In adolescents undergoing bariatric surgery, girls, those with greater weight loss, and younger individuals had greater improvements in multiple CVD-RFs.
Abstract
BACKGROUND AND OBJECTIVES:
Severely obese adolescents harbor numerous cardiovascular disease risk factors (CVD-RFs), which improve after metabolic and bariatric surgery (MBS). However, predictors of change in CVD-RFs among adolescents have not yet been reported.
METHODS:
The Teen-Longitudinal Assessment of Bariatric Surgery study (NCT00474318) prospectively collected anthropometric and health status data on 242 adolescents undergoing MBS at 5 centers. Predictors of change in CVD-RFs (blood pressure, lipids, glucose homeostasis, and inflammation) 3 years after Roux-en-Y gastric bypass and vertical sleeve gastrectomy were examined.
RESULTS:
The mean (±SD) age of participants at baseline was 17 ± 1.6 years; 76% were girls, and 72% were white, with a median BMI of 51. Participants underwent Roux-en-Y gastric bypass (n = 161), vertical sleeve gastrectomy (n = 67), or adjustable gastric banding (n = 14). Increasing weight loss was an independent predictor of normalization in dyslipidemia, elevated blood pressure (EBP), hyperinsulinemia, diabetes, and elevated high-sensitivity C-reactive protein. Older participants at time of surgery were less likely to resolve dyslipidemia compared with younger participants, whereas girls were more likely than boys to demonstrate improvements in EBP. Even those participants without frank dyslipidemia or EBP at baseline showed significant improvements in lipid and blood pressure values over time.
CONCLUSIONS:
Numerous CVD-RFs improve among adolescents undergoing MBS. Increased weight loss, female sex, and younger age predict a higher probability of resolution of specific CVD-RFs. The elucidation of predictors of change in CVD-RFs may lead to refinements in patient selection and optimal timing of adolescent bariatric surgery designed to improve clinical outcomes.
What’s Known on This Subject:
Severely obese adolescents, like adults, suffer from numerous comorbid health conditions. Bariatric surgery is safe and effective in severely obese adolescents and should be considered as a valid treatment of those in whom lifestyle interventions are not successful.
What This Study Adds:
Analysis from the largest prospective study of adolescent bariatric surgery outcomes offers important insights regarding previously unknown predictors of change in cardiovascular risk factors, which may promote future refinements in patient selection and the optimization of the timing of surgery.
Severe obesity threatens the health of 4% to 7% of the pediatric population in the United States,1–3 as evidenced by data highlighting associations with increased prevalence of cardiovascular disease risk factors (CVD-RFs), including hypertension, dyslipidemia, and type 2 diabetes along with evidence of associated end-organ damage.4–6 In conjunction with obesity-related disorders among adolescents with class 2 obesity (BMI ≥120% of the 95th percentile) or higher, there has been a rise in the use of metabolic and/or bariatric surgery (MBS) as a primary therapeutic intervention. With a doubling of procedural prevalence since the early 2000s, researchers in US literature estimate that ∼1600 adolescents undergo MBS annually.7 In contrast with the large body of adult literature, studies in which researchers examine the predictors of changes in CVD-RFs among adolescents undergoing MBS are lacking and could be of value when considering the risk/benefit balance of surgical treatment.
To address these knowledge gaps, data from the Teen-Longitudinal Assessment of Bariatric Surgery (Teen-LABS) study were used to examine predictors of change in cardiovascular disease (CVD) risk. We hypothesized that baseline characteristics (ie, age, sex, anthropomorphic measures, and ethnicity) may predict a differential response of CVD-RFs to adolescent MBS.
Methods
Study Design and Subjects
Teen-LABS (NCT00465829) design and methodology have been previously described.8,9 By using consensus guidelines, consecutive adolescents (<19 years old and Tanner Stage 4 or higher) with class 2 obesity or higher (BMI ≥35) and comorbid disease were considered eligible for MBS and study enrollment at 1 of 5 centers (February 28, 2007–December 30, 2011).1,3,10 The study protocol, data- and safety-monitoring plans, and assent and/or consent forms were approved by all institutional review boards and an independent data- and safety-monitoring board.
Collection of Data
Baseline (≤30 days presurgery) and follow-up data were collected at 6 months, 1 year, 2 years, and 3 years, as described.5,9,11,12 The majority of postoperative research visits (89%) occurred at Teen-LABS centers, with 8% occurring in participants’ homes (by using field examiners) or by collection of self-reported data (3%) by using telephone interviews and/or electronic communication. Standard definitions were employed to determine the presence or absence of comorbidities by using participant interviews, physical examinations, medical record review, and laboratory results. Data were maintained in a central database at the data-coordinating center.
Definitions
Previously reported definitions of the prevalence, remission, and incidence of CVD-RFs (dyslipidemia, elevated blood pressure [EBP], prehypertension, and type 2 diabetes) were used and adjusted to account for each participant’s age during follow-up for CVD-RFs with age-specific cutpoints (adolescents versus adults).5,13 Although potentially introducing bias, we decided to employ categorical analysis based on well-established, age-dependent cutpoints to provide relevance to published clinical guidelines in the context of a cohort transitioning into adulthood. Also, this approach will assist in future analyses, at which time a full transition of the cohort into adulthood will be complete. CVD-RF remission rates were calculated as the percentage of participants (with evaluable data) who did not have the clinical condition at each postoperative time point among those with the condition at baseline. CVD-RF incidence was calculated as the percentage of participants with the condition at each postoperative visit among those without the baseline condition. Composite scoring (the CVD-RF total) was employed by using equally weighted CVD-RFs (EBP, dyslipidemia, diabetes mellitus, and elevated high-sensitivity C-reactive protein [hs-CRP]).5 Participants were scored as having dyslipidemia if they had elevated low-density lipoprotein cholesterol (LDL-C) or fasting triglycerides, low high-density lipoprotein cholesterol (HDL-C), or were using lipid-lowering medications. For participants <21 years old, triglyceride ≥130 mg/dL, LDL-C ≥130 mg/dL, or high HDL-C <40 mg/dL were considered abnormal. For those >21 years old, triglyceride ≥200 mg/dL, LDL-C ≥160 mg/dL, or HDL-C <40 mg/dL (men) and <50 mg/dL (women) were considered abnormal. Dyslipidemia remission for participants <21 years old was defined as triglyceride <130 mg/dL, LDL-C <130 mg/dL, HDL-C ≥40 mg/dL, and an absence of lipid-lowering medications. Remission for participants >21 years old was defined as triglyceride <200 mg/dL, LDL-C <160 mg/dL, HDL-C ≥40 mg/dL (men) or HDL-C ≥50 mg/dL (women), and an absence of lipid-lowering medication. Abnormal thresholds for triglyceride–to–HDL-C ratios were defined as ≥3.0 for non-black and ≥2.5 for black participants.14–16 Average systolic blood pressure (SBP) and diastolic blood pressure (DBP) (≥2 separate measurements) were obtained by using a Welch Allyn Spot Vital Signs Monitor (4200B). EBP was defined as SBP or DBP ≥95th percentile for age, sex, and height for subjects <18 years old or SBP ≥140 mm Hg or DPB ≥90 mm Hg for those ≥18 years old. Irrespective of age, EBP was assigned to those who were using antihypertensive medications. Because measurements were obtained at 1 occasion rather than multiple, separate occasions, the term hypertension is replaced by EBP. Normalization of EBP was defined as SBP and DBP within the defined normal range for age without antihypertensive medications. Impaired fasting glucose (IFG) was defined as glucose ≥100 mg/dL. Diabetes was defined by using self-reported diagnoses, medical record review, medication use for the treatment of diabetes (excluding metformin with a concomitant diagnosis of polycystic ovary syndrome), hemoglobin A1c (HbA1c) ≥6.5%, IFG ≥126 mg/dL, or 2-hour oral glucose tolerance test results ≥200 mg/dL within 2 weeks before enrollment.17 Fasting insulin, HbA1c, and hs-CRP were abnormal at >17 µU/mL, ≥6.5%, and ≥0.3 mg/dL, respectively. The homeostasis model assessment insulin resistance (HOMA-IR) index was calculated as (glucose [mg/dL] × insulin [mg/dL])/405 and scored as abnormal on the basis of participant age (>18 years or <18 years).18,19 HOMA-IR ≥4 was considered abnormal for the pediatric population because this corresponds to the 85th percentile for lean adolescents on the basis of our previous unpublished data and correlates with cross-sectional studies in which HOMA-IR ≥4 represents moderate insulin resistance.20,21 To account for the relative state of insulin resistance in the pediatric population, HOMA-IR ≥3, which is considered abnormal in adults, was used for participants ≥18 years old during longitudinal analysis.22 Participants with diabetes were excluded from homeostasis model assessment analysis. Subjects who were receiving exogenous insulin were excluded from the analysis of changes in insulin and the homeostasis model assessment. Remission of diabetes was defined as the absence of related medications and HbA1c <6.5% (or IFG <126 mg/dL if HbA1c wasn’t available). Laboratory values were measured centrally (Northwest Lipid Metabolism and Diabetes Research Laboratories, Seattle, WA).
Statistical Methods
The baseline and longitudinal (6 months, 1 year, 2 years, and 3 years) prevalences of CVD-RFs were assessed by using percentages and frequencies and evaluated by using generalized linear mixed models. The weights of pregnant female participants (second or third trimester) and up to 6 months postpartum were set to missing (n = 3 at 1 year; n = 7 at 2 years; n = 8 at 3 years). Generalized estimating equation models were performed while simultaneously accounting for independent variables of weight change percentage, age, sex, race, CVD-RF count, clinical site, and procedure consisting of Roux-en-Y gastric bypass (RYGB) and vertical sleeve gastrectomy (VSG) only to evaluate associations between the remission of CVD-RF and each independent variable among participants with abnormal baseline levels. Modeling analyses employed a generalized estimating equation approach with Poisson distribution to obtain robust confidence intervals (CIs) for the relative risk (RR) estimates.23 The potential effects of baseline BMI were evaluated by categorizing participants into groups: Group 1 (BMI <50), Group 2 (BMI ≥50–<60), and Group 3 (BMI ≥60). Categories were chosen to ensure that each group had sufficient participants to optimize statistical analysis. Age was modeled continuously, whereas sex (male and female) and race (white or people of color) were modeled categorically. Linear mixed modeling was used to evaluate associations of baseline risk factor presence with postoperative blood pressure, triglycerides, and HDL-C values, adjusting for age at surgery, sex, race, surgical procedure, clinical center, and BMI. All analyses included variable data from all procedures consisting of RYGB, VSG, and adjustable gastric banding (AGB) with the exception of generalized estimating equation models as mentioned above, which did not include AGB. Missing data were addressed by using multivariate imputation by chained equations. Twenty imputed data sets were generated for use in multivariable modeling analyses. SAS Proc MiAnalyze (SAS Institute, Inc, Cary, NC) was used to generate estimates from the multiple imputed data sets. Comparison modeling from imputed and nonimputed data did not indicate meaningful differences. Therefore, results represent the nonimputed data. Analyses were performed by using SAS version 9.4.
Results
Participants were predominately girls (76%) and white (72%), with a mean age of 17 ± 1.6 years and median BMI of 50 (range 34–88). The majority underwent RYGB (n = 161), with the remainder undergoing VSG (n = 67) or AGB (n = 14). BMI declined by 27% at 3 years (28%, 26%, and 8% for RYGB, VSG, and AGB, respectively; all P < .01).
Changes in Markers of CVD Risk
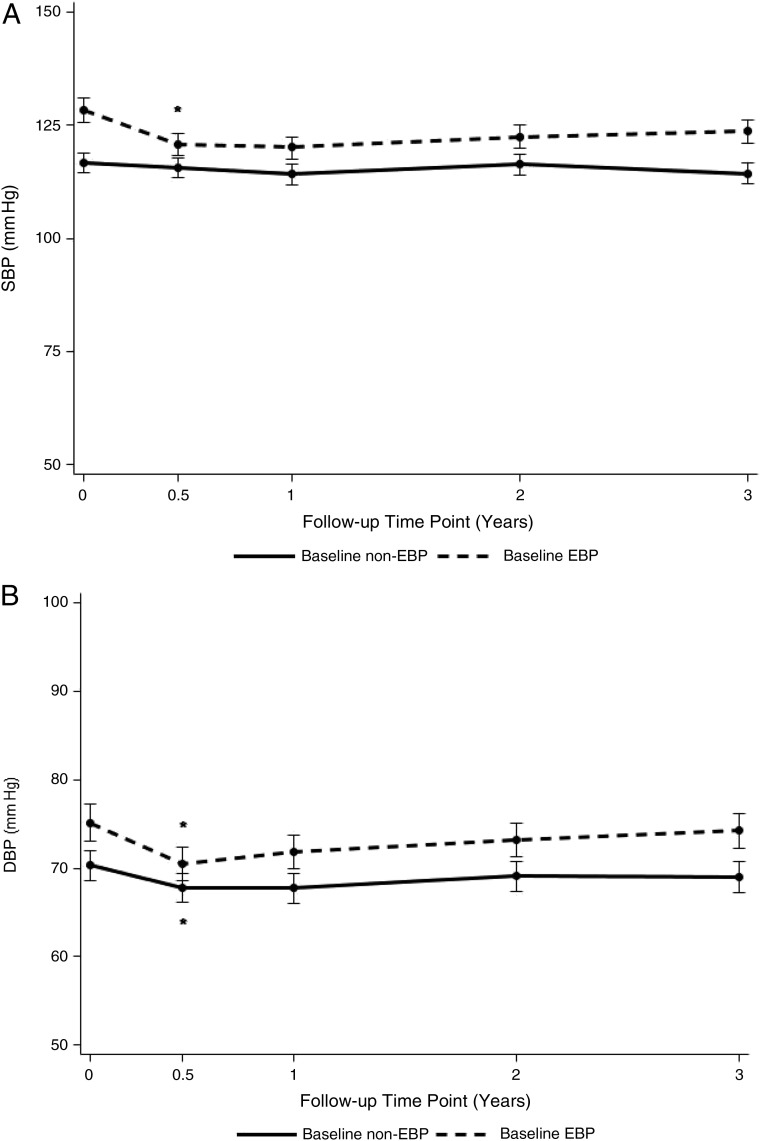
In addition to BMI reduction, improvements were shown in SBP (−6 mm Hg), DBP (−5 mm Hg), triglyceride (−42 mg/dL), and HDL-C (15 mg/dL; Table 1). Baseline EBP was observed in 44% of participants, declining to 15% at 3 years (Table 2). Furthermore, EBP showed a higher prevalence among male versus female participants at baseline (63% male versus 37% female; P = .001) with a reduction to 31% and 10% (P = .002), respectively, by 3 years (data not shown). The baseline BMI range (ie, low, middle, and high) showed a significantly lower prevalence of EBP among participants in the low BMI range (<50; 30%) versus middle (50–59; 51%; P < .001) and high (≥60; 63%; P < .001), and this was age independent. The comparative prevalences at year 3 were indistinguishable (15%, 18% and 14%, respectively). To determine if blood pressure was differentially affected in those with and without baseline EBP, the mean change in SBP and DBP was examined before and after MBS. Participants with baseline EBP demonstrated an 11 mm Hg mean reduction in SBP by 6 months with no demonstrable change thereafter, whereas no significant change was observed among participants without baseline EBP (Fig 1A). An analysis of DBP showed a similar pattern of early and durable reduction (−6 and −4 mm Hg, respectively) among those with and without baseline EBP (Fig 1B). These results suggest that maximal improvements in blood pressure are durable and occur shortly after MBS for participants with baseline EBP while also suggesting partial improvement among those with normal blood pressure (ie, DBP). In addition, 7 incident cases of EBP (4 RYGB and 3 AGB) were identified at 3 years among the 98 participants with available data who had not had the condition at baseline (4%; 95% CI, 0–8; data not shown).
TABLE 1.
Longitudinal Changes in Age and Anthropomorphic and Comorbid Variables
| Baseline | 3 y | |||
|---|---|---|---|---|
| n | Mean (SD) or Median (Q1, Q3) | n | Mean (SD) or Median (Q1, Q3) | |
| Age, y | 242 | 17.1 (1.6) | 196 | 20.2 (1.5) |
| Wt, kg | 242 | 148.5 (30.9) | 193 | 110.4 (33.0) |
| BMI | 242 | 52.5 (9.3) | 190 | 39.0 (11.3) |
| SBP, mm Hg | 238 | 125.6 (13.4) | 191 | 118.2 (13.8) |
| DBP, mm Hg | 238 | 74.4 (10.1) | 191 | 71.7 (9.3) |
| Triglycerides, mg/dL | 238 | 113.0 (82.0, 162.0) | 186 | 71.0 (53.0, 93.0) |
| LDL-C, mg/dL | 238 | 92.8 (25.7) | 186 | 82.8 (24.4) |
| HDL-C, mg/dL | 238 | 37.6 (9.0) | 186 | 52.7 (13.9) |
| Glucose, mg/dL | 238 | 90.5 (84.0, 100.0) | 186 | 85.0 (80.0, 89.0) |
| HbA1c, % | 231 | 5.4 (0.9) | 191 | 5.1 (0.7) |
| Insulin, µU/mL | 230 | 25.4 (16.9, 38.3) | 185 | 9.5 (5.8, 15.0) |
| hs-CRP, mg/dL | 238 | 0.6 (0.3, 1.2) | 187 | 0.4 (0.0, 0.3) |
| HOMA-IR | 230 | 5.8 (3.5, 9.4) | 184 | 1.9 (1.2, 3.3) |
Comparison of demographic characteristics (age, wt, BMI, SBP and DBP, triglyceride, HDL-C and LDL-C, glucose, HbA1c, insulin, and HOMA-IR) between baseline (preoperative time point) and the 3-y time point. Q1, First Quartile; Q3, Third Qaurtile.
TABLE 2.
Longitudinal Changes in the Markers of CVD-RFs
| Baseline | 6 mo | 12 mo | 24 mo | 36 mo | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | |
| EBP | 238 | 43.6 (36.3–51.3) | 206 | 20.2 (14.7–27.1) | 213 | 16.8 (11.9–23.2) | 198 | 10.9 (7.0–16.5) | 190 | 15.5 (10.6–22.0) |
| IFG | 234 | 26.0 (19.9–33.1) | 190 | 5.2 (2.7–9.7) | 202 | 4.3 (2.2–8.3) | 191 | 4.1 (2.0–8.2) | 181 | 3.9 (1.8–8.1) |
| Diabetes | 239 | 12.6 (8.2–18.7) | 200 | 5.9 (3.2–10.9) | 206 | 1.9 (0.7–5.3) | 193 | 1.8 (0.6–5.2) | 187 | 0.6 (0.1–3.8) |
| Dyslipidemia | 238 | 75.2 (68.7–80.8) | 204 | 53.1 (45.4–60.7) | 210 | 26.8 (20.7–33.8) | 196 | 25.8 (19.6–33.0) | 184 | 29.4 (22.6–37.3) |
| LDL-C ≥130 mg/dL | 238 | 7.9 (4.7–13.1) | 204 | 6.9 (3.8–12.2) | 210 | 5.3 (2.8–10.0) | 197 | 5.0 (2.5–9.7) | 186 | 4.2 (2.0–8.8) |
| HDL-C <40 mg/dL | 238 | 63.5 (56.2–70.3) | 204 | 42.4 (34.8–50.4) | 210 | 18.7 (13.6–25.2) | 197 | 14.1 (9.6–20.2) | 186 | 15.2 (10.4–21.6) |
| Triglycerides ≥130 mg/dL | 238 | 40.6 (33.5–48.2) | 204 | 14.2 (9.7–20.3) | 210 | 6.8 (4.0–11.3) | 197 | 12.5 (8.3–18.4) | 186 | 11.4 (7.3–17.4) |
| Abnormal triglyceride–to–HDL-C ratio | 226 | 53.7 (45.9–61.3) | 195 | 23.7 (17.5–31.1) | 201 | 9.8 (6.2–15.2) | 188 | 11.0 (7.1–16.9) | 175 | 13.3 (8.7–19.8) |
| Elevated HOMA-IRa | 209 | 75.8 (68.9–81.5) | 191 | 26.2 (20.0–33.6) | 206 | 21.1 (15.6–27.7) | 191 | 18.5 (13.3–25.2) | 185 | 25.0 (18.8–32.4) |
| Insulin >17.0 U/mL | 230 | 73.8 (67.1–79.5) | 196 | 29.9 (23.3–37.3) | 206 | 16.9 (12.1–23.0) | 189 | 14.9 (10.3–21.1) | 185 | 20.6 (15.0–27.5) |
| HbA1c ≥6.5% | 231 | 5.9 (2.9–11.8) | 199 | 1.9 (0.6–5.8) | 206 | 1.8 (0.6–5.6) | 193 | 2.1 (0.7–6.1) | 191 | 1.2 (0.3–4.7) |
| hs-CRP ≥0.3 mg/dL | 238 | 75.1 (68.4–80.8) | 203 | 42.6 (34.9–50.6) | 210 | 29.5 (23.0–37.0) | 195 | 23.6 (17.6–30.8) | 187 | 25.1 (18.8–32.8) |
Changes in the prevalence (CI) of multiple CVD-RF variables determined at baseline (preoperative) and the 6-, 12-, 24-, and 36-mo time points.
FIGURE 1.
A, Changes in the mean SBP (mm Hg) among participants with baseline EBP versus without baseline EBP. B, Changes in the mean DBP (mm Hg) among participants with baseline EBP versus without baseline EBP. Linear mixed modeling was used to evaluate associations of baseline presence of EBP with postoperative SBP and DBP values adjusted for age at surgery, sex, race, surgical procedure, clinical center, and BMI. * P < .05 versus previous time point.
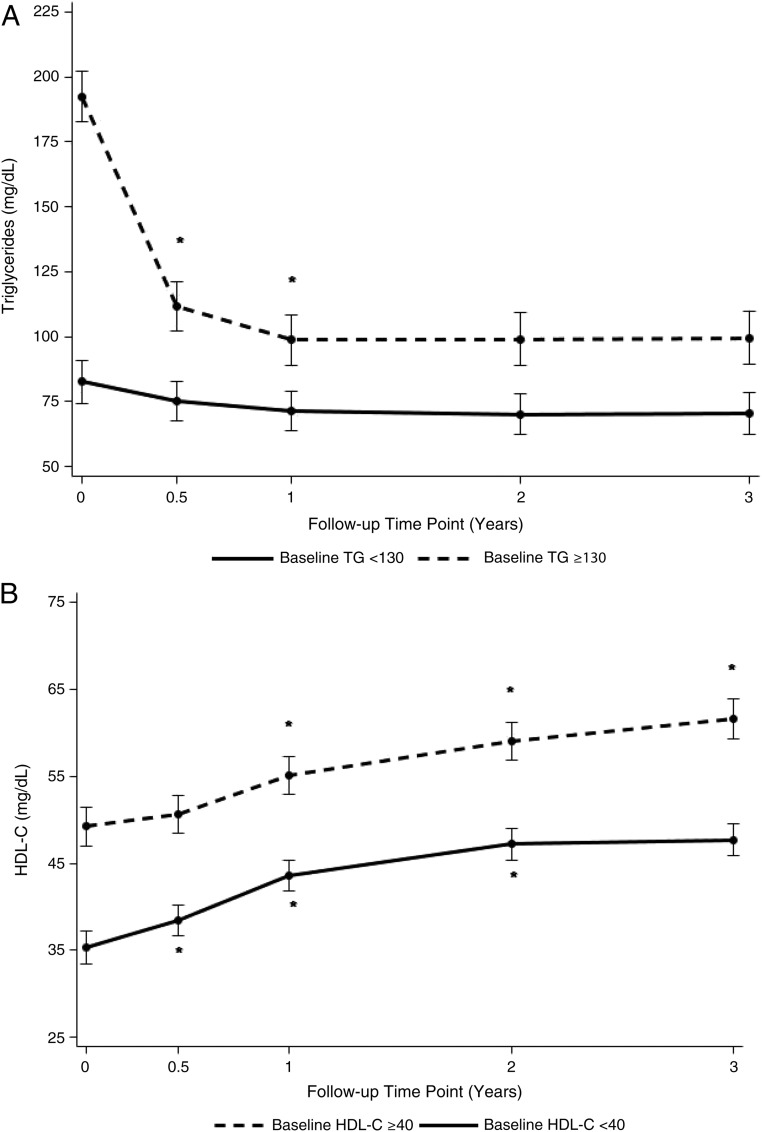
A major reduction in dyslipidemia was also observed, with 75% affected at baseline, declining to 27% by 1 year and 29% by 3 years (Table 2). The primary drivers of improvement relate to changes in triglyceride and HDL-C (Table 1). Hypertriglyceridemia declined from 41% to 11%, whereas abnormal HDL-C (<40 mg/dL) declined from 64% to 15% (Table 2). Similar to improvements in blood pressure, a partial differentiation was observed between those with and without abnormal baseline lipid profiles (ie, triglyceride and HDL-C levels). Namely, participants with baseline hypertriglyceridemia (>130 mg/dL) experienced a 94 mg/dL decline by 3 years (Fig 2A), whereas those without elevated baseline triglyceride showed no change. Furthermore, in contrast with the early but fixed changes in blood pressure, improvements in triglyceride levels among those with hypertriglyceridemia were observed for up to 1 year. A corresponding analysis of those with and without abnormal HDL-C (<40 mg/dL) showed similar changes by 3 years (15 and 16 mg/dL, respectively) with continuous improvement beyond the first postoperative year in both subgroups (Fig 2B). Of the 59 participants without baseline dyslipidemia, data were available to define the 3-year status for 43 of them. Five incident cases of dyslipidemia (11.6%) were observed (1 RYGB, 2 VSG, and 2 AGB). The main drivers for the incidence of dyslipidemia were related to a rise in LDL-C (1 VSG and 1 AGB) or triglyceride (1 VSG and 1 RYGB) or a reduction in HDL-C (1 AGB; data not shown).
FIGURE 2.
A and B, Changes in median triglyceride levels among participants with elevated baseline triglyceride (>130 mg/dL) versus nonelevated baseline triglyceride (<130 mg/dL) levels. B, Changes in median HDL-C levels among participants with low baseline HDL-C (<40 mg/dL) versus nonreduced HDL-C (>40 mg/dL) levels. Linear mixed modeling was used to evaluate associations of baseline presence of abnormal triglyceride and HDL-C levels with corresponding values adjusted for age at surgery, sex, race, surgical procedure, clinical center, and BMI. * P < .05 versus previous time point.
Baseline diabetes was present in 13% of participants with major metabolic improvement (0.5%) by 3 years (Table 2). Similarly, baseline IFG (26%) and hyperinsulinemia (74%) dramatically improved by year 3 (4% and 20%, respectively). Additionally, insulin resistance (defined as elevated HOMA-IR) declined from 76% to 25%, whereas hs-CRP (a biomarker of low-grade systemic inflammation) declined from 75% at baseline to 26% at 3 years.
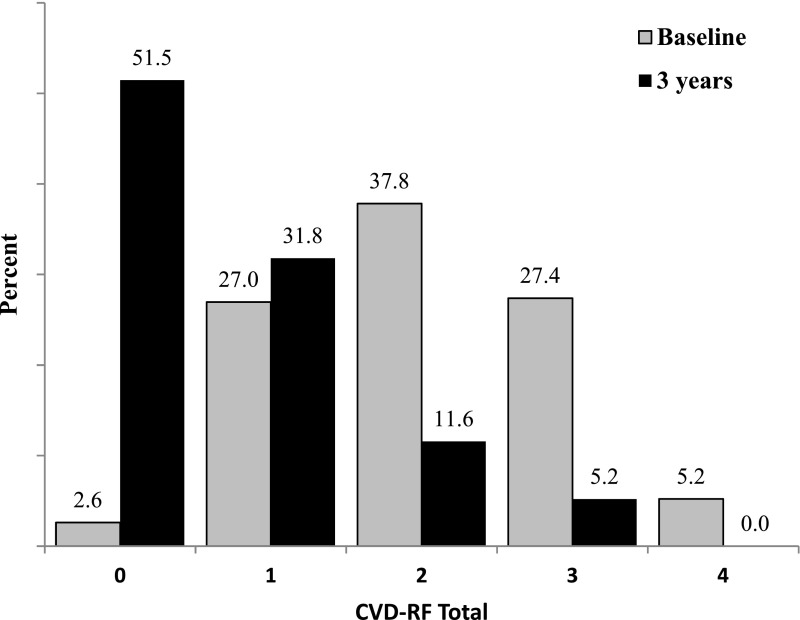
The CVD-RF total score was used to determine the multiplicity of comorbid disease. At baseline, 97% of participants exhibited ≥1 CVD-RF, whereas at 3 years, less than half (48%) demonstrated similar CVD-RF multiplicity. Those with ≥3 baseline CVD-RFs (33%) decreased to 5% at 3 years (P < .001; Fig 3).
FIGURE 3.
Longitudinal changes in the total number of CVD-RFs (CVD-RF Total). CVD-RF Total represents a composite score of 4 equally weighted, independent CVD-RFs (EBP, dyslipidemia, diabetes, and abnormal hs-CRP).
Predictors of CVD Risk Remission
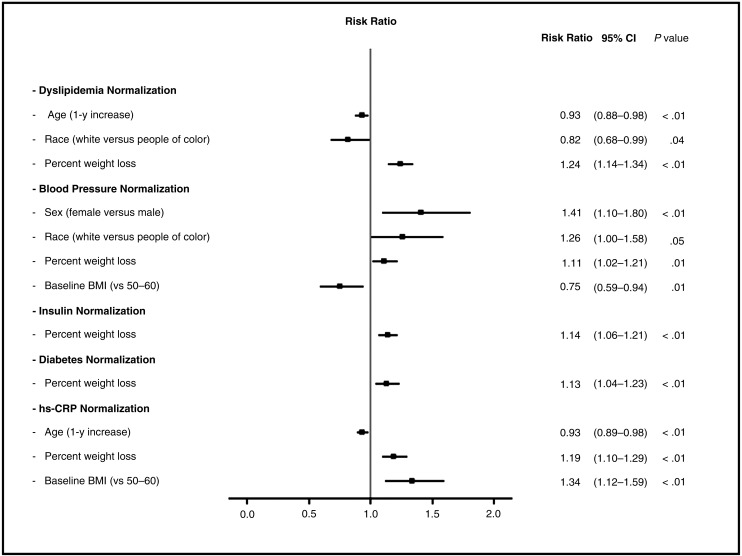
Multivariable logistic regression analysis was used to discern the predictors of CVD-RF remission and/or normalization after MBS. For every 10% increase in weight loss, participants were 24%, 11%, 14%, 13%, and 19% more likely to achieve resolution of dyslipidemia, EBP, hyperinsulinemia, diabetes, and elevated hs-CRP, respectively (Fig 4). Increasing baseline age was independently associated with a lower likelihood of dyslipidemia remission (RR 0.93; CI 0.88–0.98). Female (RR 1.41; CI 1.10–1.80) and white (RR 1.26; CI 1.00–1.58) participants were more likely to achieve normalization of EBP versus male participants and participants of color.
FIGURE 4.
Significant predictors of CVD-RF normalization 3 years after bariatric surgery. RRs and 95% CIs for CVD-RF normalization among subjects with abnormal risk factor levels at baseline are shown. Each model included age, sex, race, percent weight change from baseline, baseline BMI groups, CVD-RF total, surgical procedure, and clinical center as independent variables. Only RR relationships with significant P values (< .05) are displayed.
Discussion
Researchers in recent studies have concluded that severe obesity is extremely difficult to reverse, and outcomes from nonsurgical weight loss (ie, diet and exercise and behavior modification) are disappointing at best.24–28 Observations that cardiometabolic risk is established during childhood and worsens over time have led to an increased focus on MBS as a means to mitigate longitudinal adverse effects on cardiovascular end points beyond adolescence.26,29–31 In the current study, we report the predictors of change in CVD risk in a large cohort of adolescents undergoing MBS, thereby extending our previous findings describing the baseline prevalence of CVD-RFs within this same cohort.5,9 The current analysis shows that reductions in CVD-RFs are associated with not only weight loss but also age at the time of surgery, preoperative BMI, sex, and race.
The identification of the predictors of change in CVD-RFs is novel and important. We offer clear evidence that weight loss after adolescent MBS predicts the degree of longitudinal improvement in elevated hs-CRP, hyperinsulinemia, dyslipidemia, and diabetes. In addition, we demonstrate an important relationship between highest baseline BMI and decreased probability of hs-CRP normalization. In conjunction with data showing that adolescents in the highest BMI categories have a lower likelihood of achieving a normal postoperative BMI,32,33 these results are particularly relevant to patient selection for surgery. Specifically, the optimal time to perform MBS may be before individuals achieve BMI values that predict resistance to a reversal of obesity and reduced probability of improvement of certain CVD-RFs (ie, hs-CRP). Thus, the evidence suggests that better long-term outcomes may be anticipated among individuals undergoing MBS at lower BMI levels (ie, <50).
Although relationships between change in CVD-RFs and postoperative weight reduction are not unexpected, additional interactions should also be considered. Increasing age at the time of MBS was associated with a reduced likelihood of dyslipidemia remission and normalization of hs-CRP. These findings suggest that even within the narrow age range of this adolescent cohort, distinct advantages to undergoing MBS earlier may exist. Although earlier surgical intervention presents an attractive hypothesis that CVD-RFs and end-organ damage may be reduced, the ability to offer clear guidance regarding an ideal age is limited by a paucity of studies that specifically address this issue. Although recent reports show favorable outcomes among preteen-aged and early-childhood cohorts,34,35 high-quality data addressing the advantages and disadvantages of earlier surgery are lacking. Our findings underscore the importance of long-term analysis to demonstrate whether the more beneficial responses of CVD-RFs in younger adolescents and children allow these individuals to enjoy even greater longitudinal health benefits than individuals undergoing MBS later in adolescence.
LDL-C concentrations are associated with CVD development but do not tell the whole story and are not related to BMI in a purely linear fashion. Indeed, only 8% of our cohort had raised baseline LDL-C.34 The LDL-C phenotype is influenced by central obesity, insulin resistance, glucose intolerance, and elevated triglycerides, and it is characterized by small, dense, apolipoprotein B–rich LDL-C particles, which are highly atherogenic.36,37 Thus, a reduction in LDL-C–related risk with weight loss likely reflects changes in factors associated with the atherogenic phenotype through the effect of MBS on triglyceride-rich lipoprotein kinetics rather than changes in concentration.38
Finally, the collective interpretation of the dramatic improvements in a number of CVD risk parameters, including IFG, insulin, hs-CRP, and EBP, as well as improvements in HOMA-IR, representing the normalization of cardiometabolic homeostasis, serves as 1 of the most powerful arguments in support of MBS in adolescents to date. In the context of data highlighting the adverse effects of untreated childhood obesity in adulthood29,30 as well as evidence demonstrating the important mitigating influence of MBS on numerous CVD-RFs and related disease entities (ie, diabetes, EBP, and dyslipidemia) among adolescents13 and adults,39 the current report strongly supports the overall hypothesis that MBS performed during adolescence may provide unique benefits by altering the probability of future adverse cardiovascular events later in life, including the development and progression of impaired glucose metabolism, atherosclerosis, heart failure, and stroke.
This study has several limitations. Based on the high BMI range, the findings are not representative of the wider obese population but rather are specific to the severely obese. Furthermore, the overrepresentation of girls, white people, and participants undergoing RYGB further limit the generalizability, and the use of categorical analysis based on the differentiation of age-dependent CVD-RF cutpoints may also introduce bias. Also, abnormal blood pressure measurements did not meet the strict definition of hypertension, thereby limiting our ability to compare outcomes to corresponding literature. Finally, because the analysis does not consider data beyond 3 years, our ability gain insight(s) related to weight loss durability, weight regain, and predictive analysis of incidence or re-emergence of CVDRFs remains beyond the scope of this study and will be the focus of future reporting. Despite these limitations, the large sample size and uniformity of data collection (including the use of a central laboratory, standardized definitions, and high subject retention) are clear strengths of this study.
Conclusions
In this first large-scale analysis of the predictors of change in CVD-RFs among adolescents after MBS, we report on differential patterns of early improvement and a reduction in the multiplicity of cardiometabolic risk factors. Furthermore, the identification of specific predictors of CVD-RF normalization and/or remission on the basis of sex, race, preoperative BMI, and age at surgery may serve to improve future study design and insights regarding the optimization of treatment strategies. Collectively, these data demonstrate a reduction in the risk for development of CVD in adulthood and offer additional, compelling support for MBS in adolescents.
Acknowledgments
We acknowledge the significant contributions made by the Teen-LABS Consortium as well as our parent study, the Longitudinal Assessment of Bariatric Surgery Consortium (grant U01 DK066557). The National Institute of Diabetes and Digestive and Kidney Diseases project scientist was involved in the design and conduct of the study, interpretation of the data, review and approval of the article, and decision to submit the article for publication. Finally, the consortium is grateful for the important work done by the adjudication committee.
Glossary
- AGB
adjustable gastric banding
- CI
confidence interval
- CVD
cardiovascular disease
- CVD-RF
cardiovascular disease risk factor
- DBP
diastolic blood pressure
- EBP
elevated blood pressure
- HbA1c
hemoglobin A1c
- HDL-C
high-density lipoprotein cholesterol
- HOMA-IR
homeostasis model assessment insulin resistance
- hs-CRP
high-sensitivity C-reactive protein
- IFG
impaired fasting glucose
- LDL-C
low-density lipoprotein cholesterol
- MBS
metabolic and/or bariatric surgery
- RR
relative risk
- RYGB
Roux-en-Y gastric bypass
- SBP
systolic blood pressure
- Teen-LABS
Teen-Longitudinal Assessment of Bariatric Surgery
- VSG
vertical sleeve gastrectomy
Appendix
The following Teen-LABS Consortium members are nonauthor contributors. Cincinnati Children’s Hospital Medical Center: Meg Zeller, PhD; Avani Modi, PhD; Stavra Xanthakos, MD, MS; Larry Dolan, MD; Rosie Miller, RN, CCRC; Rachel Akers, MPH; and Stephen Daniels, MD, PhD. University of Cincinnati: Ralph Buncher, ScD. Texas Children’s Hospital and Baylor University Medical Center: Vadim Sherman, MD; David Allen, BS; Gia Washington, PhD; and Karin Price, PhD. Children’s Hospital of Alabama and University of Alabama at Birmingham: Richard Stahl, MD, and Beverly Haynes, BSN. University of Pittsburgh Medical Center: Ramesh Ramanathan, MD; Carol A. McCloskey, MD; George M. Eid, MD; William Gourash, MSN, CRNP, and Dana Rofey, PhD, MS. Nationwide Children’s Hospital: Steven Teich, MD; Karen Carter, CCRC; Melinda Helton, RN; Bonny Bowen, RN; Robert David Murray, MD; Amy Baughcum, PhD; Cody Brennan, CCRP; and Ihuoma Eneli, MD. National Institute of Diabetes and Digestive and Kidney Diseases: Mary Horlick, MD; Mary Evans, PhD; Rebecca Torrance, RN, MSN; Rebekah Van Raaphorst, MPH; and Susan Yanovski, MD.
Footnotes
Dr Michalsky was primarily responsible for data interpretation, drafted the initial manuscript, and oversaw subsequent manuscript revisions; Dr Inge conceptualized and designed the study and assisted in data interpretation and manuscript preparation and revisions; Drs Jenkins and Xie collected data, conducted the initial analyses, and reviewed and revised the manuscript; Drs Courcoulas, Helmrath, Brandt, Harmon, Chen, Dixon, and Urbina assisted in data interpretation and manuscript preparation and revisions; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
This trial has been registered at www.clinicaltrials.gov (identifier: NCT00474318).
FINANCIAL DISCLOSURE: Dr Inge serves as a consultant for Standard Bariatrics, UpToDate Inc, and Independent Medical Expert Consulting Services, all of which are unrelated to this project. Dr Dixon’s research is supported through a National Health and Medical Research Council research fellowship. Dr Courcoulas has received grants from Medtronic Minimally Invasive Therapies (formerly Covidien) and Ethicon J&J Healthcare System; the other authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: The Teen-Longitudinal Assessment of Bariatric Surgery Consortium was funded by cooperative agreements with the National Institute of Diabetes and Digestive and Kidney Diseases through grants U01DK072493, UM1DK072493, and UM1DK095710 (University of Cincinnati). The study was also supported by grants UL1 TR000077-04 (Cincinnati Children’s Hospital Medical Center), UL1RR025755 (Nationwide Children’s Hospital), M01-RR00188 (Texas Children’s Hospital and Baylor University College of Medicine), UL1 RR024153 and UL1TR000005 (University of Pittsburgh), and UL1 TR000165 (University of Alabama at Birmingham). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: Dr Inge serves as a consultant for Standard Bariatrics, UpToDate Inc, and Independent Medical Expert Consulting Services, all of which are unrelated to this project. Dr Harmon served on an advisory panel for the Stryker Corporation from 1998 to 2015, which was unrelated to this project. Dr Dixon has consulted for Apollo Endosurgery, Medtronic Minimally Invasive Therapies (formerly Covidien), Bariatric Advantage, Nestle Health Science, Inova, and Novo Nordisk; the other authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Pratt JS, Lenders CM, Dionne EA, et al. . Best practice updates for pediatric/adolescent weight loss surgery. Obesity (Silver Spring). 2009;17(5):901–910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Michalsky M, Kramer RE, Fullmer MA, et al. . Developing criteria for pediatric/adolescent bariatric surgery programs. Pediatrics. 2011;128(suppl 2):S65–S70 [DOI] [PubMed] [Google Scholar]
- 3.Apovian CM, Baker C, Ludwig DS, et al. . Best practice guidelines in pediatric/adolescent weight loss surgery. Obes Res. 2005;13(2):274–282 [DOI] [PubMed] [Google Scholar]
- 4.Michalsky MP, Raman SV, Teich S, Schuster DP, Bauer JA. Cardiovascular recovery following bariatric surgery in extremely obese adolescents: preliminary results using cardiac magnetic resonance (CMR) imaging. J Pediatr Surg. 2013;48(1):170–177 [DOI] [PubMed] [Google Scholar]
- 5.Michalsky MP, Inge TH, Simmons M, et al. ; Teen-LABS Consortium . Cardiovascular risk factors in severely obese adolescents: the Teen Longitudinal Assessment of Bariatric Surgery (Teen-LABS) Study. JAMA Pediatr. 2015;169(5):438–444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ippisch HM, Inge TH, Daniels SR, et al. . Reversibility of cardiac abnormalities in morbidly obese adolescents. J Am Coll Cardiol. 2008;51(14):1342–1348 [DOI] [PubMed] [Google Scholar]
- 7.Zwintscher NP, Azarow KS, Horton JD, Newton CR, Martin MJ. The increasing incidence of adolescent bariatric surgery. J Pediatr Surg. 2013;48(12):2401–2407 [DOI] [PubMed] [Google Scholar]
- 8.Inge TH, Zeller M, Harmon C, et al. . Teen-Longitudinal Assessment of Bariatric Surgery: methodological features of the first prospective multicenter study of adolescent bariatric surgery. J Pediatr Surg. 2007;42(11):1969–1971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Inge TH, Zeller MH, Jenkins TM, et al. ; Teen-LABS Consortium . Perioperative outcomes of adolescents undergoing bariatric surgery: the Teen-Longitudinal Assessment of Bariatric Surgery (Teen-LABS) study. JAMA Pediatr. 2014;168(1):47–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Michalsky M, Reichard K, Inge T, Pratt J, Lenders C; American Society for Metabolic and Bariatric Surgery . ASMBS pediatric committee best practice guidelines. Surg Obes Relat Dis. 2012;8(1):1–7 [DOI] [PubMed] [Google Scholar]
- 11.Belle SH, Berk PD, Courcoulas AP, et al. ; Longitudinal Assessment of Bariatric Surgery Consortium Writing Group . Safety and efficacy of bariatric surgery: Longitudinal Assessment of Bariatric Surgery. Surg Obes Relat Dis. 2007;3(2):116–126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mackey RH, Belle SH, Courcoulas AP, et al. ; Longitudinal Assessment of Bariatric Surgery Consortium Writing Group . Distribution of 10-year and lifetime predicted risk for cardiovascular disease prior to surgery in the longitudinal assessment of bariatric surgery-2 study. Am J Cardiol. 2012;110(8):1130–1137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Inge TH, Courcoulas AP, Jenkins TM, et al. ; Teen-LABS Consortium . Weight loss and health status 3 years after bariatric surgery in adolescents. N Engl J Med. 2016;374(2):113–123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xanthakos SA, Jenkins TM, Kleiner DE, et al. ; Teen-LABS Consortium . High prevalence of nonalcoholic fatty liver disease in adolescents undergoing bariatric surgery. Gastroenterology. 2015;149(3):623–634.e8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Morris PB, Ballantyne CM, Birtcher KK, Dunn SP, Urbina EM. Review of clinical practice guidelines for the management of LDL-related risk. J Am Coll Cardiol. 2014;64(2):196–206 [DOI] [PubMed] [Google Scholar]
- 16.Marotta T, Russo BF, Ferrara LA. Triglyceride-to-HDL-cholesterol ratio and metabolic syndrome as contributors to cardiovascular risk in overweight patients. Obesity (Silver Spring). 2010;18(8):1608–1613 [DOI] [PubMed] [Google Scholar]
- 17.Michalsky MP. Adolescent bariatric surgery in the United Kingdom; a call for continued study and open dialogue. Arch Dis Child. 2014;99(10):885–886 [DOI] [PubMed] [Google Scholar]
- 18.Wallace TM, Levy JC, Matthews DR. Use and abuse of HOMA modeling. Diabetes Care. 2004;27(6):1487–1495 [DOI] [PubMed] [Google Scholar]
- 19.Levy JC, Matthews DR, Hermans MP. Correct homeostasis model assessment (HOMA) evaluation uses the computer program. Diabetes Care. 1998;21(12):2191–2192 [DOI] [PubMed] [Google Scholar]
- 20.Gayoso-Diz P, Otero-González A, Rodriguez-Alvarez MX, et al. . Insulin resistance (HOMA-IR) cut-off values and the metabolic syndrome in a general adult population: effect of gender and age: EPIRCE cross-sectional study. BMC Endocr Disord. 2013;13:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yin J, Li M, Xu L, et al. . Insulin resistance determined by homeostasis model assessment (HOMA) and associations with metabolic syndrome among Chinese children and teenagers. Diabetol Metab Syndr. 2013;5(1):71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sumner AE, Cowie CC. Ethnic differences in the ability of triglyceride levels to identify insulin resistance. Atherosclerosis. 2008;196(2):696–703 [DOI] [PubMed] [Google Scholar]
- 23.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706 [DOI] [PubMed] [Google Scholar]
- 24.van der Baan-Slootweg O, Benninga MA, Beelen A, et al. . Inpatient treatment of children and adolescents with severe obesity in the Netherlands: a randomized clinical trial. JAMA Pediatr. 2014;168(9):807–814 [DOI] [PubMed] [Google Scholar]
- 25.Inge TH, Siegel RM, Xanthakos SA. Weight loss maintenance: a hard nut to crack. JAMA Pediatr. 2014;168(9):796–797 [DOI] [PubMed] [Google Scholar]
- 26.Treadwell JR, Sun F, Schoelles K. Systematic review and meta-analysis of bariatric surgery for pediatric obesity. Ann Surg. 2008;248(5):763–776 [DOI] [PubMed] [Google Scholar]
- 27.Marcus MD, Foster GD, El Ghormli L. Stability of relative weight category and cardiometabolic risk factors among moderately and severely obese middle school youth. Obesity (Silver Spring). 2014;22(4):1118–1125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Danielsson P, Kowalski J, Ekblom Ö, Marcus C. Response of severely obese children and adolescents to behavioral treatment. Arch Pediatr Adolesc Med. 2012;166(12):1103–1108 [DOI] [PubMed] [Google Scholar]
- 29.Twig G, Tirosh A, Leiba A, et al. . BMI at age 17 years and diabetes mortality in midlife: a nationwide cohort of 2.3 million adolescents. Diabetes Care. 2016;39(11):1996–2003 [DOI] [PubMed] [Google Scholar]
- 30.Twig G, Yaniv G, Levine H, et al. . Body-mass index in 2.3 million adolescents and cardiovascular death in adulthood. N Engl J Med. 2016;374(25):2430–2440 [DOI] [PubMed] [Google Scholar]
- 31.Freedman DS, Mei Z, Srinivasan SR, Berenson GS, Dietz WH. Cardiovascular risk factors and excess adiposity among overweight children and adolescents: the Bogalusa Heart Study. J Pediatr. 2007;150(1):12–17.e2 [DOI] [PubMed] [Google Scholar]
- 32.Inge TH, Jenkins TM, Xanthakos SA, et al. . Long-term outcomes of bariatric surgery in adolescents with severe obesity (FABS-5+): a prospective follow-up analysis. Lancet Diabetes Endocrinol. 2017;5(3):165–173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Inge TH, Jenkins TM, Zeller M, et al. . Baseline BMI is a strong predictor of nadir BMI after adolescent gastric bypass. J Pediatr. 2010;156(1):103–108.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alqahtani A, Alamri H, Elahmedi M, Mohammed R. Laparoscopic sleeve gastrectomy in adult and pediatric obese patients: a comparative study. Surg Endosc. 2012;26(11):3094–3100 [DOI] [PubMed] [Google Scholar]
- 35.Alqahtani A, Elahmedi M, Qahtani AR. Laparoscopic sleeve gastrectomy in children younger than 14 years: refuting the concerns. Ann Surg. 2016;263(2):312–319 [DOI] [PubMed] [Google Scholar]
- 36.Livingston EH, Chandalia M, Abate N. Do current body mass index criteria for obesity surgery reflect cardiovascular risk? Surg Obes Relat Dis. 2007;3(6):577–585 [DOI] [PubMed] [Google Scholar]
- 37.Després JP. The insulin resistance-dyslipidemic syndrome of visceral obesity: effect on patients’ risk. Obes Res. 1998;6(suppl 1):8S–17S [DOI] [PubMed] [Google Scholar]
- 38.Padilla N, Maraninchi M, Béliard S, et al. . Effects of bariatric surgery on hepatic and intestinal lipoprotein particle metabolism in obese, nondiabetic humans. Arterioscler Thromb Vasc Biol. 2014;34(10):2330–2337 [DOI] [PubMed] [Google Scholar]
- 39.Fox CS, Golden SH, Anderson C, et al. ; American Heart Association Diabetes Committee of the Council on Lifestyle and Cardiometabolic Health; Council on Clinical Cardiology; Council on Cardiovascular and Stroke Nursing; Council on Cardiovascular Surgery and Anesthesia; Council on Quality of Care and Outcomes Research; American Diabetes Association . Update on prevention of cardiovascular disease in adults with type 2 diabetes mellitus in light of recent evidence: a scientific statement from the American Heart Association and the American Diabetes Association. Diabetes Care. 2015;38(9):1777–1803 [DOI] [PMC free article] [PubMed] [Google Scholar]