Abstract
Background:
Currently, depression among medical students is an important health issue at the global level. There is also a paucity of information on its relation to the stress level.
Objective:
The aim of this study is to assess the prevalence of depression and its relation to stress level and other factors among medical students.
Materials and Methods:
A cross-sectional study was conducted among medical students at a tertiary care medical institution in Puducherry, coastal south India. Beck Depression Inventory Scale was used for screening of depression and Cohen's Perceived Stress scale to assess perceived stress level. Data on associated factors were collected by self-administered questionnaire.
Results:
The overall prevalence of depression was found to be 48.4% (215/444). According to the cutoff scores, 229 (51.6%) students scored as normal (0–9), 149 (33.6%) as mild (10–18), 60 (13.5%) as moderate (19–29), 3 (0.7%) as severe (30–40), and 3 (0.7%) students scored as very severe (>40) depression. Depression was significantly less among those with mild stress (adjusted odds ratio [OR] = 0.010) and moderate stress level (adjusted OR = 0.099) compared to severe stress level and those without interpersonal problems (adjusted OR = 0.448).
Conclusion:
Depression is more common among medical students. Stress coping mechanisms and improvement of interpersonal relationship may help to reduce depressive symptoms among medical students.
Keywords: Depression, India, medical students, perceived stress
Recently, the medical student population is increasing every year, especially in developing countries including India. Change in lifestyle because of urbanization and globalization coupled with high-level competition in the medical field could lead to increase in stress and depression among medical students. Depression in younger age group may lead to serious developmental and functional consequences like an academic failure or persistent psychosocial problems.[1]
There are studies which quantify the problem of depression among medical students in developing countries.[2,3,4,5,6,7,8] However, there are few studies conducted in developed countries to ascertain the stress as an associated factor for depression[9,10] and information in this regard is lacking from developing countries like India. Brazil study highlighted the fact that depressive symptoms were 7.43 times more among those with emotional stress.[10] Some stressful life events related to social activities were associated with the higher depression scores for medical students.[11]
There are also various other factors such as social and interpersonal factors associated with depressive symptoms among the medical students. A Korean study showed that low levels of perceived interpersonal support increased the risk of depression by more than ten times.[12] A recent study showed that age, study year, satisfaction with major, parental relationship, and mother's education were also significantly associated with depression among medical students.[13] Smoking, alcohol use, family history of depression, academic achievement, interpersonal problems, problems in the family were also found to be associated with depression among medical students.[3] In view of the above, it is important to look for the association of these factors in depressive symptoms among the medical students.
The risk factor exposure may differ in different geographical locations and hence that its magnitude as causation for the depression may vary in different locations. In this context, identification of the magnitude of the problem and associated factors of depression helps in taking appropriate interventional measures among medical students. With this background, the present study was conducted to assess the prevalence of depression and its relation to stress level and certain associated factors among medical students.
MATERIALS AND METHODS
Study design and setting
A cross-sectional study was conducted during January 2012 to June 2013 among medical students at a tertiary care medical institution in Puducherry, coastal south India.
Ethical issues
The study was approved by the scientific and ethical committee of the institute. Before permission was obtained from the Dean of the Institute. Written informed consent was obtained from the participants.
Sample size estimation
By considering the prevalence of depression among medical students as 71%[3] and absolute precision at 5% level, sample size was 330. After adding a nonresponse rate of 10%, total required minimum sample size was 363.
Sampling procedure
The study included all the 500 medical students as subjects studying from the 1st to 5th year of the study. The participant were explained the objectives of the study before initiating the study. They were assured confidentiality and given the option to participate in the study. Subjects who refused to participate in the study or who were absent on the day of study and/or could not be contacted even after two visits were considered as nonrespondents.
Study tools
The Beck Depression Inventory Scale was used for screening depression among medical students which was tested and validated.[14,15] This screening instrument assesses depressive symptoms based on subjective nature, and therefore, the participantshas to be further evaluated to confirm the diagnosis. The cutoff value of 10 and above were considered to define the depression among medical students.[3] According to the cutoff scores, students were classified as normal (0–9), mild (10–18), moderate (19–29), severe (30–40), and very severe (>40) depression.
The assessment of perceived stress level was performed using Cohen's Perceived Stress scale[16] and classified into low (0–11), average (12–15), high (16–20), and very high (21 and above) based on the total stress score.
Method of data collection
The investigators collected the data by using a self-administered semi-structured questionnaire which included variables on age, sex, class studying, social factors such as alcohol and tobacco use, interpersonal problems, family problems, family history of depression, and marks obtained in the previous examination. Perceived stress level and depression were assessed by using standard instruments. Any subject with at least one unit of alcohol intake at least once in the past 12 months was considered as alcohol user in the current study. The presence of family problem was assessed as any perceived worries by the subject regarding the particular family problem. The family history of depression was assessed based on earlier diagnosis among first or second degree relatives.
Data analysis
Data were entered and analyzed by using Statistical Package for Social Sciences (IBM PASW Statistics- version 19.0, Chicago) for windows. Data were expressed in terms of proportion or percentages. Univariate analysis was used to test the association between depression and variables. Multiple logistic regression analysis was carried out to look for the independent association of variables with the depression. The value of P < 0.05 was considered as statistically significant.
RESULTS
A total of 444 students participated in the study with a response rate of 88.8%. There were 228 (51.4%) males and 216 (48.6%) females. The overall prevalence of depression was found to be 48.4%. According to the cutoff scores, 229 (51.6%) students scored as normal (0–9), 149 (33.6%) as mild (10–18), 60 (13.5%) as moderate (19–29), 3 (0.7%) as severe (30–40), and 3 (0.7%) as very severe (>40) depression. Among those with depression, a majority (97.2%) had a mild and moderate degree of depression. It was found that 83.7% of the subjects (372/444) had moderate, high, and very high-stress level. The prevalence of depression was 84.8% (140/165) among the subjects who had moderate, high, and very high-stress level.
The present study showed that depression prevalence was similar in both sexes (Males-109/229 = 47.8% and Females- 106/216 = 49.1%) and the association between the grade of depression and sex was not statistically significant (χ2 = 2.39, P = 0.793) [Table 1]. The prevalence of depression was more in the 2nd year students (66.3%) compared to other class students and the difference found between the grade of depression and year of studying was statistically significant (χ2 = 47.142, P = 0.001) [Table 2].
Table 1.
Grading of depression according to sex
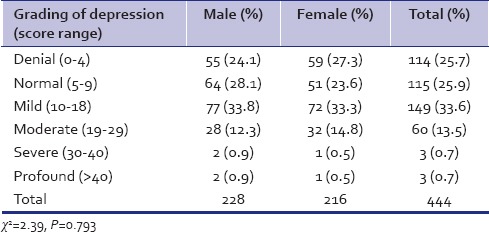
Table 2.
Grading of depression according to classes
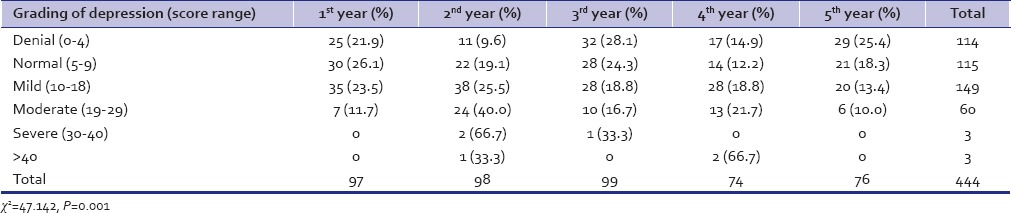
About half (52.3%, 81/155) of those aged 17–18 years were depressed followed by 21–24 years (46.5%, 67/144) and 19–20 years (46.2%, 67/145). Depression was more common in the 2nd year of the study (66.3%, 65/98) followed by 4th year (58.1%, 43/74), 1st year (43.3%, 42/97), 3rd year (39.4%, 39/99) and 5th year (34.2%, 26/76) of the study and the difference was found to be statistically significant (χ2 = 25.755, P = 0.000). Prevalence of depression was found to be 54.8% (51/93) among subjects whose mothers education level was 1st to 12th standard compared to 46.7% (164/351) of the subjects whose mothers education level was graduation and above and it was not found to be statistically significant (χ2 = 1.939, P = 0.164).
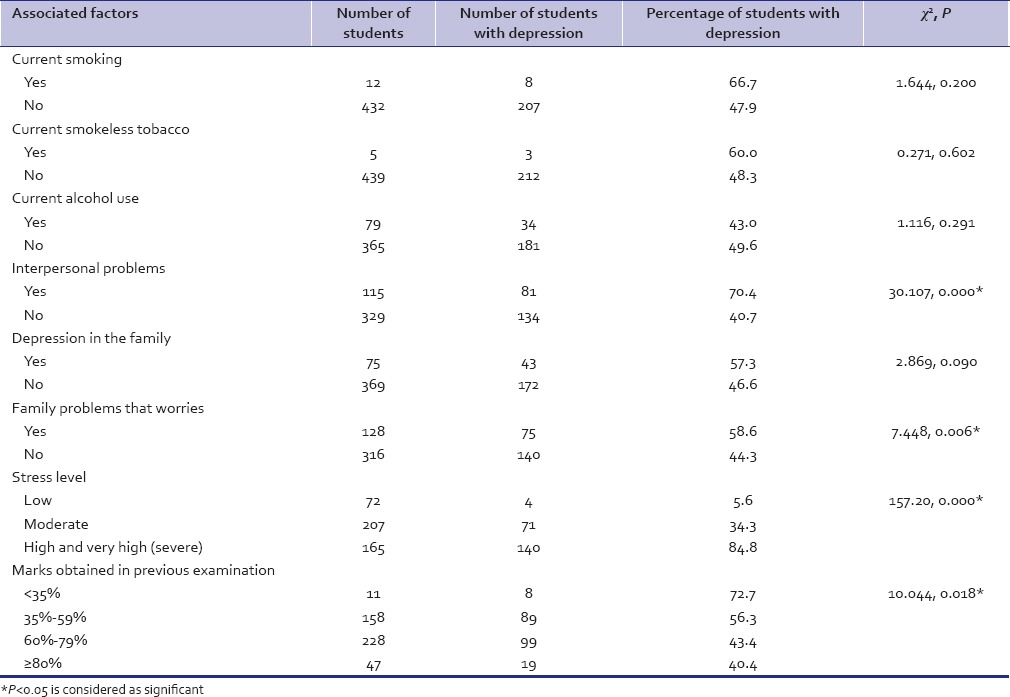
Univariate analysis showed that year of studying, interpersonal problems, family problems that worries, stress level, and marks obtained in the previous examination were associated significantly with depression [Table 3]. Multiple logistic regression analysis where all the variables (age, sex, year of studying, education of father and mother, occupation of father and mother, current smoking, tobacco use, alcohol use, family history of depression, interpersonal problems, family problems, stress level and marks obtained in the previous examination) were included showed that having mild stress (adjusted odds ratio [OR] = 0.010) and moderate stress (adjusted OR = 0.099) level compared to high and very high (severe) stress and absence of interpersonal problems (adjusted OR = 0.448) were significantly associated with depression among medical students.
Table 3.
Prevalence of depression according to associated factors
DISCUSSION
This study showed that 48.4% of the medical students had depressive symptoms. The prevalence rate of depression in our study was found to be comparatively more than other studies.[5,6,9,13,17,18,19,20,21,22] A recent study from China reported the prevalence of depression as 11.7% which was lesser than our study.[13] The proportion of participants with severe (0.7%) and very severe depression (0.7%) in this study was lesser compared to another Indian study which reported it as 7.5% and 6.7%, respectively.[3] The study finding is consistent with another Indian study which showed the prevalence rate of depression among medical students as 45.3%.[4] A study from Pakistan also showed similar findings with the prevalence rate as 43.9%.[7] A recent study from Brazil found the prevalence of depression among medical students as 40.5% with 1.2% had very severe depressive symptoms.[10] The higher prevalence in our study compared to some of the above studies may be because of difference in the methodology adopted, instruments used for the screening, low cutoff values used for the definition of depression and socioeconomic background characteristics of the medical students.
Depression is comparatively more (66.3%) in the 2nd year in contrast to a French study which reported that depression is comparatively more in 4th year with 44.3% prevalence rate.[23] Although other studies found the depression prevalence significantly more among females (8.1% among males vs. 16.1% among females,[9] 9% among males vs. 18% among females,[22] female gender vs. male gender with OR of 1.85[24]) this study could not find any statistical difference for the prevalence rate of 49.1% for females and 47.8% for males (χ2 = 2.39, P = 0.793). This observation may be because of other influencing factors affecting depression and different methodology adopted in other studies.
A study showed that parental relationship and mother's education status were significantly associated with depression, but this study could not find any statistical difference.[13] The study showed that students with poor school performance had more chances of depressive symptoms with those who scored < 35% in the previous examination had 72.7% prevalence rate of depression. A study in Turkey showed that prevalence of depression was 62.9% among those with poor school performance students compared to an overall prevalence rate of 26.2%.[18] Another study showed that depression odds is 2.13 times higher among those with dissatisfaction for own academic performance compared to those who are not dissatisfied.[20] This study could not find the association of substance use with depressive symptoms in contrast to other studies.[8,21] This may be because of smaller sample size related to alcohol and tobacco use in this study.
The current study has got some limitations. The study findings may not be generalizable to students of other medical institutions because of difference in medical seat admission process and academic level policies. Due to the cross-sectional study nature, temporal relationship of the risk factors with depression may not be ascertained.[25] Certain factors such as physical activity level, sleep pattern were not analyzed. Adequate sample size, inclusion of all the classes, assessment of depression and stress level based on standard instruments, detailed evaluation of personal and social factors were the strengths of the study.
CONCLUSION
Depression symptoms are more common among medical students. About 83.7% of the medical students had moderate, high, and very high-stress level and the prevalence of depression was 84.8% (140/165) among the subjects who had moderate, high, and very high-stress level. Furthermore, prevalence was found to be more among those with interpersonal problems (70.4%) compared to those without interpersonal problems (40.7%). In view of the above, stress alleviation and improvement of interpersonal relationship may help to reduce the depressive symptoms in medical students.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank the Dean of the institute for permitting us to conduct the study and the subjects participated in the study.
REFERENCES
- 1.Mojs E, Warchoł-Biedermann K, Głowacka MD, Strzelecki W, Ziemska B, Marcinkowski JT, et al. Are students prone to depression and suicidal thoughts? Assessment of the risk of depression in university students from rural and urban areas. Ann Agric Environ Med. 2012;19:770–4. [PubMed] [Google Scholar]
- 2.Waghachavare VB, Dhumale GB, Kadam YR, Gore AD. A study of stress among students of professional colleges from an urban area in India. Sultan Qaboos Univ Med J. 2013;13:429–36. [PMC free article] [PubMed] [Google Scholar]
- 3.Kumar GS, Jain A, Hegde S. Prevalence of depression and its associated factors using Beck Depression Inventory among students of a medical college in Karnataka. Indian J Psychiatry. 2012;54:223–6. doi: 10.4103/0019-5545.102412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gupta S, Basak P. Depression and type D personality among undergraduate medical students. Indian J Psychiatry. 2013;55:287–9. doi: 10.4103/0019-5545.117151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Basnet B, Jaiswal M, Adhikari B, Shyangwa PM. Depression among undergraduate medical students. Kathmandu Univ Med J (KUMJ) 2012;10:56–9. doi: 10.3126/kumj.v10i3.8021. [DOI] [PubMed] [Google Scholar]
- 6.Aniebue PN, Onyema GO. Prevalence of depressive symptoms among Nigerian medical undergraduates. Trop Doct. 2008;38:157–8. doi: 10.1258/td.2007.070202. [DOI] [PubMed] [Google Scholar]
- 7.Jadoon NA, Yaqoob R, Raza A, Shehzad MA, Zeshan SC. Anxiety and depression among medical students: A cross-sectional study. J Pak Med Assoc. 2010;60:699–702. [PubMed] [Google Scholar]
- 8.Khan MS, Mahmood S, Badshah A, Ali SU, Jamal Y. Prevalence of depression, anxiety and their associated factors among medical students in Karachi, Pakistan. J Pak Med Assoc. 2006;56:583–6. [PubMed] [Google Scholar]
- 9.Dahlin M, Joneborg N, Runeson B. Stress and depression among medical students: A cross-sectional study. Med Educ. 2005;39:594–604. doi: 10.1111/j.1365-2929.2005.02176.x. [DOI] [PubMed] [Google Scholar]
- 10.Costa EF, Santana YS, Santos AT, Martins LA, Melo EV, Andrade TM, et al. Depressive symptoms among medical intern students in a Brazilian public university. Rev Assoc Med Bras (1992) 2012;58:53–9. [PubMed] [Google Scholar]
- 11.Aktekin M, Karaman T, Senol YY, Erdem S, Erengin H, Akaydin M, et al. Anxiety, depression and stressful life events among medical students: A prospective study in Antalya, Turkey. Med Educ. 2001;35:12–7. doi: 10.1046/j.1365-2923.2001.00726.x. [DOI] [PubMed] [Google Scholar]
- 12.Jeong Y, Kim JY, Ryu JS, Lee KE, Ha EH, Park H, et al. The associations between social support, health-related behaviors, socioeconomic status and depression in medical students. Epidemiol Health. 2010;32:e2010009. doi: 10.4178/epih/e2010009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen L, Wang L, Qiu XH, Yang XX, Qiao ZX, Yang YJ, et al. Depression among Chinese university students: Prevalence and socio-demographic correlates. PLoS One. 2013;8:e58379. doi: 10.1371/journal.pone.0058379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Basker M, Moses PD, Russell S, Russell PS. The psychometric properties of Beck Depression Inventory for adolescent depression in a primary-care paediatric setting in India. Child Adolesc Psychiatry Ment Health. 2007;1:8. doi: 10.1186/1753-2000-1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 16.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- 17.Ibrahim N, Al-Kharboush D, El-Khatib L, Al-Habib A, Asali D. Prevalence and predictors of anxiety and depression among female medical students in King Abdulaziz University, Jeddah, Saudi Arabia. Iran J Public Health. 2013;42:726–36. [PMC free article] [PubMed] [Google Scholar]
- 18.Bostanci M, Ozdel O, Oguzhanoglu NK, Ozdel L, Ergin A, Ergin N, et al. Depressive symptomatology among university students in Denizli, Turkey: Prevalence and sociodemographic correlates. Croat Med J. 2005;46:96–100. [PubMed] [Google Scholar]
- 19.Mancevska S, Bozinovska L, Tecce J, Pluncevik-Gligoroska J, Sivevska-Smilevska E. Depression, anxiety and substance use in medical students in the Republic of Macedonia. Bratisl Lek Listy. 2008;109:568–72. [PubMed] [Google Scholar]
- 20.Pereyra-Elías R, Ocampo-Mascaró J, Silva-Salazar V, Vélez-Segovia E, Costa-Bullón AD, Toro-Polo LM, et al. Prevalence and associated factors with depressive symptoms in Health Sciences students from a private university in Lima, Peru 2010. Rev Peru Med Exp Salud Publica. 2010;27:520–6. doi: 10.1590/s1726-46342010000400005. [DOI] [PubMed] [Google Scholar]
- 21.Mackenzie S, Wiegel JR, Mundt M, Brown D, Saewyc E, Heiligenstein E, et al. Depression and suicide ideation among students accessing campus health care. Am J Orthopsychiatry. 2011;81:101–7. doi: 10.1111/j.1939-0025.2010.01077.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schwenk TL, Davis L, Wimsatt LA. Depression, stigma, and suicidal ideation in medical students. JAMA. 2010;304:1181–90. doi: 10.1001/jama.2010.1300. [DOI] [PubMed] [Google Scholar]
- 23.Mehanna Z, Richa S. Prevalence of anxiety and depressive disorders in medical students. Transversal study in medical students in the Saint-Joseph University of Beirut. Encephale. 2006;32:976–82. doi: 10.1016/s0013-7006(06)76276-5. [DOI] [PubMed] [Google Scholar]
- 24.Kaya M, Genç M, Kaya B, Pehlivan E. Prevalence of depressive symptoms, ways of coping, and related factors among medical school and health services higher education students. Turk Psikiyatri Derg. 2007;18:137–46. [PubMed] [Google Scholar]
- 25.Park K. Principles of epidemiology and epidemiologic methods. In: Park K, editor. Park's Textbook of Preventive and Social Medicine. 22nd ed. Jabalpur, India: Banarsidas Bhanot Publishers; 2013. p. 67. [Google Scholar]


