Abstract
Background
Individuals with chronic pain are among the most frequent users of health care. Still, a significant percentage does not utilize health care for pain. A range of factors predict chronic pain‐related health care utilization.
Design
A cross‐sectional study aimed at identifying predictors of chronic pain‐related health care utilization and comparing predictors between men and women.
Methods
A postal questionnaire measuring sociodemographic variables, pain characteristics, health‐related quality of life (HRQoL) and pain‐related health care utilization, was sent to a sample of 4500 individuals randomly drawn from the national population of Iceland. The relationships between sociodemographic and pain‐related factors and pain‐related health care utilization among participants reporting chronic pain (≥3 months) were tested by using bivariate and multivariate statistical analysis.
Results
Among participants reporting chronic pain, 53.2% had consulted a health care provider for pain during the previous 6 months. Predictors for chronic pain‐related health care utilization differed between men and women. Interference with life and pain pattern was the strongest predictors among women, as compared with interference with life and the physical components of HRQoL for men. Pain‐related health care utilization was not linked to sociodemographic factors.
Conclusions
Pain‐related variables are better predictors of chronic pain‐related health care utilization than sociodemographic factors. Even though gender does not predict chronic pain‐related health care utilization, there are gender differences in the relationships between pain‐related variables and health care utilization. Men tend to postpone health care consultations for chronic pain longer than women.
Keywords: chronic pain, health care utilization, predictors
Introduction
Chronic pain is one of the most common health problems, and patients with chronic pain are among the most frequent users of health care.1, 2 However, pain‐related diagnoses in primary care only partly reflect the occurrence of self‐reported chronic pain in the population.3, 4 Earlier studies have shown that 25–60% of people with chronic pain do not consult health care for pain or discuss pain with health care providers.3, 5, 6
Health care utilization in relation to chronic pain may not only depend on its severity, but also on its nature, localization and interference with daily life.7, 8 Investigators of health care utilization have also emphasized the importance of socio‐demographic characteristics and beliefs about health and illness, as well as access to health care.9, 10, 11, 12 Some studies have shown that women are more likely than men to seek health care for pain6, 13, 14, 15 and female patients are overrepresented in chronic pain clinics16 and primary care.17 However, results on gender differences in pain‐related health care utilization are inconsistent.18 Residency and access to care are also important factors in predicting health care utilization.6, 19, 20, 21
Results from studies investigating health care utilization have varied depending on methodology and sampling methods.15, 18 Studying the relationship between chronic pain and use of health care is complex and requires a comprehensive methodological frame where prediction of different variables is carefully and simultaneously investigated. The Behavioural Model of Health Service Use9, 10 is a framework for viewing relationships between societal factors, health services systems and individual factors as determinants of health care utilization (Fig. 1). The model depicts the use of health care as affected by three major components: (i) predisposing factors, including socio‐demographic factors as well as health‐ and illness beliefs22, 23 and causes of symptoms;12, 13 (ii) enabling factors, as family income and access to care;21, 24, 25 and (iii) need for care, referring to the individual's perceived and evaluated need.9, 10, 21, 26
Figure 1.
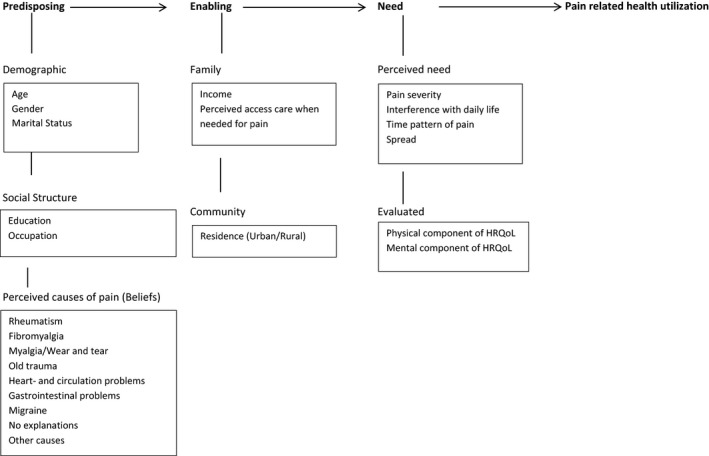
Conceptual diagram of the behavioural model of health service use and individual determinants.
Given the complexity of the relationship between chronic pain and health care utilization, studies should acknowledge the multiple factors inherent in this relationship. Therefore, the relationship needs to be investigated with regard to various socio‐demographic factors, access to care and symptom‐related factors, concurrent with testing which of these factors most strongly predict health care utilization for chronic pain. As women are more likely than men to consult health care for pain13, 14 and the relationship between gender and health care utilization is complex, a parallel comparison on gender differences is needed as well. Drawing on the Behavioural Model of Health Service Use, the aims of this study were to (i) investigate what predicts health care utilization in relation to chronic pain and (ii) to investigate whether there are gender differences in variables predicting chronic pain‐related health care utilization.
Methods
Sample and data collection procedures
This study is part of a research project on the prevalence and characteristics of chronic pain in the national population of Iceland.27 The Icelandic health care system is publicly financed, providing a generally easy access to care for the citizens with relatively low out of pocket cost. Two main hospitals in urban areas (Capital area and Akureyri), provide specialized care while health care centres and smaller community hospitals in rural areas provide general care.28
A questionnaire package was sent to a sample of 4500 individuals, aged 20–70 years, randomly drawn from the Icelandic National Registry. The National Registry holds information about names, birth dates and addresses of all residents of Iceland. To secure a proportional sample of men and women and people from all regions of the country, the sample was stratified in relation to gender and residence. To improve response rate, individuals who did not respond within 2 weeks received a reminder postcard and those who had not responded within 4 weeks received a new questionnaire along with an information letter. To avoid disturbing those who had already responded and select those who had not and still ensuring privacy, questionnaires were marked with an identifying number on the back side. The study was approved by the Icelandic National Bioethics Committee (VSNb2011030002/03.7) and the Icelandic Data Protection Authority (S5197/2011). Completing and returning the questionnaire was considered to denote informed consent for participation in the study.
Measures
The questionnaires measured socio‐demographic data, pain and pain characteristics, health‐related quality of life (HRQoL), and use of health care service for pain. All participants were asked to answer questions on HRQoL and whether they had felt pain during the previous week. Those who reported pain during the previous week were asked to answer questions on the duration and characteristics of pain (e.g. severity, time pattern, interference with activities of daily living), what they perceived to be the major cause of their pain, and whether they had consulted any kind of health provider for their pain during the previous 6 months. Study variables are presented here as predisposing, enabling, and need variables in accordance with the Behavioural Model of Health Service Use (Fig. 1).9, 10
Independent variables
Predisposing factors
Predisposing variables were demographic information (age, gender, marital status), social structure (education, occupation) and beliefs about the main cause of pain. Participants were asked to indicate what they perceived to be the primary cause of their pain (What do you believe to be the main cause of your pain?) by choosing from a list of possible causes (e.g. rheumatism, fibromyalgia, myalgia).
Enabling factors
Enabling factors were defined as household income per month, perceived access to health care for pain when needed (How easy is your access to the health care service you need for your pain? Five point Likert scale, very bad–very good) and place of residency (urban/rural). Communities with more than 15 000 inhabitants were defined as urban and smaller towns, villages and farms as rural.
Need for care
Perceived need was based on several pain characteristics including severity, interference, time pattern and spread (number of locations). Measures for evaluated need were physical and mental components of HRQoL, as measured by the Short Form 36v2 health survey (SF‐36v2).
The Icelandic version of the Brief Pain Inventory (BPI) was used to evaluate pain severity and life interference.29, 30 The BPI contains four questions regarding pain severity (least, worst, average pain and pain now) and questions regarding the impact of pain on seven items of daily life.27, 31 All questions are rated on a scale of 0–10, where 0 is no pain or impact on life and 10 is worst imaginable pain or ‘completely interferes’ with life.29 By taking the mean of the four severity items and the seven interference items, two composite scores, the Pain Severity Index and the Pain Interference Index were calculated.32
The BPI has been translated into Icelandic and validated in a general population sample of Icelandic adults experiencing pain of various origins and found to be both reliable and valid.30 In the present study, the internal consistency was acceptable for both scales, Chronbach's alpha for the severity scale was 0.89 and 0.91 for the interference scale. In the Icelandic BPI version, the time reference is the past week instead of the past 24 h as in the English version.30
Respondents were asked to answer a question about the time pattern of pain, classified as: Constant pain (pain all the time), daily intermittent (daily pain with one or a few hours break during the day), frequent intermittent (pain most days but pain‐free days in between) and periodic (pain‐free periods for days or weeks but pain episodes in between). Spread of pain was classified as number of pain locations. Participants were asked to indicate all areas of the body where they sensed pain by marking them on a list of 19 areas of the body (e.g. head, neck, upper back, lower back etc.).
HRQoL was measured by using a commercially available Icelandic translation of the Short Form 36v2 health survey (SF‐36v2).33 The instrument comprises 36 multiple‐choice questions, designed to assess eight different health domains: (i) physical functioning, (ii) role physical, (iii) bodily pain, (iv) general health, (v) vitality, (vi) social functioning, (vii) role emotional and (viii) mental health.34, 35 Each dimension is scored from 0 (worst) to 100 (best possible health status).35 In addition, the eight sub‐scales are combined to form two standardized components scores assessing physical component and mental component with lower scores implying poorer health.33 The physical component scale includes physical functioning, role physical, bodily pain and general health domains while the mental component comprises vitality, social functioning, role emotional and mental health domains. The instrument's reliability and validity for measuring HRQoL in relation to many different health conditions has been widely tested and confirmed.33 In the present study, the internal consistency was acceptable. Chronbach's alpha for the physical component scale was 0.87 and 0.89 for the mental component scale.
Outcome variable
Pain‐related use of health care
Responders who reported chronic pain (≥3 months) were asked whether they had consulted a health care service for their pain during the previous 6 months (Have you consulted health care services for your pain the past 6 months? Yes/No).
Statistical analyses
Data were analysed using SPSS for Windows (SPSS Inc., Chicago, IL, USA, version 20.0). Descriptive statistics were used to present the sample's characteristics as means of variables included in the predisposing, enabling and need factors. The relationship between individual variables and health care utilization was examined with t‐tests and chi‐square. Series of backward stepwise logistic regression analysis were used to calculate conditional relationships between independent variables and the dependent variable.
Statistical analyses were conducted in four steps:
Step 1. Bivariate analyses (t‐test and Chi‐square) were used to assess the independent effect of predictors on pain‐related health care use.
Step 2. Variables in each factor (predisposing, enabling, need), were tested against the outcome variable (pain‐related health care use) in separate Backward Stepwise logistic regression models, to test their predictability in relation to other variables in the same factor.
Step 3. Variables included in the predisposing, enabling and need factors were tested against the outcome variable by analysing them in three blocks, corresponding to the Behavioural Model of Health Service Use. Variables in the predisposing factor (age, gender, marital status, education, occupation, perceived cause of pain) were entered in block 1 and variables included in the enabling factor (income, access, residence) in block 2. In block 3, variables in the need factor, pain severity, interference, pattern and spread, as well as physical and mental components of HRQoL, were entered.
Step 4. Finally, variables included in the predisposing, enabling, and need factors were tested against the outcome variable separately for male and female participants by using the same three‐block model as in Step 3. This was done to investigate whether there were gender differences in how variables included in the predisposing, enabling and need factors predicted chronic pain‐related health care utilization.
Results
Response rate and characteristics of the total sample
Of the 4500 mailed questionnaires, 191 were undelivered due to unknown address, and 10 were reported unable to fill in the questionnaire. Of the 4299 remaining questionnaires, a total of 1629 were returned (37.9%). Sixty‐three questionnaires were returned empty and 1586 completed (36.9%). Response rate was significantly higher among women (40.7%) compared with men (30.0%) (z = 7.4297, P < 0.001). The total sample mean age was 46.2 years (SD = 14.0, range 20–70 years) (women 45.3 years, men 47.3 years). Respondents were significantly older than non‐respondents (mean age of non‐participants 38.7, P < 0.005). A majority of respondents were married or cohabitating (71.8%), and 26.3% had <11 years of school education. Of all responders, 74.4% reported having visited a health care service in the previous 6 months.27
Characteristics of chronic pain sample
The prevalence of chronic pain (≥3 months) among respondents was 47.5% (n = 754) with mean duration of 9.3 years (women = 9.4/men = 9.1), SD = 10.0 (Median = 6.0 years, Range = 0.25–54 years). The prevalence of chronic pain was slightly higher among women (49.7%) compared with men (45.6%) but the difference was non‐significant (z = 1.60, P = 0.110). Majority (73.7%) were married or cohabiting. One third (29.4%) had basic education as their final degree (<11 years) and about the same proportion (27.9%) had completed a university degree. More than half reported having good or very good access to care they needed for pain. Two thirds of participants with chronic pain lived in urban areas (>15 000 inhabitants) and 31.7% in rural areas (smaller towns, villages and farms; Table 1).
Table 1.
Descriptive statistics and bivariate analysis for chronic pain patients; users and nonusers of health care service
| Pain ≥ 3 months n = 754 | Pain ≥ 3 months Not user of pain‐related health care n = 296 | Pain ≥ 3 months User of pain‐related health care n = 401 | P‐value | Women n = 435 | Men n = 307 | P‐value | |
|---|---|---|---|---|---|---|---|
| Predisposing factors | |||||||
| Age, mean (SD/n) | 47.23 (13.7/743) | 45.98 (13.5/294) | 48.06 (13.8/393) | 0.049 1 | 46.46 (13.9/433) | 48.37 (13.5/305) | 0.063 1 |
| Gender (%) | |||||||
| Women | 435 (57.7) | 169 (57.1) | 234 (58.4) | 0.759 2 | |||
| Men | 307 (40.7) | 122 (41.2) | 161 (40.8) | ||||
| Missing | 12 (1.6) | 5 (1.7) | 6 (1.5) | ||||
| Marital status (%) | |||||||
| Married/cohabit | 556 (73.7) | 222 (75.0) | 293 (73.1) | 0.528 2 | 328 (75.4) | 225 (73.3) | 0.493 2 |
| Single/Divorced/Widowed | 186 (24.7) | 69 (23.3) | 102 (25.4) | 105 (24.1) | 81 (26.4) | ||
| Missing | 12 (1.6) | 5 (1.7) | 6 (1.5) | 2 (0.5) | 1 (0.3) | ||
| Education (%) | |||||||
| Basic education (<11 years) | 222 (29.4) | 72 (24.3) | 135 (33.7) | 0.025 2 | 140 (32.2) | 81 (26.4) | 0.001 2 |
| Secondary school (11–14 years) | 302 (40.1) | 128 (43.2) | 147 (36.7) | 151 (34.7) | 147 (47.9) | ||
| University | 210 (27.9) | 89 (30.1) | 109 (27.9) | 138 (31.7) | 72 (23.5) | ||
| Missing | 20 (2.7) | 7 (2.4) | 10 (2.5) | 6 (1.4) | 7 (2.3) | ||
| Occupation (%) | |||||||
| Official/Administrator w/univ. degree | 161 (21.4) | 73 (24.7) | 79 (19.7) | 0.0222 | 103 (23.7) | 58 (18.9) | <0.001 2 |
| Office‐service/sales/front‐desk | 227 (30.1) | 96 (32.4) | 119 (29.7) | 161 (37.0) | 63 (20.5) | ||
| Unskilled work | 151 (20.0) | 56 (18.9) | 78 (19.5) | 31 (7.1) | 118 (38.4) | ||
| Disabled, pensioner, unemployed | 87 (11.5) | 21 (7.1) | 59 (14.7) | 55 (12.6) | 30 (9.8) | ||
| Student. Not in paid employment | 73 (9.7) | 31 (10.5) | 35 (8.7) | 55 (12.6) | 18 (5.9) | ||
| Missing | 55 (7.3) | 19 (6.4) | 31 (7.7) | 30 (6.9) | 20 (6.5) | ||
| Perceived causes of pain (%) | |||||||
| Rheumatism | 234 (31) | 68 (23.0) | 151 (37.7) | <0.001 2 | 143 (32.9) | 88 (28.7) | 0.223 2 |
| Fibromyalgia | 90 (11.9) | 26 (8.8) | 62 (15.5) | 0.009 2 | 75 (17.2) | 13 (4.2) | <0.001 2 |
| Myalgia/wear and tear | 380 (50.4) | 157 (53.0) | 218 (54.4) | 0.729 2 | 245 (56.3) | 131 (42.7) | <0.001 2 |
| Old trauma | 237 (31.4) | 82 (27.7) | 143 (35.7) | 0.026 2 | 137 (31.5) | 96 (31.3) | 0.948 2 |
| Heart‐ and circulatory problems | 38 (5.0) | 5 (1.7) | 32 (8.0) | <0.001 2 | 17 (3.9) | 20 (6.5) | 0.108 2 |
| Gastro‐intestinal problems | 97 (12.9) | 35 (11.8) | 61 (15.2) | 0.200 2 | 61 (14.0) | 34 (11.1) | 0.237 2 |
| Migraine | 63 (8.4) | 21 (7.1) | 40 (10.0) | 0.183 2 | 50 (11.5) | 12 (3.9) | <0.001 2 |
| No explanations | 48 (6.4) | 27 (9.1) | 18 (4.5) | 0.014 2 | 23 (5.3) | 23 (7.5) | 0.220 2 |
| Other causes 2 | 160 (21.2) | 57 (19.3) | 98 (24.4) | 0.104 2 | 93 (21.4) | 65 (21.2) | 0.946 2 |
| Enabling factors | |||||||
| Income (%) | |||||||
| <500 000 IKR per month | 398 (52.8) | 150 (50.7) | 216 (53.9) | 0.158 2 | 242 (55.6) | 153 (49.8) | 0.094 2 |
| ≥500 000 IKR or more per month | 307 (40.7) | 133 (44.9) | 153 (38.2) | 166 (38.2) | 136 (44.3) | ||
| Missing | 49 (6.5) | 13 (4.4) | 32 (8.0) | 27 (6.2) | 18 (5.9) | ||
| Access to health care for pain (very easy/easy) (%) | 395 (52.4) | 144 (48.6) | 246 (61.3) | 0.001 2 | 235 (54.0) | 155 (50.5) | 0.3422 |
| Residence (%) | |||||||
| Urban | 515 (68.3) | 208 (70.3) | 264 (65.8) | 0.216 2 | 299 (68.7) | 207 (67.4) | 0.706 2 |
| Rural | 239 (31.7) | 88 (29.7) | 137 (34.2) | 136 (31.3) | 100 (32.6) | ||
| Need factors | |||||||
| Pain severity NRS (0–10) | 3.45 (1.83/700) | 2.79 (1.66/283) | 3.92 (1.82/382) | <0.001 1 | 3.58 (1.85/401) | 3.22 (1.78/287) | 0.011 1 |
| Pain interference with life | 2.63 (2.20/643) | 1.65 (1.54/277) | 3.39 (2.33/357) | <0.001 1 | 2.71 (2.26/374) | 2.46 (2.09/257) | 0.157 1 |
| Pain pattern (%) | |||||||
| Constant pain | 225 (29.8) | 65 (22.0) | 144 (35.9) | <0.001 2 | 140 (32.2) | 83 (27.0) | 0.179 2 |
| Daily intermittent | 151 (20.0) | 42 (14.2) | 105 (26.2) | 93 (21.4) | 55 (17.9) | ||
| Frequent intermittent | 196 (26.0) | 99 (33.4) | 88 (21.9) | 110 (25.3) | 82 (26.7) | ||
| Periodical | 133 (17.6) | 79 (26.7) | 50 (12.5) | 69 (15.9) | 63 (20.5) | ||
| Missing | 49 (6.5) | 11 (3.7) | 14 (3.5) | 23 (5.3) | 24 (7.8) | ||
| Spread – number of locations | 4.92 (3.58/752) | 4.20 (3.25/294) | 5.47 (3.75/401) | <0.001 1 | 5.50 (3.76/434) | 4.13 (3.20/307) | <0.001 1 |
| Physical component score | 45.1 (10.86/740) | 49.8 (8.73/287) | 41.6 (10.77/396) | <0.001 1 | 44.6 (11.29/427) | 46.1 (9.96/301) | 0.067 1 |
| Mental component score | 48.2 (11.78/744) | 49.1 (10.61/291) | 47.0 (12.74/396) | 0.021 1 | 47.6 (12.05/431) | 49.0 (11.34/301) | 0.128 1 |
1 T‐test comparing two means between user of pain‐related health care and nonuser of pain‐related health care.
2Chi‐square test between user of pain‐related health care and nonuser of pain‐related health care.
3Other causes e.g. discus prolapse, chronic pain after pregnancy/child birth, neurological diseases, physical handicap.
The mean value for the pain severity index for chronic pain was 3.45 (SD = 1.83) and 2.63 (SD = 2.20) for the interference index. One third reported pain to be constant (29.8%) and 20.0% daily intermittent. Frequent intermittent pain (pain most days but pain‐free days in between) was reported by 26.0 and 17.6% reported periodic pain with pain‐free periods for days or weeks. The most frequently reported causes of chronic pain were myalgia/wear and tear, old trauma) and rheumatism (Rheumatoid arthritis, osteoarthritis; Table 1).
Pain‐related health care utilization
Bivariate analysis (Step 1)
Descriptive data and bivariate analysis on the sample's predisposing, enabling and need variables are presented in Table 1. Among participants reporting chronic pain (n = 754), 53.2% (n = 401) consulted a health care provider for the pain during the previous 6 months.
There was a non‐significant gender difference in pain‐related health care use (women 53.8% vs. men 52.4%). Mean age was significantly higher among users of pain‐related health care than non‐users. Individuals with basic education (<11 years) and those who were on disability benefits, retired or unemployed were also more likely to have consulted health care for pain during the previous 6 months, as were those who reported easy access to care when needed for pain. There was also a significant relationship between use of health care for pain and all pain characteristics as well as HRQoL.
Multivariate analysis – separate factors (Step 2)
Predisposing factors
There was a positive significant relationship between age and pain‐related health care utilization. However, this relationship was no longer significant when controlled for predisposing social structure variables.
Individuals who were retired, unemployed and on disability benefits, were more likely to have consulted health care for pain during the previous 6 months (OR = 2.055, P < 0.05). That significance remained when controlled for perceived causes of pain (Table 2).
Table 2.
Logistic regression coefficients for regression of use of pain‐related health care predisposing variables, enabling variables and illness level variables
| OR | 95% CI | P‐value | Model χ2 | P‐value | |
|---|---|---|---|---|---|
| Predisposing | 36.784 | <0.001 | |||
| Demographic | |||||
| Age | 1.001 | 0.988–1.015 | 0.872 | ||
| Gender | 1.087 | 0.757–1.562 | 0.651 | ||
| Social structure | |||||
| Occupation (Official/administrator w/univ. degree) | 0.242 | ||||
| Office‐service/sales/front‐desk | 1.103 | 0.718–1.694 | 0.656 | ||
| Unskilled work | 1.244 | 0.744–2.08 | 0.406 | ||
| Disabled, pensioner, unemployed | 2.055 | 1.1–3.84 | 0.024 | ||
| Student. Not in paid employment | 1.096 | 0.597–2.014 | 0.767 | ||
| Perceived causes of pain | |||||
| Rheumatism | 1.874 | 1.278–2.747 | 0.001 | ||
| Old trauma | 1.494 | 1.045–2.136 | 0.028 | ||
| Heart‐ and circulatory problems | 3.587 | 1.316–9.775 | 0.013 | ||
| Enabling | 17.358 | <0.001 | |||
| Family | |||||
| Income (<500 000 IKR per month) | 1.335 | 0.972–1.835 | 0.075 | ||
| Access (very easy/easy) | 1.881 | 1.369–2.584 | <0.001 | ||
| Need | 124.409 | <0.001 | |||
| Perceived need | |||||
| Interference | 1.310 | 1.165–1.474 | <0.001 | ||
| Pattern | 0.077 | ||||
| Constant pain vs. periodical | 1.338 | 0.762–2.349 | 0.311 | ||
| Daily intermittent vs. periodical | 2.112 | 1.166–3.825 | 0.014 | ||
| Frequent intermittent vs. periodical | 1.169 | 0.698–1.958 | 0.552 | ||
| Evaluated need | |||||
| Physical component score | 0.952 | 0.929–0.976 | <0.001 | ||
Logistic regression, Variables entered into the model: Age and Gender.
Backward stepwise Logistic Regression, Predisposing variables not included in model: Marital Status, Education, Fibromyalgia, Myalgia/wear and tear, No explanations, Gastro‐ Intestinal Problems, Migraine and Other causes, n = 629. Enabling variables not included in model: Residence. n = 652. Illness Level variables not included in model: Severity, Spread, Mental Component Score. n = 584.
Pain‐related consultations were significantly related to some, but not all perceived causes of pain (Table 2). The most prominent predictor among perceived causes (belief variables) was problems in heart and circulatory system (OR = 3.587, P < 0.05). Other predictive perceived causes of pain were arthritis (OR = 1.874, P < 0.05) and old trauma (OR = 1.494, P < 0.05).
Enabling factors
Participants who reported good or very good access to pain‐related health care when needed, were more likely to have consulted health care for pain during the previous 6 months than those reporting neither good nor bad access or very bad access (OR = 1.888, P < 0.001). Use of pain‐related health care was not related to family income or place of residence (Table 2).
Need for care
Pain‐related use of health care was significantly related to pain interference, time pattern and the physical component of HRQoL (Table 2). Pain severity and spread (number of painful locations) did not predict consultations for pain nor did the mental component of HRQoL.
Multivariate analysis – all factors (Step 3)
After testing interaction between variables in each of the three factors separately, all the independent variables were tested against the outcome variable by analysing them in three blocks corresponding to the Behavioural Model of Health Service Use.10 Variables in the predisposing factor (age, gender, marital status, education, occupation, beliefs about the cause of pain) were entered in block 1, and variables included in the enabling factor (income, access, location of residence) into block 2. Finally, variables in the need factor, pain severity, interference, time‐pattern and spread, as well as physical and mental components of HRQoL, were entered into block 3.
Table 3 presents the findings from a three block backward stepwise logistic regression assessing the predictive impact of predisposing, enabling and need characteristics on the chronic pain‐related use of health care service. Some of the perceived causes (rheumatism, old trauma/wear and tear, and heart and circulatory problems) were significantly predictive for health care use for pain, problems in the heart and circulatory system being the most decisive. None of the demographic variables (age, gender, marital status) or the social structure variables (education, occupation) predicted pain‐related health care use.
Table 3.
Logistic regression coefficients for regression of use of pain‐related health care on predisposing, enabling and illness level variables
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P‐value | OR | 95% CI | P‐value | OR | 95% CI | P‐value | |
| Predisposing | |||||||||
| Age | 1.003 | 0.988–1.018 | 0.732 | 0.999 | 0.984–1.014 | 0.907 | 0.994 | 0.977–1.011 | 0.492 |
| Gender | 0.97 | 0.666–1.415 | 0.876 | 0.935 | 0.638–1.372 | 0.733 | 0.851 | 0.556–1.303 | 0.459 |
| Education | 0.063 | 0.022 | 0.143 | ||||||
| Lower secondary vs. university | 1.521 | 0.936–2.472 | 0.091 | 1.661 | 1.012–2.727 | 0.045 | 1.030 | 0.585–1.815 | 0.919 |
| Upper secondary vs. university | 0.878 | 0.572–1.348 | 0.553 | 0.856 | 0.554–1.322 | 0.483 | 0.660 | 0.402–1.082 | 0.099 |
| Perceived causes of pain | |||||||||
| Rheumatism | 1.852 | 1.204–2.85 | 0.005 | 1.845 | 1.191–2.858 | 0.006 | 1.212 | 0.735–1.999 | 0.451 |
| Old trauma | 1.588 | 1.067–2.363 | 0.023 | 1.612 | 1.077–2.414 | 0.02 | 1.187 | 0.751–1.877 | 0.463 |
| Heart‐ and circulatory problems | 5.444 | 1.55–19.117 | 0.008 | 5.419 | 1.525–19.255 | 0.009 | 2.288 | 0.594–8.807 | 0.229 |
| Enabling | |||||||||
| Access when in pain (very easy/easy) | 2.034 | 1.391–2.975 | <0.001 | 3.199 | 2.037–5.022 | <0.001 | |||
| Need | |||||||||
| Interference | 1.428 | 1.240–1.645 | <0.001 | ||||||
| Pattern | 0.043 | ||||||||
| Constant pain vs. periodical | 1.162 | 0.609–2.216 | 0.649 | ||||||
| Daily intermittent vs. periodical | 2.336 | 1.186–4.604 | 0.014 | ||||||
| Frequent intermittent vs. periodical | 1.040 | 0.583–1.856 | 0.894 | ||||||
| Physical component score | 0.947 | 0.919–0.976 | <0.001 | ||||||
| Model χ2 | 33.128 | <0.001 | 46.758 | <0.001 | 153.976 | <0.001 | |||
| Degrees of freedom | 7 | 8 | 13 | ||||||
| χ2 change | 13.630 | <0.001 | 107.218 | <0.001 | |||||
| Degrees of freedom | 1 | 5 | |||||||
Logistic regression, Variables entered into the model: Age and Gender.
Backward stepwise Logistic Regression, Variables not included in model: Marital Status, Occupation, Fibromyalgia, Myalgia/wear and tear, No explanations, Gastro‐ intestinal problems, Migraine, Other causes, Income, Residence, Severity, Spread, Mental Component Score. n = 504.
When enabling variables (income, perceived access, residence) were added into the regression model, the same belief categories continued to have an independent significant impact, not explained by the enabling factors. Perceived access was the only significant predictor in the enabling factor. Participants who reported easy/very easy access to care were more likely to have consulted health care for pain during the previous 6 months than those reporting neither good nor bad access or very bad access to care (OR = 2.034, P < 0.001).
When the six need variables (severity, interference, pattern, spread, physical component scale, mental component scale) were entered into the regression model, all perceived causes of pain became insignificant, but the significance of perceived access remained. The only predictors among pain characteristics were pain interference and pattern. The physical component of HRQoL was also a significant predictor but not the mental component. Pain severity and spread did not predict health care utilization for chronic pain.
Gender specific analysis (Step 4)
To test gender differences in variables predicting health care utilization for chronic pain, a similar backward stepwise regression model was done separately for men and women. The results are shown in Table 4.
Table 4.
Logistic regression coefficients for regression of use of pain‐related health care on predisposing, enabling and illness level variables
| Female | Male | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P‐value | OR | 95% CI | P‐value | |
| Predisposing | ||||||
| Age | 0.995 | 0.970–1.020 | 0.683 | 0.978 | 0.952–1.005 | 0.112 |
| Education | 0.013 | |||||
| Lower secondary vs. university | 1.487 | 0.706–3.132 | 0.296 | |||
| Upper secondary vs. university | 0.499 | 0.259–0.961 | 0.038 | |||
| Perceived causes of pain | ||||||
| Rheumatism | 1.540 | 0.771–3.077 | 0.221 | |||
| Fibromyalgia | 3.579 | 0.587–21.822 | 0.167 | |||
| Heart‐ and circulatory problems | 1.552 | 0.178–13.534 | 0.691 | 3.229 | 0.575–18.128 | 0.183 |
| Old trauma | 1.418 | 0.701–2.871 | 0.331 | |||
| Enabling | ||||||
| Easy access to care | 3.130 | 1.692–5.791 | <0.001 | 3.849 | 1.914–7.740 | <0.001 |
| Need | ||||||
| Interference | 1.642 | 1.374–1.962 | <0.001 | 1.403 | 1.139–1.727 | 0.001 |
| Physical component score | 0.936 | 0.895–0.980 | 0.005 | |||
| Pattern | 0.002 | |||||
| Constant pain vs. periodical | 2.382 | 1.008–5.626 | 0.048 | |||
| Daily intermittent vs. periodical | 5.611 | 2.168–14.52 | <0.001 | |||
| Frequent intermittent vs. periodical | 1.446 | 0.631–3.312 | 0.383 | |||
| Model χ2 | 109.073 | <0.001 | 55.143 | <0.001 | ||
Female: Backward stepwise Logistic Regression, Variables not included in model: Marital Status, Occupation, Fibromyalgia, Myalgia/wear and tear, Old trauma, No explanations, Gastro‐ intestinal problems, Migraine, Other causes, Income, Residency, Severity, Spread, Physical Component Score, Mental Component Score n = 296.
Male: Backward stepwise Logistic Regression, Variables not included in model: Marital Status, Education Occupation, Rheumatism, Myalgia/wear and tear, No explanations, Gastro‐ intestinal problems, Migraine, Other, Income, Residency, Severity, Pattern, Spread, Mental Component Score n = 208.
Age entered into the model for both genders.
The first column in Table 4 displays the findings from the backward stepwise logistic regression for female participants reporting chronic pain. Women with secondary school as a final educational degree were half as likely to have consulted health care for pain during the previous 6 months compared with women with university degree. Women with basic education (<11 years) reported more use of health care in the previous 6 months than women with university degree. However, this relationship was not significant when controlled for other variables.
Rheumatism was the only perceived cause of pain individually predicting pain‐related health care utilization among women and remained so after controlling for enabling variables. Perceived easy access to care was the only enabling variable predicting utilization for women. When need variables were added, the access variables and education remained significant. Among need variables, interference with life‐ and time pattern were the only significant predictors for pain‐related health care utilization. Women who reported constant or daily pain were significantly more likely to have consulted health care for pain the previous 6 months, than women reporting intermittent or periodic pain.
The second column of Table 4 shows findings from the backward stepwise logistic regression, for male participants reporting chronic pain. Fibromyalgia, old trauma and heart and circulation problems were the most prominent causes of pain predicting chronic pain‐related health care utilization among men. However this was not significant when controlled for pain‐related variables (need variables). Perceived easy access was the only enabling variable predicting chronic pain‐related health care use for men. When need variables were added in model 3, the access variable remained as a significant predictor. Pain interference with life and the physical component of HRQoL were the only need variables that predicted pain‐related health care utilization during the previous 6 months among men.
Discussion
The purpose of this study was to investigate what predicts chronic pain‐related health care utilization and whether gender differences occur in these relationships. The results show that the pain‐related variables interference with daily life, pattern and the physical component of HRQoL are the most important predictors of pain‐related health care utilization along with perceived easy access to health care. Pain severity and spread are significantly higher among those who consult health care for chronic pain. However, these variables are no longer significant when controlled for other pain characteristics. Even though gender is not a predictor of chronic pain‐related health care utilization, there is a gender difference in which variables are the most important predictors in this relationship. Interference with life and pain pattern are the strongest predictors among women, whereas for men it is interference with life and the physical components of HRQoL.
Earlier studies have found similar pain characteristics to be important predictors for health care use, for example, frequent pain1 as well as disability and poor health related to pain.11, 15 Results from this study are also similar to results from a population‐based study on health care utilization among individuals with chronic pain (N = 840) by Elliott et al.5 where those who had used health care service the previous 12 months had poorer HRQoL than non‐users, even when controlled for pain severity. This indicates that the influence of pain on daily life is greater than the pain itself when decision to seek health care is made.
Even though prior research has revealed that socio‐demographic factors and access to health care are prominent predictors of health care utilization,10, 12, 26 socio‐demographic variables did not predict health care use for chronic pain in this study. Retired and unemployed individuals and those receiving disability benefits were more likely to have consulted health care for chronic pain during the previous 6 months than other occupation groups, but this relationship was no longer significant when controlled for need (pain‐related) variables. No relationship between occupation and employment status as well as socio‐demographic characteristics among users and no‐users of health care service have been demonstrated previously.5 Need as a predictor for health care use, unrelated to socio‐demographic characteristics, has also been demonstrated earlier.36
It is worth noting that results on the importance of socio‐demographic or economic variables in relation to health care utilization are inconsistent in the literature. Some have suggested that health care utilization is related to a mixture of socio‐demographic and symptom related factors,15 while others have shown perceived health status and symptom severity to be more important for this relationship.1, 5, 36 Differences in culture, social structure as well as the infrastructure and financing of health care systems can also be of importance here. Societies with different cultures and at different stages of development may define access and need differently.37
The use of different methodology and study variables makes comparison between results from previous studies difficult. For example, in a literature review by Cornally and McCarthy15 (N = 23 studies), psychosocial aspects such as past experience from health care consultations, outcome expectancy, social influence and social costs were important factors for seeking health care, none of which were measured in the present study. Definitions of the concept health care utilization or help seeking have even varied between studies, making comparison all the more difficult.18
In accordance with the Behavioural Model of Health Service Use, family income and perceived access to care were enabling variables related to family, and residence (urban/rural) was an enabling community variable. The majority of participants reported easy access to care when needed for pain. Nevertheless, easy access was one of the variables predicting pain‐related health care utilization and the only predicting variable in the enabling factor, but neither family income nor residence. Family income and residence, have earlier been identified as limitations for access to, and use of, health care.19, 20 Financial barriers associated with health care have, however, been shown to act differently in different socioeconomic environments, and health care systems.13 In societies where health care service is run mainly by private initiatives, health care costs, insurance coverage and cost of insurance premiums are known to be predictors for health care utilization.19, 38 In countries with a socialized health care system and relatively low out‐of‐pocket service fees as in the Nordic countries, economic barriers are expected to be less important.4
Perceptions related to the cause of pain (beliefs) have earlier been demonstrated to influence whether or not individuals seek care for pain.13 When participants in the present study were asked what they perceived to be the cause of their pain, myalgia/wear and tear, rheumatism and old trauma were the most common causes. Those, as well as heart and circulatory problems, were also the only perceived causes that predicted health care use, even when controlled for perceived access, income and residence. However, when controlled for pain characteristics and HRQoL, perceived causes of pain were no longer significant.
Even though only 35 of the participants reporting chronic pain reported heart and circulatory problems to be the major cause of their pain, the odds ratio for having consulted health care for pain was the highest for this variable of all variables tested. Similar tendencies have been seen in earlier studies regarding relationships between health care consultancies and pain causes or localizations.6, 17 Watkins et al.6 found individuals with chest pain more likely to seek health care while headaches were less likely to be reported, even though pain localization in general had limited effect on health‐care‐seeking behaviour. Variations in recovery rates, acceptability or worry about a specific pain and its location may modulate the attendance to health care system because of pain.3
The second aim of this study was to investigate whether predictors for chronic pain health care utilization differ between men and women. Even though a number of earlier studies have shown women to be more likely to seek health care for pain,13, 14, 39 this was not the case in the current study. Regardless of this, there were some gender differences in pain‐related predictors for health care utilization. The most prominent predictors among women were interference with daily life and time pattern of pain (constant or daily pain), while pain interference with life and the physical components of HRQoL were the main predictors for men. According to results from another part of this study,27 physical impairment of chronic pain is mainly mediated by pattern of pain (constant and daily pain) as well as severity. Therefore, it could be argued that male participants had waited longer than female participants before consulting professional care for their pain. For men, constant or daily pain may have evolved into physical impairment before they sought professional treatment. Earlier studies have shown that men have higher threshold for experimental pain,40 are less willing to report pain and have a higher threshold for seeking care than women.15, 16 The reason for this is not known, but some kind of social learning or ‘social stereotyping’ has been suggested: that men are expected to have higher tolerance and endurance for pain, leading to a higher suffering threshold for reporting pain which results in more suffering and HRQoL impairment.16, 40 This might have played a part in the gender differences found in this study.
Studies have also suggested that negative expectations about the outcome, fear of not being believed or being labelled as a hypochondriac, if symptoms are not severe ‘enough’, may constitute a barrier to seeking treatment.41, 42, 43 This study does not reveal whether poor results from earlier treatments, or negative past experience from consulting health care professionals for chronic pain, may explain the decision not to seek professional care for chronic pain. However, earlier research has suggested that many individuals struggle with pain on their own until the pain has started to interfere with daily life or even physical functional ability.6 This delay of seeking health care might be more prominent among men than women. Early identification of pain and referral to suitable health care may be important to prevent pain from becoming chronic with quality of life impairment as a result. Thus, it is important to encourage people to seek care for their pain before it has started to cause severe interference with activities of daily living. In light of the results of this study this is especially important for men.
Strengths and limitations
The major strength of this study is that it provides valuable data about the relationship between chronic pain and health care utilization for chronic pain and what variables are important predictors for chronic pain‐related health care utilization. Another important strength is that this study is based on a nationwide sample and data was obtained from 92.4% of those reporting chronic pain.
There are a number of limitations, however, that should be taken into account. This cross‐sectional population‐based study has a relatively low total‐response rate (36.9%) and is solely based on self‐reported data. Nevertheless, it is worth noting that the prevalence of chronic pain among responders was relatively high, which suggests that those who accepted invitation to participate might have been more likely to do so because they felt pain and had done so for a long time.
Future research
This study provides important knowledge, not only about variables predicting chronic pain‐related health care utilization, but also, and even more importantly, appoints to important gender differences. It is essential to look carefully into why men tend to hesitate to seek health care until pain starts to interfere with their physical ability. It is also important to investigate chronic pain‐related health care utilization in relation to earlier experience from seeking health care and perceived treatment outcome to determine whether the decision to seek care or not is related to the quality or structure of the health care service.
Conclusion
This study suggests that pain interference on daily life, pattern of pain and the physical components of HRQoL, together with perceived access to health care when needed for pain, are the most prominent predictors for chronic pain‐related health care utilization. Even though gender does not predict chronic pain‐related health care utilization, there are gender differences in the relationships between health care utilization and pain‐related variables. Men tend to postpone health care consultations for chronic pain longer than women. Encouraging people to seek care for chronic pain before it has started to cause physical impairment is important, especially for men.
Source of funding
The data collection for this project was funded by The University of Akureyri Research Fund, Borgir v/Nordurslod, 600 Akureyri, Iceland and The Icelandic Nurses' Association Research Fund, Sudurlandsbraut 22, 108 Reykjavik, Iceland, Ingibjorg R. Magnusdottir Research Fund, Reykjavik, Iceland.
Conflict of interest
There are no conflict of interests, financial or otherwise, regarding the content or data in this article.
Acknowledgements
We are grateful to all those who participated in this study. We also want to thank Thor Aspelund for his assistance and advice in statistical analysis.
References
- 1. Gerdle B, Bjork J, Henriksson C, Bengtsson A. Prevalence of current and chronic pain and their influences upon work and healthcare‐seeking: a population study. Journal of Rheumatology, 2004; 31: 1399–1406. [PubMed] [Google Scholar]
- 2. Peolsson M, Borsbo B, Gerdle B. Generalized pain is associated with more negative consequences than local or regional pain: a study of chronic whiplash‐associated disorders. Journal of Rehabilitation Medicine, 2007; 39: 260–268. [DOI] [PubMed] [Google Scholar]
- 3. Andersson HI, Ejlertsson G, Leden I, Schersten B. Musculoskeletal chronic pain in general practice. Studies of health care utilisation in comparison with pain prevalence. Scandinavian Journal of Primary Health Care, 1999; 17: 87–92. [DOI] [PubMed] [Google Scholar]
- 4. Lindal E, Uden A. Why do people seek medical advice for back pain: a comparison of consulters and nonconsulters. Clinical Journal of Pain, 1989; 5: 351–358. [DOI] [PubMed] [Google Scholar]
- 5. Elliott AM, Smith BH, Hannaford PC. Chronic pain and health status: how do those not using healthcare services fare? British Journal of General Practice, 2004; 54: 614–616. [PMC free article] [PubMed] [Google Scholar]
- 6. Watkins E, Wollan PC, Melton LJ III, Yawn BP. Silent pain sufferers. Mayo Clinic Proceedings, 2006; 81: 167–171. [DOI] [PubMed] [Google Scholar]
- 7. Andersson HI, Ejlertsson G, Leden I, Schersten B. Impact of chronic pain on health care seeking, self care, and medication. Results from a population‐based Swedish study. Journal of Epidemiology and Community Health, 1999; 53: 503–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bergman S, Jacobsson LT, Herrstrom P, Petersson IF. Health status as measured by SF‐36 reflects changes and predicts outcome in chronic musculoskeletal pain: a 3‐year follow up study in the general population. Pain, 2004; 108: 115–123. [DOI] [PubMed] [Google Scholar]
- 9. Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. The Milbank Memorial Fund Quarterly. Health and Society, 1973; 51: 95–124. [PubMed] [Google Scholar]
- 10. Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? Journal of Health and Social Behavior, 1995; 36: 1–10. [PubMed] [Google Scholar]
- 11. Bosworth HB, Butterfield MI, Stechuchak KM, Bastian LA. The relationship between self‐rated health and health care service use among women veterans in a primary care clinic. Women's Health Issues, 2000; 10: 278–285. [DOI] [PubMed] [Google Scholar]
- 12. Dixon‐Woods M, Kirk D, Agarawal S et al Vulnerable Groups and Access to Health Care: A Critical Interpretive Review. London, UK: Report for the National Co‐ordinating Centre for NHS Service Delivery and Organisation R&D (NCCSDO), 2005. [Google Scholar]
- 13. Walker BF, Muller R, Grant WD. Low back pain in Australian adults. Health provider utilization and care seeking. Journal of Manipulative and Physiological Therapeutics, 2004; 27: 327–335. [DOI] [PubMed] [Google Scholar]
- 14. Rustoen T, Wahl AK, Hanestad BR, Lerdal A, Paul S, Miaskowski C. Gender differences in chronic pain–findings from a population‐based study of Norwegian adults. Pain Management Nursing, 2004; 5: 105–117. [DOI] [PubMed] [Google Scholar]
- 15. Cornally N, McCarthy G. Help‐seeking behaviour for the treatment of chronic pain. British Journal of Community Nursing, 2011; 16: 90–98. [DOI] [PubMed] [Google Scholar]
- 16. Robinson ME, Riley JL III, Myers CD et al Gender role expectations of pain: relationship to sex differences in pain. The Journal of Pain, 2001; 2: 251–257. [DOI] [PubMed] [Google Scholar]
- 17. Watkins EA, Wollan PC, Melton LJ III, Yawn BP. A population in pain: report from the Olmsted County health study. Pain Medicine, 2008; 9: 166–174. [DOI] [PubMed] [Google Scholar]
- 18. Adamson J, Hunt K, Nazareth I. The influence of socio‐demographic characteristics on consultation for back pain–a review of the literature. Family Practice, 2011; 28: 163–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sinay T. Access to quality health services: determinants of access. Journal of Health Care Finance, 2002; 28: 58–68. [PubMed] [Google Scholar]
- 20. Hausdorf K, Rogers C, Whiteman D et al Rating access to health care: are there differences according to geographical region? Australian and New Zealand Journal of Public Health, 2008; 32: 246–249. [DOI] [PubMed] [Google Scholar]
- 21. Vilhjalmsson R. Failure to seek needed medical care: results from a national health survey of Icelanders. Social Science and Medicine, 2005; 61: 1320–1330. [DOI] [PubMed] [Google Scholar]
- 22. Ndao‐Brumblay SK, Green CR. Predictors of complementary and alternative medicine use in chronic pain patients. Pain Medicine, 2010; 11: 16–24. [DOI] [PubMed] [Google Scholar]
- 23. DeVoe JE, Wallace LS, Fryer GE Jr. Measuring patients' perceptions of communication with healthcare providers: do differences in demographic and socioeconomic characteristics matter? Health Expectations, 2009; 12: 70–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Vilhjalmsson R, Jorundsdottir E, Sigurdardottir H, Johannsdottir TB. Thaettir tengdir aðgengi að læknisþjónustu á Íslandi In: Sveinsdottir H, Nyysti A. (eds) Framtidarsyn innan heilsugæsluhjúkrunar. Reykjavík, Iceland: Háskólaútgáfan, 2001: 70–94. [Google Scholar]
- 25. Tripp DA, VanDenKerkhof EG, McAlister M. Prevalence and determinants of pain and pain‐related disability in urban and rural settings in southeastern Ontario. Pain Research and Management, 2006; 11: 225–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bradley EH, McGraw SA, Curry L et al Expanding the Andersen model: the role of psychosocial factors in long‐term care use. Health Services Research, 2002; 37: 1221–1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Jonsdottir T, Aspelund T, Jonsdottir H, Gunnarsdottir S. The relationship between chronic pain pattern, interference with life and health‐related quality of life in a nationwide community sample. Pain Management Nursing doi: 10.1016/j.pmn.2013.07.005. [DOI] [PubMed] [Google Scholar]
- 28. Halldorsson M. Health Care Systems in Transition: Iceland. Copenhagen: WHO Regional Office for Europe on behalf of the European Observatory on Health Sysems and Policies, 2003. [Google Scholar]
- 29. Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Annals of the Academy of Medicine, Singapore, 1994; 23: 129–138. [PubMed] [Google Scholar]
- 30. Gunnarsdottir S, Ward S, Serlin RC. Attitudinal barriers to cancer pain management in the Icelandic population. Cancer Nursing, 2008; 31: 95–102. [DOI] [PubMed] [Google Scholar]
- 31. Jonsdottir T, Jonsdottir H, Gunnarsdottir S. Validation of the patients' perceived involvement in care scale among patients with chronic pain. Scandinavian Journal of Caring Sciences, 2013; 27: 740–749. [DOI] [PubMed] [Google Scholar]
- 32. Zelman DC, Gore M, Dukes E, Tai KS, Brandenburg N. Validation of a modified version of the Brief Pain Inventory for painful diabetic peripheral neuropathy. Journal of Vascular Nursing, 2005; 23: 97–104. [DOI] [PubMed] [Google Scholar]
- 33. Ware JE Jr. SF‐36® health survey update. 2012. Available at: http://www.sf-36.org/tools/SF36.shtml#TRANS, accessed 11 November 2012.
- 34. Wallin MK, Raak RI. Quality of life in subgroups of individuals with whiplash associated disorders. European Journal of Pain, 2008; 12: 842–849. [DOI] [PubMed] [Google Scholar]
- 35. Ware JE Jr. SF‐36 health survey update. Spine, 2000; 25: 3130–3139. [DOI] [PubMed] [Google Scholar]
- 36. Bedson J, Mottram S, Thomas E, Peat G. Knee pain and osteoarthritis in the general population: what influences patients to consult? Family Practice, 2007; 24: 443–453. [DOI] [PubMed] [Google Scholar]
- 37. Gulzar L. Access to health care. Image ‐ The Journal of Nursing Scholarship, 1999; 31: 13–19. [DOI] [PubMed] [Google Scholar]
- 38. Song HJ, Han HR, Lee JE et al Does access to care still affect health care utilization by immigrants? Testing of an empirical explanatory model of health care utilization by Korean American immigrants with high blood pressure. Journal of Immigrant and Minority Health, 2010; 12: 513–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hagen KB, Bjorndal A, Uhlig T, Kvien TK. A population study of factors associated with general practitioner consultation for non‐inflammatory musculoskeletal pain. Annals of the Rheumatic Diseases, 2000; 59: 788–793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Alabas OA, Tashani OA, Tabasam G, Johnson MI. Gender role affects experimental pain responses: a systematic review with meta‐analysis. European Journal of Pain, 2012; 16: 1211–1223. [DOI] [PubMed] [Google Scholar]
- 41. Cornally N, McCarthy G. Help‐seeking behaviour: a concept analysis. International Journal of Nursing Practice, 2011; 17: 280–288. [DOI] [PubMed] [Google Scholar]
- 42. Hansson KS, Fridlund B, Brunt D, Hansson B, Rask M. The meaning of the experiences of persons with chronic pain in their encounters with the health service. Scandinavian Journal of Caring Sciences, 2011; 25: 444–450. [DOI] [PubMed] [Google Scholar]
- 43. Sanders C, Donovan JL, Dieppe PA. Unmet need for joint replacement: a qualitative investigation of barriers to treatment among individuals with severe pain and disability of the hip and knee. Rheumatology (Oxford), 2004; 43: 353–357. [DOI] [PubMed] [Google Scholar]


