Abstract
Background
To examine sexual violence across the lifespan among transgender and cisgender people living with HIV (PLWH), and its associations with recent risk behaviors.
Setting
Seven community-based sites serving priority populations disproportionately affected by HIV in the U.S., including major metropolitan areas in the West and East Coast, as well as the suburban-Mid-Atlantic and Rural-Southeastern regions.
Methods
From 2013–2016, baseline survey data were collected from participants (N=583) of a multisite community-based HIV linkage to/retention in care study conducted at seven sites across the U.S. Adjusted mixed-effects logistic regression models with random effect for site assessed associations of sexual violence and gender identity with risk outcomes including condomless sex, sex trade involvement, and substance use-related harms.
Results
One-third of participants reported a history of sexual violence; transgender-(AOR= 5.1, 95% CI= 2.6, 10.1) and cisgender women (AOR= 3.8, 95% CI= 2.3, 6.4), were more likely than cisgender men to experience sexual violence. Sexual violence was associated with experiencing drug-related harms (AOR= 2.6, 95% CI= 1.2, 5.5). Transgender women were more likely than cisgender men to have sold sex (AOR= 9.3, 95% CI= 1.7, 50.0).
Conclusion
History of sexual violence is common among transgender and cisgender women PLWHA, and increases risk for drug-related harms. Transgender women are also more likely to report selling sex.
Keywords: Sexual Violence, HIV, Gender, Transgender, Sexual Orientation
INTRODUCTION
Sexual violence, as defined by the Centers for Disease Control and Prevention (CDC), reflects the experience of a sexual act (e.g., rape, unwanted sexual touching, pressure or coercion to engage in sexual acts) committed against an individual without their freely given consent.1 These acts are disproportionatelytargeted against members of marginalized groups such as women (relative to men),2 sexual minorities (relative to heterosexuals),3 and transgender persons4 (relative to cisgender persons [i.e., an individual whose personal gender identity corresponds to the sex they were assigned at birth5]). In the United States, national estimates indicate that 19.3% and 43.9% of women have experienced rape (i.e., “completed or attempted forced penetration or alcohol- or drug-facilitated penetration”) or other forms of sexual violence, respectively, in their lifetime; this is a prevalence almost 10 times that of men.2
While nationally representative data do not provide insight into experiences of sexual violence among transgender individuals, a review of estimates across studies of transgender people indicates an even higher prevalence of sexual violence in this population, where most studies found approximately 50% of transgender persons were affected.4 As the prevalence of sexual violence varies by gender, so too does the age at which sexual violence is first experienced across the lifespan, with cisgender men and transgender people being more likely to initially experience sexual violence in childhood4 compared to cisgender women who more typically first experience sexual violence in adolescence and young adulthood.2 To date, there have been limited efforts to examine experiences of sexual violence by gender that extend beyond the cisgender man-woman binary.
Experiences of sexual violence have been well-documented to increase individuals’ risk for numerous health concerns, including injury, pelvic pain, mental health, and trauma symptoms, as well as poorer sexual and reproductive health outcomes, including HIV.6–9 Prior research has demonstrated heightened sexual and substance-using risk behaviors known to increase the risk of acquiring or transmitting HIV among persons with a history of sexual violence.10, 11 This work demonstrates historic sexual abuse such as that occurring in childhood, as well as recent experiences of sexual violence, as significant correlates of both HIV and risk behaviors associated with HIV transmission and includes research mostly with cisgender women and sexual minority men at risk for HIV.12–15 Less research has explored whether gender identity, inclusive of transgender women, and sexual violence are associated with ongoing sexual and substance use risk behavior among people living with HIV (PLWH). Such analyses are needed given the disproportionate prevalence of HIV (estimated 22%–28%)16, 17 and sexual violence4 facing transgender women in the U.S.
To explore these issues among PLWH, this paper will assess experiences of sexual violence across the lifespan among a sample of adult PLWH recruited from community-based organizations in the US, and whether such experiences, in terms of both timing and perpetrator, differ by gender identity (cisgender male, cisgender women, transgender women). We also examine the associations between lifetime history of sexual violence and gender identity with recent sexual and substance use risk behaviors. Documentation of the relationships between ongoing HIV risk and experiences of sexual violence among PLWH could meaningfully inform ways sexual violence, as a determinant of health, may contribute to the ongoing transmission of HIV. Identifying ways such relationships might differ by gender identity could further inform a more targeted gender- and trauma-responsive public health response, vis-à-vis policy, and service delivery efforts, that integrates the prevention and treatment of sexual violence into national efforts aimed at reducing future HIV infections.
METHODS
Participants and Procedures
Baseline data was collected (October 2013 – August 2016) as part of a multi-site community-based HIV test and treat initiative. Seven community agencies across the United States recruited PLWH not engaged in–or tenuously engaged in (i.e., inconsistent use of care across the past year or no use in the past 6 months)–HIV medical care. These agencies serve communities reflective of priority populations disproportionately affected by HIV/AIDS in the U.S. Epidemic in both major metropolitan areas (Black and Latino MSM, transgender women, women of color, recently incarcerated persons, persons who inject drugs), as well as the suburban-Mid-Atlantic and Rural-Southeastern regions (low-income African Americans). Sites recruited participants via outreach using health care client listings, service programs (e.g., substance abuse treatment, re-entry), advertisements and snowball sampling, and/or via outreach at specific venues (e.g., bath houses), focusing on their populations of interest (e.g., transgender women, substance using, prison re-entry, Black women), which varied by site. Participants were required to be age 18 or older and diagnosed with HIV or at risk for HIV and willing to test at time of enrollment. Only participants diagnosed with HIV were included in current analyses (N=583), excluding 31 HIV-negative participants.
Subsequent to eligibility verification and informed consent acquisition, eligible participants were asked to complete an in-person baseline survey administered by trained agency or external evaluation staff. All surveys were conducted in private locations on paper or using mobile tablets, per agency preference. Participants were then linked to either an enhanced intervention to support engagement in HIV care and uptake of antiretroviral therapy (ART) or the agencies’ standard of care services reflecting a control comparison, per the larger study’s evaluation design. Three and six-month follow-up surveys were conducted, but are not included in current analyses. Remuneration for participants’ time given to study activities was decided by each study site with a concerted effort to be responsive to the needs of their clientele while maintaining an established rapport with their respective communities. Remuneration values for the baseline assessment ranged from $10 to $25. All study procedures were approved by the institutional review boards of each site and/or the institution of the multi-site initatives evaluation team.
Measures
Sociodemographic items included age, sexual orientation (bisexual, lesbian/gay/queer [LGQ], heterosexual), and gender identity (man, woman, or transgender women [male-to-female], or transgender man [female-to-male]). No participants identified as transgender men. With the recognition that transgender individuals may self-identify as men or women, rather than transgender in the survey, a validity assessment was done based on agency gender identity records. If the individual reported as transgender in either the study survey or the agency record, they were defined as transgender for these analyses to reflect their potential exposure to gender-based vulnerabilities. Participants not identified as having a lived transgender experience by either method were coded as a cisgender man or a cisgender woman. A single item also assessed time since HIV diagnosis, dichotomized as < 12 months or ≥12 months.
Sexual violence was measured using a series of items taken from a previously published measure on violence created for use with clinic-based populations living with or at risk for HIV/STI.18–20 Experiences of sexual violence were defined as, ‘having been forced or pressured for sex,’ or having someone ‘physically hurting the sexual parts of your body, including touching that made you feel uncomfortable.’ Participants indicated if they had ever (Yes, No) experienced sexual violence, and then indicated at which time points in their lifetime they experienced such events (Yes, No): childhood (infancy – 11 years), adolescence (12–17 years), young adulthood (18–24 years), adulthood (25 years or older), and more recently (past 12 months). For each time point on which they reported yes (multiple time points could be selected), they were asked about their relationship to the perpetrator (e.g., parent, partner) via a series of closed-ended options and an additional open-ended “other” option. Based on frequencies across categories including “other”, responses were categorized as: family members/caregivers (parents, other family members, current/former partners of a family member, foster family members, non-family caregivers [e.g., teacher, babysitter]), partners (previous/current sexual or primary partner), personal or family acquaintances (peers, acquaintances, family friend/neighbor, acquaintance of a family member), persons from drug and sex work interactions (sex work clients, drug dealers), and other (strangers, gang members, prisoners, law enforcement, perpetrator type not specified).
Risk behaviors included both sex and substance use-related risks. Sexual risk behavior having occurred in the past 90 days reflected participants who indicated (Yes, No) whether they had engaged in condomless sex (vaginal or anal), had multiple (>1) sexual partners, or ‘sold sex in exchange for money, drugs, food, or other goods.’ Drug and alcohol-related risk behaviors were assessed using the TCU-DS2 and an adapted version of the AUDIT-10 (items 1–3, 9–10),21 respectively.22 Drug-related risk (Yes, No) in the past 30 days reflected any self-reported illicit drug use (excluding marijuana) or having experienced any harms (i.e., creating difficulties in relationships or daily functioning) because of this use. Alcohol-related risk (Yes, No) reflected participants who indicated they had engaged in binge drinking (≥5 drinks in one setting; adapted from AUDIT item 3) in the past 30 days or experienced alcohol-related harms (i.e., one’s drinking resulting in injury to self or others; AUDIT items 9–10) in the past 12 months.
Statistical Analysis
Descriptive statistics were used to characterize the sample’s basic demographics, histories of sexual violence including timing and perpetrator types, and more recent sexual and substance use-related risk behaviors. Fisher’s exact test (P<.05) assessed for between-group differences in histories of sexual violence across the lifespan by gender identity. Mixed-effects logistic regression models (GLMM) with a random effect for study site (agency) were used to test for associations between gender identity and history of sexual violence across the lifespan, and to test for the associations of gender identity and having experienced lifetime sexual violence on more recent sexual and substance use risk behaviors. All models adjusted for sexual orientation, age and time since HIV diagnosis. Education, homelessness, and history of incarceration were considered for inclusion as covariates but were not significantly associated with outcomes. To investigate potential effect modification, the interaction between gender identity and sexual orientation was added to all adjusted models, and statistical significance of the interaction term was evaluated at the α=.15 level. All tests were two-tailed, and analyses were conducted using SAS, Version 9.4 (Cary, NC).
RESULTS
Participant Characteristics
Participants (N=583, median age=45.0 years, range: 18–78; 6.2% young adults age 18–24) were 55.1% cisgender men, 34.1% cisgender women and 10.8% transgender women (see Table 1). Just over half of the sample (55.4%) identified as heterosexual, 29.0% were LGQ, and 15.6% identified as bisexual. The majority of both cisgender and transgender women identified as heterosexual (79.5% and 63.9%, respectively), compared with 38.7% of men. While 43.8% of men identified as LGQ or bisexual, only 6.2% of cisgender women and 26.2% of transwomen women identified as such. The majority were Black (75.5%) or Hispanic (15.1%). Most participants (86.5%) had been diagnosed as HIV-positive for 12 months or more (7.9%, < 3 months). Most participants were not employed full-time (90.9%) and lived on $1,000 per month or less (81.3%).
Table 1.
Sociodemographic Characteristics and Risk Behaviors (n = 583)
| Characteristic | Full sample | Cisgender Men | Cisgender Women | Transgender Women |
|---|---|---|---|---|
| No. (%) | No. (%) | No. (%) | No. (%) | |
| Total | - | 321 (55.1) | 199 (34.1) | 63 (10.8) |
|
| ||||
| Age | ||||
| Mean (SD) | 43.4 (11.6) | 42.2 (11.9) | 45.8 (11.1) | 41.6 (10.6) |
| median; range | 45; 18–78 | 45 19–78 | 48; 18–76 | 40; 23–72 |
| Young adults (18–24) | 36 (6.2) | 25 (7.8) | 10 (5.0) | 1 (1.6) |
|
| ||||
| Sexual orientation | ||||
| Heterosexual | 315 (55.4) | 121 (38.7) | 155 (79.5) | 39 (63.9) |
| Homosexual/Gay/Lesbian/Queer | 165 (29.0) | 137 (43.8) | 12 (6.2) | 16 (26.2) |
| Bisexual | 89 (15.6) | 55 (17.6) | 28 (14.4) | 6 (9.8) |
|
| ||||
| Race/ethnicity | ||||
| White | 28 (4.8) | 17 (5.3) | 9 (4.5) | 2 (3.2) |
| Black/African American | 440 (75.5) | 215 (67.0) | 173 (86.9) | 52 (82.5) |
| Hispanic/Latino | 88 (15.1) | 74 (23.1) | 10 (5.0) | 4 (6.4) |
| Other | 27 (4.6) | 15 (4.7) | 7 (3.5) | 5 (7.9) |
|
| ||||
| Time since HIV diagnosis | ||||
| < 3 months | 45 (7.9) | 33 (10.5) | 12 (6.2) | 0 (0.0) |
| 3 months-1 year | 32 (5.6) | 20 (6.4) | 11 (5.6) | 1 (1.6) |
| 1–4 years | 75 (13.1) | 41 (13.0) | 22 (11.3) | 12 (19.4) |
| 5–9 years | 118 (20.6) | 57 (18.1) | 42 (21.5) | 19 (30.7) |
| ≥ 10 years | 302 (52.8) | 164 (52.1) | 108 (55.4) | 30 (48.4) |
|
| ||||
| Did not complete high school | 180 (30.9) | 90 (28.0) | 67 (33.7) | 23 (36.5) |
|
| ||||
| No full-time employment | 529 (90.9) | 284 (88.8) | 188 (94.5) | 57 (90.5) |
|
| ||||
| Low income (≤ $1,000 per month) | 474 (81.3) | 255 (79.4) | 170 (85.4) | 49 (77.8) |
|
| ||||
| Homelessness, past 90 days | 177 (30.4) | 107 (33.3) | 44 (22.1) | 26 (41.9) |
|
| ||||
| Prior incarceration | ||||
| Yes, in past 12 months | 169 (29.0) | 131 (40.8) | 21 (10.6) | 17 (27.0) |
| Yes, but not in past 12 months | 233 (40.0) | 96 (29.9) | 100 (50.3) | 37 (58.7) |
|
| ||||
| Substance Use | ||||
| Illicit drug use, past 30 daysa | 111 (19.0) | 49 (15.3) | 56 (28.1) | 6 (9.5) |
| Drug-related harm, past 30 daysa | 80 (13.7) | 30 (9.4) | 45 (22.6) | 5 (7.9) |
| Binge drinking, past 30 days | 95 (16.3) | 52 (16.2) | 26 (13.1) | 17 (27.0) |
| Alcohol-related harm, past 12 months | 59 (10.1) | 36 (11.2) | 19 (9.6) | 4 (6.4) |
|
| ||||
| Sex with multiple partners, past 90 days | 134 (23.1) | 94 (29.6) | 22 (11.1) | 18 (28.6) |
|
| ||||
| Condomless anal or vaginal sex, past 90 days | 129 (22.3) | 69 (21.8) | 36 (18.1) | 24 (38.1) |
|
| ||||
| Sold sex, past 90 days | 52 (9.0) | 13 (4.1) | 16 (8.1) | 23 (37.1) |
Note. Significant differences tested with Fisher exact test (P <.05) are in bold text.
Excluding marijuana/hashish.
Regarding sexual risk behaviors in the past 90 days, almost one-quarter (23.1%) had multiple sex partners, 22.3% reported condomless anal or vaginal sex, and 9.0% had sold sex in this timeframe. Both condomless sex and selling sex were more common among transgender women (38.1% and 37.1%, respectively) relative to men (21.8% and 4.1%) and cisgender women (18.1% and 8.1 %). Substance use behaviors in the past 30 days reflected 19.1% of the sample who reported any illicit drug use (excluding marijuana) and 13.7% who reported experiencing harms related to their use. Sixteen percent (16.3%) reported binge drinking in the past 30 days, and approximately 10% of participants reported experiencing harms related to their alcohol use in the past 12 months.
Histories of Sexual Violence by Gender Identity
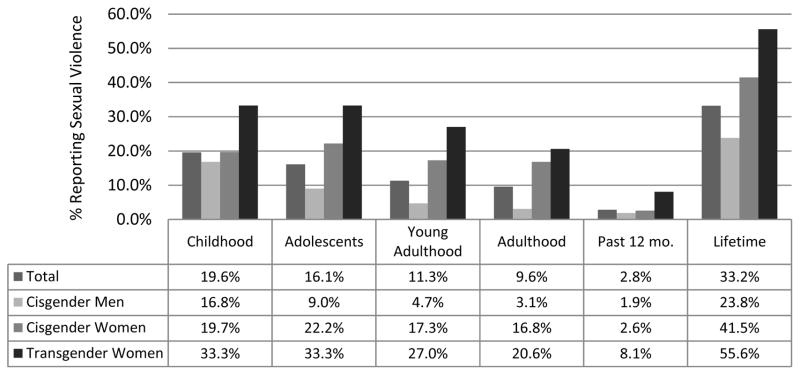
In total, 33.2% of the sample reported having ever experienced sexual violence in their lifetime (see Table 2). In general, experiences of sexual violence across the lifespan were highest in childhood (19.6%), gradually decreasing through adolescence (16.1%), young adulthood (11.3%), and into adulthood (9.6%); acknowledging that 6.2% of participants (cisgender men 4.3%, cisgender women 1.7%, transgender women 0.2%) were still young adults. Significant differences by gender identity were observed in the proportion of participants experiencing sexual violence across the lifespan, demonstrating a disproportionate burden of sexual violence affecting transgender women at each developmental timeframe (childhood: 33.3%, P = .015; adolescence: 33.3%, P<.001; young adulthood: 27.0%, P<.001; adulthood: 20.6%, P<.001; past 12-months: 8.1%, P = .04; lifetime: 55.6%, P<.001) compared to cisgender men. A similar pattern was observed for cisgender women across the lifespan compared to cisgender men. Focusing on experiences of sexual violence in the past 12 months, we also observed a significantly higher proportion of transgender women (8.1%) who were affected compared to cisgender men (1.9%) and cisgender women (2.6%).
Table 2.
Sexual violence (SV) perpetrator type by gender identity across the lifespan
| Timing of SV | Full sample (n=583), No. (%) | Cisgender Men (n=321), No. (%) | Cisgender Women (n=199), No. (%) | Transgender Women (n=63), No. (%) |
|---|---|---|---|---|
| SV in Childhood | 113 (19.6) | 54 (16.8) | 38 (19.6) | 21 (33.3) |
| Family members/caregivers | 72 (63.7) | 30 (55.6) | 29 (76.3) | 13 (61.9) |
| Personal or family acquaintances | 27 (23.9) | 16 (29.6) | 6 (15.8) | 5 (23.8) |
| Drug and sex work interactions | 1 (0.9) | 0 (0.0) | 1 (2.6) | 0 (0.0) |
| Other | 36 (31.9) | 14 (25.91) | 10 (26.3) | 12 (57.1) |
|
| ||||
| SV in Adolescence | 93 (16.1) | 29 (9.0) | 43 (22.2) | 21 (33.3) |
| Family members/caregivers | 46 (49.5) | 12 (41.4) | 22 (51.2) | 12 (57.1) |
| Current/former partners | 10 (10.8) | 3 (10.3) | 5 (11.6) | 2 (9.5) |
| Personal or family acquaintances | 22 (23.7) | 9 (31.0) | 7 (16.3) | 6 (28.6) |
| Drug and sex work interactions | 3 (3.2) | 0 (0.0) | 2 (4.7) | 1 (4.8) |
| Other | 31 (33.3) | 11 (37.9) | 12 (27.9) | 8 (38.1) |
|
| ||||
| SV in Young Adulthood | 65 (11.3) | 15 (4.7) | 33 (17.3) | 17 (27.0) |
| Family members/caregivers | 10 (15.4) | 2 (13.3) | 5 (15.2) | 3 (17.7) |
| Current/former partners | 25 (38.5) | 4 (26.7) | 11 (33.3) | 10 (58.8) |
| Personal or family acquaintances | 7 (10.8) | 4 (26.7) | 2 (6.1) | 1 (5.9) |
| Drug and sex work interactions | 6 (9.2) | 0 (0.0) | 3 (9.1) | 3 (17.7) |
| Other | 32 (49.2) | 8 (53.3) | 19 (57.6) | 5 (29.4) |
|
| ||||
| SV in Adulthood | 55 (9.6) | 10 (3.1) | 32 (16.8) | 13 (20.6) |
| Family members/caregivers | 3 (5.5) | 1 (10.0) | 1 (3.1) | 1 (7.7) |
| Current/former partners | 20 (36.4) | 3 (30.0) | 11 (34.4) | 6 (46.2) |
| Personal or family acquaintances | 10 (18.2) | 3 (30.0) | 7 (21.9) | 0 (0.0) |
| Drug and sex work interactions | 1 (2.1) | 0 (0.0) | 1 (3.6) | 0 (0.0) |
| Other | 31 (56.4) | 4 (40.0) | 20 (62.5) | 7 (53.9) |
|
| ||||
| SV in the Past 12 Months | 16 (2.8) | 6 (1.9) | 5 (2.6) | 5 (8.1) |
| Family members/caregivers | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Current/former partners | 7 (43.8) | 3 (50.0) | 2 (40.0) | 2 (40.0) |
| Personal or family acquaintances | 3 (18.8) | 2 (33.3) | 0 (0.0) | 1 (20.0) |
| Drug and sex work interactions | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Other | 8 (50.0) | 2 (33.3) | 3 (60.0) | 3 (60.0) |
|
| ||||
| SV ever in Lifetime | 192 (33.2) | 76 (23.8) | 81 (41.5) | 35 (55.6) |
Note. Multiple responses per respondent were possible. “Other” includes: stranger, gang member, law enforcement, prisoners, unidentified. Significant differences tested with Fisher exact test (P <.05) are in bold text.
As reported in Table 2, amongst those experiencing sexual violence in childhood and adolescence, most reported that these experiences were perpetrated by family members/caregivers (childhood: 63.7%, adolescence: 49.5%), personal or family acquaintances (childhood: 23.9%, adolescence: 23.7%), or other types of persons including strangers and perpetrators that participants chose not to identify (childhood: 31.9%, adolescence: 33.3%). However, perpetrators of sexual violence in young adulthood and adulthood reflected an increase in these ‘other’ types of perpetrators reported (young adulthood: 49.2%, adulthood: 56.4%) by those experiencing sexual violence, as well as sexual violence perpetrated by current/former partners (young adulthood: 38.5%, adulthood: 36.4%). This pattern was also observed among those reporting sexual violence in the past 12 months (current/former partner: 43.8%, other: 50.0%). Additionally, we observed an increase in cisgender and transgender women reporting experiences of sexual violence in relation to drug and sex work interactions in adolescence (cisgender women: 4.7%, transgender women: 4.8%) and young adulthood (cisgender women: 9.1%, transgender women, 17.7%). However, no significant differences in the perpetrators of sexual violence by gender identity were observed.
In the adjusted regression analysis (see Table 3), the odds of having ever experienced sexual violence in one’s lifetime were five times greater for transgender women (adjusted odds ratio [AOR] = 5.1, 95% confidence interval [CI] = 2.6, 10.1) and nearly four times greater (AOR = 3.8, 95% CI = 2.3, 6.4) for cisgender women than cisgender males. Transgender women, relative to cisgender men, were at greater odds of having experienced sexual violence during each life stage (childhood: AOR = 2.9, 95% CI = 1.4, 6.0; adolescence: AOR = 6.3, 95% CI = 2.0, 19.7; young adulthood: AOR = 8.0, 95% CI = 3.6, 18.0; adulthood: AOR = 8.0, 95% CI = 3.2, 20.2). For cisgender women, this pattern of increased odds for experiencing sexual violence, relative to cisgender males, was first identified in adolescence (childhood: AOR = 1.6, 95% CI = 0.9, 2.9; adolescence: AOR = 3.4, 95% CI = 1.5, 7.4; young adulthood: AOR = 5.5, 95% CI = 2.6, 11.4; adulthood: AOR = 7.5, 95% CI = 3.3, 17.0). No significant differences were observed between transgender women and cisgender women.
Table 3.
Adjusted logistic generalized linear mixed models (GLMMs) assessing associations of sociodemographic characteristics and time since HIV diagnosis with sexual violence outcomes
| SV in Childhood | SV in Adolescence | SV in Young Adulthood | SV in Adulthood | SV in the Past 12 Months | SV Ever in Lifetime | |
|---|---|---|---|---|---|---|
|
| ||||||
| Variable | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) |
| Gender Identity | ||||||
| Transgender women | 2.9 (1.4, 6.0) | 6.3 (2.0, 19.7) | 8.0 (3.6, 18.0) | 8.0 (3.2, 20.2) | 3.6 (0.7, 18.5) | 5.1 (2.6, 10.1) |
| Cisgender women | 1.6 (0.9, 2.9) | 3.4 (1.5, 7.4) | 5.5 (2.6, 11.4) | 7.5 (3.3, 17.0) | 1.5 ( 0.3, 6.6) | 3.8 (2.3, 6.4) |
| Cisgender men (Ref) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
|
| ||||||
| Sexual Orientation | ||||||
| Bisexual | 1.6 (0.8, 2.9) | 2.2 (1.1, 4.3) | 1.2 (0.5, 2.6) | 1.7 (0.7, 3.9) | 1.0 (0.2, 4.2) | 2.8 (1.6, 4.9) |
| Lesbian/Gay/Queer | 1.6 (0.9, 2.8) | 1.7 (0.9, 3.4) | 1.5 (0.7, 3.0) | 1.8 (0.8, 3.9) | 0.5 (0.1, 2.2) | 2.2 (1.3, 3.8) |
| Heterosexual (Ref) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
|
| ||||||
| Agea | 0.9 (0.8, 1.0) | 0.9 (0.8, 0.96) | 0.9 (0.8, 1.0) | 1.0 (0.9, 1.2) | 0.7 (0.6, 0.97) | 0.9 (0.8, 0.95) |
|
| ||||||
| Time Since HIV Diagnosis | ||||||
| < 12 Months | 0.6 (0.3, 1.2) | 0.5 (0.2, 1.1) | 0.7 (0.3, 1.8) | 0.5 (0.2, 1.8) | 1.6 (0.4, 6.3) | 0.4 (0.2, 0.8) |
| ≥ 12 Months (Ref) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
Note. AOR = adjusted odds ratio; CI = confidence interval. Site is a random effect; all other variables are fixed effects. Significant AORs in bold text.
Odds ratio estimates are for 5-year increases in age.
Independent of gender identity, sexual minority participants, compared to heterosexuals, were found to have over two times greater odds of having ever experienced sexual violence in their lifetime (bisexual: AOR = 2.8, 95% CI = 1.6, 4.9; LGQ: AOR = 2.2, 95% CI = 1.3, 3.8), with bisexual persons demonstrating increased risk of experiencing sexual violence during adolescence (AOR = 2.2, 95% CI = 1.1, 4.3). Both age (AOR = 0.9, 95% CI = 0.8, 0.95) and recent HIV diagnosis (AOR = 0.4, 95% CI = 0.2, 0.8) were associated with decreased odds of having experienced sexual violence in one’s lifetime.
In post-hoc analyses, the only outcome for which there was a significant interaction effect between gender identity and sexual orientation was lifetime sexual violence (P=.10). See Supplemental Table 1. Adjusting for this interaction term reduced the odds of experiencing lifetime sexual violence for transgender women from 5.1 to 3.9 (95% CI = 1.8, 8.6) times higher relative to cisgender men. Additionally, the effect for LGQ participants became non-significant. When the results were restricted to cisgender men (see Supplemental Table 2), sexual minority men were more likely to have experienced lifetime sexual violence (Bisexual men: AOR = 4.3, 95% CI = 1.8, 10.1; LGQ men: AOR = 4.0, 95% CI = 1.9, 8.4) than heterosexual men. Among cisgender women, bisexual women had 3.1 (95% = CI 1.3, 7.4) times higher odds of being a victim of sexual violence relative to heterosexual women, whereas no such differences were found among transgender women.
Lifetime Sexual Violence and Recent Risk Behavior
Adjusting for gender identity, sexual orientation, age, and time since HIV diagnosis, participants who reported a lifetime history of sexual violence (vs. those who did not) were 2.6 times more likely (95% CI = 1.2, 5.5) to report harmful outcomes associated with their illicit drug use in the past 30 days. Associations between lifetime history of sexual violence and other recent sexual- or drug-risk related behaviors in this sample (see Table 4), reflected increased odds of reporting illicit drug use in the past 30 days (AOR = 1.9, 95% CI = 1.01, 3.6), and non-significant trends toward higher odds of reporting alcohol-related harms in the past 12 months (AOR = 1.7, 95% CI = 0.9, 3.1), and having sold sex in the past 90 days (AOR = 1.8, 95% CI = 0.9, 3.7).
Table 4.
Adjusted logistic generalized linear mixed models (GLMMs) for association of sexual violence history and HIV-related risk behaviors
| Condomless Sexa | Multiple partnersa | Illicit drug useb, c | Drug-related harmb, c | Binge drinkingb | Alcohol-related harmd | Selling sexa | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Variable | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) |
| History of Sexual Violence | |||||||
| Yes | 1.1 (0.7, 1.7) | 1.4 (0.9, 2.3) | 1.9 (1.01, 3.6) | 2.6 (1.2, 5.5) | 1.1 (0.7, 1.8) | 1.7 (0.9, 3.1) | 1.8 (0.9, 3.7) |
| No (Ref) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
|
| |||||||
| Gender Identity | |||||||
| Transgender women | 2.9 (0.98, 8.4) | 1.0 (0.3, 2.9) | 0.4 (0.1, 2.6) | 0.5 (0.1, 4.0) | 2.0 (0.96, 4.1) | 0.5 (0.2, 1.6) | 9.3 (1.7, 50.0) |
| Cisgender women | 1.7 (0.8, 3.5) | 0.6 (0.3, 1.2) | 1.2 (0.5, 2.8) | 1.1 (0.5, 2.6) | 1.0 (0.6, 1.9) | 0.9 (0.4, 1.9) | 1.7 (0.6, 4.9) |
| Cisgender men (Ref) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
|
| |||||||
| Sexual Orientation | |||||||
| Bisexual | 1.4 (0.7, 2.7) | 3.9 (2.1, 7.4) | 1.3 (0.6, 2.8) | 0.8 (0.3, 2.0) | 1.8 (0.9, 3.5) | 1.3 (0.6, 2.9) | 1.4 (0.5, 3.7) |
| Lesbian/Gay/Queer | 1.7 (0.9, 3.0) | 2.5 (1.4, 4.5) | 1.1 (0.5, 2.5) | 0.9 (0.3, 2.2) | 1.8 (0.99, 3.2) | 1.6 (0.8, 3.3) | 1.1 (0.5, 2.8) |
| Heterosexual (Ref) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
|
| |||||||
| Agee | 0.9 (0.8, 1.0) | 1.0 (0.9, 1.1) | 1.3 (1.1, 1.5) | 1.1 (0.9, 1.3) | 0.9 (0.8, 1.0) | 1.0 (0.9, 1.1) | 0.9 (0.8, 1.1) |
|
| |||||||
| Time Since HIV Diagnosis | |||||||
| < 12 Months | 1.8 (0.96, 3.2) | 1.6 (0.9, 3.0) | 1.6 (0.6, 4.0) | 1.9 (0.6, 5.5) | 0.9 (0.4, 1.8) | 1.3 (0.6, 2.9) | 1.2 (0.4, 3.7) |
| ≥ 12 Months (Ref) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
Note. AOR = adjusted odds ratio; CI = confidence interval. Site is a random effect; all other variables are fixed effects. Significant AORs in bold text.
Past 90 days.
Past 30 days.
Excluding marijuana/hashish.
Past 12 months.
Odds ratio estimates are for 5-year increases in age.
Similarly, gender identity was not significantly associated with any of the risk-related outcomes except for selling sex, for which transgender women were nine times more likely (AOR = 9.3, 95% CI = 1.7, 50.0) to report selling sex relative to cisgender men. A non-significant trend was observed suggesting transgender women had increased odds of reporting binge drinking in the past 30 days (AOR = 2.0, 95% CI = 0.96, 4.1) and engaging in condomless sex in the past 90 days (AOR = 2.9, 95% CI = 0.98, 8.4) relative to cisgender men. Exploratory analyses tested for interaction effects between lifetime sexual violence and gender identity on having sold sex in the past 90 days. No significant interaction effects were identified (P<.15), though these findings may be due to small cell sizes.
Additionally, sexual minority participants had an increased odds of reporting multiple sex partners in the past 90 days (bisexual: AOR = 3.9, 95% CI = 2.1, 7.4; LGQ: AOR = 2.5, 95% CI = 1.4, 4.5), but were not more likely to have increased odds of condomless sex relative to heterosexuals. In contrast to the negative relationship observed between age and sexual violence, the odds of illicit drug use increased for every five additional years of age (AOR = 1.3, 95% CI = 1.1, 1.5).
DISCUSSION
Experiences of sexual violence were exceedingly common in this community-recruited HIV-positive sample, with one-third of adults reporting a lifetime history. Experiences of lifetime sexual violence for cisgender women (42.0%) and cisgender men (23.8%) in this HIV-positive sample were relatively comparable to national estimates of the general population in the United States (Women 43.9%; Men 23.4%).2 National estimates are not available for transgender women at this time. While limited research with PLWH has focused on the prevalence of lifetime sexual violence, estimates suggest between 30%23–35%24 of men, and 22%-44%25 of women are affected, though one study observed 68% of HIV-positive women in the sample had a lifetime experience of sexual violence.24 Another study observed well over half (67%) of HIV-positive transgender women in San Francisco reported experiences of forced sex or rape.26 Comparatively, fewer men in our HIV-positive sample reported experiences of lifetime sexual violence, though estimates for cisgender women and transgender women were relatively similar to previous work.
For different developmental periods measured across the lifespan, the burden of sexual violence, relative to cisgender men, was disproportionately shouldered by transgender and cisgender women. This gendered disparity was most pronounced for transgender women in this HIV-positive sample, where over half had experienced sexual violence at some point in their lifetime, one-third of whom reported experiences of victimization in childhood and adolescence. Despite these disparities, it is important to recognize that the lifetime prevalence of sexual violence among men, and in particular sexual minority men, was quite high, predominantly reflecting experiences of sexual violence in childhood (16.8%). During these early developmental stages, PLWH reported experiences of sexual violence were predominantly perpetrated by family members/caregivers. Sexual violence was increasingly perpetrated by sexual partners and ‘other’ persons outside their family and personal networks as the developmental assessment periods moved from childhood towards adulthood. In relation to more recent risk-related vulnerabilities, PLWH with a lifetime history of sexual violence were significantly more likely to report harmful patterns of illicit drug use in the past 30 days, with trends towards increased engagement in harmful drinking patterns and sex work. Previous research has identified a heightened risk for sexual and substance use behaviors among persons with a prior history of sexual victimization; subsequently placing them at increased risk of acquiring HIV.10, 11 Similarly, among PLWH with a prior history of sexual violence, this increased risk for sexual and substance use behaviors are also observed, which can contribute to an increased risk of subsequent transmission and poorer HIV treatment outcomes (e.g., ART non-adherence, poorer viral suppression).13, 15, 27, 28
These findings suggest that as out-of-care HIV-positive transgender women, one in three were victimized in their youth. Such acts of sexual violence during their childhood and adolescents was most commonly perpetrated by family members and caregivers charged with their safety and well-being, as well as, ‘other’ types of persons external to their home environments (e.g., strangers). Given the high rates of victimization experienced by these transgender women early in their development both within and outside of the home environment, it appears critical that public institutions, such as schools, must provide targeted gender-affirming primary violence prevention efforts throughout these key developmental states. Enacting such protections echoes the need for further sociostructural actions to reduce the social marginalization of transgender and gender non-conforming youth, extending beyond the Obama Administration’s unprecedented Transgender Bathroom Directive that aimed to protect the right of transgender youth to use the bathroom that corresponds with their gender identity in public schools.29, 30 Nationally institutionalized sociostructural actions that aim to educate the public about gender minority youth and adults, and ensure protected access across school, recreational, employment, housing and other civic activities are needed to establish and reinforce gender-inclusive social norms and civil liberties in the U.S. The recent removal of the Transgender Bathroom Directive by the Trump Administration limits the potential reach of such sociostructural protections to the discretion of individual states.31
Findings further identify heightened vulnerability for transgender women at each assessment period across the lifespan, who were more likely to report currently engaging in sex work and exposure to sexual violence within sex work and drug-related contexts in adolescence and young adulthood. Experiences of sexual violence in the recent past were predominantly perpetrated by romantic partners and ‘other’ types of individuals external to their immediate social networks (e.g., strangers, law enforcement). The extant literature suggests sexual violence, especially early in life, may increase women’s entrance into sex work.11 For transgender women, in particular, sex work may be viewed as one of the few gender-affirming employment options when faced with stigma and discrimination that limits access to more traditional job opportunities.32, 33 In this context, our findings suggest secondary violence and HIV prevention efforts need to prioritize gender-affirming employment opportunities to help protect against exposure to subsequent sexual violence vis-à-vis sex work or economic dependence on sexually abusive romantic partners.5, 34 This would require the advancement of policies to generate trans-inclusive employment opportunities, and extend federal non-discrimination protections beyond those afforded to transgender military service members and transgender employees of federal contractors under the Obama Administration.35–37 To date, transgender persons lack protections from broad-based discrimination (e.g., housing, employment, education, public accommodations, etc.) in 31 U.S. states.38
The generalizability of the current study is limited by cross-sectional analyses of self-report data from a diverse, but non-nationally representative, community-based sample of PLWH across the U.S. Reflecting potentially stigmatizing experiences, sexual violence is typically underreported,39 and recall bias may differentially affect reports of sexual violence across different contexts (e.g., sexual assault involving drugs or alcohol vs. forcible rapes),40 and over the different developmental periods covered (e.g., childhood vs. young adulthood).41 For example, recall of experiences of sexual violence from early childhood may differ from that in the past 12 months; as such these data may reflect a more conservative estimate of sexual violence across the lifespan. Similarly, HIV-related risk behaviors were not assessed across equivalent recall periods, with harms related to alcohol use assessed over a longer recall period than others (12-months vs. 30 or 90-day recall). For those few participants more recently diagnosed, recall of sexual and substance use may be reflective of behaviors prior to HIV diagnosis. Despite these limitations, the sample reflects respondents from priority populations in the U.S. HIV epidemic,42 inclusive of a sample of transgender women large enough to allow comparative analyses of experiences with sexual violence by gender identity that extends beyond the cisgender man-woman binary.
These findings overall suggest that HIV programming for PLWH must assess for a history of sexual violence and the sequelae of its long-term associated traumas, particularly as they may be driving ongoing behavioral health risks (e.g., substance use and sexual health vulnerabilities). In kind, services responsive to these sequelae should be integrated into ongoing HIV treatment as prevention efforts aimed at improving individual health and reducing subsequent HIV incidence in priority populations across the U.S. Such programming, particularly for cisgender and transgender women should be gender-affirming, recognizing the unique social vulnerabilities all women face across the lifespan. For transgender women, these findings underscore an urgent need for both primary and secondary violence prevention efforts to reduce their social marginalization and afford legal protections from further sexual, social, and economic victimization.
Supplementary Material
FIGURE 1. Prevalence of Sexual Violence across the Lifespan by Gender Identity (N=583).
Significant difference between groups with Fisher’s Exact Test (P<.05) were found for all time points
Acknowledgments
Sources of support: Supported by Kaiser Permanente (Grant Number 20030041). The development and dissemination of the current subanalyses were supported by an NIH-NIDA–funded career development award (K01 DA039767) and NIH-NIMHD Loan Repayment Program Award (L60 MD009353) to LRS and NIH NIDA-funded career development award (K01 DA036439) to LU. No authors hold any financial disclosures associated with this work.
The authors would like to thank the community-based agencies, staff, and participants of the larger HIV Test and Treat initiative, as well as the Kaiser Permanente Community-Based HIV Test and Treat Study Team (Alexandra X. Caraballo, John Edmiston, Pamela M. Schwartz, Melissa Ramos), without whom this study would not be possible. We are also indebted to the countless hours of administrative and analytic support provided by Sankri Ayyaluru and Sanne P. Møller respectively.
Footnotes
Meetings at which part of the data was presented
Smith, L. R., Yore, J., Urada, L. A., Triplett, D. P, Moller, S. P., Ayyaluru, S., Nemoto, T., Edmiston, J. L., Ramos, M., Schwartz, P. M., Caraballo, A. X., Raj, A. (2016, September). Gender Identity, Sexual Violence, and HIV: Assessing gender-based disparities across the lifespan among a US sample of people living with HIV. Poster [Abstract 2173] presented at the 20th annual U.S. Conference on AIDS, Fort Lauderdale, FL.
Contributor Information
Laramie R. Smith, Center on Gender Equity and Health, Division of Global Public Health, Department of Medicine
Jennifer Yore, Center on Gender Equity and Health, Division of Global Public Health, Department of Medicine.
Daniel P. Triplett, Center on Gender Equity and Health, Division of Global Public Health, Department of Medicine.
Lianne Urada, Center on Gender Equity and Health, Division of Global Public Health, Department of Medicine.
Tooru Nemoto, Public Health Institute, Oakland, CA, United States, Kaiser Permanente Community-Based HIV Test and Treat Study Team, Kaiser Permanente, Oakland, CA, United States
Anita Raj, Center on Gender Equity and Health, Division of Global Public Health, Department of Medicine
References
- 1.Basile KC, Smith S, Breiding M, et al. Sexual violence surveillance: Uniform definitions and recommended data elements. Centers for Injury Prevention and Control; 2014. [Google Scholar]
- 2.Breiding MJ, Smith SG, Basile KC, et al. Prevalence and characteristics of sexual violence, stalking, and intimate partner violence victimization--national intimate partner and sexual violence survey, United States, 2011. MMWR Surveill Summ. 2014;63:1–18. [PMC free article] [PubMed] [Google Scholar]
- 3.Rothman EF, Exner D, Baughman AL. The Prevalence of Sexual Assault Against People Who Identify as Gay, Lesbian, or Bisexual in the United States: A Systematic Review. Trauma, Violence, & Abuse. 2011;12:55. doi: 10.1177/1524838010390707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stotzer RL. Violence against transgender people: A review of United States data. Aggression and Violent Behavior. 2009;14:170–9. [Google Scholar]
- 5.Schuster MA, Reisner SL, Onorato SE. Beyond Bathrooms—Meeting the Health Needs of Transgender People. N Engl J Med. 2016;375:101–3. doi: 10.1056/NEJMp1605912. [DOI] [PubMed] [Google Scholar]
- 6.Browne A, Finkelhor D. Impact of child sexual abuse: a review of the research. Psychol Bull. 1986;99:66. [PubMed] [Google Scholar]
- 7.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14:245–58. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 8.Krug EG, Mercy JA, Dahlberg LL, et al. The world report on violence and health. The Lancet. 2002;360:1083–8. doi: 10.1016/S0140-6736(02)11133-0. [DOI] [PubMed] [Google Scholar]
- 9.Zierler S, Feingold L, Laufer D, et al. Adult survivors of childhood sexual abuse and subsequent risk of HIV infection. Am J Public Health. 1991;81:572–5. doi: 10.2105/ajph.81.5.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Draucker CB, Mazurczyk J. Relationships between childhood sexual abuse and substance use and sexual risk behaviors during adolescence: An integrative review. Nurs Outlook. 2013;61:291–310. doi: 10.1016/j.outlook.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 11.Senn TE, Carey MP, Vanable PA. Childhood and adolescent sexual abuse and subsequent sexual risk behavior: Evidence from controlled studies, methodological critique, and suggestions for research. Clin Psychol Rev. 2008;28:711–35. doi: 10.1016/j.cpr.2007.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stall R, Mills TC, Williamson J, et al. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am J Public Health. 2003;93:939–42. doi: 10.2105/ajph.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cohen M, Deamant C, Barkan S, et al. Domestic violence and childhood sexual abuse in HIV-infected women and women at risk for HIV. Am J Public Health. 2000;90:560–5. doi: 10.2105/ajph.90.4.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stockman JK, Campbell JC, Celentano DD. Sexual violence and HIV risk behaviors among a nationally representative sample of heterosexual American women: the importance of sexual coercion. J Acquir Immune Defic Syndr. 2010;53:136–43. doi: 10.1097/QAI.0b013e3181b3a8cc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schafer KR, Gupta S, Dillingham R. HIV-infected men who have sex with men and histories of childhood sexual abuse: implications for health and prevention. Journal of the Association of Nurses in AIDS Care. 2013;24:288–98. doi: 10.1016/j.jana.2012.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baral SD, Poteat T, Strömdahl S, et al. Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. The Lancet infectious diseases. 2013;13:214–22. doi: 10.1016/S1473-3099(12)70315-8. [DOI] [PubMed] [Google Scholar]
- 17.Herbst JH, Jacobs ED, Finlayson TJ, et al. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS and Behavior. 2008;12:1–17. doi: 10.1007/s10461-007-9299-3. [DOI] [PubMed] [Google Scholar]
- 18.Reed E, Silverman JG, Welles SL, et al. Associations between perceptions and involvement in neighborhood violence and intimate partner violence perpetration among urban, African American men. J Community Health. 2009;34:328–35. doi: 10.1007/s10900-009-9161-9. [DOI] [PubMed] [Google Scholar]
- 19.Welles SL, Corbin TJ, Rich JA, et al. Intimate partner violence among men having sex with men, women, or both: early-life sexual and physical abuse as antecedents. J Community Health. 2011;36:477–85. doi: 10.1007/s10900-010-9331-9. [DOI] [PubMed] [Google Scholar]
- 20.Raj A, Reed E, Welles SL, et al. Intimate partner violence perpetration, risky sexual behavior, and STI/HIV diagnosis among heterosexual African American men. Am J Mens Health. 2008;2:291–5. doi: 10.1177/1557988308320269. [DOI] [PubMed] [Google Scholar]
- 21.Babor TF, Higgins-Biddle JC, Saunders JB, et al. AUDIT: the alcohol use disorders identification test guidelines for use in primary care. World Health Organization; Geneva: Switzerland: 2001. [Google Scholar]
- 22.Knight K, Simpson DD, Hiller ML, et al. Screening and referral for substance-abuse treatment in the criminal justice system. Treatment of drug offenders: Policies and issues. 2002:259–72. [Google Scholar]
- 23.Whetten K, Leserman J, Lowe K, et al. Prevalence of childhood sexual abuse and physical trauma in an HIV-positive sample from the deep south. Am J Public Health. 2006;96:1028–30. doi: 10.2105/AJPH.2005.063263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kalichman SC, Sikkema KJ, DiFonzo K, et al. Emotional adjustment in survivors of sexual assault living with HIV-AIDS. J Trauma Stress. 2002;15:289–96. doi: 10.1023/A:1016247727498. [DOI] [PubMed] [Google Scholar]
- 25.Pantalone DW, Rood BA, Morris BW, et al. A systematic review of the frequency and correlates of partner abuse in HIV-infected women and men who partner with men. JANAC: Journal of the Association of Nurses in AIDS Care. 2014;25:S15–35. doi: 10.1016/j.jana.2013.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Clements-Nolle K, Marx R, Guzman R, et al. HIV prevalence, risk behaviors, health care use, and mental health status of transgender persons: implications for public health intervention. Am J Public Health. 2001;91:915–21. doi: 10.2105/ajph.91.6.915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Arnsten JH, Demas PA, Grant RW, et al. Impact of Active Drug Use on Antiretroviral Therapy Adherence and Viral Suppression in HIV-infected Drug Users. Journal of general internal medicine. 2002;17:377–81. doi: 10.1046/j.1525-1497.2002.10644.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Malta M, Strathdee SA, Magnanini MM, et al. Adherence to antiretroviral therapy for human immunodeficiency virus/acquired immune deficiency syndrome among drug users: a systematic review. Addiction. 2008;103:1242–57. doi: 10.1111/j.1360-0443.2008.02269.x. [DOI] [PubMed] [Google Scholar]
- 29.U.S. Departments of Justice Division of Civil Rights. U.S. Departments of Justice and Education Release Joint Guideance to Help Schools Ensure the Rights of Transgender Students. 2016. [Google Scholar]
- 30.Eilperin J, Brown E. The Washington Post. 2016. Obama administraton directs schools to accomodate transgender students. Politics. [Google Scholar]
- 31.Somashekhar S, Brown E, Balingit M. The Washington Post. 2017. Trump administration rolls back protections for transgender students. Educaiton. [Google Scholar]
- 32.Sausa LA, Keatley J, Operario D. Perceived risks and benefits of sex work among transgender women of color in San Francisco. Arch Sex Behav. 2007;36:768–77. doi: 10.1007/s10508-007-9210-3. [DOI] [PubMed] [Google Scholar]
- 33.Sevelius JM. Gender affirmation: A framework for conceptualizing risk behavior among transgender women of color. Sex roles. 2013;68:675–89. doi: 10.1007/s11199-012-0216-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Winter S, Settle E, Wylie K, et al. Synergies in health and human rights: a call to action to improve transgender health. The Lancet. 2016;388:318–21. doi: 10.1016/S0140-6736(16)30653-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Grant JM, Mottet L, Tanis JE, et al. Injustice at Every Turn: A Report of the National Transgender Discrimination Survey. National Center for Transgender Equality; 2011. [Google Scholar]
- 36.Maher A, Bower K, Fitzgerald ST. White House Executive Order Protects Transgender Workers in the Federal Government. Workplace health & safety. 2014:62. doi: 10.3928/21650799-20141118-04. [DOI] [PubMed] [Google Scholar]
- 37.Rosenberg M. The New York Times. Jun 30, 2016. Transgender people will be allowed to serve openly in the minitary. [Google Scholar]
- 38.American Civil Liberties Union (ACLU) LGBT Rights: What’s at stake. 2016 Available at: https://www.aclu.org/issues/lgbt-rights.
- 39.Truman JL, Langton L. Criminal Victimizaiton, 2014. U S Department of Justice Office of Justice Programs Bureau of Justice Statistics. 2015:1–20. NCJ 248973. [Google Scholar]
- 40.Wolitzky-Taylor KB, Resnick HS, McCauley JL, et al. Is reporting of rape on the rise? A comparison of women with reported versus unreported rape experiences in the National Women’s Study-Replication. J Interpers Violence. 2011;26:807–32. doi: 10.1177/0886260510365869. [DOI] [PubMed] [Google Scholar]
- 41.Kjellsson G, Clarke P, Gerdtham U. Forgetting to remember or remembering to forget: a study of the recall period length in health care survey questions. J Health Econ. 2014;35:34–46. doi: 10.1016/j.jhealeco.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 42.U.S. Office of National AIDS Policy. National HIV/AIDS Strategy for the United States: Updated through 2020. 2015. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.