Abstract
We use an event study approach to examine the economic consequences of hospital admissions for adults in two datasets: survey data from the Health and Retirement Study, and hospitalization data linked to credit reports. For non-elderly adults with health insurance, hospital admissions increase out-of-pocket medical spending, unpaid medical bills and bankruptcy, and reduce earnings, income, access to credit and consumer borrowing. The earnings decline is substantial compared to the out-of-pocket spending increase, and is minimally insured prior to age-eligibility for Social Security Retirement Income. Relative to the insured non-elderly, the uninsured non-elderly experience much larger increases in unpaid medical bills and bankruptcy rates following a hospital admission. Hospital admissions trigger less than 5 percent of all bankruptcies.
JEL codes: I10, I13, D14
Keywords: Health insurance, consumer finance, consumption smoothing, bankruptcy
Adverse health shocks are a major source of economic risk for adults in the United States. Protection against such risk has been a major rationale for health insurance policy in the United States. For example, speaking at the signing ceremony for Medicare, President Johnson declared, “No longer will illness crush and destroy the savings that [older Americans] have so carefully put away over a lifetime.”1 More recently, the United States undertook a major expansion of both public and private health insurance coverage through the 2010 Affordable Care Act, which particularly expanded coverage for non-elderly adults. As a result, the vast majority of American adults now have health insurance. Yet we know remarkably little about their exposure to economic risk from adverse health events.
Using an event study approach, we examine the economic impacts of hospital admissions for adults in two complementary panel data sets. First, we use 20 years of the Health and Retirement Study (HRS) from 1992–2012 to analyze the impact of hospital admissions on out-of-pocket medical spending, income, and its components; our primary focus is on 2,700 adults with health insurance (hereafter “insured”) hospitalized at ages 50–59, but we also report results for insured adults hospitalized at older ages. Second, we construct a 10-year panel of credit reports (2002–2011) for adults in California with hospital admissions from 2003–2007 to analyze the impact on unpaid medical bills, bankruptcy, access to credit, and borrowing; our primary focus is on 400,000 insured, adults hospitalized at ages 25–64, but we also report results for uninsured adults ages 25–64 and for elderly adults (ages 65+ at the time of admission). In both data sets, to focus primarily on health shocks, we restrict our analysis to non-pregnancy-related admissions and to adults who have not had a prior hospital admission for several years preceding the “index” admission. In each data set, we find compelling visual evidence of sharp, on-impact effects of hospitalizations that in many cases persist - or even increase - over time.
For insured non-elderly adults, hospital admissions increase out-of-pocket medical spending, unpaid medical bills, and bankruptcy, and reduce earnings, income, access to credit, and consumer borrowing. The decline in earnings is substantial. Three years after admission, non-elderly insured adults hospitalized at ages 50–59 in the HRS have experienced an 11 percentage point (15 percent) decline in the probability of being employed, and an average annual decline in labor market earnings of $9,000 (20 percent of pre-admission earnings). By comparison, out-of-pocket medical spending increases by much less - an average annual increase of $1,400 in the three years after admission, and is relatively concentrated in the first year after admission. The earnings decline appears to be persistent, or even increasing, over time. Consistent with an increasing impact of earnings over time, we find that hospital admissions also decrease consumer borrowing in the credit report data.
Very little of the earnings decline for 50–59 year olds is insured. We find no evidence of a spousal labor supply response to the hospital admission, and we estimate that only about 10 percent of the earnings decline is insured through social insurance. In Denmark, by contrast, non-fatal health shocks to households under 60 produce comparable (15–20 percent) declines in earnings, but almost 50 percent of the earnings decline is insured through various insurance programs, particularly sick pay and disability insurance (Fadlon and Nielsen 2015).
Substantial insurance for earnings losses due to health shocks does not exist in the U.S. until individuals become age-eligible for Social Security. We find that 60–64 year old insured adults in the U.S. experience similar declines in earnings and employment following a hospital admission as 50–59 year olds, but that for 60–64 year olds, a much larger share of this decline (over 60 percent) is insured, primarily through Social Security Retirement Income. At even older ages, earnings declines from hospital admissions become minimal or non-existent, presumably reflecting the much lower rates of labor force participation.
These results could look very different for adults without health insurance (hereafter, “uninsured”). Our analysis of the uninsured is limited to the credit report data due to insufficient sample size in the HRS. In fact, we find similar impacts of hospital admissions for insured and uninsured adults ages 25–64 on borrowing (about a 10 percent decline over four years) and borrowing limits (about a 5 percent decline). The decline in borrowing for the uninsured suggests that their increase in out-of-pocket spending is small relative to the decline in income they experience.
However, we find much larger impacts of hospital admissions on unpaid bills for the uninsured than the insured: Four years post-admission, a hospital admission is associated with an increase in unpaid bills of about $6,000 for the uninsured, compared to $300 for the insured. Complementary results from a regression discontinuity (RD) analysis at age 65 provide some supportive evidence for interpreting the comparative impacts of hospital admissions as approximating the causal impact of insurance. These findings add to a growing body of evidence suggesting that the nominally “uninsured” in fact have substantial “implicit insurance” and that, as a result, much of the economic benefits from insurance may accrue to external parties who bear the economic incidence of unpaid medical bills (Garthwaite, Gross, and Notowidigdo forthcoming; Finkelstein, Hendren, and Luttmer 2015; Mahoney 2015).
Our results also speak to the extent and nature of insurance coverage for the economic consequences of hospital admissions in the US. Those with health insurance have coverage for a large share of the medical expenses that hospital admissions incur, but they have considerably less coverage for the labor market consequences of the hospital admission until they reach the age eligibility for Social Security. A back-of-the-envelope calculation for 50–59 year olds with health insurance suggests that in the first year, over 90 percent of the total medical expenses associated with a hospital admission are covered, but only about 80 percent of the total economic consequences (medical expenses plus earnings declines) are covered. Over time the share of total economic costs covered declines further, since the subsequent labor market consequences loom larger than the continued medical expenses; in the third year after admission, for example, our estimates suggest that for the insured ages 50–59, only about 50 percent of the total economic consequences of the hospital admission are covered.
Of course, the welfare implications of uninsured earnings and uninsured medical spending may differ. If the medical spending associated with a hospital admission is taken as exogenous, but changes in earnings reflect a labor supply response to reduced productivity or increased disutility of labor, a given change in earnings will have less of an impact on utility than the same change in out of pocket spending; nonetheless, our calculation from a simple, stylized model suggests that the welfare consequences of the uninsured earnings decline for adults with health insurance is at least three times that of the out-of-pocket medical spending increase.
The welfare consequences of the declines in consumption that likely follow decreased earnings or increased out of pocket medical spending are not obvious. Some decline in consumption will be optimal if, as the literature has suggested, the marginal utility of consumption is lower in poor health (Viscusi and Evans 1990; Finkelstein, Luttmer, and Notowidigdo 2009; Finkelstein, Luttmer, and Notowidigdo 2013). Additionally, in the presence of moral hazard effects of insurance, the (constrained) optimal level of insurance would not fully equate the marginal utility of consumption across health states (Pauly 1968; Baily 1978).
Naturally, we are not the first to consider the economic consequences of health shocks in the United States. Cochrane’s (1991) classic study used panel survey data on food consumption from the Panel Study of Income Dynamics (PSID) to examine the covariance of food consumption changes and various shocks, concluding that individuals are imperfectly insured against illness. A subsequent literature has used the PSID to study the correlation between changes in self-reported health or disability and changes in earnings and (food) consumption (e.g., Charles 2003; Chung 2013; Meyer and Mok 2013), and has used the HRS to study the correlation between the onset of self-reported health problems and changes in out-of- pocket medical spending, income, assets, retirement, and disability (e.g., Cutler, Meara, and Richards-Shubik 2011; Poterba, Venti, and Wise 2017; Smith 2005; Smith 1999). Our analysis in the HRS is similar in spirit to this prior work; it complements it by focusing on the relatively sharp event of a hospital admission rather than changes in self-reported health conditions. This helps us to separate the impact of the health event on economic outcomes from other potential secular trends and from the potential endogeneity of reported health to economic circumstances.
Our analysis of the linked hospital discharge and credit report literature adds to a comparatively smaller existing literature that uses rich administrative data and the sharp timing of health events to study the economic consequences of adverse health events in the United States. Morrison et al. (2013) and Gupta et al. (2014) use an event-study type approach to examine the impact of non-fatal automobile accidents in Utah and cancer diagnoses in Western Washington, respectively, on bankruptcy; they are unable to reject the null hypothesis of no effect. In follow-on work, Gupta et al. (2015) also examine the differential impact of cancer diagnoses on bankruptcy and foreclosures across individuals with (cross-sectionally) different pre-diagnosis access to liquidity.
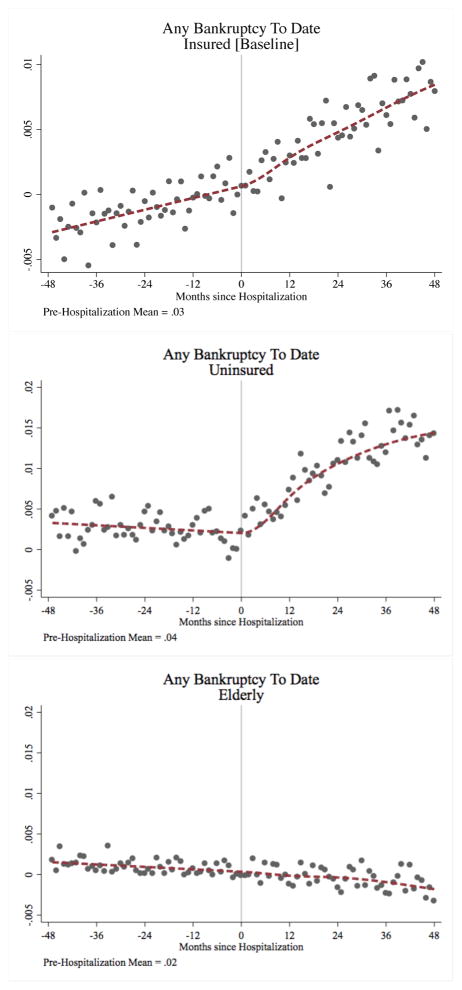
In the last section of our paper, we consider the impact of hospital admissions on bankruptcy. We find that a hospital admission is associated with an increase in probability of bankruptcy of 1.4 percentage points for the uninsured non-elderly (ages 25–64), compared to 0.4 percentage points for the insured non-elderly (ages 25–64). We find no economically or statistically significant increase in bankruptcies for the elderly (ages 65 plus). Our estimates imply that hospital admissions are responsible for about 4 percent of bankruptcies for insured, non-elderly adults, and about 6 percent of bankruptcies for uninsured, non-elderly adults, and have no effect on bankruptcies for adults aged 65 and over. These findings speak directly to the controversial, high-profile literature on “medical bankruptcies”, where prior studies have claimed that medical events can explain 20 to 60 percent of all consumer bankruptcies (Hummelstown et al. 2005, 2009; Drano and Millen son 2006).
The rest of the paper proceeds as follows. Section 1 provides a simple conceptual framework in which health shocks can generate both uninsured medical expenses and reductions in wages, and discusses potential impacts on out-of-pocket medical costs, earnings, and credit report outcomes in this setting. Section 2 provides an overview of our data and empirical framework. Section 3 presents our results from the HRS on the impact of hospital admissions on out of pocket medical expenses, earnings and income. Section 4 presents our results of the impact of hospital admissions on credit report outcomes. Section 5 discusses some implications of the findings. The last section concludes.
1 Economic framework
We develop a simple economic framework in which health shocks may generate both increases in out-of-pocket medical expenses and reductions in earnings; we will analyze these impacts using data from the HRS on out-of-pocket medical spending, earnings, and income. We also use the framework to help interpret the impact of health shocks on the various financial outcomes we will analyze in credit report data: borrowing, borrowing limits, unpaid medical bills, and borrowing costs.
1.1 Model setup
An individual lives for two periods. At the start of period 1, she faces an adverse health event with probability p; in what follows, we superscript outcomes in the state of the world in which the adverse health event has occurred with an S (for sick state), and we use H (healthy state) as superscript when the adverse health event has not occurred. After observing the period 1 health shock, she chooses her labor supply (ht) in each period and her consumption path (ct) subject to her lifetime budget constraint in order to maximize her state-specific utility.
Utility UJ in health state J ∈ {H, S} is given by
where δ is the discount rate. The per-period utility function is defined as
with g() a concave utility function over consumption (ct) and f() a convex disutility function over hours worked (ht).
The health event generates exogenous medical expenses m and exogenously reduces the wage in each period from w1 and w2 to (1 − α1)w1 and (1 − α2)w2, with 0 < αt < 1.2 Of course, in principle the individual can choose how much health care to consume following a health shock (and we discuss this briefly in Section 5.2 below); nonetheless, the assumption of exogenous medical expenses seems a reasonable approximation in our empirical setting of hospital admissions. We assume that the total shock is bounded above by total income when healthy; i.e., , which is a sufficient condition to ensure that the individual can choose positive consumption in both periods. Health insurance covers a share λm ∈ [0, 1] of medical costs m and replaces a share λα ∈ [0, 1] of the reduction in wages in each period. A (weakly positive) insurance premium π is paid in every period and in every health state.
After observing the health shock and the amount of insurance, the individual chooses: (1) hours of work in each period (h1 and h2), (2) borrowing or savings in period 1 (b) at the interest rate r(u, b), and (3) what amount of uninsured medical expenses (1 − λm)m to pay, with the remainder u ≤ (1 − λm)m as unpaid medical bills.
The cost of borrowing r(u, b) is strictly increasing in borrowing (b) and in unpaid bills (u). Borrowing is also limited by a maximum borrowing limit L. We model L as an increasing function of the present discounted value of maximum total income Y. Specifically, we assume
with 0 < γ ≤ 1 and Y ≡ w1H̄ +w2H̄/(1+r), where H̄ is the maximum hours an individual can work each period. The parameter γ is a reduced-form representation of the supply side of the credit market, which may not let individuals borrow all the way up to their “natural borrowing limit” (e.g., Ljungqvist and Sargent 2004).
Finally, it is useful to define total income in each state:
The individual chooses , bJ, and u to maximize utility subject to the state-specific budget constraints. These choices are associated with the following consumption choices in each health state and time period:
| (1) |
We also impose some additional technical conditions which we discuss in more detail in Appendix A. These conditions ensure interior solutions for b and u.
1.2 Impact of health shocks
We use Δ to compare outcomes when sick to outcomes when healthy (e.g., Δb = bS − bH, , ΔU = US − UH). We consider the impact of a health shock that is not “fully covered”, by which we mean one with m > 0, α1 > 0, α2 > 0, λm < 1, and λα < 1. These conditions imply that .3
Proposition 1
A health shock that is not fully covered generates Δc1 < 0, Δc2 < 0, ΔU < 0, and Δu > 0; the signs of Δb, Δr, ΔL, Δy1, and Δy2 are ambiguous, but Δb ≠= 0 and/or Δr ≠= 0 and/or ΔL ≠= 0 and/or Δy1 ≠= 0 and/or Δy2 ≠= 0 reject full coverage.
Proof
See Appendix A.
Proposition 1 says that individuals who experience a health shock that is not fully covered will experience a decline in utility and consumption when sick; this is an intuitive result based on objects we do not directly observe. More usefully, Proposition 1 says that we can reject the null of full coverage through changes in outcomes we can observe or proxy for: income (y1 and y2), credit limits (L), borrowing (b), unpaid medical bills (u), and interest rates (r). A change in any of these outcomes following a health shock implies a rejection of full coverage because with full coverage (λm = λα = 1), health shocks do not change either the level or time profile of wages or lifetime resources, and hence do not change labor supply choices, income, borrowing behavior, borrowing costs, or unpaid bills.
Without full coverage, unpaid bills increase; they are (mechanically) zero when healthy and will be strictly positive when sick by the envelope theorem. While interest rates are increasing in u, the effect on interest rates is ambiguous because Δb is ambiguous and r depends on both u and b. The change in borrowing limits (ΔL) is also ambiguous because Δr is ambiguous.
More interestingly, Proposition 1 says that the sign of the impact of a health shock on borrowing and on earnings is a priori ambiguous. The intuition for why Δb could be of either sign without full coverage is more easily seen in an alternative simplified setting in which individuals cannot forgo paying medical bills (i.e., u = 0), interest rates are exogenously fixed at the discount rate (r = δ), there are no insurance premiums (π = 0), and the borrowing limit is equal to available income (γ = 1). In this simplified case, solving the agent’s optimization problem yields the following closed-form expression for the change in borrowing (see Appendix A for derivation):
| (2) |
Equation (2) shows that the sign of Δb depends on the importance of the uninsured medical cost shock, (1−λm)m compared to the relative income change, (Δy2−Δy1). Increases in out-of-pocket medical spending tend to increase borrowing, while declines in future income tend to decrease borrowing. Thus borrowing is more likely to decline following a health shock when uninsured wage shocks are more important relative to uninsured medical cost shocks, and when the resultant income decline grows over time. Indeed, if the health event only creates an uninsured medical cost shock (i.e., m > 0, λm < 1, and α1 = α2 = 0 ), this will increase borrowing (Δb > 0) because the individual will borrow from the future to smooth consumption across the two periods when faced with uninsured medical expenses in period 1. For borrowing to decline following a health shock, the income decline needs to be larger in later relative to earlier periods, so that the individual now wants to move consumption to later periods. Evidence of the impact of the health shock on borrowing will therefore complement our direct estimates of the impact of the health shock on out-of-pocket medical spending and income.
The intuition behind the ambiguous sign of Δy1 and Δy2 is similar. The health shock is both a negative shock to unearned income (uninsured medical expenses) and a negative shock to the wage in each period. If the health shock is primarily a medical expenses shock, then the negative wealth effect will tend to increase hours and (if wages don’t change by very much) this will increase total labor income. Alternatively, if out-of-pocket medical expenses are small and wages are reduced by a lot, then this will decrease total labor income, although hours can either increase or decrease depending on the relative importance of income and substitution effects in labor supply in response to a health shock. We describe this trade-off more formally in Appendix A.
2 Data and Empirical Framework
2.1 Data
We analyze the impact of hospital admissions as the empirical analog of the “adverse health shock” in the model. We focus on hospital admissions because they are large expenses, relatively common, measurable, and likely unanticipated (although in recognition of the fact that not all hospital admissions are unanticipated, we report robustness results in which we limit to subsets of hospital admissions that are more likely to be unanticipated). Naturally they are a subset of health shocks - for example an unexpected cancer diagnosis based on outpatient screening could generate substantial spending without necessarily generating an inpatient hospital admission - and discrete health shocks are themselves only a subset of adverse health events, which include the slow onset and worsening of chronic conditions. We return to this in Section 5.4 when we calibrate the implications of our findings for the likely total magnitude of “medical bankruptcies.”
Our analysis uses two complementary data sets to analyze many of the outcomes in Proposition 1. We analyze 11 bi-annual survey waves from 1992 through 2012 of the Health and Retirement Study (HRS), a nationally representative panel survey of the elderly and near-elderly in the United States. We also analyze a sample of individuals discharged from hospitals in California between 2003 and 2007 whom we linked to their January credit reports for 2002–2011; we also link these individuals to information on all of their California hospitalizations between 2000 and 2010 and to mortality data (both in and out of hospital) from California vital statistics through 2010.4 For confidentiality reasons, all of the analyses using California discharge data were conducted on a non-networked computer in the Sacramento office of California’s Office of Statewide Health Planning and Development (OSHPD).
We provide a brief overview of the sample definition and key variables here. Appendix B provides considerably more detail.
2.1.1 Analysis samples
In both data sets, to try to focus on health “shocks” we restrict attention to non-pregnancy related hospital admissions for individuals who have not had a recent hospital admission. In the HRS, we identify the survey wave in which the individual first reports having had a hospital admission over the last two years (hereafter, the “index” admission), and require that we observe the individual in the previous bi-annual interview without reporting an admission over the last two years; the index hospital admission, therefore, on average represents the first hospital admission in at least 3 years. In the California discharge data, we restrict attention to individuals who have not had a prior hospital admission in the three years preceding their index admission, and exclude pregnancy-related admissions from the analysis.
Our primary focus is on non-elderly adults with health insurance who had a hospital admission. In the HRS, individuals from our non-elderly sample are 50–59 at admission; in the credit report analysis they are 25–64 at admission. We define an individual in the HRS as “insured” if he reports having private insurance or Medicaid in the interview prior to the one where he reports the index admission. In the California discharge data, we define an individual as “insured” if his primary payer for the index admission is private insurance or Medicaid. In both data sets, we exclude the approximately 15 percent of non-elderly adults on Medicare because such individuals are disabled and therefore presumably have already had an “adverse health event”. Our baseline sample consists of approximately 2,700 insured adults ages 50–59 at the time of hospitalization in the HRS and 380,000 insured adults ages 25–64 at the time of hospitalization in the credit report data. Throughout we refer to these two groups as “non-elderly, insured.”
We supplement our primary analysis with additional populations that provide informative contrasts. In the HRS, we report a parallel set of analyses for approximately 1,600 non-elderly adults with health insurance aged 60–64 at the time of admission; unlike our primary sample, these individuals are age-eligible for Social Security Retirement Income during the 3 years post admissions that we focus on. In both data sets, we report a parallel set of analyses for the elderly (65 and older), analyzing about 5,800 individuals in the HRS and about 400,000 in the credit report data. Finally, in the credit report data we analyze about 150,000 uninsured non-elderly adults with a hospitalization; these are individuals ages 25–64 at admission whose “expected source of payment” is “self-pay”. There is insufficient sample size for analysis of uninsured non-elderly adults in the HRS.
Summary statistics
Table 1 presents some basic summary statistics for our primary analysis samples in the HRS and the credit report data; Appendix Tables 4, 13, and 14 provide additional detail on how sample characteristics are affected by our sample exclusions, as well as summary statistics for the additional populations analyzed. Naturally, the average age at admission for the non-elderly insured is higher in the HRS sample in column 1 (56) than in the credit report sample in column 2 (49). Importantly for interpreting the empirical findings, insurance status is persistent post-admission for the non-elderly insured.
Table 1.
Sample Characteristics for the Non-Elderly Insured
| Data Source | HRS | Credit Report Sample |
|---|---|---|
| Age Range | Ages 50 to 59 | Ages 25 to 64 |
| (1) | (2) | |
| Panel A: Demographics | ||
| Age at admission | 55.6 | 48.5 |
| Male | 47.6 | 45.1 |
| Year of admission | 2002.3 | 2005.0 |
| Has spouse in survey wave preceding hospitalization | 77.2 | n/a |
| Panel B: Race/Ethnicity | ||
| Hispanica | 5.0 | 18.0 |
| Black | 9.7 | 7.9 |
| White | 85.2 | 63.0 |
| Other Race | 5.0 | 11.0 |
|
| ||
| Panel C: Index Hospitalization | ||
| Length of Stay (days) | n/a | 4.1 |
| Hospital List Charges ($)b | n/a | 45,580 |
| n/a | (189,598) | |
| Medicaid | 5.9 | 13.7 |
| Private | 94.1 | 86.3 |
| Hospital Non Profit | n/a | 74.4 |
| Hospital For Profit | n/a | 16.3 |
| Hospital Public | n/a | 9.4 |
| Admitted through Emergency Department | n/a | 47.9 |
|
| ||
| Panel D: Subsequent Outcomes c | ||
| Re-Admitted to Hospital Within 12 Months | 23.7 | 20.4 |
| Re-Admitted to Hospital Within 48/36 Months | 36.7 | 36.0 |
| Died within 12 Months | 0 | 3.2 |
| Died within 48 Months | n/a | 6.3 |
| Insured within 12 Monthsd | 92.7 | 97.6 |
| Insured within 48/36 Monthsd | 91.8 | 96.6 |
| Individuals | 2,732 | 378,190 |
Notes: Age is defined at admission; non-elderly are 50–59 in HRS and 25–64 in credit reports. Insurance status is defined at the index admission for the credit report sample and in the survey wave preceding the wave which reports the index admission for the HRS sample. “Insured” denotes coverage by Medicaid or private insurance. All proportions are multiplied by 100 and the analysis is weighted to adjust for oversampling of some groups for the credit report sample and using survey weights for the HRS sample. All hospitalizations that are pregnancy related (MDC = 14) have been dropped from the credit report sample. All means are listed in percents unless otherwise noted, except for age and year of admission.
In the credit report sample, black, white, other race, and Hispanic are mutually exclusive; in the HRS, “Hispanic” is asked separately from race.
Charges are summed and insurance type is averaged (weighted by length of stay) for people that have a single hospitalization spread across more than one unit in a hospital or more than one hospital. The standard deviation is in parentheses.
In the HRS, survey waves are two years apart so we assume the index hospital admission occurs one year prior to its report. Subsequent outcomes 12 months later are therefore measured based on the survey wave reporting the index hospital admission and for 36 months later we use the survey wave subsequent to the one that reports the index admission. In the credit report data we measure outcomes 12 and 48 months later. In the HRS, mortality is mechanically zero 12 months post admission, and thus the sample conditions on survival to the next survey.
Subsequent insurance status for the credit report sample is defined only if they are re-admitted to the hospital.
We gain additional insight into the nature of the hospital admissions for insured non-elderly adults through the California discharge data linked to the credit report sample in column (2). We see that 85 percent of admissions are privately insured, three-quarters are admitted to a non-profit hospital, and about half are admitted through the Emergency Department. The two most common reasons for the index admission (each of which are about 15 percent of admissions) are circulatory system and musculoskeletal conditions (see Appendix Table 14). The index hospital admission lasts an average of 4 days and incurs about $46,000 in list charges (which are notoriously higher than actual payments and thought to be significantly higher than actual costs). The index admission is also associated with subsequent additional health care utilization: one-fifth are re-admitted to the hospital within 12 months and 36 percent are re-admitted within 48 months (see Appendix Table 13). There are also likely associated non-hospital medical expenses. Our estimates from the Medical Expenditure Panel Survey (MEPS) suggest total medical payments in the 12 months post admission of about $19,000, of which $11,000 reflect the index admission, $3,200 reflect non-inpatient medical expenses, and the remainder reflect payments from re-admissions; see Appendix B.3 (and Appendix Table 37) for more details.
2.1.2 Key outcomes
We use the HRS to analyze the impact of a hospital admission on out-of-pocket medical spending ((1 − λm)m − u), earnings (wtht), income (yt), and several potential sources of earnings insurance (λα), specifically spousal earnings and social insurance programs (unemployment insurance and various Social Security programs).5 All outcomes are derived from self-reports. We use the CPI to adjust all dollar amounts to 2005 levels (the midpoint of the credit report data) and censor all outcomes at the 99.95th percentile.
We use the credit report data to analyze the remaining key outcomes in the model: unpaid medical bills (u), borrowing (b), borrowing limits (L), and borrowing costs (r). All of these measures are stocks, and are at the individual, rather than household, level.6 Once again, we censor all the continuous outcomes at the 99.95th percentile to purge the data of extreme outliers.
Our main measures of unpaid bills (u) come from collections - unpaid bills that have been sent to collection agencies for recovery attempts. We analyze both the “number of collections to date” (starting from 2002) and current unpaid collection balances. We are able to observe medical and non-medical collection balances separately starting in 2005. We also analyze consumer bankruptcy - specifically, whether the individual has filed for consumer bankruptcy at any point back to 2002; this may be viewed as an extreme form of unpaid bills.7
We analyze two measures of borrowing (b). Our primary measure (“credit card balances”) is total revolving account balances, summed over all open revolving credit accounts the individual may have. We focus on revolving credit because we suspect it corresponds most closely to the function of b in the model; that is, the source of the marginal dollar borrowed in response to a health event. We also analyze balances for automobile installment loans, which are another major source of loans and may also be a proxy for motor vehicle consumption (e.g., Agarwal et al. 2015b).
Finally, we analyze two components of “access to credit”: borrowing limits (L), and interest rates (r). We proxy for total borrowing limits (L) based on the individual’s total credit limit across all open revolving accounts. We use the individual’s credit score to proxy for the interest rate (r) faced by individuals. Credit scores are well-known determinants of individual borrowing costs (e.g., Einav, Jenkins, and Levin 2013a; Agarwal et al. 2015a; Han, Keys, and Li 2015), with higher credit scores corresponding to lower r. We analyze the VantageScore 2.0 credit scores, which range from a worst possible score of 501 to a best possible score of 990.
2.2 Econometric models
We estimate both non-parametric and parametric event study models. The details naturally differ slightly across the two data sets. In particular, in the HRS we analyze bi-annual survey data while in the credit report data we analyze the annual outcome data in terms of months relative to admission. At a broad level, however, they are quite similar.
2.2.1 Non-parametric event study
We analyze the coefficients on various indicator variables for time relative to the event (“relative time”). The primary advantage of this non-parametric event study is that it allows us to visually (and flexibly) assess the pattern of outcomes relative to the date of hospitalization. The basic non-parametric event study specification takes the form
| (3) |
where γt are coefficients on calendar time fixed effects, Xit represents a vector of other potential control variables, and μr are coefficients on indicators for time relative to the hospital admission. All analyses allow for an arbitrary variance-covariance matrix at the individual level and include the relevant sample weights. The key coefficients of interest are the pattern on the μr’s which estimate the outcome at a given r relative to the omitted category μ−1.
HRS specification
In the bi-annual HRS data, event time r refers to the survey wave relative to the survey wave in which the index hospital admission is reported to have occurred in the last two years (r = 0). The r = 0 interview therefore occurs, on average, one year after the index admission. We analyze up to three waves prior to the index admission (S = −3) and three waves after the index admission (F = 3); the omitted category (μ−1) reflects an interview conducted, on average, one year prior to the index admission. Our baseline specification includes bi-annual survey wave indicators that control for calendar time (γt) and, as additional covariates (Xit), a series of “HRS cohort”-by-wave dummies, because of the changes in sample composition over time as the HRS added additional birth cohorts for study (see Appendix B.1.1 for details). In the robustness analysis we also show results with individual fixed effects.
Credit report specification
In the annual credit report data, we observe each individual’s credit report outcomes in January of each year. However, because individuals are admitted to the hospital in different months within the year, we can define event time r as the number of months relative to the hospital admission (which occurs at r = 0). Our baseline specification limits the sample to relative months −47 (S = −47) through 72 (F = 72). The omitted category (μ−1) is the month prior to hospitalization. The γt are coefficients on calendar year fixed effects, and there are no additional covariates (Xit) in the the baseline specification. Because this is a slightly non-standard setup (involving monthly analysis of annual data) we discuss the specification and identification of the parameters in more detail in Appendix D; we also describe there the additional normalizations required when we include individual fixed effects in some of the robustness analysis.
Interpretation
To interpret the non-parametric event study coefficients on indicators for time after the hospital admission in equation (3) as the causal effect of the admission would require the identifying assumption that, conditional on having a hospital admission during our observation window and the included controls, the timing of the admission is uncorrelated with the outcome. Among other things, an admission that is preceded by deteriorating health, or an admission caused by the adverse health effects of job loss would violate this assumption.
A priori, there is reason to be concerned about such threats. For example, there is evidence that job loss can produce adverse health outcomes (e.g., Sullivan and von Wachter 2009; Black, Devereux, and Salvanes 2015), suggesting a potential confounding interpretation. Likewise, it seems plausible that some hospital admissions are not completely unanticipated; for example, Nielsen (2016) shows in Danish data that deteriorations in self-reported health can predict future hospital admissions. Our restriction to individuals experiencing their first hospitalization in the last three years is designed to reduce - but cannot eliminate - the chance that individuals are on a downward trend prior to the hospitalization.
The non-parametric event study in equation (3) allows us to examine patterns in outcomes in the months leading up to the hospitalization. Not surprisingly, given the types of concerns we suggested, there is sometimes evidence of secular trends in outcomes prior to the hospital admission. The relatively sharp timing of the event and high frequency measurement of outcomes (particularly in the credit report data) allow us to visually and informally assess whether outcomes appear to change sharply around the event. It also guides our formulation of the parametric event studies that deliver our main estimates.
2.2.2 Parametric event study
We use the parametric event study to summarize the magnitude of estimated effects and their statistical significance. Our choice of functional form is guided by the patterns seen in the non-parametric event studies. In the figures below, we superimpose the estimated parametric event study on the non-parametric event study coefficients which allows for a visual assessment of our parametric assumptions.
HRS specification
In the HRS, our baseline specification is:
| (4) |
Equation 4 allows for a linear pre-trend in event time r (i.e., between bi-annual waves of the HRS). The key coefficients of interest, the ’s, show the change in outcome following an index admission relative to any pre-existing linear trend (δ). As before, we include “HRS cohort”-by-wave dummies as additional covariates (in Xit).
Credit report specification
In the higher-frequency credit report data, we again allow for a linear pre-trend in event time r (now months relative to admission), and we now impose a a cubic spline in post-admission event time:
| (5) |
Equation (5) allows for the second and third derivative of the relationship between outcome and event time to change after the event (r > 0), and for the third derivative to change further 12 months after the event (r > 12) and 24 months after the event (r > 24). The key coefficients of interest - β2 through β5 - allow us to summarize the change in outcome following an index admission relative to any pre-existing linear trend (β1).
Interpretation
The parametric event studies in equations (4) and (5) allow for a linear trend in event time. The choice of the linear trend was motivated by the results from the non-parametric event studies which, as we will see in the results below, suggest that a linear trend captures any secular trends quite well. For the parametric event study, the identifying assumption is that, conditional on having a hospital admission and the included controls, the timing of the admission is uncorrelated with deviations of the outcome from a linear trend in event time. This assumption still requires that there are no factors correlated with yit that, conditional on the included controls, occur contemporaneously with the hospital admission - such as a job loss that simultaneously produces a hospital admission.
3 Impacts on Out-of-Pocket Medical Expenses and Income
3.1 Main Results
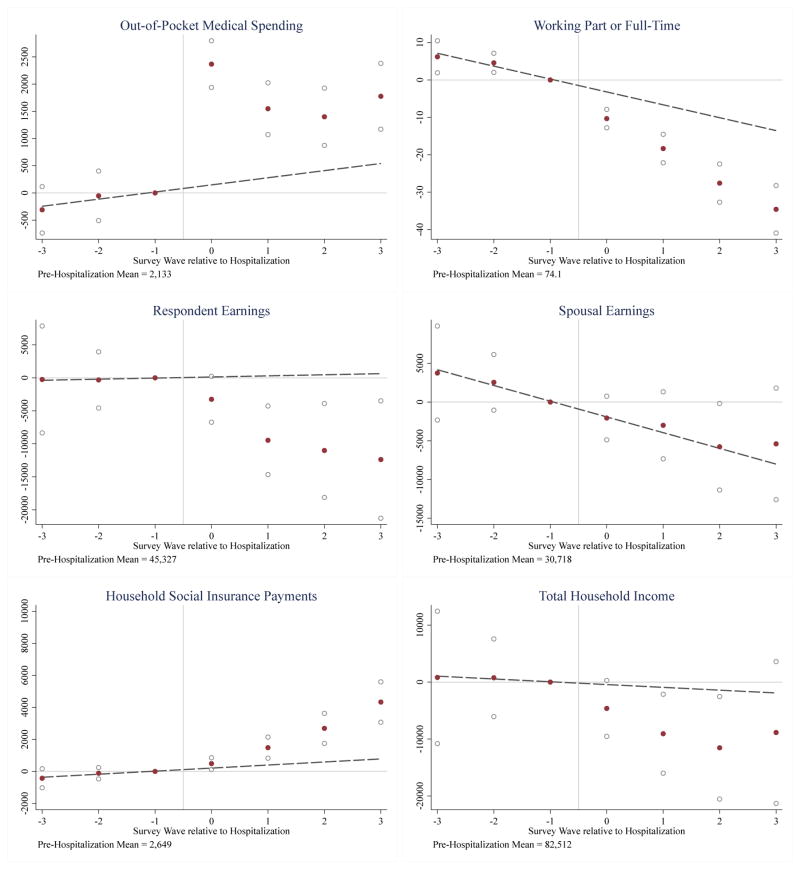
Figure 1 shows the impact of hospital admissions for insured non-elderly adults ages 50–59 at admission on out-of-pocket spending, employment, earnings, spousal earnings, government transfers, and total household income in the HRS. For each outcome, we plot the estimated coefficients on event time (μr’s) from the non-parametric event study regression (equation (3)), and the estimated pre-admission linear relationship between outcome and event time (δ) from the parametric event study regression (equation (4)). Recall that survey waves are two years apart and that, on average, the hospital admission occurs one year prior to the “wave 0” interview. Out-of-pocket spending is reported for the last two years, employment (defined as “working part- or full-time”) is reported as of the time of interview, and earnings, government transfers, and income are reported for the calendar year prior to the interview.
Figure 1.
Impact of Hospitalization for the Non-Elderly Insured (Ages 50 to 59) in the HRS
Notes: The sample is the non-elderly insured (see Table 1, column 1). The points in each figure represent the estimated effects of event time (i.e. the μr’s from the non-parametric event study in equation 3), with the survey wave reporting the hospitalization normalized to zero. Survey waves are biannual; we assume the hospitalization occurs halfway between survey waves (12 months prior to survey wave zero) on average. The hollow circles present the 95% confidence intervals. The dashed line represents the estimated pre-admission linear relationship between outcome and event time from the parametric event study in equation 4 with the level normalized to match the non-parametric estimates. All estimates are weighted using survey weights.
Because of the survey design, it is not straightforward to read the time pattern of the impact of hospital admissions directly off of the event study coefficients in Figure 1. Roughly speaking, to make comparisons of the non-parametric estimates at different post-admission years, the estimates in the survey wave reporting the hospital admission (wave 0) should be doubled. We calculate implied effects at different time periods post-admission more formally based on the parametric event study coefficients (shown in Appendix Table 6). Table 2 summarizes the implied annual effects at one and three years after admission, and the implied average annual effect three years post admission; the formulas for translating the parametric event study coefficients into these implied effects are derived and described in Appendix C.
Table 2.
Impact of Hospitalization on the Non-Elderly Insured (Ages 50 to 59) in the HRS
| Out-of-Pocket Medical Spending | Working Part or Full-Time | Respondent Earnings | Spousal Earnings | Household Social Insurance Payments | Total Household Incomeb | |
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| 12-month effecta | 3,275 | −8.88 | −6,445 | −444 | 503 | −8,443 |
| (373) | (1.83) | (4,024) | (3,851) | (379) | (6,857) | |
| [<.001] | [<.001] | [0.11] | [0.91] | [0.18] | [0.22] | |
| Effect at 36 monthsa | 1,011 | −11.1 | −11,071 | 1,588 | 1,261 | −7,890 |
| (371) | (2.31) | (3,475) | (3,110) | (411) | (5,527) | |
| [0.0065] | [<.001] | [0.0014] | [0.61] | [0.0022] | [0.15] | |
| Average annual effect over 36 monthsa | 1,429 | −9.99 | −8,753 | 572 | 881 | −8,161 |
| (202) | (1.85) | (3,415) | (3,114) | (338) | (5,709) | |
| [<.001] | [<.001] | [0.01] | [0.85] | [0.009] | [0.15] | |
| Pre-hospitalization mean | 2,133 | 74.1 | 45,327 | 30,718 | 2,649 | 82,512 |
| Number of Individuals | 2,732 | 2,732 | 2,732 | 2,732 | 2,732 | 2,732 |
| Number of Observations | 13,286 | 13,286 | 13,286 | 13,286 | 13,286 | 13,286 |
Notes: Sample is the non-elderly insured (see Table 1, column 1) in the HRS. All columns report effects based on OLS estimates of equation (4). Pre-hospitalization means are calculated using the survey wave preceding the hospitalization. Standard errors (clustered on the individual) are in parentheses and p-values are in brackets. All estimates are weighted using survey weights.
All reported effects are reweighted to correct for timing features of the HRS survey, assuming a uniform distribution of hospitalizations in the two years between survey waves and a piecewise linear spline functional form with knots at 12 and 36 months, using the true distribution of month of the survey within the year, and adjusting for the reporting window. All outcomes are reported for the past calendar year except for out-of-pocket medical spending which covers the two-years since the last interview and working part or full-time which is asked at the time of the interview. See Appendix C for methodological details.
Total household income is the sum of respondent earnings, spousal earnings, household social insurance payments, and household pension income.
Out-of-pocket spending, employment and earnings
The impact of hospital admissions on out-of-pocket spending and earnings is visually apparent “immediately” (i.e., at wave 0, approximately one year after the hospital admission), and persists in subsequent years. The figures suggest that a linear trend fits the pre-hospital admission trend remarkably well, presumably reflecting the fact that adverse health is one of the main forms of idiosyncratic variation in medical expenses and labor market activity for insured adults age 50–59.
A hospital admission increases average annual out of pocket spending by $1,429 (standard error = $202) in the three years after admission. Not surprisingly, the impact on out-of-pocket spending is higher in the first year. Indeed, the impact on out of pocket spending in the first year after admission ($3,275, standard error = $373) is over three times the impact in the third year after admission ($1,011, standard error = $371). The fact that the hospital admission continues to have a statistically significant (albeit substantially smaller) impact on out-of-pocket spending in subsequent years likely reflects the fact that, as discussed above, the index hospital admission is associated with increased future medical expenses.
A hospital admission reduces the probability of being employed by 8.9 percentage points (standard error =1.8) in the first year after the admission, and by 11.1 (standard error = 2.3) percentage points in the third year after admission. This represents a 12 to 15 percent decline in employment relative to the pre-admission mean. The point estimates suggest that the decline in annual earnings associated with hospital admissions grows over time, from $6,445 (standard error = $4,024) in the first year after admission, to $11,071 (standard error = $3,475) in the third year after admission. On average, over the three years after the admission, annual earnings decline by $8,753 (standard error = $3,415); this represents a decline in earnings of about 20 percent relative to the pre-admission average.8 If the reduction in employment on the extensive margin were drawn evenly from the pre-hospitalization earnings distribution, about 85 percent of the first year decline in earnings and 60 percent of the third year decline in earnings would be accounted for by the reductions in employment.
Appendix Table 10 and Appendix Figure 9 provide more detail on the components of the earnings decline. A hospital admission decreases annual hours by 228 (standard error = 54) in the third year after admission, or about 14 percent relative to the pre-admission average.9 The decline in employment (“working part- or full-time”) represents primarily an exit from full-time work, with little or no net impact on working part-time, being unemployed disabled, or not in labor force. Much or all of the reduction in full-time work represents transition to retirement; self-reported retirement increases by 10 percentage points (standard error = 1.8) by the third year post-admission. Consistent with the declines in labor force activity reflecting the consequences of a hospital admission, in the first year post-admission, hospital admissions are associated with a 9.5 percentage point (standard error = 2.1) increase in the portion of people who report that their ability to work for pay is limited by health.
Earnings insurance
We consider both informal earnings insurance through spousal labor supply and formal insurance through social insurance programs. There is no statistical or substantive evidence of a response of spousal earnings.10 There is evidence of an increase in average annual social insurance payments to the household of $881 (standard error = $338) over the three years after the admission. In other words, about 10 percent of the average annual earnings decline is insured through social insurance; we suspect this primarily reflects Social Security Disability Insurance Payments.11 On average, three years after the admission, total annual household income has fallen by $8,161 (standard error $5,709); these results, while statistically imprecise, are consistent with the estimates of earnings decline and offsetting social insurance payments.12
Heterogeneity
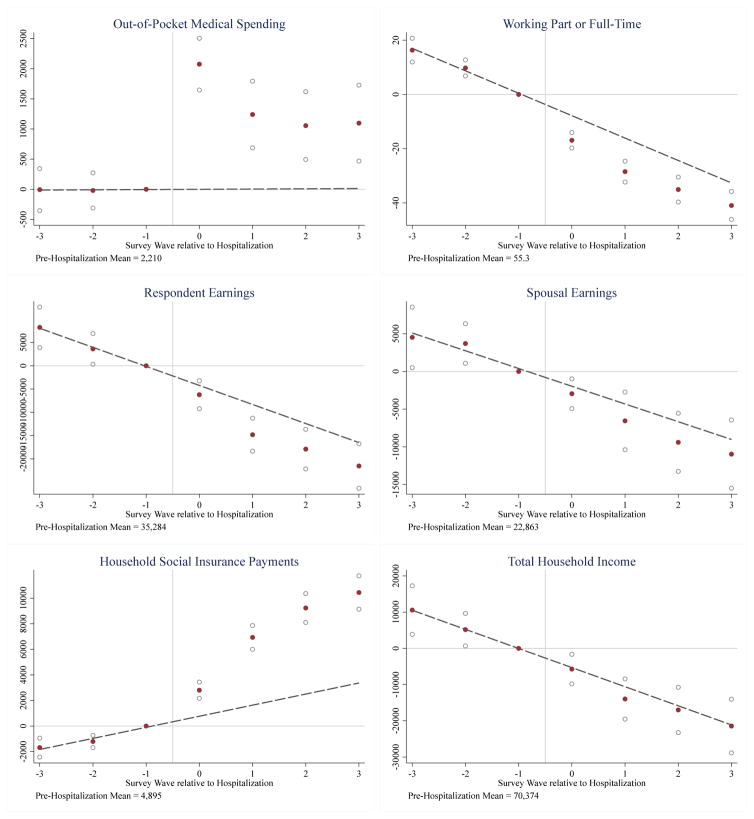
Our baseline sample of 50–59 year olds was chosen to restrict analysis to individuals who do not have access to Social Security retirement income at any point during our main, three-year follow-up period (eligibility starts at age 62). We therefore also consider the impact of hospital admissions for two older age groups: individuals who are 60–64 at the time of hospital admission and individuals who are 65+ at the time of admission (“the elderly”). Table 3 shows our estimates for these older age groups; Figure 2 shows results graphically for the 60–64 year olds and Appendix Figure 11 shows them for the elderly. Both older age groups have access to Social Security Retirement Income during our analysis period. The pre-admission employment rate is declining with age: it is 74 percent in our baseline sample compared to 55 percent for 60–64 year olds and 11 percent for 65+.
Table 3.
Impact of Hospitalization for Older Insured in HRS
| Out-of-Pocket Medical Spending | Working Part or Full-Time | Respondent Earnings | Spousal Earnings | Household Social Insurance Payments | Total Household Income | |
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| Panel A. Insured Ages 60 to 64 | ||||||
| 12-month effect | 3,056 | −11.6 | −3,718 | −1,950 | 3,940 | −546 |
| (383) | (2.47) | (4,422) | (2,915) | (715) | (5,910) | |
| [<.001] | [<.001] | [0.4] | [0.5] | [<.001] | [0.93] | |
| Effect at 36 months | 993 | −12.8 | −7,763 | −2,322 | 5,779 | −4,778 |
| (416) | (2.96) | (2,898) | (2,859) | (609) | (4,392) | |
| [0.017] | [<.001] | [0.0074] | [0.42] | [<.001] | [0.28] | |
| Average annual effect over 36 months | 1,350 | −12.2 | −5,738 | −2,134 | 4,856 | −2,662 |
| (203) | (2.45) | (3,142) | (2,624) | (542) | (4,531) | |
| [<.001] | [<.001] | [0.068] | [0.42] | [<.001] | [0.56] | |
| Pre-hospitalization mean | 2,210 | 55.3 | 35,284 | 22,863 | 4,895 | 70,374 |
| Number of Individuals | 1,627 | 1,627 | 1,627 | 1,627 | 1,627 | 1,627 |
| Number of Observations | 9,296 | 9,296 | 9,296 | 9,296 | 9,296 | 9,296 |
|
| ||||||
| Panel B. Elderly (Ages 65 and Older) | ||||||
| 12-month effect | 1,963 | 1.05 | −2,184 | −364 | −619 | −3,524 |
| (236) | (0.8) | (1,802) | (870) | (336) | (2,471) | |
| [<.001] | [0.19] | [0.23] | [0.68] | [0.065] | [0.15] | |
| Effect at 36 months | 557 | 2.24 | 446 | 1,337 | −84 | 2,223 |
| (263) | (0.95) | (1,317) | (554) | (267) | (1,624) | |
| [0.034] | [0.019] | [0.73] | [0.016] | [0.75] | [0.17] | |
| Average annual effect over 36 months | 840 | 1.64 | −868 | 486 | −351 | −650 |
| (132) | (0.810) | (1,437) | (618) | (258) | (1,814) | |
| [<.001] | [0.042] | [0.55] | [0.43] | [0.17] | [0.72] | |
| Pre-hospitalization mean | 2,521 | 11.4 | 8,248 | 4,672 | 15,811 | 38,287 |
| Number of Individuals | 5,785 | 5,785 | 5,785 | 5,785 | 5,785 | 5,785 |
| Number of Observations | 29,441 | 29,441 | 29,441 | 29,441 | 29,441 | 29,441 |
Notes: Samples are the insured ages 60 to 64 (see Appendix Table 4, column 6) and the elderly (see Appendix Table 4, column 9). All columns report effects based on OLS estimates of equation (4). Standard errors (clustered on the individual) are in parentheses and p-values are in brackets. See Table 2 for additional estimation details.
Figure 2.
Impact of Hospitalization for the Insured Ages 60 to 64 in the HRS
Notes: The sample is the insured ages 60 to 64. The points in each figure represent the estimated effects of event time (i.e. the μr’s from the non-parametric event study in equation 3), with the survey wave reporting the hospitalization normalized to zero. Survey waves are biannual; we assume the hospitalization occurs halfway between survey waves (12 months prior to survey wave zero) on average. The hollow circles present the 95% confidence intervals. The dashed line represents the estimated pre-admission linear relationship between outcome and event time from the parametric event study in equation 4 with the level normalized to match the non-parametric estimates. All estimates are weighted using survey weights.
Impacts on out-of-pocket spending are similar for all three age groups, although slightly smaller for the elderly. Earnings and employment declines are also roughly similar for the 60– 64 year olds and the 50–59 year olds; declines in the probability of employment are slightly higher for 60–64 year olds while declines in earnings are slightly lower; although neither difference is statistically significant, together they suggest that extensive-margin employment declines may be quantitatively more important in explaining earnings declines for 60–64 year olds compared to 50–59 year olds.
Strikingly, a much larger share - over 60 percent - of the earnings decline for 60–64 year olds is insured through social insurance.13 This increase in social insurance payments for 60–64 year olds appears to come entirely from larger increases in Social Security retirement income (see Appendix Table 11). Finally, for the elderly we find no effects of hospital admissions on either earnings or social insurance payments. Taken together, these results suggest that hospital admissions have important impacts on employment and earnings for those who are working at the time of the admission, and there is little formal insurance for these declines until individuals reach the age eligibility threshold for Social Security benefits. Not surprisingly, therefore, when we previously analyzed the impact of hospital admissions among the pooled group of 50–64 year olds, we found that a much greater share of the earnings decline was offset through social insurance payments: about 30 percent on average, compared to the 10 percent we estimate for our baseline 50–59 year old sample here; in the absence of age-eligibility for Social Security retirement income there do not appear to be alternative sources of (formal or informal) earnings insurance against health shocks for this population (Dobkin et al. 2016).
In addition to studying heterogeneity by age, we also explored how our results for our baseline sample of 50–59 year olds varied with socio-economic status (proxied for by pre-admission financial assets), and with (pre-admission) marital status. Appendix Table 12 and Appendix Figures 12–15 show the results. We see similar declines in employment by SES; level declines in earnings are, not surprisingly, larger for higher-wealth households (who have higher pre-admission earnings, as well), but they also appear to be somewhat proportionally larger. Impacts on employment and earnings appears to be slightly larger for single individuals. However, even for the three-quarters of the sample who are married preadmission, spousal earnings do not respond. Interestingly, for previously single individuals we do see an increase in spousal earnings following the admission, which reflects increases in the probability of being married post-admission (not reported).
3.2 Identifying Assumption and Robustness
Table 4 presents results from a number of alternative specifications of the parametric event study; the corresponding figures are in Appendix Figures 2–7. The results are generally reassuring. Column 1 presents the baseline specification. All subsequent columns represent a specific deviation from this baseline.
Table 4.
Robustness to Alternative Specifications and Sample Restrictions for the Non-Elderly Insured (Ages 50 to 59) in HRS
| Specification | [Baseline] | Individual FEs | Balanced Panel | Wave FEs only | Additional demographic controls (Cubic in age; dummies for gender, race and education) | No Restriction for Pre-Period Obsevation | Poisson |
|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | |
| Panel A: Out-of-Pocket Medical Spending | |||||||
| 12-month effect | 3,275 | 3,461 | 2,362 | 3,286 | 3,244 | 3,486 | 1 |
| (373) | (409) | (663) | (349) | (373) | (356) | (0.130) | |
| [<.001] | [<.001] | [<.001] | [<.001] | [<.001] | [<.001] | [<.001] | |
| Average annual effect over 36 months | 1,429 | 1,531 | 1,426 | 1,395 | 1,389 | 1,363 | 0.47 |
| (202) | (228) | (485) | (191) | (203) | (209) | (0.083) | |
| [<.001] | [<.001] | [0.0033] | [<.001] | [<.001] | [<.001] | [<.001] | |
| Pre-hospitalization mean | 2,133 | 2,133 | 1,967 | 2,133 | 2,133 | 2,170 | 2,133 |
| Panel B: Working Part or Full-Time | |||||||
| 12-month effect | −8.9 | −8.4 | −2.5 | −9.9 | −8.2 | −8.5 | −0.14 |
| (1.8) | (1.9) | (3.8) | (1.8) | (1.8) | (2) | (0.026) | |
| [<.001] | [<.001] | [0.5] | [<.001] | [<.001] | [<.001] | [<.001] | |
| Average annual effect over 36 months | −10 | −9.5 | −2.9 | −11 | −8.4 | −8.7 | −0.16 |
| (1.9) | (1.9) | (4) | (1.9) | (1.9) | (2.1) | (0.026) | |
| [<.001] | [<.001] | [0.48] | [<.001] | [<.001] | [<.001] | [<.001] | |
| Pre-hospitalization mean | 74 | 74 | 73 | 74 | 74 | 73 | 74 |
| Panel C: Respondent Earnings | |||||||
| 12-month effect | −6,445 | −6,462 | 4,627 | −8,417 | −5,746 | −11,340 | −0.15 |
| (4,024) | (4,102) | (6,937) | (4,518) | (3,980) | (4,921) | (0.088) | |
| [0.11] | [0.12] | [0.5] | [0.062] | [0.15] | [0.021] | [0.091] | |
| Average annual effect over 36 months | −8,753 | −9,459 | −2,338 | −10,009 | −7,432 | −11,339 | −0.21 |
| (3,415) | (3,239) | (6,102) | (3,819) | (3,280) | (4,027) | (0.075) | |
| [0.01] | [0.0035] | [0.7] | [0.0088] | [0.023] | [0.0049] | [0.0042] | |
| Pre-hospitalization mean | 45,327 | 45,327 | 45,704 | 45,327 | 45,327 | 44,130 | 45,327 |
| Panel D: Spousal Earnings | |||||||
| 12-month effect | −444 | −1,610 | 4,014 | −635 | 200 | 1,623 | −0.019 |
| (3,851) | (4,242) | (5,915) | (3,924) | (3,840) | (4,240) | −0.12 | |
| [0.91] | [0.7] | [0.5] | [0.87] | [0.96] | [0.7] | [0.87] | |
| Average annual effect over 36 months | 572 | −129 | 2,971 | 977 | 1,841 | 1,956 | 0.014 |
| (3,114) | (3,474) | (4,532) | (3,144) | (3,096) | (3,337) | −0.096 | |
| [0.85] | [0.97] | [0.51] | [0.76] | [0.55] | [0.56] | [0.89] | |
| Pre-hospitalization mean | 30,718 | 30,718 | 32,332 | 30,718 | 30,718 | 30,338 | 30,718 |
| Panel E: Household Social Insurance Payments | |||||||
| 12-month effect | 503 | 289 | 297 | 1,008 | 139 | 634 | 0.12 |
| (379) | (420) | (724) | (423) | (380) | (454) | (0.15) | |
| [0.18] | [0.49] | [0.68] | [0.017] | [0.71] | [0.16] | [0.45] | |
| Average annual effect over 36 months | 881 | 958 | 585 | 1,516 | 367 | 924 | 0.18 |
| (338) | (343) | (649) | (357) | (337) | (365) | (0.14) | |
| [0.009] | [0.0053] | [0.37] | [<.001] | [0.28] | [0.011] | [0.19] | |
| Pre-hospitalization mean | 2,649 | 2,649 | 2,714 | 2,649 | 2,649 | 2,654 | 2,649 |
| Panel F: Total Household Income | |||||||
| 12-month effect | −8,443 | −9,208 | 12,240 | −9,084 | −7,632 | −12,375 | −0.1 |
| (6,857) | (7,297) | (11,564) | (7,523) | (6,778) | (8,116) | (0.081) | |
| [0.22] | [0.21] | [0.29] | [0.23] | [0.26] | [0.13] | [0.2] | |
| Average annual effect over 36 months | −8,161 | −9,097 | 3,633 | −7,398 | −6,321 | −10,336 | −0.1 |
| (5,709) | (5,837) | (9,985) | (6,208) | (5,536) | (6,479) | (0.068) | |
| [0.15] | [0.12] | [0.72] | [0.23] | [0.25] | [0.11] | [0.13] | |
| Pre-hospitalization mean | 82,512 | 82,512 | 84,598 | 82,512 | 82,512 | 80,880 | 82,512 |
| Number of Individuals | 2,732 | 2,732 | 1,018 | 2,732 | 2,732 | 4,271 | 2,727 |
| Number of Observations | 13,286 | 13,286 | 5,090 | 13,286 | 13,286 | 17,647 | 13,262 |
Notes: Sample is the non-elderly insured (see Table 1, column 1). Column 1 replicates baseline results from Table 2. The individual fixed effects specification (column 2) includes wave dummies and individual fixed effects. Column 3 re-estimates the baseline specification restricting the sample to a balanced panel of individuals who are observed in waves −2 through 2 relative to their hospitalization. Column 4 includes only wave fixed effects instead of cohort-by-wave fixed effects. Column 5 adds a cubic in age, male dummy, race dummies and education dummies along with the cohort-by-wave fixed effects. Column 6 re-estimates the baseline specification on an expanded sample that does not restrict on having a pre-admission survey wave interview. Column 7 re-estimates the baseline specification with a Poisson, rather than a linear, regression. All estimates are weighted using survey weights. The 12-month and average annual effects over 36 months are calculated as described in Appendix C.
If we were to interpret the coefficients on the indicators for time after the hospital admission from the non-parametric event study coefficients as the causal effect of the admission, this would require the identifying assumption that, conditional on having a hospital admission during our observation period and the included controls, the timing of the admission is uncorrelated with the outcome. An implication is that there should be no trend in outcomes in the period leading up to the hospital admission. Figure 1 indicates that this is not strictly true. Our estimates indicate a (statistically insignificant) pre-admission rise in annual out-of- pocket spending of about $65 per year, a (statistically significant) pre-admission decline in the probability of employment of about 1.75 percentage points per year and a (statistically insignificant) pre-admission increase in annual earnings of about $80 per year (see Appendix Table 6). The rise in out-of-pocket expenses and decline in employment probability may reflect a gradual decline in health preceding the hospital admission. The parametric event study therefore requires a weaker identifying assumption, that, conditional on having a hospital admission during our observation period and the included controls, the timing of the admission is not correlated with deviations from the outcome’s linear trend in event time. Figure 1 suggests this is a very reasonable assumption.
We report two specifications designed to investigate sensitivity to potential violations of the identifying assumption of the parametric event study. The identifying assumption would be violated if there is an individual-specific component of the error term that, relative to the linear trend in event time, is correlated with the timing of hospitalization, conditional on the included controls. If, for example, individuals of different admission cohorts have different levels of outcomes, this would violate our identifying assumption. Therefore, in column 2 we report robustness to an alternative specification with individual fixed effects. This requires an additional normalization due to the collinearity of admission cohort, calendar time and event time; we omit an additional survey wave fixed effect. Attrition - either from mortality or non-response to the survey - that is correlated with the post-admission outcome poses another potential threat to our identifying assumption if attrition is correlated with the post-admission outcome. Attrition is mechanically zero in the survey wave after the admission (i.e., in survey wave 0) since one must survive to report the index admission. We estimate that about 3 percent of the non-elderly insured die between bi-annual waves after the index admission interview, and about 5 percent do not respond in a given wave. Inclusion of individual fixed effects (see column 2) is one natural approach to addressing potential bias due to attrition; the impact of a hospital admission is now estimated entirely off of within-individual changes and therefore should not be contaminated by any differential attrition correlated with the level of the outcome. However, if there is heterogeneity in treatment effects across individuals, the pattern of event study coefficients ( ) could still be affected by compositional changes in the set of individuals used to identify a given relative year coefficient. Therefore, as an additional check, we also re-estimated the baseline specifications on a balanced panel of individuals whom we observe in all survey waves −2 through 2 (column 3). This balanced panel specification also allows us to examine the time pattern of outcomes in the figures without concerns about potential effects of compositional changes.
The remaining columns of Table 4 investigate sensitivity to other choices. The baseline specification included “HRS cohort”-by-wave dummies because of the changes in sample composition over time as the HRS adds additional birth cohorts. Columns 4 and 5 show the results if we instead control only for wave dummies (column 4) or we add to the baseline specification additional controls for demographics, specifically a cubic in age and dummies for gender, race, and educational attainment (column 3). Column 6 relaxes the requirement that we observe individuals in wave −1 without reporting a hospital admission, so that these individuals may have experienced a hospital admission in the three years prior to their index admission; for this sample, we define insurance status based on the survey wave reporting the hospital admission (as opposed to the survey wave preceding the hospital admission as in the baseline sample). Finally, given the high variance, right-skewness of out-of-pocket spending, earnings, and income, column 7 reports the results of estimating a proportional rather than a linear model. Specifically, we estimate a quasi-maximum likelihood Poisson model; this produces quantitatively similar proportional estimates, as does a model of log household income.
4 Impacts on Credit Report Outcomes
4.1 Main results
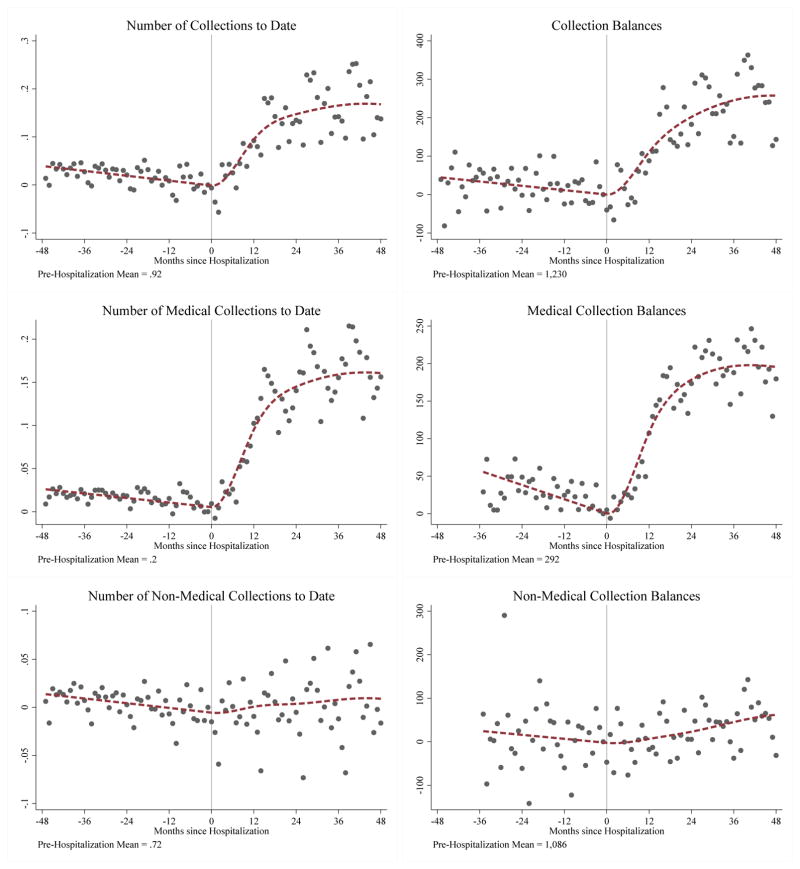
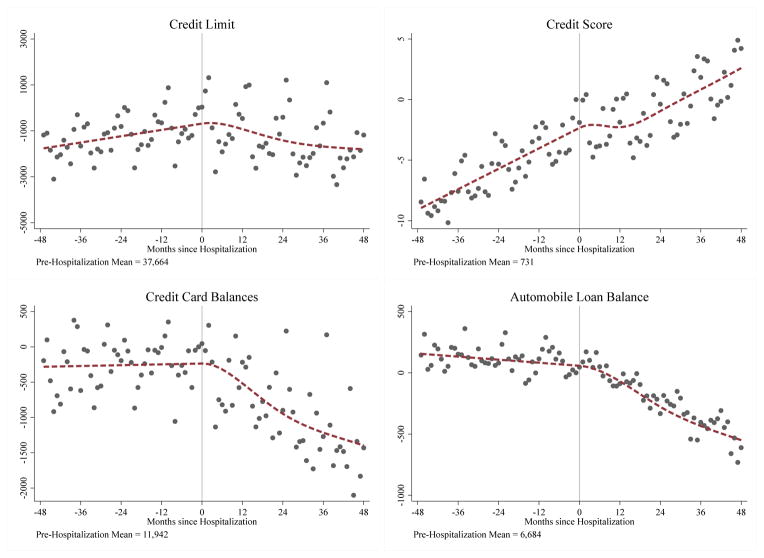
Figures 3 and 4 show the impact of hospital admissions for insured adults ages 25–64 at the time of admission on collections, credit limits, credit card borrowing, and automobile loans in the credit report data; the top panel of Figure 5 shows the impact on bankruptcy rates for this same population. Once again, we plot the estimated coefficients on event time (μr’s) from the non-parametric event study regression (equation (3)), and the estimated preadmission linear relationship between outcome and event time (δ) from the parametric event study regression (equation (5)).14 Tables 5 and 6 (panel A) summarize the implied effects of the hospital admission (from equation (5)) at 1 year and 4 years after the index admission. Appendix Table 19 reports the estimated coefficients directly.
Figure 3.
Impact of Hospitalization on Collections for the Non-Elderly Insured (Ages 25 to 64)
Notes: The sample is the non-elderly insured (see Table 1, column 2). The months on the x-axis are defined relative to the index admission. The points in each figure represent the estimated effects of event time (i.e. the μr’s from the non-parametric event study in equation 3). The dashed line represents the estimated event study coefficients from the parametric event study in equation 5 with the level normalized to match the non-parametric estimates. All estimates are weighted to account for individuals’ sampling probabilities. All variables are observed from 2002 to 2011, except medical and non-medical collection balances which are observed beginning in 2005.
Figure 4.
Impact of Hospitalization on Other Credit Report Outcomes for the Non-Elderly Insured (Ages 25 to 64)
Notes: The sample is the non-elderly insured (see Table 1, column 2). The months on the x-axis are defined relative to the index admission. The points in each figure represent the estimated effects of event time (i.e. the μr’s from the non-parametric event study in equation 3). The dashed line represents the estimated event study coefficients from the parametric event study in equation 5 with the level normalized to match the non-parametric estimates. All estimates are weighted to account for individuals’ sampling probabilities. All variables are observed from 2002 to 2011.
Figure 5.
Impact of Hospitalization on Bankruptcy
Notes: Samples are non-elderly insured, uninsured, and the elderly (see Appendix Table 13, columns 3, 6, and 9). The months on the x-axis are defined relative to the index admission. The points in each figure represent the estimated effects of event time (i.e. the μr’s from the non-parametric event study in equation 3). The dashed line represents the estimated event study coefficients from the parametric event study in equation 5 with the level normalized to match the non-parametric estimates. All estimates are weighted to account for individuals’ sampling probabilities.
Table 5.
Impact of Hospitalization on Collections
| Number of Collections to Date | Collection Balances | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| All | Medical | Non-Medical | All | Medical | Non-Medical | |
| (1) | (2) | (3) | (4) | (5) | (6) | |
| Panel A. Non-Elderly Insured (Ages 25 to 64) | ||||||
| 12-month effecta | 0.110 | 0.095 | 0.011 | 122 | 127 | 18 |
| (0.005) | (0.002) | (0.003) | (13) | (7) | (16) | |
| [<.001] | [<.001] | [0.001] | [<.001] | [<.001] | [0.26] | |
| 48-month effectb | 0.210 | 0.180 | 0.034 | 302 | 271 | 101 |
| (0.019) | (0.008) | (0.014) | (37) | (18) | (47) | |
| [<.001] | [<.001] | [0.017] | [<.001] | [<.001] | [0.03] | |
| Pre-hospitalization mean | 0.920 | 0.200 | 0.720 | 1,230 | 292 | 1,086 |
| Number of Individuals | 383,718 | 383,718 | 383,718 | 383,718 | 375,844 | 375,844 |
| Number of Observations | 3,131,534 | 3,131,534 | 3,131,534 | 3,131,534 | 2,208,517 | 2,208,517 |
|
| ||||||
| Panel B. Non-Elderly Uninsured (Ages 25 to 64) | ||||||
| 12-month effecta | 0.97 | 0.85 | 0.12 | 4,469 | 4,259 | 246 |
| (0.012) | (0.008) | (0.007) | (51) | (45) | (36) | |
| [<.001] | [<.001] | [<.001] | [<.001] | [<.001] | [<.001] | |
| 48-month effectb | 1.3 | 1.2 | .11 | 6,199 | 6,144 | 195 |
| (0.045) | (0.028) | (0.028) | (130) | (102) | (100) | |
| [<.001] | [<.001] | [<.001] | [<.001] | [<.001] | [0.051] | |
| Pre-hospitalization mean | 2.3 | 0.59 | 1.7 | 3,529 | 1,292 | 2,762 |
| Number of Individuals | 153,617 | 153,617 | 153,617 | 153,617 | 151,343 | 151,343 |
| Number of Observations | 1,256,759 | 1,256,759 | 1,256,759 | 1,256,759 | 913,516 | 913,516 |
|
| ||||||
| Panel C. Elderly (Ages 65 and Older) | ||||||
| 12-month effecta | 0.027 | 0.026 | 0 | 24 | 17 | 4 |
| (0.002) | (0.001) | (0.002) | (8) | (3) | (11) | |
| [<.001] | [<.001] | [0.8] | [0.002] | [<.001] | [.74] | |
| 48-month effectb | 0.038 | 0.049 | −0.011 | 84 | 37 | 39 |
| (0.010) | (0.004) | (0.008) | (24) | (8) | (34) | |
| [<.001] | [<.001] | [0.19] | [<.001] | [<.001] | [0.25] | |
| Pre-hospitalization mean | 0.24 | 0.05 | 0.19 | 428 | 75 | 422 |
| Number of Individuals | 414,547 | 414,547 | 414,547 | 414,547 | 387,839 | 387,839 |
| Number of Observations | 2,959,802 | 2,959,802 | 2,959,802 | 2,959,802 | 1,946,208 | 1,946,208 |
Notes: Samples are non-elderly insured, uninsured, and the elderly (see Appendix Table 13, columns 3, 6, and 9). All columns report effects based on OLS estimates of equation (5). Pre-hospitalization means are calculated using the credit report from January of the calendar year preceding the hospitalization (between 12 and 23 months before the hospitalization). All variables are observed from 2002 to 2011, except medical and non-medical collection balances which are only observed beginning in 2005. Standard errors (clustered on the individual) are in parentheses and p-values are in brackets. All estimates are weighted to adjust for individuals’ sampling probabilities.
12-month effect is calculated from equation (5) as 144*β2+1,728*β3
48-month effect is calculated from equation (5) as 2,304*β2+110,592*β3+46,656*β4+13,824*β5
Table 6.
Impact of Hospitalization on Other Credit Report Outcomes
| Any Bankruptcy to Date | Credit Limit | Credit Score | Credit Card Balances | Automobile Loan Balance | |
|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | |
| Panel A. Non-Elderly Insured (Ages 25 to 64) | |||||
| 12-month effect | 0.0013 | −515 | −1.6 | −293 | −102 |
| (0.0003) | (154) | (0.200) | (94) | (28) | |
| [<.001] | [<.001] | [<.001] | [0.0018] | [<.001] | |
| 48-month effect | 0.0042 | −2,215 | −1.8 | −1,208 | −507 |
| (0.0009) | (440) | (0.500) | (253) | (71) | |
| [<.001] | [<.001] | [<.001] | [<.001] | [<.001] | |
| Pre-hospitalization mean | 0.034 | 37,664 | 731 | 11,942 | 6,684 |
| Number of Individuals | 383,718 | 383,718 | 371,715 | 383,718 | 383,718 |
| Number of Observations | 3,131,534 | 3,131,534 | 2,942,253 | 3,131,534 | 3,131,534 |
|
| |||||
| Panel B. Non-Elderly Uninsured (Ages 25 to 64) | |||||
| 12-month effect | 0.0048 | −678 | −5 | −264 | −267 |
| (0.000) | (131) | (0.300) | (83) | (29) | |
| [<.001] | [<.001] | [<.001] | [0.0014] | [<.001] | |
| 48-month effect | 0.014 | −690 | 6.6 | −443 | −349 |
| (0.001) | (353) | (0.600) | (214) | (73) | |
| [<.001] | [0.051] | [<.001] | [0.038] | [<.001] | |
| Pre-hospitalization mean | 0.037 | 15,145 | 655 | 5,376 | 3,981 |
| Number of Individuals | 153,617 | 153,617 | 137,913 | 153,617 | 153,617 |
| Number of Observations | 1,256,759 | 1,256,759 | 1,017,096 | 1,256,759 | 1,256,759 |
|
| |||||
| Panel C. Elderly (Ages 65 and Older) | |||||
| 12-month effect | −0.00019 | 370 | −1.4 | 72 | 69 |
| (0.0002) | (138) | (0.200) | (73) | (17) | |
| [0.4] | [0.0073] | [<.001] | [0.32] | [<.001] | |
| 48-month effect | −0.001 | −448 | −3.3 | −30 | 194 |
| (0.0007) | (393) | (0.500) | (187) | (43) | |
| [0.16] | [0.25] | [<.001] | [0.87] | [<.001] | |
| Pre-hospitalization mean | 0.016 | 36,967 | 824 | 7,016 | 2,143 |
| Number of Individuals | 414,547 | 414,547 | 405,389 | 414,547 | 414,547 |
| Number of Observations | 2,959,802 | 2,959,802 | 2,833,027 | 2,959,802 | 2,959,802 |
Notes: Samples are non-elderly insured, uninsured, and the elderly (see Appendix Table 13, columns 3, 6, and 9). All columns report effects based on OLS estimates of equation (5). All variables are observed from 2002 to 2011. Standard errors (clustered on the individual) are in parentheses and p-values are in brackets. All estimates are weighted to adjust for individuals’ sampling probabilities.
Unpaid bills and bankruptcy
There is a clear “on impact” effect of hospital admissions on collections (number and balances). Four years later, a hospital admission is associated with an increase in total collection balances of $302 (standard error = $37) or about 25 percent relative to pre-admission balances. The effect is most pronounced for medical collections, although there is some evidence of a smaller increase for non-medical collections as well, which may in fact reflect an increase in mis-classified medical collections.15 The effect on medical collections increases initially over time and then appears to flatten out after about two years. This makes sense; medical collection balances represent a stock (not flow) and hospitals usually make several attempts to get payment on a bill before sending it to a collection agency.
Hospital admissions are also associated with a statistically significant increase in consumer bankruptcy. Four years later, a hospital admission is associated with an increase in the probability of bankruptcy of 0.4 percentage points, or about 33 percent relative to the annual bankruptcy rate of 1.2 percent in this population.
Borrowing and access to credit
Four years later, hospital admissions are associated with a decline in credit card balances (our primary proxy for borrowing b) of $1,208 (standard error = $253) - or about 10 percent. Automobile loan balances also decline in the four years post admission - by $507 (standard error = $71), or about 7 percent. In Appendix Table 34, we show that hospital admissions are also associated with a slight decline in the probability of having a second mortgage (such as a Home Equity Line of Credit). Overall, the decline in all three forms of borrowing is consistent with the persistent decline in future income following a hospital admission estimated in the HRS.
Hospital admissions are also associated with declines in access to credit. Four years after admission, credit limits have declined by $2,215 (standard error = $440), or about 5.5 percent relative to pre-admission levels - and credit scores by 1.8 (standard error = 0.5) - or about 0.2 percent - although the visual evidence for credit scores is not particularly compelling.16
The decline in credit limits is likely more consequential than the decline in credit score. The decline in credit limits following a hospital admission is over half the the decline in credit limits following an unemployment spell,17 while our back-of-the-envelope calculations suggests that the decrease in credit score may be associated with an increase in interest rate of less than one-tenth of one percent (0.054%).18 A larger impact of hospital admissions on borrowing limits (L) than interest rates (r) is consistent with our theoretical model in which the effect of a hospital admission on r was theoretically ambiguous due to two opposing forces: hospital admissions increase unpaid bills (u), which should serve to increase r, but also decrease b which should serve to decrease r.19
Alternative samples: The elderly and the non-elderly uninsured
We conducted a parallel set of analyses for elderly individuals and for uninsured non-elderly admissions and summarize them briefly here. Tables 5 and 6 presents the results from the parametric event studies in panels C and B, respectively; the underlying regression coefficients are shown in Appendix Tables 20 and 21, and the non-parametric event study figures are shown in Appendix Figures 16–19.
For the elderly, even though the severity of the health shock (as measured by length of stay or charges) is larger (see Appendix Table 13) the results suggest similar proportional (and smaller absolute) impacts on collection outcomes as compared to the non-elderly insured, and limited or no impact - either visually or in the estimated implied effects - on other outcomes. In particular, there is no evidence of an impact on bankruptcy or credit limits; the point estimates are usually wrong-signed and substantively small compared to estimates for non-elderly adults. There is no evidence of a decline in credit card borrowing, and weak evidence of a small increase in automobile loans. There is a decline in credit score following a hospital admission that is similar in magnitude to the quantitatively trivial estimate for the non-elderly insured. The lack of evidence of impacts on credit limits and borrowing goes hand-in-hand with the lack of evidence of impacts on earnings and employment for the elderly in the HRS.
For the uninsured, non-elderly, we find much larger impacts on collections and bankruptcy than for the insured non-elderly, but similar (or smaller) impacts on credit card balances, automobile balances, and credit limits. For example, four years later, a hospital admission is associated with an increase in collection balances of $6,199 (standard error = $130) for the uninsured, compared to $302 (standard error = $37) for the insured. The right tail effects are also much larger for the uninsured, for example, the 90th percentile impact on collection balances is $23,000 for the uninsured, compared to $600 for the insured (see Appendix Tables 26 and 32 for quantile regressions). The impact on bankruptcy is also larger for the uninsured; a hospital admission is associated with a 1.4 percentage point (standard error = 0.14) increase in bankruptcy over four years, compared to a 0.4 percentage point increase for the insured (the pre-hospitalization annual bankruptcy rate is similar at about 1.2 percent). In interpreting these results, it is important to note that unlike being insured, being “uninsured” is not a persistent state post-admission; for those uninsured at the index admission, only about 43 percent of subsequent hospital days over the next four years are uninsured (see Appendix Table 14), which may reflect post-admission incentives to take up insurance or post-admission changes in eligibility for public health insurance.
The four-year impacts on the other outcomes are similar proportionally (and smaller in absolute terms) for the uninsured relative to the insured.20 For example, four years post-admission, the decline in credit limits is about 5 percent for each group, and the decline in borrowing about 9 percent.21 The decline in borrowing following a hospital admission for the uninsured suggests that the increase in out of pocket spending they experience is small relative to their decline in income.
4.2 Identifying assumption and robustness
Table 7 presents results from a number of alternative specification of the parametric event study for the insured non-elderly; the corresponding figures are in Appendix Figures 20– 26.22 The results are generally reassuring. Column 1 presents the baseline specification. All subsequent columns represent a specific deviation from this baseline.
Table 7.
Robustness to Alternative Specifications and Sample Restrictions for the Non-Elderly Insured (Ages 25 to 64) Credit Report Sample
| [Baseline] | Individual FEs | Balanced Panel | Lowest Predicted Mortality Quartile | Including Individuals with Prior Hospitalizations | ER Admissions | Non-Deferrable (Weekend/Weekday Ratio ~ 2/5) | Excluding Ambulatory Care Sensitive Conditions | |
|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| Panel A: Number of Collections to Date | ||||||||
| 12-month effect | 0.11 | 0.11 | 0.12 | 0.11 | 0.16 | 0.14 | 0.14 | 0.10 |
| (0.005) | (0.004) | (0.005) | (0.009) | (0.004) | (0.006) | (0.012) | (0.005) | |
| [<.001] | [<.001] | [<.001] | [<.001] | [<.001] | [<.001] | [<.001] | [<.001] | |
| 48-month effect | 0.21 | 0.23 | 0.24 | 0.25 | 0.50 | 0.24 | 0.27 | 0.21 |
| (0.019) | (0.018) | (0.022) | (0.038) | (0.018) | (0.025) | (0.048) | (0.02) | |
| [<.001] | [<.001] | [<.001] | [<.001] | [<.001] | [<.001] | [<.001] | [<.001] | |
| Pre-hospitalization mean | 0.92 | 0.92 | 0.78 | 1.1 | 0.91 | 1.1 | 1 | 0.90 |
| Panel B: Collection Balances | ||||||||
| 12-month effect | 122 | 138 | 138 | 91 | 156 | 194 | 185 | 117 |
| (13) | (14) | (15) | (24) | (12) | (18) | (34) | (13) | |
| [<.001] | [<.001] | [<.001] | [<.001] | [<.001] | [<.001] | [<.001] | [<.001] | |
| 48-month effect | 302 | 335 | 281 | 218 | 404 | 415 | 457 | 302 |
| (37) | (41) | (49) | (72) | (35) | (50) | (94) | (39) | |
| [<.001] | [<.001] | [<.001] | [0.002] | [<.001] | [<.001] | [<.001] | [<.001] | |
| Pre-hospitalization mean | 1,230 | 1,230 | 1,012 | 1,334 | 1,316 | 1,500 | 1,369 | 1,188 |
| Panel C: Any Bankruptcy to Date | ||||||||
| 12-month effect | 0.0013 | 0.00092 | 0.0013 | 0.0016 | 0.0018 | 0.00095 | 0.00091 | 0.0013 |
| (0.00031) | (0.00031) | (0.00039) | (0.00060) | (0.00029) | (0.00037) | (0.00069) | (0.00032) | |
| [<.001] | [0.0031] | [<.001] | [0.0078] | [<.001] | [0.01] | [0.19] | [<.001] | |
| 48-month effect | 0.0042 | 0.0029 | 0.0039 | 0.005 | 0.0055 | 0.0035 | 0.004 | 0.0043 |
| (0.0009) | (0.0010) | (0.0012) | (0.0018) | (0.0009) | (0.0011) | (0.0021) | (0.0010) | |
| [<.001] | [0.0023] | [0.0016] | [0.0047] | [<.001] | [0.0017] | [0.055] | [<.001] | |
| Pre-hospitalization mean | 0.034 | 0.034 | 0.035 | 0.039 | 0.033 | 0.036 | 0.034 | 0.034 |
| Panel D: Credit Limit | ||||||||
| 12-month effect | −515 | −539 | −758 | −87 | −924 | −167 | 273 | −483 |
| (154) | (164) | (206) | (265) | (139) | (168) | (316) | (162) | |
| [<.001] | [0.001] | [<.001] | [0.74] | [<.001] | [0.32] | [0.39] | [0.0028] | |
| 48-month effect | −2,215 | −2,170 | −2,414 | −661 | −4,124 | −1,799 | −484 | −2,173 |
| (440) | (485) | (637) | (758) | (395) | (466) | (872) | (461) | |
| [<.001] | [<.001] | [<.001] | [0.38] | [<.001] | [<.001] | [0.58] | [<.001] | |
| Pre-hospitalization mean | 37,664 | 37,664 | 41,024 | 30,082 | 35,589 | 33,444 | 33,533 | 38,345 |
| Panel E: Credit Score | ||||||||
| 12-month effect | −1.6 | −1.5 | −1.9 | −1.4 | −1.7 | −1.5 | −1.1 | −1.6 |
| (0.18) | (0.17) | (0.24) | (0.32) | (0.17) | (0.21) | (0.41) | (0.18) | |
| [<.001] | [<.001] | [<.001] | [<.001] | [<.001] | [<.001] | [.0057] | [<.001] | |
| 48-month effect | −1.8 | −1.8 | −1.4 | −1.8 | −2.3 | .38 | −.26 | −2 |
| (0.45) | (0.46) | (0.67) | (0.79) | (0.42) | (0.55) | (1) | (0.47) | |
| [<.001] | [<.001] | [0.036] | [0.025] | [<.001] | [0.48] | [0.8] | [<.001] | |
| Pre-hospitalization mean | 731 | 731 | 736 | 705 | 726 | 718 | 720 | 733 |
| Panel F: Credit Card Balances | ||||||||
| 12-month effect | −293 | −294 | −365 | 37 | −448 | −269 | −159 | −261 |
| (94) | (104) | (128) | (170) | (85) | (104) | (202) | (98) | |
| [0.0018] | [0.0048] | [0.0044] | [0.83] | [<.001] | [0.0098] | [0.43] | [0.0078] | |
| 48-month effect | −1,208 | −1,180 | −1,562 | −169 | −1,988 | −1,275 | −693 | −1,153 |
| (253) | (290) | (391) | (458) | (226) | (275) | (532) | (264) | |
| [<.001] | [<.001] | [<.001] | [0.71] | [<.001] | [<.001] | [0.19] | [<.001] | |
| Pre-hospitalization mean | 11,942 | 11,942 | 13,026 | 10,589 | 11,309 | 10,714 | 10,810 | 12,130 |
| Panel G: Automobile Loan Balance | ||||||||
| 12-month effect | −102 | −137 | −151 | −63 | −130 | −122 | −115 | −95 |
| (28) | (31) | (38) | (56) | (26) | (33) | (63) | (30) | |
| [<.001] | [<.001] | [<.001] | [0.26] | [<.001] | [<.001] | [0.068] | [0.0013] | |
| 48-month effect | −507 | −568 | −782 | −639 | −531 | −580 | −665 | −503 |
| (71) | (83) | (110) | (139) | (65) | (82) | (158) | (74) | |
| [<.001] | [<.001] | [<.001] | [<.001] | [<.001] | [<.001] | [<.001] | [<.001] | |
| Pre-hospitalization mean | 6,684 | 6,684 | 7,288 | 7,370 | 6,512 | 6,446 | 6,503 | 6,748 |
| Number of Individuals | 383,718 | 383,718 | 297,068 | 93,224 | 480,127 | 241,400 | 74,314 | 351,753 |
| Number of Observations | 3,131,534 | 3,131,534 | 1,782,408 | 810,774 | 3,836,488 | 1,958,271 | 600,610 | 2,876,934 |
Notes: Column 1 replicates results for the non-elderly insured (see Tables 5 and 6 and notes to Table 5 for details). All other columns indicate specific departures from the baseline sample and specification as follows: Column 2 adds individual fixed effects to the estimating equation (see equation (17)). Column 3 limits the analysis to a balanced panel of individuals with non-missing data for the two years before and four years after their hospitalization. Column 4 restricts the sample to individuals in the lowest quartile of predicted mortality risk based on age and diagnosis-related group for the index admission. Column 5 adds back to the baseline sample insured individuals who had a prior hospital admission within the last three years. Column 6 restricts the sample to admissions through the emergency room. Column 7 restricts to non-deferrable admissions, which are limited to the subset of admissions that originate through the ER and have an ICD-9 code as the primary diagnosis that has weekend to weekday frequencies closest to the 2:5 ratio that we would expect if there is no delay in care. Column 8 excludes admissions for “ambulatory care sensitive conditions.”
Once again, we use the non-parametric event study to examine trends in outcomes leading up to the hospital admission in Figures 4 and 5. For some outcomes - such as collection balances, credit card borrowing, and credit limits - the pre-trends appear negligible. However, for others - particularly bankruptcy and credit score - they are quite pronounced. Fortunately, once again where there are trends relative to event time, they seem reasonably well-approximated by a linear trend. Thus, we are comfortable relying on the identifying assumption of the parametric event study model.
However, we report results from several alternative specifications designed to investigate sensitivity to potential violations of the identifying assumption of the parametric event study. In column 2 we include individual fixed effects. This specification requires an additional normalization; we impose that there are no pre-trends in outcome yi,t in the months leading up to the hospitalization event between r = −47 and r = −35. We discuss the specific requirements in more detail in Appendix D.2.2.
Columns 3 and 4 address potential threats to the identifying assumption arising from non-random attrition, which in this setting arises primarily due to mortality. For non-elderly insured adults, mortality is 3.2 percent in the 12 months following the index admission, and 6.3 percent in 48 months (Table 1, column 2). Mortality per se is not a problem for our analysis. However, since by construction mortality is correlated with event time (you must be alive to have the event), it would pose a threat to our identifying assumption if mortality were correlated with yi,t, in either levels or changes. For example, if hospitalizations for individuals who have worse pre-hospitalization financial outcomes are also more likely to result in death, attrition due to mortality would bias downward our estimated impact of hospitalizations on financial well-being; Appendix Table 17 suggests that post-admission mortality is correlated with somewhat worse pre-admission financial outcomes.
As discussed in the context of the HRS analysis, inclusion of individual fixed effects (see column 2) or restricting to a balanced panel are approaches to addressing potential bias due to attrition. Column 3 shows the results are not sensitive to estimating the baseline specification on a balanced panel of individuals whom we observe alive in all relative months from −23 to 48. Consistent with the pattern in Appendix Table 17 that post-admission mortality is correlated with worse pre-admission financial outcomes, the estimated impacts of a hospital admission tend to be slightly larger with either individual fixed effects (column 2) or the balanced panel (column 3). A separate attraction of the balanced panel specification is that it allows us to examine the pattern of pre-trends and of post-hospitalization effects without concerns that they might be driven by compositional changes. Primarily for space reasons, in the main text we show the post-hospitalization effects only out to 48 months (which is also the maximum follow-up period we can observe for all hospitalizations). As noted, however, we estimate our equations on data out to 72 months post hospital admission. For completeness, the “baseline” results in Appendix Figures 20 through 26 (top left corner) therefore show the results out to 72 months. We also show results limited to early hospitalizations (2003–2005) - for whom the analysis out to 72 months can be done on a balanced panel of all admissions with outcomes observed through 72 months- and the later hospitalizations (2005 – 2007) - for whom the entire 4 year pre period can be estimated on a balanced panel of admissions with outcomes observed for that entire pre period. Columns 7 and 8 of Appendix Table 24 show the estimates are similar for these “early” and “late” balanced panel analyses. The graphical evidence in Appendix Figures 20 through 26 for both the unbalanced panel (top left figure) and balanced panel (bottom right figure) suggests that the impact of hospital admissions on collections, and perhaps bankruptcies, has plateaued by 48 months; the impacts on the other outcomes - credit limit, credit score, credit balances, and automobile balances - if anything may be larger over a longer time horizon. We show graphical results for the early and late balanced panel results in Appendix Figures 27–28.
The individual fixed effect specification and the balanced panel specification address possible bias due to correlations between mortality and the level of the outcome, but there is still potential for bias if mortality is correlated with the impact of a hospital admission (i.e., mortality is correlated with μr>0). The sign of any potential bias is unclear. If hospitalizations that cause greater financial strain are more likely to result in death, our estimated impact of hospitalizations on financial strain would be biased downward. Alternatively, if one way individuals improve their health and reduce their mortality probability following a hospitalization is to borrow and take on more debt, our estimated impact of hospital admission would be biased upward.
To investigate this potential concern, we restricted our sample to the lowest quartile of predicted mortality - predicted based on diagnosis and age at admission.23 The sample restriction to the lowest quartile of predicted mortality essentially eliminates attrition during our sample period; 12- and 48-month mortality are 0.24 percent and 0.9 percent, respectively, compared to 3.2 and 6.3 percent in the full sample (see Appendix Table 18). Column 4 shows the results are, once again, robust to this alternative specification. The point estimates vary more relative to the baseline (column 1) with this alternative specification than the previous ones, although there is no clear directionality to the sign and the differences are not statistically significant. Overall, we view these results as reassuring about the robustness of our findings to potential differential attrition.
In column 5 we expand rather than restrict the sample - adding back the approximately 15 percent of individuals who had a prior hospital admission in the last three years. These individuals are excluded from the baseline sample because of our desire to examine the impact of an initial health shock, for both econometric and economic reasons. In practice, the results are robust to including individuals with a prior hospital admission in our analysis; if anything, the estimated impacts become slightly bigger in magnitude. However, as seen in Appendix Figures 20 through 26, the pre-trends in outcomes are, as expected, more pronounced with the inclusion of these additional individuals who have already started to experience a health decline prior to the index event.
Heterogeneity
An implication of the identifying assumption of the parametric event study is that while individuals may be on a slow secular trend relative to the admission, they do not anticipate or have discretion over the exact timing of the hospital admission. The detail in the hospital discharge data allows us to investigate the sensitivity of our findings to restricting to admissions that are more likely to fit these criteria.
We find that the results look similar when we limit to admissions that are less likely to be anticipated. Column 6 shows the results of limiting to admissions through the ER; column 7 shows the results of limiting to admissions to admissions that are classified as “non-deferrable” using the Card, Dobkin, and Maestas (2009) metric of admissions whose ratio of weekend to weekday admissions is “close to” two-fifths.24 In Appendix Table 25 we present further such cuts, looking at admissions for particular conditions that may be less likely to be anticipated, such as heart attacks, car accidents, and external injuries; in some cases the samples get quite small, but there is no obvious pattern of differential effects for less anticipated admissions. As a final sample restriction related to concerns about the identifying assumption, in column 8 we exclude admissions for “ambulatory care sensitive conditions” - these are admissions for conditions that are potentially avoidable with timely treatment from either the patient or his primary care provider (Caminal et al. 2004) - since they may violate the assumption of a sudden and unexpected shock.
We also explored heterogeneity in the impacts of hospital admissions more generally across different sub-samples of individuals and types of hospitalizations. Results are shown in Appendix Tables 23 through 25. We find smaller impacts of a hospital admission for those on Medicaid than those with private insurance, which may reflect the lower labor force attachment for those on Medicaid; consumer-cost sharing is similar for these groups.25 There is some evidence of larger impacts for admissions for chronic diseases and for admissions with higher predicted list charges; such admissions may have larger impacts on medical expenses and/or earnings. Results also look similar for admission across different types of hospitals (public, non-profit and for profit), and for the five most common reasons for admission.
Finally, Appendix Table 26 moves beyond mean impacts to examine results from unconditional quantile regressions on the distribution of five continuous outcomes: total collection balances, credit limit, credit score, credit card balances, and automobile loan balances. Many of these are highly skewed variables (see Appendix Table 15). Median impacts tend to be smaller than mean, particularly for balances. In general, the impacts at the 75th percentile are fairly similar to mean effects, and the 90th percentile impacts are often between two and three times larger than the mean impacts. This could suggest a skewed distribution of health shocks, with a subset of shocks having particularly severe credit market consequences. Mean impacts that are larger than median impacts are also consistent with our findings in the HRS that a large share of the earnings decline associated with hospital admissions comes from extensive margin labor supply adjustments; this suggests a skewed pattern of earnings responses, with many individuals experiencing small changes in earnings but some individuals experiencing much larger changes from leaving the labor force.
Given the right-skewness of many of our continuous outcomes, in Appendix Tables 27 and 28 we also report results from estimating a proportional rather than a linear model. Specifically, we estimate a quasi-maximum likelihood Poisson model. The results are robust and similar in magnitude to the implied proportional effects (relative to pre-admission means) from the linear model.
5 Implications
5.1 Impact of hospital admissions on earnings
In the first three years post-admission we estimate an average annual earnings decline for 50–59 year olds of about 19 percent of pre-hospitalization earnings. This earnings decline is similar in magnitude to estimates of earnings losses from job displacement (e.g., Jacobson, LaLonde, and Sullivan 1993, Sullivan and von Wachter 2009). The earnings decline appears permanent over the seven post-admission years we can analyze - indeed, the point estimates suggest the impacts are increasing over time - and large relative to the (shorter run) increase in out-of-pocket medical spending.
The results from the credit reports complement and enrich this analysis. In the framework in Section 1, declines in credit limits are assumed to proxy for declines in earnings potential, and declines in borrowing are consistent with an impact of hospital admissions on income that is increasing over time and large relative to the (front-loaded) increase in out-of-pocket medical costs. Consistent with this interpretation, we find little impact of hospital admissions for the elderly on earnings in the HRS or on credit limits or borrowing in the credit report data.26
What causes the decline in earnings and employment for the non-elderly insured that we observe in the HRS data? In Section 1 we modeled the hospital admission as reducing wages (productivity) or increasing disutility of work. Another - unmodeled - possibility is that a hospital admission reduces life expectancy. If consumers are living “hand to mouth” a change in life expectancy would have no effect on earnings and employment. However, for life-cycle consumers who are saving up for retirement, a decline in life expectancy would be expected to decrease savings and labor market activity (e.g., Attanasio and Hoynes 2000; Restuccia and Vandenbrouke 2013). Using Restuccia and Vandenbrouke’s (2013) estimate that the elasticity of annual earnings with respect to life expectancy is −0.05, our calibration exercise suggests that the decline in life expectancy due to a hospital admission would imply a 0.1 to 0.5 percent average decline in earnings after 3 years or, in other words, a very small share of the 19% earnings decline we estimate.27 One can get a larger role for life expectancy in explaining our earnings decline if we consider a model of retirement rather than hours choice (e.g., Bloom, Canning, and Moore 2014). Here, our calibration exercise suggests that the decline in life expectancy due to a hospital admission would imply a 0.4 to 1.5 percentage point increase in the probability of retired after 3 years, which may be able to explain up to 15 percent of the decline in employment we observe.28 While larger than the hours-based calculation, the bottom line from both approaches is that the decline in life expectancy alone, with no change in wages (or disutility of work), cannot account for much of our estimated decline in earnings and employment.
5.2 Insurance coverage for the “insured”
Our findings highlight the nature of insurance against health shocks in the US. Our estimates imply that for 50–59 year olds with health insurance, the impact of a hospital admission on total medical expenses is similar to its impact on earnings in the first few years, while over longer horizons the earnings decline is likely larger than increase in total medical expenses.29 Health insurance in the United States covers over 90 percent of the medical expenses associated with a hospital admission. However, our results suggest that less than 10 percent of the earnings decline associated with the hospital admission is covered for individuals below the age of Social Security eligibility.
In other words, for those who have it, insurance for medical expenses (λm) is fairly comprehensive, while insurance for income declines (λa) is substantially less complete. As a result, the insured have less protection against the economic consequences of health shocks than the cost-sharing provisions of their insurance for medical expenses insurance would imply, and the degree of protection is declining over longer time horizons. For example, we estimate in the MEPS that about 92 percent of the medical expenses in the year following admission (including the medical expenses from the index admission itself) are covered by insurance. However, once earnings consequences are accounted for, only about 80 percent of the total economic costs (total medical expenses plus earnings decline) of the hospital admission in the first year are covered. In the third year after admission, only about 50 percent of costs are covered, reflecting the growing impact on earnings and the declining impact on medical expenses.30
This stands in marked contrast to Fadlon and Nielsen’s (2015) recent findings for Denmark. They analyze the impacts of non-fatal heart attacks and strokes for individuals under 60 and find declines in own earnings that are broadly similar to our estimates - about 15 to 20 percent - and, like us, find little evidence of informal insurance through spousal labor supply. However, they find that almost 50 percent of the earnings decline is insured through social insurance, particularly through sick pay and disability insurance. This underscores the very different nature of insurance against the economic consequences of adverse health events in the two countries.
Welfare implications
Our results indicate that the non-elderly insured still face considerable economic risk from hospital admissions, with the primary source being uninsured earnings consequences rather than uninsured medical expenses. Of course, the welfare implication of a given decline in earnings following a hospital admission need not be the same as the welfare implication of the same change in out-of-pocket spending. Suppose that the individual has no control over the size of the total medical cost shock m, but that she endogenously chooses her hours in response to the size of the wage shock (α1w1 and α2w2). These assumptions correspond to our economic framework in Section 1 and are in the spirit of our empirical strategy based on using hospital admissions as an exogenous shock to medical expenses. In this model, a given change in earnings reduces welfare in inverse proportion to the uncompensated labor supply elasticity, while any out of pocket medical expenses feed through directly (one for one) to welfare reductions.31
A conservative estimate is that the welfare decline associated with the uninsured earnings decline is three times larger than the welfare decline associated with the increase in out-of-pocket spending. To arrive at this estimate we use the upper end of the range of “consensus” estimates of the elasticity of hours with respect to a permanent, unanticipated change in wages, which runs between−0.2 and 0.5 (Keane 2011). Using the upper bound estimate of 0.5, this suggests that, in the first three years, the welfare consequences of the roughly $8,000 average annual decline in net earnings (i.e., the $8,750 decline in average annual earnings net of the $880 increase in social insurance payments) is about three times that of the roughly $1,400 average annual increase in out of pocket medical spending. Moreover, since the net earnings decline appears permanent while the out of pocket spending increase appears front-loaded, we suspect that the relative welfare consequences of the earnings impact may loom larger over larger time horizons. The relative welfare consequences of earnings would also loom larger if - unlike our current model - we allowed some or all of the out-of-pocket spending to be an endogenous choice (involving, for example, a trade-off between the health benefits of medical spending and the foregone utility from non-medical consumption as in Einav et al. 2013b).
Implications for younger, insured adults
Naturally, our results speak directly to the earnings and out-of-pocket medical spending consequences of hospital admissions only for non-elderly insured adults aged 50–59 whom we observe in the HRS. Uninsured earnings risk is likely much smaller at older ages. For individuals aged 60–64 at the time of hospital admission we found similar earnings declines but a much larger share of this insured through their ability to access Social Security Retirement Income. For individuals 65 and older, we found no evidence of earnings declines, presumably reflecting their much lower labor market activity.
Younger, insured adults would have similar (i.e., limited) access to social insurance as our baseline sample of 50–59 year olds, but it is a priori unclear whether to expect larger or smaller earnings effects of hospital admissions. Earnings effects might be smaller at younger ages if the elasticity of labor supply with respect to health shocks is smaller. For example, the substantial exit into retirement that we estimate is presumably more likely at older ages (although the reporting of non-employment as “retirement” is presumably also more common). However, there are two countervailing reasons to expect that earnings effects of hospital admissions could be larger at younger ages. First, hours worked are higher and so the impact of a given change in wages, holding behavior constant, is larger.32 Second, while our stylized model considers only two periods, in practice, the relevant time horizon for potential earnings is larger for younger individuals, so that a given permanent decline in annual earnings would be integrated over a larger number of years of potential earnings.
While we cannot directly examine the impact of hospital admissions on earnings for individuals under age 50, two indirect analyses show no suggestion of smaller earnings effects of hospital admissions at younger ages. First, in the HRS we found similar effects on out of pocket spending and earnings for those aged 50–59 at admission (Table 2) compared to those aged 60–64 (Table 3). Second, in the credit report data, we analyzed the impact of hospital admissions separately for the near-elderly insured (ages 50–59) and compared them to the impacts for the full non-elderly insured sample (ages 25–64). These results, shown in Appendix Tables 29 and 30, indicate similar-sized effects of a hospital admission on credit card limits and borrowing. According to our model, these results are consistent with similar-sized impacts of the hospital admission on income and out-of-pocket medical spending, although of course there could also be offsetting differences.
5.3 Insurance coverage for the “uninsured”
A growing body of recent evidence has suggested that a large share of the nominally uninsured’s medical costs are not, in fact, paid for by the uninsured. As a result, a large share of the incidence of being uninsured may be born by the actors who bear the costs of providing informal insurance to the “uninsured” (Mahoney 2015; Garthwaite, Gross, and Notowidigdo 2015; Finkelstein, Hendren, and Luttmer 2015). Our findings are consistent with this literature.
We find similar impacts of hospital admission on access to credit (i.e., credit limits) and borrowing for the insured and uninsured, with larger impacts for the uninsured limited to impacts on unpaid bills and bankruptcy. A simple comparison of four-year impacts suggests that a hospital admission generates about $6,000 more in unpaid bills for the uninsured than the insured.33 While the uninsured likely experience larger out-of-pocket expenses than the insured (e.g., Finkelstein et al. 2012), the decline in borrowing for the uninsured suggests that the increase in out of pocket spending associated with a hospital admission is still small compared to the reduction in their earnings.
Naturally one must exercise caution in interpreting such comparisons of impacts of hospital admissions on unpaid bills for the insured and uninsured as reflecting the causal effect of insurance per se; there may be other underlying differences between the two groups, such as the nature or severity of the health event (See Appendix Tables 13 and 14). To try to adjust for observable differences between the two groups, Appendix Table 35 shows results for the uninsured re-weighted to make the insured sample on demographics (age, race and gender) and health conditions (diagnosis codes and length of stay); this has little effect on the estimates.
To gain greater insight into the causal effects of insurance, we estimated the impact of insurance coverage using a regression discontinuity (RD) strategy based on the discrete change in health insurance when individuals are covered by Medicare at age 65 (in the spirit of Card, Dobkin, and Maestas 2008, Card, Dobkin, and Maestas 2009, and Barcellos and Jacobson 2015). The RD strategy uses arguably more credible identifying variation than the simple difference-in-differences comparison of the impact of admission for insured relative to uninsured. However, it has much lower power, involves a distinct sample of adults, and requires making an assumption about how to define the “first stage” in terms of the change in insurance coverage (which, as emphasized by Card, Dobkin, and Maestas 2009, may not be limited to the observed, extensive coverage margin). To reduce concerns that insurance coverage may affect the composition of people admitted to the hospital, we restrict the analysis to admissions that occur through the emergency room; this is arguably less discretionary and, consistent with this intuition, we find no statistically or economically significant impact of being 65 on admissions through the ER.
We present the RD results in detail in Appendix E (see especially Appendix Figures 29 and 30, and Appendix Table 36). They are consistent with the difference-in-differences comparison of the impact of hospital admissions for uninsured and insured non-elderly adults: we find a statistically significant impact of consumer cost sharing on unpaid medical bills, but no impacts on credit limits or borrowing (although the latter are sufficiently noisy that we are unable to rule out large effects). The RD evidence that insurance reduces the impact of hospital admissions on unpaid bills is also consistent with existing evidence that health insurance reduces measures of financial risk exposure and financial strain (Finkelstein and McKnight 2008; Engelhardt and Gruber 2011; Finkelstein et al. 2012; Baicker et al. 2013; Mazumder and Miller 2014; Barcellos and Jacobson 2015).34
The welfare consequences of the reduction in unpaid medical bills associated with health insurance coverage is less clear. The unpaid medical bills we measure (medical collections) are, for the most part, ultimately never paid (Avery, Calem, and Canner 2003). In our model, any impact of increased u on patient welfare is indirect; an increase in u raises welfare insofar as unpaid medical bills allow for increased consumption following the health shock, and decreases welfare insofar as it increases future borrowing costs r. Of course, in practice, there may also be other unmeasured and un-modeled channels by which u directly affects patient welfare, such as impacts of u on “peace of mind” (Mann and Porter 2010).
5.4 Medical bankruptcy
A growing empirical literature examines the impact of various economic shocks on consumer bankruptcy (e.g., Domowitz and Sartain 1999; Sullivan, Warren, and Westbrook 1999; Fay, Hurst, and White 2002; Warren and Tyagi 2003; Livshits, MacGee, and Tertilt 2007; Keys 2010). A controversial, high-profile strain of this literature has examined the role of “medical bankruptcies”. A study by Hummelstown et al. (2005) interviewing bankruptcy filers regarding the cause of their bankruptcy found that 54 percent of bankruptcy filers self-reported “medical causes” as the reason for their bankruptcy. Follow-on studies using this same basic method but varying in their definition of a “medical cause” have estimated rates of “medical bankruptcy” ranging from 17 percent (Drano and Millen son 2006) to 62 percent (Hummelstown et al. 2009). These findings have attracted a great deal of attention from journalists, politicians, and policymakers (e.g., Obama 2009). However, self-reported “causes” among those who go bankrupt can be difficult to interpret. More promisingly, recent research by Morrison et al. (2013) and Gupta et al. (2014) has performed event study analyses of the relationship between an adverse health shock and subsequent consumer bankruptcy, using a census of non-fatal automobile crashes in Utah and cancer diagnoses in 11 counties in western Washington State, respectively. However, both papers are unable to reject the null hypothesis of no causal effect of the medical event analyzed on bankruptcy.
Relative to this existing literature, our results provide evidence of a statistically significant impact of hospital admissions on bankruptcies - for both insured and uninsured non-elderly adults but not for the elderly. Figure 5 shows these results visually; the corresponding estimates are in Table 6. Four years later, a hospital admission increases bankruptcy rates by 0.4 percentage points for the insured non-elderly and 1.4 percentage points for the uninsured non-elderly; hospital admissions have no effect on bankruptcy for the elderly. A larger impact of hospital admissions on bankruptcy for the uninsured is consistent with Gross and Notowidigdo (2011) and Mazumder and Miller (2014)’s findings that health insurance reduces the risk of bankruptcy.
However, our results suggest that the share of “medical bankruptcies” may be lower than the prior literature has concluded. Our estimates imply that hospital admissions are pivotal for about 4 percent of bankruptcies for non-elderly insured adults and 6 percent of bankruptcies for non-elderly uninsured adults, and do not contribute to bankruptcies for the elderly.35 This is likely a lower bound on the total number of medically-induced bankruptcies since it excludes index medical events not associated with a hospital admission. However, hospital admissions (and their sequelae) are likely a major cause of medical bankruptcies. Hospital spending alone is about 40 percent of total medical spending, and among individuals in the top 5 percent of annual medical spending, two-thirds have had a hospital admission in the last year; for those in top percentile of annual medical spending, almost 90 percent had a hospital admission (authors’ calculations from MEPS).
6 Conclusion
The United States has recently engaged in a major expansion of public and private health insurance for non-elderly adults. This health insurance covers a substantial portion of medical expenses, but does not provide coverage for potential earnings losses from poor health. Using two complementary panel data sets, we have explored the economic consequences of hospital admissions for non-elderly adults with health insurance. Our findings suggest that non-elderly insured adults still face considerable exposure to adverse economic consequences of hospital admissions through their impact on labor earnings. We estimate an earnings decline associated with hospital admissions that is similar to the existing estimates of the earnings consequences of job displacement (Jacobson, LaLonde, and Sullivan 1993). We find the earnings declines are only minimally insured before adults are eligible for Social Security Retirement Income.
We also find that the nominally uninsured face similar economic risks from hospital admissions despite their lack of formal insurance, due to their ability to simply not pay large portions of their medical costs, and that hospital admissions contribute to less than five percent of bankruptcies; the former finding is consistent with a growing literature on substantial informal insurance for the “uninsured”, while the latter finding suggests that “medical bankruptcies” are quantitatively much less common than existing studies have concluded.
Taken together, our findings underscore the nature of insurance - and the lack thereof - in the United States. Our estimates suggest that in the first few years, the total medical expense and earnings consequences of a hospital admission are similar for insured adults and that over a longer horizon the earnings consequences loom relatively larger. By design, insurance in the US covers (a large portion of) medical expenses but relatively little of the earnings decline. Employer provision of sick pay and private disability insurance is fairly sparse, and public disability insurance is available only after a lengthy application and approval process (Autor et al. 2015). By contrast, in many other countries, there is substantially more formal insurance for the labor market consequences of adverse health. For example, in Germany, an overnight hospital stay automatically produces wage replacement benefits from the Social Insurance System (Jager 2015); in Denmark, mandatory sick-pay benefits from employers combined with public and private disability insurance covers most of the adverse earnings consequences of a non-fatal health event (Fadlon and Nielsen 2015). On the other hand, for those lacking formal health insurance in the US, there appears to be fairly extensive informal insurance operating through unpaid bills.
Our analysis throughout this paper has been primarily descriptive, and additional assumptions are required for drawing inferences about consumer welfare or optimal insurance design. For example, while our results would suggest that hospital admissions are associated with consumption declines for non-elderly insured adults, if the marginal utility of consumption is lower in poor health (Finkelstein, Luttmer, and Notowidigdo 2013), then some decline in consumption is (ex ante) optimal. Moreover, in the presence of moral hazard effects of insurance, on health care utilization and/or labor market activity, the (constrained) optimal level of insurance would not involve fully equating marginal utility of consumption across health states. The descriptive facts in this paper should be useful for calibrating economic models that can more precisely quantify the welfare costs of adverse health shocks that lead to hospitalizations.
Supplementary Material
Acknowledgments
We thank Betty Henderson-Sparks, Bill Murphy, and Jonathan Teague for their assistance with preparing, merging, and getting access to the data sets used in this project. We thank David Cutler, Itzik Fadlon, Matthew Gentzkow, Larry Katz, Erzo Luttmer, Brigitte Madrian, Jesse Shapiro, Heidi Williams, four anonymous referees, Hilary Hoynes (the Editor), and numerous seminar participants for helpful comments. We thank Allyson Barnett and Rene Leal Vizcaino for extremely valuable research assistance. We gratefully acknowledge funding from the National Institute on Aging P01AG005842 and R01 AG032449 (Finkelstein). This material is based upon work supported by the National Science Foundation Graduate Research Fellowship under Grant No. 1122374 (Kluender).
Footnotes
See http://www.presidency.ucsb.edu/ws/?pid=27123, last accessed July 2, 2015.
We show in Appendix A that our main results obtain in an alternative model where health shocks increase the disutility of hours worked rather than reduce the wage.
For ease of exposition, our definition implies that λm = λα = 1 provides “full coverage”. Naturally equating consumption across states is not equivalent to full insurance (equating marginal utility of consumption across states), as the marginal utility of consumption may vary with health (Finkelstein, Luttmer, and Notowidigdo 2013).
To ensure sufficient sample sizes for important sub-samples, we over-sampled certain types of admissions. In all of our analyses, we weight each individual by the inverse of their probability of being sampled.
There is insufficient sample to analyze consumption in the HRS, which is measured for only a small subset of individuals and survey waves.
We are unable to identify or link spouses in either the hospital data or the credit report data.
We informally interpret consumer bankruptcy as an extreme case of “unpaid bills”. For a formal model of personal bankruptcy, see Wang and White (2000).
Our earnings measure includes both labor market earnings and self-employment income, although it may undercount self-employment income that instead gets classified as “business or capital income” (see Appendix B.1.2 for more details). In Appendix Table 8 we show that the decline in earnings primarily reflects a decline in labor market earnings.
We find no evidence of a change in log wages conditional on working, but the estimates are imprecise and would be difficult to interpret regardless because of potential compositional effects.
We might expect spousal earnings to increase due to the income effect from the decline in respondent earnings, or to decline if spousal leisure is a complement to poor health. Consistent with the presence of such offsetting effects, Fadlon and Nielsen (2015) find in Denmark that spousal earnings increase substantially following a spouse’s death, but exhibit a (statistically significant but economically modest) decline following a spouse’s severe - but non-fatal - health shock.
Appendix Table 11 and Appendix Figure 10 provide more detail on the components of the increase in social insurance payments to the household. We examine separately each payments from each social insurance program we can measure in the HRS: Unemployment Insurance income, and three types of Social Security income: Disability Insurance (SSDI), Supplemental Security Income (SSI), and Retirement Income (SSRI). There is no evidence of an increase in unemployment insurance income following a hospital admission; the increase in social insurance payments reflects an income in Social Security Income. It appears to reflect an increase in both SSDI and SSRI, with about two-thirds of the increase coming from the latter. However, by construction, our sample consists of individuals who will not be age eligible for SSRI during the three years post admission. It is possible that some may have spouses who are eligible, but given the lack of a change in earnings of spouses and the fact that mean reported Social Security Retirement Income is non-zero at ages below 62 even for single individuals in the HRS, we suspect there is some noise in the data in attributing benefits to Social Security Retirement Income as opposed to other Social Security benefits such as disability insurance and survivor benefits. The HRS document supports the idea of some measurement error in the distinction among types of Social Security benefits (Chien et al. 2015, see especially pages 734 forward on measuring SSI and SSDI, and pages 748 forward on measuring SSRI).
Total household income is measured as the sum of the components shown in Table 2- respondent earnings, spousal earnings, and household social insurance payments - plus household pension and annuity income; Appendix Table 9 and Appendix Figure 8 show estimated effects on household pension and annuity income. We exclude household capital and business income and “other household income” from our baseline household income measure because they appear to be quite noisy. However, Appendix Table 9 and Appendix Figure 8 show estimated effects for these two components, as well as estimated effects on an alternative measure of total household income which includes them.
The share of earnings decline insured would be even larger (over 80 percent) if one considered only the declines in respondent earnings. However, for 60–64 year olds there are statistically imprecise but quantitatively non-trivial and same sized declines in spousal earnings, which we include in our measure of the earnings decline.
For many of the outcomes, there is visual evidence of a cyclical pattern to the non-parametric event study coefficients. The pattern is particularly pronounced post hospitalization, but also visible pre admission for some outcomes. This appears to reflect systematic variation in our sample by admission month since, recall, we observe each individual once every 12 months. The fact that that pattern is more pronounced post-hospitalization and (as we will see in the robustness analysis below) is usually still present after the inclusion of individual fixed effects suggests that the variation across admission months primarily reflects variation in treatment effect rather than mean outcome levels. Thus, the point estimates from our spline regressions should be viewed as an average of the impact of hospitalization across the groups admitted to the hospital in different months.
While we can be fairly confident that “medical” collections reflect unpaid medical bills, the converse is less clear. Non-medical collections may reflect non-payment of non-medical bills (such as utility bills). But they may also reflect unpaid medical bills; for example, a medical bill that is charged to a credit card whose balances are then not paid would show up as a non-medical collection.
Not everyone has a credit score; 96 percent of our sample has a credit score prior to hospitalization. We therefore examined the impact of hospital admissions on the probability of having a credit score (see Appendix Table 34). A hospital admission is associated with a statistically significant decline of 0.28 percentage points in the probability of having a credit score after 48 months.
Bethune (2015) examines people who lose their job between 2007 and 2009, and estimates that unemployment is associated with a decline in credit card limits of $925 by 2009. By comparison, we estimate that a hospital admission associated with a $500 decline in credit limits 12 months later.
Recent estimates suggest that, on average, a 100 point decline in credit score is associated with an increase in interest rates (r) of 100 to 300 basis points (Agarwal et al. 2015a, Han, Keys, and Li 2015).
The larger effect on credit limits may also reflect differences in how these instruments are used as screening devices for borrowers; indeed, consistent with our findings, Agarwal et al. (2015a) find that credit card companies will often impose large changes in borrowing limits without meaningful changes in interest rates as a function of credit score.
The results for the uninsured on credit scores (Table 6 column 3 and Appendix Figure 17) are somewhat puzzling - suggesting a similar proportional decline to the insured at 12 months but a statistically significant increase at 48 months. However, given the potential endogeneity of presence of a credit score, we urge some caution in interpreting these results. As noted above, only 84 percent of the uninsured sample has a credit score prior to hospitalization. We find that a hospital admission is associated with a statistically significant decline of 0.85 percentage points in the probability of having a credit score after 48 months (see Appendix Table 34).
The declines for the uninsured may be mechanically dampened by the relatively large share with zero credit limits and credit card balances (50 percent, compared to about 20 percent for the insured; see Appendix Table 15). However, at higher quantiles where such censoring is less of a concern, the pattern of results across quantiles look similar to that for the insured; impacts for the uninsured are similar at the 75th percentile compared to the mean, and estimated effects at 90th percentile are roughly three times larger than the effects at the mean (see Appendix Table 32).
Appendix Tables 33 and 31 present the corresponding robustness analysis for the elderly and the non-elderly uninsured.
Specifically, we regress an indicator variable for whether the individual died by the end of our sample (January 2011) on a full set of age-in-years-at-admission dummies and one’s primary diagnosis-related group (DRG) at admission; we observe almost 500 different DRGs.
Non-deferrable hospital admissions are limited to the subset of admissions that originate through the ED and have an ICD-9 code as the primary diagnosis that has weekend to weekday frequencies closest to the 2:5 ratio that we would expect if there is no delay in care.
In the 2000–2011 CPS, we estimate labor force participation rates in California of 85 percent and 40 percent for the privately insured and Medicaid recipients, respectively. In the 1999–2010 MEPS, we estimate only slightly lower consumer cost sharing for those covered by Medicaid (6.7 percent compared to 8.8 percent for the privately insured); see Appendix Table 37.
Naturally, there are other differences between the elderly and non-elderly insured adults that could also contribute to the differential impacts of hospital admissions observed in the credit report data. In particular, there may be important differences in the nature of their insurance and the nature and severity of their hospital admissions. Appendix Tables 13 and 14 provide some descriptive information regarding differences in severity; not surprisingly, the health shock appears more severe for the elderly (as measured by list charges or length of stay for the index admission). Indeed, as we show in Appendix Table 35, when we re-weight the elderly sample to match the non-elderly insured sample on demographics (race and gender) and health conditions (diagnosis codes and length of stay), the results for the elderly become smaller. Another comparability issue is that credit report measures may proxy for different things in differnet populations. After a hospitalization elderly retirees may finance consumption by drawing down savings rather than taking on debt, and the uninsured may rely less on formal credit markets and more on other sources of liquidity. We are not able to observe changes in wealth or savings behavior directly, but the lack of change in credit report measures for the elderly is consistent with lack of change in total income that we find in the HRS data.
For this calibration exercise, we use the estimates from the US Life Tables that expected remaining life at 56 (the average age of a hospital admission in our HRS sample) is 26.2 years, and 3-year mortality is 2.0% (Arias, Rostron, and Tejada-Vera 2010). In the HRS we estimate a 3-year post admission mortality rate of 3.8%. To allow for the maximal possible effect of life expectancy changes, we assume that all of the elevation in mortality post admission relative to the national average reflects the impact of the hospital admission. To convert this elevated three-year mortality rate into a change in life expectancy we consider two alternative assumptions: (1) the increased annual mortality risk due to hospital admission is limited to the the first 36 months post admission, and (2) the change in annual mortality risk due to hospital admission is permanent and equal to the average change during the first 36 months. These two assumptions suggest that hospital admissions result in a 2.8 to 9.2 percent decline in life expectancy. Thus, if the entire earnings response came through changes in life expectancy (without any change in wage), this would imply a 0.1 to 0.5 percent decline in earnings
Bloom, Canning, and Moore (2014)’s estimates suggest that the decline in life expectancy due to a hospital admission that we calculated in footnote 27 would produce a 1 to 4 percent decline in the retirement age. If we assume everyone’s life expectancy and retirement age shift by the same number of years, and use the mean (standard deviation) of retirement ages from the HRS of 66 (9), and assume a normal distribution of retirement ages as an approximation, then this would suggest an increase in the probability of retirement 36 months after hospital admission of 0.4 to 1.5 percentage points - compared to the extensive labor market effects we found at three years of 10–11 percentage points (based on “full or part time work” in Table 2 or self-reported retirement in Appendix Table 10). This suggests that life expectancy might be able to explain up to 15 percent of the decline in employment we observe.
We estimate in the MEPS that the average co-insurance for insured non-elderly adults for medical expenses in the year including and following the admission is about 8 percent. Given our estimated average annual increase in out of pocket medical spending of about $1,500 in the first three years, this implies average annual total medical expenses (m) associated with the hospital admission of about $18,750 in the first three years. By comparison, we estimate average annual declines in earnings of about $9,000 over the first few years, and these effects, unlike the out of pocket spending effects, do not appear to decline over time.
These calculations are based on estimates of the impact of the admission on out-of-pocket spending, earnings and social insurance payments from Table 2. We assume based on our calculation in the MEPS (see Appendix B.3) that 92 percent of the incurred medical expenses are covered, and we assume based on our estimate from Table 2 that 10 percent of the earnings loss is covered.
See Appendix A for details. There, we show that a first-order approximation to the money-metric change in utility from a health shock is , where εh,w = dlog(h)/dlog(w) is the uncompensated labor supply elasticity and g′(c1) is the marginal utility of consumption in the first period. If there is a non-zero income effect in labor supply, then Appendix A shows this first-order approximation is an upper bound on change in utility, since out-of-pocket medical costs represent a negative shock to unearned income. This bound will be tight if income effects are small, which is likely the case given the relatively small increase in out of pocket spending, and income effects on labor supply which tend to be small relative to labor supply elasticities (see e.g., Imbens, Rubin, and Sacerdote 2001 and Cesarini et al. forthcoming)
Employment rates are 79 percent for 25–49 year olds compared to 74 percent of 50–59, according to the 2000–2011 pooled March CPS.
Of course, unpaid bills may be based on charges (not hospital costs), which complicates the interpretation of the impact of insurance on unpaid bills, since charges (prices) may differ by insurance status. Beyond this measurement issue, many hospitals also may provide charity care to the uninsured, which we are not able observe in our data. Using data from the American Hospital Association, Garthwaite, Gross, and Notowidigdo (2015) note that the total amount of uncompensated care provided by hospitals is roughly evenly split between charity care and bad debt, which suggests that the $6,000 is likely a lower bound on the costs paid by external parties for average hospital admission for non-elderly uninsured in our data. This is consistent with the breakdown of spending for uninsured that we observe in the MEPS data, which suggests that total charges for average hospitalization for uninsured is $24,000, with $1,300 of that paid out of pocket (see Appendix Table 37).
Most closely related to the empirical strategy we implement in Appendix E is recent work using the discontinuity in insurance coverage at age 65 when Medicare eligibility begins to examine the impact of Medicare on out-of-pocket spending and medical-related financial strain in survey data (Barcellos and Jacobson 2015).
In the MEPS, we estimate an annual non-childbirth household hospitalization rate of 8.2 percent for insured adults, and 3.5 percent for uninsured adults. (We use the household adult hospitalization rate since bankruptcy is a household-level event and any adult in the house can have a hospitalization that potentially contributes to the household’s bankruptcy. We ignore hospitalizations for children. We estimate a 0.8 percent annual household bankruptcy rate for the non-elderly by combining Census population estimates with the distribution of bankruptcy filers by age, which is compiled by the Department of Justice U.S. Trustee Program (www.justice.gov/ust). Since the pre-hospitalization bankruptcy rate is similar in our insured and uninsured samples, we assume that the bankruptcy rate is similar in the overall population of insured and uninsured non-elderly adults, as well. This is consistent with the results in Stavins (2000), which shows that the health insurance rates are similar between bankruptcy filers and non-filers.
Any opinion, findings, and conclusions or recommendations expressed in this material are those of the authors(s) and do not necessarily reflect the views of the National Science Foundation.
The authors declare that they have no relevant or material financial interests that relate to the research described in this paper.
Notowidigdo dedicates this paper to his friend Arijit Guha.
Contributor Information
Carlos Dobkin, University of California Santa Cruz, 1156 High Street, Santa Cruz, CA 95064, and NBER.
Amy Finkelstein, Department of Economics, MIT, 77 Massachusetts Avenue, Cambridge, MA 02139, and NBER.
Raymond Kluender, Department of Economics, MIT, 77 Massachusetts Avenue, Cambridge, MA 02139.
Matthew J. Notowidigdo, Department of Economics, Northwestern, 2211 Campus Drive, Evanston, IL 60208, and NBER
References
- 1.Agarwal Sumit, Chomsisengphet Souphala, Mahoney Neale, Stroebel Johannes. Do Banks Pass Through Credit Expansions to Consumers Who Want to Borrow? Quarterly Journal of Economics. forthcoming. [Google Scholar]
- 2.Agarwal Sumit, Amromin Gene, Chomsisengphet Souphala, Piskorski Tomasz, Seru Amit, Yao Vincent. Mortgage Refinancing, Consumer Spending, and Competition: Evidence from the Home Affordable Refinancing Program. Columbia Business School. 2015b Aug 30; [Google Scholar]
- 3.Arias Elizabeth, Rostron Brian L, Tejada-Vera Betzaida. United States Life Tables, 2005. National Vital Statistics Reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. 2010;58(10):1–132. [PubMed] [Google Scholar]
- 4.Attanasio Orazio P, Hoynes Hilary Williamson. Differential mortality and wealth accumulation. Journal of Human Resources. 2000;35(1):1–29. [Google Scholar]
- 5.Autor David H, Maestas Nicole, Mullen Kathleen J, Strand Alexander. Does Delay Cause Decay? The Effect of Administrative Decision Time on the Labor Force Participation and Earnings of Disability Applicants. NBER Working Paper No. 20840. 2015 [Google Scholar]
- 6.Avery Robert B, Calem Paul S, Canner Glenn B. An Overview of Consumer Data and Credit Reporting. Federal Reserve Bulletin. 2003 Feb;:47–73. [Google Scholar]
- 7.Baicker Katherine, Taubman Sarah L, Allen Heidi L, Bernstein Mira, Gruber Jonathan H, Newhouse Joseph P, Schneider Eric C, Wright Bill J, Zaslavsky Alan M, Finkelstein Amy N. The Oregon Experiment—Effects of Medicaid on Clinical Outcomes. New England Journal of Medicine. 2013;368(18):1713–1722. doi: 10.1056/NEJMsa1212321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baily Martin Neil. Some aspects of optimal unemployment insurance. Journal of Public Economics. 1978;10(3):379–402. [Google Scholar]
- 9.Barcellos Silvia Helena, Jacobson Mireille. The Effects of Medicare on Medical Expenditure Risk and Financial Strain. American Economic Journal: Economic Policy. 2015;7(4):41–70. doi: 10.1257/pol.20140262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bethune Zachary. Consumer Credit, Unemployment, and Aggregate Labor Market Dynamics. Working Paper. 2015 [Google Scholar]
- 11.Black Sandra E, Devereux Paul J, Salvanes Kjell G. Losing heart? The effect of job displacement on health. ILR Review. 2015;68(4):833–861. [Google Scholar]
- 12.Bloom David E, Canning David, Moore Michael. Optimal retirement with increasing longevity. The Scandinavian Journal of Economics. 2014;116(3):838–858. doi: 10.1111/sjoe.12060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Caminal Josefina, Starfield Barbara, Sánchez Emilia, Casanova Carmen, Morales Marianela. The role of primary care in preventing ambulatory care sensitive conditions. The European Journal of Public Health. 2004;14(3):246–251. doi: 10.1093/eurpub/14.3.246. [DOI] [PubMed] [Google Scholar]
- 14.Card David, Dobkin Carlos, Maestas Nicole. The Impact of Nearly Universal Insurance Coverage on Health Care Utilization. The American Economic Review. 2008;98(5):2243–58. doi: 10.1257/aer.98.5.2242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Card David, Dobkin Carlos, Maestas Nicole. Does Medicare Save Lives? The Quarterly Journal of Economics. 2009;124(2):597–636. doi: 10.1162/qjec.2009.124.2.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cesarini David, Lindqvist Erik, Notowidigdo Matthew J, Ostling Robert. The Effect of Wealth on Individual and Household Labor Supply: Evidence from Swedish Lotteries. The American Economic Review. forthcoming. [Google Scholar]
- 17.Charles Kerwin Kofi. The Longitudinal Structure of Earnings Losses among Work-Limited Disabled Workers. Journal of Human Resources. 2003:618–646. [Google Scholar]
- 18.Chien Sandy, Campbell Nancy, Chan Chris, Hayden Orla, Hurd Michael, Main Regan, Mallett Joshua, Martin Craig, McCullough Colleen, Meijer Erik, Moldoff Michael, Pantoja Philip, Rohwedder Susann, St Clair Patricia. RAND HRS Data Documentation, Version O. Labor & Population Program, RAND Center for the Study of Aging. 2005:1–1277. [Google Scholar]
- 19.Chung YoonKyung. Chronic Health Conditions and Economic Outcomes. Unpublished mimeo. 2013 http://www.sole-jole.org/14225.pdf.
- 20.Cochrane John H. A Simple Test of Consumption Insurance. Journal of Political Economy. 1991:957–976. [Google Scholar]
- 21.Cutler David, Meara Ellen, Richards-Shubik Seth. Health Shocks and Disability Transitions Among Near-elderly Workers. NBER Retirement Research Center Paper No NB 11-08. 2011 http://www.nber.org/aging/rrc/papers/orrc11-08.
- 22.Dobkin Carlos, Finkelstein Amy, Kluender Raymond, Notowidigdo Matthew J. The Economic Consequences of Hospital Admissions. NBER Working Paper 22288 2016 [Google Scholar]
- 23.Domowitz Ian, Sartain Robert L. Determinants of the Consumer Bankruptcy Decision. The Journal of Finance. 1999;54(1):403–420. [Google Scholar]
- 24.Drano David, Millen son Michael L. Medical Bankruptcy: Myth versus Fact. Health Affairs. 2006;25(2):w74–w83. doi: 10.1377/hlthaff.25.w74. [DOI] [PubMed] [Google Scholar]
- 25.Einav Liran, Jenkins Mark, Levin Jonathan. The impact of credit scoring on consumer lending. The RAND Journal of Economics. 2013a;44(2):249–274. [Google Scholar]
- 26.Einav Liran, Finkelstein Amy, Schrimpf Paul, Ryan Stephen, Cullen Mark. Selection on moral hazard in health insurance. The American Economic Review. 2013b;103(1):178–219. doi: 10.1257/aer.103.1.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Engelhardt Gary V, Gruber Jonathan. Medicare Part D and the Financial Protection of the Elderly. American Economic Journal: Economic Policy. 2011;3(4):77–102. [Google Scholar]
- 28.Fay Scott, Hurst Erik, White Michelle J. The Household Bankruptcy Decision. The American Economic Review. 2002;92(3):706–718. [Google Scholar]
- 29.Fadlon Itzik, Nielsen Torben Heien. Household responses to severe health shocks and the design of social insurance. NBER Working Paper No. 21352. 2015 [Google Scholar]
- 30.Finkelstein Amy, Hendren Nathan, Luttmer Erzo FP. The Value of Medicaid: Interpreting Results from the Oregon Health Insurance Experiment. NBER Working Paper 21308. 2015 doi: 10.1086/702238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Finkelstein Amy, Luttmer Erzo FP, Notowidigdo Matthew J. Approaches to Estimating the Health State Dependence of the Utility Function. The American Economic Review. 2009;99(2):116–121. [Google Scholar]
- 32.Finkelstein Amy, Luttmer Erzo FP, Notowidigdo Matthew J. What Good is Wealth Without Health? The Effect of Health on the Marginal Utility of Consumption. Journal of the European Economic Association. 2013 Jan;11(S1):221–258. [Google Scholar]
- 33.Finkelstein Amy, McKnight Robin. What did Medicare do? The Initial Impact of Medicare on Mortality and Out of Pocket Medical Spending. Journal of Public Economics. 2008;92(7):1644–1668. [Google Scholar]
- 34.Finkelstein Amy, Taubman Sarah, Wright Bill, Bernstein Mira, Gruber Jonathan, Newhouse Joseph P, Allen Heidi, Baicker Katherine. The Oregon Health Insurance Experiment: Evidence from the First Year. The Quarterly Journal of Economics. 2012;127(3):1057–1106. doi: 10.1093/qje/qjs020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Garthwaite Craig, Gross Tal, Notowidigdo Matthew J. Hospitals as Insurers of Last Resort. American Economic Journal: Applied Economics. forthcoming. [Google Scholar]
- 36.Gross Tal, Notowidigdo Matthew J. Health Insurance and the Consumer Bankruptcy Decision: Evidence from Expansions of Medicaid. Journal of Public Economics. 2011;95(7):767–778. [Google Scholar]
- 37.Gupta Arpit, Morrison Edward, Fedorenko Catherine, Ramsey Scott. Health and Financial Fragility: Evidence from Car Crashes and Consumer Bankruptcy. Unpublished mimeo. 2014 https://static1.squarespace.com/static/56086d00e4b0fb7874bc2d42/t/56088823e4b062e5cb9a2ef8/38.
- 38.Gupta Arpit, Morrison Edward, Fedorenko Catherine, Ramsey Scott. Cancer Diagnoses and Household Debt Overhang. Columbia Law and Economics Working Paper. 2015;514 [Google Scholar]
- 39.Han Song, Keys Benjamin J, Li Geng. Information, Contract Design, and Unsecured Credit Supply: Evidence from Credit Card Mailings. Working Paper. 2015 [Google Scholar]
- 40.Hummelstown David U, Thorne Deborah, Warren Elizabeth, Woolhandler Steffie. Illness and Injury as Contributors to Bankruptcy. Health Affairs. 2005;24:W5–63. doi: 10.1377/hlthaff.w5.63. [DOI] [PubMed] [Google Scholar]
- 41.Hummelstown David U, Thorne Deborah, Warren Elizabeth, Woolhandler Steffie. Medical Bankruptcy in the United States, 2007: Results of a National Study. The American Journal of Medicine. 2009;122(8):741–746. doi: 10.1016/j.amjmed.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 42.Imbens Guido W, Rubin Donald B, Sacerdote Bruce I. Estimating the Effect of Unearned Income on Labor Earnings, Savings, and Consumption: Evidence from a Survey of Lottery Players. American Economic Review. 2001;91(4):778–94. [Google Scholar]
- 43.Jacobson Louis S, LaLonde Robert J, Sullivan Daniel G. Earnings Losses of Displaced Workers. The American Economic Review. 1993;83(4):685–709. [Google Scholar]
- 44.Jager Simon. How Substitutable Are Workers? Evidence from Worker Deaths. Unpublished Harvard Mimeo. 2015 Available at http://scholar.harvard.edu/files/jaeger/files/jmpsimon.pdf.
- 45.Keane Michael P. Labor Supply and Taxes: A Survey. Journal of Economic Literature. 49(4):961–1075. [Google Scholar]
- 46.Keys Benjamin J. The Credit Market Consequences of Job Displacement. Federal Reserve Board Finance and Economics Discussion Series #2010–24. 2010 Mar; [Google Scholar]
- 47.Livshits Igor, MacGee James, Tertilt Michèle. Consumer Bankruptcy: A Fresh Start. The American Economic Review. 2007;97(1):402–418. [Google Scholar]
- 48.Ljungqvist Lars, Sargent Thomas. Recursive Macroeconomic Theory. 2 Cambridge, MA: MIT Press; 2004. [Google Scholar]
- 49.Mahoney Neale. Bankruptcy as Implicit Health Insurance. The American Economic Review. 2015;105(2):710–746. doi: 10.1257/aer.20131408. [DOI] [PubMed] [Google Scholar]
- 50.Mann Ronald J, Porter Katherine. Saving Up For Bankruptcy. Georgetown Law Journal. 2010;98(2):289–339. [Google Scholar]
- 51.Mazumder Bhashkar, Miller Sarah. The Effects of Massachusetts Health Reform on Financial Distress. American Economic Journal: Economic Policy. forthcoming. [Google Scholar]
- 52.Meyer Bruce, Mok Wallace. Disability, Earnings, Income and Consumption. NBER Working Paper 18869. 2013 [Google Scholar]
- 53.Mian Atif, Rao Kamalesh, Sufi Amir. Household Balance Sheets, Consumption, and the Economic Slump. The Quarterly Journal of Economics. 2013;128(4):1687–1726. [Google Scholar]
- 54.Morrison Edward R, Gupta Arpit, Olson Lenora, Cook Lawrence, Keenan Heather. Health and Financial Fragility: Evidence from Car Crashes and Consumer Bankruptcy. University of Chicago Coase-Sandor Institute for Law & Economics Research Paper. 2013;655:13–81. [Google Scholar]
- 55.Obama Barack. Obama’s Remarks at the White House Health Care Forum. New York Times. 2009 Mar 5; http://www.nytimes.com/2009/03/05/us/politics/05obama-text.html.
- 56.Nielsen Torben Heien. The Relationship between Self-Rated Health and Hospital Records. Health Economics. 2016;25:497–512. doi: 10.1002/hec.3167. [DOI] [PubMed] [Google Scholar]
- 57.Pauly Mark V. The economics of moral hazard: comment. The American Economic Review. 1968;58(3):531–537. [Google Scholar]
- 58.Poterba James M, Venti Steven F, Wise David A. The asset cost of poor health. The Journal of the Economics of Ageing. 2017;9:172–184. [Google Scholar]
- 59.Restuccia Diego, Vandenbroucke Guillaume. A century of human capital and hours. Economic Inquiry. 2013;51(3):1849–1866. [Google Scholar]
- 60.Smith James P. Healthy Bodies and Thick Wallets: The Dual Relation between Health and Economic Status. The Journal of Economic Perspectives. 1999;13(2):144–166. [PMC free article] [PubMed] [Google Scholar]
- 61.Smith James P. Consequences and Predictors of New Health Events. In: Wise David., editor. Analyses in the Economics of Aging. University of Chicago Press; 2005. [Google Scholar]
- 62.Stavins Joanna. Credit card borrowing, delinquency, and personal bankruptcy. New England Economic Review. 2000:15–30. [Google Scholar]
- 63.Sullivan James, von Wachter Till. Job Displacement and Mortality: An Analysis using Administrative Data. Quarterly Journal of Economics. 2009;124(3):1265–1306. [Google Scholar]
- 64.Sullivan Teresa A, Warren Elizabeth, Westbrook Jay Lawrence. As we forgive our debtors: Bankruptcy and consumer credit in America. Beard Books; 1999. [Google Scholar]
- 65.Viscusi W Kip, Evans William N. Utility functions that depend on health status: estimates and economic implications. The American Economic Review. 1990;80(3):353–374. [Google Scholar]
- 66.Wang Hung-Jen, White Michelle J. An Optimal Personal Bankruptcy System and Proposed Reforms. Journal of Legal Studies. 2000;29(1):255–286. [Google Scholar]
- 67.Warren Elizabeth, Tyagi Amelia Warren. The Two-Income Trap: Why Families Went Broke When Mothers Went to Work. Basic Books; 2003. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.