Abstract
Here we report our experience of ceritinib in crizotinib-pretreated patients with anaplastic lymphoma kinase (ALK) positive (ALK+) non-small cell lung cancer (NSCLC) in a French temporary authorisation for use (TAU) study.
The French TAU study included crizotinib-pretreated patients with advanced ALK+ or ROS proto-oncogene 1 positive (ROS1+) tumours. Patients received oral ceritinib (750 mg·day−1 as a starting dose) and best tumour response (as evaluated by the investigator) and safety were reported every 3 months.
A total of 242 TAUs were granted from March 12, 2013 to August 05, 2015. Of the 242 patients, 228 had ALK+ NSCLC and 13 had ROS1+ NSCLC. The median age of ALK+ patients (n=214) was 58.5 years, 51.9% were female, 70.8% had an Eastern Cooperative Oncology Group (ECOG) performance status (PS) of 0–1 and 50.0% had brain metastases. Of the 149 efficacy evaluable ALK+ NSCLC patients, 5.4% had a complete response (CR), 47.0% had a partial response (PR) and 22.8% had stable disease (SD). At September 05, 2015, the median duration of ceritinib treatment (n=182) was 3.9 months but 5.5 months for patients (n=71) with a follow-up of ≥12 months. Higher objective response rate (ORR) was observed for patients with ECOG PS 0 to 1 (55.0% versus 42.4%) and those receiving prior crizotinib for >5 months (51.6% versus 36.1%). Treatment-related adverse events (AEs) were reported in 118 of 208 patients (56.7%), the most common being diarrhoea (22.1%) and hepatic toxicity (19.7%).
Ceritinib (750 mg·day−1) demonstrated efficacy similar efficacy to ASCEND-1, ASCEND-2 and phase 3 ASCEND-5 trials with manageable safety in crizotinib-pretreated patients with ALK+ NSCLC.
Short abstract
Ceritinib (750 mg per day) showed similar efficacy as in clinical trials in crizotinib-pretreated ALK+ NSCLC patients http://ow.ly/8oXe30h27D0
Introduction
Anaplastic lymphoma kinase (ALK) rearrangements occur in approximately 5% of patients with non-small cell lung cancer (NSCLC) [1]. Crizotinib is the first ALK-targeted approved agent and targets cMET, ALK and ROS1 [2, 3]. Results from phase 3 trials have demonstrated the superiority of crizotinib over chemotherapy in patients with ALK-rearranged (ALK+) NSCLC in both second-line and first-line settings [4, 5]. However, most patients responding on crizotinib acquire resistance within 1 year, with recurrence most commonly occurring in the brain or liver [6–8]. Ceritinib (LDK378) is a selective oral ALK-inhibitor with a potency 20-times greater than crizotinib in enzymatic assays and a nanomolar potency against patient-derived crizotinib-resistant tumour cell lines [9].
Ceritinib is approved for the treatment of patients with ALK+ metastatic or advanced NSCLC previously treated with crizotinib by several health authorities, including the United States Food & Drug Administration (FDA) and the European Medicines Agency (EMA) [10, 11].
In the phase 1 ASCEND-1 study, ceritinib (750 mg·day−1) demonstrated robust anti-tumour activity (both intracranial and extracranial) in heavily pretreated patients with ALK+ NSCLC, for both ALK-inhibitor naïve and ALK-inhibitor pretreated patients [12, 13]. Also, in two phase 2 studies, ceritinib (750 mg·day−1) demonstrated a high objective response rate (ORR) as well as intracranial responses with promising progression-free survival (PFS) in patients with ALK+ NSCLC, for both ALK-inhibitor naïve (ASCEND-3) and crizotinib-pretreated patients (ASCEND-2) [14, 15]. More recently, two phase 3 trials have confirmed that ceritinib was more effective than chemotherapy in first-line (ASCEND-4) [16] and second-line (ASCEND-5) [17] settings.
Regulatory processes and local reimbursement can delay the availability to patients of new and promising drugs. The French compassionate-use program, the Temporary Authorisation for Use or TAU program, helps to provide early access of new and promising drugs. It is also a unique opportunity to gain insight into the safety and effectiveness of innovative drugs in a real-life situation. Therefore, we report the efficacy and safety data of ceritinib (at 750 mg·day−1) in ALK+ NSCLC patients from the TAU program.
Patients and methods
TAU program design and treatment
A TAU is granted on the basis of a positive benefit–risk ratio assessment by the French National Agency for Medicines and Health Products Safety (the Agence Nationale de Sécurité du Médicament et des Produits de Santé (ANSM)). There are two types of TAU: 1. a nominative TAU available on a named-patient basis under the responsibility of the prescribing physician; and 2. a cohort TAU intended to apply to a group of patients and established at the request of a pharmaceutical company for specific indications [18, 19].
The first nominative TAU for ceritinib was granted on March 12, 2013. On January 24, 2014, the ANSM, in agreement with Novartis, established a Protocol for Therapeutic Use and Information Collection (PUT) concerning this nominative TAU and, on September 12, 2014, granted a cohort TAU for ceritinib and validated the PUT for it. The first patient was enrolled in the cohort TAU on October 07, 2014 and it ended on August 05, 2015, the date on which commercial batches of Zykadia (ceritinib) were made available to hospital pharmacies.
The TAU program was conducted at centres across France. All patients received from their physicians both verbal information and a patient's information leaflet on the TAU program (explaining the drug and its known adverse effects (AEs)) before enrolment, as specified by the PUT.
Patients received oral ceritinib (750 mg·day−1) until disease progression, unacceptable toxicity, or a patient's or physician's decision led to treatment being stopped. Treatment beyond progression was allowed, at the physician's discretion, for patients still deriving clinical benefit from it.
Patients included in the TAU
The TAU program included patients with advanced ALK+ NSCLC, ROS1+ NSCLC, or other ALK+ tumours. ALK and ROS1 testing were performed by the French National Cancer Institute certified genetics centres [1]. Patients with ALK+ NSCLC were eligible if they had advanced NSCLC with ALK-rearrangement, as demonstrated by fluorescent in situ hybridisation (FISH) and/or immunohistochemistry (IHC), and were considered ineligible for or unable to enrol in ongoing clinical trials of ceritinib in France at that time (ASCEND-4 (NCT01828099) and ASCEND-5 (NCT01828112), see https://clinicaltrials.gov). All patients were pretreated with crizotinib.
Data collection and assessment
The patients enrolled on the TAU program were required to have a mandatory follow-up, as specified by the PUT, with prospective data collection (forms completed by the physician). Patient demographics and baseline clinical characteristics were recorded at the first visit, although smoking habit was not registered. Data were collected every 3 months for the following outcomes: ORR (proportion of patients with complete response (CR) or partial response (PR), as assessed by the investigator), stable disease (SD), progressive disease (PD), and safety.
Best tumour response was evaluated radiologically by the investigator (Response Evaluation Criteria in Solid Tumours (RECIST) version 1.1 was preferred). Confirmation of response was not required. Efficacy data were provided for all evaluable patients with ALK+ NSCLC. Safety assessments included monitoring of AEs, laboratory abnormalities and vital signs. All AEs were defined using the National Cancer Institute (NCI) Common Terminology Criteria for Adverse Events (CTCAE) (version 3.0). Patients were monitored until at least 28 days after the last dose of the study drug. The end date of treatment was considered as the date of the last dose in case of permanent discontinuation or the last assessment date (last date recorded within the PUT or the cut-off date). Patients were not followed up after completing treatment with ceritinib.
Safety analyses were reported for all patients with NSCLC (ALK+/ROS1+) who received ≥1 dose of ceritinib and safety data were collected from January 24, 2014 (date of named patient PUT implementation) until October 07, 2015. In accordance with the rules for reporting AEs within the scope of a TAU program, in most cases the prescriber reported events for which a causal relationship with ceritinib was suspected. AEs for which the prescriber did not consider a causal relationship were defined by default as “suspected” if the assessment was missing for serious AEs and as “unassessable” if the assessment was missing for nonserious AEs.
Statistical analysis
Descriptive statistics was used for analyses of patient and disease characteristics. The Kaplan–Meier method was used for estimating overall treatment duration and subgroup analyses. SAS version 9.3 (SAS, Cary, NC, USA) was used to perform all statistical calculations. Statistical analyses were performed by Novartis Pharma SAS, France.
Results
Patients’ disposition in the TAU
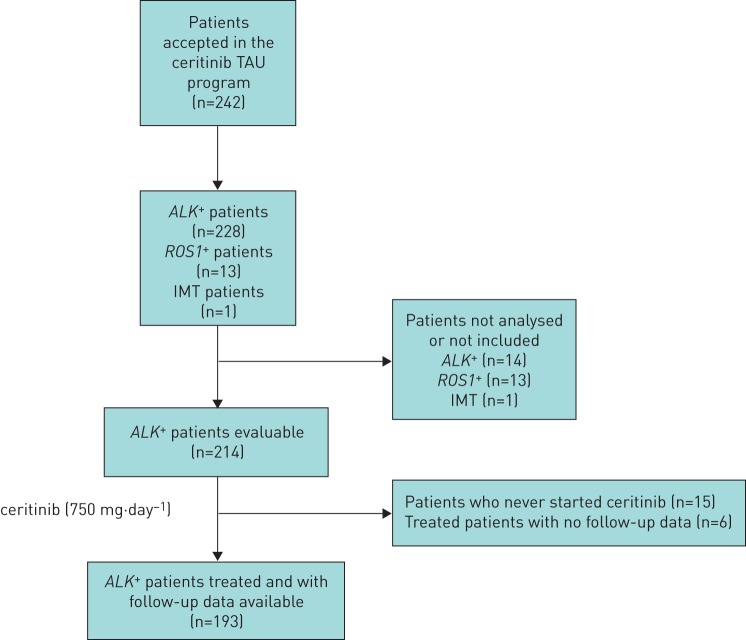
A total of 242 TAUs were granted from March 12, 2013 to August 05, 2015 (118 nominative TAUs and 124 cohort TAUs). Of the 242 patients included in the TAU program, 228 had ALK+ NSCLC, 13 had ROS1+ NSCLC and the remaining patient had an ALK+ inflammatory fibroblastic tumour (IMT) (figure 1). ROS1+ data are not communicated here. As of September 05, 2015, 214 patients with ALK+ NSCLC were followed up within the scope of the PUT (the remaining 14 patients included before PUT implementation were not analysed, in the context of French clinical research rules). Some 167 physicians across 106 hospitals enrolled ≥1 patient.
FIGURE 1.
Patient disposition in the temporary authorisation for use (TAU) programme. ALK+: anaplastic lymphoma kinase positive; ROS1+: ROS proto-oncogene 1 positive; IMT: inflammatory fibroblastic tumour
Of the 214 patients with ALK+ NSCLC, an initial form, a follow-up form, or a treatment discontinuation form were available for 193 of those treated with ceritinib (750 mg·day−1). Of these 193 patients, 117 (60.6%) discontinued the treatment. Reasons for discontinuation of treatment were disease progression (n=68), AEs (n=10), patient's request (n=7), death (n=19), and unknown reasons (n=13).
Baseline characteristics of ALK+ NSCLC patients (n=214)
Baseline characteristics of patients with ALK+ NSCLC at ceritinib introduction are shown in table 1. The median time between diagnosis and the start of treatment with ceritinib among the evaluable patients (n=206, 96.3%) was 23.2 months (range 1.7–192.8). The median age was 58.5 years (range 19.0–89.9) and 51.9% of patients were female. The majority of patients (70.8%) had an Eastern Cooperative Oncology Group (ECOG) performance status (PS) of 0−1. Histological type was available for 207 patients (96.7%) and 199 patients (96.1%) had adenocarcinoma. In total, 50.0% patients (105 out of 210) had brain metastases. All 213 patients for whom previous treatment data were available had received crizotinib in different lines of therapy. 15 patients (7.0%) received only one line of therapy (crizotinib) before ceritinib. A total of 97 patients (45.5%) received ceritinib as a third-line therapy after previously receiving chemotherapy and crizotinib, while 101 patients (47.4%) received ceritinib as a fourth-line therapy or further. Altogether, 73% of patients received ceritinib immediately after crizotinib. Furthermore, crizotinib was stopped due to AEs in 16 patients.
TABLE 1.
Baseline characteristics of patients with anaplastic lymphoma kinase positive (ALK+) non-small cell lung cancer (NSCLC)
| Characteristic | Patients (n=214) |
| Age years (n=211) | 58 (19–90) |
| Sex (n=214) | |
| Female | 111 (51.9) |
| ECOG performance status (n=205) | |
| 0–1 | 145 (70.7) |
| ≥2 | 60 (28.9) |
| Histology (n=207) | |
| Adenocarcinoma | 199 (96.1) |
| Undifferentiated carcinoma | 2 (1.0) |
| Other | 6 (2.9) |
| Number of metastatic sites (n=177) | |
| 0–2 | 117 (66.1) |
| ≥3 | 60 (33.9) |
| Metastatic localizations (n=210) | |
| Brain | 105 (50.0) |
| ALK test method (n=203) | |
| FISH only | 107 (52.7) |
| IHC only | 19 (9.4) |
| FISH and IHC | 74 (36.5) |
| Other | 3 (1.5) |
| Time from initial diagnosis to inclusion in TAU months (n=206) | 23.2 (1.7–192.8) |
| Prior medication regimens (including crizotinib) (n=213) | |
| 1 (crizotinib only) | 15 (7.0) |
| 2 | 97 (45.5) |
| >2 | 101 (47.4) |
| Median | 2 |
| Treatment line for crizotinib administration# (n=213) | |
| 1 | 27 (12.7) |
| 2 | 130 (61.0) |
| 3 | 35 (16.4) |
| >4 | 37 (17.4) |
| Crizotinib as last prior regimen# (n=213) | |
| Yes | 156 (73.2) |
| Duration of crizotinib treatment months (n=208) | 9.1 (0.1–52.0) |
| 25%–75% | 5.0–15.0 |
| Reason to stop crizotinib# (n=222) | |
| Disease progression | 203 (91.4) |
| Toxicity | 16 (7.2) |
| Other | 3 (1.4) |
Data are presented as n (%) or median (range) unless otherwise stated. ECOG: Eastern Cooperative Oncology Group; FISH: fluorescent in situ hybridisation; IHC: immunohistochemistry; TAU: temporary authorisation for use. #: crizotinib could be administered as more than one line/regimen for the same patient.
Efficacy for ALK+ NSCLC patients (n=193)
Of the 193 patients with ALK+ NSCLC who started ceritinib (90.2%), a documented radiological and/or clinical efficacy data assessment was available for 149 patients (77.2%). Of these, 8 patients (5.4%) had a CR, 70 (47.0%) had a PR and 34 (22.8%) had SD (table 2). On September 05, 2015 the median duration of ceritinib treatment (n=182) was 3.9 months (range 0.4–23.0; immature data, as only 123 patients were documented as permanent discontinuation). In the 71 patients followed up for ≥12 months, the median duration of ceritinib treatment was 5.5 months (range 0.4–23.0). A total of 16 patients (22.5%) were still receiving ceritinib or were censored at the cut-off date of September 05, 2015 (77.5% maturity) (table 3).
TABLE 2.
Physician-assessed response and treatment duration in patients with anaplastic lymphoma kinase positive (ALK+) non-small cell lung cancer (NSCLC)
| Radiological tumour evaluation | ALK+ NSCLC patients (n=149) |
| CR | 8 (5.4) |
| PR | 70 (47.0) |
| SD | 34 (22.8) |
| PD | 19 (12.8) |
| Not realised | 18 (12.1) |
| ORR | 78 (52.3) |
| DCR | 112 (75.2) |
| Duration months (n=182) | 3.9 (0.4–23.0) |
Data is presented as n (%) or median (range). CR: complete response; PR: partial response; SD: stable disease; PD: progressive disease; ORR: overall response rate; DCR: disease control rate.
TABLE 3.
Duration of ceritinib treatment according to duration of follow-up in patients with anaplastic lymphoma kinase positive (ALK+) non-small cell lung cancer (NSCLC)
| All evaluable ALK+ patients# | Patients with follow-up ≥6 months | Patients with follow-up ≥12 months¶ | |
| Subjects n | 182 | 136 | 71 |
| Duration months | 5.8 | 6.8 | 8.1 |
| 3.9 (0.4–23.0) | 5.5 (0.4–23.0) | 5.5 (0.4–23.0) |
Data are presented as mean or median (range) unless otherwise stated. #: discontinuation of ceritinib was documented for 117 out of 182 patients (64.2%) at the cut-off (64.3% maturity); ¶: 16 out of 71 patients (22.5%) were still receiving ceritinib or were censored at cut-off (77.5% maturity).
Table 4 shows efficacy data for patients according to ECOG PS and the presence or absence of brain metastases. Patients with ECOG PS 0–1 had a numerically higher ORR (55.0% versus 42.4%) and a longer duration of treatment (median duration 4.6 months versus 2.3 months) compared to those with ECOG PS ≥2. The ORR in patients with brain metastases was 48.6% while in patients with 1–3 metastatic localisations (n=138) and >3 localisations (n=12) it was 52.9% and 66.7%, respectively.
TABLE 4.
Physician-assessed response and treatment duration in patients with anaplastic lymphoma kinase positive (ALK+) non-small cell lung cancer (NSCLC) according to subgroups based on Eastern Cooperative Oncology Group (ECOG) performance status and presence of brain metastases
| Radiological tumour evaluation | ECOG performance status | Brain metastases | ||
| 0–1 (n=134) | 2–4 (n=51) | Present (n=97) | Absent (n=64) | |
| Assessed response | ||||
| Evaluable subjects | 109 | 33 | 72 | 50 |
| CR | 8 (7.3) | 0 (0.0) | 2 (2.8) | 4 (8.0) |
| PR | 52 (47.7) | 14 (42.4) | 33 (45.8) | 26 (52.0) |
| SD | 28 (25.7) | 4 (12.1) | 18 (25.0) | 6 (12.0) |
| PD | 11 (10.1) | 8 (24.2) | 8 (11.1) | 8 (16.0) |
| Not realised | 9 (8.3) | 6 (18.2) | 10 (13.9) | 5 (10.0) |
| Not evaluable | 1 (0.9) | 1 (3.0) | 1 (1.4) | 1 (2.0) |
| ORR | 60 (55.0) | 14 (42.4) | 35 (48.6) | 30 (60.0) |
| Treatment duration | ||||
| Subjects | 131 | 43 | 92 | 60 |
| Duration months | 4.6 (0.4–22.4) | 2.3 (0.4–19.9) | 3.3 (0.4–23.0) | 4.5 (0.4–22.2) |
Data are presented as n, n (%) or median (range) unless otherwise stated. CR: complete response; PR: partial response; SD: stable disease; PD: progressive disease; ORR: overall response rate.
Although ORR and treatment duration were similar in patients who received ≤2 previous and >2 previous lines of treatment, ORR was lower in patients who received prior crizotinib treatment for ≤5 months (36.1%) compared to those receiving >5 months of crizotinib treatment (>51.6%) (table 5). However, efficacy did not differ between patients treated immediately after receiving crizotinib (ORR 53.2%) compared to those who received crizotinib followed by chemotherapy (ORR 51.3%). Finally, among the 15 patients who received only one prior line of treatment (crizotinib only), ten patients were evaluable for efficacy and the ORR was 75.0%.
TABLE 5.
Physician-assessed response in patients with anaplastic lymphoma kinase positive (ALK+) non-small cell lung cancer (NSCLC) according to subgroups based on the number of previous lines of treatment, the duration of previous treatment with crizotinib and dose reduction
| Radiological tumour evaluation | Previous lines of treatment | Duration of previous crizotinib treatment# | Dose reduction¶ | |||||
| ≤2 lines (n=98) | >2 lines (n=94) | <Q1 (n=47) | Q1−Q2 (n=47) | Q2−Q3 (n=46) | ≥Q3 (n=49) | With dose reduction (n=84) | Without dose reduction (n=109) | |
| Assessed response | ||||||||
| Evaluable subjects | 72 | 76 | 36 | 31 | 35 | 43 | 74 | 75 |
| CR | 5 (6.9) | 3 (3.9) | 0 (0.0) | 4 (12.9) | 2 (5.7) | 2 (4.7) | 5 (6.8) | 3 (4.0) |
| PR | 35 (48.6) | 35 (46.1) | 13 (36.1) | 12 (38.7) | 20 (57.1) | 23 (53.5) | 36 (48.6) | 34 (45.3) |
| SD | 18 (25.0) | 15 (19.7) | 10 (27.8) | 5 (16.1) | 7 (20.0) | 10 (23.3) | 17 (23.0) | 17 (22.7) |
| PD | 10 (13.9) | 9 (11.8) | 10 (27.8) | 3 (9.7) | 3 (8.6) | 3 (7.0) | 8 (10.8) | 11 (14.7) |
| Not realised | 3 (4.2) | 13 (17.1) | 3 (8.3) | 5 (16.1) | 3 (8.6) | 5 (11.6) | 6 (8.1) | 10 (13.3) |
| Not evaluable | 1 (1.4) | 1 (1.3) | 0 (0.0) | 2 (6.5) | 0 (0.0) | 0 (0.0) | 2 (2.7) | 0 (0.0) |
| ORR | 40 (55.5) | 38 (50.0) | 13 (36.1) | 16 (51.6) | 22 (62.8) | 25 (58.2) | 41 (55.4) | 37 (49.3) |
| Treatment duration | ||||||||
| Subjects | 91 | 90 | 43 | 45 | 43 | 47 | 83 | 99 |
| Duration months | 3.8 (0.4–23.0) | 3.7 (0.4–22.4) | 2.3 (0.4–15.9) | 3.0 (0.4–23.0) | 5.1 (0.4–19.9) | 7.6 (0.9–22.2) | 4.9 (0.4–22.2) | 2.7 (0.4–23.0) |
Data are presented as n, n (%) or median (range). CR: complete response; PR: partial response; SD: stable disease; PD: progressive disease; ORR: overall response rate. #: <Q1 means <5 months of crizotinib, Q1–Q2 means 5 to <9.2 months of crizotinib, Q2–Q3 means 9.2 to <16 months of crizotinib >Q3 means >16 months of crizotinib. ¶: dose reduction is <750 mg·day−1 of ceritinib or a temporary discontinuation in the first 6 months of treatment.
The ORR was similar in patients with and without dose reduction for treatment-related AEs (55.4% and 49.3%, respectively). Furthermore, the median duration of treatment was not shorter in patients with dose reductions (4.9 months versus 2.7 months).
Safety of patients receiving ceritinib during the TAU program (n=225)
A total of 208 out of 225 patients with NSCLC (93.7%) were assessable for toxicity. Treatment-related AEs were reported in 56.7% of patients and the severity of AEs was assessed by physicians as severe in 35.6% of patients. The most common AEs suspected to be related to the study drug were diarrhoea (22.1%), hepatic toxicity (19.7%), nausea (16.8%) and vomiting (16.3%) (table 6).
TABLE 6.
Summary of adverse events (AEs) suspected of being related to the study drug
| Event | Any grade (n=208) | Severe (n=208) |
| Any AE | 138 (66.3) | 105 (50.3) |
| Any AE considered to be drug related | 118 (56.7) | 74 (35.6) |
| Drug reduction and/or interruption | 67 (32.2) | |
| Drug discontinuation | 13 (6.3) | |
| Most common AEs | ||
| Diarrhoea | 46 (22.1) | 12 (5.8) |
| Nausea | 35 (16.8) | 11 (5.3) |
| Vomiting | 34 (16.3) | 11 (5.3) |
| Hepatic toxicity (ALT/AST-increased or other) | 41 (19.7) | 26 (12.5) |
| Abdominal pain | 12 (5.8) | 1 (0.5) |
| Weight decrease | 12 (5.8) | 5 (2.4) |
| Asthenia | 10 (4.8) | 7 (3.4) |
| Decreased appetite | 9 (4.3) | 5 (2.4) |
| Creatinine increase/renal insufficiency | 14 (6.7) | 8 (3.8) |
| Fatigue | 6 (2.9) | 2 (1.0) |
| Pericardial tamponade/effusion | 5 (2.4) | 3 (1.4) |
| Hyperglycaemia | 3 (1.4) | 2 (1.0) |
| Dyspnoea | 3 (1.4) | 3 (1.4) |
| Thrombocytopenia | 4 (1.9) | 3 (1.4) |
| Skin disorders | 2 (1.0) | 0 (0.0) |
| Dehydration | 2 (1.0) | 2 (1.0) |
Data are presented as n (%). ALT: alanine aminotransferase; AST: aspartate aminotransferase.
Ceritinib was permanently discontinued in 13 patients (6.3%) due to the following: liver toxicity with fatal outcome and suspected interaction between ceritinib and levetiracetam (n=1), severe dehydration leading to kidney failure then acute respiratory failure after volume overload (n=1), acute respiratory failure (n=1), digestive disorders (n=8), hepatic cytolysis associated with digestive disorders (n=1) and thrombocytopenia (n=1). A total of 67 patients (32.2%) had dose reductions and/or dose interruptions due to AEs.
Overall, eight drug-related deaths were reported (four from the 13 patients who permanently discontinued ceritinib). These deaths were attributed as follows: hepatic failure (n=1), severe dehydration with renal and respiratory failure (n=1), acute respiratory distress (n=1), metastatic haemorrhage (n=1) and deaths of unknown reason (n=4).
Discussion
The TAU program for ceritinib is the largest real-life cohort for ceritinib use in crizotinib-pretreated ALK+ NSCLC patients outside of clinical trials [20, 21]. The diagnosis of ALK-rearrangement was robust and was performed in >90% of cases using the FISH break-apart method, which has been validated by a nationwide quality assurance program [22]. Only 9.4% of ALK+ disease was diagnosed only by IHC testing and, more recently, the use of IHC for first screening and then FISH for confirmation of positive ALK-cases has become a widely used algorithm in routine practice in France [23].
ALK+ NSCLC patients included in the TAU program had a poor prognosis profile and were heavily pretreated at the time of ceritinib introduction: 29.3% had PS ≥2 (including 22.4% PS 2, 4.9% PS 3 and 2% PS 4), 33.9% had ≥3 metastatic localisations, 51.2% had brain metastases and 47.4% received >2 prior treatment regimens (including crizotinib). Furthermore, 15 out of 214 patients with ALK+ NSCLC (7%) could not initiate ceritinib treatment due to death or rapid deterioration. These findings were very similar to those of crizotinib-pretreated ALK+ patients in the ceritinib registration trials (ASCEND-1 and ASCEND-2) and the phase 3 ASCEND-5 trial (table 7).
TABLE 7.
Characteristics and outcomes of patients from the French temporary authorisation for use (TAU) ceritinib study with other ceritinib data in crizotinib-pretreated patients with anaplastic lymphoma kinase positive (ALK+) non-small cell lung cancer (NSCLC)
| French TAU ceritinib study | ASCEND-1 (phase 1) | Gainor cohort | ASCEND-2 (phase 2) | ASCEND-5 (phase 3) | |
| Subjects n | 214 | 163 | 73# | 140 | 115 |
| ECOG % | |||||
| PS 0–1 | 70.8 | 87.1 | NA | 85.7 | 92.2 |
| PS 2–4 | 29.3 | 12.9 | NA | 14.3¶ | 7.8¶ |
| Prior lines % | |||||
| 1 | 7 | 16 | NA | 0 | 0 |
| 2 | 45.5 | 27.6 | NA | 43.6 | 87.8 |
| >2 | 47.4 | 56.0 | NA | 56.4 | 11.3+ |
| Brain metastases % | 51 | 61 | NA | 71 | 56.5 |
| ORR % | 52.4 | 56.4 | NA | 38.6 | 39.1 |
| DCR % | 75.2 | 74.2 | NA | 77.1 | 76.5 |
| Median ceritinib duration/exposure months | 3.9 (all patients) 5.5 (>12 months follow-up, 78% maturity) |
||||
| Median PFS months | NA | 6.9 | 7.8 | 5.7 | 5.4 |
| Median OS months | Not evaluable or not mature | 16.7 | 49.4 (from diagnosis) 30.3 (from crizotinib start) |
14.9 (42% maturity) | 18.1 (∼50% maturity) |
| Dose reduction/interruption % | 32.2 | 62 (reduction) 74 (interruption) |
NA | 54.3 | 80.0 |
| Discontinuation due to AEs % | 6.3 | 11 | NA | 7.9 | 5.2 |
ECOG: Eastern Cooperative Oncology Group; PS: performance status; NA: not available; ORR: objective response rate; DCR: disease control rate; PFS: progression-free survival; OS: overall survival; AE: adverse event. #: 71 subjects from ASCEND-1; ¶: PS 2; +: three prior lines of therapy.
The prior treatments were in line with the European Society for Medical Oncology (ESMO) recommendations for care in advanced NSCLC [24]; however, at that time, crizotinib was not authorised for use in first-line treatment in France. First-line treatment included platinum-based combination in 85.0% of cases with pemetrexed in 61.5% of patients and addition of bevacizumab in 18% of patients. A total of 10.6% of patients received platinum-based combination as a second-line treatment, although monochemotherapy was most commonly used (21.7%), with pemetrexed being administered in 9.6% of patients.
Patients in the TAU program were able to receive crizotinib for a median duration of 9.1 months (12.7% received crizotinib in first-line treatment, 61.0% in second-line treatment and 33.8% in ≥4 treatment lines). Duration of crizotinib exposure was longer than the 7.7 months PFS observed in the PROFILE 1007 trial [4], probably reflecting the wide use of crizotinib beyond progression in real-life settings and before access to ceritinib in the market. The majority of the TAU patients (73.2%) received crizotinib as the last regimen before ceritinib and very few of them received another ALK-targeted therapy (such as alectinib (n=10) or crizotinib plus HSP90 inhibitor (n=11)).
In the TAU program, ORR was reported in 52.4% of patients which is comparable to the ORR reported in the ASCEND-1 trial in ALK-inhibitor pretreated patients (56%) [12] and greater than the ORR in the ASCEND-2 and ASCEND-5 trials (38.6% and 39.1%, respectively) (table 7) [15, 17]. Although response was not reviewed centrally, investigators had to report tumour evaluation centrally every 3 months. Finally, although investigators usually overestimate the ORR compared to centralised review [25], the disease control rate (DCR) observed was very similar in both the TAU cohort and the ASCEND trials (table 7), confirming the similar efficacy of ceritinib both in real-life and in clinical trials.
As the TAU program involved collection of data but no monitoring of data after discontinuation of treatment it is difficult to calculate/estimate the survival outcomes (PFS and overall survival (OS)). As such, exposure duration is an acceptable estimate to compare with the PFS data in clinical trials. The median duration of ceritinib exposure for all evaluable patients in the TAU program was 3.9 months (range 0.4–23.0). Exposure duration was also calculated for patients who were followed up for ≥6 months and ≥12 months (which is similar to the follow-up for ASCEND-1) (table 7). With 74.7% and 39% of patients with ≥6 months and ≥12 months follow-up, respectively, the median ceritinib exposure in the TAU program was 5.5 months in both cohorts (similar to the PFS observed in the ASCEND trials) (table 7). Moreover, 22% of patients were still on ceritinib with a follow-up of more than 12 months.
Efficacy data were not reported for about 20% of the patients in the TAU program. It has to be noted that, being a compassionate use program, TAU methodology is different from clinical trial methodology (including the capacity to collect and/or clean follow-up data) and less robust. There is no monitoring and data are retrospectively collected from the TAU program charts. Furthermore, a significant proportion of patients were enrolled in the TAU program in the last weeks before closure, and, as such, follow-up and efficacy data were not available for all patients at the time of analysis.
Efficacy was observed in all patient subgroups in the TAU program. No major differences in ORR or the median duration of response of ceritinib were observed in relation to the presence or absence of brain metastases at inclusion and ≤2 or >2 previous lines of treatment. Patients with ECOG PS ≥2 had a lower ORR; however, comparison to other data is limited for these patients since they are rarely included in clinical studies.
Efficacy was similar (ORR 53% versus 51%) regardless of whether ceritinib was administered immediately after crizotinib or not but there was a possible trend for a longer treatment duration in the case of ceritinib being administered immediately (4.2 months versus 3.3 months, respectively). As suggested by the PROFILE 1007 and PROFILE 1014 trials for crizotinib [4, 5], delaying ALK-inhibitor exposure may decrease its efficacy (table 3). Finally, patients with longer response to crizotinib (>16 months) benefited longer from ceritinib in the TAU program (median duration of exposure: 7.6 months (range 0.9–22.2)). These results seem to confirm observations in clinical practice and are probably explained by the characteristics and aggressiveness of the tumours associated with maintained good/long response through each of the successive lines of ALK-inhibitors. Interestingly, it has also been reported that the efficacy of ALK-inhibitors (especially crizotinib) might be related to the type of ALK-rearrangement [26]. Comparative molecular analysis of patients with appropriate clinical profiles would be of interest at diagnosis and at disease progression.
The safety profile for ceritinib in the TAU program was similar to that reported in clinical trials of ceritinib. The most common AEs suspected to be related to the study drug were diarrhoea (22.1%), hepatic toxicity (19.7%), nausea (16.8%) and vomiting (16.3%) (table 6). Although, the TAU program was not able to properly capture the full spectrum of side-effects compared to a prospective clinical trial, it was interesting to note that 32.2% of patients had dose reductions and/or interruptions due to AEs compared to 62%, 54.3% and 73.0% in the ASCEND-1, ASCEND-2 and ASCEND-5 trials, respectively [12, 15, 17]. The lower percentage of dose reductions in the TAU program may be attributed to a better understanding by the physicians of the management of gastro-intestinal (GI) events, thereby preventing the need to reduce doses, and the sharing of best practice and emerging data on better management of GI issues. Only 13 patients (6.3%) permanently discontinued ceritinib in the TAU program. Of note, patients who had dose reductions did not experience a shorter duration of treatment than patients who did not (4.9 months versus 2.7 months in patients with no dose reduction), which reflects the usefulness of reducing dosage to maintain treatment in the case of unacceptable AEs (e.g. GI AEs and hepatitis). This finding also suggests that patients and physicians have together learned to better manage side-effects in the real-life use of ceritinib during the TAU program. It is to be hoped that progress will come from pharmacology data obtained from the ASCEND trials and better knowledge of the pharmacokinetics of ceritinib with food intake, as recently illustrated in the ASCEND-8 preliminary data (presented at the World Conference on Lung Cancer (WCLC) 2016), which suggests that taking ceritinib (450 mg·day−1) with food has similar exposure and significantly reduces GI toxicity [27].
Although the TAU program is different from the clinical trial setting where patients are followed even after treatment discontinuation, the patients included in the TAU program were of high unmet need and warranted early access to ceritinib treatment. In conclusion, ceritinib (750 mg·day−1) demonstrated similar efficacy for crizotinib-pretreated patients with ALK+ NSCLC in the TAU program as is seen in clinical trials and with a manageable safety profile.
Disclosures
C. Audigier-Valette 00058-2017_Audigier-Valette (1.2MB, pdf)
F. Barlesi 00058-2017_Barlesi (1.2MB, pdf)
B. Besse 00058-2017_Besse (1.2MB, pdf)
A. Buturuga 00058-2017_Buturuga (1.2MB, pdf)
J. Cadranel 00058-2017_Cadranel (1.2MB, pdf)
A.B. Cortot 00058-2017_Cortot (1.2MB, pdf)
E. Dansin 00058-2017_Dansin (1.2MB, pdf)
S. Friard 00058-2017_Friard (1.2MB, pdf)
H. Lena 00058-2017_Lena (1.2MB, pdf)
B. Mennecier 00058-2017_Mennecier (1.2MB, pdf)
D. Moro-Sibilot 00058-2017_Moro-Sibilot (1.2MB, pdf)
M. Perol 00058-2017_Perol (1.2MB, pdf)
K. Slimane 00058-2017_Slimane (1.2MB, pdf)
L. Thiberville 00058-2017_Thiberville (1.2MB, pdf)
A. Vergnenegre 00058-2017_Vergnenegre (1.2MB, pdf)
V. Westeel 00058-2017_Westeel (1.2MB, pdf)
Acknowledgements
The authors thank the participating patients, their families and all investigators. We also thank Pushkar Narvilkar and Shiva Krishna Rachamadugu (Novartis Healthcare Pvt. Ltd.) for providing medical editorial assistance with this manuscript.
Footnotes
Conflict of interest: Disclosures can be found alongside this article at openres.ersjournals.com
References
- 1.Barlesi F, Mazieres J, Merlio JP, et al. . Routine molecular profiling of patients with advanced non-small-cell lung cancer: results of a 1-year nationwide programme of the French Cooperative Thoracic Intergroup (IFCT). Lancet 2016; 387: 1415–1426. [DOI] [PubMed] [Google Scholar]
- 2.Shaw AT, Ou SH, Bang YJ, et al. . Crizotinib in ROS1-rearranged non-small-cell lung cancer. N Engl J Med 2014; 371: 1963–1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Camidge DR, Bang YJ, Kwak YL, et al. . Activity and safety of crizotinib in patients with ALK-positive non-small-cell lung cancer: updated results from a phase 1 study. Lancet Oncol 2012; 13: 1011–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shaw AT, Kim DW, Nakagawa K, et al. . Crizotinib versus chemotherapy in advanced ALK-positive lung cancer. N Engl J Med 2013; 368: 2385–2394. [DOI] [PubMed] [Google Scholar]
- 5.Solomon BJ, Mok T, Kim DW, et al. . First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N Engl J Med 2014; 371: 2167–2177. [DOI] [PubMed] [Google Scholar]
- 6.Katayama R, Shaw AT, Khan TM, et al. . Mechanisms of acquired crizotinib resistance in ALK-rearranged lung cancers. Sci Transl Med 2012; 4: 120ra17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ou SH, Jänne PA, Bartlett CH, et al. . Clinical benefit of continuing ALK inhibition with crizotinib beyond initial disease progression in patients with advanced ALK-positive NSCLC. Ann Oncol 2014; 25: 415–422. [DOI] [PubMed] [Google Scholar]
- 8.Weickhardt AJ, Scheier B, Burke JM, et al. . Local ablative therapy of oligoprogressive disease prolongs disease control by tyrosine kinase inhibitors in oncogene-addicted non-small-cell lung cancer. J Thorac Oncol 2012; 7: 1807–1814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Friboulet L, Li N, Katayama R, et al. . The ALK inhibitor ceritinib overcomes crizotinib resistance in non-small cell lung cancer. Cancer Discov 2014; 4: 662–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.US Food and Drug Administration. FDA broadens ceritinib indication to previously untreated ALK-positive metastatic NSCLC https://wayback.archive-it.org/7993/20170722151127/ https://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm560873.htm
- 11.European Medicines Agency (EMA) Zykadia. www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/003819/smops/Positive/human_smop_000796.jsp&mid=WC0b01ac058001d127 Date last accessed: March 10, 2015.
- 12.Shaw AT, Kim DW, Mehra R, et al. . Ceritinib in ALK-rearranged non-small-cell lung cancer. N Engl J Med 2014; 370: 1189–1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim DW, Mehra R, Tan DS, et al. . Activity and safety of ceritinib in patients with ALK-rearranged non-small-cell lung cancer (ASCEND-1): updated results from the multicentre, open-label, phase 1 trial. Lancet Oncol 2016; 17: 452–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Felip E, Orlov S, Park K, et al. . Phase 2 study of ceritinib in ALKi-naïve patients (pts) with ALK-rearranged (ALK+) non-small cell lung cancer (NSCLC): whole body responses in the overall pt group and in pts with baseline brain metastases (BM). Ann Oncol 2016; 27: Suppl. 6, 1208O. [Google Scholar]
- 15.Crinò L, Ahn MJ, De Marinis F, et al. . Multicenter phase II study of whole-body and intracranial activity with ceritinib in patients with ALK-rearranged non-small-cell lung cancer previously treated with chemotherapy and crizotinib: results from ASCEND-2. J Clin Oncol 2016; 34: 2866–2873. [DOI] [PubMed] [Google Scholar]
- 16.Soria JC, Tan DS, Chiari R, et al. . First-line ceritinib versus platinum-based chemotherapy in advanced ALK-rearranged non-small-cell lung cancer (ASCEND-4): a randomised, open-label, phase 3 study. Lancet 2017; 389: 917–929. [DOI] [PubMed] [Google Scholar]
- 17.Shaw AT, Kim TM, Crinò L, et al. . ASCEND-5: a randomised, phase 3 study of ceritinib versus chemotherapy in adult patients with ALK-rearranged non-small cell lung cancer, previously treated with chemotherapy and crizotinib. Lancet Oncol 2017; 18: 874–886. [DOI] [PubMed] [Google Scholar]
- 18.Cohen J, Faden L, Predaris S, et al. . Patient access to pharmaceuticals: an international comparison. Eur J Health Econ 2007; 8: 253–266. [DOI] [PubMed] [Google Scholar]
- 19.Degrassat-Théas A, Paubel P, Parent de Curzon O, et al. . Temporary authorization for use: does the French patient access programme for unlicensed medicines impact market access after formal licensing? Pharmacoeconomics 2013; 31: 335–343. [DOI] [PubMed] [Google Scholar]
- 20.Cadranel J, Park K, Arrieta O, et al. . Characteristics, treatment patterns, and survival among ALK+ non-small cell lung cancer (NSCLC) patients treated with crizotinib: A chart review study. Lung Cancer 2016; 98: 9–14. [DOI] [PubMed] [Google Scholar]
- 21.Gainor JF, Tan DS, De Pas T, et al. . Progression-free and overall survival in ALK-positive NSCLC patients treated with sequential crizotinib and ceritinib. Clin Cancer Res 2015; 21: 2745–2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lantuejoul S, Rouquette I, Blons H, et al. . French multicentric validation of ALK rearrangement diagnostic in 547 lung adenocarcinomas. Eur Respir J 2015; 46: 207–218. [DOI] [PubMed] [Google Scholar]
- 23.McLeer-Florin A, Moro-Sibilot D, Melis A, et al. . Dual IHC and FISH testing for ALK gene rearrangement in lung adenocarcinomas in a routine practice: a French study. J Thorac Oncol 2012; 7: 348–354. [DOI] [PubMed] [Google Scholar]
- 24.Besse B, Adjei A, Baas P, et al. . 2nd ESMO Consensus Conference on Lung Cancer: non-small-cell lung cancer first-line/second and further lines of treatment in advanced disease. Ann Oncol 2014; 25: 1475–1484. [DOI] [PubMed] [Google Scholar]
- 25.Tang PA, Pond GR, Chen EX. Influence of an independent review committee on assessment of response rate and progression-free survival in phase III clinical trials. Ann Oncol 2010; 21: 19–26. [DOI] [PubMed] [Google Scholar]
- 26.Duruisseaux M, Mc Leer-Florin A, Moro-Sibilot D, et al. . Are all ALK rearrangements created equal? Transl Cancer Res 2017; 6: S585–S586.28868241 [Google Scholar]
- 27.Cho BC, Kim D-W, Bearz A, et al. . ASCEND-8: a randomized phase 1 study of ceritinib, 450 mg or 600 mg, taken with a low-fat meal versus 750 mg in fasted state in patients with anaplastic lymphoma kinase (ALK)-rearranged metastatic non–small cell lung cancer (NSCLC). J Thorac Oncol 2017; 12: 1357–1367. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
C. Audigier-Valette 00058-2017_Audigier-Valette (1.2MB, pdf)
F. Barlesi 00058-2017_Barlesi (1.2MB, pdf)
B. Besse 00058-2017_Besse (1.2MB, pdf)
A. Buturuga 00058-2017_Buturuga (1.2MB, pdf)
J. Cadranel 00058-2017_Cadranel (1.2MB, pdf)
A.B. Cortot 00058-2017_Cortot (1.2MB, pdf)
E. Dansin 00058-2017_Dansin (1.2MB, pdf)
S. Friard 00058-2017_Friard (1.2MB, pdf)
H. Lena 00058-2017_Lena (1.2MB, pdf)
B. Mennecier 00058-2017_Mennecier (1.2MB, pdf)
D. Moro-Sibilot 00058-2017_Moro-Sibilot (1.2MB, pdf)
M. Perol 00058-2017_Perol (1.2MB, pdf)
K. Slimane 00058-2017_Slimane (1.2MB, pdf)
L. Thiberville 00058-2017_Thiberville (1.2MB, pdf)
A. Vergnenegre 00058-2017_Vergnenegre (1.2MB, pdf)
V. Westeel 00058-2017_Westeel (1.2MB, pdf)