Abstract
Endothelial progenitor cells (EPCs) are an important component of stem-cell niches, which are able to promote the self-renewal and pluripotency of mesenchymal stem cells (MSCs). The biological functions of these two cell types is dependent on adhesion, and the adhesion between MSCs and EPCs is important due to their critical role in neovascularization and bone regeneration in tissue engineering. Intercellular adhesion molecule-1 (ICAM-1, also known as cluster of differentiation 54), is a member of the immunoglobulin supergene family, which functions in cell-cell and cell-matrix adhesive interactions. Compared with other adhesion molecules, ICAM-1 is expressed in hematopoietic and nonhematopoietic cells, and can mediate adhesive interactions. The present study aimed to investigate the importance of ICAM-1 in the adhesion of MSCs and EPCs, and demonstrated that adhesion between these cells could be regulated by interleukin (IL)-1β via the p38 mitogen-activated protein kinase pathway. In addition, the results confirmed that ICAM-1 served a critical role in regulation of adhesion between MSCs and EPCs. ELISA, cell immunofluorescence, western blot analysis and adhesion assay were used to confirm our theory from phenomenon to essence. The present study provided evidence to support and explain the adhesion between MSCs and EPCs. Furthermore, the present findings provide a theoretical basis for further stem-cell niche transplantation to increase understanding of the function of MSCs and the crosstalk between MSCs and EPCs in the stem-cell niche.
Keywords: mesenchymal stem cells, endothelial progenitor cells, adhesion, stem-cell niche, interleukin-1β, intercellular adhesion molecule-1, p38 mitogen-activated protein kinase signaling pathway
Introduction
Mesenchymal stem cells (MSCs) are multipotent stem cells derived from the bone marrow (BM), which can differentiate into osteoblasts, chondrocytes and adipocytes (1–3). Therefore, MSCs are considered as the most important seed cells for tissue engineering. Maintenance of the self-renewing and multipotent properties of MSCs is regulated by molecular signals from the specific microenvironment where they reside, which is also known as the stem-cell niche (4–6).
Our previous study reported that MSCs exhibit high levels of interaction with cluster of differentiation (CD)31+ endothelial progenitor cells (EPCs) in the BM microenvironment, thus forming cell clusters in the sinus of the BM cavity (7). Therefore, it was hypothesized that EPCs are a significant component of stem-cell niches, which may promote the self-renewing and multipotent properties of MSCs. EPCs (8–10) reside in niches located in the BM and assist in homeostasis by maintaining vascular function. In addition, combination of EPCs with MSCs has been reported to enhance neovascularization and bone regeneration (11–14). These findings provided a novel basis for clinical bone injury treatment and vascular bone regeneration; however, what mediates the adhesion between MSCs and EPCs, and the underlying molecular mechanism, remain unclear.
Intercellular adhesion molecule-1 (ICAM-1, also known as CD54) is a member of the immunoglobulin supergene family, and functions in cell-cell and cell-matrix adhesive interactions. Compared with other adhesion molecules, ICAM-1 is expressed in hematopoietic and nonhematopoietic cells, and can mediate adhesive interactions (15–18). Interleukin (IL)-1β is an important inflammatory mediator that regulates the expression of ICAM-1 (19–21), and serves as a hallmark for bone damage (22–25) and vascular injury (26,27). Therefore, investigating the effects of IL-1β on ICAM-1, and the effects of ICAM-1 on cohesion between MSCs and EPCs may contribute to further understanding of stem-cell niche adhesion. Nevertheless, adhesion is mediated by numerous intracellular signaling pathways. Previous studies have suggested that the p38 mitogen-activated protein kinase (MAPK) pathway has a critical role in the expression of ICAM-1, and IL-1β has been reported to activate the p38 MAPK pathway (28–31). Therefore, the present study hypothesized that the p38 MAPK signaling pathway may be important in the crosstalk between MSCs and EPCs in the stem-cell niche.
Materials and methods
Animal preparation and cell culture
A total of 24 male C57BL/6J (wild-type) mice (age, 6–8 weeks; weight, 28–35 g) were used to obtain cells for use in the present study. All mice were purchased from Xinjiang Medical University (Ürümqi, China; certificate no. SYXK [Xin] 2010-0001). The mice were maintained in the Animal Facility of the Shihezi University (Shihezi, China) under controlled conditions (temperature, 20°C; humidity, 55±5%; 12-h light/dark cycles), with free access to food and water and were used as a cell source. All mice used in the present study were matched for age and gender. Both isolated cell types underwent similar techniques with regards to culture and harvest; however, the media and materials used for culture were different between the cell types. Third generation cells were used for all experiments. All experimental protocols used in the present study were reviewed and approved by the Animal Care and Use Committee of Shihezi University.
Isolation and culture of MSCs and EPCs from murine BM
MSCs and EPCs were isolated from murine BM obtained from the tibia and femur according to our previous study (7). Briefly, mice (C57BL/6J; age, 6–8 weeks) were euthanized by cervical dislocation and BM cells were collected. The cells were cultured in low glucose Dulbecco's modified Eagle's medium (LG-DMEM) supplemented with 10% lot-selected fetal bovine serum (FBS) (both from Gibco; Thermo Fisher Scientific, Inc., Waltham, MA, USA), 2 mM glutamine, 100 U/ml penicillin and 100 µg/ml streptomycin (all from Sigma-Aldrich; Merck KGaA, Darmstadt, Germany) at 37°C in a humidified incubator containing 5% CO2 for 48 h of adhesion. Subsequently, non-adherent cells were collected and cultured in EBM-2 medium (Lonza Group Ltd., Basel, Switzerland) supplemented with 100 U/ml penicillin and 100 µg/ml streptomycin at 37°C in a humidified incubator containing 5% CO2 for 48 h. In particular, the EPCs were initially plated in a 60 mm fibronectin (BD Biosciences, Franklin Lakes, NJ, USA) coated cell culture dish to promote cell adhesion and growth. Adherent cells were maintained and the non-adherent cells were removed with medium replacement every 48 h to form uniform cells. The adherent cells were then retrieved by trypsin digestion supplemented with 0.25% EDTA (HyClone; GE Healthcare, Logan, UT, USA) and were incubated at 37°C for 30 min with Sca-1 [-phycoerythrin (PE); cat. no. 108107; 0.2 mg/ml; 1:50], CD29 [-fluorescein isothiocyanate (FITC); cat. no. 102205; 0.2 mg/ml; 1:50], CD45 [-peridinin chlorophyll protein complex (PerCP); cat. no. 202220; 0.2 mg/ml; 1:50] and CD11b [-allophycocyanin (APC); cat. no. 201809; 0.2 mg/ml; 1:50] mouse monoclonal antibodies (BioLegend, Inc., San Diego, CA, USA). The cells underwent flow cytometry and were analyzed using FACSDIVA software version 6.1.3 (both from BD Biosciences). Sorted Sca-1+ CD29+ CD11b− CD45− cells (MSCs) were obtained for further culture in the LG-DMEM supplemented with 10% lot-selected FBS (both from Gibco; Thermo Fisher Scientific, Inc.), 2 mM glutamine, 100 U/ml penicillin and 100 µg/ml streptomycin (all from Sigma-Aldrich; Merck KGaA) at 37°C in a humidified incubator containing 5% CO2 for enrichment. According to the aforementioned technique, sorted CD133+ (-FITC; eBioscience, San Diego, CA, USA) CD31+ (-PE/Cy7; BioLegend) CD144+ (-PE, BD Biosciences) and CD11b− (-APC; BioLegend) cells (EPCs) were obtained for further culture in EBM-2 medium (Lonza Group Ltd) for enrichment. All of the EPC cells were plated in a 60 mm cell culture dish coated with fibronectin to promote cell adhesion and growth.
Coculture of MSCs and EPCs
MSCs and EPCs were cocultured in cell number ratios of 1:1 in 6-well plates or 60 mm cell culture dishes. Cells were cultured in LG-DMEM without FBS at 37°C in a humidified incubator containing 5% CO2 for 24 h. Inoculation density was in accordance with experimental requirements and cells were then prepared for subsequent experiments.
Determination of IL-1β expression by ELISA
All of the groups: MSCs, EPCs, MSCs + EPCs, EPC-CM-MSCs and MSC-CM-EPCs, were seeded at 2×105 cells/well in 6-well plates alongside 2 ml serum- and factor-free medium for 24 h. We used MSC-CM to stimulate EPC cells and collected the supernatant to detect the IL-1β expression by ELISA kit. For the same reason, we named the EPC-CM to stimulate the MSC cells group as EPC-CM-MSC. We aim to collect the IL-1β expression in each group for comparison and analysis. Subsequently, supernatants were collected and centrifuged (4°C; 5,000 × g; 10 min) in order to measure IL-1β expression using an IL-1β ELISA kit (cat. no. SEA563Mu; Uscn Life Sciences, Inc., Wuhan, China) according to the manufacturer's protocol.
Detection of ICAM-1 by cell immunofluorescence
Cells were plated onto coverslips (2×104 cells/sample), which were cultured in 6 mm dishes with 2 ml corresponding medium (LG-DMEM supplemented with 10% lot-selected FBS, both from Gibco; Thermo Fisher Scientific, Inc.) for 24 h. Subsequently, the medium was replaced with serum- and factor-free medium supplemented with IL-1β (25 µg/ml) or p38 MAPK inhibitor SB203580 (20 µmol/ml), and cells were incubated for a further 24 h. After culturing for 24 h, the coverslips were rinsed in PBS three times and fixed with 4% paraformaldehyde for 20 min. Subsequently, the cells were blocked in 5% bovine serum albumin (BSA) for 30 min at room temperature and incubated overnight with anti-mouse ICAM-1 monoclonal antibodies (ab171123, 1:100) or isotype control antibody (ab81032, 1:100) (both from Abcam, Cambridge, MA, USA) at 4°C. After rinsing in PBS three times, the cells were incubated with FITC-conjugated goat anti mouse immunoglobulin (Ig) G (cat. no. ZB2305; 1:100; OriGene Technologies, Inc., Beijing, China) in the dark for a further 1 h. After washing, the nuclei were stained with propidium iodide (PI, 10 µg/ml; cat. no. P4170; Sigma-Aldrich; Merck KGaA) solution and washed a further three times with PBS. Subsequently, 70% glycerol was used to mount the coverslips onto slides and expression was detected using a confocal laser scanning microscope (LSM 510 META; Zeiss GmbH, Jena, Germany). The experiments were performed and repeated >3 times.
Western blotting to detect ICAM-1 and p38 MAPK expression
Following pretreatment, the cells (2×106 cells/sample) were washed three times with ice-cold PBS and protein samples were extracted using radioimmunoprecipitation assay buffer (500 µl) with phenylmethylsulfonyl fluoride (5 µl) (both from Thermo Fisher Scientific, Inc.). Protein concentration was determined using a bicinchoninic acid protein assay kit (Thermo Fisher Scientific, Inc.). Subsequently, protein samples were treated with 5X loading buffer (100 µl; Thermo Fisher Scientific, Inc.) and heated for 8 min at 100°C. Protein samples (40 µg) were then separated by 10% SDS-PAGE and were transferred onto a polyvinylidene difluoride membrane. The membrane was blocked with 5% skim milk or 5% BSA, and incubated overnight with anti-ICAM-1 (ab171123, 1:500; Abcam), anti-p38 MAPK (cat. no. #8690; 1:1,000) and anti-p-p38 MAPK (cat. no. #4511; 1:1,000; both from Cell Signaling Technology, Inc., Danvers, MA, USA) at 4°C. After washing three times with Tris-buffered saline containing 0.1% Tween-20, the membrane was incubated with goat anti-mouse (1:10,000; cat. no. ZB2305) or goat anti-rabbit (1:10,000; cat. no. ZB2301) IgG horseradish peroxidase-conjugated antibodies (OriGene Technologies, Inc.) at room temperature for 2 h and was detected by enhanced chemiluminescence (34094; Thermo Fisher Scientific, Inc.) for 12 h at 4°C. GAPDH (1:1,000; 12 h, 4°C; cat. no. #51332; Cell Signaling Technology, Inc.) was used to normalize the relative protein expression levels. The results and integrated optical density (IOD) values were analyzed by Gel-Pro Analyzer 4.0 (Media Cybernetics, Inc., Rockville, MD, USA). Experiments were performed independently and were repeated three times.
Labeling of MSCs with DAPI and EPCs with MitoTracker red
MSCs were washed three times with PBS and incubated with DAPI (2 µl/ml; Sigma-Aldrich; Merck KGaA) for 30 min at 37°C. Subsequently, cells were washed three times with PBS and were detected using a fluorescence microscope. The same methods were adopted to label EPCs with MitoTracker red (200 nM/ml; Thermo Fisher Scientific, Inc.).
MSCs and EPCs adhesion assay
Matrigel (BD Biosciences) was incubated at 4°C overnight to melt into liquid. Subsequently, a 24-well plate was coated with Matrigel (200 µl/well) on ice and was incubated at 37°C for 30 min in a humidified incubator containing 5% CO2 to allow the Matrigel to solidify. MSCs-DAPI (5×104 cells/well) and EPCs-MitoTrack red (5×104 cells/well) were seeded into the pretreated 24-well plate with EPCs culture medium (1 ml; EBM-2 medium; cat. no. CC-3156; Lonza Group Ltd.) supplemented with anti-ICAM-1 neutralizing antibody (ab171123, 1:50; Abcam), IL-1β (030447, 25 µg/ml; PeproTech, Inc., Rocky Hill, NJ, USA) or SB203580 (cat. no. S8307, lot. no. 104M4605v; 20 µmol/ml; Sigma-Aldrich). After culturing for 6–8 h at 37°C in a humidified incubator containing 5% CO2, the plates were randomly imaged under a fluorescence microscope.
Statistics analysis
Data are expressed as the means ± standard deviation. SPSS 17.0 statistical software (SPSS, Inc., Chicago, IL, USA) was used to analyze results. Statistical significance of group data was assessed using one-way analysis of variance (ANOVA) followed by SNK post hoc multiple comparisons test. P<0.05 was considered to indicate a statistically significant difference.
Results
IL-1β expression in culture medium
To determine the expression levels of IL-1β in MSCs, EPCs, MSCs + EPCs, EPC-CM-MSCs and MSC-CM-EPCs (Fig. 1), the groups were seeded into 6-well plates (2×105 cells/well) and treated with serum- and factor-free medium for 24 h. The results indicated that both MSCs and EPCs can secrete IL-1β, and in the MSCs + EPCs (49.13±6.21 ng/ml) group, IL-1β expression was higher than in the MSCs group (8.96±2.70 ng/ml, P<0.05) and the EPCs group (22.14±1.83 ng/ml, P<0.05). In addition, in the EPC-CM-MSCs group (35.02±1.19 ng/ml) and the MSC-CM-EPCs group (33.85±1.37 ng/ml) IL-1β expression was higher compared with in the MSCs group (8.96±2.70 ng/ml, P<0.05) and the EPCs group (22.14±1.83 ng/ml, P<0.05), but not compared with in the MSCs + EPCs group (49.13±6.21 ng/ml, P>0.05).
Figure 1.

ELISA was used to detect the expression levels of IL-1β in MSCs, EPCs, MSCs + EPCs, EPC-CM-MSCs and MSC-CM-EPCs. IL-1β was expressed in all groups at different levels. *P<0.05. EPCs, endothelial progenitor cells; IL-1β, interleukin-1β; MSCs, mesenchymal stem cells.
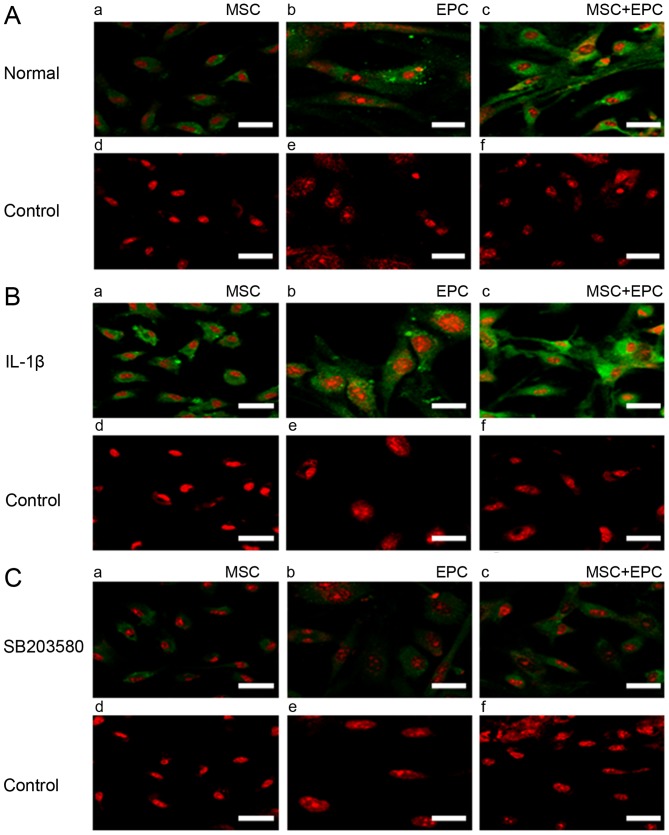
Immunofluorescence detection of ICAM-1 expression
Cells were seeded on coverslips (2×104 cells/sample) and were cultured in 6 mm dishes with 2 ml corresponding medium for 24 h. Subsequently, medium was replaced with serum- and factor-free medium supplemented with IL-1β (25 µg/ml) or p38 MAPK inhibitor SB203580 (20 µmol/ml) for 24 h. ICAM-1 expression was then detected by immunofluorescence (Fig. 2). The results indicated that MSCs and EPCs are able to express low levels of ICAM-1; however, in the MSCs + EPCs group the expression of ICAM-1 was increased. All of the IL-1β-treated groups (Fig. 2B) exhibited increased ICAM-1 expression compared with in the normal (Fig. 2A) and SB203580 groups (Fig. 2C). ICAM-1 expression was lowest in the SB203580 groups compared with in the untreated and IL-1β-treated groups.
Figure 2.
Immunofluorescence detection of ICAM-1 expression. (A) (a–c) Expression of ICAM-1 (FITC) in MSCs, EPCs and MSCs + EPCs normally cultured in vitro, as determined by cell immunofluorescence under a laser confocal microscope. (d–f) Mouse IgG control (FITC) staining. (B) (a–c) Expression of ICAM-1 (FITC) in MSCs, EPCs and MSCs + EPCs treated with IL-1β (25 µg/ml) in vitro. (d–f) Mouse IgG control (FITC) staining. (C) (a–c) Expression of ICAM-1 (FITC) in MSCs, EPCs and MSCs + EPCs treated with the p38 mitogen-activated protein kinase inhibitor SB203580 (20 µmol/ml) in vitro. (d–f) Mouse IgG control (FITC) staining. Scale bar, 5 µm. EPCs, endothelial progenitor cells; FITC, fluorescein isothiocyanate; ICAM-1, intercellular adhesion molecule-1; IgG, immunoglobulin G; IL-1β, interleukin-1β; MSCs, mesenchymal stem cells.
Western blotting to detect the expression levels of ICAM-1 and p38 MAPK
The protein expression levels of ICAM-1 and p38 MAPK were detected in MSCs, EPCs and MSCs + EPCs using western blotting (Fig. 3A). The relative ICAM-1/GAPDH IOD (Fig. 3B) and p-p38 MAPK/total-p38 MAPK IOD values (Fig. 3C) were then determined for statistical analysis. Normally cultured MSCs + EPCs (0.21±0.01, P<0.05) exhibited increased ICAM-1 expression compared with in the corresponding MSCs group (0.11±0.02, P<0.05) and EPCs group (0.11±0.02, P<0.05); however, there was no significant difference between the MSCs and EPCs groups. In the IL-1β-stimulated MSCs + EPCs group (0.38±0.02, P<0.05) the expression levels of ICAM-1 were increased compared with in the corresponding MSCs group (0.23±0.02, P<0.05) and EPCs group (0.25±0.02, P<0.05). The p38 MAPK inhibitor SB203580-treated MSCs + EPCs group (0.10±0.02, P<0.05) exhibited increased ICAM-1 expression compared with in the corresponding MSCs group (0.05±0.01, P<0.05) and EPCs group (0.05±0.01, P<0.05). ICAM-1 expression was increased in the IL-1β-stimulated groups (P<0.05), but was decreased in the SB203580-stimulated groups (P<0.05) compared with in the normal groups. Normally cultured MSCs + EPCs (0.52±0.02, P<0.05) exhibited increased p-p38 MAPK expression compared with in the corresponding MSCs group (0.35±0.02, P<0.05) and EPCs group (0.36±0.01, P<0.05); however there was no significant difference between the MSCs and EPCs groups. In the IL-1β-stimulated MSCs + EPCs group (0.74±0.06, P<0.05), the expression levels of p-p38 MAPK were increased compared with in the corresponding MSCs group (0.54±0.04, P<0.05) and EPCs group (0.47±0.03, P<0.05). The p38 MAPK inhibitor SB203580-stimulated MSCs + EPCs group (0.37±0.02, P<0.05) exhibited increased p-p38 MAPK expression compared with in the corresponding MSCs group (0.26±0.03, P<0.05) and EPCs group (0.17±0.01, P<0.05). The expression levels of p-p38 MAPK were increased following IL-1β treatment (P<0.05); however, they were decreased following treatment with the p38 MAPK inhibitor SB203580 (P<0.05), respectively. The expression levels of total p38 MAPK remained constant in all groups following various treatments.
Figure 3.
(A) Western blot analysis of ICAM-1, GAPDH, p-p38 MAPK and total p38 MAPK in MSCs, EPCs and MSCs + EPCs, with or without IL-1β (25 µg/ml) or p38 MAPK inhibitor SB203580 (20 µmol/ml) treatment. Lanes 1–3, normally cultured MSCs, EPCs and MSCs + EPCs groups, respectively; lanes 4–6, IL-1β (25 µg/ml)-stimulated MSCs, EPCs and MSCs + EPCs groups, respectively; lanes 7–9, p38 MAPK inhibitor SB203580 (20 µmol/ml)-stimulated MSCs, EPCs and MSCs + EPCs groups, respectively. (B) ICAM-1/GAPDH and (C) p-p38 MAPK/total-p38 MAPK IOD relative values were determined. Data are presented as the means ± standard deviation of three independent experiments. *P<0.05. EPCs, endothelial progenitor cells; ICAM-1, intercellular adhesion molecule-1; IL-1β, interleukin-1β; IOD, integrated optical density; MAPK, mitogen-activated protein kinase; MSCs, mesenchymal stem cells.
MSCs and EPCs adhesion assay
MSCs were labeled with DAPI and EPCs were labeled with MitoTracker red. MSCs-DAPI and EPCs-Mitotrack-red were cocultured in Matrigel-coated 24-well plates (5×104 cells/well, 1:1) with EPCs culture medium supplemented with anti-ICAM-1 neutralizing antibody (), IL-1β (25 µg/ml) or p38 MAPK inhibitor SB203580 (20 µmol/ml). Subsequently, the cells were cultured for 6–8 h at 37°C in a humidified incubator containing 5% CO2. The results indicated that treatment with anti-ICAM-1 neutralizing antibody or p38 MAPK inhibitor SB203580 resulted in a decrease in adhesion between MSCs and EPCs; however, supplementation with IL-1β markedly increased adhesion (Fig. 4).
Figure 4.
Adhesion of MSCs (DAPI, blue staining) and EPCs (Mitrotrack red, red staining) was detected in Matrigel-coated plates. (A) Adhesion of normally cultured MSCs and EPCs. Adhesion of MSCs and EPCs treated with (B) anti-ICAM-1 neutralizing antibody, (C) IL-1β (25 µg/ml) and (D) p38 mitogen-activated protein kinase inhibitor SB203580 (20 µmol/ml). (E–H) White-light image of (A–D), respectively. Scale bar, 100 µm. EPCs, endothelial progenitor cells; ICAM-1, intercellular adhesion molecule-1; IL-1β, interleukin-1β; MSCs, mesenchymal stem cells.
Discussion
The microenvironment surrounding stem cells, which is also known as the stem-cell niche, is composed of adjacent cells, extracellular matrix and adhesive molecules, and regulates stem cell self-renewal and differentiation. The stem-cell niche also aids regulation of cell fate, and is an interactive structural unit that functions via the cross-talk of key signaling and molecular factors (4–6). The functions of the stem-cell niche are reliant on adhesion molecules, which anchor stem cells in the niche and regulate communication with surrounding cells or various molecules.
As previously reported, EPCs likely interact with MSCs in the BM stem-cell niche (7); interactions between EPCs and MSCs may enhance neovascularization and bone regeneration (11–14). Therefore, focusing on the adhesion of MSCs and EPCs may provide information regarding clinical bone injury and vascular bone regeneration. However, the underlying mechanism that mediates the adhesion of MSCs and EPCs remains unclear. ICAM-1 is an important adhesion molecule and a member of the immunoglobulin supergene family, which participates in cell-cell and cell-matrix adhesive interactions, including those between tumor cells, endothelial cells, T cells, leukocytes and vascular cells (32–34). Furthermore, adhesion may be decreased by suppressing ICAM-1 expression. As an important adhesion molecule, previous studies have suggested that ICAM-1 may regulate IL-1β (19–21), tumor necrosis factor-α (35) and lipopolysaccharide (36). The present study focused on the stimulatory effects of IL-1β on ICAM-1, since IL-1β is an important inflammatory mediator, which not only affects nearly every cell type and interacts with numerous cytokines and small mediator molecules, but also participates in various physiological functions and diseases, including clinical bone injury (22–25) and vascular injury (26,27).
The present study demonstrated that both MSCs and EPCs could express low levels of ICAM-1; however, coculturing MSCs with EPCs increased ICAM-1 expression, particularly following treatment with IL-1β; however, treatment with the p38 MAPK inhibitor SB203580 inhibited ICAM-1 expression. These results indicated that IL-1β may activate the p38 MAPK pathway. Furthermore, cocultured MSCs and EPCs were seeded in Matrigel-coated plates; the results demonstrated that supplementation with anti-ICAM-1 neutralizing antibody or SB203580 effectively inhibited adhesion between MSCs and EPCs, whereas supplementation with IL-1β had the opposite effect. These results highlighted the importance of ICAM-1 for the adhesion between MSCs and EPCs, and this may be regulated by IL-1β through the p38 MAPK signaling pathway. However, at present, it remains unknown as to whether MSCs regulate EPCs function, or whether EPCs regulate MSCs function; potential joint action may serve an important role in the stem-cell niche. Previously, our laboratory indicated that EPCs promoted osteogenic differentiation of MSCs in a paracrine manner (37). Burlacu et al reported that MSCs may promote angiogenesis of EPCs in a paracrine manner (13). Furthermore, Ern et al demonstrated that EPCs and MSCs can secrete osteogenic or angiogenic factors to promote proliferation and differentiation in a paracrine manner (38). Therefore, the present study hypothesized that paracrine signaling is critical for the regulation of the effects of MSCs and EPCs coculture. The present study indicated that MSCs and EPCs could secrete IL-1β, whereas coculturing MSCs with EPCs enhanced the secretion of IL-1β. In addition, EPC-CM-MSCs and MSC-CM-EPCs groups exhibited higher levels of IL-1β compared with MSC-CM and EPC-CM; however they were not higher than in the MSCs + EPCs group. These results provided convincing evidence to explain the increased expression of ICAM-1 in cocultured MSCs and EPCs.
In conclusion, the present study demonstrated that IL-1β may induce ICAM-1 expression, thus enhancing the cohesion between MSCs and EPCs via the p38 MAPK signaling pathway. These findings provide effective evidence to support and explain previous findings regarding the adhesion of MSCs and EPCs. In addition, the present study provided a theoretical basis for further stem-cell niche transplantation to increase understanding regarding the function of MSCs and for subsequent experimental research. However, the factors that regulate secretion of IL-1β remain unclear; our future studies aim to focus on this, and to conduct further in vitro experiments regarding clinical application (clinical bone injury treatment, vascular bone regeneration, tissue repair and immune disorder therapy).
Acknowledgments
The present study was supported by grants from the National Natural Science Foundation of China (grant nos. 81760570 and 31271458), the Science and Technology program of Xinjiang Production and Construction Corps (grant no. 2014AB047), the Scientific Research Foundation for the Returned Overseas Chinese Scholars, Ministry of Human Resources and Social Security of the People's Republic of China (grant no. RSLX201201) and the Shihezi University Youth Science and Technology Research and Development program, basis and application research project (grant no. 20142RKXYQ20).
Footnotes
Competing interests
The authors declare there is no competing interest.
References
- 1.Friedenstein AJ, Chailakhjan RK, Lalykina KS. The development of fibroblast colonies in monolayer cultures of guinea-pig bone marrow and spleen cells. Cell Tissue Kinet. 1970;3:393–403. doi: 10.1111/j.1365-2184.1970.tb00347.x. [DOI] [PubMed] [Google Scholar]
- 2.Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, Moorman MA, Simonetti DW, Craig S, Marshak DR. Multilineage potential of adult human mesenchymal stem cells. Science. 1999;284:143–147. doi: 10.1126/science.284.5411.143. [DOI] [PubMed] [Google Scholar]
- 3.Jiang Y, Jahagirdar BN, Reinhardt RL, Schwartz RE, Keene CD, Ortiz-Gonzalez XR, Reyes M, Lenvik T, Lund T, Blackstad M, et al. Pluripotency of mesenchymal stem cells derived from adult marrow. Nature. 2002;418:41–49. doi: 10.1038/nature00870. [DOI] [PubMed] [Google Scholar]
- 4.Moore KA, Elmendorf SC. Propagule vs. niche limitation: Untangling the mechanisms behind plant species' distributions. Ecol Lett. 2006;9:797–804. doi: 10.1111/j.1461-0248.2006.00923.x. [DOI] [PubMed] [Google Scholar]
- 5.Spradling A, Drummond-Barbosa D, Kai T. Stem cells find their niche. Nature. 2001;414:98–104. doi: 10.1038/35102160. [DOI] [PubMed] [Google Scholar]
- 6.Moore KA, Lemischka IR. Stem cells and their niches. Science. 2006;311:1880–1885. doi: 10.1126/science.1110542. [DOI] [PubMed] [Google Scholar]
- 7.Zhang H, Xian L, Lin Z, Yang C, Zhang M, Feng W, Peng X, Chen X, Wu X. Endothelial progenitor cells as a possible component of stem cell niche to promote self-renewal of mesenchymal stem cells. Mol Cell Biochem. 2014;397:235–243. doi: 10.1007/s11010-014-2191-3. [DOI] [PubMed] [Google Scholar]
- 8.Asahara T, Murohara T, Sullivan A, Silver M, van der Zee R, Li T, Witzenbichler B, Schatteman G, Isner JM. Isolation of putative progenitor endothelial cells for angiogenesis. Science. 1997;275:964–967. doi: 10.1126/science.275.5302.964. [DOI] [PubMed] [Google Scholar]
- 9.Kalka C, Masuda H, Takahashi T, Kalka-Moll WM, Silver M, Kearney M, Li T, Isner JM, Asahara T. Transplantation of ex vivo expanded endothelial progenitor cells for therapeutic neovascularization. Proc Natl Acad Sci USA. 2000;97:3422–3427. doi: 10.1073/pnas.97.7.3422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Minamino T, Miyauchi H, Yoshida T, Ishida Y, Yoshida H, Komuro I. Endothelial cell senescence in human atherosclerosis: Role of telomere in endothelial dysfunction. Circulation. 2002;105:1541–1544. doi: 10.1161/01.CIR.0000013836.85741.17. [DOI] [PubMed] [Google Scholar]
- 11.Grellier M, Bordenave L, Amédée J. Cell-to-cell communication between osteogenic and endothelial lineages: Implications for tissue engineering. Trends Biotechnol. 2009;27:562–571. doi: 10.1016/j.tibtech.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 12.Fu WL, Xiang Z, Huang FG, Gu ZP, Yu XX, Cen SQ, Zhong G, Duan X, Liu M. Coculture of peripheral blood-derived mesenchymal stem cells and endothelial progenitor cells on strontium-doped calcium polyphosphate scaffolds to generate vascularized engineered bone. Tissue Eng Part A. 2015;21:948–959. doi: 10.1089/ten.tea.2014.0267. [DOI] [PubMed] [Google Scholar]
- 13.Burlacu A, Grigorescu G, Rosca AM, Preda MB, Simionescu M. Factors secreted by mesenchymal stem cells and endothelial progenitor cells have complementary effects on angiogenesis in vitro. Stem Cells Dev. 2013;22:643–653. doi: 10.1089/scd.2012.0273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zigdon-Giladi H, Bick T, Lewinson D, Machtei EE. Co-transplantation of endothelial progenitor cells and mesenchymal stem cells promote neovascularization and bone regeneration. Clin Implant Dent Relat Res. 2015;17:353–359. doi: 10.1111/cid.12104. [DOI] [PubMed] [Google Scholar]
- 15.Zuckerman LA, Pullen L, Miller J. Functional consequences of costimulation by ICAM-1 on IL-2 gene expression and T cell activation. J Immunol. 1998;160:3259–3268. [PubMed] [Google Scholar]
- 16.Agarwal SK, Brenner MB. Role of adhesion molecules in synovial inflammation. Curr Opin Rheumatol. 2006;18:268–276. doi: 10.1097/01.bor.0000218948.42730.39. [DOI] [PubMed] [Google Scholar]
- 17.Shaw SK, Ma S, Kim MB, Rao RM, Hartman CU, Froio RM, Yang L, Jones T, Liu Y, Nusrat A, et al. Coordinated redistribution of leukocyte LFA-1 and endothelial cell ICAM-1 accompany neutrophil transmigration. J Exp Med. 2004;200:1571–1580. doi: 10.1084/jem.20040965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sumagin R, Sarelius IH. Intercellular adhesion molecule-1 enrichment near tricellular endothelial junctions is preferentially associated with leukocyte transmigration and signals for reorganization of these junctions to accommodate leukocyte passage. J Immunol. 2010;184:5242–5252. doi: 10.4049/jimmunol.0903319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chang MC, Hung HP, Lin LD, Shyu YC, Wang TM, Lin HJ, Chan CP, Huang CC, Jeng JH. Effect of interleukin-1β on ICAM-1 expression of dental pulp cells: Role of PI3K/Akt, MEK/ERK, and cyclooxygenase. Clin Oral Investig. 2015;19:117–126. doi: 10.1007/s00784-014-1227-0. [DOI] [PubMed] [Google Scholar]
- 20.Shikama Y, Aki N, Hata A, Nishimura M, Oyadomari S, Funaki M. Palmitate-stimulated monocytes induce adhesion molecule expression in endothelial cells via IL-1 signaling pathway. J Cell Physiol. 2015;230:732–742. doi: 10.1002/jcp.24797. [DOI] [PubMed] [Google Scholar]
- 21.Yamagami H, Yamagami S, Inoki T, Amano S, Miyata K. The effects of proinflammatory cytokines on cytokine-chemokine gene expression profiles in the human corneal endothelium. Invest Ophthalmol Vis Sci. 2003;44:514–520. doi: 10.1167/iovs.02-0498. [DOI] [PubMed] [Google Scholar]
- 22.Horton JE, Raisz LG, Simmons HA, Oppenheim JJ, Mergenhagen SE. Bone resorbing activity in supernatant fluid from cultured human peripheral blood leukocytes. Science. 1972;177:793–795. doi: 10.1126/science.177.4051.793. [DOI] [PubMed] [Google Scholar]
- 23.Dewhirst FE, Stashenko PP, Mole JE, Tsurumachi T. Purification and partial sequence of human osteoclast-activating factor: Identity with interleukin 1 beta. J Immunol. 1985;135:2562–2568. [PubMed] [Google Scholar]
- 24.Stashenko P, Dewhirst FE, Peros WJ, Kent RL, Ago JM. Synergistic interactions between interleukin 1, tumor necrosis factor, and lymphotoxin in bone resorption. J Immunol. 1987;138:1464–1468. [PubMed] [Google Scholar]
- 25.Xiong Y, Donovan KA, Kline MP, Gornet MK, Moon-Tasson LL, Lacy MQ, Dispenzieri A, Gertz MA, Greipp PR, Lust JA. Identification of two groups of smoldering multiple myeloma patients who are either high or low producers of interleukin-1. J Interferon Cytokine Res. 2006;26:83–95. doi: 10.1089/jir.2006.26.83. [DOI] [PubMed] [Google Scholar]
- 26.Zhang R, Jiang F, Chen CS, Wang T, Feng J, Tao T, Qin X. Serum levels of IL-1β, IL-6, TGF-β, and MMP-9 in patients undergoing carotid artery stenting and regulation of MMP-9 in a new in vitro model of THP-1 cells activated by stenting. Mediators Inflamm. 2015;2015:956082. doi: 10.1155/2015/956082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alfaidi M, Wilson H, Daigneault M, Burnett A, Ridger V, Chamberlain J, Francis S. Neutrophil elastase promotes interleukin-1β secretion from human coronary endothelium. J Biol Chem. 2015;290:24067–24078. doi: 10.1074/jbc.M115.659029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wuyts WA, Vanaudenaerde BM, Dupont LJ, Demedts MG, Verleden GM. Involvement of p38 MAPK, JNK, p42/p44 ERK and NF-kappaB in IL-1β-induced chemokine release in human airway smooth muscle cells. Respir Med. 2003;97:811–817. doi: 10.1016/S0954-6111(03)00036-2. [DOI] [PubMed] [Google Scholar]
- 29.Hsu WY, Chao YW, Tsai YL, Lien CC, Chang CF, Deng MC, Ho LT, Kwok CF, Juan CC. Resistin induces monocyte-endothelial cell adhesion by increasing ICAM-1 and VCAM-1 expression in endothelial cells via p38 MAPK-dependent pathway. J Cell Physiol. 2011;226:2181–2188. doi: 10.1002/jcp.22555. [DOI] [PubMed] [Google Scholar]
- 30.Liang B, Wang X, Zhang N, Yang H, Bai R, Liu M, Bian Y, Xiao C, Yang Z. Angiotensin-(1-7) attenuates angiotensin II-induced ICAM-1, VCAM-1, and MCP-1 expression via the MAS Receptor through suppression of P38 and NF-κB pathways in HUVECs. Cell Physiol Biochem. 2015;35:2472–2482. doi: 10.1159/000374047. [DOI] [PubMed] [Google Scholar]
- 31.Lee SJ, Drabik K, Van Wagoner NJ, Lee S, Choi C, Dong Y, Benveniste EN. ICAM-1-induced expression of proinflammatory cytokines in astrocytes: Involvement of extracellular signal-regulated kinase and P38 mitogen-activated protein kinase pathways. J Immunol. 2000;165:4658–4666. doi: 10.4049/jimmunol.165.8.4658. [DOI] [PubMed] [Google Scholar]
- 32.Park JS, Kim KM, Kim MH, Chang HJ, Baek MK, Kim SM, Jung YD. Resveratrol inhibits tumor cell adhesion to endothelial cells by blocking ICAM-1 expression. Anticancer Res. 2009;29:355–362. [PubMed] [Google Scholar]
- 33.Deane JA, Abeynaike LD, Norman MU, Wee JL, Kitching AR, Kubes P, Hickey MJ. Endogenous regulatory T cells adhere in inflamed dermal vessels via ICAM-1: Association with regulation of effector leukocyte adhesion. J Immunol. 2012;188:2179–2188. doi: 10.4049/jimmunol.1102752. [DOI] [PubMed] [Google Scholar]
- 34.Lacal PM, Petrillo MG, Ruffini F, Muzi A, Bianchini R, Ronchetti S, Migliorati G, Riccardi C, Graziani G, Nocentini G. Glucocorticoid-induced tumor necrosis factor receptor family-related ligand triggering upregulates vascular cell adhesion molecule-1 and intercellular adhesion molecule-1 and promotes leukocyte adhesion. J Pharmacol Exp Ther. 2013;347:164–172. doi: 10.1124/jpet.113.207605. [DOI] [PubMed] [Google Scholar]
- 35.Kim KH, Lee EN, Park JK, Lee JR, Kim JH, Choi HJ, Kim BS, Lee HW, Lee KS, Yoon S. Curcumin attenuates TNF-α-induced expression of intercellular adhesion molecule-1, vascular cell adhesion molecule-1 and proinflammatory cytokines in human endometriotic stromal cells. Phytother Res. 2012;26:1037–1047. doi: 10.1002/ptr.3694. [DOI] [PubMed] [Google Scholar]
- 36.Park GS, Kim JH. LPS Up-regulates ICAM-1 expression in breast cancer cells by stimulating a MyD88-BLT2-ERK-linked cascade, which promotes adhesion to monocytes. Mol Cells. 2015;38:821–828. doi: 10.14348/molcells.2015.0174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang M, Zhang H, Feng W, Wang Y, Yin S, Chen X, Wu X. Endothelial progenitor cells promote osteogenic differentiation of marrow stromal cells in a paracrine manner. Zhonghua Yi Xue Za Zhi. 2015;95:1253–1257. In Chinese. [PubMed] [Google Scholar]
- 38.Ern C, Krump-Konvalinkova V, Docheva D, Schindler S, Rossmann O, Böcker W, Mutschler W, Schieker M. Interactions of human endothelial and multipotent mesenchymal stem cells in cocultures. Open Biomed Eng J. 2010;4:190–198. doi: 10.2174/1874120701004010190. [DOI] [PMC free article] [PubMed] [Google Scholar]