Abstract
Objective
The latent factor structure of posttraumatic stress disorder (PTSD) remains a source of considerable variability. The current study compared several a priori factor structures, as well as a novel 2-factor structure of posttraumatic psychological distress as measured by the Clinician Administered PTSD scale for the DSM-5 (CAPS-5). Additionally, variability in diagnostic rates according to the divergent DSM-5 and ICD-11 criteria were explored.
Method
The setting for this study was a level 1 trauma center in a U.S. metropolitan city. Data were pooled from two studies (N = 309) and participants were administered the CAPS-5 at one (n = 139) or six months post-injury (n =170). Confirmatory factor analysis (CFA) was used to compare several factor models, and prevalence rates based on DSM-5 and ICD-11 criteria were compared via z-tests and kappa.
Results
Confirmatory factor analyses of five factor structures indicated good fit for all models. A novel 2-factor model based on competing models of PTSD symptoms and modification indices was then tested. The 2-factor model of the CAPS-5 performed as well or better on most indices compared to a 7-factor hybrid. Comparisons of PTSD prevalence rates found no significant differences, but agreement was variable.
Conclusions
These findings indicate that the CAPS-5 can be seen as measuring two distinct phenomena: posttraumatic stress disorder and general posttraumatic dysphoria. This is an important contribution to the current debate on which latent factors constitute PTSD and may reduce discordance.
Keywords: PTSD diagnosis, CAPS-5, DSM-5, ICD-11, confirmatory factor analysis
Cross-nationally, 70% of people will experience a potentially traumatic event. Within the U.S., this estimate increases to 82.7% (Benjet et al., 2016). Some of the most commonly reported traumatic experiences are injuries that result from life-threatening accidents and assaults. Many of these individuals are evaluated in emergency departments, with a significant minority admitted to the hospital for their injuries. On average, approximately 20% of individuals admitted to the trauma service of a level 1 trauma center will go on to develop posttraumatic stress disorder (PTSD; deRoon-Cassini, Mancini, Rusch, & Bonanno, 2010). In addition to the psychosocial difficulties associated with physical injury, those with co-occurring PTSD are at risk for significantly lower quality of life (Brasel, deRoon-Cassini, & Bradley, 2010), increased risk for suicide (Gradus et al., 2010), and poorer overall physical health outcomes (Pacella, Hruska, & Delahanty, 2013).
Given these findings, it is concerning that the precise underlying factor structure of posttraumatic psychological distress remains a source of considerable variability. Recently, significant debate has arisen (Friedman, Kilpatrick, Schnurr, & Weathers, 2016; Guina, 2016; Hansen, Hyland, Armour, Shevlin, & Elklit, 2015; Hoge, Riviere, Wilk, Herrell, & Weathers, 2014; Hoge et al., 2016; O’Donnell et al., 2014) following the changes to the criteria in the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5; APA, 2013). Specifically, some researchers posit that there are “core” symptoms of PTSD which include only reexperiencing, avoidance, and hyperarousal (Brewin, Lanius, Novac, Schnyder, & Galea, 2009) symptoms, in opposition to the more broadly defined current iteration in the DSM-5 (Friedman, 2013). A narrower conceptualization is currently supported by the International Classification of Diseases, eleventh revision (ICD-11) work group (Maercker et al., 2013). It follows that a valid, reliable diagnostic assessment is critical for posttraumatic evaluation and treatment, as well as for bolstering scientific understanding of the neurological and biological underpinnings of symptomatology.
Review of Factor Structure in the DSM
First introduced in the DSM-III (APA, 1980), the diagnosis of PTSD was based on 12 symptoms, clustered into three factors: 1) reexperiencing of the trauma, 2) numbing or reduced involvement with the external world, and 3) autonomic, dysphoric, or cognitive symptoms. The next iteration, the DSM-III-Revised, increased the number of symptoms to 17 and reorganized the three factors to accommodate for changes in the theory of the latent structure: 1) reexperiencing of the trauma, 2) avoidance of trauma-related stimuli or numbing, and 3) increased arousal.
Changes to diagnostic criteria in the DSM-IV/IV-TR (APA, 1994; 2000) involved the relocation of only the physiological reactivity symptom to the reexperiencing cluster. Although this relative consistency hinted at the possibility of agreement among experts, the reality was that factor analyses conducted following the introduction of DSM-IV criteria produced variable structures. This was due in part to differences in sample, assessment, and analytical processes (Palmieri, Weathers, Difede, & King, 2007), with many investigators failing to find support for a 3-factor model of PTSD, and thus spurring additional exploration. Initially, the 4-factor Emotional Numbing (King, Leskin, King, & Weathers, 1998) and Dysphoria (Simms, Watson, & Doebbelling, 2002) models gained significant support across a number of trauma populations and assessment methods (Elhai et al., 2011; Yufik & Simms, 2010). With these models came two important, novel inferences: 1) individuals display variable patterns of symptom combinations that may be accurately represented as subtypes of PTSD (King et al., 1998); and 2) the possibility of a new dysphoria factor that includes nonspecific symptoms of several mood and anxiety disorders (e.g., sleep disturbance, irritability, difficulties with concentration, loss of interest, restricted affect, and detachment; Simms et al., 2002).
Indeed, the dysphoria factor demonstrated significant correlational relationships to symptoms of depression and generalized anxiety, indicating that this factor captures symptomatology related to more general psychological distress. An expanded 5-factor model, the Dysphoric Arousal model (Elhai et al., 2011), took into account each of these 4-factor models and concluded that dysphoric arousal symptoms represent a unique construct that is specific to neither anxiety nor depression. Although this 5-factor model is well-supported (Pietrzak, Tsai, Harpaz-Rotem, Whealin, & Southwick, 2012), much of this support was not established until after the development of the DSM-5, therefore limiting its influence on the criteria within.
In response to the ongoing shifts in theory, the DSM-5 PTSD committee added three symptoms to the diagnostic criteria, structured the diagnosis across four symptom clusters, and made significant revisions to the wording of items. Empirical investigations of this internal structure have paralleled the inconsistencies that arose from attempts to confirm the DSM-IV factor structure. For example, analyses have suggested 6-factor models of PTSD symptoms, including the Anhedonia model (Liu et al., 2014) and the Externalizing Behavior model (Tsai et al., 2014). These models align in their argument for distinct reexperiencing, avoidance, and arousal constructs. Findings associated with the Anhedonia model go on to provide support for the proposition, originally suggested by Elhai and colleagues (Elhai et al., 2011), that anhedonia, negative affect, and dysphoric arousal are also unique constructs of PTSD. This contrasts with the Externalizing Behavior model, which supports the constructs of anhedonia and negative affect as a single factor and differentiates a unique externalizing behaviors factor from half of the items classified as dysphoric arousal in the Anhedonia model.
Recently, research examining the dimensionality of PTSD has suggested that a 7-factor Hybrid model most accurately represents the underlying factor structure of the DSM-5 criteria (Armour et al., 2015). Authors of the Hybrid model assert that it integrates two major theoretical and empirical conclusions proposed by the separate six-factor models. First, the 7-factor model is argued to account for hyperarousal symptoms being comprised of distinct anxious and dysphoric arousal factors (Elhai et al., 2011). Second, this model makes distinctions between externalizing and internalizing behaviors, as well as between increased negative and decreased positive affect (Armour et al., 2015). This ongoing expansion suggests that PTSD may be a moving target, as it continues to be conceptualized with an ever-increasing number of factors. The aforementioned ICD-11 conceptualization has taken a much more parsimonious approach, suggesting that just six items are necessary for the diagnosis of PTSD. These items are separated into three clusters with two items each. The clusters are 1) reexperiencing, 2) avoidance, and 3) a persistent sense of current threat that is manifested by exaggerated startle and hypervigilance (Table 1; Karatzias et al., 2016). This model has been shown to have very strong fit across samples with varying trauma histories and has performed well when compared to the DSM-5 model (Hansen et al., 2015).
Table 1.
Item Mappings
| DSM-5 Symptom | DSM-5 | Dysphoric arousal | Externalizing behavior | Anhedonia | Hybrid | ICD-11 |
|---|---|---|---|---|---|---|
| 1. Intrusive thoughts | R | R | R | R | R | |
| 2. Distressing dreams/nightmares | R | R | R | R | R | R |
| 3. Flashbacks | R | R | R | R | R | R |
| 4. Cued psychological distress | R | R | R | R | R | |
| 5. Cued physiological distress | R | R | R | R | R | |
| 6. Avoidance of thoughts/memories | Av | Av | Av | Av | Av | Av |
| 7. Avoidance of external reminders | Av | Av | Av | Av | Av | Av |
| 8. Trauma-related amnesia | NACM | NACM | N | NACM | NA | |
| 9. Negative beliefs | NACM | NACM | N | NACM | NA | |
| 10. Distorted blame | NACM | NACM | N | NACM | NA | |
| 11. Negative trauma-related emotions | NACM | NACM | N | NACM | NA | |
| 12. Loss of interest | NACM | NACM | N | An | An | |
| 13. Detachment from others | NACM | NACM | N | An | An | |
| 14. Restricted positive affect | NACM | NACM | N | An | An | |
| 15. Irritability, anger | A | DA | EB | DA | EB | |
| 16. Self-destructive behavior | A | DA | EB | DA | EB | |
| 17. Hypervigilance | A | AA | AA | AA | AA | S |
| 18. Exaggerated startle response | A | AA | AA | AA | AA | S |
| 19. Concentration difficulties | A | DA | DA | DA | DA | |
| 20. Sleep disturbance | A | DA | DA | DA | DA |
Note. A = alterations in arousal/reactivity; AA = anxious arousal; An = anhedonia; Av = avoidance; DA = dysphoric arousal; EB = externalizing behaviors; N = numbing; NA = negative affect; NACM = negative alterations in cognition and mood; R = re-experiencing (DSM-5 intrusions); S = sense of threat
As one might guess, rates for PTSD are notably different when considering one diagnostic system over the other. In a multi-site investigation of traumatic injury survivors, O’Donnell and colleagues (2014) evaluated differences in diagnostic rates for PTSD using both DSM-5 and ICD-11. Following DSM-5 criteria, 6.7% of participants received a PTSD diagnosis whereas only 3.3% of participants met criteria according to ICD-11. Statistical comparison of these rates showed a significant difference in prevalence. Additionally, findings were presented that demonstrated higher rates of comorbidity with depression when using DSM-5 criteria. These empirical results fit with the theoretically more inclusive diagnostic approach of the DSM-5, and the divergence from this taken by the ICD-11 toward a more restricted system. Notably, however, the authors underscore that only 42% of participants met criteria for PTSD under both DSM-5 and ICD-11 (O’Donnell et al., 2014). Thus, most participants identified as having PTSD according to one system did not have PTSD according to the other—a finding that was not accounted for by the relative inclusivity of DSM-5 criteria. Consequently, we continue to experience critical issues related not only to the lack of consistency in models that offer the “best” fit, but also in the translational influence that these models have for health care accessibility, treatment compensation/coverage, and the efficacy of clinical interventions according to symptom presentation in one system versus another.
Present Study
To allow for a direct statistical comparison of competing models, the current study utilized confirmatory factor analyses (CFA) of several a priori factor structures of PTSD symptoms measured by the Clinician Administered PTSD Scale for DSM-5 ([CAPS-5]; Weathers et al., 2013). Additional analyses included a modified, novel 2-factor model that included all 20 symptoms presented in the DSM-5. The inclusion of this 2-factor model was based on the discordance in the literature about what symptoms constitute PTSD and the DSM-5 revisions that broadened criteria to include aspects of posttraumatic psychological distress common to other disorders (Friedman, 2013). The 7-factor Hybrid model (Table 1) was used as a guide for the initial distribution of CAPS-5 items into two factors. Specifically, items allocated to the Hybrid model factors that may be considered components of other disorders (i.e., Negative Affect, Anhedonia, and Externalizing Behavior factors), and thus not unique to PTSD symptomatology, were loaded onto a single factor. The remaining Hybrid model factors (Reexperiencing, Avoidance, Anxious Arousal, and Dysphoric Arousal) were used to create an analog factor representing symptoms of PTSD. The final 2-factor model was derived using both theory and statistical output from the CFAs (see Results for further explanation).
It is not suggested that this 2-factor model is a model of PTSD; rather this model is based on the premise that the CAPS-5 is measuring more than PTSD, which is causing the increase in underlying factors. A post hoc CFA was also run on the proposed ICD-11 criteria alone; however, since they are not derived from the exact same underlying parameters, no direct comparison can be made to the other models utilizing the 20 DSM-5 items. Following CFA, a comparison of the DSM-5 and proposed ICD-11 criteria was conducted to explore potential variability in diagnostic rates within this sample.
Method
Participants and Procedures
Data were pooled from two separate studies approved by the institution’s internal review board. Three hundred and nine participants were included in the analyses. Both samples were comprised of adult injured trauma survivors admitted to the trauma service of a level 1 trauma center in the United States. Inclusion criteria were identical for the two samples. Exclusion criteria were as follows: 1) younger than 18 years of age, 2) head injury that resulted in a serious alteration of consciousness (Glasgow Coma Scale score <13 on emergency department arrival) or moderate to severe traumatic brain injury (TBI), 3) self-inflicted injuries, 4) injuries that resulted in an inability to communicate, and 5) non-English speaking. Potential participants were identified using the trauma census, a real-time list of admissions due to a mechanism of injury. The CAPS-5 was administered at either one month (n = 139) or six months (n = 170) after injury. Demographic and self-report information is presented in Table 2. The two pooled samples (n1 = 173; n2 = 136) did not differ significantly from each other on participant demographics (i.e., age, gender, race) or trauma-related measures (i.e., mechanism of injury, CAPS-5 total/subscale severity scores).
Table 2.
Demographic and Clinical Interview Data (N = 309)
| M | SD | |
|---|---|---|
| CAPS-5 Total Severity Score | 14.50 | 15.34 |
| Agea | 42.03 | 16.78 |
|
| ||
| Percentage | n | |
|
| ||
| Sex: Male | 71.5% | 221 |
| Race | ||
| Caucasian | 47.2% | 146 |
| African American | 41.4% | 128 |
| Latino | 9.1% | 28 |
| Native American/Alaska Native | 1.3% | 4 |
| Other | 1.0% | 3 |
| Mechanism of Injury | ||
| MVC | 30.4% | 94 |
| GSW | 17.5% | 54 |
| Fall | 15.5% | 48 |
| MCC | 12.0% | 37 |
| Stabbing | 9.4% | 29 |
| PSV | 5.2% | 16 |
| Industrial accident | 3.9% | 12 |
| Recreational | 3.6% | 11 |
| Other | 1.6% | 5 |
| Blunt Assault | 1.0% | 3 |
Note.
Range = 18 – 89. GSW = gunshot wound, MVC = motor vehicle crash, MCC = motor cycle crash, PSV = pedestrian struck by vehicle
Measure
The CAPS-5 (Weathers et al., 2013) was administered by masters and doctoral level research assistants trained via a standardized protocol and supervised by doctoral level professionals throughout the studies. This instrument utilizes a clinician-administered structured diagnostic interview which allows for a dimensional (severity) and dichotomous diagnosis. Previous research indicates excellent psychometric properties of the CAPS for DSM-IV. In a large Veteran study (N = 838), severity scores for the three symptom clusters yielded intraclass correlations ranging from 0.88 – 0.91, with alphas between 0.82 – 0.88. Considering the measure as a whole, the intraclass correlation across all 17 symptom severity scores was 0.95 and α = 0.94 (Weathers, Ruscio, & Keane, 1999). Additionally, interrater reliability for PTSD diagnosis has been found to be very strong while utilizing the CAPS with veteran populations (Blake et al., 1995), with test-retest reliability in the moderate-to-high range (Mueser et al., 2001). Although, at this time, no such data are published for the CAPS-5, the current sample demonstrated good reliability. Alphas for the four symptom clusters severity scores ranged from 0.76 - 0.84, and the total measure severity score yielded α = 0.94.
Statistical Analyses
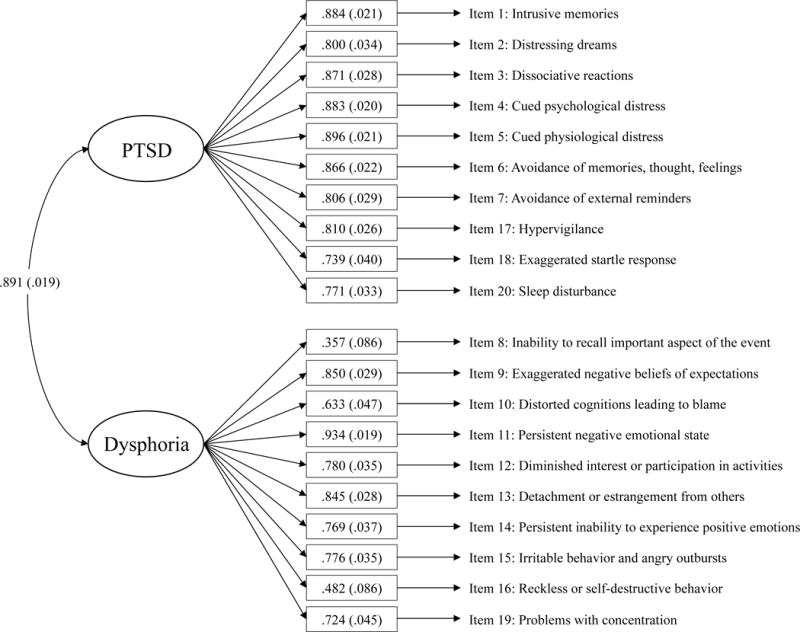
Data analyses were carried out in two main steps. The first step involved examining the internal structure of the CAPS-5 via CFA using Mplus© Version 7.4 (Muthén & Muthén, 2012). Previously examined models (Table 1) were explored, followed by the examination of a significantly reduced model (Figure 1). Symptom severity scores for the 20 items were entered as input variables for each model evaluation; there were no missing data for the CAPS-5 for any participant. Weighted least squares (WLS) estimation was used as the data were ordinal, with a robust mean- and variance-adjusted test statistic (i.e., “WLSMV” in Mplus; Muthén & Muthén, 2012). Goodness-of-fit indices were interpreted following the guidelines set forth by Hu and Bentler (1999): RMSEA ≤ .06, and CFI and TLI ≥ .95. For comparison of nested models, corrected chi-squared difference (Δχ2) tests were carried out via Mplus (Muthén & Muthén, 2012). Maximum likelihood estimation was used to derive the Akaike information criterion (AIC; Akaike, 1974) and Bayesian information criterion (BIC; Schwarz, 1978). The AIC and BIC can be used to compare the relative fit of multiple nested or non-nested models fit to the same data. Although chi-squared difference (Δχ2) testing cannot be carried out on non-nested models, non-nested models fit to the same data can be compared via incremental fit indices (e.g., CFI and TLI) because the independence model is nested within all of the factor models, which are all nested within the same saturated model (Bentler & Bonett, 1980; Widaman & Thompson, 2003).
Figure 1.
The second step involved comparing various diagnostic rates using IBM SPSS® Version 24, z-test of sample proportions, and the calculation of the kappa statistic to assess convergent validity. This step was undertaken to assess consistency across diagnostic criteria and included a comparison of DSM-5 and ICD-11 prevalence rates as measured by the CAPS-5. DSM-5 diagnosis and prevalence statistics were obtained with the original CAPS-5 scoring system. To derive an ICD-11 diagnosis and prevalence, the CAPS-5 scoring system was used in which a severity score above 2 (moderate/threshold) on the corresponding item indicated the presence or absence of a symptom. Those who were found to have ≥1 symptom present in each of the three ICD-11 clusters (Table 1) were considered positive.
Results
Step 1: CFA of a priori Models and Reduced Model
Five separate CFAs were run using factor structures supported in previous studies (Table 1) that examined measures designed to assess DSM-5 PTSD (Armour, Műllerová, & Elhai, 2016; Armour et al., 2015). In chi-square difference testing, the 7-factor model was a significantly better fit when compared to the four other nested models used for comparison (DSM-5, Δχ2(15) = 69.820, p < .001; Dysphoric Arousal, Δχ2(11) = 37.916, p < .001; Externalizing Behaviors, Δχ2(6) = 16.792, p = .010; Anhedonia, Δχ2(6) = 24.145, p < .001). All models demonstrated good fit, and additional fit statistics are presented in Table 3.
Table 3.
Fit Statistics for Confirmatory Factor Analyses of the CAPS-5 (N = 309)
| df | χ2 | RMSEA (90% CI) | CFI | TLI | AIC | BIC | |
|---|---|---|---|---|---|---|---|
| DSM-5 – 4-factor | 164 | 266.741 | .045 (.035, .055) | .988 | .987 | 15,380.237 | 15,626.638 |
| Dysphoric arousal – 5-factor | 160 | 238.032 | .040 (.029, .050) | .991 | .990 | 15,355,.473 | 15,616.806 |
| Externalizing behavior – 6-factor | 155 | 222.009 | .037 (.026, .048) | .992 | .991 | 15,346.983 | 15,626.983 |
| Anhedonia – 6-factor | 155 | 225.799 | .038 (.027, .049) | .992 | .990 | 15,340.779 | 15,620.780 |
| Hybrid – 7-factor | 149 | 208.277 | .036 (.023, .047) | .993 | .991 | 15,327.884 | 15,630.285 |
| 2-factor | 169 | 230.315 | .034 (.020, .042) | .993 | .992 | 15,331.706 | 15,559.440 |
Note. RMSEA = root-mean-square error of approximation; CFI = comparative fit index; TLI = Tucker Lewis index; AIC = Akaike information criterion; BIC = Bayesian information criterion.
The 2-factor model was then run using the 7-factor hybrid model as a guide (Table 1). Items that loaded on negative affect, anhedonia, and externalizing behavior factors were loaded on a new factor separate from the PTSD items measuring reexperiencing, avoidance, anxious arousal, and dysphoric arousal. Mplus output indicated a single modification index (M.I. = 20.701) for item 19. Given its non-specific relationship to general psychological distress (including depression; Paelecke-Habermann, Pohl, & Leplow, 2005), this item was removed from the PTSD factor and placed on the new factor, which given the qualities of the redistributed items was termed general posttraumatic dysphoria (Figure 1).
The novel 2-factor model (RMSEA = .034 (.020, .042), CFI = .993, TLI = .992, AIC = 15,331.706, BIC = 15,559.440) of the CAPS-5 was compared to the 7-factor Hybrid (RMSEA = .036 (.023, .047), CFI = .993, TLI = .991, AIC = 15.327.884, BIC = 15,360.285). Comparisons of the 2-factor model to the 7-factor Hybrid indicated that the 2-factor result performed as well or better on all indices except for the AIC, which tends to favor more complex models (Dziak, Coffman, Lanza, & Li, 2012). Although the BIC is an approximation (-2*logarithm) of the Bayes factor, the difference of 70.845 suggests very strong evidence that the 2-factor model is a better fit (Kass & Raferty, 1995). This suggests that DSM-5 PTSD criteria, as assessed by the CAPS-5, may be measuring a general posttraumatic dysphoria factor in addition to a PTSD factor. In fact, although no direct statistical comparisons can be made, fit for the 6-item, 3-factor proposed ICD-11 criteria (Table 1) was very strong in this sample (RMSEA = .016 (.000, .077), CFI = 1.00, TLI = .999).
Step 2: Comparison of Prevalence Rates Across DSM-5 and ICD-11
PTSD prevalence rates were not statistically significantly different in comparisons of the DSM-5 and ICD-11 in the full sample (28.5% vs 23.6%, z = 1.4, p = .17; κ = .724), and agreement was 89.3% overall. PTSD prevalence rates were also not significantly different within sub-analyses and were as follows: assaultive traumas (n = 86, DSM-5 = 47.7%, ICD-11 = 41.9%, z = .80, p = .44; κ = .789); non-assaultive traumas (n = 223; DSM-5 = 21.1%, ICD-11 = 16.6%, z = 1.2, p = .22; κ = .649); men (n = 221; DSM-5 = 25.3%, ICD-11 = 21.3%, z = 1.0, p = .32; κ = .760); women (n = 88; DSM-5 = 36.4%, ICD-11 = 29.5%, z = 1.0, p = .33; κ = .642); Caucasians (n = 146; DSM-5 = 10.3%, ICD-11 = 8.9%, z = .40, p = .68; κ = .526); racial minorities (n = 163; DSM-5 = 44.8%, ICD-11 = 36.8%, z = 1.5, p = .14; κ = .735). Notably, the rate of PTSD was higher for the DSM-5 than the ICD-11 across all groups.
Discussion
The findings from these factor analyses indicate that the CAPS-5 appears to measure two distinct phenomena: posttraumatic stress and general posttraumatic dysphoria. When compared to the various models presented herein, the fit of the 2-factor model was roughly equivalent or superior across many of the fit indices. This provides support for the ICD-11 work group supposition that PTSD consists of a core group of symptoms unique to PTSD. However, these findings are potentially due to the nature of single-incident traumatic injury and subsequent psychiatric sequelae. In fact, evidence for a 2-factor model was found in another study of injured trauma survivors who were administered the CAPS at six years post-injury.
Unlike the current study, however, these authors combined the reexperiencing (i.e., intrusion) and avoidance factors into one factor, and the NACM and the arousal factors into another, which demonstrated roughly equivalent fit across many of the fit indices presented in their results (Forbes et al., 2015). Since this time, additional studies have been published which indicate that this 2-factor structure may not be a good fit for other populations (Hyland, Brewin, & Maercker, 2017).
Although the DSM-5 had higher diagnostic rates than the ICD-11, prevalence of PTSD was not significantly different between the two systems as presented in a previous study of traumatic injury survivors (O’Donnell et al., 2014). An additional analysis of whether individuals identified as having PTSD according to DSM-5 were the same as those identified by the ICD-11 suggested that the concordance between the two systems (89.3%) is much higher than previously reported (42%). This implies that the DSM-5 and the ICD-11 may be reasonably aligned with one another, despite the more inclusive nature of the DSM-5 symptom list. However, based on the results of the factor analyses presented herein, and the variable rates in diagnosis and kappa within the subgroups, future research needs to examine whether this is the result of the DSM-5 including additional items that capture PTSD symptoms, or a result of the inclusion of the dysphoric elements of posttraumatic psychological distress.
A narrower definition of PTSD may also provide further synchrony between the psychological, neurobiological, and behavioral phenomena associated with the disorder. For example, neuroimaging studies have found that phenomena such as depression, PTSD, and their comorbid occurrence may result in distinctly different patterns of neural activity (Kemp et al., 2007; Lanius et al., 2007; Whalley, Rugg, Smith, Dolan, & Brewin, 2009). From a dimensional perspective, future investigators may want to examine whether including specific subtypes of posttraumatic psychological distress enhances validity and reliability. For example, an individual may present with significantly more reexperiencing symptoms than avoidance or hyperarousal, but in conjunction with depression or general posttraumatic dysphoria. A unique diagnostic category for this presentation, such as posttraumatic stress following an acute injury: intrusive and depressive type, could reduce inconsistencies, misdiagnosis, as well as over- and/or under-diagnosis.
Within the context of the current study sample, dysphoria may be the result of major resource loss after trauma, such as physical illness and functional limitations in combination with the financial burdens of physical impairment. This is distinct from a dysphoria that is a secondary reaction to the increased psychosocial stress that accompanies PTSD symptoms. Although dysphoria in each of these forms may have similar symptom presentations, they imply different etiological and psychogenic processes. As such, different treatments and interventions may yield very different results. Searching for an all-encompassing set of criteria for PTSD might be a set-up for the field to be in perpetual disagreement. Instead, a more effective direction might be to focus theoretical and empirical energies on identifying variants of posttraumatic psychological distress unique to certain individuals.
This may further help clinicians in selecting appropriate treatments and potentially give more accurate prognoses for aspects of treatment. Research examining psychiatrists’ attitudes on current classification systems indicated a preference for a simpler, more flexible diagnostic system that included fewer categories and a dimensional element in diagnosis (Reed, Correia, Esparza, Saxena, & Maj, 2011). The ICD-11 conceptualization seems to address some of these issues, as well as addressing the need for variable types of posttraumatic psychological reactions by introducing a range of diagnoses from Acute Stress Reaction, which is not classified as a disorder, to Complex Posttraumatic Stress Disorder, which seems to integrate aspects of possible character traits such as difficulties in emotion regulation (Cloitre, Garvert, Brewin, Bryant, & Maercker, 2013; Maercker et al., 2013). While the integration of personality or characterological disturbances will complicate factor analyses, the implementation of gradations or types is likely to clarify the operationalization of certain mental phenomena.
The limitations of this study include the smaller sample size, issues of temporality, and the generalizability of the findings. Ideally, this sample would be larger; however, there is debate regarding the sample size necessary when using WLSMV depending upon the magnitude of factor loadings and the number of factor indicators (Moshagen & Musch, 2014). Using data from two different time points may confound findings as well; although, current conceptualizations of PTSD do not assume or imply differences in the latent structure over time. Also, the generalizability of the findings may be limited to the traumatic injury population, or may be impacted by other unique characteristic of the CAPS-5, such as the administration style. Further research will need to address these limitations as well as assess replicability. An evaluation of comorbidities (e.g., depression) as they relate to the 2-factor model might also shed light on what is actually being measured. Finally, future work may further enhance the applicability of such a measure by performing factor analyses on items designed specifically to measure the core symptoms of PTSD.
Contributor Information
Joshua C. Hunt, Medical College of Wisconsin Department of Surgery, Division of Trauma and Critical Care, 9200 W. Wisconsin Ave. Milwaukee, Wisconsin 53226 414-805-8624.
Samantha A. Chesney, Marquette University
Terrence D. Jorgensen, University of Amsterdam
Nicholas R. Schumann, Medical College of Wisconsin
Terri A. deRoon-Cassini, Medical College of Wisconsin
References
- Akaike H. A new look at the statistical model identification. IEEE Transactions on Automatic Control. 1974;19:716–723. doi: 10.1109/TAC.1974.1100705. [DOI] [Google Scholar]
- Armour C, Műllerová J, Elhai JD. A systematic literature review of PTSD’s latent structure in the Diagnostic and Statistical Manual of Mental Disorders: DSM-IV to DSM-5. Clinical Psychology Review. 2016;44:60–74. doi: 10.1016/j.cpr.2015.12.003. [DOI] [PubMed] [Google Scholar]
- Armour C, Tsai J, Durham TA, Charak R, Biehn TL, Elhai JD, Pietrzak RH. Dimensional structure of DSM-5 posttraumatic stress symptoms: Support for a hybrid anhedonia and externalizing behaviors model. Journal of Psychiatric Research. 2015;61:106–113. doi: 10.1016/j.jpsychires.2014.10.012. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3rd. Washington, DC: Author; 1980. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th. Washington, DC: Author; 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th. Washington, DC: Author; 2000. text revision. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th. Washington, DC: Author; 2013. [Google Scholar]
- Benjet C, Bromet E, Karam EG, Kessler RC, McLaughlin KA, Ruscio AM, Koenen KC. The epidemiology of traumatic event exposure worldwide: Results from the World Mental Health Survey Consortium. Psychological Medicine. 2016;46:327–343. doi: 10.1017/S0033291715001981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychological Bulletin. 1980;88:588–606. doi: 10.1037/0033-2909.88.3.588. [DOI] [Google Scholar]
- Blake D, Weathers F, Nagy L, Kaloupek D, Gusman F, Charney D, Keane T. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1002/jts.2490080106. [DOI] [PubMed] [Google Scholar]
- Brasel KJ, deRoon-Cassini TA, Bradley CT. Injury severity and quality of life: whose perspective is important? Journal of Trauma and Acute Care Surgery. 2010;68:263–268. doi: 10.1097/TA.0b013e3181caa58f. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Lanius RA, Novac A, Schnyder U, Galea S. Reformulating PTSD for DSM-V: Life after Criterion A. Journal of Traumatic Stress. 2009;22:366–373. doi: 10.1002/jts.20443. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Garvert DW, Brewin CR, Bryant RA, Maercker A. Evidence for proposed ICD-11 PTSD and complex PTSD: A latent profile analysis. European Journal of Psychotraumatology. 2013;4 doi: 10.3402/ejpt.v4i0.20706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- deRoon-Cassini TA, Mancini AD, Rusch MD, Bonanno GA. Psychopathology and resilience following traumatic injury: a latent growth mixture model analysis. Rehabiltation Psychology. 2010;55:1–11. doi: 10.1037/a0018601. [DOI] [PubMed] [Google Scholar]
- Dziak JJ, Coffman DL, Lanza ST, Li R. Sensitivity and specificity of information criteria. The Methodology Center and Department of Statistics, Penn State, The Pennsylvania State University. 2012:1–10. [Google Scholar]
- Elhai JD, Biehn TL, Armour C, Klopper JJ, Frueh BC, Palmieri PA. Evidence for a unique PTSD construct represented by PTSD’s D1–D3 symptoms. Journal of Anxiety Disorders. 2011;25:340–345. doi: 10.1016/j.janxdis.2010.10.007. [DOI] [PubMed] [Google Scholar]
- Forbes D, Lockwood E, Elhai JD, Creamer M, Bryant R, McFarlane A, O’Donnell M. An evaluation of the DSM-5 factor structure for posttraumatic stress disorder in survivors of traumatic injury. Journal of Anxiety Disorders. 2015;29:43–51. doi: 10.1016/j.janxdis.2014.11.004. [DOI] [PubMed] [Google Scholar]
- Friedman MJ. Finalizing PTSD in DSM-5: Getting here from there and where to go next. Journal of Traumatic Stress. 2013;26:548–556. doi: 10.1002/jts.21840. [DOI] [PubMed] [Google Scholar]
- Friedman MJ, Kilpatrick DG, Schnurr PP, Weathers FW. Correcting misconceptions about the diagnostic criteria for posttraumatic stress disorder in DSM-5. JAMA Psychiatry. 2016;73:753–754. doi: 10.1001/jamapsychiatry.2016.0745. [DOI] [PubMed] [Google Scholar]
- Gradus JL, Qin P, Lincoln AK, Miller M, Lawler E, Sørensen HT, Lash TL. Posttraumatic stress disorder and completed suicide. American Journal of Epidemiology. 2010;171:721–727. doi: 10.1093/aje/kwp456. [DOI] [PubMed] [Google Scholar]
- Guina J. Changes to the definition of posttraumatic stress disorder in the DSM-5. JAMA Psychiatry. 2016;73:1201–1202. doi: 10.1001/jamapsychiatry.2016.2381. [DOI] [PubMed] [Google Scholar]
- Hansen M, Hyland P, Armour C, Shevlin M, Elklit A. Less is more? Assessing the validity of the ICD-11 model of PTSD across multiple trauma samples. European Journal of Psychotraumatology. 2015;6 doi: 10.3402/ejpt.v6.28766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge CW, Riviere LA, Wilk JE, Herrell RK, Weathers FW. The prevalence of post-traumatic stress disorder (PTSD) in US combat soldiers: A head-to- head comparison of DSM-5 versus DSM-IV-TR symptom criteria with the PTSD checklist. The Lancet Psychiatry. 2014;1:269–277. doi: 10.1016/S2215-0366(14)70235-4. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Yehuda R, Castro CA, McFarlane AC, Vermetten E, Jetly R, Rauch SA. Unintended consequences of changing the definition of posttraumatic stress disorder in DSM-5: Critique and call for action. JAMA Psychiatry. 2016;73:750–752. doi: 10.1001/jamapsychiatry.2016.0647. [DOI] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural equation modeling: A Multidisciplinary Journal. 1999;6:1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Hyland P, Brewin CR, Maercker A. Predictive Validity of ICD-11 PTSD as Measured by the Impact of Event Scale-Revised: A 15-Year Prospective Study of Political Prisoners. Journal of Traumatic Stress. 2017;30:125–132. doi: 10.1002/jts.22171. [DOI] [PubMed] [Google Scholar]
- Karatzias T, Shevlin M, Fyvie C, Hyland P, Efthymiadou E, Wilson D, Cloitre M. An initial psychometric assessment of an ICD-11 based measure of PTSD and complex PTSD (ICD-TQ): Evidence of construct validity. Journal of Anxiety Disorders. 2016;44:73–79. doi: 10.1016/j.janxdis.2016.10.009. [DOI] [PubMed] [Google Scholar]
- Kass RE, Raftery AE. Bayes factors. Journal of the American Statistical Association. 1995;90(430):773–795. [Google Scholar]
- Kemp AH, Felmingham K, Das P, Hughes G, Peduto AS, Bryant RA, Williams LM. Influence of comorbid depression on fear in posttraumatic stress disorder: An fMRI study. Psychiatry Research: Neuroimaging. 2007;155:265–269. doi: 10.1016/j.pscychresns.2007.01.010. [DOI] [PubMed] [Google Scholar]
- King DW, Leskin GA, King LA, Weathers FW. Confirmatory factor analysis of the clinician-administered PTSD Scale: Evidence for the dimensionality of posttraumatic stress disorder. Psychological Assessment. 1998;10:90–96. doi: 10.1037/1040-3590.10.2.90. [DOI] [Google Scholar]
- Lanius RA, Frewen PA, Girotti M, Neufeld RW, Stevens TK, Densmore M. Neural correlates of trauma script-imagery in posttraumatic stress disorder with and without comorbid major depression: a functional MRI investigation. Psychiatry Research: Neuroimaging. 2007;155:45–56. doi: 10.1016/j.pscychresns.2006.11.006. [DOI] [PubMed] [Google Scholar]
- Liu P, Wang L, Cao C, Wang R, Zhang J, Zhang B, Fan G. The underlying dimensions of DSM-5 posttraumatic stress disorder symptoms in an epidemiological sample of Chinese earthquake survivors. Journal of Anxiety Disorders. 2014;28:345–351. doi: 10.1016/j.janxdis.2014.03.008. [DOI] [PubMed] [Google Scholar]
- Maercker A, Brewin CR, Bryant RA, Cloitre M, Ommeren M, Jones LM, Rousseau C. Diagnosis and classification of disorders specifically associated with stress: proposals for ICD-11. World Psychiatry. 2013;12:198–206. doi: 10.1002/wps.20057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moshagen M, Musch J. Sample size requirements of the robust weighted least squares estimator. Methodology: European Journal of Research Methods for the Behavioral and Social Sciences. 2014;10:60–70. doi: 10.1027/1614-2241/a000068. [DOI] [Google Scholar]
- Mueser KT, Rosenberg SD, Fox L, Salyers MP, Ford JD, Carty P. Psychometric evaluation of trauma and posttraumatic stress disorder assessments in persons with severe mental illness. Psychological Assessment. 2001;13:110–117. doi: 10.1037/1040-3590.13.1.110. [DOI] [PubMed] [Google Scholar]
- Muthén L, Muthén B. Mplus User’s Guide. Los Angeles, CA: Muthén & Muthén; 2015. [Google Scholar]
- O’Donnell ML, Alkemade N, Nickerson A, Creamer M, McFarlane AC, Silove D, …Forbes D. Impact of the diagnostic changes to post-traumatic stress disorder for DSM-5 and the proposed changes to ICD-11. The British Journal of Psychiatry. 2014;205:230–235. doi: 10.1192/bjp.bp.113.135285. [DOI] [PubMed] [Google Scholar]
- Pacella ML, Hruska B, Delahanty DL. The physical health consequences of PTSD and PTSD symptoms: A meta-analytic review. Journal of Anxiety Disorders. 2013;27:33–46. doi: 10.1016/j.janxdis.2012.08.004. [DOI] [PubMed] [Google Scholar]
- Paelecke-Habermann Y, Pohl J, Leplow B. Attention and executive functions in remitted major depression patients. Journal of Affective Disorders. 2005;89:125–135. doi: 10.1016/j.jad.2005.09.006. [DOI] [PubMed] [Google Scholar]
- Palmieri PA, Weathers FW, Difede J, King DW. Confirmatory factor analysis of the PTSD Checklist and the Clinician-Administered PTSD Scale in disaster workers exposed to the World Trade Center Ground Zero. Journal of Abnormal Psychology. 2007;116:329–341. doi: 10.1037/0021-843X.116.2.329. [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Tsai J, Armour C, Mota N, Harpaz-Rotem I, Southwick SM. Functional significance of a novel 7-factor model of DSM-5 PTSD symptoms: Results from the National Health and Resilience in Veterans Study. Journal of Affective Disorders. 2015;174:522–526. doi: 10.1016/j.jad.2014.12.007. [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Tsai J, Harpaz-Rotem I, Whealin JM, Southwick SM. Support for a novel five-factor model of posttraumatic stress symptoms in three independent samples of Iraq/Afghanistan veterans: a confirmatory factor analytic study. Journal of psychiatric research. 2012;46:317–322. doi: 10.1016/j.jpsychires.2011.11.013. [DOI] [PubMed] [Google Scholar]
- Reed GM, Correia JM, Esparza P, Saxena S, Maj M. The WPA-WHO global survey of psychiatrists’ attitudes towards mental disorders classification. World Psychiatry. 2011;10(2):118–131. doi: 10.1002/j.2051-5545.2011.tb00034.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarz G. Estimating the dimension of a model. The Annals of Statistics. 1978;6(2):461–464. [Google Scholar]
- Simms LJ, Watson D, Doebbelling BN. Confirmatory factor analyses of posttraumatic stress symptoms in deployed and nondeployed veterans of the Gulf War. Journal of Abnormal Psychology. 2002;111:637–647. doi: 10.1037//0021-843X.111.4.637. [DOI] [PubMed] [Google Scholar]
- Wang L, Zhang L, Armour C, Cao C, Qing Y, Zhang J, Zhao Z. Assessing the underlying dimensionality of DSM-5 PTSD symptoms in Chinese adolescents surviving the 2008 Wenchuan earthquake. Journal of Anxiety Disorders. 2015;31:90–97. doi: 10.1016/j.janxdis.2015.02.006. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, Keane TM. The Clinician-Administered PTSD Scale for DSM- 5 (CAPS-5) 2013 doi: 10.1037/pas0000486. Interview available from the National Center for PTSD at www.ptsd.va.gov. [DOI] [PMC free article] [PubMed]
- Weathers FW, Ruscio AM, Keane TM. Psychometric properties of nine scoring rules for the Clinician-Administered Posttraumatic Stress Disorder Scale. Psychological Assessment. 1999;11:124. doi: 10.1037/1040-3590.11.2.124. [DOI] [Google Scholar]
- Whalley MG, Rugg MD, Smith AP, Dolan RJ, Brewin CR. Incidental retrieval of emotional contexts in post-traumatic stress disorder and depression: An fMRI study. Brain and Cognition. 2009;69:98–107. doi: 10.1016/j.bandc.2008.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widaman KF, Thompson JS. On specifying the null model for incremental fit indices in structural equation modeling. Psychological Methods. 2003;8:16–37. doi: 10.1037/1082-989X.8.1.16. [DOI] [PubMed] [Google Scholar]
- Yufik T, Simms LJ. A meta-analytic investigation of the structure of posttraumatic stress disorder symptoms. Journal of Abnormal Psychology. 2010;119:764–776. doi: 10.1037/a0020981. [DOI] [PMC free article] [PubMed] [Google Scholar]


