Abstract
Background
This study extends research on receptivity to tobacco marketing over a key developmental period for cigarette smoking experimentation.
Purpose
Understand the effect of receptivity to tobacco marketing and exposure to friends who smoke on smoking experimentation.
Methods
Participants were 10- to 13-year-olds who had never tried cigarettes (n=878), interviewed six times at 8-month intervals.
Results
At baseline, 25% percent of the 10 and 11 year olds in the sample of never smokers were receptive to tobacco marketing, while less than 5% had friends who smoked. Having a friend who smoked at study baseline, and acquiring such friends for the first time during the study, were the strongest predictors of smoking experimentation. Initial receptivity to tobacco marketing increased the risk of smoking experimentation independently of having friends who smoke at baseline or acquiring friends who smoke throughout the study period.
Conclusions
The high level of receptivity observed even among 10 and 11 year olds and its robust relationship with cigarette smoking experimentation independent of the significant risk associated with having friends who smoke suggests that successful prevention of receptivity may require intervention at an early age.
Keywords: Receptivity to Tobacco Marketing, Tobacco Advertising, Smoking Experimentation, Parenting, Depression
Introduction
Receptivity to tobacco marketing and exposure to friends who smoke cigarettes are considered two of the strongest predictors of smoking experimentation in adolescents(1-2). Yet, the relative impact of marketing versus friendship on smoking uptake is unknown, as few longitudinal studies have included enough measures over time to isolate the developmental influences of each variable on cigarette smoking experimentation. In this paper, we investigate the relative roles of marketing and exposure to friends who smoke during the earliest portion of the smoking experimentation process, using a six-wave national longitudinal study in the United States.
The vast majority of studies of smoking experimentation in adolescence suggest that acquiring friends who smoke is commonly a precursor to adolescent experimentation with tobacco (2-6). Friends are in part a socializing influence promoting smoking, but can also serve as a social mechanism by which motivated adolescents obtain cigarettes to experiment (7-10). In regards to social influences, it is often assumed that friends influence smoking behavior through an observational learning process as described by the social cognitive theory (11,12). Other researchers believe that young adolescents can feel “pressured” to smoke when friends are smoking; however, the evidence for this hypothesis is weaker (13-15). The strongest support for the hypothesis that adolescents who are curious about experimenting with tobacco seek-out or “select” friendships with other adolescents who smoke comes from studies of young adolescents. For example, Distefan et al (2004) noted that even when very few young adolescents had friends who smoked, favorable cognitions about tobacco alone could identify future smokers (16). This suggests that cognitions about tobacco products may increase risk for experimentation and may precede the exposure to friends who smoke.
Early evidence that tobacco marketing influenced experimentation came from ecological studies noting that the Virginia Slims campaign selectively increased experimentation in adolescent girls in the US (17). As most marketing messages appeal to only a segment of the population (18), an index of receptivity to tobacco marketing was developed (19) using the “hierarchy of effects” framework from McGuire's theory of persuasive communications (20,21). This index characterizes degrees of receptivity: having a favorite cigarette advertisement indicates moderate receptivity, and willingness to wear a promotional item with a marketing image indicates high receptivity. This latter concept was supported in Tobacco Industry documents where a teen's willingness to wear a “Joe Camel” image was lauded as the ultimate evidence of a successful campaign (22). This receptivity index was shown to be a significant predictor of smoking experimentation in young adolescents (23) and later, a study of two separate cohorts showed that an adolescent who was receptive to cigarette marketing was 1.5 to 2 times more likely to become an adult smoker (24).
A number of other variables can influence smoking experimentation in adolescents, including living with a smoker, academic performance, single parent family status, parenting practices, and internalizing symptoms such as depression and anxiety (2). Parental smoking has been linked with experimentation and trajectories of smoking in some (25-28), but not all studies (29-31). Lower smoking experimentation has been associated with a responsive parent-teen bond (described as close and supportive) (32-35), and parental limit-setting of unsupervised time (25,36,37). Higher smoking experimentation rates have also been observed in single parent families.(38). A number of studies have identified older sibling smoking as a stronger influence on teen experimentation than parental smoking (39-41).
High school graduates are 2.6 times more likely to be smokers than college graduates, evidence of a strong and growing trend for higher smoking rates among adults with lower levels of education that was first identified in 1989 [41]. This trend was notable given that the vast majority of smokers initiate tobacco use before completing high school (2,42). Numerous studies have reported that middle and high school students with lower grades are more likely to be smokers (32,38,43-46). Intrapersonal vulnerabilities including general attitudes about school, such as low motivation for academic achievement (47-49) and indices of internalizing symptoms of mental health such as depression (50-52), are known to increase risk for smoking experimentation. Patten et al (2001)(53) noted that many adolescents had persistent depressive symptoms over a 4-year period and symptoms were associated with smoking experimentation, a finding that was replicated by Audrain-McGovern et al (2009) (54).
Improving our understanding of the factors that promote cigarette smoking experimentation is important to preventing smoking uptake. In this paper, we disaggregate the influences of receptivity to tobacco marketing and exposure to friends who smoke using data from a national six-wave longitudinal study. This study of families, drawn from a US national sample, was developed to investigate the role of parenting to prevent problem behaviors in the eldest child (55). We present initial levels of our two key variables: receptivity to tobacco marketing and exposure to friends who smoke, as well as trajectories throughout the study. We investigate predictors of both the initial level and the growth in exposure to friends who smoke and receptivity to tobacco marketing variables over time. We examine two primary aims. First, we hypothesized that both initial levels of receptivity and higher levels of receptivity over time will be related independently to both acquiring friends who smoke and to risk of smoking experimentation (Aim 1). We expect these effects to be present after adjusting for sociodemographic characteristics, parenting influences, and intrapersonal vulnerabilities. Second, we hypothesized that the risk for smoking experimentation associated with exposure to friends who smoke would in part be due to resulting increases in receptivity to tobacco marketing (Aim 2).
Methods
Study Participants
Participants were 10 to 13 years old at trial enrollment in 2003 for a study on parenting to prevent adolescent problem behaviors. As part of another national random-digit dial telephone screening study that over sampled for indivudals with Black racial backgrounds, we identified 3079 households with an oldest child (including only child) aged 9-13 years, and invited these families to participate in a study to prevent problem behaviors in teens. Over the next 14 months, 1036 (33.6% of identified households) families were randomized to an active telephone-based parenting intervention to prevent problem behaviors (n=514) or an assessment only control group (n=522) when their child was 10 to 13 years of age. The study interventions only involved parents and a detailed protocol has been published (55). The parenting intervention was based on Dishion (56) and focused on helping the parents work with their child to build positive behaviors, set effective limits, and strengthen their relationship. Tobacco use would be an example of a problem behavior that may be targeted by the intervention. Adolescent assent and parent consent were obtained at each of the six waves of assessment and participants received gift card reimbursements for completing follow-up surveys. University of California, San Diego Institutional Review Board approved the study protocol.
Participant Assessments
Adolescents (n=1036) were interviewed at baseline (from September 2003 to October 2004) and during five follow-up assessments at approximately 8-month intervals. The current study selected adolescents who at baseline reported that they had never tried cigarettes (even a puff) and had at least one follow-up assessment (n=878). Of this sample, 494 completed all six assessments (baseline and 5 follow-ups), 172 completed five, 107 completed four, 53 completed three, and 53 completed two assessments.
Measures
Sociodemographic
During the baseline assessment, adolescents self-reported their age, gender, ethnicity, and whether or not they currently lived in a single parent household.
Socioenvironmental: Exposure to smoking
At baseline, we assessed whether adolescents lived with a smoker with the question “Have any people that you live with now smoked cigarettes in the last year?” rated as yes or no.
Parenting Measures: Parental Responsiveness Scale
Adolescents rated six items from the Parental Responsiveness Scale as ‘just like,’ ‘a lot like,’ ‘sort of like’, or ‘not like’ their parent (57-60). The statements were ‘helps me calm down,’ ‘listens to what I have to say,’ ‘likes me just the way I am,’ ‘tells me when I do a good job,’ ‘wants to hear about my problems,’ and ‘respects my thoughts and feelings.’ The set of items was reliable in the current sample (Coefficient alpha = 0.87).
Parental Monitoring
A brief four-item parental monitoring scale was adapted from the Perceived Parental Demandingness Scale (57,60-63); which included statements on parental knowledge and questioning behavior such as what the teen did with friends, about homework, whether parents knew if the teen came home on time, and whether the parent let the teen get away with bad behavior. Each statement was rated as ‘just like,’ ‘a lot like,’ ‘sort of like,’ or ‘not like’ their parent and summed to create an index of parental monitoring. The index had adequate inter-item correlations (average r=0.47) although reliability was limited by the number of items and the broad domains included (coefficient alpha=0.52).
Parental Limit Setting - Hours Allowed Out
Following Steinberg et al. (60,62); adolescents were asked to report how many nights they went out for fun during the week and to indicate their typical curfew time for nights out on weekdays and weekends. The number of potential evening hours (6pm or later) that the adolescent went out during the week was calculated from these items.
Tobacco Parenting
At baseline, an index of tobacco-specific behaviors was created using a summation of positive response to three questions: ‘Have your parents ever discussed tobacco use with you?’ ‘Have you and your parents ever made an agreement that they will give you a reward for not smoking?’ and ‘Have you and your parents ever made an agreement that you would face some consequences if you smoked cigarettes and they were to find this out?’ Inter-item correlations ranged from 0.33-0.55 and reliability for this brief three-item index was 0.54.
Intrapersonal
Academic Performance
At baseline, adolescents ranked their performance in school as “much better than average,” “better than average,” “average,” or “below average” on the scale of academic performance developed for the Teenage Attitudes and Practices Survey (TAPS) (64).
Depressive Symptoms
At baseline, depressive symptoms during the past 6 months were assessed with Kandel's six-item index (65) that includes feeling tired, sad/depressed, hopeless about future, nervous/tense, as well as worry too much and too tired to do things. Each item was rated as never, rarely, sometimes, or often. This index has been validated in a similar population (66) and has an adequate reliability (Coefficient alpha=0.79).
Receptivity to Tobacco Marketing
Receptivity to tobacco marketing was measured at each assessment with these two questions: 1) “Think back to the cigarette advertisements you have recently seen. What is the name of the cigarette brand of your favorite cigarette advertisement?” and 2) “If you were given a tee shirt or a bag that had a tobacco industry cigarette brand image on it, would you use it?” For the first question, participants either named the brand of their favorite cigarette advertisement or indicated that they did not have a favorite cigarette advertisement. For the second question, participants were given four response choices from definitely yes to definitely not. Those who responded ‘probably yes’ or ‘definitely yes’ that they would use a branded promotional item were classified as ‘Highly Receptive.’ Those not classified as ‘Highly Receptive,’ but who named a favorite cigarette advertisement were classified as ‘Moderately Receptive.’ Those who would not use a branded promotional item and did not name a favorite cigarette advertisement were classified as having ‘Low Receptivity.’ Responses are included for all current never smokers at each wave of assessment. Although marketing restrictions from the MSA should prevent access to promotional items, these questions are expected to assess willingness and receptivity to use a branded promotional item.
Friends who smoke
At baseline and five follow-up waves of assessment we asked “How many of your best friends smoke?” rated ‘none,’ ‘some,’ ‘most,’ or ‘all,’ and coded dichotomously as either ‘none’ or ‘some/most/all.’
The Smoking Experimentation Process
To determine if the adolescent had experimented with cigarette use, at each assessment the survey asked, “Have you ever smoked a cigarette?” and, if not, “Have you ever tried or experimented with cigarette smoking, even a few puffs?” A positive response to either question classified the adolescent as having experimented with cigarette use.
Analysis
To address our first and second aim, we evaluated both baseline levels and changes in receptivity to tobacco marketing (low, moderate, or high) and exposure to friends who smoke over the six assessment waves using a parallel process growth curve model (67,68) that accommodates categorical variables and maximum likelihood estimation (69). In addition, this latent variable modeling framework enables assessment of these growth parameters as independent predictors of smoking experimentation. To evaluate the influence of initial status (i.e. intercepts) and change (i.e. slopes) in levels of receptivity to marketing and exposure to friend smoking on smoking experimentation (Aim 1), we combined the parallel growth model in a joint growth-survival model to calculate adjusted hazard ratios (HR) for the risk of smoking experimentation (69,70). Growth parameters were evaluated as independent predictors of time to smoking experimentation within a Cox proportional hazards model (69). Finally, by estimating relationships simultaneously we were able to evaluate hypothesized mediation (Aim 2). We assessed whether having friends who smoked influenced change in receptivity status (path ‘a’) and whether this change in turn predicted (path ‘b’) earlier smoking experimentation. We used a product of coefficients method (71,72) and bias corrected bootstrap confidence interval (73,74) to determine if this indirect effect was significantly different than zero.
All models included planned covariates reflecting demographic and socio-environmental characteristics, and treatment group allocation. Initial growth models for levels of receptivity over time and changes in exposure to smoking (i.e. friends who smoke) were evaluated with unconditional growth models (i.e. no covariates). We used maximum likelihood estimation with robust standard errors for models, allowing flexible handling of missing data and inclusion of individual cases with at least one follow-up assessment during the six waves (n=878). We collected smoking experimentation status from 96%, 91%, 84%, 80%, and 62% of adolescents at waves 2-6 respectively. We examined patterns of missing smoking data during the follow-up periods and noted that the likelihood of missing data was associated with baseline socio-demographic, treatment group assignment and academic performance status. Hence, in further multivariable modeling procedures our choice to adjust for these covariates allowed for the assumption that missing outcome data or dropouts were missing at random conditional on the fitted covariates. If this specification is correct, than our model provides unbiased estimates of examined study relationships with respect to biases resulting from missing data (75).
Results
Baseline Characteristics
Two-thirds of the 878 never-smoking adolescents came from the South or Midwest regions of the United States. Half were female, 64% self-identified as non-Hispanic White and 15% as Black (Table 1). At baseline, 23% lived in a single parent household, 35% reported living with a smoker and 10% reported having a friend who smoked. One third reported their school performance as average, while the majority reported better than average (36%) or much better than average (25%). Over a third (38%) were receptive to tobacco marketing.
Table 1.
Baseline characteristics of the sample of adolescents who had never smoked before their baseline assessment (N=878).
| Variable | N | % | Mean | SD |
| Sociodemographic | ||||
|
| ||||
| Age (range 10-13) | 11.87 | 0.87 | ||
| Female | 438 | 50% | ||
|
| ||||
| Race/Ethnicity | ||||
|
| ||||
| Non-Hispanic White | 559 | 64% | ||
| Black | 128 | 15% | ||
| Other race | 182 | 21% | ||
|
| ||||
| Region | ||||
|
| ||||
| Northeast | 138 | 16% | ||
| Midwest | 216 | 25% | ||
| South | 349 | 40% | ||
| West | 175 | 20% | ||
| Single parent | 202 | 23% | ||
|
| ||||
| Socio-environmental | ||||
|
| ||||
| Friends who smoke | 84 | 10% | ||
| Lives with a smoker | 311 | 35% | ||
|
| ||||
| Parenting | ||||
|
| ||||
| Parental responsiveness | 10.21 | 6.85 | ||
| Parental monitoring | 3.38 | 0.56 | ||
| Tobacco parenting | 1.49 | 0.89 | ||
| Parental limit setting | 2.73 | 0.48 | ||
|
| ||||
| Intrapersonal | ||||
|
| ||||
| School Achievement: Average | 310 | 35% | ||
| School Achievement: Better than average | 318 | 36% | ||
| School Achievement: Much better than average | 223 | 25% | ||
| School Achievement: Missing | 27 | 3% | ||
| Depressive symptoms | 7.76 | 3.96 | ||
|
| ||||
| Receptivity to marketing | ||||
|
| ||||
| Low | 544 | 62% | ||
| Moderate | 262 | 30% | ||
| High | 64 | 7% | ||
| Missing | 8 | 1% | ||
Changes in Receptivity and Exposure to Friends who Smoke Over Time
Over the five follow-up surveys, the proportion of adolescents who acquired close friends who smoked increased significantly. Given rates of smoking experimentation are known to be associated with age during adolescents, Figure 1a presents this growth separately for four single-age cohorts included in wave 1 (i.e. 10-13 years). Growth is presented within age-cohorts to highlight age-related differences in developmental influences. At age 10, few participants had friends who smoked. By age 14 years, over 25% had peers who smoked in three of the cohorts and the cohort that was below 25% increased rapidly in the following year. By the 6-year follow-up, more than 50% of all cohorts reported having friends who smoked.
Figure 1.
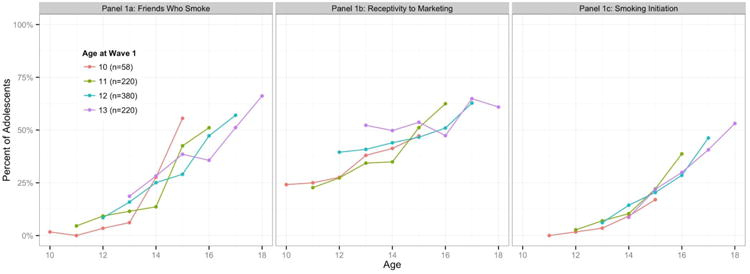
Growth over teen years of 1a) Exposure to friends who smoke, 1b) Receptivity to tobacco marketing and 1c) percent of teens who reported smoking experimentation at each assessment. These patterns are graphed separately for each of the four age cohorts of participant at wave 1 and aligned by chronological age.
The growth in receptivity to marketing is presented in Figure 1b. Although rates of receptivity were relatively high upon study entry, receptivity increased significantly over the six waves of assessment. Over 25% of 10 year olds were already receptive to tobacco marketing at study entry. In the cohort who entered at age 13 years, 50% were receptive. By age 15, approximately half of all respondents were receptive to tobacco marketing and by age 17-18, two-thirds of this population was receptive to tobacco marketing.
The percentage of never smoking participants from each age-cohort who subsequently reported having experimented with smoking at each assessment is presented in Figure 1c. Experimentation began to rapidly increase at age 14 years so that by 15 years, close to one fifth of the sample had experimented with smoking. By age 18, over 50% of participants had experimented with smoking.
Predictors of Baseline Levels of Exposure to Friends who Smoke and Receptivity to Marketing
At baseline, 10% of teens had a friend who smoked (Table 1). Predictors of exposure to friends who smoke are presented in Table 2 (1st column). The odds that an adolescents was exposed to friend smoking at baseline was higher if they were older at study entry, female, were from a single parent family, lived with a smoker, reported depressive symptoms, had lower scores on the parental responsiveness scale, and had more unsupervised free time. Aside from baseline variables, growth parameters described initial status and change over time. Initial receptivity to tobacco marketing was the only relevant growth parameter and was strongly associated with an increase in the odds of reporting friends who smoked at baseline (b=0.71, SE=0.08, p<0.01).
Table 2.
Influences on initial status and growth over 6 years in a) receptivity to tobacco marketing and b) exposure to friends who smoke. Parallel growth models were used to estimate the influence of parenting practices, socio-environmental tobacco use factors, and intrapersonal factors.
| Effect on BASELINE Measures of | Effect on CHANGE in | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||||
| 1. Friends Who Smoke | 2. Initial Receptivity | 3. Friends Who Smoke | 4. Receptivity | |||||||||
|
|
|
|
|
|||||||||
| Effect | SE | p | Effect | SE | p | Effect | SE | p | Effect | SE | p | |
| Covariates | ||||||||||||
|
| ||||||||||||
| Group | 0.37 | 0.24 | 0.13 | -0.15 | 0.18 | 0.41 | -0.06 | 0.07 | 0.41 | -0.02 | 0.06 | 0.78 |
| Female | 0.68 | 0.25 | 0.01 | -0.58 | 0.18 | 0.00 | -0.31 | 0.07 | 0.00 | -0.05 | 0.08 | 0.55 |
| Age | 1.38 | 0.17 | 0.00 | 0.02 | 0.14 | 0.91 | -0.13 | 0.05 | 0.01 | -0.05 | 0.06 | 0.36 |
| Race/Ethinicity | ||||||||||||
| Black vs White | -0.04 | 0.23 | 0.85 | -0.09 | 0.17 | 0.62 | 0.01 | 0.06 | 0.94 | -0.05 | 0.06 | 0.33 |
| Other vs White | 0.19 | 0.22 | 0.39 | 0.11 | 0.16 | 0.50 | -0.02 | 0.06 | 0.69 | -0.01 | 0.06 | 0.93 |
| Region | ||||||||||||
| North vs. East | -0.35 | 0.26 | 0.19 | -0.24 | 0.18 | 0.19 | 0.06 | 0.07 | 0.41 | 0.06 | 0.07 | 0.35 |
| Midwest vs. East | -0.05 | 0.23 | 0.84 | 0.14 | 0.17 | 0.41 | -0.07 | 0.07 | 0.27 | -0.04 | 0.05 | 0.51 |
| West vs. East | -0.10 | 0.27 | 0.70 | 0.02 | 0.19 | 0.94 | 0.02 | 0.07 | 0.84 | -0.02 | 0.06 | 0.75 |
| Single Parent | 0.64 | 0.30 | 0.03 | -0.09 | 0.21 | 0.67 | -0.08 | 0.08 | 0.37 | 0.06 | 0.07 | 0.36 |
|
| ||||||||||||
| Socio-environmental | ||||||||||||
|
| ||||||||||||
| Lives with smoker | 0.55 | 0.26 | 0.03 | 0.29 | 0.19 | 0.12 | 0.18 | 0.08 | 0.02 | -0.12 | 0.07 | 0.11 |
|
| ||||||||||||
| Parenting | ||||||||||||
|
| ||||||||||||
| Parental Responsive | -0.64 | 0.29 | 0.03 | 0.17 | 0.20 | 0.37 | 0.08 | 0.08 | 0.28 | -0.06 | 0.07 | 0.38 |
| Patental Monitoring | 0.14 | 0.32 | 0.67 | -0.22 | 0.23 | 0.35 | -0.02 | 0.09 | 0.85 | 0.08 | 0.08 | 0.30 |
| Tobacco Parenting | -0.12 | 0.15 | 0.44 | 0.13 | 0.11 | 0.25 | 0.06 | 0.04 | 0.15 | -0.05 | 0.04 | 0.21 |
| Parental limit setting | 0.38 | 0.12 | 0.00 | -0.11 | 0.09 | 0.25 | -0.09 | 0.03 | 0.01 | 0.05 | 0.04 | 0.21 |
|
| ||||||||||||
| Intrapersonal | ||||||||||||
|
| ||||||||||||
| School Achievement | -0.24 | 0.17 | 0.15 | -0.11 | 0.12 | 0.35 | -0.11 | 0.05 | 0.01 | 0.05 | 0.04 | 0.29 |
| Internalizing | 0.67 | 0.17 | 0.00 | -0.11 | 0.12 | 0.39 | -0.03 | 0.05 | 0.55 | 0.02 | 0.04 | 0.73 |
|
| ||||||||||||
| Growth Parameters | ||||||||||||
|
| ||||||||||||
| Initial receptivity | 0.71 | 0.08 | 0.00 | -- | -- | -- | -0.43 | 0.12 | 0.00 | -- | -- | -- |
| Change in receptivity | -- | -- | -- | -- | -- | -- | 0.38 | 0.21 | 0.08 | -- | -- | -- |
| Initial Friends Who Smoke | -- | -- | -- | -- | -- | -- | -- | -- | -- | 0.12 | 0.18 | 0.51 |
We also considered which variables were associated with the 37% of youth who were receptive to tobacco marketing at baseline (Table 2, 2nd column). In contrast to the many predictors of initial exposure to peer smoking, there was only one variable that was predictive of marketing receptivity: adolescents who were females had lower odds of marketing receptivity
Growth in Exposure to Friend Smoking
A preliminary evaluation of an unconditional growth model for exposure to friend smoking suggested that a linear specification provided a good fit to the data (RMSEA=0.05, CFI=0.99; TLI=0.98; X2(11)=30.6, p<0.01). The conditional effects of the predictors are presented in Table 2 (3rd column). Baseline predictors of the 48% of teens who acquired friends who smoked during the study include age, living with a smoker, lower parental limit setting, and school performance. We consider the initial receptivity level as a growth parameter. Given that initial receptivity was strongly associated with the initial reporting of friends who smoke, there was a less rapid escalation in acquiring a friend who smoked over time among those with higher baseline levels of receptivity (b= -0.43, SE= 0.12, p < 0.001). Given the above, the association between change in receptivity to marketing and change in friends who smoke only reached borderline significance (p=0.08) in the model.
Growth in Receptivity to Marketing
The unconditional growth models for receptivity to tobacco marketing was a good fit to the data (RMSEA=0.06, CFI=0.96; TLI=0.97; X2(16)=67.7, p<0.01). We present the conditional effects of the predictors in Table 2 (4th column). Sociodemographic, parenting, and intrapersonal vulnerability indices were not significantly associated with observed increases in levels of receptivity to tobacco marketing during the 6 years of the study. Although the initial reporting of friends who smoke was not related to change in receptivity over time (p=0.51), as noted earlier, there is a strong relationship between initial status in reporting friends who smoke and initial level of receptivity to marketing.
Influences on smoking experimentation
Table 3 presents the results of the joint parallel growth-survival model that estimates the prospective and independent associations of the above set of variables on the risk of smoking experimentation. Considering the covariates first, being randomized to the intervention group in the parenting study was not associated with smoking experimentation (HRadj=0.96, p=0.37). Adolescents who identified as Black, tended to initiate smoking later than whites (HRadj=0.74, p<0.01). Aside from race, only two other covariates were associated with smoking experimentation: living in a single parent family (HRadj=1.17, p<0.01)) and lower levels of parental limit setting at baseline (HRadj=1.13, p<0.01) both increased the risk of smoking experimentation. After adjustment for covariates, we considered the growth parameters for friends who smoke and receptivity to marketing, although the two were highly correlated. Both exposure to friends who smoke at baseline, (HRadj=2.50, p<0.01) and acquiring friends who smoke during the study (HRadj=1.70, p<0.01) were by far the strongest predictors of smoking experimentation. Yet, being receptive to marketing at baseline also independently increased the risk of smoking experimentation by 24% (HRadj=1.24, p<0.01). Increasing receptivity to tobacco marketing during the study did not independently add to this predictive model of experimentation.
Table 3.
Estimates of the independent association of initial status and growth in both receptivity to tobacco marketing and exposure to friends who smoke along with parenting practices, other socio-environmental factors, and intrapersonal factors on risk for smoking experimentation using a Cox proportional hazards survival model.
| Variable | Effect | SE | p | HR | 95% CI | ||
|---|---|---|---|---|---|---|---|
| Covariates on Initiation | |||||||
|
| |||||||
| Group | -0.04 | 0.05 | 0.37 | 0.96 | 0.87 | 1.05 | |
| Female | 0.06 | 0.06 | 0.30 | 1.06 | 0.95 | 1.19 | |
| Age | 0.01 | 0.06 | 0.82 | 1.01 | 0.90 | 1.14 | |
| Race/Ethnicity | |||||||
| Black vs White | -0.30 | 0.08 | 0.00 | 0.74 | 0.63 | 0.87 | |
| Other vs White | 0.26 | 0.07 | 0.00 | 1.29 | 1.12 | 1.49 | |
| Region | |||||||
| North v East | 0.03 | 0.07 | 0.65 | 1.03 | 0.90 | 1.18 | |
| Midwest v East | -0.01 | 0.07 | 0.88 | 0.99 | 0.87 | 1.13 | |
| West v East | 0.00 | 0.07 | 0.96 | 1.00 | 0.88 | 1.13 | |
| Single Parent | 0.16 | 0.05 | 0.00 | 1.17 | 1.06 | 1.28 | |
|
| |||||||
| Socio-environmental | |||||||
|
| |||||||
| Lives with smoker | -0.02 | 0.05 | 0.75 | 0.98 | 0.89 | 1.09 | |
|
| |||||||
| Parenting | |||||||
|
| |||||||
| Parental Responsive | -0.03 | 0.06 | 0.65 | 0.98 | 0.87 | 1.09 | |
| Patental Monitoring | 0.02 | 0.06 | 0.77 | 1.02 | 0.91 | 1.14 | |
| Tobacco Parenting | -0.01 | 0.05 | 0.81 | 0.99 | 0.89 | 1.09 | |
| Parental limit setting | 0.13 | 0.05 | 0.02 | 1.13 | 1.02 | 1.25 | |
|
| |||||||
| Intrapersonal | |||||||
|
| |||||||
| School Performance | -0.07 | 0.05 | 0.17 | 0.93 | 0.84 | 1.03 | |
| Internalizing | 0.06 | 0.05 | 0.26 | 1.06 | 0.96 | 1.17 | |
|
| |||||||
| Growth Parameters | |||||||
|
| |||||||
| Initial: Receptivity | 0.21 | 0.09 | 0.02 | 1.24 | 1.03 | 1.48 | |
| Change: Receptivity | 0.04 | 0.07 | 0.57 | 1.04 | 0.91 | 1.19 | |
| Initial: Some Friends Smoke | 0.90 | 0.10 | 0.00 | 2.45 | 2.02 | 2.97 | |
| Change: Some Friends Smoke | 0.54 | 0.10 | 0.00 | 1.71 | 1.40 | 2.09 | |
Note: HR = adjusted hazard ratio;
To address aim 2, we estimated whether the effect of exposure to friends who smoke on risk for smoking experimentation might be partially explained by an indirect relationship with receptivity to marketing. We estimated the indirect effects using a product of coefficients method for survival outcomes (71,72) and empirical estimation of standard errors (73,74). The estimate of the indirect effect of growth in exposure to peer smoking through growth in receptivity was not significantly different from zero (a*b=0.04, SE= 0.08, p=0.58), suggesting a lack of evidence for the hypothesis that friends increase receptivity to tobacco marketing, which then in turn increases risk for smoking experimentation.
Discussion
This six wave nationally representative study, which included pre-adolescent youth as young as 10 years old, incorporated the starting points for smoking experimentation, receptivity to tobacco marketing and exposure to friends who smoked. It was clear that by this early age there had already been significant penetration of tobacco marketing with up to one quarter reporting a favorite cigarette advertisement at baseline. During the study, we observed a linear growth in the proportion of adolescents who were both receptive to marketing and exposed to friends who smoked. As in previous studies, the two strongest predictors of smoking experimentation in our model were having a friend who smoked at study baseline, followed by acquiring such friends for the first time during the study. This is consistent with the hypotheses that friends provide the access to first cigarette use, and that social factors are important in facilitating cigarette smoking experimentation. These predictors were followed by being receptive to tobacco marketing (having a favorite cigarette ad) at baseline; becoming receptive to tobacco marketing at a later time, however, did not independently increase the risk of smoking experimentation.
Of particular interest in this study is that becoming increasingly receptive to tobacco marketing during the study was not independently associated with experimentation in our model that included the influence of increasing exposure to friends who smoke. However, the initial level of receptivity was strongly associated with the proportion who had friends who smoked at baseline. Levels of receptivity to marketing remained significantly associated with having friends who smoked throughout the study observational period. Thus, our data are consistent with the hypothesis that becoming receptive to tobacco marketing can precede exposure to friends who smoke. By contrast, we did not find evidence supporting the hypothesis that receptivity to marketing follows being exposed to friends who smoke. Given these findings, inoculating teens who are receptive to tobacco marketing from the influence of friends who smoke may be an important strategy in smoking prevention campaigns. However, the high level of receptivity to marketing that we observed, even among the 10 year olds who entered this study, and its robust relationship with an increased risk for smoking experimentation suggest that such a successful intervention should focus on preventing receptivity to tobacco industry marketing even at earlier ages (76).
Approximately 5 years before the start of this study, the Master Settlement Agreement (77,78) was designed, in large part, to eliminate tobacco industry marketing that targeted adolescents in the United States. Although this resulted in the discontinuance of cartoon characters and promotional materials, this study has documented the awareness of tobacco marketing in childhood. Children as young as 10 years continue to be highly receptive to tobacco marketing imagery, and that this receptivity was a major influence encouraging them to start smoking. One third of the adolescents in this study had moderate-to-high levels of receptivity to marketing at baseline, when they were 10 to 13 years of age, much younger than age 18, the legal age to buy cigarettes in most states. This suggests that the terms of the Master Settlement Agreement alone may not adequately protect adolescents from tobacco marketing. Further development of measures of receptivity is needed to overcome reliance on inquiries of willingness to use branded promotional items that are no longer in use in the United States.
The original parenting study (55) sought to address adolescent smoking experimentation and other problem behaviors by helping parents improve their parenting skills through building a more responsive relationship with their child, limiting their child's unsupervised free time, and using rewards to build positive behaviors, as outlined by Dishion et al (56,79,80). In the current analyses, only the level of limit setting that the child reported at baseline was associated with later experimentation. Both parental responsiveness and limit-setting were associated with baseline levels of exposure to peers who smoked, although neither was related to whether the teen was receptive to tobacco marketing at baseline or developed such receptivity during the study. We did not find an association between tobacco-related parenting and the initial levels or growth in either exposure to friends who smoke or receptivity to marketing. Future studies are needed among children younger than 10 years that focus on reducing receptivity to tobacco marketing as well as improving parenting limit-setting skills.
Compounding the difficulties of regulating tobacco marketing is the major change in the communication media through which messages can be seen by and targeted to children. The proliferation of social media usage, especially in the young, has opened the possibility of exposure to marketing messages through various channels, including consumer-to-consumer chat, with some messages going “viral.” Continuing to monitor and evaluate how receptivity to tobacco marketing changes over time and the factors that influence receptivity to various forms of marketing materials will be important in future studies as social media continues to expand and evolve.
Adolescents with intrapersonal vulnerability including poor perceptions of academic performance and reports of depressive symptoms are at greater risk for smoking experimentation (81,82). That depression was related to increased exposure to friends who smoke in the current study suggests that adolescents who struggle with depression may form friendships with other adolescents who are prone to using tobacco products. Non-smoking teens with mental health problems such as depression represent a vulnerable population at elevated risk for persistent depressive disorders (83), uptake of persistent tobacco use (84) and progression to nicotine dependence (85-87). Vulnerability to peer influences may reflect another independent pathway explaining the high prevalence.
A major strength of these analyses included a US national sample of adolescents, oversampling of respondents who identified as Black, an important demographic group typically underrepresented in studies of risk for tobacco use. Further, the sampling frame included six waves at approximately annual intervals, each of which measured a wide range of domains that have been shown previously to influence smoking experimentation. However, several limitations should be noted. Because participants were recruited into a study focused on parenting and smoking, it is likely that enrollment was higher among parents who were concerned about their child's approaching adolescence. Thus, the study may have sampled from among those who were already engaging in more effective parenting overall, and this could partially explain our low smoking experimentation rates. Longer follow-up into the early adult years would have allowed the analysis to focus on adult smoking behavior as a study outcome of concern to the prevention community. Some have argued that more frequent measurements (every three months) provide more appropriate monitoring of change among adolescents (88); however, increased measurement frequency can also modify the behavior being studied, which would be an undesirable effect. Another limitation is that these results are limited to cigarette use. Future investigations should expand this line of research to include measures of other types of tobacco products used by the adolescent, their friends, and the people they live with. Lastly, longitudinal research such as this may be limited by sample attrition and differential loss to follow-up.
Conclusion
This national study identified the expected trajectories of smoking experimentation in adolescents from the ages of 10 through 20 years. With multiple measurements, we have identified that receptivity to tobacco marketing in early adolescents preceded a large increase in exposure to friends who smoke. Indeed, that one in four 10 year olds were already receptive to tobacco marketing suggests the need for more focused prevention efforts in young populations. This study did not support the mediating hypothesis that friend smoking influenced the probability that teens would be receptive to tobacco marketing which then led to experimentation with cigarettes. It will be important to continue to evaluate connections between intrapersonal vulnerabilities, marketing messages, and smoking experimentation with more recent and expansive data that includes a range of tobacco products.
Acknowledgments
Support: Funding for the primary data collection was provided by National Cancer Institute grant CA093982, an American Legacy Foundation grant, and Tobacco Related Disease Research Program grants 17RT-0088, 21XT-0076 and 15RT-0238 from the University of California. Funding for this analysis and manuscript preparation has been funded with Federal funds from the National Institute on Drug Abuse, National Institutes of Health, and the Food and Drug Administration, Department of Health and Human Services, under Contract No. HHSN271201100027C, and Tobacco Related Disease Research Program grant 21RT-01335. The views and opinions expressed in this presentation are those of the authors only and do not necessarily represent the views, official policy or position of the US Department of Health and Human Services or any of its affiliated institutions or agencies.
Footnotes
COI and Ethical Adherence: All authors have adhered to the Principles of the Ethical Practice of Public Health. In addition, all authors declare no conflicts of interest.
References
- 1.Wellman RJ, Dugas EN, Dutczak H, et al. Predictors of the Onset of Cigarette Smoking. Am J Prev Med. 2016;51(5):767–778. doi: 10.1016/j.amepre.2016.04.003. [DOI] [PubMed] [Google Scholar]
- 2.Services USDoHaH. Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2012. [Google Scholar]
- 3.Bauman Ke EST. On the importance of peer influence for adolescent drug use: commonly neglected considerations. Addiction. 1996;91(2):185–198. [PubMed] [Google Scholar]
- 4.Kobus K. Peers and adolescent smoking. Addiction. 2003;98(1):37–55. doi: 10.1046/j.1360-0443.98.s1.4.x. [DOI] [PubMed] [Google Scholar]
- 5.Arnett JJ. The myth of peer influence in adolescent smoking initiation. Health Educ Behav. 2007;34(4):594–607. doi: 10.1177/1090198105285330. [DOI] [PubMed] [Google Scholar]
- 6.USDHHS. Preventing Tobacco Use Among Young People: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion Office on Smoking and Health; 1994. [Google Scholar]
- 7.Harrison PA, Fulkerson JA, Park E. The relative importance of social versus commercial sources in youth access to tobacco, alcohol, and other drugs. Prev Med. 2000;31(1):39–48. doi: 10.1006/pmed.2000.0691. [DOI] [PubMed] [Google Scholar]
- 8.Forster J, Chen V, Blaine T, Perry C, Toomey T. Social exchange of cigarettes by youth. Tob Control. 2003;12(2):148–154. doi: 10.1136/tc.12.2.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.White MM, Gilpin EA, Emery SL, Pierce JP. Facilitating adolescent smoking: who provides the cigarettes? Am J Health Promot. 2005;19(5):355–360. doi: 10.4278/0890-1171-19.5.355. [DOI] [PubMed] [Google Scholar]
- 10.Robinson LA, Murray DM, Alfano CM, Zbikowski SM, Blitstein JL, Klesges RC. Ethnic differences in predictors of adolescent smoking onset and escalation: a longitudinal study from 7th to 12th grade. Nicotine Tob Res. 2006;8(2):297–307. doi: 10.1080/14622200500490250. [DOI] [PubMed] [Google Scholar]
- 11.Bandura A. Social Learning Theory. Englewood Cliffs, NJ: Prentice Hall; 1977. [Google Scholar]
- 12.Bandura A. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- 13.Urberg KA, Shyu SJ, Liang J. Peer influence in adolescent cigarette smoking. Addict Behav. 1990;15(3):247–255. doi: 10.1016/0306-4603(90)90067-8. [DOI] [PubMed] [Google Scholar]
- 14.Simon Tr SSDCWBDFBR. Correlates of exclusive or combined use of cigarettes and smokeless tobacco among male adolescents. Addictive Behavior. 1993;18(6):623–634. doi: 10.1016/0306-4603(93)90016-3. [DOI] [PubMed] [Google Scholar]
- 15.Hoving C, Reubsaet A, de Vries H. Predictors of smoking stage transitions for adolescent boys and girls. Prev Med. 2007;44(6):485–489. doi: 10.1016/j.ypmed.2007.02.011. [DOI] [PubMed] [Google Scholar]
- 16.Distefan JM, Pierce JP, Gilpin EA. Do favorite movie stars influence adolescent smoking initiation? Am J Public Health. 2004;94(7):1239–1244. doi: 10.2105/ajph.94.7.1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pierce JP, Lee L, Gilpin EA. Smoking initiation by adolescent girls, 1944 through 1988. An association with targeted advertising [see comments] JAMA. 1994;271(8):608–611. [PubMed] [Google Scholar]
- 18.Wells W, Burnett J, Moriarty S. Advertising: principles & practice. Vol. 5. illustrated ed: Prentice Hall; 2000. [Google Scholar]
- 19.Evans N, Farkas A, Gilpin E, Berry C, Pierce JP. Influence of tobacco marketing and exposure to smokers on adolescent susceptibility to smoking. J Natl Cancer Inst. 1995;87(20):1538–1545. doi: 10.1093/jnci/87.20.1538. [DOI] [PubMed] [Google Scholar]
- 20.McGuire WJ. Personality and attitdue change: An information-processing theory. In: Greenwald AG, Brock TC, Ostrom TM, editors. Psychological foundations of attitudes. New York: Academic; 1968. pp. 171–196. [Google Scholar]
- 21.McGuire WJ. The yin and yang of progress in social psychology: Seven koan. Journal of Personality and Social Psychology. 1973;26:10. [Google Scholar]
- 22.Cohen JB. Playing to win: marketing and public policy at odds over “Joe Camel”. Journal of Public Policy and Marketing. 2000;19(2):155–167. [Google Scholar]
- 23.Pierce JP, Choi WS, Gilpin EA, Farkas AJ, Berry CC. Tobacco industry promotion of cigarettes and adolescent smoking. JAMA. 1998;279(7):511–515. doi: 10.1001/jama.279.7.511. [DOI] [PubMed] [Google Scholar]
- 24.Gilpin EA, White MM, Messer K, Pierce JP. Receptivity to tobacco advertising and promotions among young adolescents as a predictor of established smoking in young adulthood. Am J Public Health. 2007;97(8):1489–1495. doi: 10.2105/AJPH.2005.070359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Biglan A, Duncan TE, Ary DV, Smolkowski K. Peer and parental influences on adolescent tobacco use. Journal of behavioral medicine. 1995;18(4):315–330. doi: 10.1007/BF01857657. [DOI] [PubMed] [Google Scholar]
- 26.Engels RC, Vitaro F, Blokland ED, de Kemp R, Scholte RH. Influence and selection processes in friendships and adolescent smoking behaviour: the role of parental smoking. J Adolesc. 2004;27(5):531–544. doi: 10.1016/j.adolescence.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 27.Brook JS, Pahl K, Ning Y. Peer and parental influences on longitudinal trajectories of smoking among African Americans and Puerto Ricans. Nicotine Tob Res. 2006;8(5):639–651. doi: 10.1080/14622200600789627. [DOI] [PubMed] [Google Scholar]
- 28.Chassin L, Presson C, Seo DC, et al. Multiple trajectories of cigarette smoking and the intergenerational transmission of smoking: a multigenerational, longitudinal study of a Midwestern community sample. Health Psychol. 2008;27(6):819–828. doi: 10.1037/0278-6133.27.6.819. [DOI] [PubMed] [Google Scholar]
- 29.Cohen DA, Richardson J, LaBree L. Parenting behaviors and the onset of smoking and alcohol use: A longitudinal study. Pediatrics. 1994;94:368–375. [PubMed] [Google Scholar]
- 30.Flay BR, Hu FB, et al. Differential influence of parental smoking and friends' smoking on adolescent initiation and escalation of smoking. Journal of health and social behavior. 1994;35:248–265. [PubMed] [Google Scholar]
- 31.Distefan JM, Gilpin EA, Choi WS, Pierce JP. Parental influences predict adolescent smoking in the United States, 1989-1993. J Adolesc Health. 1998;22(6):466–474. doi: 10.1016/s1054-139x(98)00013-5. [DOI] [PubMed] [Google Scholar]
- 32.Scal P, Ireland M, Borowsky IW. Smoking among American adolescents: a risk and protective factor analysis. Journal of community health. 2003;28(2):79–97. doi: 10.1023/a:1022691212793. [DOI] [PubMed] [Google Scholar]
- 33.Kandel DB, Kiros GE, Schaffran C, Hu MC. Racial/ethnic differences in cigarette smoking initiation and progression to daily smoking: a multilevel analysis. Am J Public Health. 2004;94(1):128–135. doi: 10.2105/ajph.94.1.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.WJ D, W A. Family functioning and parental smoking as predictors of adolescent cigarette use: a six-year prospective sutdy. Journal of Family Psychology. 1994;8(3):347–353. [Google Scholar]
- 35.Mahabee-Gittens EM, Khoury JC, Huang B, Dorn LD, Ammerman RT, Gordon JS. The Protective Influence of Family Bonding on Smoking Initiation in Adolescents by Racial/Ethnic and Age Subgroups. Journal of child & adolescent substance abuse. 2011;20(3):270–287. doi: 10.1080/1067828X.2011.581969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dishion TJ, Capaldi D, Yoerger K. Middle childhood antecedents to progressions in male adolescent substance use: an ecologicial analysis of risk and protection. Journal of Adolescent Research. 1999;14(2):175–205. [Google Scholar]
- 37.Simons-Morton BG. Prospective analysis of peer and parent influences on smoking initiation among early adolescents. Prev Sci. 2002;3(4):275–283. doi: 10.1023/a:1020876625045. [DOI] [PubMed] [Google Scholar]
- 38.Pierce JP, Farkas AJ, Evans N, et al. Tobacco Use in California 1992 A Focus on Preventing Uptake in Adolescents. Sacramento, CA: California Department of Health Services; 1993. [Google Scholar]
- 39.Conrad KM, Flay BR, Hill D. Why children start smoking cigarettes: predictors of onset. Br J Addict. 1992;87(12):1711–1724. doi: 10.1111/j.1360-0443.1992.tb02684.x. [DOI] [PubMed] [Google Scholar]
- 40.Tyas SL, Pederson LL. Psychosocial factors related to adolescent smoking: a critical review of the literature. Tob Control. 1998;7(4):409–420. doi: 10.1136/tc.7.4.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Avenevoli S, Merikangas KR. Familial influences on adolescent smoking. Addiction. 2003;98(1):1–20. doi: 10.1046/j.1360-0443.98.s1.2.x. [DOI] [PubMed] [Google Scholar]
- 42.Pierce JP, Fiore MC, Novotny TE, Hatziandreu EJ, Davis RM. Trends in cigarette smoking in the United States. Educational differences are increasing. JAMA. 1989;261(1):56–60. [PubMed] [Google Scholar]
- 43.Dewey JD. Reviewing the relationship between school factors and substance use for elementary, middle, and high school students. Journal of Primary Prevention. 1999;19(3):177–225. [Google Scholar]
- 44.Cox RG, Zhang L, Johnson WD, Bender DR. Academic performance and substance use: findings from a state survey of public high school students. J Sch Health. 2007;77(3):109–115. doi: 10.1111/j.1746-1561.2007.00179.x. [DOI] [PubMed] [Google Scholar]
- 45.Forrester K, Biglan A, Severson HH, Smolkowski K. Predictors of smoking onset over two years. Nicotine Tob Res. 2007;9(12):1259–1267. doi: 10.1080/14622200701705357. [DOI] [PubMed] [Google Scholar]
- 46.Sutherland I, Shepherd JP. Social dimensions of adolescent substance use. Addiction. 2001;96(3):445–458. doi: 10.1046/j.1360-0443.2001.9634458.x. [DOI] [PubMed] [Google Scholar]
- 47.Morin AJ, Rodriguez D, Fallu JS, Maiano C, Janosz M. Academic achievement and smoking initiation in adolescence: a general growth mixture analysis. Addiction. 2012;107(4):819–828. doi: 10.1111/j.1360-0443.2011.03725.x. [DOI] [PubMed] [Google Scholar]
- 48.Pierce JP, Choi WS, Gilpin EA, Farkas AJ, Merritt RK. Validation of susceptibility as a predictor of which adolescents take up smoking in the United States. Health Psychol. 1996;15:355–361. doi: 10.1037//0278-6133.15.5.355. [DOI] [PubMed] [Google Scholar]
- 49.Bricker JB, Rajan KB, Zalewski M, Ramey M, Peterson AV, Andersen MR. Psychological and social risk factors in adolescent smoking transitions: a population-based longitudinal study. Health Psychol. 2009;28(4):439–447. doi: 10.1037/a0014568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chassin L, Presson CC, Pitts SC, Sherman SJ. The natural history of cigarette smoking from adolescence to adulthood in a midwestern community sample: multiple trajectories and their psychosocial correlates. Health Psychol. 2000;19(3):223–231. [PubMed] [Google Scholar]
- 51.Windle M, Windle RC. Depressive symptoms and cigarette smoking among middle adolescents: prospective associations and intrapersonal and interpersonal influences. J Consult Clin Psychol. 2001;69(2):215–226. [PubMed] [Google Scholar]
- 52.Stanton WR, Flay BR, Colder CR, Mehta P. Identifying and predicting adolescent smokers' developmental trajectories. Nicotine Tob Res. 2004;6(5):843–852. doi: 10.1080/14622200410001734076. [DOI] [PubMed] [Google Scholar]
- 53.Patten CA, Choi WS, Vickers KS, Pierce JP. Persistence of depressive symptoms in adolescents. Neuropsychopharmacology. 2001;25(5 Suppl):S89–91. doi: 10.1016/S0893-133X(01)00323-2. [DOI] [PubMed] [Google Scholar]
- 54.Audrain-McGovern J, Rodriguez D, Kassel JD. Adolescent smoking and depression: evidence for self-medication and peer smoking mediation. Addiction. 2009;104(10):1743–1756. doi: 10.1111/j.1360-0443.2009.02617.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pierce JP, James LE, Messer K, Myers MG, Williams RE, Trinidad DR. Telephone counseling to implement best parenting practices to prevent adolescent problem behaviors. Contemp Clin Trials. 2008;29(3):324–334. doi: 10.1016/j.cct.2007.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dishion TJ, Kavanagh K. Intervening in Adolescent Problem Behavior: A Family-Centered Approach. New York: Guilford Press; 2003. [Google Scholar]
- 57.Baumrind D. Parental disciplinary patterns and social competence in children. Youth & Society. 1978:239–275. [Google Scholar]
- 58.Baumrind D. The Influencing of Parenting Style on Adolescent Competence and Substance Use. Journal of Early Adolescence. 1991;11(1):56–95. [Google Scholar]
- 59.Steinberg L, Fletcher A, Darling N. Parental monitoring and peer influences on adolescent substance use. Pediatrics. 1994;93(6):1060–1064. [PubMed] [Google Scholar]
- 60.Steinberg L, Lamborn SD, Dornbusch SM, Darling N. Impact of parenting practices on adolescent achievement: Authoritative parenting, school involvement, and encouragement to succeed. Child Development. 1992;63:1266–1281. doi: 10.1111/j.1467-8624.1992.tb01694.x. [DOI] [PubMed] [Google Scholar]
- 61.Lamborn Sd MNSSLDSM. Patterns of competence and adjustment among adolescents from authoritative, authoritarian, indulgent, and neglectful families. Child Development. 1991;62(5):1049–1065. doi: 10.1111/j.1467-8624.1991.tb01588.x. [DOI] [PubMed] [Google Scholar]
- 62.Fletcher AC, Steinberg L, Williams-Wheeler M. Parental influences on adolescent problem behavior: revisiting Stattin and Kerr. Child Dev. 2004;75(3):781–796. doi: 10.1111/j.1467-8624.2004.00706.x. [DOI] [PubMed] [Google Scholar]
- 63.Jackson C, Henriksen L, Foshee VA. The Authoritative Parenting Index: predicting health risk behaviors among children and adolescents. Health Educ Behav. 1998;25(3):319–337. doi: 10.1177/109019819802500307. [DOI] [PubMed] [Google Scholar]
- 64.U.S. Department of Health Human Services. Guidelines for school health programs to prevent tobacco use & addiction. MMWR. 1994;43(RR-2):1–18. [PubMed] [Google Scholar]
- 65.Kandel DB, Davies M. Epidemiology of depressive mood in adolescents: an empirical study. Arch Gen Psychiatry. 1982;39(10):1205–1212. doi: 10.1001/archpsyc.1982.04290100065011. [DOI] [PubMed] [Google Scholar]
- 66.Choi WS, Patten CA, Gillin JC, Kaplan RM, Pierce JP. Cigarette smoking predicts development of depressive symptoms among U.S. adolescents. Ann Behav Med. 1997;19(1):42–50. doi: 10.1007/BF02883426. [DOI] [PubMed] [Google Scholar]
- 67.Cheong J, Mackinnon DP, Khoo ST. Investigation of Mediational Processes Using Parallel Process Latent Growth Curve Modeling. Structural equation modeling : a multidisciplinary journal. 2003;10(2):238. doi: 10.1207/S15328007SEM1002_5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.JB W, AG S. Using covariance structure analysis to detect correlates and predictors of individual change over time. Psychological Bulletin. 1994;116(2):363–381. [Google Scholar]
- 69.M B, A T, B M, H M, N A. Applicaitons of continuous-time survival in latent variable models for the analysis of oncology randomized clincial trial data using Mplus, Tecnical Report 2009. 2009 [Google Scholar]
- 70.Diggle PJ, Henderson R, Philipson P. Random-effects models for joint analysis of repeated-measurement and time-to-event outcomes. In: Fitzmaurice GM, Davidian M, Verbeke G, Molenberghs G, editors. Longituidnal Data Analysis. Boca Raton: Chapman & Hall/CRC Press; 2008. pp. 349–366. [Google Scholar]
- 71.MacKinnon DP, Dwyer J. Estimating Mediated Effects in Prevention Studies. Evaluation Review. 1993;17(2):144–158. [Google Scholar]
- 72.Tein J, MacKinnon DP. Estimating mediated effects with survival data. In: Yanai H, Rikkyo A, Shigemasu K, Kano Y, Meulman J, editors. New Developments in Psychometrics: Psychometric Society Proceedings. Tokyo: Springer-Verlag; 2003. pp. 405–412. [Google Scholar]
- 73.Mackinnon DP, Lockwood CM, Williams J. Confidence Limits for the Indirect Effect: Distribution of the Product and Resampling Methods. Multivariate behavioral research. 2004;39(1):99. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Tofighi D, MacKinnon DP. RMediation: an R package for mediation analysis confidence intervals. Behavior research methods. 2011;43(3):692–700. doi: 10.3758/s13428-011-0076-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Little RJ, Rubin DB. Statistical Analysis with Missing Data. 2. Wiley; 2002. [Google Scholar]
- 76.Biglan A, Brennan P, Foster S, Holder H. Helping Adolescents at Risk: Prevention of Multiple Problem Behaviors. New York: The Guilford Press; 2004. [Google Scholar]
- 77.Pierce JP, Gilpin EA. How did the Master Settlement Agreement change tobacco industry expenditures for cigarette advertising and promotions? Health Promot Pract. 2004;5(3 Suppl):84S–90S. doi: 10.1177/1524839904264600. [DOI] [PubMed] [Google Scholar]
- 78.Wikipedia. [Accessed May 21, 2013];Tobacco Master Settlement Agreement. 2013 http://en.wikipedia.org/wiki/Tobacco_Master_Settlement_Agreement.
- 79.Dishion TJ, McMahon RJ. Parental monitoring and the prevention of child and adolescent problem behavior: a conceptual and empirical formulation. Clinical child and family psychology review. 1998;1(1):61–75. doi: 10.1023/a:1021800432380. [DOI] [PubMed] [Google Scholar]
- 80.Dishion TJ, Nelson SE, Bullock BM. Premature adolescent autonomy: parent disengagement and deviant peer process in the amplification of problem behaviour. J Adolesc. 2004;27(5):515–530. doi: 10.1016/j.adolescence.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 81.Edelen MO, Tucker JS, Ellickson PL. A discrete time hazards model of smoking initiation among West Coast youth from age 5 to 23. Prev Med. 2007;44(1):52–54. doi: 10.1016/j.ypmed.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 82.Wills TA, Cleary SD. Peer and adolescent substance use among 6th-9th graders: latent growth analyses of influence versus selection mechanisms. Health Psychol. 1999;18(5):453–463. doi: 10.1037//0278-6133.18.5.453. [DOI] [PubMed] [Google Scholar]
- 83.Pine DS, Cohen E, Cohen P, Brook J. Adolescent depressive symptoms as predictors of adult depression: moodiness or mood disorder? Am J Psychiatry. 1999;156(1):133–135. doi: 10.1176/ajp.156.1.133. [DOI] [PubMed] [Google Scholar]
- 84.Kandel DB, Davies M. Adult sequelae of adolescent depressive symptoms. Arch Gen Psychiatry. 1986;43(3):255–262. doi: 10.1001/archpsyc.1986.01800030073007. [DOI] [PubMed] [Google Scholar]
- 85.Audrain-McGovern J, Lerman C, Wileyto EP, Rodriguez D, Shields PG. Interacting effects of genetic predisposition and depression on adolescent smoking progression. Am J Psychiatry. 2004;161(7):1224–1230. doi: 10.1176/appi.ajp.161.7.1224. [DOI] [PubMed] [Google Scholar]
- 86.Audrain-McGovern J, Rodriguez D, Patel V, Faith MS, Rodgers K, Cuevas J. How do psychological factors influence adolescent smoking progression? The evidence for indirect effects through tobacco advertising receptivity. Pediatrics. 2006;117(4):1216–1225. doi: 10.1542/peds.2005-0808. [DOI] [PubMed] [Google Scholar]
- 87.Fergusson DM, Goodwin RD, Horwood LJ. Major depression and cigarette smoking: results of a 21-year longitudinal study. Psychological medicine. 2003;33(8):1357–1367. doi: 10.1017/s0033291703008596. [DOI] [PubMed] [Google Scholar]
- 88.Wellman RJ, DiFranza JR, Savageau JA, Dussault GF. Short term patterns of early smoking acquisition. Tob Control. 2004;13(3):251–257. doi: 10.1136/tc.2003.005595. [DOI] [PMC free article] [PubMed] [Google Scholar]


