Abstract
Background
Patients with inflammatory bowel disease (IBD) report a range of nutritional and dietary problems and high‐quality written information should be available on these. There is little research investigating the availability and quality of such information for patients with IBD.
Objective
This study assessed the type and quality of written information on nutrition and diet available to patients with IBD and the opinions of patients and health professionals.
Setting and Participants
Seventy‐two patients with IBD were recruited from a large gastroenterology outpatient centre in England. One hundred dietitians from across the United Kingdom were also recruited.
Methods
Face‐to‐face surveys were conducted with patients with IBD. Questions regarding the use, format and usefulness of dietary information received were probed. Dietitians were surveyed regarding written dietary information used in clinical practice. Samples of IBD‐specific dietary information used across the UK were objectively assessed using two validated tools.
Main Results
The majority of patients rated written information as ‘good’ or ‘very good’, with the most useful information relating to ‘general diet and IBD’. Forty‐nine (49%) dietitians reported gaps in written information available for patients with IBD. Fifty‐three different samples of IBD‐specific information sheets were returned, with widely variable objective quality ratings. Commercially produced written information scored greater than locally produced information (BMA tool, P < 0.05).
Conclusions
Patient access to high‐quality, written, IBD‐specific dietary information is variable. IBD‐specific written nutrition information needs to be developed in accordance with validated tools to empower patients, encourage self‐management and overcome nutritional implications of IBD.
Keywords: Crohn's disease, food, inflammatory bowel disease, nutrition, patient experience, patient information, ulcerative colitis
Introduction
Inflammatory bowel disease (IBD) is a chronic relapsing remitting condition characterized by inflammation of the gastrointestinal tract and consists of both Crohn's disease (CD) and ulcerative colitis (UC). Symptoms include abdominal pain and discomfort, diarrhoea, rectal bleeding, fatigue and complications that may require surgery, such as fistula, stricture and bowel obstruction. IBD can have a major impact on patients' lives, including disruption of daily activities, social interactions, intimacy and physical and psychological function.1, 2 Food, nutrition and diet are important aspects of an individual's psychological, social and cultural well‐being and therefore linked to health‐related quality of life (QOL).3 These too may also be disturbed in patients with IBD, who have reported the effect of food and nutrition problems on weight, triggering gastrointestinal symptoms and micronutrient deficiencies, many of which had a further impact on their social function.4
In addition to the psychosocial effects of food and nutrition in IBD, malnutrition is common, with nutritional assessment and therapy being an important aspect of IBD management.5 Malnutrition may occur in up to 85% of IBD patients with protein energy malnutrition and weight loss being the most common.6 Many factors contribute to this, including inadequate dietary intake, increased nutrient requirements and gastrointestinal malabsorption, and these may depend on the nature of the disease, its location, pattern, activity and presence of surgical resection.7
Nutritional interventions form part of the overall treatment regimen in patients with IBD. For example, enteral nutrition is the replacement of all eating and drinking with a nutritionally complete liquid formula consumed orally or delivered via a feeding tube and is used for the primary treatment8 or for maintenance of remission9 in CD. However, nutritional problems are common during its use, and nutrition support is incorporated into IBD standards in the United Kingdom (UK) and new national guidelines for the dietary management of CD.6, 10, 11 Dietary interventions can also be used to manage symptoms in patients with a stoma12 or to prevent or reverse undernutrition caused by underlying physiological mechanisms or patient self‐restriction.13, 14 As such, diet and nutrition is an integral component of IBD management.
Educating patients with IBD about their disease increases knowledge.15 Knowledge confers a sense of control, enhances patients' ability to cope with chronic disease16 and is an important step in empowering them to increase their independence and self‐management.17 Education may be delivered through a variety of methods, including verbal, written or online information that can be given by a range of health professionals, or through patient support groups and charities. In the United Kingdom, the IBD Standards Working Group state that every IBD service should provide written information, education and support alongside other sources of information.11 Written information provides a permanent record and adjunct to support verbal education and the opportunity to increase knowledge above that acquired through verbal information alone,18 improve compliance with treatments19 and increase satisfaction with care.20
It is UK policy to ensure health‐care information available to the public should be of high quality, including that it should be available in a variety of formats, tailored to individual needs, evidence based and provided in a way that is comprehensible and accessible to patients.21 There are a number of instruments available with which to assess the quality of written patient information. These tend to evaluate a range of aspects, including the content, layout, readability and design.
Food and nutrition have a profound impact on the lives of patients with IBD due to the impact of eating on symptoms, the psychosocial impact of food avoidance, the high prevalence of nutrition‐related problems and the role of nutrition in the management of disease. Doctors, nurses and dietitians use written information regarding food and nutrition when educating patients with IBD, although these are usually designed by dietitians. No studies have been conducted to investigate the types and quality of nutrition‐related written information provided to patients with IBD. Therefore, the aim of this study was to investigate access to, and quality of, nutrition‐related information available for patients with IBD in the United Kingdom through surveys of patients and dietitians and an objective assessment of the quality of written information using two validated instruments.
Methods
This research consisted of two components: (i) a questionnaire survey about the perceptions of both patients and dietitians regarding access to, and quality of, nutrition‐related information available for IBD; and (ii) the use of two validated instruments to undertake an objective assessment of the quality of written information available for IBD throughout the United Kingdom.
Questionnaire surveys
A questionnaire survey of patients with IBD was undertaken in adults from outpatient gastroenterology clinics at a local NHS hospital. Patients were approached, and those willing to participate were recruited to individual face‐to‐face interviews conducted by two researchers. Adults (≥18 years) with an existing diagnosis of CD or UC and a willingness to participate were included. There were no exclusion criteria to maximize population representativeness. Every effort was made to recruit all those eligible to minimize selection bias. The interviews were conducted prior to or immediately following each patient's consultation. Assurances of confidentiality and anonymity were given, and all patients provided informed consent to participate. The Research and Ethics Committee at the local hospital deemed this questionnaire survey a needs assessment and service evaluation, and thus, advised ethical approval was not required.
The patient questionnaire was developed following a literature search regarding food and nutrition problems, information resources and health service provision in IBD. The questionnaire was pretested amongst a small group of patients prior to final modifications. The final version surveyed how health services addressed food and nutrition problems in IBD, in particular the access to and quality of the information sources used. The questionnaire consisted of closed questions (e.g. the format in which dietary information had been provided), scaled questions (e.g. satisfaction with the information provided) and open questions (e.g. aspects of written information that were most important to patients). Demographic and clinical information was also collected.
A nationwide questionnaire survey of dietitians specializing in gastroenterology was undertaken across the whole of the United Kingdom. All hospital gastroenterology departments in the United Kingdom were identified from the national IBD audit database.22 A variety of approaches were adopted to maximize response rates to ensure representativeness.23 Each department was contacted via telephone for the name of the gastroenterology specialist dietitian responsible for IBD so that each dietitian could be sent a personalized introduction letter and questionnaire. The postal questionnaire specified a 1‐month deadline and included the opportunity of entering two prize‐draws, together with a stamped addressed return envelope. Dietitians were provided with an assurance of confidentiality and anonymity. The questionnaire consisted of eleven questions, including a mixture of closed and open questions surveying the type of information they provided to patients with IBD, the format and place of production, as well as factors that influence their choice of written information, language and overall opinions on the information provided.
Objective quality assessment of written information
Dietitians who were sent a questionnaire were also asked to return hard copies of all written information relating to food, nutrition or diet they used that was specific to IBD. Generic resources not specific to IBD (e.g. general advice on low‐fibre diets) were excluded.
Following an extensive review of the literature, two validated tools were used to objectively assess the quality of the written information resources returned: the ‘British Medical Association (BMA) Patient Information Appraisal Form’24 and the ‘Ensuring Quality of Information for patients' tool (EQIP).25 These tools were judged to include all domains relevant to quality and have good psychometric properties.
The tools assess the following domains of quality: ‘design’ (e.g. visual appearance, language and imagery), ‘development’ (e.g. authors and end‐users, date and version clearly stated), ‘general content’ (e.g. scope outlined, clear information on condition and management, QOL information, glossary of terms), ‘scientific content’ (e.g. is the information evidence based?) and ‘further contacts’ (e.g. author or source information, further useful reading). The domains were rated using Likert scales ranging from 1 (poor) to 5 (excellent) (EQIP) or a score (BMA). The BMA tool score was converted to Likert scales to allow comparison with the EQIP tool. All written IBD‐specific information resources relating to food and nutrition were objectively assessed for quality using both tools by the same researcher.
Statistical analysis
All statistical analyses were performed using spss 17.0 software (SPSS Inc, Chicago, IL, USA). Complete double data entry was undertaken to check for accuracy and consistency. Continuous data are presented as mean (SD) and compared between subgroups using unpaired t‐tests. Categorical data are presented as n (%) or n/N (%) and compared using the chi‐squared test. The Kendall's tau correlation coefficient was used to determine the strength and significance of association between the BMA and EQIP tools in scoring the same written information. A P‐value ≤ 0.05 was considered statistically significant. Responses to open questions were categorized into common themes.
Results
Survey of patients with IBD
Seventy‐two (83%) patients with IBD completed the interview‐administered questionnaire, 47 with CD and 25 with UC. Fifteen (17%) patients declined to participate. Demographic and clinical characteristics were similar between CD and UC groups, with the exception of previous surgery (Table 1).
Table 1.
Demographic and clinical characteristics of participants
| Characteristics | CD (N = 47) | UC (N = 25) | Total IBD (N = 72) |
|---|---|---|---|
| Age: mean (SD) years | 38.7 (11.5) | 40.1 (12.8) | 39.2 (11.9) |
| Gender: n (%) | |||
| Female | 29 (62) | 11 (44) | 40 (56) |
| Male | 18 (38) | 14 (56) | 32 (44) |
| Ethnicity: n (%) | |||
| White | 38 (81) | 18 (72) | 56 (78) |
| Non‐white | 9 (19) | 7 (28) | 16 (22) |
| Time since diagnosis: n (%) | |||
| ≤10 years | 22 (47) | 14 (56) | 36 (50) |
| >10 years | 25 (53) | 11 (44) | 36 (50) |
| Symptoms in previous year: n (%) | |||
| None | 4 (9) | 4 (16) | 8 (11) |
| Some symptoms always present | 18 (38) | 9 (36) | 27 (38) |
| Flare‐ups and symptom‐free periods | 25 (53) | 12 (48) | 37 (51) |
| Self‐reported disease severity in last year: n (%) | (N = 44) | (N = 21) | (N = 65) |
| Mild | 9 (21) | 6 (29) | 15 (23) |
| Moderate | 15 (34) | 9 (43) | 24 (37) |
| Severe | 20 (46) | 6 (29) | 26 (40) |
| Currently in remission: n (%) | 24 (52) | 15 (65) | 39 (57) |
| Hospital stay in previous year: n (%) | 21 (45) | 6 (24) | 27 (38) |
| Previous surgerya: n (%) | 28 (60) | 3 (12) | 31 (43) |
| Previous or current stoma: n (%) | 9 (19) | 3 (12) | 12 (17) |
Significant difference CD vs. UC: (P < 0.001).
Of those patients who reported previous or current problems with food and nutrition (59/72; 82%), between 43 and 83% had discussed these with a health professional, such as their doctor or nurse, depending upon the symptom (weight changes 36/60, 60%; lethargy/tiredness 32/61, 52%; trigger foods 27/57, 47%; gut symptoms 46/61, 75%; social activities 20/46, 43%; and micronutrient deficiencies 35/42, 83%). However, only 2‐22% had discussed with a dietitian the issues of weight change (13/60, 22%), lethargy/tiredness (3/61, 5%), trigger foods (11/57, 19%), gut symptoms (1/61, 2%), social activities (3/46, 6%) and micronutrient deficiencies (1/42, 2%). Thirty‐four (47%) patients interviewed had specifically seen a dietitian for dietary advice regarding their IBD. Of those who had not seen a dietitian for their IBD, 31/38 (82%) felt this would have been useful in the past or may be in the future.
Half (36, 50%) of patients reported having received IBD‐specific food and nutrition information. Of these patients, 29 (81%) had received this information verbally, 25 (69%) had received written information, 13 (36%) had been recommended to contact an IBD support group, and 6 (17%) had been recommended a website to visit regarding food and nutrition and their IBD.
Seventeen (24%) respondents were members of patient support groups, either recommended through their IBD service or independently sought. In all cases, this was Crohn's and Colitis UK. Of these, 4 (24%) patients had used their helpline for support and advice regarding food and nutrition, and 4 (24%) had attended a patient support group where food and nutrition was discussed. Twenty‐four (33%) patients were interested in attending a group session that focused on food and nutrition in the future, and three made comments regarding the possible use of the Internet forums for information exchange.
The nutrition information provided verbally, in writing, through support groups or websites was most commonly rated as either ‘good’ or ‘very good’ (Table 2). Due to the low numbers of responses in each cell, it was not possible to statistically determine differences between the ratings for different sources of information.
Table 2.
Patient quality ratings of nutrition information received or recommended
| Type of information | Poor n (%) | Satisfactory n (%) | Good n (%) | Very good n (%) |
|---|---|---|---|---|
| Verbal advice (N = 29) | 2 (7) | 3 (10) | 10 (34) | 14 (48) |
| Written information (N = 25) | 1 (4) | 2 (8) | 7 (28) | 15 (60) |
| Websites (N = 6) | 0 (0) | 0 (0) | 3 (50) | 3 (50) |
| Patient support group (N = 13) | 0 (0) | 0 (0) | 6 (46) | 7 (54) |
Of all the patients interviewed, 10 (14%) had a first language other than English. Three patients would have preferred food and nutrition information in their first language.
During open questioning regarding the information provided to patients, a number of common themes spontaneously emerged. These included (i) the importance of individualization and personalization of information, as IBD was identified as a very ‘personal journey’, (ii) the utility of discussing food and nutrition with other family members who also had IBD and (iii) the use of the Internet forums for shared discussion, specifically Facebook™ and Crohn's and Colitis UK.
Survey of dietitians specializing in IBD
Of the 266 questionnaires mailed to dietitians, 100 (38%) eligible questionnaires were returned. Ninety‐seven (97%) worked with adults with IBD and 13 (13%) worked with children and adolescents with IBD (not mutually exclusive).
In relation to food and nutrition information for IBD, 92 (92%) reported that they provide written information and 44 (44%) recommend specific websites to visit. The most popular website recommended was Crohn's and Colitis UK (15, 15%), followed by CORE (3, 3%), the IBD Club (2, 2%), the Ileostomy Association and ActZone (both 1, 1%). The majority of dietitians recommended patients join support groups ‘sometimes’ (53, 53%), ‘most of the time’ (23, 23%) or ‘always’ (13, 13%). Crohn's and Colitis UK was the most popular support group, recommended by 86 (86%) dietitians, followed by the Ileostomy Association, recommended by 15 (15%) dietitians.
Although 92 (92%) dietitians provided written information to patients with IBD, only 77 (77%) used written information that was specific to IBD (Fig. 1). A number of factors influenced their choice of written information, and the five most frequently cited were as follows: ‘being easy to read’ (51, 51%), ‘avoiding misleading advice’ (44, 44%), ‘it contains clear explanation of IBD’ (42, 42%), ‘the availability of written information’ (n = 40, 40%) and ‘written information being up to date’ (38, 38%). Only 11 (11%) dietitians considered the extent to which written information ‘considered individual needs’.
Figure 1.
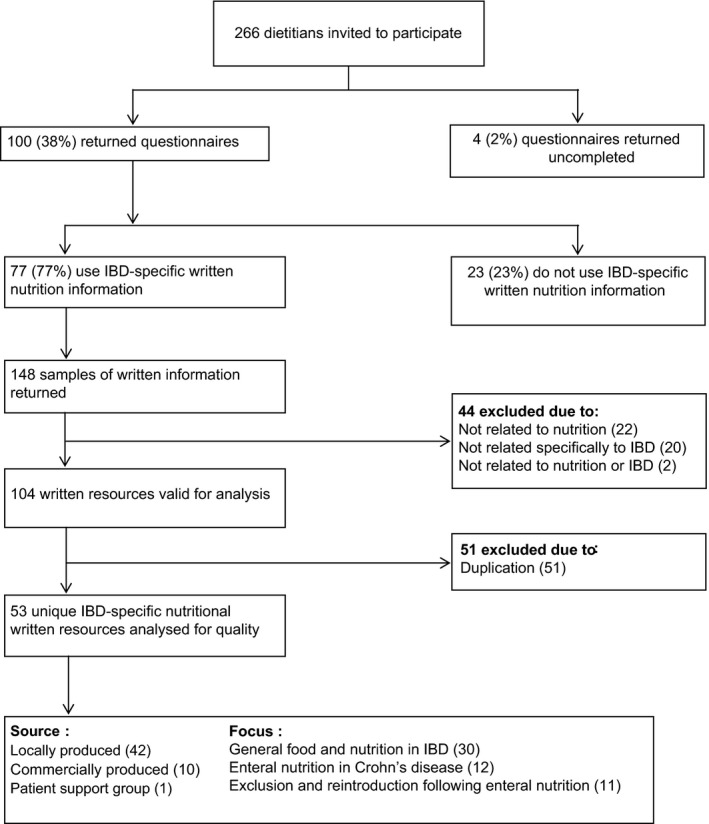
Responses from the UK national evaluation of nutritional IBD resources.
The majority of dietitians (73, 73%) reported they ‘sometimes’, ‘mostly’ or ‘always’ counselled patients with IBD from different ethnic groups. However, only seven (7%) dietitians had access to IBD‐specific written information in languages other than English, including Gujarati, Hindi/Urdu, Punjabi, Welsh, Arabic and Somali. The majority reported not having access (78, 78%) or not knowing whether they had access (13, 13%) to written information in languages other than English, although nine (9%) indicated that there was little need for this in their hospital population.
The IBD‐specific written information relating to food and nutrition that was most frequently considered the most useful was ‘Food and IBD’ produced by Crohn's and Colitis UK (n = 22, 22%). This was followed by industry‐funded resources relating specifically to enteral nutrition (n = 13, 13%). Forty‐nine (49%) dietitians considered there to be gaps in access to IBD‐specific written information, with the most common being in relation to ‘general diet and IBD’ (n = 15, 15%).
Objective quality assessment of written information
One hundred and four valid samples of written information regarding food or nutrition in IBD were returned (Fig. 1). These comprised 53 unique items of written information of which 42 (79%) were produced locally by individual hospitals, 10 (19%) were produced commercially, and one was from a patient support group.
Mean scores calculated for each domain of the BMA and EQIP evaluation tools and total score for quality assessment of the written nutritional information are recorded in Table 3. The BMA tool rated the ‘development’ (mean score, 49%), and the EQIP tool rated the ‘design’ (mean score 81%) of the written information highest.
Table 3.
Tool subgroups ranked from highest to lowest mean score
| Domain | BMA quality assessment tool, per cent score | EQIP quality assessment tool, per cent score | ||
|---|---|---|---|---|
| Mean (SD) | Min–Max | Mean (SD) | Min–Max | |
| Development | 49 (15) | 33–87 | 38 (20) | 0–100 |
| General content | 24 (12) | 0–47 | 56 (17) | 19–88 |
| Design | 38 (11) | 17–66 | 81 (12) | 50–100 |
| Scientific content | 33 (19) | 0–67 | – | – |
| Further contacts | 32 (21) | 0–67 | 51 (35) | 0–100 |
| Total | 34 (9) | 14–54 | 62 (11) | 32–81 |
There was wide variation in the scores between all items of written information in each domain. For example, the scores for ‘scientific content’ as rated by the BMA tool ranged from 0 to 67% between resources, and the scores for ‘general content’ as rated by the EQIP tool ranged from 19 to 88% (Table 3).
For the same item of written information, there was a significant correlation in scores given by the BMA and the EQIP tools, with Kendall's tau correlation coefficient ranging from 0.479 to 0.713, depending upon the domain (all P < 0.001). Despite this significant correlation, the EQIP tool resulted in higher scores overall than the BMA tool for the same written information.
The domain and total scores were compared for locally and commercially produced written information (Table 4). When compared with locally produced resources, commercially produced written information consistently scored significantly higher for ‘development’ (P = 0.024), ‘general content’ (P = 0.033), ‘further contacts’ (P = 0.01) and total score (P = 0.018) using the BMA tool, but only for ‘development’ (P = 0.01) using the EQIP tool.
Table 4.
Comparison of locally and commercially produced resources
| Domain | BMA quality assessment tool per cent score, mean (SD) | EQIP quality assessment tool per cent score, mean (SD) | ||||
|---|---|---|---|---|---|---|
| Locally produced (n = 42) | Commercially produced (n = 11) | P‐value | Locally produced (n = 42) | Commercially produced (n = 11) | P‐value | |
| Development | 47 (15) | 58 (14) | 0.024 | 34 (18) | 53 (19) | 0.011 |
| General content | 22 (12) | 30 (12) | 0.033 | 57 (16) | 60 (21) | 0.269 |
| Design | 37 (11) | 38 (8) | 0.783 | 81 (13) | 79 (10) | 0.503 |
| Scientific content | 31 (18) | 41 (23) | 0.072 | – | – | – |
| Further contacts | 28 (18) | 48 (24) | 0.010 | 51 (35) | 53 (40) | 0.905 |
| Total | 32 (8) | 40 (10) | 0.018 | 61 (11) | 65 (10) | 0.436 |
Discussion
The purpose of this research was to investigate the access to and quality of IBD‐specific food and nutrition information available for patients with IBD in the United Kingdom. This was achieved through a survey of both patients and dietitians, as well as an objective assessment of the quality of written information. Despite high reported rates of diet and nutrition problems in IBD,4 patients in this study reported variable rates of discussing these issues with any health professional. Where provided, verbal and written nutrition and dietary information were the most common forms provided to patients, and they rated the information they received highly. However, patients raised negative comments regarding the lack of sufficient information and its individualization, reflecting their personal needs and concerns. Interestingly, dietitians rarely cited individualization as an important characteristic of written information, although this might reflect its use as a reinforcement of individualized verbal information.
The benefits of individualized information and education have been demonstrated in a number of studies outside of IBD, for example improving blood lipid levels26 and maintenance of normoglycaemia in type 2 diabetes.27 Personalized nutrition advice in conjunction with written information for patients with intestinal failure has been found to significantly improve patient knowledge of their treatment regimen.17 Individualized advice has been shown to be an essential prerequisite to greater patient involvement in disease management in UC,28 and a study of communication preferences in a multinational community‐based cohort of patients with IBD concluded that individual attitudes and preferences must be considered, with a greater role for the use of electronic media.29
Less than a quarter of patients reported to be members of a support group or had used a helpline for food and nutrition‐related issues. Despite this, Crohn's and Colitis UK, the most popular patient support group for IBD in the United Kingdom, reports that approximately 16% of calls received to their patient support line relate to food or nutrition (personal communication). A small study found that patients who were members of this support group had higher IBD knowledge scores than non‐members.30 There is little published evidence for the use of support groups in IBD, particularly in relation to food and nutrition. However, these may be useful forums for sharing and disseminating information, and this is an area for future research.
A number of patients spoke a first language other than English; however, few preferred the information to be in their first language. This might reflect response bias to the face‐to‐face questionnaire interview, which was undertaken in English and meant that participants had to be reasonably fluent in this language. The availability of information in the appropriate language encourages understanding and compliance,31 and there is a need for services to assess the requirements of their local population regarding foreign language resources. Dietitians working in areas with low demand for foreign language resources may occasionally require access to such written information for a specific patient, and this could be facilitated through departments where demand is higher sharing resources with them.
In the majority, both verbal information and written information were provided to patients, complying with the UK IBD Standards Working Group recommendation that every IBD service should provide written patient information and education to support other information types. During consultations, patients prefer communication that is patient‐centred and supported by written information32, and health professionals can ascertain a patient's beliefs, concerns and expectations and indicate how the printed information matches their needs.33
The Crohn's and Colitis UK ‘Food and IBD’ booklet was reported as the most useful resource and was assessed to be of very good quality by both the BMA and EQIP tools. The reported gaps in IBD‐specific information included the lack of general food and nutrition information and unbiased information regarding enteral formula for primary management of CD. As this research was conducted, national evidence‐based written resources for diet and CD have been produced by the IBD section of the Gastroenterology Specialist Group of the British Dietetic Association,10 which begins to address some of the gaps identified in patient information resources. A further gap identified was for information regarding probiotics and prebiotics, and it has previously been shown that patients with IBD commonly use probiotics but that information about them is frequently obtained from commercial advertising rather than health professionals.34
Many people with IBD use the Internet to gain information, with patient‐focused education being widely available in online forums, support groups and on video clips.35 However, a recent study has shown that clips on one public website were a popular but poor quality source of education for people with IBD.36 The UK IBD Standards Working Group advocates recommendations to reliable websites and support groups; however, only a minority of dietitians in the present survey did so. The quality of written information available online was not reviewed in this study, and this is an important area for future research and should involve patients with IBD. Internet use is negatively associated with age and positively associated with education level in patients with IBD, and Web‐based IBD information may become increasingly important in the future.29, 37 It holds many benefits for health‐care services as an inexpensive means of disseminating information, which can be sought anonymously without the patient feeling inhibited or embarrassed. It also allows the user to engage with the information and other users with similar conditions.38, 39
An objective assessment of the quality of IBD‐specific nutrition information that is used throughout the United Kingdom was undertaken using two validated quality assessment tools. ‘Design’ scored highly, indicating ease of navigation with an appealing layout and imagery. However, it is of great concern that ‘general content’ and ‘scientific content’ scored poorly for some written information resources. Inaccurate information has the potential to cause harm and may inhibit patient ability to meet diet therapy goals. It is unsurprising that commercially produced written resources scored significantly higher for many domains as producing high‐quality information resources requires significant resources, and commercial companies may have greater resources than hospital departments in the United Kingdom for producing such information.
Previous research has highlighted the value of involving laypeople in the development of written information.40 Involving patients and care staff in setting criteria for development and assessment of such resources might enhance the provision of high‐quality, relevant and patient‐focused resources. Patient involvement can be achieved via focus groups, which enable capture of in‐depth views of a group of individuals and allow guided critique of existing resources. This method has been trialled in those with irritable bowel syndrome.41
Strengths and limitations
The patient interviews were restricted to a single large tertiary referral centre in the United Kingdom and as such the findings may not apply to a wider population. However, research in this area is limited, and the findings provide insights into potentially important areas for further research and written information development. The structured interview format may yield fewer participants than alternative methods, such as postal or telephone surveys; however, it does allow for more accurate and detailed data collection. For the dietitian survey, response bias may result in those with better access to quality written information to respond. As such, results may overestimate the amount and quality of information generally available to people with IBD.
The objective assessment of the quality of written information utilized two different validated tools, as neither were deemed to cover all aspects of quality and because any scoring system to rate quality is likely to have limitations in its application. A major strength of this study is the triangulation of methods used to measure access and quality of information, through survey of patients and dietitians and through direct objective assessment of written information. Future studies that utilize qualitative methods to explore patients' access to information relating to food and nutrition in IBD would allow more in‐depth analysis.
Conclusions
Patients with IBD value written information to support individualized tailored dietary advice provided by health professionals; however, patients and dietitians identify variable access to high‐quality written information resources. Improvements in some written resources are required, and the finding that some contain inaccurate information is of concern. Future development of IBD‐specific high‐quality written information is required with the aim to empower patients, encourage self‐management and overcome the many possible nutritional implications of IBD. These resources should be produced in collaboration with patients and health professionals to ensure specific needs and concerns are met. The use of the Internet and support groups for the dissemination and sharing of information are underused in clinical practice and should be explored in future research in this area.
Sources of funding
This research received no specific grant from any funding agency in the public, commercial or not‐for‐profit sectors.
Author contributions
AP participated in the design of the study, undertook patient recruitment, data analyses and interpretation and drafted the manuscript. AM participated in the design of the study, undertook patient recruitment, data analyses and interpretation. KW, MCEL and DR participated in the design of the study, data interpretation and contributed to drafting the manuscript. All authors read and approved the final manuscript.
Conflict of interests
The authors declare that there are no known conflict of interests associated with this publication.
Acknowledgements
The authors are grateful to the patients for their participation in this study and the clinical staff at the relevant hospitals for facilitating this research. The statistical advice of Peter Milligan (King's College London) is gratefully acknowledged.
References
- 1. Magro F, Portela F, Lago P, Deus J, Cotter J, Cremers I et al Inflammatory bowel disease: a patient's and caregiver's perspective. Digestive Diseases and Sciences, 2009; 54: 2671–2679. [DOI] [PubMed] [Google Scholar]
- 2. Ghosh S, Mitchell R. Impact of inflammatory bowel disease on quality of life: results of the European Federation of Crohn's and Ulcerative Colitis Associations (EFCCA) patient survey. Journal of Crohns and Colitis, 2007; 1: 10–20. [DOI] [PubMed] [Google Scholar]
- 3. Barr JT, Schumacher GE. The need for a nutrition‐related quality‐of‐life measure. Journal of the American Dietetic Association, 2003; 103: 177–180. [DOI] [PubMed] [Google Scholar]
- 4. Prince A, Whelan K, Moosa A, Lomer MC, Reidlinger DP. Nutritional problems in inflammatory bowel disease: the patient perspective. Journal of Crohns and Colitis, 2011; 5: 443–450. [DOI] [PubMed] [Google Scholar]
- 5. Mowat C, Cole A, Windsor A, Ahmad T, Arnott I, Driscoll R et al Guidelines for the management of inflammatory bowel disease in adults. Gut, 2011; 60: 571–607. [DOI] [PubMed] [Google Scholar]
- 6. Lomer MC. Dietary and nutritional considerations for inflammatory bowel disease. Proceedings of the Nutrition Society, 2011; 70: 329–335. [DOI] [PubMed] [Google Scholar]
- 7. Urbano AP, Sassaki LY, Dorna MS, Carvalhaes MA, Martini LA, Ferreira AL. Nutritional intake according to injury extent in ulcerative colitis patients. Journal of Human Nutrition and Dietetics, 2013; 26: 445–451. [DOI] [PubMed] [Google Scholar]
- 8. Zachos M, Tondeur M, Griffiths AM. Enteral nutritional therapy for induction of remission in Crohn's disease. Cochrane Database of Systematic Reviews, 2007; 24: CD000542. [DOI] [PubMed] [Google Scholar]
- 9. Akobeng AK, Thomas AG. Enteral nutrition for maintenance of remission in Crohn's disease. Cochrane Database Systematic Reviews, 2007: CD005984. [DOI] [PubMed] [Google Scholar]
- 10. Lee J, Allen R, Ashley S, Becker S, Cummins P, Gbadamosi A et al British Dietetic Association evidence‐based guidelines for the dietary management of Crohn's disease in adults. Journal of Human Nutrition and Dietetics, 2014; 27: 207–218. [DOI] [PubMed] [Google Scholar]
- 11. IBD Standards Working Group . Standards for the healthcare of people who have inflammatory bowel disease (IBD), 2013. Available at: http://www.ibdstandards.org.uk/uploaded_files/IBDstandards.pdf, accessed 10 April 2014.
- 12. Zutshi M, Hull TL, Hammel J. Crohn's disease: a patient's perspective. International Journal of Colorectal Disease, 2007; 22: 1437–1444. [DOI] [PubMed] [Google Scholar]
- 13. Fletcher PC, Jamieson AE, Schneider MA, Harry RJ. ‘I know this is bad for me, but…’: a qualitative investigation of women with irritable bowel syndrome and inflammatory bowel disease: part II. Clinical Nurse Specialist, 2008; 22: 184–191. [DOI] [PubMed] [Google Scholar]
- 14. O'Sullivan M, O'Morain C. Nutrition in inflammatory bowel disease. Best Practice & Research Clinical Gastroenterology, 2006; 20: 561–573. [DOI] [PubMed] [Google Scholar]
- 15. Waters BM, Jensen L, Fedorak RN. Effects of formal education for patients with inflammatory bowel disease: a randomized controlled trial. Canadian Journal of Gastroenterology, 2005; 19: 235–244. [DOI] [PubMed] [Google Scholar]
- 16. Keohane J, Shanahan F. Are patients with IBD knowledgeable about the risks of their medications? Inflammatory Bowel Disease, 2008; 14 (Suppl. 2): S70–S71. [DOI] [PubMed] [Google Scholar]
- 17. Culkin A, Gabe SM, Madden AM. Improving clinical outcome in patients with intestinal failure using individualised nutritional advice. Journal of Human Nutrition and Dietetics, 2009; 22: 290–298; quiz 300‐1. [DOI] [PubMed] [Google Scholar]
- 18. Carre PC, Roche N, Neukirch F, Radeau T, Perez T, Terrioux P et al The effect of an information leaflet upon knowledge and awareness of COPD in potential sufferers. A randomized controlled study. Respiration, 2008; 76: 53–60. [DOI] [PubMed] [Google Scholar]
- 19. Segador J, Gil‐Guillen VF, Orozco D, Quirce F, Carratala MC, Fernandez‐Parker A et al The effect of written information on adherence to antibiotic treatment in acute sore throat. International Journal of Antimicrobial Agents, 2005; 26: 56–61. [DOI] [PubMed] [Google Scholar]
- 20. Johnson A, Sandford J. Written and verbal information versus verbal information only for patients being discharged from acute hospital settings to home: systematic review. Health Education Research, 2005; 20: 423–429. [DOI] [PubMed] [Google Scholar]
- 21. Hain T. Health information appraised for quality. Health Expectations, 2004; 7: 85–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. IBD Standards Working Group . IBD audit 2006: national results for the organisation and process of IBD care in the UK, 2007. Available at: http://www.rcplondon.ac.uk/projects/ibdauditround1, accessed 10 April 2014.
- 23. Edwards PJ, Roberts I, Clarke MJ, Diguiseppi C, Wentz R, Kwan I et al Methods to increase response to postal and electronic questionnaires. Cochrane Database of Systematic Reviews, 2009: MR000008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. British Medical Association . BMA patient information awards appraisal form. Available at: http://bma.org.uk/about-the-bma/bma-library/patient-information-awards/pia-awards-appraisal-process, accessed 10 April 2014.
- 25. Moult B, Franck LS, Brady H. Ensuring quality information for patients: development and preliminary validation of a new instrument to improve the quality of written health care information. Health Expectations, 2004; 7: 165–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Tang JL, Armitage JM, Lancaster T, Silagy CA, Fowler GH, Neil HA. Systematic review of dietary intervention trials to lower blood total cholesterol in free‐living subjects. British Medical Journal, 1998; 316: 1213–1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Eccles MP, Whitty PM, Speed C, Steen IN, Vanoli A, Hawthorne GC et al A pragmatic cluster randomised controlled trial of a diabetes REcall and management system: the DREAM trial. Implementation Science, 2007; 2: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kennedy A, Robinson A, Hann M, Thompson D, Wilkin D. A cluster‐randomised controlled trial of a patient‐centred guidebook for patients with ulcerative colitis: effect on knowledge, anxiety and quality of life. Health and Social Care in the Community, 2003; 11: 64–72. [DOI] [PubMed] [Google Scholar]
- 29. Politi P, Bodini P, Mortilla MG, Beltrami M, Fornaciari G, Formisano D et al Communication of information to patients with inflammatory bowel disease: a European Collaborative Study in a multinational prospective inception cohort. Journal of Crohns and Colitis, 2008; 2: 226–232. [DOI] [PubMed] [Google Scholar]
- 30. Jones SC, Gallacher B, Lobo AJ, Axon ATR. A patient knowledge questionnaire in inflammatory bowel‐disease. Journal of Clinical Gastroenterology, 1993; 17: 21–24. [DOI] [PubMed] [Google Scholar]
- 31. Conroy SP, Mayberry JF. Patient information booklets for Asian patients with ulcerative colitis. Public Health, 2001; 115: 418–420. [DOI] [PubMed] [Google Scholar]
- 32. Hancock RE, Bonner G, Hollingdale R, Madden AM. ‘If you listen to me properly, I feel good’: a qualitative examination of patient experiences of dietetic consultations. Journal of Human Nutrition and Dietetics, 2012; 25: 275–284. [DOI] [PubMed] [Google Scholar]
- 33. White P, Smith H, Webley F, Frew A. A survey of the quality of information leaflets on hayfever available from general practices and community pharmacies. Clinical & Experimental Allergy, 2004; 34: 1438–1443. [DOI] [PubMed] [Google Scholar]
- 34. Hedin CR, Mullard M, Sharratt E, Jansen C, Sanderson JD, Shirlaw P et al Probiotic and prebiotic use in patients with inflammatory bowel disease: a case‐control study. Inflammatory Bowel Disease, 2010; 16: 2099–2108. [DOI] [PubMed] [Google Scholar]
- 35. Blumenstein I, McDermott E, Keegan D, Byrne K, Ellison M, Doherty G et al Sources of information and factual knowledge in Europeans with inflammatory bowel diseases: a cross‐cultural comparison between German and Irish patients. Journal of Crohns and Colitis, 2013; 7: e331–e336. [DOI] [PubMed] [Google Scholar]
- 36. Mukewar S, Mani P, Wu X, Lopez R, Shen B. YouTube and inflammatory bowel disease. Journal of Crohns and Colitis, 2013; 7: 392–402. [DOI] [PubMed] [Google Scholar]
- 37. Cima RR, Anderson KJ, Larson DW, Dozois EJ, Hassan I, Sandborn WJ et al Internet use by patients in an inflammatory bowel disease specialty clinic. Inflammatory Bowel Disease, 2007; 13: 1266–1270. [DOI] [PubMed] [Google Scholar]
- 38. Bedell SE, Agrawal A, Petersen LE. A systematic critique of diabetes on the world wide web for patients and their physicians. International Journal of Medical Informatics, 2004; 73: 687–694. [DOI] [PubMed] [Google Scholar]
- 39. Nguyen HQ, Carrieri‐Kohlman V, Rankin SH, Slaughter R, Stulbarg MS. Internet‐based patient education and support interventions: a review of evaluation studies and directions for future research. Computers in Biology and Medicine, 2004; 34: 95–112. [DOI] [PubMed] [Google Scholar]
- 40. McClinchy J, Dickinson A, Barron D, Thomas H. Practitioner and lay perspectives of the service provision of nutrition information leaflets in primary care. Journal of Human Nutrition and Dietetics, 2011; 24: 552–559. [DOI] [PubMed] [Google Scholar]
- 41. Kennedy A, Robinson A, Rogers A. Incorporating patients' views and experiences of life with IBS in the development of an evidence based self‐help guidebook. Patient Education and Counseling, 2003; 50: 303–310. [DOI] [PubMed] [Google Scholar]


