Abstract
Background and objectives
Patients who come for a consultation at a general practice clinic as outpatients often suffer from background anxiety and depression. The psychological state of such patients can alleviate naturally; however, there are cases when these symptoms persist. This study investigated the realities and factors behind anxiety/depression becoming prolonged.
Methods
Participants were 678 adult patients, who came to Department of General Medicine at Chiba University Hospital within a 1-year period starting from April 2012 and who completed the Hospital Anxiety and Depression Scale (HADS) during their initial consultation. Participants whose Anxiety or Depression scores in the HADS, or both, were 8 points or higher were defined as being within the anxiety/depression group, with all other participants making up the control group. A telephone interview was also conducted with participants. Furthermore, age, sex, the period from the onset of symptoms to the initial consultation at our department, the period from the initial department consultation to the telephone survey, and the existence of mental illness at the final department diagnosis were investigated.
Results
A total of 121 patients (17.8% response rate) agreed to the phone survey. The HADS score during the phone survey showed that the anxiety/depression group had a significantly higher score than the control group. The HADS scores obtained between the initial consultation and telephone survey showed a positive correlation. Logistic regression analysis extracted “age” and the “continuation of the symptoms during the initial consultation” as factors that prolonged anxiety/depression.
Conclusion
Anxiety and depression in general practice outpatients have the possibility of becoming prolonged for an extended period of time. Being aged 65 years or over and showing a continuation of symptoms past the initial consultation are the strongest factors associated with these prolonged conditions. When patients with anxiety and depression exhibit these risk factors, they should be further evaluated for treatment.
Keywords: anxiety, depression, outpatients, general practice
Background and objectives
Anxiety and depression are symptoms that are frequently encountered among primary care and general practice outpatients. Anxiety is the normal reaction to threat, but can become pathological if the reaction is too excessive, persists for too long or deteriorates over time, and is accompanied by severe physical symptoms. Depression is defined as mood disturbance. The frequencies of major depressive disorders and anxiety disorders in a primary care clinic within Japanese urban areas are 3.7% and 4.6%, respectively.1 This report shows the frequencies of clear-cut depression and anxiety disorders meeting diagnostic standards and that there is a possibility that there are even more so-called “mild cases” that do not meet the diagnostic standards. In reality, patients who suffer from anxiety or depression have physical symptoms, rather than mental symptoms, that appear on the forefront. As such, it is not rare for such patients to consult the department for physical medicine rather than a psychiatric department in an outpatient clinic. According to research by Lépine et al,2 57% of patients who exhibited depression consulted a medical institution. Of these, 51% consulted a primary care physician and 12% consulted an expert at a department of physical medicine.2 Even in Japan, 3.7% of first-time patients presenting at a primary care clinic – that is not indicated to be a psychiatric clinic – suffer from a major depressive disorder, and the main reason for their visit is actually physical symptoms such as general fatigue.1 Depression and anxiety deteriorate quality of life and can amplify patients’ physical complaints3 as well as increase medical fees.4 As such, it is very important to detect the existence of anxiety and depression among patients who consult the outpatient department of a primary care or general practice clinic when claiming to suffer from physical complaints.
On the other hand, anxiety/depression patients who do not meet the diagnostic criteria of major depressive disorder and generalized anxiety disorder have the possibility of recovering naturally, compared to patients who satisfy the diagnostic standard for major depressive disorders and generalized anxiety disorders. Concerning depression, a study that considered the general community showed that no symptom was seen in the follow-up study 3 years later. In total, 57.4% of asymptomatic patients at follow-up had major depressive disorders, and 76% patients with latent depression showed psychological symptoms at a level that did not satisfy the diagnostic standards for major depressive disorders.5 Concerning anxiety, in a follow-up research study of patients who sought consultation as a primary care outpatient clinic, for generalized anxiety disorders – the most severe and common type of anxiety disorder – 43% of the patients showed no symptoms 5 years later. By contrast, 58% of those with anxiety disorders did not satisfy the diagnostic standard for a particular illness.6 However, in our experience, it is not rare to encounter depression and anxiety that are prolonged for an extended period of time. Regarding the factors affecting why anxiety and depression become prolonged for an extended period of time, there have been studies by Pietrzak et al5 and Jackson et al,6 who looked at the relationship between the level of anxiety and depression. However, we were not able to find research studies that looked into other factors. In the present study, the realities and factors in which anxiety and depression become prolonged among first-time patients of general practice outpatient care were researched and examined.
Methods
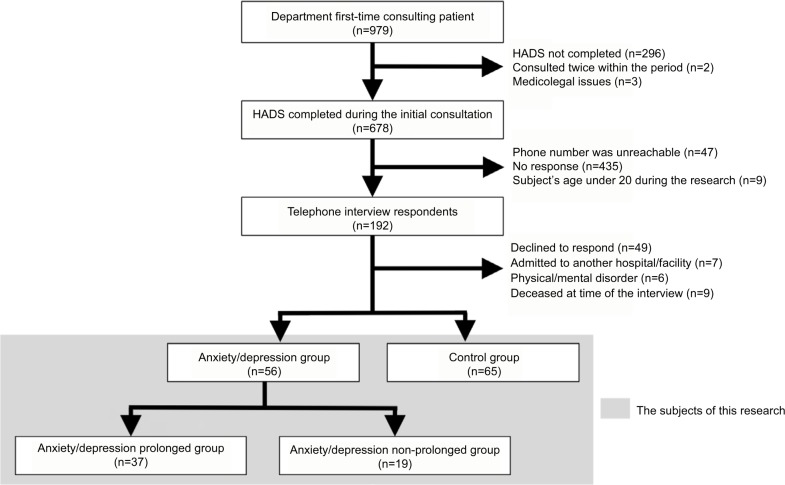
Research participants (Figure 1)
Figure 1.
Outline of the respondents.
Abbreviation: HADS, Hospital Anxiety and Depression Scale.
Of the total 979 first-time patients who received consultation in Department of General Medicine of Chiba University Hospital (hereinafter “the Department”) between April 2012 and March 2013, 680 participants (69.5%) were selected after excluding 296 patients who did not complete the Hospital Anxiety and Depression Scale (HADS).7 Three other patients who had medicolegal troubles in their medical record were excluded because the legal department intervenes in such cases, and we wanted to prevent any further legal disputes by involving them in the study. Furthermore, there were 2 patients who had visited the Department two or more times within the corresponding period, with all these consultations being their second consultation. With these patients, only the first consultation was counted. As such, 678 participants (69.3%) became the official study participants. We obtained comprehensive consent for utilizing the medical records of the participants for the study at their first medical examination. This study was conducted after obtaining approval from the Ethics Committee of Chiba University Graduate School of Medicine.
When a patient answered the telephone call for the survey, we explained the survey again and only the patients who agreed to take part were included in the survey. There was one person who refused to cooperate in this research for fears of personal information being leaked. Patient anonymity and confidentiality were respected throughout the study, despite fears among the Japanese population of personal information being disseminated. In addition, those who 1) did not add a contact telephone number on the medical record; 2) declined to respond; 3) had passed away; 4) were admitted to another hospital; or 5) could not respond owing to problems with physical/mental faculties were excluded from the analysis.
Research setting
Chiba University Hospital is a flagship hospital that is located in central Chiba, which is located approximately 40 km away from the nation’s capital, Tokyo, and has a population of approximately 1 million people. Our Department conducts consultations of cases that cannot be diagnosed in other hospitals. At the time of the research, the referral rate was approximately 90%, with the diagnosis concordance rate between the Department’s diagnosis and the specialist department within the hospital being 82%.8 In the Department, a HADS score is given to all first-time patients as a screening procedure for anxiety and depression.
Research design
This study was designed as a longitudinal cohort study (Figure 1). A telephone survey was conducted with participants where at least 3 years had passed from their initial consultation. The telephone survey was conducted by one of the principal authors, the research representative, to minimize the difference in the interpretation of the patient’s responses. Furthermore, the participants’ intentions for participating in the research study were confirmed at the start of the telephone survey after verbally explaining the study.
The items displayed in Table 1 were investigated with regard to the participants. The survey items were believed to impact the prolonging of anxiety and depression, as determined by a literature search and focus group discussion. Patients with an A score, D score, or both scores of 8 points or higher during the initial HADS testing consultation were defined as the anxiety/depression group; all other patients were defined as the control group. The participants from the anxiety/depression group that still had a high HADS score (ie, 8 or higher for the A score, D score, or both) during the telephone survey (hereinafter, “telephone survey HADS”), were defined as the “anxiety/depression prolonged group”, while all the other participants belonged to the “depression/anxiety non-prolonged group”. A multiple logistic regression analysis was conducted by using the anxiety/depression prolonged group and depression/anxiety non-prolonged group as the dependent variables, while the medical record and the telephone survey items (excluding the telephone survey HADS) were the independent variables used to examine the factors behind the prolongation of the anxiety/depression.
Table 1.
Survey item at each stage
| During initial consultation | Medical record | During telephone interview |
|---|---|---|
| HADS | Age | HADS |
| Sex | Presence of new symptoms/diseases after having consulted with the Department | |
| Number of days from the initial consultation to the telephone survey (range) | Continued presence of symptoms which the subject complained about during the initial consultation | |
| The period from the onset of symptoms present at the initial consultation to the initial consultation (%) | Has the participant been “doctor shopping” after our examination? | |
| ICPC-2 Code P status during the final diagnosis at the Department |
Abbreviations: HADS, Hospital Anxiety and Depression Scale; ICPC-2, International Classification of Primary Care revised second edition.
Survey during the first consultation
HADS can simultaneously evaluate anxiety and depression and comprises question items that are unlikely to be impacted by physical symptoms. A Japanese edition has been developed and its reliability and validity have been validated.9,10 Concerning the HADS cutoff value, Bjelland et al11 reported that if a score of 8 points was used as a cutoff point, sensitivity and specificity were reported to be approximately 80%.11 Based on the report of Bjelland et al,11 this study defined participants that had either an A score, D score, or both scores, of 8 points or higher as an anxiety/depression group; all other participants were defined as the control group.
Research of the medical records
Age, sex, the period between the initial consultation at the Department and the telephone survey, the period from the onset of illness to the initial consultation at the Department, and the existence of mental illness during the final diagnosis at the Department were investigated. The existence of mental illness during the final diagnosis at the Department was extracted from the medical records, which contained the diagnosis, as determined by a team comprising one physician with 3–5 years of clinical experience who was in charge of the initial consultation and 1–2 medical advisors with 6 or more years of clinical experience. It was then coded using the International Classification of Primary Care revised second edition (ICPC-2).12 Owing to the properties of this coding, if a patient suffers from multiple illnesses, multiple ICPC-2 codes will be given to a single patient. In this study, therefore, a patient who suffered from psychological/psychiatric illness (Code P) during the final diagnosis was viewed as a “patient with mental illness during the final diagnosis at the Department.” The diagnosis of mental illness was conducted based on the Diagnostic and Statistical Manual of Mental Disorders-IV Text Edition.13
Telephone survey
The participants were contacted using the phone numbers listed on their medical records. The HADS scoring during the telephone survey used a similar cutoff as the initial consultation HADS, with participants having 8 points or higher for an A score, D score, or both scores defined as belonging to the “anxiety/depression prolonged group” with all other patients defined as the “anxiety/depression non-prolonged group.”
The behavior of browsing and selecting doctors (so-called “doctor shopping”) as described in previous Japanese studies14 is stipulated to include consulting three or more medical institutions regarding the same symptom. In this study, if a patient consulted two or more medical institutions for the same symptom, present during their initial consultation, without referral from the Department, or in other words if the patient consulted three or more institutions including the Department, it was defined as doctor shopping behavior. Since the vague recollection can be eliminated as much as possible by limiting the time period, and doctor shopping behavior within the preceding 1-year period may have continued even at the time of the research, doctor shopping behavior within 1 year from the research period was investigated. The emergence of new symptoms/illness was defined as a symptom/function disorder that emerged after the initial consultation and continued even at the time of the research. Concerning the existence of symptoms that the participants complained of during their initial consultation, the participants were asked if these complaints persisted during the telephone survey.
Statistical analysis
The comparison between the anxiety/depression group and the control group on the baseline characteristics and the survey items were evaluated using Fisher’s exact test and Mann-Whitney U-test. To examine the change between the initial HADS and telephone survey HADS for the same subject, a Spearman’s correlation coefficient was calculated for the correlation between the initial and telephone survey HADS scores.
The comparison between the anxiety/depression prolonged group and the anxiety/depression non-prolonged group was done using Fisher’s exact test. In the multivariate logistic regression analysis, we included only independent variables that were P<0.15 in the univariate analysis. Furthermore, before the analysis, an examination was conducted using variance inflation factor (VIF) to confirm the assumption of multicollinearity.
All statistical analyses were conducted using Easy R (EZR) with the significance interval of each analysis set under 5%. EZR is a freeware program developed by using R, statistical analysis software, as its foundation. As such, its fundamental properties correspond to R.15 R is used widely for academic research purposes and has a high reliability.16
Results
Respondent outline
Of the 678 participants, 192 participants (28.3%) responded to the phone calls (Figure 1). We excluded 47 participants who did not use the telephone number provided and the 493 participants who did not respond due to reasons such as not being able to answer the phone. Of the 192 participants who responded, 48 participants declined to respond, 9 had passed away at the time of the research, 7 had been admitted to another hospital/facility, and 6 could not respond owing to their physical and mental condition at the time of the phone call; all these participants were excluded. As a result, valid responses were obtained from 121 participants (17.8%, 54 males, 67 females, mean age: 69.0 years).
Fifty-six out of the 121 participants belonged to the anxiety/depression group (46.3%, mean age: 67.5 years), with the control group having 65 participants (53.7%, mean age: 70.0 years). Of the 56 participants in the anxiety/depression group, 37 belonged to the anxiety/depression prolonged group (66.1%) and 19 to the anxiety/depression non-prolonged group (33.9%).
Results of the patient background factor and each research item
No significant difference between the two groups was found in terms of patient background factors (Table 2).
Table 2.
Baseline characteristics of each group (n=121)
| Factor | Anxiety/Depression (n=56) | Control (n=65) | P-value | |
|---|---|---|---|---|
| Age, n (range) | 67.5 (30–87) | 70.0 (21–86) | 0.307 | |
| Age, n (%) | ≥65 years | 33 (58.9) | 46 (70.8) | 0.186 |
| Sex, n (%) | Female | 35 (62.5) | 32 (49.2) | 0.199 |
| Number of days from the initial consultation to the telephone survey, n (range) | 1094.5 (1007–1295) | 1093.0 (981–1332) | 0.956 | |
| The period from the onset of symptoms present at the initial consultation to the initial consultation, n (%) | Chronic | 50 (89.3) | 51 (79.7) | 0.211 |
The anxiety/depression group had a significantly higher percentage of people who included mental illness (the anxiety/depression prolonging group [Table 3]) in their final diagnosis compared to the control group (P=0.012, P<0.001). No significant difference between the two groups was found for other items.
Table 3.
Results of evaluation items (n=121)
| Factor | Anxiety/Depression (n=56) | Control (n=65) | P-value | |
|---|---|---|---|---|
| Doctor shopping behavior, n (%) | Yes | 9 (16.1) | 4 (6.2) | 0.139 |
| Final diagnosis of our department, n (%) | Code P (+) | 25 (44.6) | 15 (22.7) | 0.012* |
| New symptoms or disease, n (%) | Emergence | 26 (46.4) | 29 (44.6) | 0.857 |
| Symptom at the time of the first medical examination, n (%) | Persistence | 30 (46.4) | 38 (58.5) | 0.713 |
| HADS score from the telephone survey, n (%) | High | 37 (66.1) | 15 (23.1) | <0.001* |
Note:
P<0.05.
Abbreviation: HADS, Hospital Anxiety and Depression Scale.
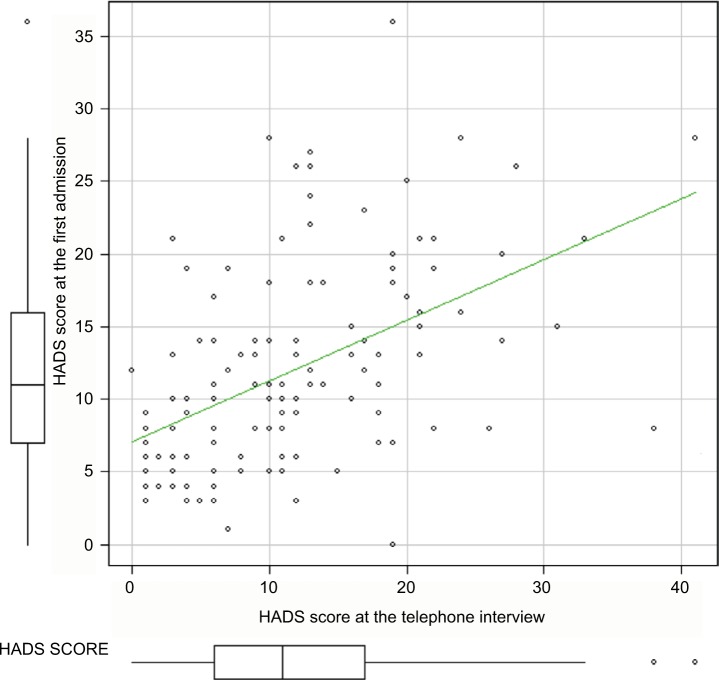
The relationship between the initial consultation HADS and the telephone survey HADS
The median of the telephone survey HADS (25 percentile [Q1], 75 percentile [Q3]) for the anxiety/depression group (15 points, Q1: 10.0 points, Q3: 20.3 points) was significantly higher than that of the control group (7 points, Q1: 4.0 points, Q3, 12.0 points) (P<0.001). A significant correlation was found between the telephone survey HADS and the initial consultation HADS (Figure 2, correlation coefficient: 0.53, P<0.001).
Figure 2.
Correlation between the initial consultation and the telephone survey.
Abbreviation: HADS, Hospital Anxiety and Depression Scale.
Factors that impact the prolongation of anxiety/depression
Concerning the survey items on the medical records and phone survey (excluding the telephone survey HADS), a comparative examination between the two groups – the anxiety/depression prolonged group and the anxiety/depression non-prolonged group – was conducted. Factors that were P<0.15 in the univariate analysis included (Table 4), “Age (65 years and older) (VIF: 1.178),” the presence of “Doctor shopping (VIF: 1.005),” and “The continuation of the initial symptom (VIF: 1.176)” all had a VIF of under 2 and did not show a strong line-type relationship. Therefore, these three variables were all used as independent variables in the multivariate logistic regression analysis. As a result, “Age (65 years old and above)” (odds ratio [OR]: 4.36, 95% confidence interval [CI]: 1.16–16.40) and “The remaining symptoms during the initial consultation” (OR: 5.72, 95% CI: 1.51–21.70) were extracted as the protraction of anxiety/depression.
Table 4.
Impact of factors on prolongation of anxiety/depression
| Univariate analysis
| ||
|---|---|---|
| Factors | Prolongation rate | P-value |
| Age | ||
| ≥65 years | 75.8% | 0.089 |
| <65 years | 52.2% | |
| Sex | ||
| Female | 62.9% | 0.572 |
| Male | 71.4% | |
| Duration of disease | ||
| Acute | 40.0% | 0.324 |
| Chronic | 68.6% | |
| Doctor shopping-behavior | ||
| No | 61.7% | 0.146 |
| Yes | 88.9% | |
| Final diagnosis | ||
| Code P (−) | 61.3% | 0.571 |
| Code P (+) | 72.0% | |
| New symptoms | ||
| None | 60.0% | 0.399 |
| Emergence | 73.1% | |
| Past symptoms | ||
| Persistence | 80.0% | 0.025 |
| Disappear | 50.0% | |
|
| ||
| Multivariate analysis | Odds ratio (95% CI) | P-value |
|
| ||
| Age | ||
| ≥65 years | 4.360 (1.16–16.40) | 0.029 |
| <65 years | 1 | |
| Past symptoms | ||
| Persistence | 5.720 (1.51–21.70) | 0.010 |
| Disappear | 1 | |
Discussion
This study showed that 66% of the depression/anxiety group displayed anxiety/depression similarly during the telephone survey as during the initial consultation. This number is slightly higher compared to that found in preceding research studies.5,6,17 The study by Forsell17 examined participants who were 64 years old or younger; in Pietzak et al’s study,5 82.5% of participants were 64 years old or younger; and in Jackson et al’s6 study the mean age of participants was 55 years. Compared to these studies, the mean age of the anxiety/depression group of this study was high, at ~67.5 years. As will be mentioned later, there is a possibility that anxiety/depression is prolonged among the elderly. The fact that the participants’ mean age was high could be a reason why the percentage of those with prolonged anxiety/depression was higher in this study compared to previous studies.
In this study, age (65 years and above) was extracted as a factor influencing anxiety/depression prolongation. Sub-threshold depression among the elderly is two to three times more common compared to a major depressive disorder, with such depression progressing to a major depressive disorder at a frequency of 8–10% a year.18 Furthermore, depression that has developed at 65 years or older, compared to depression that has developed at a younger age, is more likely to be accompanied by an anxiety disorder19 with higher relapse rates20 and higher severity levels.21 These could be attributed as reasons as to why the anxiety and depression of the elderly were prolonged. Therefore, when giving medical consultations to the elderly, treatment that considers properties such as conducting early treatment interventions against anxiety/depression is believed to be important.
Another independent factor that was identified as responsible for prolonged anxiety/depression was the “continuation of symptoms during the initial consultation.” There is no doubt that an accurate diagnosis that recommends an appropriate existing treatment method will alleviate symptoms if the treatments are proven to be effective. However, it is also a fact that even if an appropriate diagnosis has been given, there are illnesses in which symptom alleviation is difficult. For example, for mental illnesses, patients with physically manifesting disorders may believe that their symptoms are caused by an organic disease and have difficulties accepting that they suffer from a mental illness22 and are prone to have their condition protracted.23 Even if the patients suffered from an organic disease, a dramatic improvement of symptoms would be difficult with functional disorders and degenerative diseases. With these illnesses, special interventions, such as cognitive behavioral therapy, are necessary.
The limitations of this research and future tasks
This study employed a telephone interview method mainly because it limited cost. However, the response rate to the telephone interview was low and there is the possibility of bias in the results. Various factors can be attributed to the low response rate. Firstly, the interview time window was limited from 9 AM to 8 PM, which resulted in a poor response rate from employed individuals (in particular, the younger demographic). This time frame may coincide with their working hours. Secondly, there were a few cases in which the participants had changed their phone number within the period of a little over 3 years. As a result of competition between phone carriers in Japan, people often change their phone numbers. This may have been a factor that resulted in many people not responding. Thirdly, the telephone interviews were performed by the lead author alone and the author was not able to call back everyone who did not respond as there was no time. The following are possible measures that can be taken in the future:
Heighten the convenience for the respondents by allowing responses to the survey via mail and the Internet.
Consider providing incentives to those cooperating in the research, such as sending a compensatory gift, to attempt to improve the response rate.
A task for the future includes intervention research on anxiety/depression during the initial consultation. An intervention study for anxiety and depression detected at the initial consultation is also necessary. Regarding the effect of the intervention on psychiatric problems in primary care settings, there is a report that both medication and cognitive and behavioral therapies are effective with regard to depression,24–26 panic disorder,27 anxiety,28 insomnia,29 chronic fatigue,30 and somatoform disorder.31 However, with respect to the treatment for anxiety and depression including physical disorders, no studies have been found in the literature. In this study, we showed that the factors influencing anxiety and depression and their prolongation were being of older age and having symptoms at the initial consultation. Therefore, in the future, it will be necessary to examine elderly and patients who have difficulty recovering from the symptoms.
A possible subject for future studies may be the development of simple and easy tools to detect anxiety and depression. According to Whooley et al reported,32 depression screening method comprised only two questions about mood and enjoyment that are known to have excellent sensitivity and specificity for the screening of depression. However, there is currently no quick screening method for anxiety that can be used during medical history taking. To detect these in the psychological history, it is important that the doctor makes efforts to discover these. However, it is difficult in busy outpatient settings to spare the time for psychiatric problems. A questionnaire method should not be used thoughtlessly as patients might begin to think that they have a mental illness. Hence questionnaires should be explained with care. The development of a quick screening method for anxiety and depression that is useful in medical interviews is expected.
Conclusion
Anxiety/depression in general practice outpatients has the possibility of being prolonged for an extended period. Being aged 65 or over and exhibiting symptoms during the initial consultation were found to be factors affecting symptom prolongation. When these factors are demonstrated among patients with anxiety and depression, further studies for this treatment are necessary.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Yamada K, Nishimura M, Ono M, et al. Mental illness in a family practice: prevalence and patient complaints. Jpn J Gen Hosp Psychiatry. 2004;16(1):18–23. [Google Scholar]
- 2.Lépine JP, Gastpar M, Mendlewicz J, Tylee A. Depression in the community: the first pan-European study DEPRES (Depression Research In European Society) Int Clin Psychopharmacol. 1997;12(1):19–29. [PubMed] [Google Scholar]
- 3.Barsky AJ, Goodson JD, Lane RS, Cleary PD. The amplification of somatic symptoms. Psychosom Med. 1988;50(5):510–519. doi: 10.1097/00006842-198809000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Katon WJ, Lin E, Russo J, Unutzer J. Increased medical costs of population-based sample of depressed elderly patients. Arch Gen Psychiatry. 2003;60(9):897–903. doi: 10.1001/archpsyc.60.9.897. [DOI] [PubMed] [Google Scholar]
- 5.Pietrzak RH, Kinley J, Afifi TO, Enns MW, Fawcett J, Sareen J. Subsyndromal depression in the United States: prevalence, course, and risk for incident psychiatric outcomes. Psychol Med. 2013;43(7):1401–1414. doi: 10.1017/S0033291712002309. [DOI] [PubMed] [Google Scholar]
- 6.Jackson JL, Passamonti M, Kroenke K. Outcome and impact of mental disorders in primary care at 5 years. Psychosom Med. 2007;69(3):270–276. doi: 10.1097/PSY.0b013e3180314b59. [DOI] [PubMed] [Google Scholar]
- 7.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 8.Graduate School of Medicine and School of Medicine, Chiba University, Medical School, Medical Department-Affiliated Hospital Achievement List, 2012 Graduate School of Medicine and School of Medicine, Chiba University, Medical Department-Affiliated Hospital. 2014:151–154. [Google Scholar]
- 9.Kitamura T. The Hospital Anxiety and Depression Scale (HADS) Arch Psychiatr Diagn Clin Eval. 1993;4:371–372. [Google Scholar]
- 10.Kugaya A, Akechi T, Okuyama T, Okamura H, Uchitomi Y. Screening for psychological distress in Japanese cancer patients. Jpn J Clin Oncol. 1998;28(5):333–338. doi: 10.1093/jjco/28.5.333. [DOI] [PubMed] [Google Scholar]
- 11.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52(2):69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization . ICPC-2; WONCA International Classification Committee: International Classification of Primary Care Revised Second Edition. Geneva: 2005. [Accessed December 4, 2017]. Available from: http://www.who.int/classifications/icd/adaptations/icpc2/en/ [Google Scholar]
- 13.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR. (Text Revision) Washington, D.C: American Psychiatric Association; 2000. [Google Scholar]
- 14.Sato T, Takeichi M, Shirahama M, Fukui T, Gude JK. Doctor-shopping patients and users of alternative medicine among Japanese primary care patients. Gen Hosp Psychiatry. 1995;17(2):115–125. doi: 10.1016/0163-8343(94)00094-t. [DOI] [PubMed] [Google Scholar]
- 15.Kanda Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 2013;48(3):452–458. doi: 10.1038/bmt.2012.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Development Core R. Team R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2011. [Google Scholar]
- 17.Forsell Y. A three-year follow-up of major depression, dysthymia, minor depression and subsyndromal depression: results from a population-based study. Depress Anxiety. 2007;24(1):62–65. doi: 10.1002/da.20231. [DOI] [PubMed] [Google Scholar]
- 18.Meeks TW, Vahia IV, Lavretsky H, Kulkarni G, Jeste DV. A tune in “a minor” can “b major”: a review of epidemiology, illness course, and public health implications of subthreshold depression in older adults. J Affect Disord. 2011;129(1–3):126–142. doi: 10.1016/j.jad.2010.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brown RP, Sweeney J, Loutsch E, Kocsis J, Frances A. Involutional melancholia revisited. Am J Psychiatry. 1984;141(1):24–28. doi: 10.1176/ajp.141.1.24. [DOI] [PubMed] [Google Scholar]
- 20.Mitchell AJ, Subramaniam H. Prognosis of depression in old age compared to middle age: a systematic review of comparative studies. Am J Psychiatry. 2005;162(9):1588–1601. doi: 10.1176/appi.ajp.162.9.1588. [DOI] [PubMed] [Google Scholar]
- 21.Kessing LV. Differences in diagnostic subtypes among patients with late and early onset of a single depressive episode. Int J Geriatr Psychiatry. 2006;21(12):1127–1131. doi: 10.1002/gps.1617. [DOI] [PubMed] [Google Scholar]
- 22.Epstein RM, Quill TE, McWhinney IR. Somatization reconsidered: incorporating the patient’s experience of illness. Arch Intern Med. 1999;159(3):215–222. doi: 10.1001/archinte.159.3.215. [DOI] [PubMed] [Google Scholar]
- 23.Jackson JL, Kroenke K. Prevalence, impact and prognosis of multisomatoform disorder in primary care: a 5-year follow-up study. Psychosom Med. 2008;70(4):430–434. doi: 10.1097/PSY.0b013e31816aa0ee. [DOI] [PubMed] [Google Scholar]
- 24.Conradi HJ, de Jonge P, Kluiter H, et al. Enhanced treatment for depression in primary care: long-term outcomes of a psycho-educational prevention program alone and enriched with psychiatric consultation or cognitive behavioral therapy. Psychol Med. 2007;37(6):849–862. doi: 10.1017/S0033291706009809. [DOI] [PubMed] [Google Scholar]
- 25.Serfaty MA, Haworth D, Blanchard M, Buszewicz M, Murad S, King M. Clinical effectiveness of individual cognitive behavioral therapy for depressed older people in primary care: a randomized controlled trial. Arch Gen Psychiatry. 2009;66(12):1332–1340. doi: 10.1001/archgenpsychiatry.2009.165. [DOI] [PubMed] [Google Scholar]
- 26.Wiles N, Thomas L, Abel A, et al. Cognitive behavioural therapy as an adjunct to pharmacotherapy for primary care based patients with treatment resistant depression: results of the CoBalT randomised controlled trial. Lancet. 2013;381(9864):375–384. doi: 10.1016/S0140-6736(12)61552-9. [DOI] [PubMed] [Google Scholar]
- 27.Roy-Byrne PP, Craske MG, Stein MB, et al. A randomized effectiveness trial of cognitive-behavioral therapy and medication for primary care panic disorder. Arch Gen Psychiatry. 2005;62(3):290–298. doi: 10.1001/archpsyc.62.3.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stanley MA, Wilson NL, Novy DM, et al. Cognitive behavior therapy for generalized anxiety disorder among older adults in primary care: a randomized clinical trial. JAMA. 2009;301(14):1460–1467. doi: 10.1001/jama.2009.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Edinger JD, Sampson WS. A primary care “friendly” cognitive behavioral insomnia therapy. Sleep. 2003;26(2):177–182. doi: 10.1093/sleep/26.2.177. [DOI] [PubMed] [Google Scholar]
- 30.Godfrey E, Chalder T, Ridsdale L, Seed P, Ogden J. Investigating the active ingredients of cognitive behaviour therapy and counselling for patients with chronic fatigue in primary care: developing a new process measure to assess treatment fidelity and predict outcome. Br J Clin Psychol. 2007;46(Pt 3):253–272. doi: 10.1348/014466506X147420. [DOI] [PubMed] [Google Scholar]
- 31.Escobar JI, Gara MA, Diaz-Martinez AM, et al. Effectiveness of a time-limited cognitive behavior therapy type intervention among primary care patients with medically unexplained symptoms. Ann Fam Med. 2007;5(4):328–335. doi: 10.1370/afm.702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Whooley MA, Avins AL, Miranda J, Browner WS. Case-finding instruments for depression. Two questions are as good as many. J Gen Intern Med. 1997;12(7):439–445. doi: 10.1046/j.1525-1497.1997.00076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]