Abstract
Background
Assessment of users' information and decision‐making needs is one key step in the development of decision‐support interventions.
Objective
To identify patients' information and decision‐making needs as a pre‐requisite for the development of high‐quality web‐based patient decision aids (PtDAs) for common mental disorders.
Search strategy
A systematic MEDLINE search for papers published until December 2012 was conducted, and reference lists of included articles and relevant reviews were searched.
Inclusion criteria
Original studies containing data on information or decision‐making needs of adults with depression, anxiety disorders, somatoform disorders, alcohol‐related disorders and schizophrenia were included.
Data extraction and synthesis
Data extraction was performed using a standardized form, and data synthesis was conducted using a theory‐based deductive approach by two independent reviewers. Studies were quality assessed using the Mixed Methods Appraisal Tool.
Main results
Twelve studies were included focusing on information needs or the identification of decisions patients with depression and schizophrenia were facing. No studies were found for the other mental disorders. Overall, seven information needs categories were identified with the topics ‘basic facts’, ‘treatment’ and ‘coping’ being of major relevance. Six decision categories were identified of which decisions on ‘medication’ and ‘treatment setting’ were most often classified.
Conclusions
This review reveals that patients with schizophrenia and depression show extensive information and decision‐making needs. The identified needs can initially inform the design of PtDAs for schizophrenia and depression. However, there is an urgent need to investigate information and decision‐making needs among patients with other mental disorders.
Keywords: mental disorders, needs assessment, shared decision making, systematic review
Introduction
Growing interest for shared decision‐making (SDM) in mental health care has been raised in the last decade given that it is considered as being a fundamental part of patient‐centred mental health care.1, 2 Besides the ethical imperative, SDM holds the promise to be a linking part between recovery‐oriented and evidence‐based mental health treatment approaches.3 Both the recovery model and SDM have been internationally established as guiding principles for mental health care on the policy level and in treatment guidelines.4, 5, 6 Furthermore, evidence suggests that patient involvement in mental health care is associated with enhanced patient satisfaction, adherence, empowerment, and guideline‐concordant care.7, 8, 9, 10 The need of providing evidence on SDM in mental health care and to develop interventions to support SDM is further reinforced by the fact that the majority of patients with mental disorders wish to be involved in decision‐making.11, 12, 13, 14 However, studies examining the degree of SDM being practised in mental health treatment decision‐making indicate low levels of SDM practice.15, 16, 17
One way to enable patients to participate in medical decisions is to provide high‐quality patient decision aids (PtDAs). PtDAs are evidence‐based tools that support people to deliberate, independently or in collaboration with others, about choices they face in the medical encounter. They are designed to support patients in considering relevant attributes of the options and forecasting how they might feel about short, intermediate and long‐term outcomes in ways which help the process of constructing preferences and eventual decision‐making.18 A Cochrane systematic review showed that SDM interventions including PtDAs and training of physicians were associated with positive decision process outcomes such as improved knowledge, patient participation, and satisfaction with care.19 Since the publication of this review, the body of evidence on the effects of SDM interventions in mental health care has been raised.20, 21, 22, 23, 24, 25, 26 However, studies investigating effects of PtDAs as solely provided interventions are still rare and show inconclusive results.20, 21, 24 As no firm conclusions can be drawn from the existing evidence, further research is needed on the effects of PtDAs in mental health care either as being solely provided or as a part of a comprehensive SDM intervention.
A current project being part of the public‐funded research network psychenet – Hamburg Network for Mental Health – aims to develop and evaluate a mental health website (www.psychenet.de) with PtDAs as a key part.27 Following international quality standards,28 assessment of needs is seen as one key element in the systematic development of PtDA. PtDAs that are tailored to the specific decisional needs of people with mental disorders are suggested to empower patients in managing their illness and to prepare patients to participate with their health provider in making informed value‐based decisions.29 However, an in‐depth assessment of needs that considers the patients', relatives', and experts' views for several mental disorders is expected to be a highly time‐ and cost‐consuming process.
To make use of the existing body of evidence, the aim of this systematic review was to identify substantive areas of information and decision‐making needs among patients with depression, anxiety disorders, somatoform disorders, alcohol‐related disorders and schizophrenia. The results of the systematic review were intended for informing the design and content development of web‐based PtDAs.
Methods
Data sources
An electronic literature search was conducted using the MEDLINE database to identify all studies published until December 2012 that reported on information and decision‐making needs throughout the course of depression, anxiety disorders, somatoform disorders, schizophrenia and alcohol‐related disorders as perceived by patients, their relatives, and health professionals. Illnesses were selected with regard to ‘years of life with disability’ or relevance to patient care.30 Each search was conducted by a combination of Medical Subject Headings (MeSH) and free text terms according to a mental disorder filter, an information needs filter and a decision‐making needs filter. To identify all studies relevant for the research question, the fairly broad additional terms ‘shared decision‐making’, ‘decision aid/decision support intervention’, ‘treatment preferences’ and ‘needs assessment’ were included. The reference lists of the included studies and relevant review articles were also screened. The full MEDLINE (Ovid) search strategy for depressive disorders, on which other searches are based, is presented in Appendix S1.
Study selection
Titles and abstracts of all eligible articles were initially screened by two reviewers (LT and CW) for possible inclusion. Full texts of articles that appeared relevant to the reviews' focus were screened by at least one of two reviewers (LT or CW). No study design was excluded. For inclusion and exclusion criteria, see Table 1.
Table 1.
Inclusion and exclusion criteria
| Inclusion criteria | Exclusion criteria |
|---|---|
| Language of publication: English or German | Needs assessment is not conducted either as the main purpose of the study or as a defined step within the study design |
| Purpose: The study investigates information or decision‐making needs | Results are not separately reported for each diagnosis |
| Participants: Adults or adolescents with depression, anxiety disorders, somatoform disorders, alcohol‐related disorders, or schizophrenia, their relatives or health professionals | |
| Diagnosis: The investigation of needs is definitely referred to depression, anxiety disorders, somatoform disorders, alcohol‐related disorders, or schizophrenia as the primary diagnosis | |
| Publication format: Original collection of data |
Data extraction
Two reviewers (LT and CW) independently extracted data from each study using a structured form created specifically for this review. The extraction form included the following thematic categories: (i) publication characteristics, (ii) health condition, (iii) purpose, (iv) methodological characteristics, (v) sample characteristics and (vi) results on decision‐making needs and information needs. The extraction form for decision‐making needs was based on the Ottawa Decision‐Support Framework (ODSF) with the categories identified decisions, decision‐making behaviour, decisional conflict, support and resources, and mode of delivery.31 Informational needs were extracted according to pre‐treatment, treatment related, and post‐treatment needs.
Data analysis
Following the methodological approach of former systematic reviews on information needs in patients with cancer and their relatives,32, 33 data analysis was performed by two reviewers (LT and SL) using a deductive approach.
In a first step, classification schemes for information needs and decision‐making needs were developed based on existing typologies. A classification of information needs was generated based on the typology of information needs in persons with severe mental disorders as proposed by Mueser and colleagues.34 Moreover, a classification scheme for ‘identified decisions’ was developed based on the categorization used in a needs assessment study from Bunn and colleagues35 that investigated decision‐making needs among disadvantaged women with a wide range of diagnoses and decisional settings. No other category of decision‐making needs was accounted for in the classification scheme as only two of the four included studies on decision‐making needs investigated decision‐making needs based on the ODSF including the categories decision‐making role, decisional conflict, decision‐making behaviour, support and resources, and mode of delivery.36, 37
In a second step, quotations related to the studies' aims (i.e. units of needs) were identified for each included study and coded according to the pre‐established classification schemes. Units of needs for which the classification schemes were not applicable were affixed to new codes, similarities and differences among various codes were identified, and new categories and subcategories were established. Both classification schemes were substantially extended and revised throughout the iterative analysis process.
In a third step, the following procedure was separately performed for each category. First, the relative frequency of articles in which units of needs were identified and coded within the respective category was calculated. Moreover, to indicate the relative frequency of needs within the respective category, the number of identified units of needs coded within the category was divided by the sum of all units of needs identified in the entire body of articles reviewed. Relative frequencies of all categories thus sum to 100%. Additionally, the number of identified units of needs coded within each of the subcategories was divided by the sum of all identified units of needs coded within the respective main category.
Moreover, to identify disorder‐specific needs, a comparison of the absolute frequency between depression and schizophrenia was done with Fisher's exact test using SAS software (SAS Institute Inc., Cary, North Carolina, USA).
Quality assessment
Quality assessment was conducted using the Mixed Methods Appraisal Tool (MMAT) developed by Pluye et al.38 Piloting suggests the MMAT being a reliable and efficient scoring system for appraising the quality of quantitative, qualitative, and mixed‐method studies.39 It provides a comprehensive manual with detailed instructions. As recommended by PRISMA,40 the methodological quality of the included studies was assessed independently by two reviewers (LT, SL). The quality assessment revealed an acceptable overall inter‐rater agreement of 79.4% and a Cohen's κ of 0.48 (P < .001). Given the exploratory purpose of our review, no study was excluded on the basis of their methodological quality. The quality assessment served to gain an understanding of the relative strengths and weaknesses of the body of evidence.
Results
Study selection
The literature search identified 955 potentially eligible articles. Finally, 12 studies were included in the literature review (Fig. 1).
Figure 1.
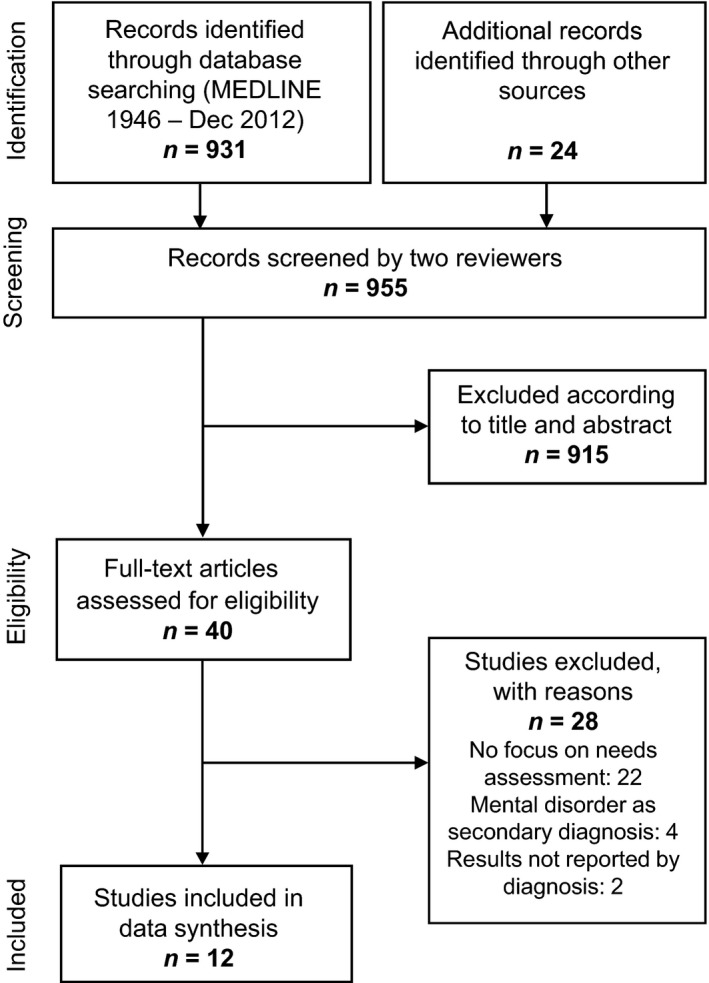
Flow chart of study inclusion process.
Characteristics of the studies
Most included studies employed a descriptive (n = 7) or cross‐sectional design (n = 2), using quantitative (n = 5), qualitative (n = 4) or mixed methods (n = 3). The samples were comprised of patients (n = 8), relatives (n = 5) and physicians (n = 2). Information and decision‐making needs were assessed for schizophrenia (n = 6), depression (n = 4), schizophrenia and depression (n = 1), and schizophrenia, depression and anxiety (n = 1). MMAT results showed that of the 12 included studies, one study scored 25% on methodological criteria, five studies scored 50%, three studies scored 75% and two studies met all criteria for methodological quality. One study did not score on one of the four criteria. The study characteristics with quality scores are outlined in Table 2.
Table 2.
Characteristics of the 12 included studies with quality scores presented in alphabetical order
| Study Country Language | Health condition | Principal objective | Design Method | Data collection Measures | Recruitment | Sample Setting | Participants |
|---|---|---|---|---|---|---|---|
|
Barney et al.41, c
Australia English |
Depressive disorder | Describe explicit and implicit information needs of users of an online depression support forum | Descriptive study Qualitative | Online data collection | Online consecutive sampling |
N = 134 board users (N = 2680 posts) Non‐clinical setting |
Female: Not specified Mean age: Not specified Level of education: Not specified Duration of illness: Not specified |
|
Chien et al.42, d
China English |
Schizophrenia | Identify specific educational needs of Chinese patients with schizophrenia |
Cross‐sectional study Quantitative |
Self‐report questionnaire Educational Needs Questionnaire34 |
Simple random sampling |
N = 192 patients Clinic‐based outpatient |
Female: 41.7% Mean age: Not specified Level of education: 21.9% primary or below, 51.0% secondary, 7.8% tertiary Duration of illness: 6.7 years |
|
Chien et al.43, d
China English |
Schizophrenia | Identify specific educational needs of Chinese families caring for a relative with schizophrenia |
Cross‐sectional study Quantitative |
Self‐report questionnaire Educational Needs Questionnaire34 |
Simple random sampling |
N = 204 relatives Clinic‐based outpatient |
Female: 50.5% Mean age: Not specified Level of education: 48.0% primary or below, 34.3% secondary, 17.7% tertiary Duration of illness: Not specified |
|
Gaskill and Cooney44, b
Australia English |
Schizophrenia | Identify the information needs of partners of schizophrenia sufferers |
Not specified Qualitative |
Audiotaped unstructured face‐to‐face Interview Not specified |
Not specified |
N = 14 partners Clinic‐based outpatient |
Female: 50.0% Mean age: Not specified Level of education: Not specified Duration of illness: Not specified |
|
Gumus and Gumus45, b
Turkey English |
Schizophrenia | Determine health education needs of patients with schizophrenia and their relatives |
Descriptive study Quantitative |
Self‐report questionnaire Educational Needs Questionnaire34 |
Consecutive sample |
N = 160 participants n = 80 patients n = 80 relatives Clinic‐based outpatient |
Female: patients 30.0%, relatives 51.3% Mean age: patients 31.4 years, relatives 46.6 years Level of education: high school level of education (52.5%), university degree (40.0%) Duration of illness: 8.8 years |
|
Hamann et al.46, b
Germany English |
Schizophrenia | Identify most recent decisions about the life and treatment of patients with schizophrenia |
Descriptive study Mixed method |
Interviews, self‐report questionnaire Autonomy Preference Index47 |
Convenience sample |
N = 90 participants n = 60 patients n = 30 psychiatrists Non‐clinical setting |
Female: Patients 43.3%, psychiatrists 50% Mean age: Patients 36.1 years, psychiatrists 36.1 years Level of education: Not specified Duration of illness: Not specified |
|
Hamann et al.48, b
Germany English |
Schizophrenia | Psychiatrist's view on whether certain patient characteristics are likely to lead to shared decision making and whether certain decision topics would be suitable for shared decision making |
Descriptive study Quantitative |
Self‐report questionnaire Not specified |
Convenience sample |
N = 352 psychiatrist Non‐clinical setting |
Female: 41.0% Mean age: 46.6 years Level of education: Not specified Duration of illness: Not specified |
|
Llewellyn‐Jones et al.49, a
United Kingdom English |
Schizophrenia Depressive disorder Anxiety disorder |
Determine patient information needs by investigating questions patients most commonly ask their psychiatrists |
Descriptive study Qualitative |
Interview Not specified |
Consecutive sample |
N=179 patients (n = 65 patients with schizophrenia, n = 52 patients with unipolar depression, n = 24 patients with bipolar disorder, n = 14 patients with anxiety disorder, n = 24 patients with personality disorder) Clinic‐based outpatient |
Female: Not specified Mean age: Not specified Level of education: Not specified Duration of illness: Not specified |
|
Mueser et al.34
United States English |
Schizophrenia Depressive disorder |
Determine specific educational needs and to compare the needs of different consumers |
Descriptive study Quantitative |
Self‐report questionnaire Educational Needs Questionnaire34 |
Consecutive sample |
N=195 participants (n = 46 patients with schizophrenia n = 14 patients with major affective disorders n = 108 relatives n = 27 close friends) Clinic‐based outpatient |
Female: Not specified Mean age: Not specified Level of education: Not specified Duration of illness: Not specified |
|
Simon et al.36, c
Germany English |
Depressive disorder | Investigate depressed patients' perceptions of the treatment decision‐making process with general practitioners |
Exploratory study Mixed method |
Semi‐structured interviews, self‐report questionnaire Patient Health Questionnaire50 |
Convenience sample |
N = 40 patients Physician‐based outpatient |
Female: 60.0% Mean age: 43.2 years Level of education: Not specified Duration of illness: Not specified |
|
Stacey et al.37, c
Canada English |
Depressive disorder | Identify decision‐making needs, factors influencing decisional conflict and resources to support decision making of patients facing depression treatment |
Descriptive study Mixed method |
Semi‐structured interviews, self‐report questionnaire Decisional Conflict Scale51 Control Preference Scale52 |
Convenience sample |
N = 94 patients Clinic‐based outpatient |
Female: 66.0% Mean age: Not specified Level of education: 74.0% higher education (> 12 grade) Duration of illness: Not specified |
|
Wittmund et al.53, b
Germany German |
Depressive disorder | Examine how spouses of depressive patients view illness behaviour and what kind of further information they need |
Baseline data of a cohort study Qualitative |
Narrative interview Not specified |
Consecutive sample | N = 54 spouses Inpatient, clinic‐based outpatient |
Female: 50.0% Mean age: 52.0 years Level of education: Not specified Duration of illness (partner): 8.0 years |
Met 25% of MMAT criteria.
Met 50% of the MMAT criteria.
Met 75% of the MMAT criteria.
Met 100% of the MMAT criteria.
Information needs
Overall, 121 units of information needs were identified across the entire body of the eight included studies on information needs and coded into the final classification scheme of seven categories and 35 subcategories. For each included study on information needs, identified units of needs could be classified into at least five categories. The seven main categories of information needs are depicted in descending order by the relative frequency of identified needs coded within each category related to the sum of 121 units of needs identified in all included studies: (i) basic facts, (ii) treatment, (iii) coping, (iv) medical system, (v) working and living conditions, (vi) enhancing social functioning, and (vii) self‐help and peer support. The final classification scheme with citations and relative frequencies for each information needs category with associated subcategories are summarized in Table 3.
Table 3.
Classification of information needs in mental disorders identified in n = 8 included articles
| Category (overall %, schizophrenia %, depression %)a | Subcategoryb | % of articlesc | References |
|---|---|---|---|
| Basic facts (34.7%, 30.6%, 40.8%) | Personal experiences of other people with mental disorders (16.7%) | 100.0, n = 8 | 34, 38, 40, 41, 50 |
| Early warning signs and relapse (16.7%) | 34, 39, 40, 42 | ||
| Symptoms (16.7%) | 34, 39, 42, 46 | ||
| Diagnostics (11.9%) | 34, 38, 41, 46 | ||
| Causal model/vulnerability (9.5%) | 34, 38, 46, 50 | ||
| Course of disease and prognosis (9.5%) | 42, 46, 50 | ||
| Recent research (7.1%) | 34 | ||
| Prevalence (4.8%) | 34, 46 | ||
| Normal or mentally ill (4.8%) | 46 | ||
| Comorbid mental health problems (2.4%) | 38 | ||
| Treatment (21.5, 20.8, 22.4) | Side‐effects of medications (46.2%) | 100.0, n = 8 | 34, 38, 39, 40, 41, 42, 46 |
| Psychiatric medications (30.8%) | 34, 38, 41, 42, 46 | ||
| Treatment options (11.5%) | 38, 46, 50 | ||
| Psychosocial treatment/ psychotherapy (11.5%) | 42, 46 | ||
| Coping (19.0, 19.4, 18.4) | Coping with symptoms (26.1%) | 87.5, n = 7 | 38, 39, 40, 42, 46, 50 |
| Strategies for solving problems (21.7%) | 34, 39, 40 | ||
| Stress management (21.7%) | 34, 40 | ||
| Coping with stigma (13.0%) | 34, 38, 42 | ||
| Recovery (13.0%) | 38, 46 | ||
| Coping with anger, violence, assaultive behaviour (4.3%) | 40 | ||
| Medical system (7.4, 5.6, 10.2) | Access to services and professionals (66.7%) | 62.5, n = 5 | 34, 38, 39, 40, 46 |
| Knowledge of health professionals (22.2%) | 38, 46 | ||
| Mental health‐care system (11.1%) | 38, 46 | ||
| Working and living conditions (6.6, 8.3, 4.1) | Legal rights (37.5%) | 50.0, n = 4 | 38, 42 |
| Financial assistance (25.0%) | 46 | ||
| What happens when parent dies (25.0%) | 34 | ||
| Roadworthiness (12.5%) | 46 | ||
| Enhancing social functioning (5.8, 8.3, 2.0) | Communication with relatives (28.6%) | 50.0, n = 4 | 39, 40 |
| Social relationships (28.6%) | 34, 39 | ||
| Leisure and recreation activities (14.3%) | 34 | ||
| Independent living skills (14.3%) | 39 | ||
| Setting limits on the patients' behaviour (14.3%) | 34 | ||
| Self‐help and peer support (5.0, 6.9, 2.0) | Patients' self‐help organizations (50.0%) | 50.0, n = 4 | 34, 39, 42 |
| Relatives' self‐help organizations and support (33.3%) | 41 | ||
| Useful books (16.7%) | 41 |
Relative frequency of identified needs coded within each of the seven main categories determined by dividing the sum of identified units of needs coded within each main category by the 121 units of identified units of needs within the entire body of included articles.
Subcategories are ordered from top to bottom related to their relative frequency by dividing the sum of identified units of needs coded within each of the 35 subcategories by the sum of all identified units of needs coded within the respective main category. In the case of identical frequencies, subcategories are ordered alphabetically.
Number and relative frequency of articles in which each main category was coded.
The category basic facts was the most frequently cited category with ten subcategories that were cited for a total of 42 times in all eight included studies investigating information needs. Therefore, 34.7% of the information needs reported in the literature were associated with disorder‐specific information. The most common subcategories cited in this category were personal experiences of other people with mental disorders (e.g. personal stories; 16.7%), early warning signs and relapse (16.7%) and symptoms (16.7%). Another prominent category was treatment with four subcategories that were cited for a total of 26 times within all studies reviewed. Thus, 21.5% of needs mentioned in the whole body of literature on information needs were related to treatment information with side‐effects of medications (46.2%), psychiatric medications (e.g. effect, dosage, duration; 30.8%), and treatment options (11.5%) being the most commonly cited subcategories. Furthermore, the six subcategories of the category coping were cited 23 times in seven of the eight included studies. Of all information needs identified in the literature, 19.0% were accordingly associated with information on coping strategies and handling the symptoms. Thereby, the subcategories coping with symptoms (26.1%), strategies for solving problems (21.7%) and stress management (21.7%) were the most frequently identified needs in this category. The remaining four categories with associated subcategories accounted for less than 7.5% of all needs identified in the studies reviewed, respectively.
Disorder‐specific differences in frequency distribution were found for the category enhancing social functioning that was significantly more often identified for schizophrenia as compared to depression (P = .034).
Decision‐making needs
Overall, 56 decisions were identified across all four included studies on decision‐making needs and classified using the final classification scheme of six decision categories and 36 subcategories. The results of each study could be coded into at least three of six categories. The six categories of decision‐making needs are depicted in descending order by the relative frequency of identified decisions coded within each category related to the sum of 58 identified decisions coded within all categories as follows: (i) medication treatment, (ii) treatment setting, (iii) general treatment issues, (iv) non‐medication treatment, (v) working and living conditions, and (vi) lifestyle. Table 4 depicts the final classification scheme of treatment decisions with citations and relative frequencies for each needs category with associated subcategories.
Table 4.
Classification of treatment decisions in mental disorders identified in n = 4 included studies on decision‐making needs
| Category (overall %, schizophrenia %, depression %)a | Subcategoryb | % of articlesc | References |
|---|---|---|---|
| Medication treatment (23.2, 21.4, 25.0) | Psychiatric medication (30.8%) | 100, n = 4 | 36, 37, 43, 45 |
| Change medication (15.4%) | 36, 37 | ||
| Dosage (15.4%) | 37, 45 | ||
| Addition of antidepressant medication (7.7%) | 45 | ||
| Application mode, that is depot or oral (7.7%) | 45 | ||
| Choice of antipsychotic agent (7.7%) | 45 | ||
| Discontinue medication (7.7%) | 37 | ||
| Tapering‐off medication (7.7%) | 36 | ||
| Treatment setting (25.0, 25.0, 25.0) | Inpatient treatment (21.4%) | 100, n = 4 | 36, 37, 45 |
| Discharge/leave hospital (14.3%) | 43, 45 | ||
| From who to seek help (14.3%) | 36, 37 | ||
| Absence from the ward (7.1%) | 45 | ||
| Attend a day programme (7.1%) | 37 | ||
| Change in treatment setting (7.1%) | 43 | ||
| Find support in vs. outside neighbourhood (7.1%) | 37 | ||
| Open vs. closed ward (7.1%) | 45 | ||
| Relocate to get specialized treatment (7.1%) | 37 | ||
| Treatment after discharge (7.1%) | 43 | ||
| General treatment issues (14.3, 21.4, 7.1) | Diagnostic examinations (25.0%) | 100, n = 4 | 43, 45 |
| Disciplinary measures/physical and social restraints (25.0%) | 43, 45 | ||
| Frequency of appointments (25.0%) | 36, 37 | ||
| Participation of relatives (12.5%) | 45 | ||
| Regular drug screens (12.5%) | 45 | ||
| Non‐medication treatment (14.3, 14.3, 14.3) | Psychotherapy (50.0%) | 100, n = 4 | 36, 37, 43, 45 |
| Attend counselling (12.5%) | 37 | ||
| Electroconvulsive therapy (12.5%) | 37 | ||
| Psychoeducation (12.5%) | 45 | ||
| Work therapy (12.5%) | 45 | ||
| Working and living conditions (14.3, 17.9, 10.7) | Employment and education (50.0%) | 100, n = 4 | 36, 37, 43, 45 |
| Live arrangements, for example group home, living on own (37.5%) | 37, 43, 45 | ||
| Legal guardianship (12.5%) | 45 | ||
| Lifestyle (8.9, 0.0, 17.9) | Give up alcohol (20.0%) | 25, n = 1 | 37 |
| Improve communication skills (20.0%) | 37 | ||
| Join a support group (20.0%) | 37 | ||
| Keep an active lifestyle (20.0%) | 37 | ||
| Participate in social activities (20.0%) | 37 |
Relative frequency of decisions coded within each of the six main categories determined by dividing the sum of identified decisions coded within each main category by the 56 decisions identified within the entire body of included articles.
Subcategories are ordered from top to bottom related to their relative frequency by dividing the sum of identified decisions coded within each of the 36 subcategories by the sum of all identified decisions coded within the respective main category. In the case of identical frequencies, subcategories are ordered alphabetically.
Number and relative frequency of articles in which each main category was coded.
The category medication treatment was the most commonly cited category with eight decision topics (i.e. subcategories) that were identified for a total of 13 times in the results of all four included studies examining decision‐making needs. Therefore, 23.2% of the decisions identified in the literature were associated with medication treatment with psychiatric medication (30.8%), change medication (15.4%) and dosage (15.4%) being the most frequently cited decisions. A further highly cited category was treatment setting with eleven subcategories that were cited for a total of 14 times within all studies on decision‐making needs. According to this, 25.0% of all decisions revealed in the literature were related to the choice of treatment setting and navigation in the mental health‐care system. Thereby, the subcategory inpatient treatment (21.4%) was the most often cited decision, followed by the subcategories discharge/leave hospital (14.3%) and from whom to seek help (14.3%). The five subcategories of the category general treatment issues were cited for a total of eight times within all studies reviewed. Thus, of all decisions revealed in the included studies, 14.3% were associated with treatment decisions across specific treatment settings. Thereby, the subcategories diagnostic examination (25.0%), disciplinary measures (25.0%) and frequency of appointment (25.0%) were most frequently coded. Furthermore, the five subcategories of the category non‐medication treatment were cited eight times in all included studies. Of all decisions identified in the literature reviewed, 19.0% were accordingly associated with treatment decisions on psychosocial interventions or other non‐medication treatment. Thereby, the subcategory psychotherapy (50.0%) was the most frequently identified decision in this category. The remaining subcategories accounted for 12.5% of all decisions coded in the category non‐medication treatment, respectively. The category working and living conditions was cited for a total of eight times, accounting for 14.3% of all decisions identified in the four included studies on decision‐making needs. The subcategory employment and education (50.0%) was the most frequently cited subcategory in this main category. However, the decision category lifestyle was only identified five times in one of the four included studies. Therefore, of all decisions revealed in the whole body of literature, only 8.9% were associated with decisions regarding lifestyle changes or coping efforts.
Disorder‐specific differences could be observed for decision‐making needs. The category general treatment issues was more commonly classified for schizophrenia compared to depression (P = .056). The category lifestyle was significantly more often identified in studies examining decisional needs in depression compared with schizophrenia (P < .001).
Discussion
This paper presents the findings of a systematic review of studies examining information and decision‐making needs among patients with depression, anxiety disorders, somatoform disorders, alcohol‐related disorders, and schizophrenia. The focus of this work was restricted to studies assessing needs among specific diagnostic groups. Therefore, studies that investigated patients' needs across different diagnoses were excluded.
The number of included studies (n = 12) was relatively small compared with 112 studies on information needs in patients with cancer identified by Rutten and colleagues33 or 40 studies that Murray and colleagues54 identified in their systematic review on decisional needs in adults with chronic kidney disease. Most of the included studies focused on information needs among patients with depression or schizophrenia and their relatives. Only one of these studies additionally assessed information needs in patients with anxiety.
The results suggest that patients and relatives with depression and schizophrenia perceive a high need for information on a wide range of topics. This finding is supported by studies investigating information and decision‐making needs across different diagnoses.14, 16, 55, 56 Information on the personal experience of others being affected by the illness and information on psychiatric medication, particularly side‐effects of medications, might be of special interest for patients and relatives with depression and schizophrenia. Furthermore, information on coping and handling the symptoms was frequently cited. The results further indicate that topics related to social functioning might be of more importance for patients with schizophrenia and their relatives compared to users suffering from depression. The latter results reflect the fact that patients with schizophrenia show significantly higher levels of social impairment compared to patients with affective disorders.57
However, only four studies on depression and schizophrenia were found related to the reviews' focus on decision‐making needs of which two studies were restricted to the identification of decision topics.46, 48 For this reason, other dimensions of decision‐making needs that are seen as essential components to inform the design of PtDAs were not included in the data analysis.58 The available data suggest that decisions on medication treatment and decisions concerning the choice of treatment setting, especially inpatient admission, may be particularly relevant for SDM in depression and schizophrenia treatment. The results also indicate that the patients' decision‐making needs may vary depending on the specific psychiatric diagnosis as the results showed that general treatment issues, for example diagnostic examination and disciplinary measures, might have been of special relevance in the treatment of patients with schizophrenia compared to depression.
Limitations
Several methodological limitations are associated with this review. First, the search process was limited to one database only. As a consequence, we might have missed relevant publications. However, this risk of bias was assumed to be low as MEDLINE covers a wide range of journals being of relevance in the field of medical decision‐making and electronic search was complemented by a thorough screening of the reference lists of included studies and relevant review articles. Selecting more databases might have resulted in a higher sensitivity but lower specificity as more irrelevant hits were expected, and therefore, the cost‐to‐benefit ratio would have been reduced. As this review was the first step in a highly time‐consuming and elaborate development process, this pragmatic approach was considered to be justifiable.
MMAT quality assessment indicates that the quality of the papers included varied considerably in methodological quality, which might bias our conclusions. Nevertheless, as this review did not aim at synthesizing evidence relating to treatment outcomes, no study was excluded due to low methodological quality. Not to exclude studies enabled us to summarize a more comprehensive and significant amount of data. The results further need to be interpreted with caution allowing for the low consistency of studies in study design, sample, outcomes, settings and countries of origin. In particular, studies considerably varied in sample size from 14 up to 352 participants.44, 48 However, the vast majority of studies showed sample sizes between 100 and 200 respondents.34, 37, 41, 42, 43, 45, 49 Moreover, the patient characteristics being assessed varied significantly. For example, less than half of publications reported on mean age,36, 45, 46, 48, 53 a third of studies assessed level of education,37, 42, 43, 45 one of four publications reported on duration of illness,42, 45, 53 and only one study assessed severity of symptoms.36 None of the identified studies reported on psychiatric or somatic comorbidity. Furthermore, the relative frequency of identified needs was dependent on how the included studies collected data (e.g. length of questionnaires, conceptualization of needs). For example, the ENQ was conducted in a number of studies and, according to that, the needs it asked were identified more often in our data analysis.34, 42, 43, 45 Thus, the relative frequency of citations in the literature does not allow for assumptions regarding the clinical relevance of particular needs.
Finally, informational and decisional needs were widely investigated in various clinical settings and were further restricted to two psychiatric diagnoses. Thus, the findings are limited in generalizability and do specifically not allow for assumptions regarding subgroups of patients classified by demographic factors, clinical settings, specific diagnoses or the severity of symptoms.
Implications
Existing evidence supports the need to provide high‐quality health information and targeted interventions to support patient participation in mental health treatment decision‐making. Although this review shows several methodological limitations and the results are of limited use for informing the design of PtDAs in detail, they hold the potential to inform the first draft of web‐based PtDAs for depression and schizophrenia.
As severe mental disorders are chronic illnesses, decision support might need to comprise multiple decision points along the course of disease and multiple delivery settings.59 According to this, this review identified numerous information needs and decision topics among patients and relatives with depression and schizophrenia. To meet the needs of a large part of potential users, PtDAs for depression and schizophrenia should cover a wide range of topics. This need could be accounted for by providing easy to understand and brief information units for each topic including the possibility to access more in‐depth information. To account for the multiple decision points along the care continuum for which patients might need decision support, short decision support tools as provided by Elwyn and colleagues60 might be integrated in a more comprehensive PtDA.
The results of this review might also give initial indications on the thematic focus of the PtDAs. It is suggested that information on medication might be of high relevance for patients with depression and schizophrenia. This assumption is supported by the results on relevant decision topics that showed decisions regarding medication treatment being most often identified in the data analysis. Decisions on the choice of treatment setting (e.g. inpatient vs. outpatient treatment) were identified as further important topics. Therefore, a special focus on the provision of medication‐related information and the choice of treatment might be appropriate. This assumption is supported by Paton and Esop61 who showed that although the NICE Guideline on schizophrenia recommends information provision that is targeted to the patients' needs as a pre‐requisite for SDM, almost half of outpatients with schizophrenia reported that they had not been given enough information about antipsychotic medication. Although the current evidence on superior effects of PtDAs that incorporate personal stories is insufficient, the results of this review that identified a need for information about the lived experience of others being affected support the assumption that personal reports from peers may improve acceptance and usage of PtDAs.62 However, more qualitative and quantitative research is needed to confirm these presumptions regarding information and decisional needs in depression and schizophrenia.
The body of evidence that was identified in our systematic search was little and largely restricted to information needs and the identification of decision topics. Additionally, no study was found that investigated informational or decisional needs in somatoform disorders or alcohol‐related disorders and only one study also examined information needs in anxiety disorders. The current work therefore revealed an important research gap given the high prevalence of these disorders and the high relevance of SDM in the treatment of mental disorders in recovery‐oriented and patient‐centred mental health care.1, 6, 63 In sum, more research is needed related to the assessment of needs as a prerequisite for the systematic development of psychoeducation and decision‐support interventions based on the IPDAS criteria.64 Thereby, disorder‐specific investigations are needed as it may be supposed that patients with diverse mental disorders show significant differences in information needs and decision‐making needs such as important topics, participation preference, decisional conflict, or support needs. The typologies of needs developed in this review may serve as a framework for developing more comprehensive and standardized assessment tools for evaluating information and decision‐making needs in patients with diverse mental disorders.
Conflict of interest
None.
Supporting information
Appendix S1. Example search strategy to identify studies from MEDLINE.
Acknowledgement
This project was funded by the German Ministry of Education and Research (Project number: 01GX0742).
References
- 1. Storm M, Edwards A. Models of user involvement in the mental health context: intentions and implementation challenges. Psychiatric Quarterly, 2013; 82: 313–327. [DOI] [PubMed] [Google Scholar]
- 2. Hamann J, Leucht S, Kissling W. Shared decision making in psychiatry. Acta Psychiatrica Scand., 2003; 107: 403–409. [DOI] [PubMed] [Google Scholar]
- 3. Mueser KT. Evidence‐based practices and recovery‐oriented services: is there a relationship? Should there be one? Psychiatric Rehabilitation Journal, 2012; 35: 287–288. [DOI] [PubMed] [Google Scholar]
- 4. Gaebel W, Becker T, Janssen B et al EPA guidance on the quality of mental health services. European Psychiatry, 2012; 27: 87–113. [DOI] [PubMed] [Google Scholar]
- 5. Härter M, Klesse C, Bermejo I, Schneider F, Berger M. Unipolar depression: diagnostic and therapeutic recommendations from the current S3/National Clinical Practice Guideline. Deutsches Ärzteblatt International, 2010; 107: 700–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Center for Mental Health Services . Shared Decision Making in Mental Health Care: Practice, Research and Future. Rockville, MD: Substance Abuse and Mental Health Service Administration, 2010. [Google Scholar]
- 7. Clever SL, Ford DE, Rubenstein LV et al Primary care patients' involvement in decision‐making is associated with improvement in depression. Medical Care, 2006; 44: 398–405. [DOI] [PubMed] [Google Scholar]
- 8. Tambuyzer E, Van Audenhove C. Is perceived patient involvement in mental health care associated with satisfaction and empowerment? Health Expectations, 2013; doi:10.1111/hex.12052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Loh A, Simon D, Wills CE, Kriston L, Niebling W, Harter M. The effects of a shared decision‐making intervention in primary care of depression: a cluster‐randomized controlled trial. Patient Education and Counseling, 2007; 67: 324–332. [DOI] [PubMed] [Google Scholar]
- 10. Woolley SB, Fredman L, Goethe JW, Lincoln AK, Heeren T. Hospital patients' perceptions during treatment and early discontinuation of serotonin selective reuptake inhibitor antidepressants. Journal of Clinical Psychopharmacology, 2010; 30: 716–719. [DOI] [PubMed] [Google Scholar]
- 11. Adams JR, Drake RE, Wolford GL. Shared decision‐making preferences of people with severe mental illness. Psychiatric Services, 2007; 58: 1219–1221. [DOI] [PubMed] [Google Scholar]
- 12. Hamann J, Neuner B, Kasper J et al Participation preferences of patients with acute and chronic conditions. Health Expectations, 2007; 10: 358–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Patel SR, Bakken S, Ruland C. Recent advances in shared decision making for mental health. Current Opinion in Psychiatry, 2008; 21: 606–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Puschner B, Neumann P, Jordan H et al Development and psychometric properties of a five‐language multiperspective instrument to assess clinical decision making style in the treatment of people with severe mental illness (CDMS). BMC Psychiatry, 2013; 13: 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Goss C, Moretti F, Mazzi MA, Del Piccolo L, Rimondini M, Zimmermann C. Involving patients in decisions during psychiatric consultations. British Journal of Psychiatry, 2008; 193: 416–421. [DOI] [PubMed] [Google Scholar]
- 16. McCabe R, Khanom H, Bailey P, Priebe S. Shared decision‐making in ongoing outpatient psychiatric treatment. Patient Education and Counseling, 2013; 91: 326–328. [DOI] [PubMed] [Google Scholar]
- 17. Goossensen A, Zijlstra P, Koopmanschap M. Measuring shared decision making processes in psychiatry: skills versus patient satisfaction. Patient Education and Counseling, 2007; 67: 50–56. [DOI] [PubMed] [Google Scholar]
- 18. Elwyn G, Frosch D, Rollnick S. Dual equipoise shared decision making: definitions for decision and behaviour support interventions. Implementation Science, 2009; 4: 75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Duncan E, Best C, Hagen S. Shared decision making interventions for people with mental health conditions. Cochrane Database of Systematic Review, 2010; 1: CD007297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hamann J, Maris N, Iosifidou P et al Effects of a question prompt sheet on active patient behaviour: a randomized controlled trial with depressed outpatients. International Journal of Social Psychiatry, 2013; 60: 227–235. [DOI] [PubMed] [Google Scholar]
- 21. Henderson C, Brohan E, Clement S et al Decision aid on disclosure of mental health status to an employer: feasibility and outcomes of a randomised controlled trial. British Journal of Psychiatry, 2013; 203: 350–357. [DOI] [PubMed] [Google Scholar]
- 22. Joosten EA, de Jong CA, de Weert‐van Oene GH, Sensky T, van der Staak CP. Shared decision‐making reduces drug use and psychiatric severity in substance‐dependent patients. Psychotherapy and Psychosomatics, 2009; 78: 245–253. [DOI] [PubMed] [Google Scholar]
- 23. Joosten EA, De Jong CA, de Weert‐van Oene GH, Sensky T, van der Staak CP. Shared decision‐making: increases autonomy in substance‐dependent patients. Substance Use and Misuse, 2011; 46: 1037–1038. [DOI] [PubMed] [Google Scholar]
- 24. van der Krieke L, Emerencia AC, Boonstra N, Wunderink L, de Jonge P, Sytema S. A web‐based tool to support shared decision making for people with a psychotic disorder: randomized controlled trial and process evaluation. Journal of Medical Internet Research, 2013; 15: e216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Westermann GM, Verheij F, Winkens B, Verhulst FC, Van Oort FV. Structured shared decision‐making using dialogue and visualization: a randomized controlled trial. Patient Education and Counseling, 2013; 90: 74–81. [DOI] [PubMed] [Google Scholar]
- 26. Woltmann EM, Wilkniss SM, Teachout A, McHugo GJ, Drake RE. Trial of an electronic decision support system to facilitate shared decision making in community mental health. Psychiatric Services, 2011; 62: 54–60. [DOI] [PubMed] [Google Scholar]
- 27. Härter M, Kentgens M, Brandes A et al Rationale and content of psychenet: the Hamburg Network for Mental Health. European Archives of Psychiatry and Clinical Neuroscience, 2012; 262(Suppl 2): S57–S63. [DOI] [PubMed] [Google Scholar]
- 28. Coulter A, Stilwell D, Kryworuchko J, Mullen P, Ng C, van der Weijden T. A systematic development process for patient decision aids. BMC Medical Informatics and Decision Making, 2013; 13(Suppl 2): S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Sepucha KR, Borkhoff CM, Lally J et al Establishing the effectiveness of patient decision aids: key constructs and measurement instruments. BMC Medical Informatics and Decision Making, 2013; 13(Suppl 2): S12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Jacobi F, Wittchen HU, Holting C et al Prevalence, co‐morbidity and correlates of mental disorders in the general population: results from the German Health Interview and Examination Survey (GHS). Psychological Medicine, 2004; 34: 597–611. [DOI] [PubMed] [Google Scholar]
- 31. O'Connor AM, Tugwell P, Wells GA et al A decision aid for women considering hormone therapy after menopause: decision support framework and evaluation. Patient Education and Counseling, 1998; 33: 267–279. [DOI] [PubMed] [Google Scholar]
- 32. Adams E, Boulton M, Watson E. The information needs of partners and family members of cancer patients: a systematic literature review. Patient Education and Counseling, 2009; 77: 179–186. [DOI] [PubMed] [Google Scholar]
- 33. Rutten LJ, Arora NK, Bakos AD, Aziz N, Rowland J. Information needs and sources of information among cancer patients: a systematic review of research (1980‐2003). Patient Education and Counseling, 2005; 57: 250–261. [DOI] [PubMed] [Google Scholar]
- 34. Mueser KT, Bellack AS, Wade JH, Sayers SL, Rosenthal CK. An assessment of the educational needs of chronic psychiatric patients and their relatives. British Journal of Psychiatry, 1992; 160: 674–680. [DOI] [PubMed] [Google Scholar]
- 35. Bunn H, Lange I, Urrutia M et al Health preferences and decision‐making needs of disadvantaged women. Journal of Advanced Nursing, 2006; 56: 247–260. [DOI] [PubMed] [Google Scholar]
- 36. Simon D, Loh A, Wills CE et al Depressed patients' perceptions of depression treatment decision‐making. Health Expectations, 2006; 10: 62–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Stacey D, Menard P, Gaboury I et al Decision‐making needs of patients with depression: a descriptive study. Journal of Psychiatric and Mental Health Nursing, 2008; 15: 287–295. [DOI] [PubMed] [Google Scholar]
- 38. Pluye P, Gagnon MP, Griffiths F, Johnson‐Lafleur J. A scoring system for appraising mixed methods research, and concomitantly appraising qualitative, quantitative and mixed methods primary studies in Mixed Studies Reviews. International Journal of Nursing Studies, 2009; 46: 529–546. [DOI] [PubMed] [Google Scholar]
- 39. Pace R, Pluye P, Bartlett G et al Testing the reliability and efficiency of the pilot Mixed Methods Appraisal Tool (MMAT) for systematic mixed studies review. International Journal of Nursing Studies, 2012; 49: 47–53. [DOI] [PubMed] [Google Scholar]
- 40. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. British Medical Journal, 2009; 339: b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Barney LJ, Griffiths KM, Banfield MA. Explicit and implicit information needs of people with depression: a qualitative investigation of problems reported on an online depression support forum. BMC Psychiatry, 2011; 11: 88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Chien WT, Kam CW, Lee IF. An assessment of the patients' needs in mental health education. Journal of Advanced Nursing, 2001; 34: 304–311. [DOI] [PubMed] [Google Scholar]
- 43. Chien WT, Norman I, Chien W‐T, Norman I. Educational needs of families caring for Chinese patients with schizophrenia. Journal of Advanced Nursing, 2003; 44: 490–498. [DOI] [PubMed] [Google Scholar]
- 44. Gaskill D, Cooney H. Coping with schizophrenia: what does the spouse need to know? Australian Journal of Advanced Nursing, 1991; 9: 10–15. [PubMed] [Google Scholar]
- 45. Gumus AB, Gumus AB. Health education needs of patients with schizophrenia and their relatives. Archives of Psychiatric Nursing, 2008; 22: 156–165. [DOI] [PubMed] [Google Scholar]
- 46. Hamann J, Mendel RT, Fink B et al Patients' and psychiatrists' perceptions of clinical decisions during schizophrenia treatment. Journal of Nervous and Mental Disease, 2008; 196: 329–332. [DOI] [PubMed] [Google Scholar]
- 47. Ende J, Kazis L, Ash A, Moskowitz MA. Measuring patients' desire for autonomy: decision making and information‐seeking preferences among medical patients. Journal of General Internal Medicine, 1989; 4: 23–30. [DOI] [PubMed] [Google Scholar]
- 48. Hamann J, Mendel R, Cohen R et al Psychiatrists' use of shared decision making in the treatment of schizophrenia: patient characteristics and decision topics. Psychiatric Services, 2009; 60: 1107–1112. [DOI] [PubMed] [Google Scholar]
- 49. Llewellyn‐Jones S, Gill J, Donnelly P. Questions patients ask psychiatrists. Psychiatric Bulletin, 2001; 25: 21–24. [Google Scholar]
- 50. Lowe B, Spitzer RL, Grafe K et al Comparative validity of three screening questionnaires for DSM‐IV depressive disorders and physicians' diagnoses. Journal of Affective Disorders, 2004; 78: 131–140. [DOI] [PubMed] [Google Scholar]
- 51. Bee P, Playle J, Lovell K, Barnes P, Gray R, Keeley P. Service user views and expectations of UK‐registered mental health nurses: a systematic review of empirical research. International Journal of Nursing Studies, 2008; 45: 442–457. [DOI] [PubMed] [Google Scholar]
- 52. Degner LF, Sloan JA, Venkatesh P. The Control Preferences Scale. Canadian Journal of Nursing Research, 1997; 29: 21–43. [PubMed] [Google Scholar]
- 53. Wittmund B, Bischkopf J, Angermeyer MC. Educational needs among spouses of depressive patients and their illness models of depression. Gesundheitswesen, 2001; 63: 536–541. [DOI] [PubMed] [Google Scholar]
- 54. Murray MA, Brunier G, Chung JO et al A systematic review of factors influencing decision‐making in adults living with chronic kidney disease. Patient Education and Counseling, 2009; 76: 149–158. [DOI] [PubMed] [Google Scholar]
- 55. Hill SA, Laugharne R. Decision making and information seeking preferences among psychiatric patients. Journal of Mental Health, 2006; 15: 75–84. [Google Scholar]
- 56. Powell J, Clarke A. Information in mental health: qualitative study of mental health service users. Health Expectations, 2006; 9: 359–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Bottlender R, Strauss A, Moller HJ. Social disability in schizophrenic, schizoaffective and affective disorders 15 years after first admission. Schizophrenia Research, 2010; 116: 9–15. [DOI] [PubMed] [Google Scholar]
- 58. O'Connor AM, Drake ER, Wells GA, Tugwell P, Laupacis A, Elmslie T. A survey of the decision‐making needs of Canadians faced with complex health decisions. Health Expectations, 2003; 6: 97–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Hoffman AS, Volk RJ, Saarimaki A et al Delivering patient decision aids on the Internet: definitions, theories, current evidence, and emerging research areas. BMC Medical Informatics and Decision Making, 2013; 13(Suppl 2): S13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Elwyn G, Lloyd A, Joseph‐Williams N et al Option Grids: shared decision making made easier. Patient Education and Counseling, 2013; 90: 207–212. [DOI] [PubMed] [Google Scholar]
- 61. Paton C, Esop R. Patients' perceptions of their involvement in decision making about antipsychotic drug choice as outlined in the NICE guidance on the use of atypical antipsychotics in schizophrenia. Journal of Mental Health, 2005; 14: 305–310. [Google Scholar]
- 62. Bekker HL, Winterbottom AE, Butow P et al Do personal stories make patient decision aids more effective? A critical review of theory and evidence. BMC Medical Informatics and Decision Making, 2013; 13(Suppl 2): S9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Wittchen HU, Jacobi F, Rehm J et al The size and burden of mental disorders and other disorders of the brain in Europe 2010. European Neuropsychopharmacology, 2011; 21: 655–679. [DOI] [PubMed] [Google Scholar]
- 64. Elwyn G, O'Connor A, Stacey D et al Developing a quality criteria framework for patient decision aids: online international Delphi consensus process. British Medical Journal, 2006; 333: 417–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Example search strategy to identify studies from MEDLINE.


