Abstract
Splenic artery aneurysm is the most common visceral arterial aneurysm. Rupture of aneurysm is a rare event but associated with a high mortality. Endovascular coil embolization of bleeding splenic artery aneurysm has emerged as a promising minimal invasive treatment and considered safer than open surgery in selected patients. Nevertheless, several complications related to coils have been reported, the rarest being coil migration and erosion. We report a case of splenic artery coil migration into the stomach and its successful removal by laparoscopic endoscopy combined surgery.
INTRODUCTION
Splenic artery is the most common site of visceral aneurysms [1]. Although most patients remain asymptomatic, spontaneous rupture occurs in 22% of patients, a catastrophic event with a mortality as high as 75% in pregnant women [2]. In recent years, endovascular transcatheter coil embolization of SAA has emerged as a less invasive first line and often the definitive intervention in hemodynamic stable patients [3, 4]. Despite its success and several advantages over open surgery, endovascular coil embolization can have serious complications such as erosion or migration into gastrointestinal tract [5].
CASE REPORT
A 65 -year-old woman with a known history of multiple splenic and hepatic aneurysms was admitted to our hospital in October 2012 with acute abdomen. Abdominal computed tomography angiography showed rupture of splenic aneurysm with active extravasation of contrast and associated large left upper quadrant hematoma with small hemoperitoneum (Fig. 1). Visceral angiogram confirmed the presence of three fusiform aneurysms involving midsplenic artery (Fig. 2). The distal most aneurysm demonstrated large extravasation (Fig. 3). Coil embolization of the proximal and midsplenic artery aneurysm was performed using multiple Nester coils (Cook Medical, USA) with cessation of antegrade flow (Fig. 4). Attempt to access distal portion of the splenic artery was unsuccessful. She recovered well and was discharged 4 days later. In December 2016, she was admitted with dyspepsia and severe iron deficiency anemia requiring blood transfusion. A colonoscopy and upper endoscopy were performed which showed the presence of metallic coils in the stomach (Fig. 5). The patient subsequently underwent a combined upper endoscopy and laparoscopy. Three 5 mm ports were used to expose the lesser sac in event of hemorrhage during extraction of the coil endoscopically. An atraumatic bowel clamp was placed distal to the Treitz ligament to prevent insufflation of the small bowel. Upper endoscopy was performed using CO2 insufflation and the Nester coils were retrieved using rat tooth forceps (Fig. 6). There was no bleeding in the lesser sac after removal of the coils. A leak test was performed to rule out gastric perforation. She had an uneventful recovery and was discharged the next day.
Figure 1:

Computed tomography showed three saccular splenic artery aneurysms with a large left upper quadrant hematoma (block white arrow) and blush from distal splenic aneurysm.
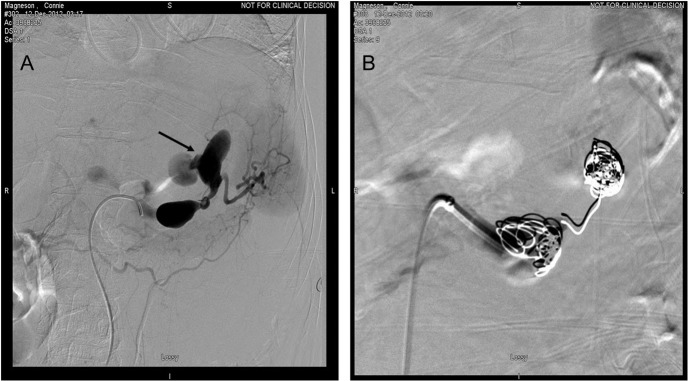
Figure 2:
(A) Visceral angiography revealed extravasation from distal saccular aneurysm (arrow). (B) Embolization of the aneurysm was done by using Nester coils.
Figure 3:

Computed tomography showing a migrated coil (arrow) in the lumen of stomach.
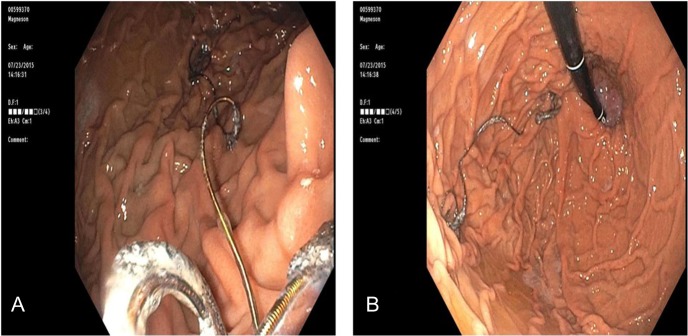
Figure 4:
(A) Endoscopy showed wire strands in the fundus of the stomach and (B) occluding the pylorus.
Figure 5:
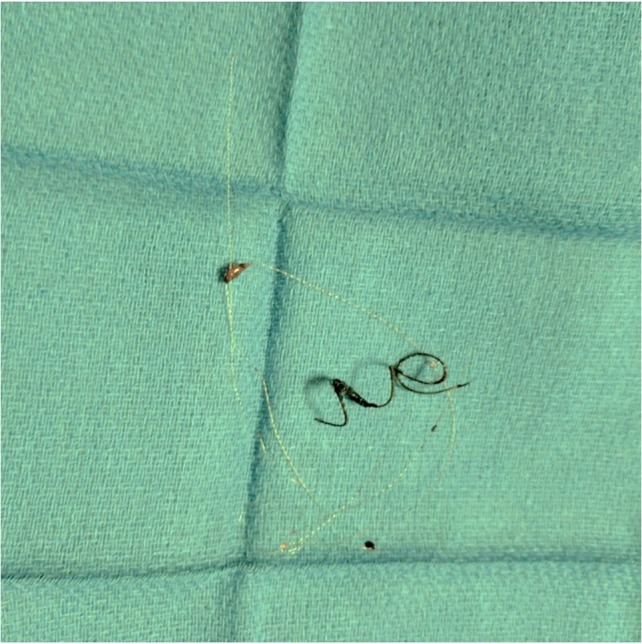
Endoscopic retrieval of coils assisted with laparoscopic visualization of lesser sac.
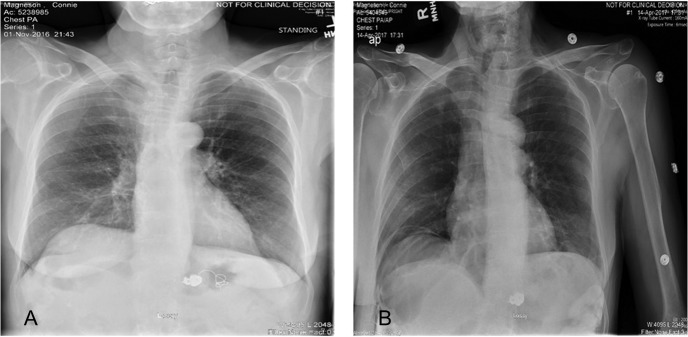
Figure 6:
(A) Plain abdominal radiograph comparing preoperative migrated coil into the stomach. (B) Postoperative film showing coil successfully retrieved.
DISCUSSION
We report a very rare and interesting case of vascular coil erosion into the stomach and its successful removal laproendoscopically. Advancements in microvascular technology have shifted the paradigm of treatment of visceral aneurysm from a traditional surgical ligation, aneurysmectomy or resection of the organ to a minimal invasive endovascular treatment with coils or covered stents. A high success rate with embolization techniques has witnessed the increasing use of coils in gastrointestinal lesions, and their associated complications. Common complications include bleeding, postembolization syndrome and infarction. Coil migration is a rare complication. To our knowledge, only 11 cases of coil migration have been reported in the English literature. Why do coils migrate? Rarity of this complication makes it difficult to answer this intriguing phenomenon. Host and procedural factors may have a role to play in coil migration and erosion. Chronic inflammation such as pancreatitis, fistulae or malignancy at the site of coil deployment or adjacent organs may incite and facilitate erosion [5, 6]. From a procedural perspective, interventionists use two main techniques for deploying coils: the ‘front and back door’ and the ‘packing’ technique; in the first coils are used to occlude the feeding and the draining arteries without deploying coils in the aneurysmal sac. In the latter, coils are deployed within the sac. Of note, in cases with large aneurysms with high flow and good collateral flow, as in our case, packing of the sac and embolization of proximal and distal feeding artery should be performed to prevent coil migration [7]. In the case described, we were unable to occlude the distal splenic artery allowing backflow via short gastric vessels and propagation of the coil toward the fundus of the stomach and subsequent erosion into the stomach. There are sparse data in the literature to make recommendations on management of eroded coils. Some coils pass spontaneously [5], some were removed endoscopically under fluoroscopic guidance [8, 9] and some necessitate a partial gastrectomy with distal pancreatectomy and splenectomy [6]. Our approach to retrieve the coil was unique in two ways. First, we used laparoscopic endoscopic combined surgery. Although some authors have reported success using endoscopy alone to remove coils, one must be cautious as unseen bleeding or perforation may ensue with endoscopic retrieval. Laparoscopy allows a minimal invasive approach to visualize the lesser sac, and control bleeding or perforation if seen on a saline leak test. Second, we used CO2 insufflation for endoscopy to minimize distention of bowel and reduce incidence of air embolism. One must monitor end tidal CO2 with this technique. In summary, we report a case of coil migration into the stomach after embolization of ruptured splenic artery aneurysm. This case shows the safety and success of laparoscopic endoscopic combined surgery for coil retrieval.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Pasha SF, Gloviczki P, Stanson AW, Kamath PS. Splanchnic artery aneurysms. Mayo Clin Proc 2007;82:472–9. [DOI] [PubMed] [Google Scholar]
- 2. Hunsaker DM, Turner S, Hunsaker JC 3rd. Sudden and unexpected death resulting from splenic artery aneurysm rupture: two case reports of pregnancy-related fatal rupture of splenic artery aneurysm. Am J Forensic Med Pathol 2002;23:338–41. [DOI] [PubMed] [Google Scholar]
- 3. Acosta S, Asciutto G. Endovascular therapy for visceral artery aneurysms. Int Angiol 2016;35:573–8. [PubMed] [Google Scholar]
- 4. Pitton MB, Dappa E, Jungmann F, Kloeckner R, Schotten S, Wirth GM, et al. Visceral artery aneurysms: Incidence, management, and outcome analysis in a tertiary care center over one decade. Eur Radiol 2015;25:2004–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Shah NA, Akingboye A, Haldipur N, Mackinlay JY, Jacob G. Embolization coils migrating and being passed per rectum after embolization of a splenic artery pseudoaneurysm, ‘the migrating coil’: a case report. Cardiovasc Intervent Radiol 2007;30:1259–62. [DOI] [PubMed] [Google Scholar]
- 6. Takahashi T, Shimada K, Kobayashi N, Kakita A. Migration of steel-wire coils into the stomach after transcatheter arterial embolization for a bleeding splenic artery pseudoaneurysm: report of a case. Surg Today 2001;31:458–62. [DOI] [PubMed] [Google Scholar]
- 7. Kasirajan K, Greenberg RK, Clair D, Ouriel K. Endovascular management of visceral artery aneurysm. J Endovasc Ther 2001;8:150–5. [DOI] [PubMed] [Google Scholar]
- 8. Mahajan A, Kumer SC, Wang AY. Electronic images of the month. Duodenal ulceration following variceal embolization with coils and vascular plugs. Clin Gastroenterol Hepatol 2010;8:e63–64. [DOI] [PubMed] [Google Scholar]
- 9. Han YM, Lee JY, Choi IJ, Kim CG, Cho S-J, Lee JH, et al. Endoscopic removal of a migrated coil after embolization of a splenic pseudoaneurysm: a case report. Clin Endosc 2014;47:183–7. [DOI] [PMC free article] [PubMed] [Google Scholar]