Abstract
Introduction
Prevalence of HIV among young women in South Africa remains extremely high. Adolescent peer groups have been found to be an important influence on a range of health behaviours. The characteristics of young women's friendships might influence their sexual health and HIV risk via connections to sexual partners, norms around sexual initiation and condom use, or provision of social support. We investigated associations between young women's friendships and their Herpes Simplex Virus Type 2 (HSV‐2) and HIV infection status in rural South Africa.
Methods
Our study is a cross‐sectional, egocentric network analysis. In 2011 to 2012, we tested 13‐ to 20‐year‐old young women for HIV and HSV‐2, and collected descriptions of five friendships for each. We generated summary measures describing friend socio‐demographic characteristics and the number of friends perceived to have had sex. We used logistic regression to analyse associations between friend characteristics and participant HIV and HSV‐2 infection, excluding likely perinatal HIV infections.
Results
There were 2326 participants included in the study sample, among whom HIV and HSV‐2 prevalence were 3.3% and 4.6% respectively. Adjusted for participant and friend socio‐demographic characteristics, each additional friend at least one year older than the participant was associated with raised odds of HIV (odds ratio (OR) = 1.37, 95% CI 1.03 to 1.82) and HSV‐2 (adjusted OR=1.41, 95% CI 1.18 to 1.69). Each additional friend perceived to have ever had sex also raised the odds of HIV (OR = 1.29, 95% CI 1.03 to 1.63) and HSV‐2 (OR=1.18, 95% CI 1.03 to 1.35).
Discussion
We found good evidence that a greater number of older friends and friends perceived to have had sex were associated with increased risk for HSV‐2 and HIV infection among young women.
Conclusions
The characteristics of young women's friendships could contribute to their risk of HIV infection. The extent to which policies or programmes influence age‐mixing and young women's normative environments should be considered.
Keywords: HIV, young women, adolescents, social networks, friendships, peer influence, social norms, HSV‐2, South Africa
1. Introduction
South Africa has a severe HIV epidemic with young women at high risk for infection 1, 2. While young women's sexual behaviours can influence their HIV risk 3, the limited impact of individual behavioural interventions on HIV incidence has pointed to the importance of structural factors that characterise and shape young women's social environments 4, 5, 6, 7, 8. Adolescents’ peers, who make up much of their day‐to‐day social environment, could be important links in causal chains from structural drivers of HIV risks to proximate HIV exposures.
Peer relationships grow in importance as children move into adolescence 9, 10, 11. They may serve as conduits for dominant norms about gender and sexuality, as well as for information and resources and as the social contacts through which young women form sexual partnerships. Research from other populations has found that characteristics of adolescents’ peers and friends can affect a range of behaviours, including sexual behaviour 12, 13, 14, 15. There are different mechanisms by which such influence could occur 16. Young women who believe that more of their friends are sexually active might become sexually active themselves. Previous research has found such perceived behaviour, often referred to as “descriptive norms,” can encourage people to align their behaviour accordingly, even when such perceptions are inaccurate 17, 18. The socio‐demographic characteristics of friends could affect the kinds of acquaintances and sexual partners a young woman is likely to meet, as well as the sexual behaviours she perceives to be normative. A previous study from the Western Cape in South Africa has found that estimated exposure to older classmates over time, common when young people repeat grades at school, was associated with sexual debut and having older sexual partners in young women 19. Friends serve as social connections, introducing young people to partners and helping to facilitate relationships 20. Because social relationships tend to exhibit a high level of homophily (similarity), male friends, friends out of school and older friends might be more likely to connect young women to older sexual partners than younger female friends 21.
This study explores the possible role of adolescent girls’ friends in their risk of acquiring HIV. While qualitative research from South Africa suggests that peers might be influential 6, 20, 22, 23, the quantitative evidence base is weak and there is no study that uses HIV as an outcome 24.The baseline survey 25 from HPTN 068: Effect of Cash Transfer for the Prevention of HIV among Young South African Women provided an opportunity to examine the evidence for these hypotheses about the associations between friendship characteristics and HIV and HSV‐2 status amongst 13‐ to 20‐year‐old young women in rural South Africa.
2. Methods
2.1. Population and setting
Participants were 13‐ to 20‐year‐old unmarried young women enrolled in grades 8 to 11 in school and recruited between March 2011 and December 2012 for HPTN 068. The trial investigated the effect of conditional cash transfers (CCT) on young women's school attendance and on HIV acquisition 26.
Participants resided in the Agincourt health and socio‐demographic surveillance system (HDSS) site 27 including 28 villages in a deprived and densely populated, but rural area in Mpumalanga province in north‐east South Africa. HIV prevalence among individuals over 15 in the site is 19.4% of women and 10.6% of men. Prevalence by age rises steeply from 5.5% of young women aged 15 to 19 to 27% among women aged 20 to 24 years 28.
2.2. Data collection
Fieldworkers visited households identified in the annual demographic census as likely to house eligible young women in order to confirm eligibility, explain the study and obtain informed consent (assent for under 18s) from one eligible young woman per household and a parent/guardian. The parent/guardian then completed a survey with information about the household and the young woman was given a time to attend a “weekend camp” at a nearby community venue or study office 26. Here, she completed her baseline survey, HIV/HSV‐2 testing and pre and post‐test counselling and randomisation to study arm.
The young woman's survey, conducted in either English or Shangaan, included sections on socio‐demographic characteristics, education, sexual behaviours, characteristics of up to three previous sexual partners and a module on friendships. Participants completed the survey alone using Audio Computer Assisted Self Interview (ACASI) for most modules to reduce social desirability bias 29. The friendship module was delivered by trained interviewers using Computer Assisted Personal Interview (CAPI) because the module structure was relatively complex and less sensitive in nature.
2.3. Measures
2.3.1. Friendship exposures
Young women were asked to think of five of their closest friends – their “friendship nets.” Personal identifiers were not collected. They described these friends and their relationship to them in terms of their socio‐demographic attributes, where and how often they saw them, how long they had known them, their perceptions of their sexual behaviour, and communication with them about sex and HIV. The questionnaire was translated and back‐translated and interpretation of “friend” in Shangaan was checked. We did not attempt to impose a definition of “friend” as we wanted to capture the diversity in friendship types that might exist.
For this analysis, we have used a “personal network exposure” approach to capture the influence of the network (also referred to as an ego‐net) 30, 31, 32, 33, rather than examining the effects of each friend separately because it is a better measure of the overall friendship environment a young woman is exposed to. Thus, friendship exposures for each participant were treated either as values between 0 and 5, or as binary variables (“has at least one friend”) for rarer friendship characteristics. Young women were excluded if they refused to give a response to one of the friendship characteristics for more than three friends.
The main friendship variables of interest to this study included: the number of friends perceived to have ever had sex; the number of friends who were more than one year older than the participant; whether the participant reported at least one friend not attending school; and whether the participant reported at least one male friend. Because approximately one‐quarter of friends were also reported to be blood relatives, we included number of friends who were also blood relatives in the analysis.
2.3.2. Outcomes
Two different, site‐validated, HIV rapid tests, the Determine™ HIV‐1/2 (Alere Medical Co., Ltd, Matsudo‐shi, Chiba, Japan) and FDA‐cleared Uni‐gold Recombigen HIV test (Trinity Biotech plc, Bray, Co. Wicklow, Ireland), were conducted in parallel. If one or both of the tests was reactive, a CD4 count and a western blot confirmatory test were conducted. Participants were considered to be HIV seropositive if western blot test was positive. HSV‐2 testing was completed using the Kalon assay (Herpes Simplex Virus Type 2 IgG ELISA; Kalon Biologics Ltd, Guildford, UK) with an index cutoff of 1.5.
2.4. Analysis
We examined differences between the sample population and those excluded for missing data. We summarised socio‐demographic characteristics of the participants alongside the characteristics of their friendship networks and their HIV and HSV‐2 status. To test whether outcomes varied by village or school, we fit two‐level logistic regression models containing only the outcome (null effects models) with random effects by school or village to examine whether the proportion of the variance explained by village or school was greater than would be expected by chance by inspecting the estimated intraclass correlation coefficients under a modified χ2 34.
The characteristics of participants, including those of their households, could plausibly affect both what kind of friends they have and their risk of HIV and HSV‐2 35. We adjusted for the participants’ age in years, school grade, whether participants’ parents were alive, relative household socio‐economic position (SEP), and parent's education. It was possible that friend characteristics could confound each other, such as confounding between friend age and perceived sexual activity. However, to avoid over‐adjusting, we first entered the socio‐demographic characteristics of friends (Model 1) and then added the number of friends perceived to have had sex to the model (Model 2). We assessed the evidence for associations using likelihood ratio tests to compare models.
To assess whether participant and friendship net characteristics might operate differently in younger (13 to 15 years old) versus older participants (16 to 20 years old), we used likelihood ratio tests to compare models with and without interaction terms.
It is plausible that some HIV‐positive young women in the study were perinatally infected. While there has been an absence of long‐term cohort studies to observe survival among adolescents born and infected prior to availability of antiretroviral treatment (ART), recent studies suggest that 20% to 30% could survive to at least age 10 36, 37, 38, 39, 40, 41. This could represent a substantial proportion of prevalent HIV cases, particularly among younger adolescents. On this basis, given the rapidly rising HIV incidence amongst antenatal attendees 42, 43 in South Africa during the period in which these young women were born (1991 to 1999), and given our findings presented in the Additional File, we chose in our primary analyses for HIV outcome to exclude young women who were HIV positive, yet reported never having had sex, n=36. (They were not excluded from HSV‐2 analyses). Evidence for this decision is presented in an Additional File, but associations with HIV discussed in this paper otherwise refer to young women excluding those judged to have been perinatally infected.
2.5. Ethics
The HPTN 068 study trial has ethical approval from the Ethics Committees of the University of North Carolina, the University of the Witwatersrand, Mpumalanga Province Health Research and Ethics Committee and the London School of Hygiene and Tropical Medicine (LSHTM). The analysis presented here has additional approval from the LSHTM.
3. Results
3.1. Participant characteristics and those of their friends
There were 2537 young women recruited to the HPTN 068 study, of whom 2326 were retained for this study, (Figure 1). Four young women were withdrawn from the study, four were excluded because HIV infection status could not be determined due to incomplete or inconclusive test results, and five were excluded because their HSV‐2 tests were inconclusive. There were 116 participants from one village who did not complete the friendship module as this was delayed in ethical review and not yet included in the survey. We did not find differences in their socio‐demographic characteristics, HIV or HSV‐2 prevalence from other participants (not shown here).
Figure 1.
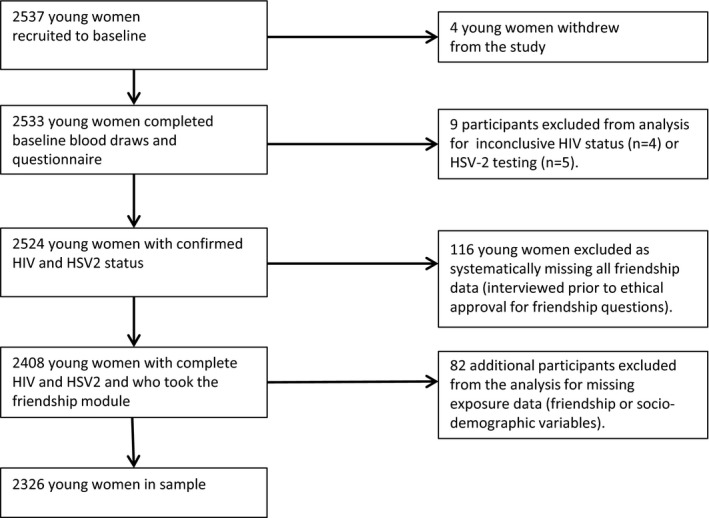
Flow diagram of study sample.
Of the 2326 young women included in the study, mean age was 15.5 years old (Table 1). For 32.0% of young women, either their father, mother or both parents had died or their vital status was unknown. Parents were reported to have a mix of educational attainments, with 16.4% of mothers and 17.0% of fathers reported to have had no schooling.
Table 1.
Characteristics of participants and their friendship nets, n=2326
| Participant characteristics | n | % |
|---|---|---|
| Participant age in years | 15.5 (mean) | 15 (median) |
| School grade | ||
| 8 | 598 | 25.7 |
| 9 | 628 | 27.0 |
| 10 | 631 | 27.1 |
| 11 | 469 | 20.2 |
| Orphanhood status | ||
| Both alive | 1581 | 68.0 |
| Father died/unknown | 465 | 20.0 |
| Mother died/unknown | 143 | 6.1 |
| Both died/unknown | 137 | 5.9 |
| Father's highest level of education | ||
| No school | 396 | 17.0 |
| Attended primary (complete and incomplete) | 421 | 18.1 |
| Attended secondary but did not complete | 431 | 18.5 |
| Completed secondary school plus | 649 | 27.9 |
| Don't know | 429 | 18.4 |
| Mother's highest level of education | ||
| No school | 381 | 16.4 |
| Attended primary (complete and incomplete) | 511 | 22.0 |
| Attended secondary but did not complete | 636 | 27.3 |
| Completed secondary school plus | 597 | 25.7 |
| Don't know | 201 | 8.6 |
| Number of friends perceived to have had sex | ||
| 0 | 913 | 39.3 |
| 1 | 330 | 14.2 |
| 2 | 254 | 10.9 |
| 3 | 261 | 11.2 |
| 4 | 260 | 11.2 |
| 5 | 308 | 13.2 |
| Number of friends >1 year older | ||
| 0 | 1085 | 46.6 |
| 1 | 621 | 26.7 |
| 2 | 337 | 14.5 |
| 3 | 192 | 8.3 |
| 4 | 64 | 2.8 |
| 5 | 27 | 1.2 |
| At least one male friend | ||
| Yes | 298 | 12.8 |
| At least one friend out of school | ||
| Yes | 451 | 19.4 |
| Number of friends who are relatives | ||
| 0 | 933 | 40.1 |
| 1 | 680 | 29.2 |
| 2 | 433 | 18.6 |
| 3 | 178 | 7.7 |
| 4 | 72 | 3.1 |
| 5 | 30 | 1.3 |
| HIV status | ||
| Positive | 76 | 3.3 |
| HSV‐2 status | ||
| Positive | 106 | 4.6 |
Of the 2326 young women in the sample, there were 76 who tested positive for HIV (3.3%, 95% CI 2.5 to 4.0), 36 of whom reported never having had sex and were therefore excluded from further analysis investigating HIV. The HSV‐2 prevalence was 4.6%, 95% CI 3.7 to 5.4 (106 participants). There was no evidence that prevalence of HIV and HSV‐2 varied significantly across schools or villages, ICCs<0.01.
Over half of participants reported that at least one of their five reported friends was more than one year older (53.4%). Only 12.8% of participants reported a male friend, and 80.6% reported that all their friends attended school. There were 59.9% who included at least one friend who was also a blood relative. For 39.3% of young women, no friends were perceived to have had sex, while 13.2% thought that all of their friends had sex.
3.2. Associations with HIV and HSV‐2, adjusted for participant age
HIV‐infected young women were on average older than HIV uninfected young women (mean age 17.4 vs. 15.5 years), and the odds of being HIV infected increased with every additional year of age (unadjusted OR 1.89; 95% CI 1.57 to 2.28) (Table 2). There was no association between HIV status and grade at school, whether parents were alive, household SEP, and mother's or father's education when adjusted for age.
Table 2.
Associations adjusted only for participant age with HIV (excluding those reporting never having had sex, n=2290) and HSV‐2 (n=2326)
| HIV, n=2290 | HSV‐2, n=2326 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HIV positive n, % | OR | 95% CI | p value | HSV‐2+ n, % | OR | 95% CI | p value | |||||
| Each additional year in age | 17.4 mean HIV positive | 15.5 mean HIV negative | 1.89 | 1.57 | 2.28 | <0.001 | 15.4 mean HSV‐2‐ | 17.0 mean HSV‐2+ | 1.73 | 1.54 | 1.95 | <0.001 |
| School grade | ||||||||||||
| 8 | 2/577 | 0.3 | 1.00 | 0.618 | 9/598 | 1.5 | 1.00 | 0.597 | ||||
| 9 | 8/622 | 1.3 | 2.11 | 0.44 | 10.18 | 15/628 | 2.4 | 1.02 | 0.43 | 2.37 | ||
| 10 | 9/626 | 1.8 | 1.32 | 0.27 | 6.45 | 39/631 | 6.2 | 1.48 | 0.67 | 3.28 | ||
| 11 | 18/465 | 4.1 | 1.84 | 0.38 | 9.07 | 43/469 | 9.2 | 1.43 | 0.62 | 3.33 | ||
| Orphanhood | ||||||||||||
| Parents alive | 22/1565 | 1.4 | 1.00 | 0.277 | 66/1581 | 4.2 | 1.00 | 0.564 | ||||
| Mother only alive | 9/457 | 2.0 | 1.25 | 0.56 | 2.76 | 22/465 | 4.7 | 1.03 | 0.62 | 1.71 | ||
| Father only alive | 3/140 | 2.1 | 1.43 | 0.41 | 4.97 | 10/143 | 7.0 | 1.71 | 0.83 | 3.50 | ||
| Neither parent alive | 6/128 | 4.7 | 2.78 | 1.08 | 7.20 | 8/137 | 5.8 | 1.19 | 0.55 | 2.59 | ||
| Household SEP | ||||||||||||
| First quintile | 10/452 | 2.2 | 1.00 | 0.631 | 33/461 | 7.2 | 1.00 | 0.010 | ||||
| Second | 7/454 | 1.5 | 0.74 | 0.27 | 2.00 | 12/460 | 2.6 | 0.36 | 0.18 | 0.71 | ||
| Third | 6/454 | 1.3 | 0.67 | 0.24 | 1.89 | 16/461 | 3.5 | 0.51 | 0.27 | 0.95 | ||
| Fourth | 11/461 | 2.4 | 1.36 | 0.56 | 3.30 | 20/468 | 4.3 | 0.68 | 0.38 | 1.23 | ||
| Fifth | 6/469 | 1.3 | 0.79 | 0.28 | 2.23 | 25/476 | 5.3 | 0.95 | 0.54 | 1.66 | ||
| Mother's education | ||||||||||||
| No school | 8/378 | 2.1 | 1.00 | 0.458 | 24/381 | 6.3 | 1.00 | 0.669 | ||||
| Attended primary but not completed | 13/502 | 2.6 | 1.38 | 0.56 | 3.42 | 25/511 | 4.9 | 0.86 | 0.47 | 1.55 | ||
| Completed primary, some high school | 10/629 | 1.6 | 0.95 | 0.37 | 2.46 | 30/636 | 4.7 | 0.91 | 0.52 | 1.61 | ||
| Completed high school | 4/582 | 0.7 | 0.52 | 0.15 | 1.78 | 21/597 | 3.5 | 0.84 | 0.45 | 1.56 | ||
| Do not know | 5/199 | 2.5 | 1.38 | 0.44 | 4.38 | 6/201 | 3.0 | 0.51 | 0.20 | 1.29 | ||
| Father's education | ||||||||||||
| No school | 8/390 | 2.1 | 1.00 | 0.728 | 26/396 | 6.1 | 1.00 | 0.055 | ||||
| Attended primary but not completed | 6/415 | 1.4 | 0.75 | 0.25 | 2.21 | 19/421 | 5.0 | 0.73 | 0.39 | 1.37 | ||
| Completed primary, some high school | 5/428 | 1.2 | 0.86 | 0.27 | 2.70 | 19/431 | 4.4 | 0.91 | 0.49 | 1.70 | ||
| Completed high school | 11/635 | 1.7 | 1.38 | 0.54 | 3.55 | 14/649 | 2.3 | 0.45 | 0.23 | 0.88 | ||
| Do not know | 10/422 | 2.4 | 1.29 | 0.50 | 3.37 | 28/429 | 6.8 | 1.12 | 0.63 | 1.98 | ||
| Each additional friend perceived to have had sex | 1.8 mean HIV negative | 3.6 mean HIV positive | 1.36 | 1.09 | 1.68 | 0.004 | 1.7 mean HSV‐2 ‐ | 3.2 mean HSV‐2 + | 1.25 | 1.10 | 1.41 | <0.001 |
| Each additional friend ≥1 year older | 1.0 mean HIV negative | 1.4 mean HIV positive | 1.44 | 1.14 | 1.83 | 0.005 | 1.0 mean HSV‐2 ‐ | 1.3 mean HSV‐2 + | 1.40 | 1.20 | 1.63 | <0.001 |
| No male friends | 31/2000 | 1.6 | 1.00 | 0.135 | 88/2028 | 4.3 | 1.00 | 0.336 | ||||
| ≥1 male friend | 9/290 | 3.1 | 1.86 | 0.86 | 4.01 | 18/298 | 6.0 | 1.31 | 0.77 | 2.24 | ||
| All friends in school | 23/1851 | 1.2 | 1.00 | 0.112 | 69/1875 | 3.7 | 1.00 | 0.155 | ||||
| ≥1 friend out of school | 17/439 | 3.9 | 1.74 | 0.89 | 3.41 | 37/451 | 8.3 | 1.38 | 0.89 | 2.15 | ||
| Each additional friend who is a relative | 2.2 mean HIV negative | 3.0 mean HIV positive | 1.09 | 0.97 | 1.23 | 0.157 | 2.2 mean HSV‐2 ‐ | 2.2 mean HSV‐2 + | 0.98 | 0.90 | 1.06 | 0.577 |
As with HIV, HSV‐2 seroprevalence increased with age (OR=1.73, 95% CI 1.54 to 1.95). In contrast to HIV, being HSV‐2 positive was less common among participants from the second and third SEP quintiles compared to the first (OR=0.36, 95% CI 0.18 to 0.71 and OR=0.51, 95% CI 0.27 to 0.95, respectively) and among young women whose fathers had completed high school compared to those whose fathers had no schooling (OR=0.45, 95% CI 0.23 to 0.88).
3.3. Friendship socio‐demographic characteristics and associations with HIV and HSV‐2
Young women who were HIV positive reported that a higher number of friends were at least one year older than themselves (mean 1.4 vs. 1.0 of the five friends). Each additional friend at least one year older was associated with increased odds of HIV infection, after adjusting for age, (adjusted OR=1.44, 95% CI 1.14 to 1.83), (Table 2). Controlling for other participant and friend socio‐demographic characteristics, weakened this association only slightly (OR=1.37 95% CI 1.03 to 1.82) (Table 3 Model 1).
Table 3.
Associations between friendship network characteristics and HIV (excluding those reporting never having had sex, n=2290) and HSV‐2 (n=2326)
| Model 1 | Model 2 | Model 1 | Model 2 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p value | OR | 95% CI | p value | OR | 95% CI | p value | OR | 95% CI | p value | |||||
| Each additional friend perceived to have had sex | 1.29 | 1.03 | 1.63 | 0.025 | 1.18 | 1.03 | 1.35 | 0.014 | ||||||||
| Each additional friend ≥1 year older | 1.37 | 1.03 | 1.82 | 0.036 | 1.26 | 0.94 | 1.69 | 0.123 | 1.41 | 1.18 | 1.69 | <0.001 | 1.34 | 1.11 | 1.61 | 0.002 |
| No male friends | 1.00 | 0.202 | 1.00 | 0.163 | 1.00 | 0.295 | 1.00 | 0.292 | ||||||||
| ≥1 male friend | 1.75 | 0.77 | 3.98 | 1.85 | 0.81 | 4.22 | 1.37 | 0.77 | 2.43 | 1.37 | 0.77 | 2.43 | ||||
| All friends in school | 1.00 | 0.755 | 1.00 | 0.851 | 1.00 | 0.734 | 1.00 | 0.808 | ||||||||
| ≥1 friend out of school | 1.13 | 0.52 | 2.49 | 1.08 | 0.49 | 2.36 | 1.09 | 0.67 | 1.78 | 1.06 | 0.65 | 1.74 | ||||
| Each additional friend who is a relative | 1.04 | 0.91 | 1.19 | 0.521 | 1.06 | 0.92 | 1.21 | 0.439 | 0.94 | 0.86 | 1.04 | 0.216 | 0.95 | 0.86 | 1.04 | 0.239 |
All models also adjusted for participant age in years, school grade, whether each parent was alive, household SEP, and mother's and father's education.
Similar results were found for HSV‐2, with the odds of infection increasing for each additional older friend, even after adjustment for age (OR 1.40, 95% CI 1.20 to 1.63) (Table 2) and participant and friend characteristics (OR 1.41 95% CI 1.18 to 1.69, Table 3, Model 1).
There was little evidence for raised odds of HIV among young women with at least one friend out of school (OR=1.74, 95% CI 0.89 to 3.41) and one friend who was male (OR=1.86, 95% CI 0.86 to 4.01) when adjusted for the participant's age (Table 2). Once adjusted for participant and friend socio‐demographic characteristics, the association reduced further (OR=1.13, 95% CI 0.52 to 2.49) in the case of a friend out of school and for an effect of having at least one male friend (OR = 1.75, 95% CI 0.77 to 3.98, Table 3 Model 1). These characteristics were not associated with HSV‐2 status. Having more friends who were relatives was also not found to be associated with either HIV or HSV‐2 (Tables 2 and 3).
3.4. Perceived ever sex among friends and associations with HIV and HSV‐2
There was good evidence that perceiving a greater number of friends to have ever had sex was associated with both HIV and HSV‐2 infection. Adjusted for participant age, each additional friend thought to have had sex was associated with raised odds of HIV, (OR=1.36 95% CI 1.09 to 1.68) and for HSV‐2 (OR=1.25 95% CI 1.10 to 1.41). The associations diminished but remained present even after further adjustment for participant and friend socio‐demographic characteristics, including the number of older friends a young woman had. After adjustment, each additional friend perceived to have had sex was associated with 1.29 times the odds of HIV (95% CI 1.03 to 1.63) and 1.18 times the odds of HSV‐2 (95% CI 1.03 to 1.35, Table 3 Model 2).
We found no evidence that associations between friendship characteristics and HIV and HSV‐2 status differed between younger (13 to 15 years) and older (16 to 20 years) participants.
4. Discussion
In this large sample from rural South Africa, the majority of young women's friends were also female and in school. Young women who had more friends who were at least one year older than themselves, and those who perceived that more of their friends had sex were more likely to be HSV‐2 positive and to be HIV positive. There was strong evidence for these associations, even when we adjusted for the participant's and friends’ socio‐demographic characteristics.
Our findings are consistent with those from Lam et al.'s study in the Western Cape, South Africa, which found that a higher estimated exposure to older school classmates was associated with earlier sexual debut 19. Grade repetition has historically been common in South African schools, particularly among those primarily serving Black South Africans and disadvantaged communities 44, under‐resourced schools, and in Limpopo and Mpumalanga provinces, where our study was set 45. Older friends could lead both to a normative environment encouraging earlier sex and could also serve as social connections to older sexual partners. Taken together, our study and that of Lam et al. suggest that high levels of age mixing in settings like schools in which young women form their friendships could have negative effects on the sexual health of young people. However, since 2012 to 2014 changes in the Department of Basic Education's grade progression policy has meant that pupils should only repeat a grade once per “phase” (every three years), so the exposure of young people to older pupils in the same grades and age‐mixing within friendships might now be decreasing 46.
While having a greater number of older friends increased the odds of HSV‐2 and HIV, there was evidence for an independent effect of perceiving more friends to have had sex on HSV‐2. For HIV, much of the association with age could be due to this norm as the strength and evidence for this association diminished when perceived friend sexual activity was added to the model (Table 3, Model 2). There have been other interventions to reduce young people's alcohol consumption via changing norms about the perceived prevalence of drinking behaviour amongst their peers 17, 47, 48. A similar approach could be taken within HIV prevention interventions in this population. Delaying sexual debut in adolescents is a valuable public health initiative with potential for impact beyond the individual.
4.1. Strengths and Limitations
Our study had a large sample size and was nested within a randomised control trial and demographic surveillance site with experienced staff and strong oversight of study procedures. Our study did not rely on self‐reported sexual behaviour as outcomes, which are subject to recall and social desirability biases 49, 50. We examined effects of friend characteristics on HIV status directly and found similar associations as with HSV‐2 status, which further strengthens our findings when excluding young women who might have been perinatally infected.
Unlike other studies of peer influence on adolescent sexual behaviour from sub‐Saharan Africa found in a recent systematic review 24, our study collected data about specific friends rather than asking about peers in general. This approach allowed us to better estimate the effects of different friend attributes within each young woman's friendship network, for example controlling for the effect of having older friends when examining the effect of having more friends who were perceived to have had sex. Distinguishing between the effects of different friend characteristics could help to focus on appropriate points for intervention, whether on perceptions of peer behaviours, the social environment in which friendships are formed, or a combination. As neither HIV nor HSV‐2 varied significantly at the school/village level, contextual confounding at this level is unlikely 51.
A limiting factor, however, is that our study was cross‐sectional, and we therefore could not attribute causal associations between participant and friend characteristics. It is possible that young women chose friends who were like themselves and this accounts for the associations seen between friendship net characteristics and HIV and HSV‐2 status 52, 53, 54, 55. It is also possible that young women might not have reported socio‐demographic characteristics of their friends accurately and that social desirability bias could have affected associations between perceived ever sex of friends and HSV‐2 and HIV status.
4.2. Further research
Further research into young women's friendships in South Africa, including their formation and dissolution, stability, levels of intimacy, factors associated with status and reputation and their influence vis‐à‐vis parents/caregivers would further benefit the interpretation of our findings.
Some qualitative evidence suggests that sexually active young women risk disapproval from the community and even from young men as not conforming to standards of “good behaviour” 20. On the other hand, research among young women has found that material goods such as toiletries, cosmetics and fashionable clothing that can serve as a motivation for transactional sex were seen as important to avoid social exclusion by one's peers 56, 57. Collecting data to inform the whole connected network of friendships would help to disentangle these seemingly contradictory pressures by exploring associations between HIV risk behaviours and status/popularity, as indicated by centrality within the whole friendship network. Furthermore, an egocentric design allows examination of friend influence only over a “path length” of one, whereas a whole network would allow analysis of clustering of behaviours amongst friends, the extent to which individual young women might “bridge” across diverse normative clusters, and how this structural network position might mediate the influence of norms. Previous research has found some evidence that individuals could be influential on the behaviours of others up to three social connections away, which is not possible to examine egocentrically 58. While there are ethical challenges to identifying friends in order to put together such a connected network 59, 60, link‐tracing network sampling methodologies that would not require participants to name alters in an interview could be promising 61. Distinguishing between peer influence and other possible explanations for the associations seen between friendship characteristics and HIV, as well as between perinatal and sexually transmitted HIV infections, would be facilitated by a longitudinal study design.
HIV prevention research among young women would benefit from assessing how interventions might influence friendship and social networks. Friendships could be investigated as possible mediators, or modifiers, of intervention effects 35. An understanding of peer influence could also be used to improve the targeting of peer‐driven and delivered HIV prevention programmes, as has been shown to be efficacious in anti‐smoking 62, 63, antisubstance use 64 and sexual health promotion 65. Behaviour change interventions might benefit from targeting whole peer groups rather than individuals in isolation of their peers. These peer or friendship groups could be discerned and targeted via a peer‐referral strategy 66, 67.
5. Conclusions
Policies and programmes that lead to age mixing within young women's social environments and friendships, including within schools, could increase risk of HSV‐2 and HIV. It may be beneficial for programmes to target norms of perceived sexual activity. We have suggested further research that could additionally strengthen and interrogate our findings. We do not suggest that young women should pick and choose friends on the basis of their characteristics. Rather, our research should be interpreted to suggest that HIV prevention interventions and policies relating to young women should consider their impact on the composition of young women's social environments in which these friendships are formed.
Competing interests
No author has competing interests to declare.
Author contributions
EF and JRH conceived the project. EF conducted analyses, led interpretation, and manuscript writing, and was supervised by JRH and RDW. AEP, CM and KK are PI's of the HPTN 068 study and contributed to the study conception, interpretation and drafting of the manuscript. AS project managed the HPTN 068 study and contributed to the manuscript. FXGO was a site leader for the HPTN 068 study and contributed to the manuscript. SDM contributed to the interpretation of findings and to the final drafting of the manuscript. OL and EPM led laboratory analyses and contributed to the manuscript. All authors have read and approved the final manuscript.
Funding
EF was funded with a Bloomsbury Colleges PhD studentship with fieldwork funding from the London International Development Centre. This work was supported by Award Numbers UM1 AI068619 (HPTN Leadership and Operations Center), UM1AI068617 (HPTN Statistical and Data Management Center) and UM1AI068613 (HPTN Laboratory Center) from the National Institute of Allergy and Infectious Diseases, the National Institute of Mental Health and the National Institute on Drug Abuse of the National Institutes of Health. This work was also supported by NIMH R01 (R01MH087118) and the Carolina Population Center and its NIH Center grant (P2C HD050924). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Additional files 1.
Additional File 1. Possible perinatal HIV infections
Additional analyses to investigate the possibility that some HIV infections were due to perinatal infection rather than sexual transmission, which supports their exclusion from the main analyses.
Background
It was possible that some young women aged 13 to 20 might have HIV not acquired through sexual transmission but through perinatal or breastfeeding transmission from their mothers (vertical transmission). Young women aged 13 to 20 in 2011/2012 would have been born between 1991 and 1999, years of rising incidence of HIV in South Africa and before availability of antiretrovirals for prevention of vertical transmission from mothers to their children in this population 42. As discussed in the main part of this paper, there is recent evidence that a larger proportion of children infected with HIV might have survived into adolescence than previously thought, even without access to ART earlier in their childhoods.
Our hypotheses concerning the role of friendships in HIV risk all posited that friend characteristics were associated with HIV via sexual behaviour or partnership characteristics. If some proportion of young women who were HIV positive did not acquire the infection sexually the estimates for the associations between friend characteristics and HIV could be biased, mostly likely downward.
We therefore sought to separate out those young women who had acquired HIV through sexual transmission and those who had been infected via MTCT (mother to child transmission).
Methods
We did not have means of knowing with certainty which young women might have been infected via MTCT. However, there were 36/76 young women who were HIV positive and who reported never having had sex. While it is possible that ever sex was under‐reported, the study did not have other data to determine non‐sexual HIV infection.
We first compared the socio‐demographic characteristics of young women who were HIV positive by whether or not they reported ever having had sex and used χ2 tests and t tests to examine whether there was statistical evidence for differences. Young women who were vertically infected were expected to be more likely to be double or single orphans (via mother's infection) and younger. If they had been HIV positive for most of their lives they were also expected to be more likely to have had interrupted schooling and therefore to have been in a lower school grade for their age.
We then compared the associations observed between participant and friend characteristics and HIV including all young women (n=2326), and excluding those who were HIV positive but reported never having had sex (n=2290). We also compared the findings of these models to those examining the association between friendship characteristics and participant ever sex and participant HSV‐2 status. Risk of being HSV‐2 positive was hypothesised to share similar causal pathways and to have similar patterns of associations with sexually acquired HIV, but not non‐sexually acquired HIV.
Results
Characteristics of HIV‐positive participants by reported ever sex
There were 36/76 (47.4%) of young women who were HIV positive but reported never having had sex, (Table 4). Comparing these young women with those who were HIV positive but who did report ever having had sex, those reporting never sex were less likely to be HSV‐2 positive (8.3% compared to 37.5%, p = 0.003). Those reporting never sex were also younger (mean age =15.0 rather than 17.4, p < 0.001) and in lower school grades (58.3% in Grade 8 compared to 5.0%, p < 0.001). There was little evidence for a difference between groups by father's education or household socio‐economic position, but young women who were HIV positive and reporting never sex tended to have higher educated mothers (8.3% had no school compared to 20.0% of those who reported ever sex). While there was a higher proportion of young women who were HIV positive and reported ever having had sex who had both parents alive (55.0% vs. 44.4% who reported never having had sex) and more of those reporting never sex were double orphans (25.0% vs. 15.0%), there was little evidence that the difference in orphanhood status was more than might be expected by chance (p = 0.706).
Table 4.
Characteristics of HIV‐positive participants by whether they report ever having had sex, n=76
| Participant characteristics | HIV‐positive reporting never sex, n=36 | HIV‐positive, reporting ever sex, n=40 | p value | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| HSV2 status | |||||
| Negative | 33 | 91.7 | 25 | 62.5 | 0.003 |
| Positive | 3 | 8.3 | 15 | 37.5 | |
| Age in years | 15.0 | (mean) | 17.4 | (mean) | <0.001 |
| School grade | |||||
| 8 | 21 | 58.3 | 2 | 5.0 | <0.001 |
| 9 | 6 | 16.7 | 8 | 20.0 | |
| 10 | 5 | 13.9 | 11 | 27.5 | |
| 11 | 4 | 11.1 | 19 | 47.5 | |
| Orphanhood | |||||
| Both parents alive | 16 | 44.4 | 22 | 55.0 | 0.706 |
| Mother only alive | 8 | 22.2 | 9 | 22.5 | |
| Father only alive | 3 | 8.3 | 3 | 7.5 | |
| Neither parent alive | 9 | 25.0 | 6 | 15.0 | |
| Household SEP | |||||
| First quintile (lowest) | 9 | 25.0 | 10 | 25.0 | 0.915 |
| Second | 6 | 16.7 | 7 | 17.5 | |
| Third | 7 | 19.4 | 6 | 15.0 | |
| Fourth | 7 | 19.4 | 11 | 27.5 | |
| Fifth | 7 | 19.4 | 6 | 15.0 | |
| Mother's education | |||||
| No school | 3 | 8.3 | 8 | 20.0 | 0.027 |
| Attended primary but not completed | 9 | 25.0 | 13 | 32.5 | |
| Completed primary, some high school | 7 | 19.4 | 10 | 25.0 | |
| Completed high school | 15 | 41.7 | 4 | 10.0 | |
| Do not know | 2 | 5.6 | 5 | 12.5 | |
| Father's education | |||||
| No school | 6 | 16.7 | 8 | 20.0 | 0.832 |
| Attended primary but not completed | 6 | 16.7 | 6 | 15.0 | |
| Completed primary, some high school | 3 | 8.3 | 5 | 21.5 | |
| Completed high school | 14 | 38.9 | 11 | 27.5 | |
| Do not know | 7 | 19.4 | 10 | 25.0 | |
Associations between HIV and friendship characteristics amongst all HIV‐positive young women
When including all young women in the analyses (n=2326), the strength of associations between HIV and young women's socio‐demographic characteristics and those of their friends with HIV reduced compared to when positive young women reporting never sex were excluded (OR=1.31, 95% CI 1.15 to 1.49 compared to OR=1.89, 95% CI 1.57 to 2.28 excluding HIV‐positive young women reporting never sex, Table 5). There was a much strengthened association with school grade, whereby being HIV positive were less likely to be in grades 9, 10 and 11, even adjusted for age and other characteristics. Orphanhood status was also associated with HIV, such that young women for whom both parents had died had 4.67 times the odds (95% CI 2.48 to 8.78) of being HIV positive compared to young women for whom both parents were alive. When excluding the young women who reported never having had sex but who were HIV positive, the strength of this association reduced (OR=2.78, 95% CI 1.08 to 7.20)
Table 5.
Associations between participant and friendship characteristics when excluding HIV‐positive young women and reporting never sex (n=2290) and when including all young women (n=2326), adjusted for participant age
| Excluding those HIV positive reporting never sex, n=2290 | Including all young women, n=2326 | |||||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p value | OR | 95% CI | p value | |||
| Each additional year in age | 1.89 | 1.57 | 2.28 | <0.001 | 1.31 | 1.15 | 1.49 | <0.001 |
| School grade | ||||||||
| 8 | 1.00 | 0.618 | 1.00 | 0.005 | ||||
| 9 | 2.11 | 0.44 | 10.18 | 0.39 | 0.19 | 0.78 | ||
| 10 | 1.32 | 0.27 | 6.45 | 0.27 | 0.13 | 0.57 | ||
| 11 | 1.84 | 0.38 | 9.07 | 0.36 | 0.17 | 0.80 | ||
| Orphanhood | ||||||||
| Parents alive | 1.00 | 0.277 | 1.00 | <0.001 | ||||
| Mother only alive | 1.25 | 0.56 | 2.76 | 1.47 | 0.82 | 2.64 | ||
| Father only alive | 1.43 | 0.41 | 4.97 | 1.76 | 0.73 | 4.26 | ||
| Neither parent alive | 2.78 | 1.08 | 7.20 | 4.67 | 2.48 | 8.78 | ||
| Household SEP | ||||||||
| First quintile | 1.00 | 0.631 | 1.00 | 0.739 | ||||
| Second | 0.74 | 0.27 | 2.00 | 0.71 | 0.34 | 1.45 | ||
| Third | 0.67 | 0.24 | 1.89 | 0.72 | 0.35 | 1.47 | ||
| Fourth | 1.36 | 0.56 | 3.30 | 1.01 | 0.52 | 1.96 | ||
| Fifth | 0.79 | 0.28 | 2.23 | 0.75 | 0.36 | 1.54 | ||
| Mother's education | ||||||||
| No school | 1.00 | 0.458 | 1.00 | 0.609 | ||||
| Attended primary but not completed | 1.38 | 0.56 | 3.42 | 1.64 | 0.78 | 3.43 | ||
| Completed primary, some high school | 0.95 | 0.37 | 2.46 | 1.05 | 0.48 | 2.27 | ||
| Completed high school | 0.52 | 0.15 | 1.78 | 1.39 | 0.65 | 2.99 | ||
| Do not know | 1.38 | 0.44 | 4.38 | 1.32 | 0.50 | 3.47 | ||
| Father's education | ||||||||
| No school | 1.00 | 0.728 | 1.00 | 0.292 | ||||
| Attended primary but not completed | 0.75 | 0.25 | 2.21 | 0.86 | 0.39 | 1.89 | ||
| Completed primary, some high school | 0.86 | 0.27 | 2.70 | 0.61 | 0.25 | 1.47 | ||
| Completed high school | 1.38 | 0.54 | 3.55 | 1.34 | 0.68 | 2.64 | ||
| Do not know | 1.29 | 0.50 | 3.37 | 1.21 | 0.59 | 2.50 | ||
| Each additional friend perceived to have had sex | 1.36 | 1.09 | 1.68 | 0.004 | 1.03 | 0.96 | 1.11 | 0.406 |
| Each additional friend ≥1 year older | 1.44 | 1.14 | 1.83 | 0.005 | 1.11 | 0.92 | 1.34 | 0.293 |
| No male friends | 0.135 | 1.00 | 0.028 | |||||
| ≥1 male friend | 1.86 | 0.86 | 4.01 | 1.93 | 1.11 | 3.37 | ||
| All friends in school | 1.00 | 0.112 | 1.00 | 0.003 | ||||
| ≥1 friend out of school | 1.74 | 0.89 | 3.41 | 2.15 | 1.31 | 3.54 | ||
| Each additional friend who is a relative | 1.09 | 0.97 | 1.23 | 0.157 | 1.06 | 0.97 | 1.16 | 0.194 |
Including all young women, there was still strong evidence for an association between friendship characteristics and HIV, but these associations differed from when HIV‐positive young women reporting never sex were excluded. Evidence for association between HIV and each friend at least one year older diminished to OR=1.11, 95% CI 0.92 to 1.34) and weakened considerably for each friend perceived to have had sex reduced to OR=1.03 (95% CI 0.96 to 1.11) from 1.36 (95% CI 1.09 to 1.68). Instead, there was strengthened evidence that young women with at least one friend out of school (OR=2.15, 95% CI 1.31 to 3.54) and at least one male friend (OR=1.93, 95% CI 1.11 to 3.37) were more likely to be HIV positive.
Discussion
Compared to HIV‐positive participants reporting ever having had sex, those reporting never sex were less likely to be HSV‐2 positive, younger and in a lower grade at school, though not more likely to be orphans.
When including all HIV‐positive women, associations between participant characteristics and HIV status changed such that associations with age weakened and associations with being in a lower grade for age and with having neither parent alive emerged and strengthened respectively. Associations were more to similar to those seen with HSV‐2 (Tables 2 and 3), a sexually transmitted infection, when excluding HIV‐positive young women who reported never having had sex.
Young women who were perinatally infected would have been HIV positive for longer and would be more likely to have been ill enough to have missed or interrupted their schooling and so might be more likely to be in a lower grade for their age, although this has also been found to be a result of orphanhood 68. It is more likely that they would be younger and that their own parents would have died than young women who acquire HIV as a sexually transmitted infection. That these factors were not associated with HSV‐2 infection lends further support to interpreting these young women as perinatally infected.
It is likely that long‐term HIV infection would affect a young woman's friendships. Cross‐sectional associations could reflect this, leading to different results when including the possibly perinatally infected young women. It is plausible that young women who had been HIV infected for a long time might be excluded from the predominantly female, in‐school friendship network and thus more likely to have male and out‐of‐school friends instead. However, it is possible that the improved evidence for these associations related partly to differences in power between models including and excluding HIV‐positive girls reporting never having had sex. It would not be appropriate to draw conclusions about this pathway from the data we have, but this is an area for further exploration, given the importance of social support for HIV‐positive adolescents 69, 70, 71.
Conclusions
While recognising that there is likely to be bias in the reporting of ever sex, and that we are unable to distinguish perinatal from sexually transmitted HIV infections with certainty, our findings are consistent with the idea that many of the young women who were HIV positive yet reported never having had sex were indeed not sexually infected. When investigating the role of friendships on the causal pathways related to sexual transmission we therefore decided that it was most appropriate to exclude these young women from primary HIV analyses.
Fearon, E. , Wiggins, R. D. , Pettifor, A. E. , MacPhail, C. , Kahn, K. , Selin, A. , Gómez‐Olivé, F. X. , Delany‐Moretlwe, S. , Piwowar‐Manning, E. and Laeyendecker, O. Associations between friendship characteristics and HIV and HSV‐2 status amongst young South African women in HPTN‐068. J Int AIDS Soc. 2017; 20(4):e25029
References
- 1. Dellar RC, Dlamini S, Karim QA. Adolescent girls and young women: key populations for HIV epidemic control. J Int AIDS Soc. 2015;18(2 Suppl 1):19408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Shisana O, Rehle T, Simbayi LC, Zuma K, Jooste S, Zungu N, et al. South African National HIV Prevalence, Incidence and Behaviour Survey, 2012. Cape Town: HSRC Press; 2014. [DOI] [PubMed] [Google Scholar]
- 3. Pettifor AE, Rees HV, Kleinschmidt I, Steffenson AE, MacPhail C, Hlongwa‐Madikizela L, et al. Young people's sexual health in South Africa: HIV prevalence and sexual behaviors from a nationally representative household survey. AIDS. 2005;19(14):1525–34. [DOI] [PubMed] [Google Scholar]
- 4. Gupta GR, Parkhurst JO, Ogden JA, Aggleton P, Mahal A. Structural approaches to HIV prevention. Lancet. 2008;372(9640):764–75. [DOI] [PubMed] [Google Scholar]
- 5. Pettifor AE, Levandowski BA, MacPhail C, Padian NS, Cohen MS, Rees HV. Keep them in school: the importance of education as a protective factor against HIV infection among young South African women. Int J Epidemiol. 2008;37(6):1266–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Harrison A, Smit J, Hoffman S, Nzama T, Leu C‐S, Mantell J, et al. Gender, peer and partner influences on adolescent HIV risk in rural South Africa. Sex Health. 2012;9(2):178–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pettifor A, Bekker LG, Hosek S, DiClemente R, Rosenberg M, Bull SS, et al. Preventing HIV among young people: research priorities for the future. J Acquir Immune Defic Syndr. 2013;63(Suppl 2):S155–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hargreaves JR, Morison LA, Kim JC, Busza J, Phetla G, Porter JD, et al. Characteristics of sexual partnerships, not just of individuals, are associated with condom use and recent HIV infection in rural South Africa. AIDS Care. 2009;21(8):1058–70. [DOI] [PubMed] [Google Scholar]
- 9. Berndt TJ. Developmental changes in conformity to peers and parents. Dev Psychol. 1979;15(6):608–16. [Google Scholar]
- 10. Brown BB. Adolescents’ relationships with peers In: Lerner RM, Steinberg L, editors. Handbook of adolescent psychology. 2nd ed Hoboken (NJ): John Wiley & Sons, Inc.; 2004. p. 363–94. [Google Scholar]
- 11. Steinberg L, Monahan KC. Age differences in resistance to peer influence. Dev Psychol. 2007;43(6):1531–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ali MM, Dwyer DS. Estimating peer effects in sexual behavior among adolescents. J Adolesc. 2011;34(1):183–90. [DOI] [PubMed] [Google Scholar]
- 13. Prinstein MJ, Meade CS, Cohen GL. Adolescent oral sex, peer popularity, and perceptions of best friends’ sexual behavior. J Pediatr Psychol. 2003;28(4):243–9. [DOI] [PubMed] [Google Scholar]
- 14. Sieving RE, Eisenberg ME, Pettingell S, Skay C. Friends’ influence on adolescents’ first sexual intercourse. Perspect Sex Reprod Health. 2006;38(1):13–9. [DOI] [PubMed] [Google Scholar]
- 15. Billy JO, Udry JR. The influence of male and female best friends on adolescent sexual behavior. Adolescence. 1985;20(77):21–32. [PubMed] [Google Scholar]
- 16. Brown BB, Bakken JP, Ameringer SW, Mahon SD. A comprehensive conceptualization of the peer influence process in adolescence. In: Prinstein MJ, Dodge KA, editors. Understanding peer influence in children and adolescents. New York (NY): The Guilford Press; 2008. p. 17–44. [Google Scholar]
- 17. Perkins HW, Haines MP, Rice R. Misperceiving the college drinking norm and related problems: a nationwide study of exposure to prevention information, perceived norms and student alcohol misuse. J Stud Alcohol. 2005;66(4):470–8. [DOI] [PubMed] [Google Scholar]
- 18. Perkins JM, Perkins HW, Craig DW. Misperceptions of peer norms as a risk factor for sugar‐sweetened beverage consumption among secondary school students. J Am Diet Assoc. 2010;110(12):1916–21. [DOI] [PubMed] [Google Scholar]
- 19. Lam D, Marteleto LJ, Ranchhod V. The influence of older classmates on adolescent sexual behavior in Cape Town, South Africa. Stud Fam Plann. 2013;44(2):147–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Harrison A. Hidden love: sexual ideologies and relationship ideals among rural South African adolescents in the context of HIV/AIDS. Cult Health Sex. 2008;10(2):175–89. [DOI] [PubMed] [Google Scholar]
- 21. Goodreau SM, Kitts JA, Morris M. Birds of a feather, or friend of a friend? Using exponential random graph models to investigate adolescent social networks. Demography. 2009;46(1):103–25. Epub 2009/04/08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. MacPhail C, Campbell C. ‘I think condoms are good but, aai, I hate those things’: condom use among adolescents and young people in a Southern African township. Soc Sci Med. 2001;52(11):1613–27. [DOI] [PubMed] [Google Scholar]
- 23. Selikow T‐A, Ahmed N, Flisher AJ, Mathews C, Mukoma W. I am not “umqwayito”: a qualitative study of peer pressure and sexual risk behaviour among young adolescents in Cape Town, South Africa. Scand J Public Health. 2009;37:107–12. [DOI] [PubMed] [Google Scholar]
- 24. Fearon E, Wiggins RD, Pettifor AE, Hargreaves JR. Is the sexual behaviour of young people in sub‐Saharan Africa influenced by their peers? A systematic review Soc Sci Med. 2015;146:62–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. HPTN 068: Effects of Cash Transfer for the Prevention of HIV in Young South African Women. HIV Prevention Trials Network; 2011. [cited 12 June 2015]; Available from: http://www.hptn.org/research_studies/hptn068.asp
- 26. Pettifor A, MacPhail C, Selin A, Gomez‐Olive FX, Hughes J, Wagner R, et al. HPTN 068 conditional cash transfer to prevent HIV infection among young women in South Africa: results of a randomized controlled trial. IAS 2015; July 21, 2015; Vancouver, Canada; 2015.
- 27. Kahn K, Collinson MA, Gomez‐Olive FX, Mokoena O, Twine R, Mee P, et al. Profile: Agincourt health and socio‐demographic surveillance system. Int J Epidemiol. 2012;41(4):988–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Gomez‐Olive FX, Angotti N, Houle B, Klipstein‐Grobusch K, Kabudula C, Menken J, et al. Prevalence of HIV among those 15 and older in rural South Africa. AIDS Care. 2013;25:1122–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Langhaug LF, Cheung YB, Pascoe SJ, Chirawu P, Woelk G, Hayes RJ, et al. How you ask really matters: randomised comparison of four sexual behaviour questionnaire delivery modes in Zimbabwean youth. Sex Transm Infect. 2011;87(2):165–73. [DOI] [PubMed] [Google Scholar]
- 30. Valente T. Social networks and health: models, methods and applications. Oxford: Oxford University Press; 2010. [Google Scholar]
- 31. Gyarmathy VA, Neaigus A. The effect of personal network exposure on injecting equipment sharing among IDUs in Budapest, Hungary. Connections. 2006;27(1):25–38. [PMC free article] [PubMed] [Google Scholar]
- 32. Valente TW. Network models of the diffusion of innovations Cresskill (NJ): Hampton Press; 1995. [Google Scholar]
- 33. Valente TW, Fujimoto K, Soto D, Ritt‐Olson A, Unger JB. A comparison of peer influence measures as predictors of smoking among predominately hispanic/latino high school adolescents. J Adolesc Health. 2013;52(3):358–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Rao JNK, Scott AJ. On chi‐squared tests for multiway contingency tables with cell proportions estimated from survey data. Ann Stat. 1984;12(1):46–60. [Google Scholar]
- 35. Brook DW, Morojele NK, Zhang C, Brook JS. South African adolescents: pathways to risky sexual behavior. AIDS Educ Prev. 2006;18(3):259–72. [DOI] [PubMed] [Google Scholar]
- 36. Lowenthal ED, Bakeera‐Kitaka S, Marukutira T, Chapman J, Goldrath K, Ferrand RA. Perinatally acquired HIV infection in adolescents from sub‐Saharan Africa: a review of emerging challenges. Lancet Infect Dis. 2014;14(7):627–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ferrand RA, Munaiwa L, Matsekete J, Bandason T, Nathoo K, Ndhlovu CE, et al. Undiagnosed HIV infection among adolescents seeking primary health care in Zimbabwe. Clin Infect Dis. 2010;51(7):844–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Marston M, Becquet R, Zaba B, Moulton LH, Gray G, Coovadia H, et al. Net survival of perinatally and postnatally HIV‐infected children: a pooled analysis of individual data from sub‐Saharan Africa. Int J Epidemiol. 2011;40(2):385–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Walker AS, Mulenga V, Sinyinza F, Lishimpi K, Nunn A, Chintu C, et al. Determinants of survival without antiretroviral therapy after infancy in HIV‐1‐infected Zambian children in the CHAP Trial. J Acquir Immune Defic Syndr. 2006;42(5):637–45. [DOI] [PubMed] [Google Scholar]
- 40. Ferrand RA, Corbett EL, Wood R, Hargrove J, Ndhlovu CE, Cowan FM, et al. AIDS among older children and adolescents in Southern Africa: projecting the time course and magnitude of the epidemic. AIDS. 2009;23(15):2039–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Eaton JW, Garnett GP, Takavarasha FR, Mason PR, Robertson L, Schumacher CM, et al. Increasing adolescent HIV prevalence in Eastern Zimbabwe–evidence of long‐term survivors of mother‐to‐child transmission? PLoS ONE. 2013;8(8):e70447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Abdool‐Karim Q, Abdool‐Karim SS. The evolving HIV epidemic in South Africa. Int J Epidemiol. 2002;31(1):37–40. [DOI] [PubMed] [Google Scholar]
- 43. Eleventh National HIV Survey of Women Attending Antenatal Clinics of the Public Health Services. Pretoria, South Africa: Department of Health; 2001. [Google Scholar]
- 44. Lam D, Ardington C, Leibbrandt M. Schooling as a lottery: racial differences in school advancement in urban South Africa. J Dev Econ. 2011;95(2):121–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Access to Education: technical report of the National Household Survey. Johannesburg, South Africa: Centre for Applied Legal Studies Social Surveys Africa; 2009. [Google Scholar]
- 46. Education NDoB . National Policy Pertaining to the Programme and Promotion Requirements of the National Curriculum Statement Grades R‐12. Pretoria, Republic of South Africa; 2013. [Google Scholar]
- 47. Schroeder CM, Prentice DA. Exposing pluralistic ignorance to reduce alcohol use among college students. J Appl Soc Psychol. 1998;28(23):2150–80. [Google Scholar]
- 48. Reid AE, Carey KB. Interventions to reduce college student drinking: state of the evidence for mechanisms of behavior change. Clin Psychol Rev. 2015;40:213–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Buve A, Lagarde E, Carael M, Rutenberg N, Ferry B, Glynn JR, et al. Interpreting sexual behaviour data: validity issues in the multicentre study on factors determining the differential spread of HIV in four African cities. AIDS. 2001;15(Suppl 4):S117–26. [DOI] [PubMed] [Google Scholar]
- 50. Cowan FM, Langhaug LF, Mashungupa GP, Nyamurera T, Hargrove J, Jaffar S, et al. School based HIV prevention in Zimbabwe: feasibility and acceptability of evaluation trials using biological outcomes. AIDS. 2002;16(12):1673–8. [DOI] [PubMed] [Google Scholar]
- 51. Cohen‐Cole E, Fletcher JM. Is obesity contagious? Social networks vs. environmental factors in the obesity epidemic. J Health Econ. 2008;27(5):1382–7. [DOI] [PubMed] [Google Scholar]
- 52. Go MH, Green HD Jr, Kennedy DP, Pollard M, Tucker JS. Peer influence and selection effects on adolescent smoking. Drug Alcohol Depend. 2010;109(1–3):239–42. [DOI] [PubMed] [Google Scholar]
- 53. Ennett ST, Bauman KE. The contribution of influence and selection to adolescent peer group homogeneity: the case of adolescent cigarette smoking. J Pers Soc Psychol. 1994;67(4):653–63. [DOI] [PubMed] [Google Scholar]
- 54. Mercken L, Steglich C, Sinclair P, Holliday J, Moore L. A longitudinal social network analysis of peer influence, peer selection, and smoking behavior among adolescents in British schools. Health Psychol. 2012;31(4):450–9. [DOI] [PubMed] [Google Scholar]
- 55. Mercken L, Snijders TA, Steglich C, Vertiainen E, de Vries H. Smoking‐based selection and influence in gender‐segregated friendship networks: a social network analysis of adolescent smoking. Addiction. 2010;105(7):1280–9. [DOI] [PubMed] [Google Scholar]
- 56. Luke N. Age and economic asymmetries in the sexual relationships of adolescent girls in sub‐Saharan Africa. Stud Fam Plann. 2003;34(2):67–86. [DOI] [PubMed] [Google Scholar]
- 57. Zembe YZ, Townsend L, Thorson A, Ekstrom AM. “Money talks, bullshit walks” interrogating notions of consumption and survival sex among young women engaging in transactional sex in post‐apartheid South Africa: a qualitative enquiry. Global Health. 2013;9:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357(4):370–9. [DOI] [PubMed] [Google Scholar]
- 59. Kadushin C. Who benefits from network analysis: ethics of social network research. Soc Networks. 2005;27(2):139–53. [Google Scholar]
- 60. Harris JK. Consent and confidentiality: exploring ethical issues in public health social network research. Connections. 2008;28(2):81–96. [Google Scholar]
- 61. Pattison P, Robins G, Snijders TAB, Wang P. Conditional estimation of exponential random graph models from snowball sampling designs. J Math Psychol. 2013;57(6):284–96. [Google Scholar]
- 62. Campbell R, Starkey F, Holliday J, Audrey S, Bloor M, Parry‐Langdon N, et al. An informal school‐based peer‐led intervention for smoking prevention in adolescence (ASSIST): a cluster randomised trial. Lancet. 2008;371(9624):1595–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Starkey F, Audrey S, Holliday J, Moore L, Campbell R. Identifying influential young people to undertake effective peer‐led health promotion: the example of A Stop Smoking In Schools Trial (ASSIST). Health Educ Res. 2009;24(6):977–88. [DOI] [PubMed] [Google Scholar]
- 64. Valente TW, Ritt‐Olson A, Stacy A, Unger JB, Okamoto J, Sussman S. Peer acceleration: effects of a social network tailored substance abuse prevention program among high‐risk adolescents. Addiction. 2007;102(11):1804–15. [DOI] [PubMed] [Google Scholar]
- 65. Kelly JA, Murphy DA, Sikkema KJ, McAuliffe TL, Roffman RA, Solomon LJ, et al. Randomised, controlled, community‐level HIV‐prevention intervention for sexual‐risk behaviour among homosexual men in US cities. Community HIV Prevention Research Collaborative. Lancet. 1997;350(9090):1500–5. [DOI] [PubMed] [Google Scholar]
- 66. Minnis AM, vanDommelen‐Gonzalez E, Luecke E, Cheng H, Dow W, Bautista‐Arredondo S, et al. Social network recruitment for Yo Puedo: an innovative sexual health intervention in an underserved urban neighborhood‐sample and design implications. J Prim Prev. 2015;36(1):51–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Amirkhanian YA, Kelly JA, Takacs J, McAuliffe TL, Kuznetsova AV, Toth TP, et al. Effects of a social network HIV/STD prevention intervention for MSM in Russia and Hungary: a randomized controlled trial. AIDS. 2015;29(5):583–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Pufall EL, Nyamukapa C, Eaton JW, Campbell C, Skovdal M, Munyati S, et al. The impact of HIV on children's education in eastern Zimbabwe. AIDS Care. 2014;26(9):1136–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Ncama BP, McInerney PA, Bhengu BR, Corless IB, Wantland DJ, Nicholas PK, et al. Social support and medication adherence in HIV disease in KwaZulu‐Natal, South Africa. Int J Nurs Stud. 2008;45(12):1757–63. [DOI] [PubMed] [Google Scholar]
- 70. Cluver L. Peer group support intervention reduces psychological distress in AIDS orphans. Evid‐Based Ment Health. 2009;12(4):120. [DOI] [PubMed] [Google Scholar]
- 71. Cluver L, Bowes L, Gardner F. Risk and protective factors for bullying victimization among AIDS‐affected and vulnerable children in South Africa. Child Abuse Negl. 2010;34(10):793–803. [DOI] [PubMed] [Google Scholar]


