Abstract
Objective
Given the importance of developmental transitions on young adults’ lives and the high rates of mental health issues among U.S. college students, first-year college students can be particularly vulnerable to stress and adversity. This pilot study evaluated the effectiveness and feasibility of mindfulness training aiming to promote first-year college students’ health and wellbeing.
Participants
109 freshmen were recruited from residential halls (50% Caucasian, 66% female). Data collection was completed in November 2014.
Methods
A randomized control trial was conducted utilizing the Learning to BREATHE (L2B) program, a universal mindfulness program adapted to match the developmental tasks of college transition.
Results
Participation in the pilot intervention was associated with significant increase in students’ life satisfaction, and significant decrease in depression and anxiety. Marginally significant decrease was found for sleep issues and alcohol consequences.
Conclusions
Mindfulness-based programs may be an effective strategy to enhance a healthy transition into college.
Keywords: Alcohol, mental health, mindfulness interventions, sleep, stress, transition to college
Introduction
College education aims to strengthen young people’s intellectual abilities and prepare them for productive and successful adulthood, however students’ high rates of mental health concerns,1 sleep issues,2 and excessive drinking3 undermine the original purpose of college. In particular, the developmental transition of entering college warrants greater understanding since it is characterized by a radical shift in personal responsibilities, a sudden drop in institutional supports, and an abrupt change of social environments.4–6 In comparison with other years, freshmen endorse higher levels of ongoing and chronic stress7,8 which provides fertile grounds for poor coping strategies, unhealthy relationships, and deteriorating academics.6 Given the complexity of challenges associated with entering college, effective institutional structures need to be developed to facilitate a healthy and integrated developmental transition to young adulthood.6,9,10
The development of stress-related difficulties and maladaptive coping is of great concern because it further perpetuates distress and mental health problems. A critical issue is the initiation and consequences of frequent binge drinking during the freshman year.11 Alcohol consequences, which are not solely a result of alcohol consumption but rather an additional construct associated with students’ willingness to experience such consequences, augment the risk for long-term negative outcomes.12 Furthermore, stress and alcohol use are closely linked to poor sleeping habits which further impacts students’ academic success and overall wellbeing.13
To attend to the current issues in the educational system, college education needs to broaden its reach and foster the “development of the ‘whole person’” 14(p4) which includes the development of socioemotional competencies as well as academic skills. There is a growing interest in using mindfulness practices to promote college students’ personal growth and wellbeing by cultivating awareness and insight. Mindfulness can be conceptualized as a practice of accepting and non-judgmental attitude to the present moment thoughts and feelings15 which establishes a groundwork for intrapersonal and interpersonal awareness. Specifically, by cultivating non-judgmental attention and caring attitude toward body sensations, thoughts, and emotions, students may learn effective stress management techniques, and emotion regulation skills. Furthermore, students may become better equipped to make healthier choices, develop healthy relationships, and be resilient to face challenges associated with the transition process.14
The burgeoning literature on mindfulness interventions in the college population has demonstrated a wide array of benefits including stress reduction,16,17 greater emotional wellbeing,18,19 and improved interpersonal relationships,20,21 as well as health-related behaviors, including the promotion of better sleep.22 A recent review of universal prevention programs for higher education students concluded that skills-oriented programs, in particular mindfulness and cognitive-behavioral strategies, were the most effective.23 The same was found for stress-targeted interventions for college students where the cognitive/behavioral/mindfulness-based programs consistently showed a positive impact on students’ psychosocial wellbeing.24
Despite the accumulating evidence, there is a lack of research on mindfulness-based trainings targeted to promote the first-year college students’ experiences. To date, there are two published studies that have implemented mindfulness-based programs during the first year of college. A quasi-experimental study of 51 students who attended first-year wellness seminar found no group differences in psychosocial adjustment and stress management.23 Only the post-test data of “self-perceived improvements” were significantly higher in the intervention group. Another quasi-experimental study of 56 students found post-test significant group differences in students’ social-emotional adjustment and stress levels in salivary cortisol.25 However, the study lacked pre-test data, warranting caution in results interpretation. At present, there continues to be a need for high-quality evidence utilizing experimental designs to evaluate the effects of incorporating developmentally tailored mindfulness programs into higher education.14
The current pilot randomized controlled trial was conducted to evaluate the efficacy and feasibility of an 8-session mindfulness training aiming to promote first-year college students’ health and wellbeing. The pilot study utilized an evidence-based, universal mindfulness program Learning to BREATHE (L2B) that has been shown to improve adolescents’ emotion regulation skills and self-perceived sense of well-being.26–28 The intention was to use a program originally designed for youth in terms of the language, expectations, and skills development that could be further adapted to the specific needs of first-year college students. The aims of the L2B program are highly relevant to the developmental tasks during the transition to college: learning stress management skills, building the capacity for emotional regulation, strengthening the ability to focus and deliver quality performance, and establishing meaningful social relationships 29,30 We hypothesized that at the end of the intervention students who participate in the L2B program, in comparison to the wait-list control group, would demonstrate better outcomes in the areas of mental health and wellbeing (depression, anxiety, life satisfaction); intrapersonal awareness (mindfulness, self-compassion); interpersonal awareness (social connectedness, compassion for others); and health behaviors (sleep, alcohol use).
Methods
Participants
Participants were 109 first-year undergraduate students recruited from a large, public university in Pennsylvania. Recruitment commenced a few days prior to, and in the first 3 weeks of the Fall 2015 academic semester. In collaboration with Residential Life Services and the Honor’s College at the institution, potential participants were recruited through recruitment e-mails offering an opportunity to participate in a stress-management mindfulness program. Furthermore, flyers were posted at commonly visited locations and information booths were held at freshmen involvement fair.
Students were considered to be eligible for the study if they were first-year students residing in on-campus residence halls, and at least 18 years of age. The participants were almost all 18 years of age (M = 18.2, SD = .4, range = 18–19) and the majority of the sample were female (66%, 72 females, 37 males). The sample was ethnically diverse with half of the sample identifying as Caucasian (50%), Asian (26%), African American (5%), Hispanic (8%), and mixed (10%). International students comprised 16% of the sample (21 international, 88 domestic). Only 14% of the sample reported attending counseling services or therapy in the previous 6 months. Twenty-two percent reported having some experience with mindfulness or meditation; of those, the majority reported practicing less than once a month.
Procedure
The flow of participants’ enrollment, randomization, and analysis is shown in Figure 1. Students were recruited via emails and flyers and emailed initial screening for eligibility. Eligible students were invited to an in-person informed consent meeting (n = 144). The students who did not show up for consent procedures (n = 35) were dropped and we did not have any further communication with them. Students who completed the informed consent were e-mailed a secure link to access a baseline questionnaire (September 2014). Since we had a predominantly female sample, the sample was stratified by gender and each group was randomized separately (using the https://www.randomizer.org/) to assure balanced number of males and females in the intervention and control group. Participants were randomized to the intervention group (n = 55, n of females = 35, Fall 2014) or to a wait-list control group (n = 54, n of females = 37, Spring 2015) and informed about their assignment by e-mail. A post-test survey was e-mailed to all participants when the intervention was completed (November 2014). Surveys were delivered using the Qualtrics program. Furthermore, half of the students from the intervention and control group were randomly assigned to complete ecological momentary assessments31 through smartphones. These data are not included in this article and will be reported elsewhere. Small financial compensation was provided for completion of the surveys. To increase responsiveness, payment increased from pre-test ($10) to post-test ($15) and was delivered after the post-test assessment (November 2014). All procedures were approved by the university Institutional Review Board.
Figure 1.
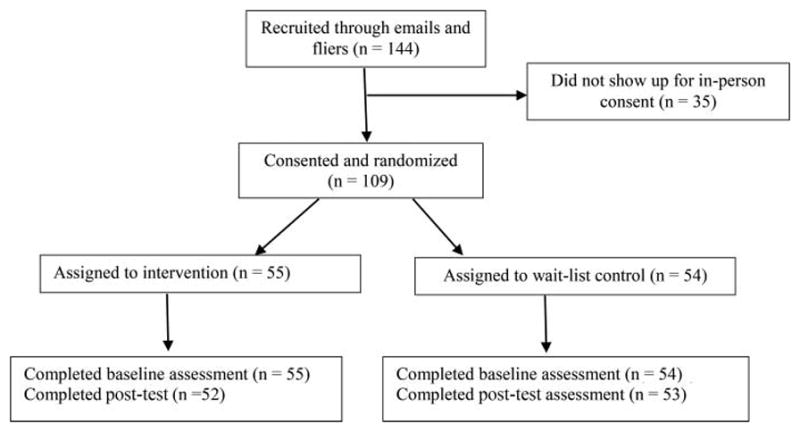
Flow diagram of participants’ enrollment, randomization, and analysis.
Intervention
In collaboration with the L2B program developer (Dr. Broderick), two trained facilitators adapted the program to target the developmental challenges specific to first-year college students. After every session, facilitators completed a fidelity log focused on delivering all content components. The program was delivered with 99% fidelity. To maximize implementation quality all lessons were videotaped and reviewed by the program developer and two additional fidelity coders who provided weekly feedback about program implementation.
Participants assigned to receive the L2B program in the fall semester were asked to attend a total of 8 sessions over 6 weeks (2 sessions per week for the first 2 weeks and 1 session for each of the remaining 4 weeks). Sessions were held in the evening in the freshman residential halls, with each session lasting approximately 80 minutes. The groups consisted of 20–25 students, with one lead and one assistant facilitator.
The L2B program is structured to gradually cultivate inner strength and empowerment throughout the eight sessions, with core themes associated with each session that are developed around the BREATHE acronym (for details, see27). Goals of the program include enhancing students’ emotion regulation skills, introducing simple mindfulness techniques so that students may better manage stressful situations, and facilitating the learning process in a supportive, group environment. To facilitate outside of classroom practice and promote program retention, students were provided with home practice cards (a simple practice associated with the core theme), stickers that reminded them to use mindfulness techniques in response to stress (eg, three mindful breaths), as well as home worksheets with additional mindfulness suggestions. Students were advised to place the handout materials in a visible place that would remind them of their participation in the L2B program and their intention to practice mindfulness skills in daily life. Further, students were provided with a link to access an audio recording of guided meditations (eg, body scan, loving-kindness practice) led by the lead facilitators.
Measures
Depression
The Primary Health Questionnaire (PHQ)32 is an 8-item screening instrument which assesses depressive symptoms (eg, feeling down, depressed or hopeless) over the previous 2 weeks. The PHQ has demonstrated validity and excellent internal consistency in research on college populations (alpha = .90).33 In the present sample, Cronbach’s alpha was .81 and .87 for the pre- and post-test scores, respectively.
Anxiety
The 7-item Generalized Anxiety Disorder Scale (GAD)34 was used to assess frequency of experiencing anxiety-related symptoms in the previous 2 weeks. The GAD has demonstrated internal consistency (alpha = .91) and concurrent validity in college populations.33 Observed reliabilities for the GAD in the present sample was .87 and .90 for the pre- and post-test scores, respectively.
Satisfaction with life
The satisfaction with life scale (SWL)35 is a brief, 5-item questionnaire which assesses one’s overall cognitive judgment of their life, with a Likert scale from 1 (strongly disagree) to 7 (strongly agree). Sample items include “If I could do my life over, I would change almost nothing” and “I am satisfied with my life.” Cronbach’s alpha for the SWLS was .88 for the SWL scores at both time points.
Mindfulness
The mindfulness attention awareness scale (MAAS)36 is a 12-item instrument which captures mindfulness by assessing the frequency of the opposing construct; mindlessness (eg, “It seems I am running on automatic without much awareness of what I am doing”). Participants are asked to rate the extent to which they function mindlessly in daily life, with a Likert scale from 1 (almost never) to 6 (almost always). Eight items with the highest factor loadings were selected for the present study. Observed reliabilities for the MAAS in this sample were .88 and .90, respectively.
Self-compassion
The Self-Compassion Scale (SCS)37 is a 12-item instrument which assesses one’s tendency to address failure and painful emotions with a sense of warmth, kindness, and understanding. Responses are provided on a 5-point Likert scale from 1 (almost never) to 5 (almost always). Cronbach’s alpha was .86 across the two time points.
Social connectedness
The Social Connectedness Scale (SCC-R)38 was used to assess individuals’ interpersonal closeness in the social context. From the full measure, 7 items of highest factor loadings were used on a Likert-type scale from 1 (strongly disagree) to 6 (strongly agree), with sample items such as, “Even around people I know, I don’t feel that I really belong.” The observed reliabilities for the SCC-R in the current sample were .89 for both time points.
Compassion
The Compassion Scale (CS)39 is a 24-item instrument which captures the degree of awareness, sympathy, and concern for others’ suffering. A Likert scale is used from 1 (almost never) to 5 (almost always). The observed reliabilities were .90 and .91, respectively.
Sleep
Subjective sleep quality was assessed using the Pittsburgh Sleep Quality Index (PSQI).40 The PSQI is a validated instrument which assessed 7 aspects of sleep: sleep latency, sleep duration, sleep efficiency, sleep disturbances, sleep medication use, daytime dysfunction, and overall sleep quality over the previous month. These component scores (ranging from 0 to 3, with 3 demonstrating greater dysfunction) are summed to yield a total sleep score ranging from 0 to 21, with higher total scores indicating poorer sleep quality.
Alcohol use
To obtain an assessment of peak drinking, participants reported the number of drinks they consumed during an occasion on which they drank the most during the past 30 days.41 Frequency of getting drunk was assessed with a single item that asked the number of times the respondent got drunk or very high from alcohol use during the past 30 days.
Alcohol consequences
Alcohol-related consequences were obtained using the Young Adult Alcohol Problems Screening Test (YAAPST).42 Students were asked to indicate the frequency of occurrence for 10 consequences from the YAAPST (eg, hangover, blacking out).
The L2B acceptability questionnaire (LAQ)43
To evaluate acceptability of the program, students in the intervention group answered 10 questions about their overall experience, practices they learned, and confidence in using mindful skills in the future. The survey included a mix of open-ended, 5-point Likert scale, 0–100 rating, and Yes/No questions.
Data analysis
Prior to data analyses, data were inspected for normality and outliers. To reduce skew and kurtosis found in alcohol measures, a square root transformation44,45 was administered to all three assessments of alcohol use and the transformed variables were used in the data analysis. Independent t-tests were computed to assess statistical differences on any baseline differences between the two groups. The two randomly assigned groups did not differ significantly on any baseline psychosocial characteristics. However, in the intervention group, there were significantly higher number of students who attended therapy in the last 6 months (t = 2.73, p < .05). Furthermore, males demonstrated higher mindfulness scores on the MAAS in comparison to females (t = 3.06, p < .05), and males reported lower anxiety in comparison to females on the GAD (t = 2.20, p < .05). To examine intervention effects data were analyzed using Analysis of Covariance (ANCOVA). Separate ANCOVAs were run for each outcome measure using gender, pre-test scores, and therapy-attendance as covariates and the group assignment as predictor. Cohen’s d for the intervention group vs. wait-list control group was computed for each outcome measure.46 All statistical analyses were performed with SPSS Version 21.0 with the alpha level used to determine two-tailed significance p < .05. Given the small sample size, reduced alpha = .10 was considered to indicate noteworthy marginal significance. The analysis was conducted as an intent-to-treat, including all randomized participants. At post-test, there was only 6% of missing data and therefore listwise deletion was utilized to handle missing data.
Results
The attendance of the L2B program was high with over 60% of participants attending at least 6 out of 8 sessions. On average, students attended 5.21 sessions (SD = 2.72). A small portion of students (14%) did not attend any session due to scheduling conflict or personal reasons.
The pre- and post-test unadjusted means are displayed in Table 1 and the adjusted post-test means, ANCOVA results, and effects sizes are displayed in Table 2. In the domain of mental health and wellbeing, the intervention participants reported significantly lower levels of depression (F (1, 98) = 6.53, p < .05, d = −.34), significantly lower levels of anxiety (F(1, 98) = 4.92, p < .05, d = −.48), and significantly higher levels of life satisfaction (F(1, 97) = 10.59, p < .05, d = .41) compared to the control participants. The indicators of intrapersonal awareness (mindfulness, self-compassion) and interpersonal awareness (social connectedness, compassion) were not significantly different between the groups at the post-test.
Table 1.
Unadjusted pre and post-test mean comparison for all outcome variables.
| Outcome variable | Intervention | Control | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Pre | Post | Pre | Post | |||||
|
|
|
|
|
|||||
| M | (SD) | M | (SD) | M | (SD) | M | (SD) | |
| Depression | 7.36 | (4.26) | 6.06 | (5.00) | 6.31 | (4.78) | 7.33 | (5.36) |
| Anxiety | 7.80 | (4.82) | 5.94 | (4.38) | 6.41 | (5.24) | 6.71 | (4.64) |
| Satisfaction with life | 21.76 | (7.52) | 23.43 | (7.11) | 22.67 | (6.95) | 21.27 | (7.65) |
| Mindfulness | 4.03 | (1.02) | 4.18 | (1.03) | 4.15 | (1.00) | 4.36 | (1.04) |
| Self-compassion | 2.77 | (0.72) | 3.02 | (0.80) | 2.98 | (0.74) | 3.10 | (0.75) |
| Social connectedness | 4.20 | (1.07) | 4.09 | (1.14) | 4.29 | (1.17) | 4.29 | (1.27) |
| Compassion | 3.80 | (0.39) | 3.80 | (0.46) | 3.78 | (0.44) | 3.76 | (0.47) |
| Sleep issues | 6.18 | (3.22) | 5.58 | (2.66) | 5.02 | (2.53) | 6.02 | (3.41) |
| Alcohol peak | 3.93 | (8.64) | 2.22 | (3.38) | 4.33 | (5.43) | 4.75 | (8.17) |
| Frequency drunk | 0.64 | (1.09) | 0.51 | (0.90) | 1.06 | (1.31) | 0.96 | (1.31) |
| Alcohol consequences | 1.87 | (3.06) | 1.57 | (3.38) | 1.91 | (2.62) | 2.39 | (3.10) |
Note. Summary statistics of alcohol-related variables represent data before transformations. N of participants = 109, intervention = 55, control = 54.
Table 2.
Intervention effects on all outcome variables, adjusted post-test means, ANCOVA results, and effects sizes.
| Outcome variable | Adjusted post-test mean and standard error | F | p | d | |||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Intervention M | (SE) | Control M | (SE) | ||||
| Depression | 5.96 | 0.55 | 7.98 | 0.55 | 6.53 | 0.012 | −0.34 |
| Anxiety | 5.43 | 0.59 | 7.23 | 0.56 | 4.92 | 0.029 | −0.48 |
| Satisfaction with life | 23.80 | 0.62 | 20.91 | 0.62 | 10.59 | 0.002 | 0.41 |
| Mindfulness | 4.22 | 0.11 | 4.31 | 0.11 | 0.29 | 0.595 | −0.07 |
| Self-compassion | 3.11 | 0.07 | 3.00 | 0.08 | 1.17 | 0.282 | 0.17 |
| Social connectedness | 4.16 | 0.12 | 4.21 | 0.12 | 0.08 | 0.771 | −0.10 |
| Compassion | 3.81 | 0.05 | 3.75 | 0.05 | 0.98 | 0.325 | 0.05 |
| Sleep issues | 5.33 | 0.39 | 6.36 | 0.40 | 3.35 | 0.070 | −0.53 |
| Alcohol peak | 0.95 | 0.18 | 1.35 | 0.18 | 2.32 | 0.131 | −0.37 |
| Frequency drunk | 0.49 | 0.08 | 0.57 | 0.07 | 0.49 | 0.485 | −0.03 |
| Alcohol consequences | 0.70 | 0.12 | 1.04 | 0.12 | 3.72 | 0.057 | −0.24 |
Note. Significance statistic was calculated using ANCOVA with treatment group as a predictor and pretest scores, gender, and therapy as covariates. Cohen’s d was calculated by using raw scores of group difference means and pooled standard deviations. N of participants = 109, intervention = 55, control = 54.
In the area of health behaviors, the intervention students reported marginally significant lower levels of sleep issues (F (1, 97) = 3.35, p < .1, d = −.53) than did the control participants. There were no significant group differences in the frequency of drinking. Alcohol peak, calculated as a number of drinks at a particular occasion, decreased in the expected direction (d = −.37), however the result was not significant. Furthermore, there was a marginally significant group difference in the alcohol consequences where the intervention group reported lower count of alcohol-related consequences in comparison with the control group (F (1, 97) = 3.72, p < .1, d = −.24).
In terms of the program evaluation, students reported learning a wide variety of new practices and ideas as a result of the program. The three most effective in-class practices were 3 mindful breaths (82%), breath awareness (50%), and mindfulness of emotions (27%). Almost all (98%) students would recommend attending the program to a friend or classmate. Most students found the program useful for (1) stress reduction and stress management (95%), (2) self-regulation skills (52%), and (3) leading a healthier lifestyle (48%). Finally, on a scale of 0–100, students reported mean level of 74.91 (SD = 21.78) confidence in using the skills they learned in future stressful situations. Separate qualitative analysis of the open-ended questions is in preparation for publication.
Comment
Given the national reports of stress-related difficulties and maladaptive behaviors in college students,1 this pilot randomized controlled study aimed to evaluate the efficacy and feasibility of an evidence-based developmentally adapted mindfulness L2B program with first-year college students. We found that attending a mindfulness program in the first semester of college led to significant improvements in students’ life satisfaction, depression, anxiety, sleep issues, and alcohol consequences in comparison with the control group. Indicators of intra- and interpersonal awareness were not impacted by the intervention. In terms of program evaluation, students rated the program highly and would recommend attending the program to their peers.
During the first year of college in particular, students need to develop skills that would reinforce their ability to manage stress-related adversity. It has been documented that the first year of college can be associated with worsened psychological and physical health.47 We found similar phenomena in the control group as students reported a decline in life satisfaction and mental health, and increase in sleep issues, alcohol use, and consequences across the first semester. However, our pilot intervention findings suggest that through mindfulness training this pattern can be prevented and students’ wellbeing can even improve in the first semester.
Mindfulness skills can provide students with a toolset of healthy ways to approach discomfort and challenging experiences associated with entering college. Rather than emotionally reacting, students learn how to regulate their emotions which leads to a sense of empowerment, a positive loop that helps students make healthier decisions.14 The intervention effects on depression, anxiety, and life satisfaction are particularly important as they play a foundational role in predicting students’ success and adjustment,47 which in turn leads to better long-term adult outcomes.10
Mindfulness trainings also tend to improve awareness of one’s self and others, providing foundation for more compassionate behaviors.20 In our pilot study, we did not find significant results in either the domain of intrapersonal and interpersonal awareness. Previous studies have discussed the difficulties with measuring mindfulness and compassion because of numerous conceptual and methodological ambiguities.48,49 Also, it may be the case that involvement in mindfulness practices can lead one to become initially aware of one’s mindlessness in everyday life. In fact, this pilot intervention program had students differentiate between mindful and mindless activities and thus the intervention group was made more aware of when they were not mindful. More intensive assessments such as ecological momentary assessments that are collected closer to the activation time31 may increase the accuracy of reporting and reveal the underlying dynamics in these outcomes.
Health behaviors in college, such as sleep and alcohol use, have been a target of interventions with moderate success.50,51 College students especially struggle with transitioning into sleep due to stress-related rumination, tension, and hyperarousal.2 However, in mindfulness studies, participants often report having easier time with sleeping because they are able to clear their minds by focusing on breathing and relaxing their bodies.52 Mindfulness practices, such as body scan when students learn to bring relaxed sense of awareness to different body parts, may more effectively prepare students for a restful sleep. Since quality sleep is associated with better academic outcomes,53 it represents an important outcome in college intervention research, warranting continued investigation of how sleep is improved through mindfulness practice and its consequences.
In terms of alcohol-related outcomes, this is the first intervention that has reported effects on alcohol consequences in a typical college freshman population. Although we did not find significant effects on alcohol use, there was an overall decrease in alcohol use in the intervention group and an increase in the control group. A recent review of alcohol interventions with freshmen found on average weighted mean effect size of .11–.19 for intervention-inactive control studies51 while we found non-significant d = −.37 for alcohol use and marginally significant d = −.24 for alcohol consequences suggesting that mindfulness practices may positively affect students’ decision-making related to substances. Since alcohol consequences are related to students’ willingness to experience the negatives associated with drinking,3 mindfulness skills may provide students with both the awareness of the negative consequences as well as the tools to make healthier decisions.
Finally, the program evaluation results showed that students found their participation in the program beneficial and meaningful. The high attendance of the program suggests that when students are given an opportunity to learn effective stress management skills they seek it out. In terms of the program format, students also indicated that they would be interested in taking a course like this for credit. In general, universal prevention programs for higher education students are recommended to be presented as routinely offered classes together with increasing campus services aiming at students’ psychosocial wellbeing.54 Our findings suggest that the adapted L2B program which is designed as a universal prevention program could be offered as a part of a freshmen orientation class, as a residential hall program offering with additional incentives, or freestanding 6-week class that is offered only to freshman. Furthermore, we would recommend the possibility that L2B could be added as a prevention effort led by the health and counseling centers to decrease the occurrence of stress-related disorders.
Limitations
Several limitations need to be noted. The small sample was recruited from a large public university in the United States, and thus it is not clear whether these results will generalize to other types of colleges. Liberal arts colleges, community colleges, or universities in other countries represent distinct cultural contexts with different base rates of mental health concerns and stressor and these setting also may provide different types of supports to their students during the first year of college. Furthermore, the lack of an active control group prevents us from isolating the specific effects of the program versus the general benefits of attending a regular group outside of classroom. Self-report measurement may increase social desirability bias and future studies would benefit from including physiological measurement, time-intensive assessments, and second-person objective perspectives on students’ lived experiences, such as assessments from family members, friends, or teachers. Students self-selected into the study, creating a potentially biased sample of students more motivated to improve their stress management and mindfulness skills than the general college population. Motivation may be a critical aspect of perceived changes and more research is needed in this area. Another limitation was that the mindfulness program was not incorporated in their course offering, fully relying on students’ motivation to attend. This also represents strength of the study because students made time for the program, although it was not required. Finally, the fact that findings are only at post-test does not offer any evidence about the retention of effects and the trajectories of mental health and wellbeing across the whole first year in college. These initial positive findings lead to the need to collect data at several follow-up time points in order to assess if there are lasting effects. This is an area that has not received sufficient attention,49 especially in college populations.
Conclusions
The first year of college is a particularly fruitful developmental period when mindfulness-based intervention efforts may prevent a decline in mental health and promote students’ wellbeing and health behaviors. The entry to college as a transition into young adulthood may be one of the last institutional and educational windows of opportunity to change young people’s life course.55 Successfully moving through the transition of emerging adulthood has a determinant impact on adult success10 and as a result students’ wellbeing is an essential part of universities’ public agenda. There is a need for further research on the potential benefits of mindfulness programs in colleges that will include larger sample sizes, long-term follow-ups, and integration with academic material. Although there are some preliminary indications of the potential benefits of mindfulness to foster students’ adjustment into college, the evidence must be strengthened before universities are willing to adopt these programs on a wider scale.
Acknowledgments
Funding
This project was supported by grants from the National Center for Advancing Translational Sciences, Clinical and Translational Science Institute, UL1 TR000127 and TR002014, National Institute on Drug Abuse, T32 DA017629, Childhood Obesity Prevention Training Program, USDA 2011-67001-30117, and the Bennett Endowment Fund at Edna Bennett Pierce Prevention Research Center. The content does not necessarily represent the official views of the National Institute on Drug Abuse or the National Institutes of Health.
Footnotes
Conflict of interest disclosure
The authors have no conflicts of interest to report. The authors confirm that the research presented in this article met the ethical guidelines, including adherence to the legal requirements, of the United States and received approval from the Institutional Review Board of The Pennsylvania State University.
References
- 1.American College Health Association. The American College Health Association National College Health Assessment (ACHA-NCHA): Fall 2012 Reference Group Executive Summary. 2014 [Google Scholar]
- 2.Jensen D. Understanding sleep disorders in a college student population.pdf. J Coll Couns. 2003;6(1):25–34. [Google Scholar]
- 3.Mallett KA, Varvil-Weld L, Borsari B, Read JP, Neighbors C, White HR. An update of research examining college student alcohol-related consequences: new perspectives and implications for interventions. Alcohol Clin Exp Res. 2013;37(5):709–716. doi: 10.1111/acer.12031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Astin AW. Student involvement : a developmental theory for higher education. J Coll Stud Dev. 1999;40(5):518–529. [Google Scholar]
- 5.Evans N, Forney D, Guido F, Patton L, Renn K. Student Development in College: Theory, Research, and Practice. San Francisco: Jossey-Bass; 2009. [Google Scholar]
- 6.Schulenberg JE, Sameroff AJ, Cicchetti D. The transition to adulthood as a critical juncture in the course of psychopathology and mental health. Dev Psychopathol. 2004;16(4):799–806. doi: 10.1017/s0954579404040015. [DOI] [PubMed] [Google Scholar]
- 7.Towbes LC, Cohen LH. Chronic stress in the lives of college students: scale development and prospective prediction of distress. J Youth Adolesc. 1996;25(2):199–217. [Google Scholar]
- 8.Misra R, McKean M. College students’ academic stress and its relation to their anxiety, time management, and leisure satisfaction. Am J Health Stud. 2000;16(1):41–51. [Google Scholar]
- 9.Hurrelmann K. Health promotion for adolescents: preventive and corrective strategies against problem behavior. J Adolesc. 1990;13(3):231–250. doi: 10.1016/0140-1971(90)90016-z. [DOI] [PubMed] [Google Scholar]
- 10.Maggs JL, Jager J, Patrick ME, Schulenberg JE. Social role patterning in early adulthood in the USA: adolescent predictors and concurrent wellbeing across four distinct configurations. Longit Life Course Stud. 2012;3(2):190–210. doi: 10.14301/llcs.v3i2.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Turrisi R, Mallett KA, Mastroleo NR, Larimer ME. Heavy drinking in college students: who is at risk and what is being done about it? J Gen Psychol. 2006;133(4):401–420. doi: 10.3200/GENP.133.4.401-420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mallett KA, Varvil-Weld L, Turrisi R, Read A. An examination of college students’ willingness to experience consequences as a unique predictor of alcohol problems. Psychol Addict Behavaviors. 2011;25(1):41–47. doi: 10.1037/a0021494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Singleton RA, Wolfson AR. Alcohol consumption, sleep, and academic performance among college students. J Stud Alcohol Drugs. 2009;70(3):355–363. doi: 10.15288/jsad.2009.70.355. [DOI] [PubMed] [Google Scholar]
- 14.Shapiro SL, Brown KW, Astin JA. Toward the integration of meditation into higher education: a review of research evidence. Teach Coll Rec. 2011;113(3):493–528. [Google Scholar]
- 15.Kabat-Zinn J. Mindfulness meditation: What it is, what it isn’t, and its role in health care and medicine. In: Haruki, Ishii Y, Suzuki M, editors. Comparative and Psychological Study on Meditation. Eburon; Netherlands: 1996. pp. 161–170. [Google Scholar]
- 16.Astin J. Stress reduction through mindfulness meditation. Psychother Psychosom. 1997;66(2):97–106. doi: 10.1159/000289116. [DOI] [PubMed] [Google Scholar]
- 17.Shapiro SL, Oman D, Thoresen CE, Plante TG, Flinders T. Cultivating mindfulness: effects on well-being. J Clin Psychol. 2008;64(7):840–862. doi: 10.1002/jclp.20491. [DOI] [PubMed] [Google Scholar]
- 18.Jain S, Shapiro SL, Swanick S, et al. A randomized controlled trial of mindfulness meditation versus relaxation training: effects on distress, positive states of mind, rumination, and distraction. Ann Behav Med. 2007;33(1):11–21. doi: 10.1207/s15324796abm3301_2. [DOI] [PubMed] [Google Scholar]
- 19.Rosenzweig S, Reibel DK, Greeson JM, Brainard GC. Mindfulness-based stress reduction lowers psychological distress in medical students. Teach Learn Med. 2003;15(2):88–92. doi: 10.1207/S15328015TLM1502_03. [DOI] [PubMed] [Google Scholar]
- 20.Cohen JS, Miller LJ. Interpersonal mindfulness training for well-being: a pilot study with psychology graduate students. Teach Coll Rec. 2009;111(12):2760–2774. [Google Scholar]
- 21.Shapiro SL, Schwartz GE, Bonner G. Effects of mindfulness-based stress reduction on medical and premedical students – shapiro schwartz bonner 1998.doc.pdf. 1998;21(6):581–599. doi: 10.1023/a:1018700829825. [DOI] [PubMed] [Google Scholar]
- 22.Greeson JM, Juberg MK, Maytan M, James K, Rogers H. A randomized controlled trial of koru: a mindfulness program for college students and other emerging adults. J Am Coll Heal. 2014;62(4):222–233. doi: 10.1080/07448481.2014.887571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Conley CS, Travers LV, Bryant FB. Promoting psychosocial adjustment and stress management in first-year college students: the benefits of engagement in a psychosocial wellness seminar. J Am Coll Heal. 2013;61(2):75–86. doi: 10.1080/07448481.2012.754757. [DOI] [PubMed] [Google Scholar]
- 24.Regehr C, Glancy D, Pitts A. Interventions to reduce stress in university students: a review and meta-analysis. J Affect Disord. 2013;148(1):1–11. doi: 10.1016/j.jad.2012.11.026. [DOI] [PubMed] [Google Scholar]
- 25.Ramler TR, Tennison LR, Lynch J, Murphy P. Mindfulness and the college transition: the efficacy of an adapted mindfulness-based stress reduction intervention in fostering adjustment among first-year students. Mindfullness. 2016;7(1):179–188. [Google Scholar]
- 26.Broderick PC. Learning to Breathe: A Mindfulness Curriculum for Adolescents to Cultivate Emotion Regulation, Attention, and Performance. Oakland, CA: New Harbinger; 2013. [Google Scholar]
- 27.Broderick PC, Metz S. Learning to BREATHE: a pilot trial of a mindfulness curriculum for adolescents. Adv Sch Ment Health Promot. 2009;2(1):35–46. [Google Scholar]
- 28.Metz SM, Frank JL, Reibel D, Cantrell T, Sanders R, Broderick PC. The effectiveness of the learning to BREATHE program on adolescent emotion regulation. Res Hum Dev. 2013;10(3):252–272. [Google Scholar]
- 29.Chickering AW, Havighurst RJ. In: The Life Cycle. Chickering AW, et al., editors. San Francisco: Jossey-Bass; 1981. [Google Scholar]
- 30.McCoy V. Adult life cycle change. Lifelong Learn Adult Years. 1977 [Google Scholar]
- 31.Moskowitz DS, Young SN. Ecological momentary assessment: what it is and why it is a method of the future in clinical psychopharmacology. J Psychiatry Neurosci. 2006;31(1):13–20. [PMC free article] [PubMed] [Google Scholar]
- 32.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 33.Singh K, Brown RJ. Health-related Internet habits and health anxiety in university students. Anxiety Stress Coping. 2014;27(5):542–554. doi: 10.1080/10615806.2014.888061. [DOI] [PubMed] [Google Scholar]
- 34.Spitzer R, Kroenke K, Williams J, Lowe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. J Am Med Assoc. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 35.Diener E, Emmons R, Larsen J, Griffin S. The satisfaction with life scale. J Personal Assessmemt. 1985;49(1):71–75. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- 36.Brown K, Ryan R. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84(4):822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- 37.Neff K. The development and validation of a scale to measure self-compassion. Self Identity. 2003;2(3):223–250. [Google Scholar]
- 38.Lee R, Robbins S. Measuring belongingness: the social connectedness and the social assurance scales. J Couns Psychol. 1995;42(2):232–241. [Google Scholar]
- 39.Pommier EA. The compassion scale. Diss Abstr Int Sect A Humanit Soc Sci. 2011;72:1174. [Google Scholar]
- 40.Buysse D, Reynolds C, Monk T. The pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 41.Marlatt G, Baer J. Screening and brief intervention for high-risk college student drinkers: results from a 2-year follow-up assessment. J Consult Clin Psychol. 1998;66(4):604–615. doi: 10.1037//0022-006x.66.4.604. [DOI] [PubMed] [Google Scholar]
- 42.Hurlbut S, Sher K. Assessing alcohol problems in college students. J Am Coll Heal. 1992;41(2):49–58. doi: 10.1080/07448481.1992.10392818. [DOI] [PubMed] [Google Scholar]
- 43.Dvorakova K, Agrusti M, Broderick PC. The L2B acceptability questionnaire. Not Publ [Google Scholar]
- 44.Howell DC. Statistical Methods for Psychology. Belmont, CA: Thomson Wadsworth; 2007. [Google Scholar]
- 45.Tabachnick BG, Fidell LS. Using Multivariate Statistics. 5. Boston, MA: Allyn and Bacon; 2007. [Google Scholar]
- 46.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2. Vol. 2. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- 47.Pritchard ME, Wilson GS, Yamnitz B. What predicts adjustment among college students? A longitudinal panel study. J Am Coll Heal. 2007;56(1):15–21. doi: 10.3200/JACH.56.1.15-22. [DOI] [PubMed] [Google Scholar]
- 48.Grossman P. On measuring mindfulness in psychosomatic and psychological research. J Psychosom Res. 2008;64(4):405–408. doi: 10.1016/j.jpsychores.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 49.Davidson RJ, Kaszniak A. Conceptual and methodological issues in research on mindfulness and meditation. Am Psychol. 2015;70(7):581–592. doi: 10.1037/a0039512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Brown FC, Buboltz WC, Jr, Soper B. Development and evaluation of the Sleep. J Am Coll Heal. 2006;54(4):231–237. doi: 10.3200/JACH.54.4.231-237. [DOI] [PubMed] [Google Scholar]
- 51.Scott-Sheldon LAJ, Carey KB, Elliott JC, Garey L, Carey MP. Efficacy of alcohol interventions for first-year college students: a meta-analytic review of randomized controlled trials. J Consult Clin Psychol. 2014;82(2):177–188. doi: 10.1037/a0035192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Howell AJ, Digdon NL, Buro K. Mindfulness predicts sleep-related self-regulation and well-being. Pers Individ Dif. 2010;48(4):419–424. [Google Scholar]
- 53.Trockel MT, Barnes MD, Egget DL. Health-related variables and academic performance among first-year college students: implications for sleep and other behaviros. J Am Coll Heal. 2000;49(3):125–131. doi: 10.1080/07448480009596294. [DOI] [PubMed] [Google Scholar]
- 54.Conley CS, Durlak JA, Dickson DA. An evaluative review of outcome research on universal mental health promotion and prevention programs for higher education students. J Am Coll Heal. 2013;61(5):286–301. doi: 10.1080/07448481.2013.802237. [DOI] [PubMed] [Google Scholar]
- 55.Masten AS, Burt KB, Roisman GI, Obradović J, Long JD, Tellegen A. Resources and resilience in the transition to adulthood: continuity and change. Dev Psychopathol. 2004;16(4):1071–1094. doi: 10.1017/s0954579404040143. [DOI] [PubMed] [Google Scholar]


