and nail salons were additional locations from which participants were recruited. Organizational membership was not a requirement for participation (see more detail, Juon & Park, 2013; Strong et al., 2012).
Data Collection Procedures
A total of 940 individuals were recruited, of which 93% (n = 877) agreed to participate and completed the study. Volunteers were required to be at least 18 years old and had never participated in hepatitis B education. Participants filled in a paper form of self-administered baseline questionnaire in their choice of the language (their native language or English).
Measures
HBV screening behavior, the dependent variable, was measured by asking participants “Have you ever had hepatitis B screening, which is not liver function test?” (Strong et al., 2012). It was coded yes (=1) or no (=0).
Descriptive norms (DN) are one dimension of normative beliefs, defined as norms which pertain to the prevalence of a behavior (Cialdini et al., 1990). DN were elicited by asking respondents three questions about their perceptions of the proportion of key groups living in the United States (friends, family members, and other Asians) having ever had HBV screening (Lapinski, Maloney, Braz, & Shulman, 2013; Rimal & Real, 2005). Response categories ranged from none (1) to all (7). Three items were used to create a composite index score for DN by summing scores, with higher scores indicating greater descriptive norms for HBV screening (n = 3, α = 0.82).
Injunctive norms (IN) were defined as norms which pertain to social pressures experienced by participants to conform (Cialdini et al., 1990). IN focused on respondents’ perceptions about support for HBV screening, specifically by asking whether participants believed other persons (family members, close friends, most people that they know, and their physician) approved of having HBV screening (Lapinski et al., 2013; Rimal & Real, 2005) (n = 4, α = 0.94). A 7-point Likert scale was used, ranging from “strongly disagree” (1) to “strongly agree” (7). Four items were used to create a composite index score for IN by summing up the scores. Then, we used the median split for making two categories (approval [=1] or disapproval [=0]).
Family Discussion (FD): Respondents were asked whether they ever discussed HBV screening with their family members (0 = no; 1 = yes).
Acculturation is measured by proportion of life spent in the U.S. which indicates how much an Asian-American is used to the American culture and lifestyle (0 = < 25% of their life; 1 = ≥25% of their life),
Control variables included age, sex (0 = male; 1 = female), education level (0 = ≤high school; 1 = ≤college; 2 = college graduate+), and family history of HBV infection (0 = no; 1 = yes).
Statistical Analysis
Logistic regression was used to assess main effects and interaction effects. Interaction effects were tested by including a cross-product in the regression model that included the two corresponding main effects (between DN and IN and between DN and FD). We conducted multivariate regression analysis in the total population and then conducted subgroup analysis by ethnicity. We used Stata version 13 for all analyses (StataCorp, 2013).
Results
Table 1 presents characteristics of study participants. The sample consisted of 877 Asian Americans (303 Chinese, 294 Koreans, 280 Vietnamese). Vietnamese Americans were younger than Chinese and Korean Americans (p < .05). There were also some ethnic differences in education, social norms, and family communication (p < .001): Chinese Americans were more highly educated than Korean and Vietnamese Americans, and they had higher levels of graduate school education (50.2%, 17.3%, and 8.2%, respectively). Chinese Americans reported the highest mean DN scores (3.34) followed by Vietnamese Americans (3.08) and Korean Americans (2.73). Vietnamese Americans had higher proportion of approving IN and family discussion than the other two ethnic groups. More than two thirds of Vietnamese Americans (69.2%) had spent more than 25% of their life in the United States, compared to Korean Americans (59.5%) and Chinese Americans (58.1%) (p < .05). Chinese Americans (54.6%) had higher HBV screening rates than Korean Americans (45.6%) and Vietnamese Americans (39.4%) (p < .001).
Table 1.
Study participant characteristics (n = 877)
| Characteristics | Korean (n = 294) N (%) |
Chinese (n = 303) N (%) |
Vietnamese (n = 280) N (%) |
p value |
|---|---|---|---|---|
| Age (mean±SD, range) | 46.1, 13.5 (19–77) | 45.9, 11.5 (21–80) | 43.1, 15.1 (18–89) | .013 |
| Gender | ||||
| Male | 113 (38.4) | 120 (39.6) | 131 (46.8) | .09 |
| Female | 191 (61.6) | 183 (60.4) | 149 (53.2) | |
| Education | ||||
| < High school | 38 (12.9) | 23 (7.6) | 55 (19.6) | <.001 |
| High school+ | 109 (37.1) | 48 (15.8) | 138 (49.3) | |
| College graduate | 96 (32.7) | 80 (26.4) | 64 (22.9) | |
| Graduate school + | 51 (17.3) | 152 (50.2) | 23 (8.2) | |
| Has some HBV infected family member | ||||
| No/not sure | 255 (87.0) | 260 (85.8) | 233 (83.8) | .544 |
| Yes | 38 (13.0) | 43 (14.2) | 45 (16.2) | |
| Proportion of life spent in the United States | ||||
| <25% in life | 119 (40.5) | 127 (41.9) | 86 (30.8) | .012 |
| ≥25% in life | 175 (59.5) | 176 (58.1) | 193 (69.2) | |
| Descriptive norms mean ± SD (1–8) | 2.73, 1.36 | 3.34, 1.70 | 3.08, 1.48 | <.001 |
| Injunctive norms (%) | ||||
| Not approved | 162 (55.1) | 186 (62.0) | 129 (46.4) | <.001 |
| Approved | 132 (44.9) | 114 (38.0) | 149 (53.6) | |
| Family discussion | ||||
| No | 245 (83.6) | 244 (80.5) | 197 (70.6) | <.001 |
| Yes | 48 (16.4) | 59 (19.5) | 82 (31.9) | |
| HBV screening | ||||
| No | 160 (54.4) | 137 (45.4) | 169 (60.6) | <.001 |
| Yes | 134 (45.6) | 165 (54.6) | 110 (39.4) | |
Zero-order correlations were computed across all variables to assess overlapping variance. Table 2 shows that three background variables (education, proportion of life spent in the United States, family history of HBV infection) were significantly associated with HBV screening. Social norms (i.e., injunctive and descriptive norms) and family discussion were also significantly related to HBV screening. This table also shows that, except for significant correlation between family history of HBV infection and family discussion (r = .38, p < .001), remaining correlations were modest and there was little risk for multicollinearity for the multivariate analyses.
Table 2.
Zero-order Pearson correlation (n = 877)
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| 1. Gender | — | |||||||
| 2. Age | .05 | — | ||||||
| 3. Education | −.15** | −.30** | — | |||||
| 4. Proportion to stay in the United States | −.02 | −.05 | −.01 | — | ||||
| 5. Family history of HBV infection | −.01 | −.07* | .06 | .03 | — | |||
| 6. Injunctive norm | −.06 | .03 | .05 | −.03 | .07* | — | ||
| 7. Descriptive norm | .07 | −.02 | .08* | −.05 | .07* | .12** | — | |
| 8. Family discussion | −.04 | −.02 | .03 | −.03 | .38** | .19** | .15** | — |
| 9. HBV screening | −.06 | −.01 | .22** | −.15** | .15** | .19** | .28** | .30** |
Note.
p < .05;
p < .01.
Logistic regression analyses combining all respondents showed that there were main effects of social norms (i.e., descriptive and injunctive norms) and family discussion on HBV screening (see Table 3). Education and proxy measure of acculturation (i.e., proportion of life spent in the United States) were also associated with HBV screening. However, there was no interaction between DN and FD and between DN and IN in bivariate analysis. In multivariate analysis, stronger social norms were associated with an increase in HBV screening (OR = 1.13, 95% CI 1.09, 1.17 for DN; OR = 1.70, 95% CI 1.24, 2.31 for IN). Those who had family discussion about HBV screening were more likely to have HBV screening than those without any family discussion (OR = 4.05, 95% CI 2.64, 6.21). In addition, acculturation was negatively associated with HBV screening: Those who spent more than 25% of their life in the United States were less likely to have HBV screening than those who spent less than 25% of their life in the United States (OR = 0.50, 95% CI 0.37, 0.69).
Table 3.
Logistic regression (odds ratio), assessing HBV screening, Asian Americans (n = 877), Baltimore–Washington metropolitan areas
| Unadjusted OR (95% CI) | Adjusted OR (95% CI) | |
|---|---|---|
| Control variables | ||
| Age | 0.99 (0.98, 1.01) | 1.01 (0.99, 1.02) |
| Gender (Ref = male) | 0.77 (0.59, 1.01) | 0.85 (0.63, 1.17) |
| Education (Ref = < high school) | ||
| High school graduate | 1.69 (1.05, 2.70)* | 1.41 (0.81, 2.44) |
| College education+ | 3.39 (2.17, 5.29)* | 3.48 (2.03, 5.94)* |
| Proportion stay in the US (Ref = < 25%) | 0.53 (0.40, 0.70)* | 0.50 (0.37, 0.69)* |
| Family history of HBV infection (Ref = no) | 2.45 (1.65, 3.64)* | 1.36 (0.84, 2.20) |
| Social Norm | ||
| Descriptive norms (DN) | 1.14 (1.10, 1.18)* | 1.13 (1.09, 1.17)* |
| Injunctive Norms (IN) (Ref = not approved) | 2.03 (1.55, 2.66)* | 1.70 (1.24, 2.31)* |
| Family Discussion (FD) (Ref = no) | 5.01 (3.46, 7.24)* | 4.05 (2.64, 6.22)* |
| Interaction 1 | ||
| DN | 1.12 (1.09, 1.17)* | - |
| FD | 3.45 (1.35, 8.80)* | |
| DN × FD | 1.03 (0.94, 1.13) | |
| Interaction 2 | - | |
| DN | 1.14 (1.09, 1.20)* | |
| IN | 1.92 (0.98, 3.74) | |
| DN × IN | 0.99 (0.93, 1.07) | |
Note.
p < .05.
In bivariate analysis (Table not shown), there were no interactions between DN and IN for all three subgroups of Asian Americans. However, we found significant interactions between DN and FD among Chinese Americans and Vietnamese Americans. Table 4 presents the results of multivariate analyses of subgroups by ethnicity including Chinese, Korean, and Vietnamese Americans. We found main effects of DN and FD on HBV screening among all three subgroups of Asian Americans: higher DN and having family communication were associated with an increase in HBV screening. IN were associated with HBV screening in Chinese Americans and Korean Americans, whereas IN had no main effect on HBV screening in Vietnamese Americans. Living a high proportion of life in the United States was associated with a decrease in HBV screening in Chinese and Korean Americans. Higher education was also associated with an increase in HBV screening in Chinese and Vietnamese Americans.
Table 4.
Multivariate logistic regression (odds ratio) by ethnicity, assessing HBV screening, Asian Americans, Baltimore–Washington metropolitan areas
| Korean (n = 294) | Chinese (n = 301) | Vietnamese (n = 280) | |
|---|---|---|---|
| Control variables | |||
| Age | 1.01 | 0.99 | 1.01 |
| Gender (Ref = male) | 0.61 | 0.88 | 0.84 |
| Education (Ref = < high school) | |||
| High school graduate | 0.74 | 1.96 | 2.01 |
| College education+ | 1.14 | 5.85** | 4.21** |
| Proportion stay in the US (Ref = < 25%) | 0.31** | 0.54* | 0.58 |
| Family history of HBV infection (Ref = no) | 1.07 | 1.51 | 1.31 |
| Social norm | |||
| Descriptive norms (DN) | 1.14** | 1.18** | 1.09* |
| Injunctive norms (IN) (Ref = not approved) | 3.12** | 2.31** | 0.87 |
| Family Discussion (FD) (Ref = no) | 6.35** | 2.78* | 5.06** |
| Interaction | |||
| DN × FD | 1.53 | 1.37* | 0.83* |
Note.
p < .05;
p < .01.
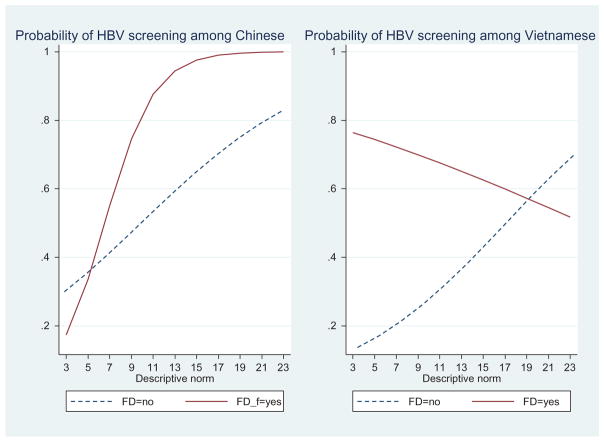
The DN and FD interaction term was significant for Chinese Americans and Vietnamese Americans. Further analysis of interaction pattern showed that among Chinese Americans, the association between DN and HBV screening was greater when they had family discussion than when they had no family discussion. Those with high DN and having FD were most likely to have HBV screening, while those with low DN and having FD were least likely to have HBV screening (OR = 1.37, p < .05). We found a different interaction pattern among Vietnamese Americans (OR = 0.83, p < .05). For those who had family discussion, there was a moderate inverse association between DN and likelihood of having HBV screening, whereas among those who did not have family discussion, the association between DN and likelihood of having HBV screening was positive and strong (steeper slope than the other one). This pattern of interaction is shown in Figure 1.
Fig. 1.
Interaction between descriptive norms and family discussion (FD). Interactions are adjusted for all covariates.
Discussion
Asian Americans are disproportionately at higher risk of liver cancer associated with HBV infection. HBV screening is the first step for hepatitis B prevention, and so investigating the various determinants of this behavior, including the role that social norms play, is important in developing effective behavioral interventions to increase HBV screening. This current study is the first to apply the theory of normative social behavior (Rimal & Real, 2005) to examine whether social norms are important determinants of the HBV screening behavior among high risk groups of Asian Americans: Chinese, Korean, and Vietnamese Americans in the Baltimore Washington metropolitan area.
These findings lend support to our hypotheses that both social norms and family discussion are important determinants of HBV screening behavior. Consistent with other research (Sieverding et al., 2010), we found that DN are significant predictors of HBV screening behavior. The fact that DN plays a meaningful role in predicting HBV screening has practical significance. It appears that HBV screening of others in the Asian American community influences their own screening behaviors. To date, we have not been able to identify an intervention increasing HBV screening that included a DN component.
The significant contribution of IN to HBV screening among two subgroups of Asian Americans (e.g., Chinese and Korean Americans) is consistent with earlier study of cancer screening behaviors (Smith-McLallen & Fishbein, 2008). In contrast, we did not observe a significant main effect of IN on HBV screening among Vietnamese Americans. Given the inconsistent independent contribution of IN to predictions of HBV screening among Vietnamese Americans, one possible explanation for this difference is that no correlation between IN and DN was noted. On the other hand, the average correlation between IN and DN was r = .12, p < .05 for Korean Americans and r = .23, p < .01 for Chinese Americans. It is perhaps the case that the relative weights of DN in predicting HBV screening behavior differed between Vietnamese Americans and other two subgroups of AAs such as Chinese- and Korean-Americans. Consistent with a previous study on contraceptive use behavior (Rimal & Lapinski, 2015), family discussion was associated with increased HBV screening among all three subgroups of AAs.
The TNSB posits that the influence of DN on behavior is modified by family discussion and IN. We found support for the first proposition: Consistent with other research on contraceptive use (Rimal & Lapinski, 2015), we found the moderating role of family discussion was an agent of normative influence on HBV screening behavior for Chinese and Vietnamese Americans, but not for Korean Americans. One of the key functions of interpersonal discussion is to transmit information about norms in the Asian American family. It is through discussions that individuals come to learn about the collective opinions that govern the appropriateness of those behaviors.
It is interesting to note that the effect of DN on HBV screening behaviors was negatively associated with family discussion among Vietnamese Americans. This is an intriguing finding: it is not clear why this pattern of findings would only apply for Vietnamese Americans. One likely (though speculative) explanation might be found in the observation that the Vietnamese American study participants were somewhat different from the Chinese and Korean American participants in that they were younger and less educated. Those who were younger and more educated (r = −.34, p < .01) might be expected to have less communication from family members. We speculate that overall communication with family (let alone discussion on HBV) is quite limited due to language and cultural barriers between them and their parents’ generation. Hence, the influence of family discussion among Vietnamese Americans needs to be explored in future study.
In addition, it is interesting that family discussion did not serve to boost the influence of DN on HBV screening behavior for Korean Americans. Family discussion has a direct influence on screening (in a positive way), but it does not have any moderating role in the relationship between normative beliefs and behaviors. This certainly warrants further inquiry, for it suggests that it may be important to study the content of those conversations, which may be different among the three groups. We did not collect data about communication content.
We did not find support for the second proposition for the moderating role of IN in the relationship between DNs and HBV screening behavior across the three Asian American groups. This was somewhat surprising because, according to the TNSB, we expected descriptive norms and injunctive norms would work synergistically to predict HBV screening behavior. In particular, the lack of an interaction effect between DN and IN in total or within subgroups of AAs was inconsistent with other research on intentions to have prostate and colon cancer screening among men (Sieverding et al., 2010). The nonsignificant moderating role of IN suggests that AAs are more likely to have HBV screening if they believe they are under pressure from significant others. Also, their perception of whether other comparable AAs are having HBV screening is equally important. Our study thus shows that both social norms influence HBV screening behaviors among Asian immigrants. Recently, few studies have examined the interaction of IN and DN on HBV screening behavior. Further research is required to explore on this process of preventive health behaviors.
The finding that greater residential tenure in the United States correlated with lower likelihood of HBV screening is intriguing. Consistent with earlier studies (Strong et al., 2012; Tanaka et al., 2014, 2013), our result shows that the more acculturated an Asian American, the less likely he/she is to have HBV screening. This may be due to lower perceived risk of HBV infection as one becomes more identified as an American, since an average American has lower risk of HBV infection than an average Asian. However, it could also suggest that more recent immigrant groups are prioritized by healthcare providers or public health outreach for HBV prevention activities, and they also may be more easily identified in geographic or cultural enclaves than immigrants who are more assimilated. However, this will need further empirical studies to confirm.
A strength of our study is that it is one of only a few research studies to examine interpersonal communication as an agent of normative influence on HBV screening. The current study’s findings will expand our scientific knowledge of the role of TNSB in HBV screening. Despite these strengths, the study is not free from limitations. First, a sampling frame from CBOs was used, and to minimize the sampling bias due to excluding those who do not attend these organizations regularly, we targeted Asian groceries, nail salons, and restaurants. The findings of the analyses should be understood in this context, and its generalizability may be limited only to the Program participants. Second, those who voluntarily participated in the study might be more motivated to learn about HBV infection, introducing selection bias.
Conclusion
Our study showed that targeting either social norms or family discussion about having HBV screening alone would be sufficient to increase HBV screening for all Asian Americans. Norms-based interventions to increase liver cancer awareness associated with HBV infection are necessary to focus on changing not only descriptive norms but also injunctive norms and family discussion. Our findings also suggest that interventions and communications targeting liver cancer prevention should give special consideration to ethnically specific tailored interventional strategies to effectively increase HBV screening among subgroups of AAs.
Acknowledgments
We thank all the participants of this study. We also appreciate the dedicated work of the members of the research team.
Funding
This study was supported by the National Cancer Institute (grant number R25CA129042; R01CA163805).
Footnotes
Color versions of one or more of the figures in the article can be found online at www.tandfonline.com/uhcm.
References
- Ali MM, Dwyer DS. Estimating peer effects in adolescent smoking behavior: A longitudinal analysis. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine. 2009;45(4):402–408. doi: 10.1016/j.jadohealth.2009.02.004. [DOI] [PubMed] [Google Scholar]
- American Cancer Society (ACS) Cancer fact & figures 2017. Atlanta, GA: Author; 2017. [Google Scholar]
- Batona G, Gagnon MP, Simonyan DA, Guedou FA, Alary M. Understanding the intention to undergo regular HIV testing among female sex workers in Benin: A key issue for entry into HIV care. Journal of Acquired Immune Deficiency Syndromes. 2015;68(Suppl 2):S206–212. doi: 10.1097/qai.0000000000000452. [DOI] [PubMed] [Google Scholar]
- Calhoun LM, Speizer IS, Rimal R, Sripad P, Chatterjee N, Achyut P, Nanda P. Provider imposed restrictions to clients’ access to family planning in urban Uttar Pradesh, India: A mixed methods study. BMC Health Services Research. 2013;13(1):1. doi: 10.1186/1472-6963-13-532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choe JH, Taylor VM, Yasui Y, Burke N, Nguyen T, Acorda E, Jackson JC. Health care access and sociodemographic factors associated with hepatitis B testing in Vietnamese American men. Journal of Immigrant and Minority Health. 2006;8(3):193–201. doi: 10.1007/s10903-006-9322-1. [DOI] [PubMed] [Google Scholar]
- Cialdini RB, Reno RR, Kallgren CA. A focus theory of normative conduct: Recycling the concept of norms to reduce littering in public places. Journal of Personality and Social Psychology. 1990;58(6):1015. doi: 10.1037/0022-3514.58.6.1015. [DOI] [Google Scholar]
- Colby SL, Ortman JM. US Census Bureau, Ed, editor. Projections of the Size and Composition of the US Population: 2014 to 2060. 2015. pp. 25–1143. [Google Scholar]
- Ecker AH, Buckner JD. Cannabis use behaviors and social anxiety: The roles of perceived descriptive and injunctive social norms. Journal of Studies on Alcohol and Drugs. 2014;75(1):74–82. doi: 10.15288/jsad.2014.75.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder JP, Broyles SL, Brennan JJ, Zuniga De Nuncio ML, Nader PR. Acculturation, parent-child acculturation differential, and chronic disease risk factors in a Mexican-American population. Journal of Immigrant Health. 2005;7(1):1–9. doi: 10.1007/s10903-005-1385-x. [DOI] [PubMed] [Google Scholar]
- Gomez SL, Noone AM, Lichtensztajn DY, Scoppa S, Gibson JT, Liu L, … Miller BA. Cancer incidence trends among Asian American populations in the United States, 1990–2008. Journal of the National Cancer Institute. 2013;105(15):1096–1110. doi: 10.1093/jnci/djt157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoeffel E, Rastogi S, Kim M, Shahid H. The Asian population: 2010. Washington, DC: US Census Bureau, Economics and Statistics Administration; 2012. [Google Scholar]
- IOM (Institute of Medicine) Hepatitis and liver cancer: A national strategy for prevention and control of hepatitis B and C. Washington, DC: The National Academies Press; 2010. [PubMed] [Google Scholar]
- Jung MY, Holt CL, Ng D, Sim HJ, Lu X, Le D, … Lee S. The Chinese and Korean American immigrant experience: A mixed-methods examination of facilitators and barriers of colorectal cancer screening. Ethnicity & Health. 2017:1–20. doi: 10.1080/13557858.2017.1296559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juon HS, Park BJ. Effectiveness of a culturally integrated liver cancer education in improving HBV knowledge among Asian Americans. Preventive Medicine. 2013;56(1):53–58. doi: 10.1016/j.ypmed.2012.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lapinski MK, Maloney EK, Braz M, Shulman HC. Testing the effects of social norms and behavioral privacy on hand washing: A field experiment. Human Communication Research. 2013;39(1):21–46. doi: 10.1111/j.1468-2958.2012.01441.x. [DOI] [Google Scholar]
- Lee S, Chae DH, Jung MY, Chen L, Juon HS. Health examination is not a priority for less acculturated Asian Americans. Journal Racial Ethnicity Health Disparities. 2016 doi: 10.1007/s40615-016-0306-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S, Chen L, Jung MY, Baezconde-Garbanati L, Juon HS. Acculturation and cancer screening among Asian Americans: Role of health insurance and having a regular physician. Journal of Community Health. 2014;39(2):201–212. doi: 10.1007/s10900-013-9763-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma GX, Lee S, Wang M, Tan Y, Gao W, Ma X, … Toubbeh JI. The role of sociocultural factors in Hepatitis B screening among Asian Americans. Southern Medical Journal. 2011;104(7):466. doi: 10.1097/SMJ.0b013e31821f8ab0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma GX, Shive SE, Fang CY, Feng Z, Parameswaran L, Pham A, Khanh C. Knowledge, attitudes, and behaviors of hepatitis B screening and vaccination and liver cancer risks among Vietnamese Americans. Journal of Health Care for the Poor and Underserved. 2007;18(1):62–73. doi: 10.1353/hpu.2007.0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mead EL, Rimal RN, Ferrence R, Cohen JE. Understanding the sources of normative influence on behavior: The example of tobacco. Social Science & Medicine (1982) 2014;115:139–143. doi: 10.1016/j.socscimed.2014.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mereish EH, Goldbach JT, Burgess C, DiBello AM. Sexual orientation, minority stress, social norms, and substance use among racially diverse adolescents. Drug and Alcohol Dependence. 2017;178:49–56. doi: 10.1016/j.drugalcdep.2017.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mollen S, Rimal RN, Ruiter RA, Kok G. Healthy and unhealthy social norms and food selection. Findings from a Field-Experiment Appetite. 2013;65:83–89. doi: 10.1016/j.appet.2013.01.020. [DOI] [PubMed] [Google Scholar]
- Office of Minority Health. Chronic hepatitis B in Asian Americans, native hawaiians and other Pacific Islanders: Background. Washington, DC: Author; 2011. [Google Scholar]
- Padon AA, Rimal RN, Jernigan D, Siegel M, DeJong W. Tapping into motivations for drinking among youth: Normative beliefs about alcohol use among underage drinkers in the United States. Journal of Health Communication. 2016;21(10):1079–1087. doi: 10.1080/10810730.2016.1222030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen ER, Osilla KC, Miles JN, Tucker JS, Ewing BA, Shih RA, D’Amico EJ. The role of perceived injunctive alcohol norms in adolescent drinking behavior. Addictive Behaviors. 2017;67:1–7. doi: 10.1016/j.addbeh.2016.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Real K, Rimal RN. Friends talk to friends about drinking: Exploring the role of peer communication in the theory of normative social behavior. Health Communication. 2007;22(2):169–180. doi: 10.1080/10410230701454254. [DOI] [PubMed] [Google Scholar]
- Rimal RN. Modeling the relationship between descriptive norms and behaviors: A Test and Extension of the Theory of Normative Social Behavior (TNSB)*. Health Communication. 2008;23(2):103–116. doi: 10.1080/10410230801967791. [DOI] [PubMed] [Google Scholar]
- Rimal RN, Lapinski MK. A re-explication of social norms, ten years later. Communication Theory. 2015;25(4):393–409. doi: 10.1111/comt.2015.25.issue-4. [DOI] [Google Scholar]
- Rimal RN, Mollen S. The role of issue familiarity and social norms: Findings on new college students’ alcohol use intentions. Journal of Public Health Research. 2013;2(1):31–37. doi: 10.4081/jphr.2013.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rimal RN, Real K. How behaviors are influenced by perceived norms a test of the theory of normative social behavior. Communication Research. 2005;32(3):389–414. doi: 10.1177/0093650205275385. [DOI] [Google Scholar]
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA: A Cancer Journal for Clinicians. 2015;65(1):5–29. doi: 10.3322/caac.21254. [DOI] [PubMed] [Google Scholar]
- Sieverding M, Matterne U, Ciccarello L. What role do social norms play in the context of men’s cancer screening intention and behavior? Application of an extended theory of planned behavior. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association. 2010;29(1):72–81. doi: 10.1037/a0016941. [DOI] [PubMed] [Google Scholar]
- Smith-McLallen A, Fishbein M. Predictors of intentions to perform six cancer-related behaviours: Roles for injunctive and descriptive norms. Psychology, Health & Medicine. 2008;13(4):389–401. doi: 10.1080/13548500701842933. [DOI] [PubMed] [Google Scholar]
- StataCorp, L. Stata multilevel mixed-effects reference manual. College Station, TX: Stata Press; 2013. [Google Scholar]
- Strong C, Lee S, Tanaka M, Juon HS. Ethnic differences in prevalence and barriers of HBV screening and vaccination among Asian Americans. Journal of Community Health. 2012;37(5):1071–1080. doi: 10.1007/s10900-012-9541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka M, Gehan E, Chen MY, Wang JH. Hepatitis B screening practice among older Chinese in the Greater Washington, DC, area. Southern Medical Journal. 2014;107(10):655–660. doi: 10.14423/smj.0000000000000177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka M, Strong C, Lee S, Juon HS. Influence of information sources on hepatitis B screening behavior and relevant psychosocial factors among Asian immigrants. Journal of Immigrant and Minority Health/Center for Minority Public Health. 2013;15(4):779–787. doi: 10.1007/s10903-012-9753-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor VM, Jackson JC, Chan N, Kuniyuki A, Yasui Y. Hepatitis B knowledge and practices among Cambodian American women in Seattle, Washington. Journal of Community Health. 2002;27(3):151–163. doi: 10.1023/A:1015229405765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson MJ, Taylor VM, Jackson JC, Yasui Y, Kuniyuki A, Tu SP, Hislop TG. Hepatitis B knowledge and practices among Chinese American women in Seattle, Washington. Journal of Cancer Education. 2002;17(4):222–226. doi: 10.1080/08858190209528842. [DOI] [PubMed] [Google Scholar]
- Torre LA, Sauer AMG, Chen MS, Kagawa-Singer M, Jemal A, Siegel RL. Cancer statistics for Asian Americans, Native Hawaiians, and Pacific Islanders, 2016: Converging incidence in males and females. CA: A Cancer Journal for Clinicians. 2016;66(3):182–202. doi: 10.3322/caac.21335. [DOI] [PMC free article] [PubMed] [Google Scholar]