Abstract
Trimethoprim-sulfamethoxazole (cotrimoxazole or TMP/SMX) is commonly used for the treatment of urinary or lower respiratory tract infections. A comprehensive review is presented of the world literature on adverse reactions to TMP/SMX since its first use in 1968, when concern was expressed about possible hematologic toxicity. The adverse reactions to TMP/SMX occur in approximately 1%–3% of persons in general population. Here, we report a case of oral erythema multiforme (EM) secondary to TMP/SMX that presented with oral and lip ulcerations typical of EM without any skin lesions and highlights the importance of distinguishing them from other ulcerative disorders involving oral cavity. The patient was treated symptomatically and given tablet prednisolone. The condition improved with stoppage of TMP/SMX therapy. It has been reported that primary attacks of oral EM is confined to the oral mucosa, but the subsequent attacks can produce more severe forms of EM involving the skin. Hence, it is important to identify for early diagnosis and management. Although EM is quite common with TMP/SMX, there are no reports of oral EM appearing after intake of this drug.
Keywords: Oral erythema multiforme, oral mucosa, trimethoprim-sulfamethoxazole, urinary tract infection, érythème polymorphe oral, muqueuse buccale, trimethoprim-sulfaméthoxazole, infection urinaire
Résumé
Le triméthoprime-sulfaméthoxazole (cotrimoxazole ou TMP / SMX) est couramment utilisé pour le traitement des voies respiratoires urinaires ou inférieures Les infections. Une revue détaillée de la littérature mondiale sur les effets indésirables de TMP / SMX depuis sa première utilisation en 1968, lorsque Des préoccupations ont été exprimées au sujet d’une éventuelle toxicité hématologique. Les réactions indésirables au TMP / SMX se produisent chez environ 1% à 3% des personnes population générale. Ici, nous rapportons un cas d’érythème polymorphe oral (EM) secondaire à TMP / SMX qui présentait des ulcérations orales et lombaires Typique de l’EM sans aucune lésion cutanée et met en évidence l’importance de les distinguer des autres troubles ulcératifs impliquant des voies orales cavité. Le patient a été traité de façon symptomatique et administré une prednisolone au comprimé. La condition s’est améliorée avec l’arrêt de la thérapie TMP / SMX. Il a été signalé que les attaques primaires d’EM oral se limitent à la muqueuse buccale, mais les attaques suivantes peuvent produire des formes plus sévères De EM impliquant la peau. Par conséquent, il est important d’identifier le diagnostic et la gestion précoces. Bien que EM soit assez courant avec TMP/SMX, il n’y a pas de rapports d’EM oral apparaissant après l’admission de ce médicament.
INTRODUCTION
Erythema multiforme (EM) is an acute inflammatory disorder that affects skin and mucous membranes or both. The precipitating and triggering factors are divided into two large categories, infection and drugs. Other occasional factors include malignancy, vaccination, autoimmune disease, and radiotherapy. Infections commonly include Herpes simplex virus infection (Types 1 and 2), tuberculosis and histoplasmosis. Causative drugs comprise barbiturates, sulfonamides, and antiseizure medications such as carbamazepine and phenytoin. Vaccinations include Bacillus Calmette–Guérin, Diphtheria - Pertussis - Tetanus, measles-mumps-rubella, hepatitis B, meningitis, smallpox, human papillomavirus, pneumococcal, and rabies.[1] Based on the severity and the number of mucosal sites involved the disease has been subclassified into EM minor and major. Typical target skin lesions are necessary along with mucosal ulcerations to consider diagnosing them as EM minor and major. A severe variant termed Stevens–Johnson syndrome usually involves the skin extensively.[2] Many investigators have reported cases of oral mucosal ulcerations and lip lesions typical of EM without any skin lesions. They have classified them into a new category called oral EM.[3] It has been reported that even if the primary attacks of oral EM are confined to the oral mucosa, the subsequent attacks can produce more severe forms of EM involving the skin. Hence, it is important to identify and distinguish them from other ulcerative disorders involving oral cavity for early management and proper follow-up.[4,5] Trimethoprim-sulfamethoxazole (TMP/SMX) is a widely prescribed antibiotic for the management of several uncomplicated infections. It is prescribed in many parts of rural India and many general dental practitioners do not know about this drug. We herein report a female with acute pyelonephritis who developed oral EM while receiving TMP/SMX therapy.
CASE REPORT
A 20-year-old female presented with complaint of superficial erosions and burning sensation in oral cavity for 5 days, swelling, crusting, and bleeding over lips and difficulty in swallowing for 4 days. Eight days back she was started on oral TMP/SMX (160/800 mg [1 double strength tablet] twice daily by a private physician for urinary tract infection). There was no history of abdominal pain, urinary complaints, breathlessness, or cough. On examination, heart rate was 110/min, respiratory rate was 24/min and blood pressure was 110/70 mmHg. Intraoral examination showed extensive, irregular ulcerations with yellow base and erythematous borders on buccal mucosa, palate, dorsal, and ventral surfaces of the tongue. On extraoral examination, both upper and lower lips showed extensive irregular ulcerations and cracking and fissuring with blood encrustation [Figure 1]. Nikolsky's sign was negative. Systemic examination was normal. A clinical diagnosis of TMP/SMX-induced oral EM was made. This can be considered as a “probable” adverse drug reaction (ADR) as per causality assessment, on Naranjo scale.[6] Biopsy was taken from buccal mucosa and for culture test; sample was collected from mucosal lesions. Patient was advised to discontinue the TMP/SMX therapy and was treated with oral antihistamines, analgesics, and topical triamcinolone acetonide gel (0.1%) for the oral ulcers. After this, patient was referred for laboratory investigations. The pathology report which came on the next day stated an EM-type drug eruption. Histopathological report showed lymphocytic infiltrate at the epithelial-connective tissue junction and around blood vessels with edema and subepidermal bullae formation [Figure 2]. Her hematological investigation which was came after 3 days showed neutrophilia and eosinophilia. C-reactive protein was positive and the erythrocyte sedimentation rate was elevated. Serology tests confirmed that the patient was negative for herpes virus infection. Furthermore, the culture test came as negative. Liver function tests, renal function tests, and serum electrolytes were normal. HIV – enzyme-linked immunosorbent assay was negative. Depending on the history, clinical examination and laboratory investigations, a final diagnosis of drug-induced oral EM was given. Patient was then prescribed corticosteroids (prednisolone 10 mg) twice a day for 3 days followed by tapering dose for 10 days. By the end of the 3rd week, there was no evidence of mucosal lesions. Rechallenge with TMP/SMX was not performed. On follow-up, after 4 months, she is asymptomatic.
Figure 1.

Erosion with bleeding on the tongue. Edematous lips with hemorrhagic crusts and purulent discharge
Figure 2.
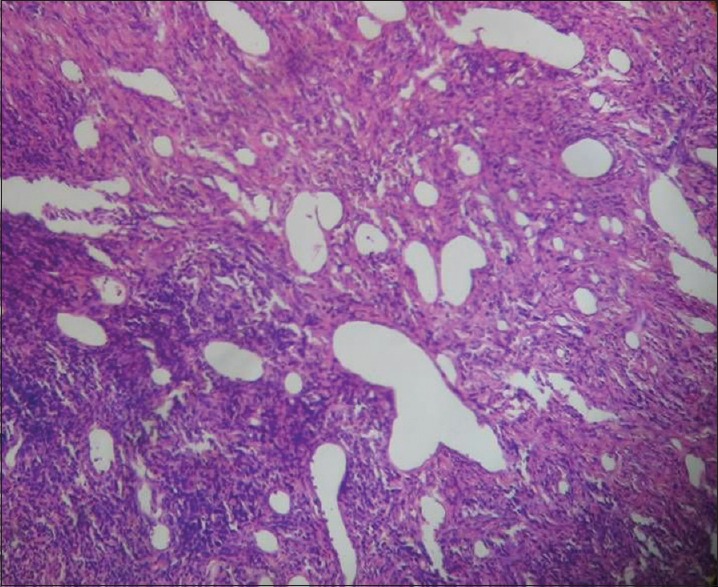
Histopathological picture shows lymphocytic infiltrate around blood vessels
DISCUSSION
An ADR is defined by the World Health Organization as “a response to a medicine which is noxious and unintended and occurs at doses normally used in man for the prophylaxis, diagnosis or therapy of disease, or for the modification of physiological function.”[7] In immunocompetent persons, the rate of ADRs to cotrimoxazole is only 1%–3%.[8] A PubMed search using the keywords “TMP/SMX” and “oral EM” revealed that no such case is reported in literature till date. Adverse reactions to systemic drug administration can have different clinical patterns such as EM minor, major, Steven Johnson's syndrome, anaphylactic stomatitis, intraoral fixed drug eruptions, lichenoid drug reactions, and pemphigoid-like drug reactions.[9] According to von Hebra, who first described EM in 1866, the patients with EM should have acrally distributed typical target lesions or raised edematous skin papules with or without mucosal involvement.[10] In 1968, Kenneth described an inflammatory oral disorder with oral lesions typical of EM but without any skin involvement. He reported nine cases seen at the Eastman Dental Hospital. The common sites involved were lips, cheeks, and tongue. These patients had irregular large ulcers with necrotic tags attached to the borders. When lips are involved the typical blood encrusted lesions were seen. In this series of cases, the typical target skin lesions were seen during the recurrences not in their initial attacks.[4] Many investigators have suggested this as a third category of EM known as oral EM that is characterized by typical oral lesions of EM but no target skin lesions. Oral EM is a distinct but less well-recognized variant of EM. The diagnosis has to be established by excluding other oral inflammatory and vesiculobullous lesions.[3] In the present case, patient showed extensive irregular erythematous ulcerations in the buccal mucosa, labial mucosa, tongue, palate, and lips with blood encrustation. The diagnosis was established based on the positive drug history, clinical appearance, and distribution of the lesion and exclusion of other ulcerative lesions. Differential diagnosis includes herpes, autoimmune vesiculobullous lesions such as pemphigus vulgaris or bullous pemphigoid and other patterns of drug reactions. Herpetic lesions are more common in the keratinized mucosa, especially the gingiva. Our case did not have any gingival ulceration. Herpetic ulcers are smaller with regular borders than ulcers associated with EM. Extensive irregular ulcerations in the lining nonkeratinized mucosa as seen in our patients were typical of EM and are not a feature of herpes infection. The presence of a temporal relationship between the drug intake and onset of the disease excludes the possibility of any infectious etiologies.[4] The positive drug histories associated with onset of ulcerations in our cases ruled out the possibility of other autoimmune vescicullobullous lesions such as pemphigus vulgaris. Unlike pemphigus vulgaris oral EM have an acute onset and does not show any desquamative gingivitis.[5] Bullous lichen planus lesions that may have similar ulcerations should have Wickham's striae, which were absent in our cases excluding it as the diagnosis.[4]
Other patterns of drug reactions such as lichenoid drug reactions, pemphigoid-like drug reactions that resemble their namesake can be easily differentiated based on the clinical patterns as abovementioned. Anaphylactic stomatitis often shows urticarial skin reactions with other signs and symptoms of anaphylaxis which were absent in our case. In mucosal fixed drug eruptions, the lesions are confined to localized areas of oral mucosa but in our case there were wide spread lesions affecting labial, buccal, palatal, and tongue mucosa along with lip involvement.[9] Since our cases were evidently triggered by drug intake and they had typical lesions of EM in the oral mucosa and lips without skin involvement, we came to a diagnosis of oral EM.
Adverse reactions to TMP/SMX are due to the hydroxylamine derivative of sulphamethaxazole, i.e., sulphamethaxazole hydroxylamine. EM seems to result from a T-cell-mediated immune reaction to the precipitating agent, which leads to a cytotoxic immunological attack on keratinocytes that express nonself antigens, with subsequent subepithelial and intraepithelial vesiculation, this leads to widespread blistering and erosions.[2]
Treatment of oral EM is symptomatic and involves treating the underlying causes. However, use of topical steroids and short course of systemic prednisone have been reported to very effective in controlling lesions of oral EM as supported by the dramatic response in our patient. In patients with severe life-threatening adverse reaction to TMP/SMX, alternative drug should be given. However, those who do not tolerate or have recurrent infections despite alternative therapy could be subjected to a trial of desensitization to TMP/SMX under close supervision.[11]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Regezi J, Sciubba J, Jordan R, editors. Oral Pathology Clinical Pathologic Correlations. 7th ed. St. Louis, Missouri: Elsevier; 2016. Ulcerative conditions; pp. 43–6. [Google Scholar]
- 2.Scully C, Bagan J. Oral mucosal diseases: Erythema multiforme. Br J Oral Maxillofac Surg. 2008;46:90–5. doi: 10.1016/j.bjoms.2007.07.202. [DOI] [PubMed] [Google Scholar]
- 3.Ayangco L, Rogers RS., 3rd Oral manifestations of erythema multiforme. Dermatol Clin. 2003;21:195–205. doi: 10.1016/s0733-8635(02)00062-1. [DOI] [PubMed] [Google Scholar]
- 4.Kennett S. Erythema multiforme affecting the oral cavity. Oral Surg Oral Med Oral Pathol. 1968;25:366–73. doi: 10.1016/0030-4220(68)90010-8. [DOI] [PubMed] [Google Scholar]
- 5.Bean SF, Quezada RK. Recurrent oral erythema multiforme. Clinical experience with 11 patients. JAMA. 1983;249:2810–2. [PubMed] [Google Scholar]
- 6.Zaki SA. Adverse drug reaction and causality assessment scales. Lung India. 2011;28:152–3. doi: 10.4103/0970-2113.80343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hallas J, Harvald B, Gram LF, Grodum E, Brøsen K, Haghfelt T, et al. Drug related hospital admissions: The role of definitions and intensity of data collection, and the possibility of prevention. J Intern Med. 1990;228:83–90. doi: 10.1111/j.1365-2796.1990.tb00199.x. [DOI] [PubMed] [Google Scholar]
- 8.Daftarian MP, Filion LG, Cameron W, Conway B, Roy R, Tropper F, et al. Immune response to sulfamethoxazole in patients with AIDS. Clin Diagn Lab Immunol. 1995;2:199–204. doi: 10.1128/cdli.2.2.199-204.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Neville BW, Damm D, Allan CM, Bouquot JE, editors. Oral and Maxillofacial Pathology. 2nd ed. Philadelphia, PA: Saunders; 2002. Allergic and immunologic diseases; pp. 285–314. [Google Scholar]
- 10.Assier H, Bastuji-Garin S, Revuz J, Roujeau J. Erythema multiforme with mucous membrane involvement and Steven-Johnson syndrome are clinically different disorders with distinct disorders. Arch Dermatol. 1995;131:539–43. [PubMed] [Google Scholar]
- 11.Douglas R, Spelman D, Czarny D, O’Hehir RE. Successful desensitization of two patients who previously developed Stevens-Johnson syndrome while receiving trimethoprim-sulfamethoxazole. Clin Infect Dis. 1997;25:1480. doi: 10.1086/516995. [DOI] [PubMed] [Google Scholar]


