Abstract
Background
Elevated tibiofemoral and patellofemoral loading in children who exhibit crouch gait may contribute to skeletal deformities, pain, and cessation of walking ability. Surgical procedures used to treat crouch frequently correct knee extensor insufficiency by advancing the patella. However, there is little quantitative understanding of how the magnitudes of crouch and patellofemoral correction affect cartilage loading in gait.
Methods
We used a computational musculoskeletal model to simulate the gait of twenty typically developing children and fifteen cerebral palsy patients who exhibited mild, moderate, and severe crouch. For each walking posture, we assessed the influence of patella alta and baja on tibiofemoral and patellofemoral cartilage contact.
Results
Tibiofemoral and patellofemoral contact pressures during the stance phase of normal gait averaged 2.2 and 1.0 MPa. Crouch gait increased pressure in both the tibofemoral (2.6–4.3 MPa) and patellofemoral (1.8–3.3 MPa) joints, while also shifting tibiofemoral contact to the posterior tibial plateau. For extended-knee postures, normal patellar positions (Insall-Salvatti ratio 0.8 – 1.2) concentrated contact on the middle third of the patellar cartilage. However, in flexed knee postures, both normal and baja patellar positions shifted pressure toward the superior edge of the patella. Moving the patella into alta restored pressure to the middle region of the patellar cartilage as crouch increased.
Conclusions
This work illustrates the potential to dramatically reduce tibiofemoral and patellofemoral cartilage loading by surgically correcting crouch gait, and highlights the interaction between patella position and knee posture in modulating the location of patellar contact during functional activities.
Keywords: Cerebral Palsy, Knee Mechanics, Patellofemoral Joint, Patella Baja, Cartilage Contact Pressure
Introduction
Crouch gait is a common abnormality in cerebral palsy, with the primary feature being excessive knee flexion during the stance phase of gait. This form of walking is physically demanding, and is often associated with patellofemoral pain [1–4]. While it is generally thought that the pain is due to large mechanical demands placed on the patellofemoral joint in crouch [2], there are no prior investigations of the patellofemoral contact pressures during crouched walking. Further, patella alta (i.e. a superiorly displaced patella) is nearly universal in those with crouch [4,5], and an imaging study has suggesteda relationship between the degree of patella alta and patellofemoral pain [6]. Hence, the relationship between alta, crouch, and patellofemoral pressures is important to explore.
Tibiofemoral cartilage loading is also important to consider in children with crouch gait. Prior studies have examined tibiofemoral loading in flexed postures [7,8] and crouch gait [9], with the latter study suggesting that tibiofemoral contact forces are as much as ~2.2 times higher in severe crouch than normal walking. It is speculated that crouch may also excessively load the posterior tibia, contributing to abnormal posterior slope of the tibial plateau [10]. However, traditional gait models lack the anatomical fidelity needed to assess the influence of crouch on knee cartilage pressure magnitudes and locations.
Patellofemoral and tibiofemoral pressures are relevant to the surgical treatment of crouch gait and patella alta. Patellar tendon advancement (PTA) is increasingly used in the treatment of crouch gait in children with cerebral palsy, and has generally been effective at reducing the degree of crouch [11]. The PTA transfers the distal insertion of the patella inferiorly on the tibia to address quadriceps insufficiency [12], which often is present in children with crouch [5]. The procedure is typically performed in a manner that places the patella in baja [11,12]. However, it is unclear how patella baja alters patellar contact pressure magnitude or location during gait. Furthermore, treatment of crouch with PTA results in reduced posterior tibal slope, especially in younger children [10]. Yet, it remains unknown whether this might be caused by alterations in tibial cartilage loading patterns.
To address these questions, we have developed a musculoskeletal model with six degrees of freedom at both the tibiofemoral and patellofemoral joints [13] to allow prediction of cartilage pressures in normal and crouch gait. This model enables patellar position to be modified and simulates the coupled influence of muscle forces, ligamentous restraints, and cartilage contact on internal knee behavior during dynamic movements such as gait. We have previously validated this model against dynamic MRI [13] and used it to predict quadriceps and patellar tendon forces during walking in crouch with varying patellar positions [14].
Hence, the objective of this study was to use our modeling framework to investigate the coupled effects of walking posture and patellar position on tibiofemoral and patellofemoral pressures. To do this, we used retrospective gait analysis data to simulate the gait of twenty healthy children with normal gait and fifteen children with varying degrees of crouch. Our goal was to provide a better understanding of the effects of patellar tendon advancement procedures on internal knee mechanics during functional activities.
Materials and Methods
Whole body kinematics and ground reaction forces were obtained from the database at Gillette Children’s Specialty Healthcare for twenty typically-developing children (mean ± SD: height 1.49 ± 0.2 m, mass 44.2 ± 16.0 kg, speed 1.1 ± 0.2 m/s) and fifteen children with cerebral palsy who exhibited mild (N = 6, height 1.41 ± 0.11 m, mass 42.5 ± 11.9 kg, speed 0.9 ± 0.2 m/s), moderate (N = 5, height 1.49 ± 0.14 m, mass 45.2 ± 13.0 kg, speed 1.0 ± 0.2 m/s), and severe (N = 4, height 1.37 ± 0.25 m, mass 35.5 ± 14.7 kg, speed 0.8 ± 0.1 m/s) crouch gait and had received clinical gait analysis as part of standard of care [15]. Crouch severity was classified by the minimum knee flexion angle during stance [16], with mean (SD) values of 5 (5), 30 (7), 45 (4), and 60 (6) degrees for normal, mild, moderate, and severe subject groups, respectively (Figure 2A). Use of these data for research has been approved by the University of Minnesota Institutional Review Board. A 12-camera motion capture system (Vicon, Denver, CO) and four overground forceplates (AMTI, Watertown, MA) recorded marker trajectories and ground reaction forces, respectively. Kinematic trajectories and ground reaction forces were low-pass filtered at 6 Hz and 30 Hz, respectively. All children walked at their self-selected speeds and without assistive aids.
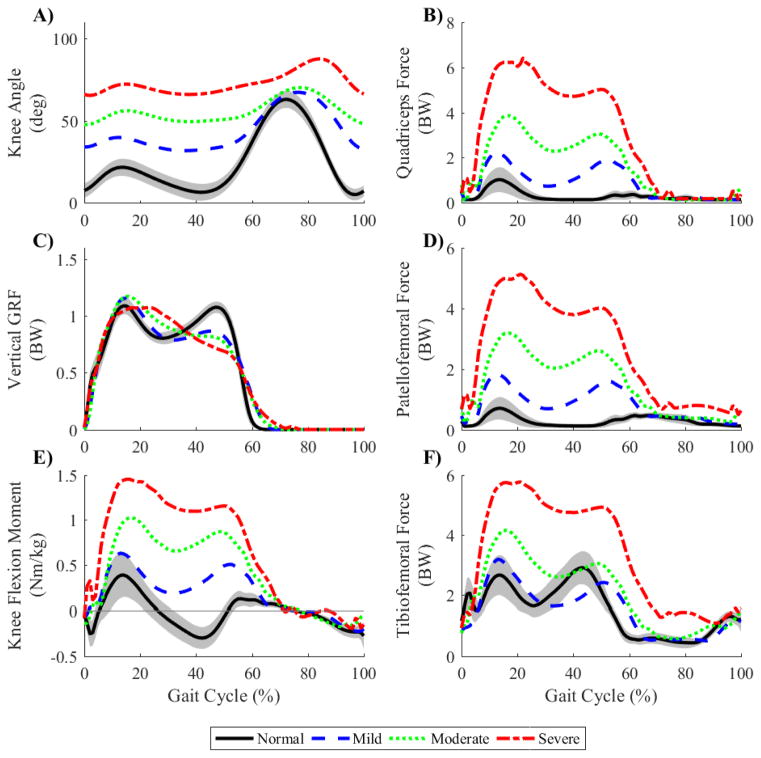
Figure 2.
Mean knee flexion angle (A), quadriceps force (B, sum of vasti and rectus femoris forces), vertical ground reaction force (C, GRF), patellofemoral contact force (D), external knee flexion moment (E), and tibiofemoral contact force (F) across the gait cycle for subjects with normal, mild crouch, moderate crouch, and severe crouch gait. All forces are normalized to body weight (BW), and the flexion moment is normalized to body mass (kg). The shaded region for the normal group represents ± one standard deviation from the mean.
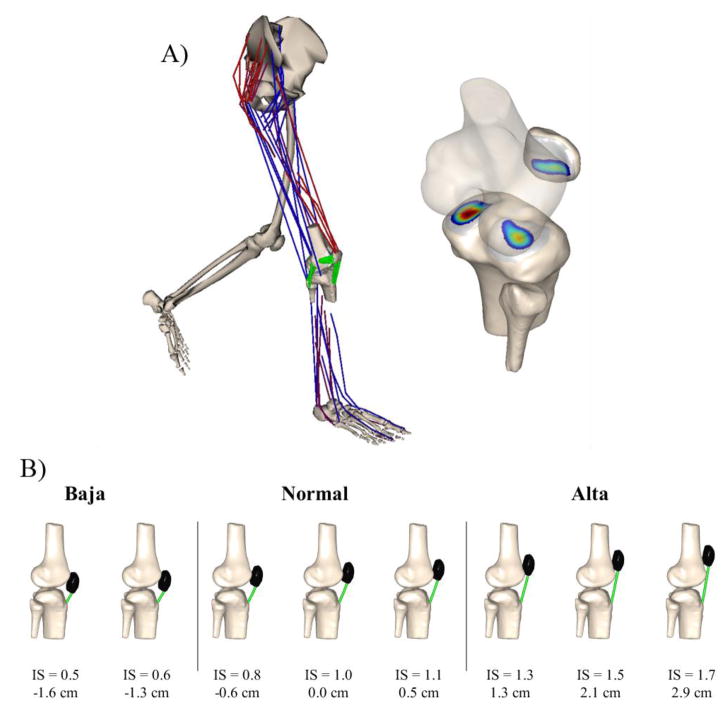
A three-body knee model, as described and validated in Lenhart et al. [13], was incorporated into a published lower extremity musculoskeletal model [17] and used to simulate knee mechanics during gait (Figure 1A). The knee model included 6 degrees of freedom (DOF) and cartilage contact at both patellofemoral and tibiofemoral joints, and multi-strand bundles for fourteen ligaments [18,19]. For this study, the femoral cartilage geometry was extended to include the anterior femur such that, when placed in alta, the patella articulated with the distal femur (Figure 1B).
Figure 1.
A) Six degree of freedom tibiofemoral and patellofemoral mechanics were simulated during gait using a musculoskeletal model. Inter-penetration of the cartilage meshes determined contact forces and pressures at each frame of simulation. B) Illustration of the eight different patellar positions tested. Patellar positions were classified as baja, normal, or alta based on the Insall-Salvati (IS) ratio[24] (Normal: 0.8 < IS < 1.2). For ease of comparison, the inferior-superior position is also described in centimeters (cm), with respect to the normal patellar position (IS = 0.98, 0.0cm). These absolute positions are scaled to the size of the representative typically-developing child (height = 1.40m).
The model was scaled for each subject using anatomical markers, then joint angles were computed at each frame of the gait cycle using inverse kinematics [20]. During inverse kinematics, the primary knee coordinate (flexion angle) was solved from motion capture data while all remaining secondary knee coordinates (non-sagittal tibiofemoral rotations, all tibiofemoral translations, and all patellofemoral DOF), which are difficult to measure using motion capture, were prescribed as functions of the flexion angle based on the passive behavior of the 12-DOF knee model [13].
We performed concurrent optimization of muscle activations and kinematics (COMAK) [21–23] to simultaneously solve for ligament forces, muscle forces, and cartilage contact pressures at every frame of the gait cycle. Briefly, COMAK estimates muscle activations and secondary knee kinematics that minimize the muscle volume-weighted sum of squared activations and the net cartilage contact elastic energy [22]. COMAK enforces dynamic constraints requiring that the simulated muscle forces, together with the internal knee contact and ligament forces exactly produced the measured hip flexion, hip adduction, hip internal rotation, knee flexion, and ankle dorsiflexion accelerations while generating zero accelerations in the secondary tibiofemoral and all patellofemoral degrees of freedom. Pelvic kinematics were prescribed to experimental values, such that whole body dynamics were implicitly resolved. COMAK solves a full gait cycle in ~20 minutes on a standard desktop computer.
For each subject, eight simulations were performed to investigate the effect of changing the patellar position from extreme alta (Insall-Salvati ratio [24], IS = 1.7) to baja (IS = 0.5) (Figure 1B). For each simulation, patellofemoral and tibiofemoral contact location and magnitude information were extracted throughout the gait cycle. To assess the shift in patellar contact location, the cartilage surface was divided into inferior, middle, or superior regions, each spanning one-third of the inferior-superior height. The percentage of the total contact area falling within each region was averaged throughout stance.
Results
Muscle and Contact Forces
At the normal patellar position, quadriceps forces (sum of vasti and rectus femoris, Figure 2B) increased over six-fold in severe crouch versus normal walking (6.4 vs. 1.0 times body weight (BW), respectively). Similarly, patellofemoral contact forces (Figure 2D) increased dramatically with crouch, with peak loads of 0.7, 1.8, 3.2, and 5.1 BW in normal, mild, moderate and severe crouch, respectively. While peak tibiofemoral forces were similar in normal gait (2.9 BW) and mild crouch (3.2 BW), peak contact forces in moderate (4.1 BW) and severe crouch (5.7 BW) were much greater (Figure 2F).
Contact Locations
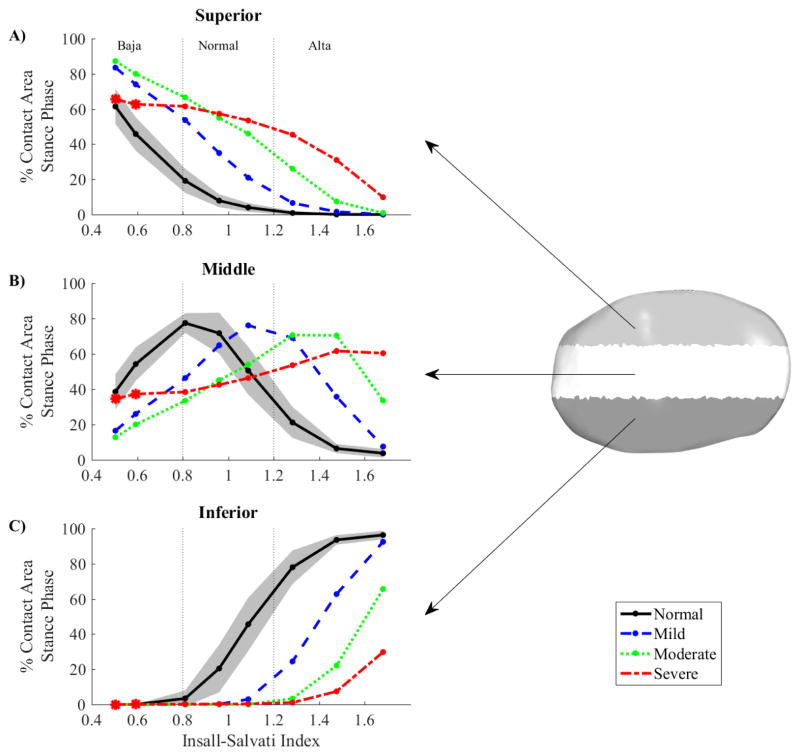
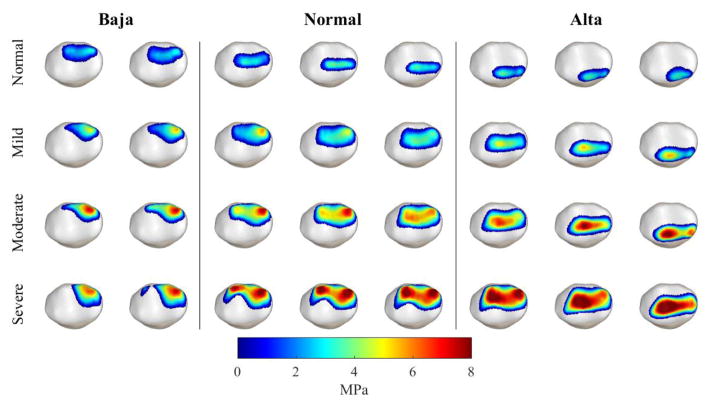
Both crouch and patellar position influenced the location of patellofemoral contact pressure. In the normal patellar position (IS = 1.0) and with normal gait, the majority of the contact area (73%, Figure 4B) fell within the middle region of the cartilage surface. However, the contact area shifted superiorly both as crouch severity increased and as the patellar position shifted from alta to baja (Figure 3, Figure 4). The majority of patellar contact was restored to the middle of the cartilage surface when the patella was shifted superiorly by approximately 0.5 cm (IS = 1.1), 1.3 cm (IS = 1.3), or 2.1 cm (IS = 1.5) for mild, moderate, and severe crouch, respectively (Figure 4B).
Figure 4.
The superior-inferior shift of the patellofemoral contact area was quantified as the percentage of the total contact area, averaged during stance, that fell within inferior, middle, or superior cartilage regions (Right). For each plot (A–C), the shaded region represents the normal patellar position (0.8 < IS < 1.2, Figure 1). Asterisk (*) symbols indicate simulations in which there was severe wrapping of the quadriceps tendon over the distal femur (severe crouch + extreme baja positions, supplementary).
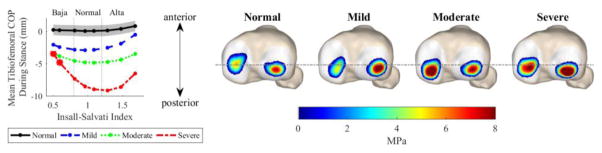
Figure 3.
Patellofemoral contact pressures for representative normal, mild, moderate, and severe crouch gait subjects (rows) across a variety of patellar positions (columns). For each subject, pressure is illustrated at the instant of peak patellofemoral contact force during gait (Figure 2). Patellar contact pressure increased dramatically with crouch severity, and the contact location shifted inferiorly as the patella was perturbed from baja (left) to alta (right). For each image, medial is left and superior is up.
The tibial contact location was highly influenced by crouch severity, and sensitive to patellar position in crouched postures (Figure 5). Compared with normal gait, the mean location of the tibiofemoral contact center of pressure (COP) during stance shifted posteriorly by 3.0, 4.8, and 8.5 mm for mild, moderate, and severe crouch, respectively (Figure 5, Insall-Salvati = 1.0). For severe crouch, baja patellar positions reduced this posterior shift in the center of pressure by approximately 5 mm (−3.5 vs −8.5mm, Figure 5). Subsequent investigation revealed that the combination of baja and large knee flexion angles causes the quadriceps to wrap around the distal femur. This wrapping aligns the quadriceps and patellar tendons, and thereby mitigates the anterior patellar tendon force acting on the tibia (see supplementary).
Figure 5.
The tibiofemoral center of pressure shifted posteriorly as crouch severity increased. Left: The mean COP location in the anterior-posterior direction, averaged throughout stance and across both medial and lateral condyles for each group. This position is referenced to the mean COP location for the normal group with normal patellar position (solid blue line, IS = 1.0, COP = 0mm) and scaled to the size of a representative typically-developing child (height = 1.4m). Right: representative illustrations of the contact pressure distributions, taken at the instant of maximal tibiofemoral contact force
Contact Pressures
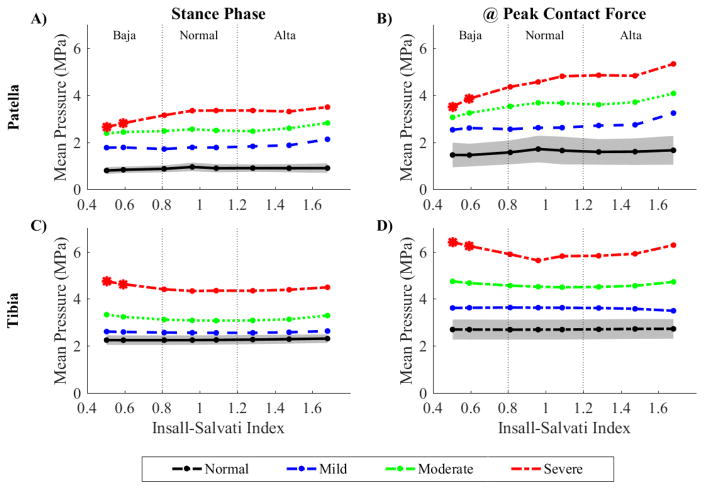
Both patellofemoral and tibiofemoral contact pressures increased with crouch severity (Figure 6). When the patella was placed in a normal position (IS = 1.0), mean patellofemoral pressure, averaged throughout stance, increased from 1.0 MPa in normal gait to 3.3 MPa in severe crouch (Figure 6A), while the mean pressure at the instant of peak contact force showed a greater increase from 1.7 to 4.6 MPa for normal and severe crouch, respectively (Figure 6B). Similarly, mean tibiofemoral pressure during stance increased from 2.2 MPa in normal gait to 4.3 MPa in severe crouch, while the mean pressure at the instant of peak contact loading increased from 2.8 to 5.6 MPa for normal to severe crouch, respectively.
Figure 6.
Mean pressure throughout the contact area, averaged across the stance phase (A,C), and at the instant of peak contact force during gait (B,D) for patellar (A,B) and tibial (C,D) cartilage. Contact pressure increased with crouch severity, but was relatively unaffected by changes in patellar position. Asterisk (*) symbols indicate simulations in which patellar pressure decreased due to severe wrapping of the quadriceps tendon over the distal femur (severe crouch + extreme baja positions, supplementary).
Patellofemoral and tibiofemoral pressures were relatively insensitive to changes in patellar position (Figure 6). However, for subjects with severe crouch, mean patellofemoral pressure during stance phase decreased from 3.3 MPa to 2.6 MPa when the patella was shifted from a normal (IS = 1.0) to a baja (IS = 0.5) position (Figure 6A). Conversely, the mean tibiofemoral pressure increased from 4.3 MPa to 4.7 MPa for the same positions, respectively (Figure 6B). As described previously, these changes in pressure were attributed to quadriceps wrapping (see supplementary).
Discussion
The goal of this study was to determine the combined effects of a crouched walking posture and patellar position on knee cartilage contact pressures during walking. We found that walking with crouch gait greatly magnified contact pressures at both the patellofemoral and tibiofemoral joints, while shifting tibiofemoral pressure posteriorly on the tibial plateau. Patellar position substantially affected the location of patellofemoral contact pressure, with alta positions concentrating pressure on the middle region of the patellar cartilage when walking in crouch. In contrast, baja patellar positions concentrated pressure on the superior edge of the patella in flexed knee postures. These results are important both for understanding potential causes of patellofemoral pain in children with crouch gait, and when considering the implications of surgically altered patellar position and walking posture on internal knee mechanics during gait.
It is recognized that joint contact pressures may directly contribute to patellofemoral pain and abnormal skeletal growth in children who exhibit crouch. However, despite this clinical relevance, we are not aware of prior investigations of knee cartilage pressures in crouch gait. In normal walking, tibiofemoral and patellofemoral pressures have been estimated to be approximately 1.7–3.1 MPa [25] and 2.4 MPa [26,27], respectively, which are comparable to estimates in this study (Figure 6). While both tibiofemoral and patellofemoral pressure magnitudes increase in crouch, our models suggest the effect on the patellofemoral joint is more dramatic with mean patellofemoral pressure increasing more than threefold, and patellofemoral contact forces increasing more than seven-fold, from normal to severe crouch. The sensitivity of the patellofemoral joint is attributed to the more-flexed knee posture creating a more-acute angle between the quadriceps and patellar tendons, which directly increases the contact force at the patellofemoral joint [28,29]. Similar effects are present in stair climbing, where patellofemoral pressure estimates (4–5 MPa) [30] are comparable to those computed for our severe crouch condition. While the two-fold increase in tibiofemoral pressure from normal to severe crouch was more modest, there was a marked, and progressive, posterior migration of the contact location on the tibial plateaus from mild to severe crouch (Figure 5). This result lends credence to the belief that abnormal mechanical loading of tibiofemoral joint, and hence the underlying physis, may contribute to the abnormal posterior tibial slope seen in children who exhibit crouch gait [10].
We have previously shown that our modeling approach provides reasonable estimates of in vivo contact forces [22] and kinematics [13]. Further, our estimates of net knee forces in crouched gait are generally consistent with prior studies. Steele and others [9] found that increasing crouch severity increased tibiofemoral contact forces during walking, with values (normal = 3.0 BW, mild = 3.2 BW, moderate = 4.2 BW, severe = 6.5 BW) very similar to the current study (Figure 2). The patellofemoral force during normal walking has been estimated between 0.5 and 1.0 BW[31,32], and during stair climbing between 3.3 and 3.5 BW [31,32], which is similar to our normal, mild, and moderate crouch findings.
This work has several limitations which should be acknowledged. First, we scaled a generic model to represent individual subjects. It is known that children with cerebral palsy exhibit highly variable gait patterns [33] and have skeletal abnormalities such as femoral anteversion, abnormal tibial slope, and elongated patellas, which may affect results. Hence, while our results provide fundamental insight into the overall effects of differing crouch severity, subject-specific gait analysis and articular geometries are needed to examine cartilage pressure patterns for a specific patient. Second, our pressure predictions are limited by the assumption of uniform cartilage thickness; the current study likely underestimates contact pressures at the edges of the patella where cartilage is thinner, and overestimates in the middle where cartilage is thicker [34,35]. Non-uniform cartilage thickness could be included in the model by using MRI to characterize subject-specific cartilage thickness maps [36], but these data were not available for the current subjects. Finally, our modeling efforts necessarily rely on optimization techniques to resolve muscle redundancy [37], which do not account for antagonist muscle co-contraction. Given that muscle forces aren’t directly measurable, it is not possible to directly validate this aspect of our analysis. Thus, our analysis was designed to examine sensitivities of tissue loading to variations in patellar position while maintaining the same assumed muscle distribution algorithm. The presence of static muscle contractures and spasticity is likely to induce greater levels of co-contraction than estimated via optimization, which means that joint loads in cerebral palsy patients may well be higher than we estimate. Future work should investigate the sensitivity of contact pressures to abnormal muscle properties and neuromuscular coordination.
This work has implications for the surgical treatment of crouch gait. First, our work highlights the importance of correcting crouch to reduce contact pressures at both the tibiofemoral and patellofemoral joints. Both pain [38] and cartilage degeneration [39,40] have been linked to abnormally large contact pressures. Therefore, surgical correction of crouch may both improve gait function and preserve cartilage health. Second, our models show that patellar position affects both moment arms [14] and contact pressure location and pattern in gait (Figure 3, Figure 5), suggesting the final patellar position should be carefully chosen. Current crouch gait treatments often include a patellar tendon advancement (PTA) surgery, which relocates the patella inferiorly to correct an extension deficit and/or to tighten the quadriceps[12]. Clinicians who re-introduced the PTA procedure have recommended “overcorrection” of patellar position to correct the extension deficit and crouch gait; this often leaves children with patella baja [11]. Our model results agree with ex vivo data [41] which suggest that baja positions cause an increasingly superior patellar pressure region with increasing knee flexion (Figure 3, Figure 4). While baja might lead to reasonable, or even slightly reduced (Figure 6), patellofemoral contact pressure magnitudes during walking, our model did not account for decreased thickness towards the periphery of cartilage [34,35], and therefore may have underestimated pressure in this region. Additionally, the combination of baja with flexed-knee postures may cause the quadriceps to wrap around the femur [42], altering the normal load transmission around the knee joint (see supplementary). While increased quadriceps wrapping reduces patellofemoral contact forces, it is unclear how this affects quadriceps tendon health. Further, quadriceps wrapping decreases the patellar tendon moment arm [14], which leads to an increase in the tibiofemoral joint forces (Figure 6). This situation may be problematic when a child attempts activities requiring strength in flexed postures. Thus, our analysis suggests that placing the patella in a normal, or even slightly alta, position may be beneficial both to enhance moment arms [14] and to normalize the patellar contact location if patients are performing high flexion activities such as stair climbing, rising from a chair, or walking in moderate or severe crouch despite surgery. Finally, our model prediction of a posterior shift in tibial plateau loading with increasing crouch severity may have implications for long-term cartilage health [43] and skeletal growth in developing children [10]. Indeed, a prior study found that children who were treated with a distal femoral extension osteotomy for crouch exhibited a reduction in the posterior tibial slope [10], which our models suggest could arise from the contact pressure moving anteriorly on the tibial plateau as a more upright gait is achieved (Figure 5).
In conclusion, we have shown that walking posture substantially affects knee joint loading during walking, with crouch postures dramatically increasing both patellofemoral and tibiofemoral contact pressures and inducing a posterior migration of the tibiofemoral contact. While extreme alta and baja positions may cause abnormally located patellofemoral contact pressure during gait, a small amount of alta seems to normalize contact locations during high-flexion activities such as stair-climbing, and rising from a chair. These findings substantiate the importance of correcting crouch as well as carefully considering the amount of distalization and therefore patellar position post-surgically.
Supplementary Material
Highlights.
Perturbed patella position and computed knee contact during normal and crouch gait
Tibiofemoral pressure nearly doubled (2.2 to 4.3 MPa) from normal to severe crouch
Patellofemoral pressure tripled (1.0 to 3.3 MPa) from normal to severe crouch
Patellar contact shifted superiorly as the patella was perturbed from alta to baja
Surgery for crouch and patella alta may both reduce and re-locate pressure
Acknowledgments
This work was supported by the National Institutes of Health [grant numbers R21HD084213, U01EB015410, F30AR065838, UL1TR000427, andT32GM00869].
Footnotes
Conflict of interest statement: none.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Gage JR, Schwartz MH, Koop SE, Novacheck TF, editors. The Identification and Treatment of Gait Problems in Cerebral Palsy. 2. John Wiley & Sons; 2009. [Google Scholar]
- 2.Senaran H, Holden C, Dabney KW, Miller F. Anterior knee pain in children with cerebral palsy. J Pediatr Orthop. 2007;27:12–6. doi: 10.1097/BPO.0b013e31802b715c. [DOI] [PubMed] [Google Scholar]
- 3.Miller F. Cerebral Palsy. Springer-Verlag; New York: 2005. [DOI] [Google Scholar]
- 4.Topoleski TA, Kurtz CA, Grogan DP. Radiographic abnormalities and clinical symptoms associated with patella alta in ambulatory children with cerebral palsy. J Pediatr Orthop. 2000;20:636–9. doi: 10.1097/01241398-200009000-00016. [DOI] [PubMed] [Google Scholar]
- 5.Lotman DB. Knee flexion deformity and patella alta in spastic cerebral palsy. Dev Med Child Neurol. 1976;18:315–9. doi: 10.1111/j.1469-8749.1976.tb03653.x. [DOI] [PubMed] [Google Scholar]
- 6.Sheehan FT, Babushkina A, Alter KE. Kinematic determinants of anterior knee pain in cerebral palsy: a case-control study. Arch Phys Med Rehabil. 2012;93:1431–40. doi: 10.1016/j.apmr.2012.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Perry J, Antonelli D, Ford W. Analysis of knee-joint forces during flexed-knee stance. J Bone Joint Surg Am. 1975;57:961–7. http://www.ncbi.nlm.nih.gov/pubmed/1194303. [PubMed] [Google Scholar]
- 8.Thambyah A, Goh JCH, Das De S. Contact stresses in the knee joint in deep flexion. Med Eng Phys. 2005;27:329–35. doi: 10.1016/j.medengphy.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 9.Steele KM, Demers MS, Schwartz MH, Delp SL. Compressive tibiofemoral force during crouch gait. Gait Posture. 2012;35:556–60. doi: 10.1016/j.gaitpost.2011.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patthanacharoenphon C, Maples DL, Saad C, Forness MJ, Halanski MA. The effects of patellar tendon advancement on the immature proximal tibia. J Child Orthop. 2013;7:139–146. doi: 10.1007/s11832-012-0480-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stout JL, Gage JR, Schwartz MH, Novacheck TF. Distal Femoral Extension Osteotomy and Patellar Tendon Advancement to Treat Persistent Crouch Gait in Cerebral Palsy. J Bone Jt Surgery-American Vol. 2008;90:2470–2484. doi: 10.2106/JBJS.G.00327. [DOI] [PubMed] [Google Scholar]
- 12.Novacheck TF, Stout JL, Gage JR, Schwartz MH. Distal femoral extension osteotomy and patellar tendon advancement to treat persistent crouch gait in cerebral palsy. Surgical technique. J Bone Joint Surg Am. 2009;91(Suppl 2):271–86. doi: 10.2106/JBJS.I.00316. [DOI] [PubMed] [Google Scholar]
- 13.Lenhart RL, Kaiser J, Smith CR, Thelen DG. Prediction and Validation of Load-Dependent Behavior of the Tibiofemoral and Patellofemoral Joints During Movement. Ann Biomed Eng. 2015;43:2675–85. doi: 10.1007/s10439-015-1326-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lenhart RL, Brandon SCE, Smith CR, Novacheck TF, Schwartz MH, Thelen DG. Influence of patellar position on the knee extensor mechanism in normal and crouched walking. J Biomech. 2017;51:1–7. doi: 10.1016/j.jbiomech.2016.11.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davis RB, Õunpuu S, Tyburski D, Gage JR. A gait analysis data collection and reduction technique. Hum Mov Sci. 1991;10:575–587. doi: 10.1016/0167-9457(91)90046-Z. [DOI] [Google Scholar]
- 16.Steele KM, Seth A, Hicks JL, Schwartz MH, Delp SL. Muscle contributions to vertical and fore-aft accelerations are altered in subjects with crouch gait. Gait Posture. 2013;38:86–91. doi: 10.1016/j.gaitpost.2012.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Arnold EM, Ward SR, Lieber RL, Delp SL. A model of the lower limb for analysis of human movement. Ann Biomed Eng. 2010;38:269–79. doi: 10.1007/s10439-009-9852-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bei Y, Fregly BJ. Multibody dynamic simulation of knee contact mechanics. Med Eng Phys. 2004;26:777–89. doi: 10.1016/j.medengphy.2004.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Smith CR, Won Choi K, Negrut D, Thelen DG. Efficient computation of cartilage contact pressures within dynamic simulations of movement. Comput Methods Biomech Biomed Eng Imaging Vis. 2016;1163:1–8. doi: 10.1080/21681163.2016.1172346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lu T-W, O’Connor JJ. Bone position estimation from skin marker co-ordinates using global optimisation with joint constraints. J Biomech. 1999;32:129–134. doi: 10.1016/S0021-9290(98)00158-4. [DOI] [PubMed] [Google Scholar]
- 21.Lenhart RL, Smith CR, Vignos MF, Kaiser J, Heiderscheit BC, Thelen DG. Influence of step rate and quadriceps load distribution on patellofemoral cartilage contact pressures during running. J Biomech. 2015;48:2871–8. doi: 10.1016/j.jbiomech.2015.04.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smith CR, Vignos MF, Lenhart RL, Kaiser J, Thelen DG. The Influence of Component Alignment and Ligament Properties on Tibiofemoral Contact Forces in Total Knee Replacement. J Biomech Eng. 2016;138:21017. doi: 10.1115/1.4032464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Smith CR, Lenhart RL, Kaiser J, Vignos MF, Thelen DG. Influence of Ligament Properties on Tibiofemoral Mechanics in Walking. J Knee Surg. 2016;29:99–106. doi: 10.1055/s-0035-1558858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Insall J, Salvati E. Patella Position in the Normal Knee Joint. Radiology. 1971;101:101–104. doi: 10.1148/101.1.101. [DOI] [PubMed] [Google Scholar]
- 25.Mamat N, Osman NAA. 2012 Int Conf Biomed Eng. IEEE; 2012. Numerical measurement of contact pressure in the tibiofemoral joint during gait; pp. 38–43. [DOI] [Google Scholar]
- 26.Powers CM, Ward SR, Chen Y, Chan L, Terk MR. The effect of bracing on patellofemoral joint stress during free and fast walking. Am J Sports Med. 2004;32:224–31. doi: 10.1177/0363546503258908. [DOI] [PubMed] [Google Scholar]
- 27.Ward SR, Powers CM. The influence of patella alta on patellofemoral joint stress during normal and fast walking. Clin Biomech (Bristol, Avon) 2004;19:1040–7. doi: 10.1016/j.clinbiomech.2004.07.009. [DOI] [PubMed] [Google Scholar]
- 28.Hefzy MS, Yang H. A three-dimensional anatomical model of the human patello-femoral joint, for the determination of patello-femoral motions and contact characteristics. J Biomed Eng. 1993;15:289–302. doi: 10.1016/0141-5425(93)90005-J. [DOI] [PubMed] [Google Scholar]
- 29.Hirokawa S. Three-dimensional mathematical model analysis of the patellofemoral joint. J Biomech. 1991;24:659–671. doi: 10.1016/0021-9290(91)90331-G. [DOI] [PubMed] [Google Scholar]
- 30.Powers CM, Ward SR, Chen Y-J, Chan L-D, Terk MR. Effect of bracing on patellofemoral joint stress while ascending and descending stairs. Clin J Sport Med. 2004;14:206–14. doi: 10.1097/00042752-200407000-00003. [DOI] [PubMed] [Google Scholar]
- 31.Chen Y-J, Scher I, Powers CM. Quantification of patellofemoral joint reaction forces during functional activities using a subject-specific three-dimensional model. J Appl Biomech. 2010;26:415–23. doi: 10.1123/jab.26.4.415. http://www.ncbi.nlm.nih.gov/pubmed/21245501. [DOI] [PubMed] [Google Scholar]
- 32.Reilly DT, Martens M. Experimental analysis of the quadriceps muscle force and patello-femoral joint reaction force for various activities. Acta Orthop Scand. 1972;43:126–37. doi: 10.3109/17453677208991251. [DOI] [PubMed] [Google Scholar]
- 33.Schwartz MH, Rozumalski A. The Gait Deviation Index: a new comprehensive index of gait pathology. Gait Posture. 2008;28:351–7. doi: 10.1016/j.gaitpost.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 34.Cohen Z, Mow V, Henry JHMD, Levine WNMD, Ateshian G, ZACPD, VCMPD, Henry JHMD, Levine WNMD, GAAPD Templates of the cartilage layers of the patellofemoral joint and their use in the assessment of osteoarthritic cartilage damage. Osteoarthr Cartil. 2003;11:569–579. doi: 10.1016/S1063-4584(03)00091-8. [DOI] [PubMed] [Google Scholar]
- 35.Draper CE, Besier TF, Gold GE, Fredericson M, Fiene A, Beaupre GS, Delp SL. Is cartilage thickness different in young subjects with and without patellofemoral pain? Osteoarthr Cartil. 2006;14:931–7. doi: 10.1016/j.joca.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 36.Van Rossom S, Smith CR, Zevenbergen L, Thelen DG, Vanwanseele B, Van Assche D, Jonkers I. Knee Cartilage Thickness, T1ρ and T2 Relaxation Time Are Related to Articular Cartilage Loading in Healthy Adults. PLoS One. 2017;12:e0170002. doi: 10.1371/journal.pone.0170002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Crowninshield RD, Brand RA. A physiologically based criterion of muscle force prediction in locomotion. J Biomech. 1981;14:793–801. doi: 10.1016/0021-9290(78)90045-3. [DOI] [PubMed] [Google Scholar]
- 38.Farrokhi S, Keyak JH, Powers CM. Individuals with patellofemoral pain exhibit greater patellofemoral joint stress: a finite element analysis study. Osteoarthr Cartil. 2011;19:287–94. doi: 10.1016/j.joca.2010.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Segal NA, Kern AM, Anderson DD, Niu J, Lynch J, Guermazi A, Torner JC, Brown TD, Nevitt M. Elevated tibiofemoral articular contact stress predicts risk for bone marrow lesions and cartilage damage at 30 months. Osteoarthr Cartil. 2012;20:1120–1126. doi: 10.1016/j.joca.2012.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Buckwalter JA, Anderson DD, Brown TD, Tochigi Y, Martin JA. The Roles of Mechanical Stresses in the Pathogenesis of Osteoarthritis: Implications for Treatment of Joint Injuries. Cartilage. 2013;4:286–294. doi: 10.1177/1947603513495889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Meyer SA, Brown TD, Pedersen DR, Albright JP. Retropatellar contact stress in simulated patella infera. Am J Knee Surg. 1997;10:129–38. http://www.ncbi.nlm.nih.gov/pubmed/9280107. [PubMed] [Google Scholar]
- 42.Singerman R, Davy DT, Goldberg VM. Effects of patella alta and patella infera on patellofemoral contact forces. J Biomech. 1994;27:1059–1065. doi: 10.1016/0021-9290(94)90222-4. [DOI] [PubMed] [Google Scholar]
- 43.Andriacchi TP, Mündermann A, Smith RL, Alexander EJ, Dyrby CO, Koo S. A framework for the in vivo pathomechanics of osteoarthritis at the knee. Ann Biomed Eng. 2004;32:447–57. doi: 10.1023/b:abme.0000017541.82498.37. http://www.ncbi.nlm.nih.gov/pubmed/15095819. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.