Abstract
Background
There is an increasing need to assess the performance of emergency ambulance services using measures other than the time taken for an ambulance to arrive on scene. In line with government policy, patients and carers can help to shape new measures of ambulance service performance.
Objective
To investigate the aspects of emergency ambulance service care valued by users.
Design
Qualitative interview study.
Setting
One of 11 ambulance services in England.
Participants
Twenty‐two users and eight of their spouses (n = 30).
Results
Users of the emergency ambulance service, experiencing different types of ambulance service response, valued similar aspects of their pre‐hospital care. Users were often extremely anxious about their health, and the outcome they valued was reassurance provided by ambulance service staff that they were receiving appropriate advice, treatment and care. This sense of being reassured was enhanced by the professional behaviour of staff, which instilled confidence in their care; communication; a short wait for help; and continuity during transfers. A timely response was valued in terms of allaying anxiety quickly.
Discussion and conclusions
The ability of the emergency ambulance service to allay the high levels of fear and anxiety felt by users is crucial to the delivery of a high quality service. Measures developed to assess and monitor the performance of emergency ambulance services should include the proportion of users reporting feeling reassured by the response they obtained.
Keywords: communication, emergency medical services, patient experience, patient satisfaction, prehospital care
Introduction
Ambulance services were originally conceived as a transport service to take acutely injured or ill people to hospital. In recent years, the role and function of emergency ambulance services has evolved to include providing pre‐hospital patient care and treatment. Internationally, there are different models of delivering this care,1 but all have a common purpose of assessing and treating life‐threatening or life‐changing illness and injury as well as transporting patients to definitive care. In the United Kingdom (UK), the level and speed of response provided is determined by the clinical need of the patient within a wider national performance and regulatory framework. Levels of response include: enhanced clinical telephone assessment with no ambulance response (‘hear and treat’); on‐scene treatment by appropriately skilled practitioners for patients who do not require hospital admission (‘see and treat’); and pre‐hospital assessment and treatment before transportation to acute care (‘see and convey’).
Internationally, ambulance service performance measurement has been dominated by the process measure of response time – how quickly an ambulance arrives at the scene of an incident.1 The rationale for using this process performance measure is based on research evidence showing the relationship between time and patient outcome for specific clinical conditions, primarily out‐of‐hospital cardiac arrest.2 However, this group accounts for only two percent of patients attended by ambulance services in the UK.3 There is a need to develop further outcome measures of emergency ambulance services, relevant to the majority of patients.
Recent UK health policy has emphasised the importance of understanding patient perspectives of the care they receive.4 The focus has been on using surveys to elicit patient satisfaction with,5, 6, 7 and experience of, ambulance care. Qualitative research exploring users' experiences of emergency ambulance services has often focused on specific patient groups, for example those suffering symptoms of pain,8 or conditions such as stroke or acute myocardial infarction,9 rather than the range of users. It is important to explore the outcomes as well as processes of care, important to ambulance users, that are relevant to the range of ambulance users including those who do not have a life‐threatening condition and those who are managed using telephone advice only.
As part of a large programme of research to develop more meaningful ways of measuring the impact and quality of pre‐hospital care, Prehospital Outcomes for Evidence Based Evaluation (PhOEBE),10 we undertook a qualitative study of the views of recent users of emergency ambulance services. Our research question was: what do users value about their emergency ambulance service experience?
Methods
Design
A qualitative design was employed, interviewing recent users of the emergency ambulance service. Depending on participants' preferences, we undertook face‐to‐face or telephone interviews.
Setting and participants
We undertook the study in one of 11 ambulance services in England in 2012. East Midlands Ambulance Service NHS Trust (EMAS) delivers services to a population of around 4.8 million people, answering 616 200 calls in 2012–2013. EMAS covers five counties of mixed urban and rural populations. We sampled users of the emergency ambulance service from 1 week in the summer and 1 week in the autumn of 2012 to represent typical weeks. We included adults aged 16 years and over living in their own home or in residential and nursing homes. The following exclusion criteria were applied: any public location without a specific address to which a request for interview could be sent; any address where a patient had expressed a wish not to be contacted by EMAS; and people who could not participate using the English language. We also excluded vulnerable groups because we felt that these needed specific research protocols to meet their needs. These included patients who had the following recorded in their notes during the call and dispatch stage: attempted suicide, violent assaults, enduring psychiatric disorders, domestic violence or drug overdoses, people with Do Not Attempt Resuscitation on their ambulance records, or any address which appeared on the EMAS safeguarding register.
After excluding people in these groups, we purposively sampled to recruit users experiencing three types of response from the ambulance service: ‘hear and treat’, ‘see and treat’ and ‘see and convey’. The rationale for this sampling strategy was that users in these groups may value different outcomes. EMAS staff used random numbers to identify 50 patients from each of the three groups. For ‘hear and treat’ and ‘see and treat’, EMAS staff sent each user a covering letter, participant information sheet, consent form, reply slip and reply paid envelope to request an interview. For the ‘see and convey’ group, EMAS staff wrote to the patients' GPs to check whether or not they considered it appropriate to contact the patient. This extra step was introduced because this group was most likely to include people with severe health problems, and we wanted to reduce the possibility that our request would upset relatives of people who had died or were still critically ill. If the GP felt that contact was appropriate, EMAS staff contacted users using the same approach as the other two groups.
We had intended to undertake maximum diversity sampling once those contacted had responded positively. However, recruitment rates were low, and we interviewed everyone who agreed. The first round of contacting 150 people yielded nine participants for interview. We had planned to interview 16–24 people based on data saturation,11 so the recruitment strategy was repeated, contacting a different set of patients, which yielded a further 13 interviews.
Ethics approval
The study was approved by an NHS Research Ethics Committee (12/EM/022). Approval for research management and governance was sought and gained from EMAS NHS Trust.
Interviews
Eighteen face‐to‐face and four telephone interviews were conducted by FT and VHP between September 2012 and January 2013. Prior to commencing the main interview, we asked participants to answer several questions around their demographic characteristics including employment status and ethnicity. Within this questioning process, we asked participants to self‐report their reason for calling the ambulance service. Spouses were present and contributed to eight interviews because they had usually made the initial telephone call to the emergency ambulance service. We used a semi‐structured interview schedule to explore participants' experiences. Rather than ask directly about outcomes important to them, the first part of the interview used the critical‐incident technique to determine positive and negative aspects of key stages of their ambulance service experience.12 The second part asked them more explicitly to identify what they valued most about the service received and how performance should be measured. Interviews lasted on average 25 minutes (range 15–60 min).
Analysis
All interviews were digitally recorded and transcribed verbatim. We undertook the five stages of framework analysis13 using NVivo 8 to facilitate data management. Two researchers (FT and VHP) first familiarised themselves with the data by reading and rereading transcripts (Stage 1). They then developed an initial thematic framework based on reading the transcripts (Stage 2) before presenting this to the wider team (AOC, NS and JT) for discussion. Following agreement, FT and VHP coded all transcripts to these themes adding any new emerging themes (Stage 3). FT summarised the findings based on data extracted from the initial and emerging themes (Stage 4). During discussions of these findings, the team constructed a thematic map (see Fig. 1) related to the issues that participants valued, showing that reassurance was the outcome they valued and the relationship of process issues in achieving reassurance (Stage 5).
Figure 1.
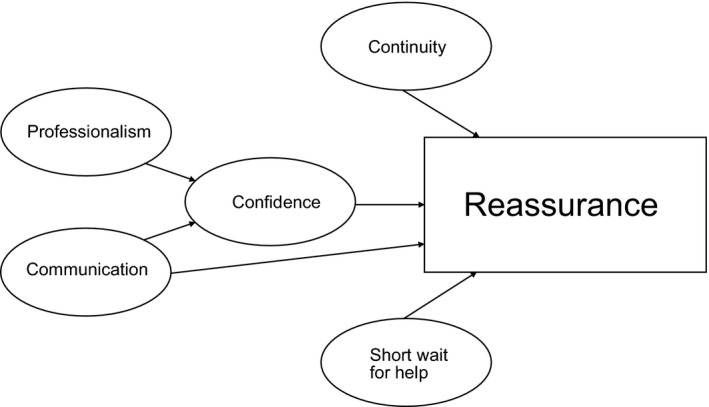
Thematic map of aspects of the emergency ambulance service valued by users.
Findings
Description of sample
We interviewed patients with spouses across a range of ambulance service response types (n = 30; 22 patients and 8 spouses): hear and treat (n = 2 patients and 1 spouse), see and treat (n = 7 patients and 2 spouses) and see and convey (n = 13 patients and 5 spouses). Please see Table 1. For eleven participants, this was the first time that they had called the emergency ambulance service. At the end of 22 interviews, we had the option of selecting a third sample. On reflection, we felt that we had achieved data saturation because no new issues had been raised in our last few interviews.
Table 1.
Demographic characteristics of patients
| Study ID | Gender of patient | Age | Category | Self‐reported reason for calling the ambulance service | Ethnicity |
|---|---|---|---|---|---|
| P1 | Female | 55–64 | See and convey | Breathing difficulties | White British |
| P2 | Female | 45–54 | Hear and treat | Agony, severe stomach ache and could hardly stand up | White British |
| P3a + b | Male | 65+ | See and treat | Diabetic hypoglycaemia | White British |
| P4a + b | Male | 55–64 | See and convey | Disorientation and low pulse | Participant declined to give ethnicity data |
| P5 | Female | 65+ | See and convey | Anxiety attack with high blood pressure | White British |
| P6 | Male | 45–54 | See and convey | Hernia Bleed – infection | White British |
| P7a + b | Male | 65+ | See and convey | Suspected Stroke (TIA) | White English |
| P8 | Male | 35–44 | See and convey | Kidney Stones | White British |
| P9 | Female | 25–34 | See and treat | Son had high temperature | White British |
| P10 | Female | 65+ | See and convey | Sickness and diarrhoea | White British |
| P11 | Male | 65+ | See and treat | Stroke (suspected stroke) | White British |
| P12 | Female | 65+ | See and convey | Abdominal pain and pancreatitis? | White British |
| P13a + b | Male | 65+ | See and convey | Breathing difficulties | White British |
| P14 | Male | 65+ | See and convey | Neck pain | White British |
| P15a +b | Female | 65+ | See and treat | Side‐effects of MS tablets | White British |
| P16 | Female | 65+ | See and convey | Severely out of breath | White British |
| P17 | Male | 55–64 | See and convey | Chest tightness | Asian or Asian British/Indian |
| P18a + b | Male | 45–54 | Hear and treat | Extreme pain in groin area and leg, and worst pain ever experienced | White and black Caribbean – English |
| P19a + b | Male | 65+ | See and treat | Fallen and smashed face open, and bleeding head from old scar | White British |
| P20 | Female | 65+ | See and treat | Fallen | White British |
| P21a + b | Female | 65+ | See and convey | Patient couldn't stand up, collapsed and couldn't walk | White British |
| P22 | Female | 55–64 | See and convey | Breathing difficulties | White British |
Summary of results
Participants in our study, regardless of clinical condition or level of ambulance service response received, valued similar aspects of their pre‐hospital care experience. The outcome they valued was reassurance to alleviate the anxiety, fear or panic that they experienced at the time of calling an ambulance. The processes they valued helped to achieve this reassurance: professionalism, communication, short wait for help and continuity across transfer points. These processes helped to achieve reassurance either directly or through instilling confidence in the ambulance service (see Fig. 1).
Reassurance and confidence
Sources of reassurance
Reassurance – that is having doubts or fears reduced or removed – was highly valued by the range of ambulance service users we interviewed. All participants described feelings of fear, anxiety and panic caused by concerns about the seriousness of the episode of illness/injury they were experiencing. All of them described how these feelings were reduced by care received from staff who they perceived knew what to do and how to help them safely and appropriately:
Because I was sat on my own, because my wife and children were all asleep, so I had somebody sort of talking to me… and calming me down, saying right we'll get you to the ambulance, we'll get you to hospital, you'll be there soon so they was calming me down as well and the reassurance that they could do something when, if it started to get a lot worse. (P8, Male, 35–44 years, see and convey, first‐time user, kidney stones)
He was so good and he was lovely. He did everything that, you know I've never had to call an ambulance out before, so…basically, he talked us through everything he was doing and we kind of both felt at ease and reassured with what he was doing so, there wasn't anything I could have said ‘oh yes, maybe he could have done that or maybe he could have done this. He didn't rush off; he spent the time with us. (P9, Female, 25–34 years, see and treat, first time user, young son had high temperature)
A different type of reassurance, which was not related to the reason why they called the ambulance service, was gained by a few participants when staff affirmed that they had made the right decision by calling an ambulance. Users and/or their spouses often expressed feelings of guilt or uncertainty about using valuable resources that might be needed for someone, who they perceived to have a more urgent need than them. It was important to users that the call handler or attending clinicians allayed these feelings of guilt:
And he was nice. He was…made me feel…because I was like, falling over myself to apologise even though I couldn't properly talk but I'd felt awful that I'd phoned A&E. You just don't do it really do you? You imagine it's for car accidents or if someone's fainted or…I don't know. I felt bad phoning them but he was really, really nice. (P2, Female, 45–54 years, hear & treat, first time user, severe abdominal pains)
Confidence in the service
Feeling reassured was closely associated with confidence, that is the feeling or belief that something or someone can be relied on. Participants generally expressed an inherent confidence that by calling 999, they placed responsibility for their care in the hands of health‐care professionals who would know what to do and how to help them. This inherent confidence was the starting position from which the rest of their ambulance service care experience was based:
Interviewer: How did that make you feel?
Participant: More confident. I panic until I know somebody's on their way. Once I've dialled 999, I then calm down and I'm fine
(P3 spouse, Female, 65+, see & treat, used service before, diabetic hypoglycaemia)
Professionalism
Participants used the term ‘professional’ when describing both positive and negative behaviours and conduct of ambulance staff. For example:
They come in and introduce themselves and get on with the job with what they've got to do but be nice and pleasant about it…Not being bossy or arrogant or anything else, just got to be right about it…That's what I mean about being professional. (P21, Female, 65+, see & convey, used service before, collapsed)
Participants achieved reassurance from the competence and skill of clinicians who they perceived to be knowledgeable and thorough in their clinical assessment and treatment. Reassurance was also gained from the interpersonal skills such as being calm, kind and informative. Both call handlers and ambulance crews were valued for these skills, which users and their spouses described as reducing high levels of anxiety and maintaining confidence in the service.
I think he covered everything, I don't think there is anything that he could have done any more on. You know, I think he knew what to talk to you about, he knew how to talk to you and he gave you confidence because he was such a pleasant person. (P15, Female, 65+, see and treat, first time use, side‐effects of medication)
I think they appeared very well to know their job, they get on with what needs to be doing, sticking things all over your body you know that sort of thing, it's no problem. They'll say ‘we need to take your medication with us have you got your handbag, have you locked the door?’ and everything falls into place very very well. (P5, Female, 65+, see & convey, used service before, anxiety attack with high blood pressure)
Communication
Verbal and non‐verbal communication of ambulance staff was central to participants feeling reassured. Their ‘professional calmness’ (P4 spouse, 65+, see and convey, first time user, disorientation & low pulse) was a non‐verbal expression of being in control of the situation, which helped to alleviate patients' anxiety. We identified three important aspects of communication: feeling listened to, being informed and communication style.
Feeling listened to
When people initially contact the ambulance service, call handlers need to obtain information from the caller using a computerised protocol. They use this to assess whether or not an ambulance is the most appropriate response and the urgency of response needed. In the case of ‘hear and treat’ calls, users are provided with telephone advice by call handlers, paramedics or nurses at the call centre. They may expect an ambulance, so call handlers may have to explain that an ambulance will not be sent. In this situation, the caller feeling listened to was extremely important, as illustrated by two contrasting experiences from ‘hear and treat’ users in our sample. Both users were advised that an ambulance would not be the most appropriate course of action for them. However, the way in which they perceived this information was given was markedly different. One user concluded that ‘exactly what he recommended was the best course of action for me’ (p2, Female, 45–54, hear & treat, first time user, severe abdominal pain) whereas the other summarised their experience as ‘disgusting’ (P18, Male, 45–54, hear & treat, first time user, extreme pain in leg), even though both were essentially given the same advice. The key difference between the two experiences was that in the first situation, the user felt that the call handler listened to them and then advised accordingly: ‘It was friendly. They were concerned, friendly, gave me good advice and what he actually said was true’ (p2, Female, 45–54, hear & treat, first time user, severe abdominal pain). The dissatisfied user felt that the call handler could have shown ‘a little bit more compassion’ given the upsetting nature of the situation. This perceived lack of compassion led the participant to feel as though ‘…he didn't care. It was just when I was speaking to him he wasn't sort of listening’ (P18 spouse, Female, 45–54, hear & treat, first time user, extreme pain in leg).
Being informed
Information provided by the call handler (who could advise on ambulance arrival time and what to do while waiting) and ambulance staff on arrival also offered reassurance because this reduced uncertainty in a stressful situation:
because I said what I am concerned about is I can't stop any of the blood, and they was telling me you know to pinch the end of his nose and to keep an eye on him and they were just talking me through and saying what is happening now and they were on the phone until the Rapid Response came (P19 spouse, Male, 65+, see & treat, first time user, fell, injured face)
Communication style
Reassurance was gained not only through information content but also the manner in which this was communicated. Users generally appreciated the informal style of communication which many clinicians adopted, for example using humour or first names to address them. This friendly style was seen as part of ambulance clinicians' professionalism:
Interviewer: So do you think that manner then that you mentioned, that kind of jokey manner is, is a good thing?
Participant's spouse: It's a good thing. Yeah, a good thing yes.
Participant: Yes.
Interviewer: What is it about that that you think's good?
Participant: Well they're not, they're not talking about, I mean they're not forgetting what they're here for, they are discussing what you've got, but in a pleasant way, not in a morbid way is it?
Interviewer: Okay, so it's important to kind of be nice really?
Participant: I think it puts more people at ease, you know.
(P13, Male, 65+ and spouse, see and convey, used service before, breathing difficulties)
Occasionally, there was a mismatch between user preferences and the way in which clinicians' spoke, where humour was viewed as inappropriate by some users and relatives.
… But they were like… ‘We will soon have you on your legs… you'll soon be running the marathon’ and I thought do I really need this? This is not me and I can't run a marathon, legs like this. And you're thinking, don't need this. (P21, Female, 65+, see and convey, used service before, collapsed)
Short wait for help
Users valued a quick response of an ambulance on‐scene, whether they had a life‐threatening emergency or not: ‘that was the critical bit as far as we were concerned, the fact that we had somebody here within ten minutes’ (P19 spouse, Female, 65+, see and treat, first time user, fell and injured face). Even relatively short waiting times of a few minutes could feel too long when the user was in a state of panic, and this particularly applied to users who were on their own at the time of the event:
Interviewer: Do you remember how long it took them to get to you?
Participant: I would say about 10 minutes
Interviewer: Right. Did it feel like a long time?
Participant: Well it did because of the breathing problems. I was starting to panic.
(P1, Female, 55–64, see & convey, used service before, breathing difficulties)
Most participants did not express direct concern about their waiting time for help but several described hypothetical scenarios in which a quicker response would have been desirable: ‘…it wasn't so serious this time but it could have been serious and for that reason, yes, they could have been quicker’ (P17, Male, 55–64, see & convey, used service before, chest tightness). This highlights the extent to which anxiety is central to patients' experiences and short waits can offer reassurance. However, participants were also aware of culpability – the extent to which they could apportion blame to a service for perceived poor quality care. They acknowledged the impact that traffic, distance and busy times could have on their waiting time. It was also the case that if the response time was longer than the user wanted then the clinicians' ability to provide reassurance on arrival could compensate for this: ‘I know it took them about 10 minutes to get here but they reassured me when they got here. Yeah it was alright… Well I know the traffic from the [hospital name] is chaotic. So it's…I would say it's not their fault.’ (P1, Female, 55–64, see & convey, used service before, breathing difficulties)
Continuity across the transfer points
Users often experienced handovers between health‐care staff during their contact with the ambulance service, in particular from call handler to ambulance crew and from ambulance crew to hospital staff. Participants gained reassurance from the continuous presence of health‐care staff, whether by telephone or in person, because being left alone increased their anxiety and fear. This is illustrated in the quotes below, one by a participant who appreciated the call handler staying on the telephone until the ambulance crew arrived and the other who experienced a discontinuity:
I then phoned 999 and explained the situation to the operator and he said ‘there is somebody on the way to you; I'll carry on talking to you until they arrive… Is your door unlocked?’ I went ‘no’. He went ‘run down and unlock your door’. I ran down, unlocked the door, went back again. Started talking to him again. I then heard a car pull up and I said ‘Oh I think they're here. I looked out of the window and said ‘Yeah, they're here’ and he said ‘Right I'll leave you in their capable hands now’. (P3 spouse, Male, 65+, see & treat, used service before, diabetic hypoglycaemia)
The only comment that I would probably have is probably to say for them to stay on the line a little bit longer for the ambulance man or ambulance people had actually got here, because between that time of them finishing the conversation to the ambulance team or first response team arriving it's quite scary because you're kind of like, what happens, what happens if anything else happens between that time? (P9 on behalf of child, Female, 25–34, see & treat, first time user, high temperature)
Similarly, once the ambulance had arrived at the hospital, the continued presence of a health‐care professional offered reassurance. Users also valued a handover process that involved them, that is one in which they were informed of what was going on and what would happen to them.
One of them stayed with me while I was wheeled through the hospital and she was explaining to the doctor that I'd had an operation, what medication I'd been taking and stuff like that. (P6, Male, 45–54, see & convey, first time user hernia bleed)
For ‘see and treat’ users, a sense of continuity was established through the instruction by ambulance crews that if their health deteriorated further they should call again for assistance. This was reassuring because it bridged the gap between being under the care of health professionals and being completely responsible for their own health: ‘Oh yes, I was fine, especially when he said you know, if you need [us] to come back, please call again and I'll come back to you’ (P15, Female, 65+, see & treat, first time user, side‐effects of medication).
Discussion
Summary of main findings
Users call emergency ambulance services for a range of health problems of varying severity and experience different types of response. Despite this variation, participants in this study told us that they valued a similar outcome of their pre‐hospital care – reassurance – and gained this reassurance from a similar set of processes. Users described their extreme anxiety about their health during the episode and valued being reassured that they were in safe hands and would get the care and treatment they required. Processes that helped to deliver this reassurance were: the professional behaviour and communication skills of staff, which instilled confidence; a short wait for help; and continuity during transfers of care. A timely response was typically valued not from the perspective of clinical need but in terms of allaying anxiety quickly.
Comparison with existing literature
Fear or anxiety as a driver for users seeking emergency and urgent care, and the accompanying need for reassurance, has been identified for other services such as NHS Direct (the 24 h nurse‐led triage service),14 emergency departments15 and use of emergency ambulances for primary care problems.16 The ways in which we found that reassurance was gained were similar to issues which ambulance users with specific conditions have described as important, such as communication and perceived professionalism of clinicians.9 Findings were also similar to those of a survey of ambulance users where the attitude of the call handler, simply knowing the service was available for use, and receiving confirmation that the decision to utilise the service had been the correct one were identified as important.14
There were many similarities in the experience of reassurance shared by our pre‐hospital participants and those who took part in a hospital‐based study, which asked the question ‘what does the experience of being reassured by the nurses mean to you?’.17 Fareed17 argued that the fundamental structure of reassurance included components such as: receiving information and knowledge of facts, interpersonal skills, ‘being there’ and being cared for.17 The notion of ‘being there’ included the knowledge that ‘they were accessible or available’ when needed. This was ‘enough to convey a sense of security’, rather than necessarily implying the physical presence of the person providing reassurance.17 This also applied to our study, where participants talked about the value placed on maintaining telephone contact with call handlers prior to the arrival of a crew. Fareed17 also describes the relationship between information provision and elimination of fear, which we also found. Obtaining accurate information about their health‐care condition, likely treatment and on‐going care helped to give the users a sense of control and reduced the uncertainty they were experiencing.9
Strengths and limitations
Qualitative studies that have explored users' experiences of emergency ambulance services have focused either on specific conditions, for example stroke and heart attack,9 specific aspects of care, such as pain management,8 or specific parts of the pathway, including the first point of contact with clinicians on‐scene.18 A strength of this study was that the views of users with a wide range of conditions and injuries and a wide range of responses from the emergency ambulance service, that is hear and treat, see and treat, see and convey, were included. The inclusion of spouses' experiences provided additional insight and enhanced our understanding of the overall picture of what is valued within the pre‐hospital care experience. A further strength was the varied backgrounds of the researchers, bringing perspectives to the analysis from backgrounds in psychology (FT), social policy (VHP), health services research (AOC, JT, ANS) and clinical practice (ANS).
There were several limitations. Firstly, we sampled from one ambulance service in the UK only. However, this service covers a wide geographical area of varied population. Secondly, although our sample was diverse, we explicitly excluded users from some vulnerable groups and users that were unable to conduct the interview in English. In addition, 24 of the 30 participants were aged over 55 years, so the views of younger participants were less well represented. The views of these groups may have been different to those that participated in our study. Furthermore, although the inclusion of spouses was identified above as strength, it could also be considered a limitation in terms of the influence and impact of their views and experiences on the patient's recollection of their pre‐hospital experience. Future research should focus on obtaining the views of groups not included here because they require specific recruitment approaches sensitive to their needs. Thirdly, only a small proportion of people we approached agreed to be interviewed, and there may have been selection bias in our sample, for example those with particularly good or poor experiences may have been more likely to respond. Finally, more research is needed to determine the generalizability of our findings that the aspects of care most valued by users were not specific to the type of ambulance service response that they received. Ideally, the views of ‘hear and treat’ and ‘see and treat’ patients should be explored in greater depth.
Implications for practice and future research
Reassurance was an outcome valued by users of the emergency ambulance service. Our findings demonstrate that a high standard of clinical care, although important, may not be sufficient for a good patient experience. The implication of this for the future measurement of the performance of pre‐hospital care is that the proportion of users reporting feeling reassured by the ambulance service response should be measured alongside current measures such as response times and clinical performance indicators. These findings could be used to inform the development of a standardised measure of patient experience for ambulance services.
Conclusion
The ability of the emergency ambulance service to allay the high levels of fear and anxiety felt by users is crucial to the delivery of a high quality service. Measures developed to assess and monitor the performance of emergency ambulance services should include the proportion of users reporting feeling reassured by the response they obtained.
Funding
The study formed part of the Prehospital Outcomes for Evidence Based Evaluation (Phoebe) programme that is independent research funded by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research (PGfAR) scheme (Grant Reference Number RP‐PG‐0609‐10195). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We thank the patients and relatives who contributed to the interviews and Mrs. Stacey Knowles for her assistance with the recruitment process.
References
- 1. Pickering A, Mason S, Turner J, Bradley P, Irving S. A Comparative Review of Ambulance Service Best Practice. London: Office of the Strategic Health Authorities, 2009. [Google Scholar]
- 2. Pell JP, Sirel JM, Marsden AK, Ford I, Cobbe SM. Effect of reducing ambulance response times on deaths from out of hospital cardiac arrest: cohort study. British Medical Journal, 2001; 322: 1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Turner J, Nicholl J, O'Keeffe C, Dixon S. The Costs and Benefits of Implementing the new Ambulance Service Response Time Standards. Final report to the Department of Health. Sheffield: Medical Care Research Unit, University of Sheffield, 2006. [Google Scholar]
- 4. Darzi A. High Quality Care for all: NHS Next Stage Review Final Report. London: Stationery Office, 2008. [Google Scholar]
- 5. O'Cathain A, Turner J, Nicholl J. The acceptability of an emergency medical dispatch system to people who call 999 to request an ambulance. Emergency Medicine Journal, 2002; 19: 160–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. O'Cathain A, Turner J, Withers A, Nicholl J. Views of people who call 999 to request an ambulance. Pre‐Hospital Immediate Care, 1999; 3: 131–135. [Google Scholar]
- 7. Turner J, Snooks H, Youren A et al The Costs and Benefits of Managing Some Low Priority 999 Ambulance Calls by NHS Direct Nurse Advisers. Final Report to the NHS Executive Service Delivery and Organisation R&D Programme. Sheffield: Medical Care Research Unit, University of Sheffield, 2006. [Google Scholar]
- 8. Iqbal M, Spaight PA, Siriwardena AN. Patients' and emergency clinicians' perceptions of improving pre‐hospital pain management: a qualitative study. Emergency Medicine Journal, 2013; 30: e18. [DOI] [PubMed] [Google Scholar]
- 9. Togher FJ, Davy Z, Siriwardena AN. Patients' and ambulance service clinicians' experiences of prehospital care for acute myocardial infarction and stroke: a qualitative study. Emergency Medicine Journal, 2013; 30: 942–948. [DOI] [PubMed] [Google Scholar]
- 10. http://www.shef.ac.uk/scharr/sections/hsr/mcru/phoebe
- 11. Guest G, Bruce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods, 2006; 18: 59–82. [Google Scholar]
- 12. Flanagan JC. The critical incident technique. Psychological Bulletin, 1954; 4: 51. [DOI] [PubMed] [Google Scholar]
- 13. Ritchie J, Spencer L. Qualitative data analysis for applied policy research In: Bryman A, Burgess RG. (eds) Analyzing Qualitative Data. London and New York: Routledge, 1994: 172–194. [Google Scholar]
- 14. O'Cathain A, Munro J, Nicholl J, Knowles E. How helpful is NHS Direct? Postal survey of callers. British Medical Journal, 2000; 320: 1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Agarwal S, Banerjee J, Baker R, Conroy S, Hsu R, Rashid A, et al Potentially avoidable emergency department attendance: interview study of patients' reasons for attendance. Emergency Medicine Journal, 2012; 29: e3. [DOI] [PubMed] [Google Scholar]
- 16. Booker MJ, Simmonds RL, Purdy S. Patients who call emergency ambulances for primary care problems: a qualitative study of the decision‐making process. Emergency Medicine Journal, 2014; 31: 448–452. [DOI] [PubMed] [Google Scholar]
- 17. Fareed A. The experience of reassurance: patients' perspectives. Journal of Advanced Nursing, 1996; 23: 272–279. [DOI] [PubMed] [Google Scholar]
- 18. Elmqvist C, Fridlund B, Ekebergh M. More than medical treatment: the patient's first encounter with prehospital emergency care. International Emergency Nursing, 2008; 16: 185–192. [DOI] [PubMed] [Google Scholar]


