Abstract
Objectives
The primary objective was to determine if the pain and function response to the McKenzie system of Mechanical Diagnosis and Therapy (MDT) differs by MDT classification category at two and four weeks following the start of MDT treatment for shoulder complaints. The secondary objective was to describe the frequency of discharge over time by MDT classification.
Methods
International, MDT-trained study collaborators recruited 93 patients attending physiotherapy for rehabilitation of a shoulder problem. The Numeric Pain Rating Scale (NPRS) and the Upper Extremity Functional Index (UEFI) were collected at the initial assessment and two and four weeks after treatment commenced. A two-way mixed model analysis of variance with planned pairwise comparisons was performed to identify where the differences between MDT classification groups actually existed.
Results
The Derangement and Spinal classifications had significantly lower NPRS scores than the Dysfunction group at week 2 and week 4 (p < 0.05). The Derangement and Spinal classifications had significantly higher UEFI scores than the Dysfunction group at week 2 and week 4 (p < 0.05). The frequency of discharge at week 2 was 37% for both Derangement and Spinal classifications, with no discharges for the Dysfunction classification at this time point. The frequency of discharge at week 4 was 83, 82 and 15% for the Derangement, Spinal and Dysfunction classifications, respectively.
Discussion
Classifying patients with shoulder pain using the MDT system can impact treatment outcomes and the frequency of discharge. When MDT-trained clinicians are allowed to match the intervention to a specific MDT classification, the outcome is aligned with the response expectation of the classification.
Level of Evidence: 2b
Keywords: McKenzie, Mechanical Diagnosis and Therapy (MDT), shoulder
Introduction
Shoulder pain is a common problem in the general population with reported rates ranging from 100 to 160 per 1000 patients [1]. Once present, shoulder symptoms have proven to be persistent and recurrent, with 50% still unresolved after 18 months [2]. It is thus not surprising that shoulder pain is one of the leading causes of referrals to physiotherapy [1]. The complexity of the shoulder joint, poor accuracy of shoulder clinical tests [3−6] and the lack of uniformity of diagnostic labeling [7] make a precise diagnosis difficult to achieve. Without a precise diagnosis, treatment is likely to be more arbitrary than targeted which may contribute to the lack of efficacy for most interventions [8]. This difficulty for clinicians is compounded by the knowledge that many pathological findings revealed on diagnostic tests such as MRI, x-rays, or ultrasound are asymptomatic [9–13] and so cannot be relied upon to make informed clinical decisions as to the source of the pain.
The issue of uniformity and accuracy of diagnosis and treatment is an important concern to address. These confounding factors have led to the call for and proposal of alternative methods of assessment and classification [7,14,15]. Though some alternative classification systems have been developed, their widespread use and acceptance among practitioners has proven to be challenging. This may be due to their relatively recent introduction and a dearth of research exploring their validity. If such a system was successfully embraced it would reduce the variation in clinical practice amongst clinicians, and potentially lead to an enhanced effect of treatment [16,17].
The McKenzie system of Mechanical Diagnosis and Therapy (MDT) is one alternative approach to the assessment, classification and treatment of musculoskeletal disorders. The MDT system was initially described in 1981 with the introduction of a new approach to the classification and management of back pain [18]. It uses non-pathology specific classifications that are based on a detailed history and a physical examination exploring the effects of repeated movements, positions and loading strategies on symptoms and motion [19]. Each classification is matched to a different management approach [19].
A series of systematic reviews support application of the MDT system in the management of acute and chronic low back pain [20–27]. McKenzie’s original description [18] indicated that MDT could also be applied to extremity problems, the application of which is outlined in his book on the human extremities [28]. According to McKenzie, extremity problems can be classified into the following syndromes and ‘Other’ subgroups: [28]
-
•
Derangement, identified by the presence of a directional preference which will give a lasting positive change in symptoms, in range of movement and in function;
-
•
Articular Dysfunction, identified by intermittent pain consistently produced at a restricted end range with no rapid change of symptoms or range;
-
•
Contractile Dysfunction, identified by intermittent pain, consistently produced by loading the musculo-tendinous unit, for instance, with an isometric contraction against resistance;
-
•
Postural syndrome is only produced by sustained loading – the rest of the physical examination would be normal;
-
•
‘Other’ subgroups are considered when none of the above syndrome patterns are present. Each has a definition and criteria that together complete the classification for all remaining presentations. Examples include Inflammatory, Trauma and Chronic Pain Syndrome (Appendix 1).
Despite the number of studies on the utility of the MDT system for spinal pain [20–32], there is limited scientific literature about its application with extremity musculoskeletal disorders. For shoulder disorders, only three case studies [33–35], and one case series [36] have been published. The prevalence of MDT syndromes in the extremities has been investigated in a number of separate surveys [37,38 and in a more recently conducted survey by May and Rosedale [15]. The latter showed that more than one third of patients with extremity disorders were classified as Derangements. The authors suggested that if further research shows the rapid treatment response of this subcategory in the extremities, as it is proven to be in the spine, this would have a significant impact on the future treatment of a major group of patients with extremity disorders. Our previous study revealed substantial inter-rater agreement (Kappa = 0.90) between MDT-trained experts when classifying McKenzie upper extremity syndromes in vignettes of patients with shoulder disorders [39]. Therefore, the next logical step would be to investigate the application of the MDT system in patients with shoulder problems.
The primary objective of this study was to determine if the response of pain and function to MDT treatment differs by classification category at two and four weeks following the start of physiotherapy treatment. The secondary objective was to describe the frequency of discharge over time by MDT classification category.
We hypothesized that patients with Derangement classification would be discharged earlier, and there would be a statistically significant treatment response in pain reduction, and improved function compared to patients with shoulder Dysfunction at two weeks and four weeks from their admission.
Methodology
Study design and setting
This study utilized a prospective longitudinal design. An international group of 15 licensed physiotherapists recruited and collected data from consecutive eligible patients attending their clinic for rehabilitation of a shoulder problem. These study collaborators were McKenzie Institute International diploma or credential holders who had greater than one year of experience in using the MDT system with patients who complained of upper extremity problems.
Instructions, consent forms, and data collection sheets (Appendices 2–4) were distributed to all the study collaborators. In order to minimize bias, the collaborators had no awareness of the study objectives and hypotheses. Completed data sheets were sent to the primary investigators and stored in a password protected database. Patients’ baseline demographic and historical variables were recorded including age, sex, hand dominance, physical demands of job/daily activities, previous episodes and duration of symptoms. Ethics approval for the study was obtained from the Health Sciences Research Ethics Board of Western University. Clinical data from a total of 105 patients were collected from March 2013 to November 2014. Sample size was estimated to ensure a reasonable number of cases across subcategories.
Participants
To be included in the study, patients were required to be over the age of 18, English speaking, and have shoulder pain for which they were seeking physiotherapy intervention. No specific shoulder diagnosis was required for inclusion. Patients were excluded if they had a surgical procedure on their shoulder within six months prior to the start of physical therapy treatment. No specific shoulder diagnoses were excluded as the intent was to classify all patients presenting with shoulder pain using the MDT system.
Examination and classification
Patients were assessed and treated using the MDT method and principles. A ‘treatment-as-usual’ approach was followed. A standard MDT evaluation method was used for all participants, and the patients’ diagnoses were classified according to the MDT system utilized in the extremities. The patients were classified to one of the five following subgroups: Derangement, Articular Dysfunction, Contractile Dysfunction, Other and Spinal; the latter was included as patients referred with ‘shoulder pain’ could eventually be diagnosed as a condition originating from the cervical spine. Spinal classification is believed to be a cervical spine Derangement and is anticipated to respond to treatment in a similar manner as shoulder Derangement. Other refers to the patients who did not meet the definition for any one of the above-mentioned classifications.
Intervention
Treatment ensued based on accepted procedures for each classification, and patients were treated with individually matched exercises and the appropriate progression of forces following the MDT method [28]. The detailed intervention and progression of forces were left to the discretion of the treating practitioners. There would have been multiple individually tailored exercise programs based on each patient’s specific classification and response to repeated movements; the patient classified as having a shoulder Derangement with a directional preference for extension for example, would have been given repeated end range extension exercises by the clinician. They would have been advised to perform these exercises regularly, every one to three hours, in sets of 10–15 repetitions. They may also have been advised to temporarily avoid certain exacerbating movements and positions. If the patient improved, the intervention would remain unchanged; however, if progress plateaued then the patient may be guided to apply more force, as long as more force demonstrated a positive effect. Once resolution was well underway the patient would be encouraged to resume all movements with confidence, but integrate the directional preference movements into their daily routine. Those patients classified as having an Articular Dysfunction would have been given repeated end range exercises in the direction of the painful and limited movement, approximately 10 repetitions every two to three hours. This would be performed until the movement became full and pain-free and the patient felt confident to move freely in all directions. Those with Contractile Dysfunctions would have been treated with a progressive resisted exercise regime in the direction of the painful movement until the movement became painfree with resistance and full activity restored.
Other MDT subgroups would have been managed depending on the particular subgroup. For example, a patient with Chronic Pain Syndrome would be managed with pain education, graded exposure activity and the addressing of psychosocial barriers to recovery. If the shoulder pain was classified as Spinal i.e. from a Cervical Derangement, the patient would have been advised to perform repeated end range exercises in the directional preference with the same details as outlined above for shoulder Derangements.
The patients were followed up until their discharge from physiotherapy, or after 4 weeks, or 8 treatment sessions, whichever came first. The patients’ clinical information was collected at the initial assessment, and the treatment effects were evaluated at primary and secondary target points. The primary target point was the fifth treatment session, or two weeks since the start of treatment, or discharge from physiotherapy treatment, whichever came first. The secondary target point was the eighth treatment session, or four weeks since the start of treatment, or discharge from physiotherapy treatment, whichever came first.
Outcomes
Patients were monitored for change in the primary outcome measures used for the study [the Upper Extremity Functional Index (UEFI) [40], and the Numeric Pain Rating Scale (NPRS) [41]. The UEFI is a patient-reported outcome measure consisting of 20 items that capture a variety of upper extremity activities. Its purpose is to examine patients’ current upper extremity functional status [40]. Scores can vary from 0 to 80, with higher scores indicating less functional limitation [40] It has been shown to have excellent test-retest reliability (Intraclass Correlation Coefficient = 0.85–0.95), and internal consistency (Coefficent alpha) of 0.94 [40,42] The minimal level of detectable change (MDC) is 9 points [40], with a minimal clinically important difference (MCID) of 9–10 points [42].
The NPRS is an 11-point scale with scores that can vary from 0 (no pain) to 10 (the worst possible pain) [41]. It has been shown to have adequate test-retest reliability (r = 0.63–0.92) and excellent internal consistency (Coefficient alpha = 0.84–0.98) [43]. The MDC for the NPRS has been reported to be 2.5–3 in patients with shoulder and upper extremity disorders [44,45], with a MCID of 2.17 reported in both surgical and non-surgical patients with shoulder problems after 3–4 weeks of rehabilitation [46].
Data on the primary outcomes were included in the analysis when they were available for at least two out of three data collection points. In case a patient was discharged before their third data collection point, the Last Observation Carried Forward (LOCF) imputation method was utilized to fill in the missing score for the third data collection point. The secondary outcome was the rate of discharge for each one of the MDT classifications at both study target points.
Data analysis
Descriptive statistics were calculated for the MDT classifications, patient characteristics and the two primary outcome variables at baseline. The comparison for the primary outcomes of pain and function was performed among the three major classifications of Spinal, Derangement, and Dysfunction. As there were fewer patients in Articular and Contractile Dysfunction classifications, the two subcategories were merged to make up a general classification of Dysfunction in order to have a more balanced sample size in comparison to the Derangement and Spinal classifications. Both Articular and Contractile Dysfunction are believed to demonstrate similar responses to treatment over time.
Depending on whether the compared variable was continuous or categorical, one-way analysis of variance (ANOVA) or Chi square analysis was conducted to compare the following baseline characteristics and potential confounding variables among the MDT subcategories: NPRS and UEFI scores at baseline, age, sex, hand dominancy of the affected shoulder, and duration of symptoms, history of previous episodes of same condition, medication use, concurrent physiotherapy treatments received, and physical demand of work/daily activities.
For the primary objective, a two-way mixed model ANOVA was conducted for the primary outcomes of pain (measured by the NPRS) and function (measured by the UEFI) to compare the interaction between MDT classifications (Spinal, Derangement, and Dysfunction) and time (baseline, week 2, and week 4). When the sphericity assumption was not met by our data, a Greenhouse-Geisser correction was used. In the presence of a significant interaction between MDT classifications and time, one-way ANOVA and planned pairwise comparisons were performed for each time point (baseline, week 2, and week 4) to further investigate where the differences between the MDT classifications actually existed. For the secondary objective frequency of discharge by MDT classification and time was reported in percent. The SPSS version 20 (SPSS Inc, Chicago, IL) was used for all data analyses.
Results
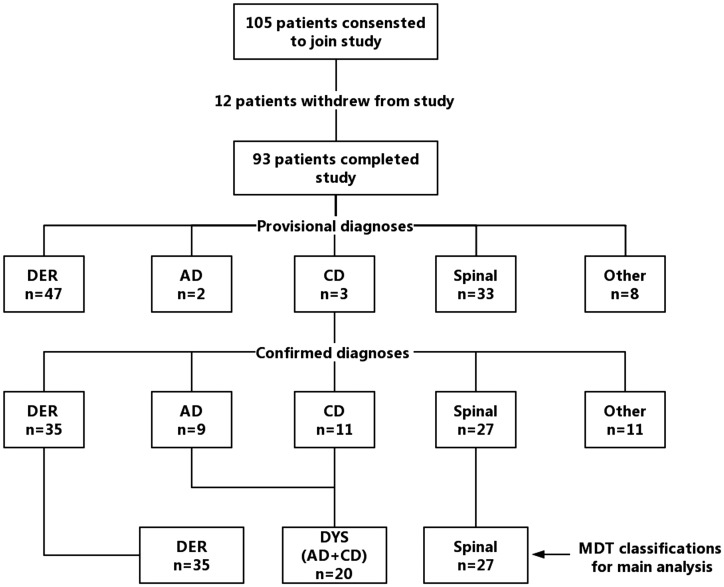
Between March 2013 and November 2014, 105 patients consented to participate in the study and were recruited. The flow of patient recruitment and MDT classifications is shown in Figure 1. Of the 105 patients recruited for the study, 12 patients subsequently dropped out after their initial visits, for the following reasons: shoulder manipulation performed by orthopedic surgeon (n = 1); treatment sought in another clinic closer to home (n = 1); change in insurance coverage prompted treatment by another physiotherapy clinic (n = 1); treating practitioner took emergency leave of absence (n = 2); travel out-of-town for extended period of time (n = 3); failure to return for follow up treatment after initial visit (n = 4).
Figure 1.
Flow of patients and MDT classifications.
Abbreviations: AD, Articular Dysfunction; CD, Contractile Dysfunction; DER, Derangement; DYD, Dysfunction; MDT, Mechanical Diagnosis and Therapy.
Of the 93 patients who completed the study, 11 patients had either a concurrent condition of two MDT classifications, or were classified under the Other MDT subgroup. These patients were excluded, leaving 82 patients for the main analyses. In 63.4% of the cases, the provisional diagnoses remained unchanged over the course of treatment. The distribution of MDT classifications is shown in Table 1.
Table 1.
Distribution of the MDT classifications at baseline.
| MDT classification | Frequency | Percent | May and Rosedale [28] (%) |
|
|---|---|---|---|---|
| DER | 35 | 37.6 | 42.5 | |
| AD | 9 | 9.7 | 10.8 | |
| CD | 11 | 11.8 | 11.7 | |
| Spinal | 27 | 29.0 | Other | 35.0 |
| DER with residual AD | 2 | 2.2 | ||
| DER with residual CD | 1 | 1.1 | ||
| Spinal with residual AD | 2 | 2.2 | ||
| Spinal with DER | 1 | 1.1 | ||
| Spinal with residual CD | 1 | 1.1 | ||
| Other | 4 | 4.3 | ||
| Total | 93 | 100.0 | ||
Abbreviations: AD, Articular Dysfunction; CD, Contractile Dysfunction; DER, Derangement; MDT, Mechanical Diagnosis and Therapy.
There was no significant difference (p > 0.05) among the three MDT classifications at baseline for NPRS and UEFI scores, and other baseline characteristics (Table 2). Only two patients in the Derangement group received concurrent treatments (a cold pack) along with their MDT-directed treatments. The remaining patients received solely the MDT-directed treatments, therefore, no comparison was conducted among the MDT classifications for this variable.
Table 2.
Patient characteristics and primary outcome scores at baseline.
| Variable |
MDT classifications |
P-value | |||
|---|---|---|---|---|---|
| Derangement (n = 35) | Dysfunction (n = 20) | Spinal (n = 27) | |||
| Age, mean (SD) | 47.1 (15.1) | 54.1 (15.8) | 50.0 (18.1) | 0.32* | |
| Sex, n (% female) | 13 (37.1) | 8 (40.0) | 16 (59.3) | 0.19* | |
| NPRS, mean (SD) | 5.4 (1.9) | 4.7 (2.1) | 5.7 (1.6) | 0.15* | |
| UEFI, mean (SD) | 56.0 (15.1) | 54.2 (16.0) | 52.3 (16.3) | 0.66* | |
| Hand Dominancy, n (% dominant) | 25 (71.4) | 13(65.0) | 18 (66.7) | 0.86* | |
| Previous episodes, n (% yes) | 14 (40.0) | 8 (40.0) | 14 (51.9) | 0.60* | |
| Medication use, n (% yes) | 15 (42.9) | 6 (30.0) | 10 (37.0) | 0.64* | |
| Duration of symptoms | ≤12 weeks | 21 (60.0) | 7 (35.0) | 17 (63.0) | 0.12* |
| >12 weeks | 14 (40.0) | 13 (65.0) | 10 (37.0) | ||
| Physical activities | Sedentary-light | 20 (57.1) | 11 (55.0) | 19 (70.4) | 0.47* |
| Medium-heavy | 15 (42.9) | 9 (45.0) | 8 (29.6) | ||
Abbreviations: MDT, Mechanical Diagnosis and Therapy; NPRS, Numeric Pain Rating Scale; UEFI, Upper Extremity Functional Index; SD, standard deviation.
not significant.
Main analysis
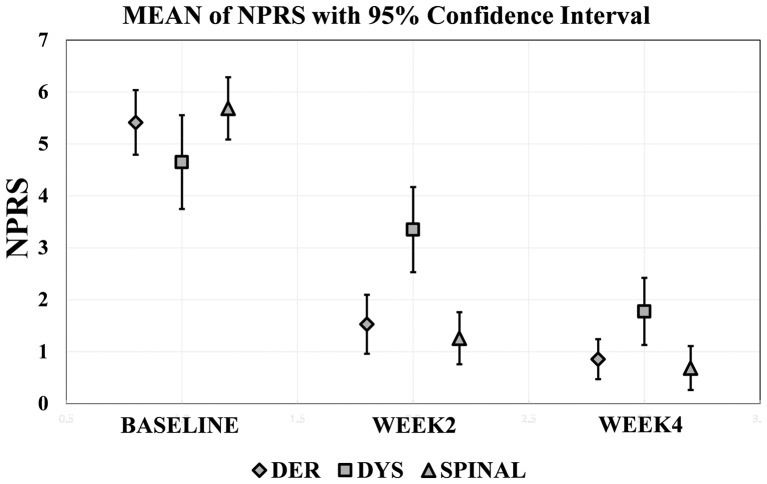
For the NPRS outcome measure, a significant interaction effect was present between our between-group variable of MDT classifications, and the within-group variable of time [Greenhouse-Geisser corrected F(3.2–126.1) = 1057, p < 0.001]. This indicates that although the NPRS scores were significantly affected by the factor of time [Greenhouse-Geisser corrected F(1.6–126.1) = 239.63, p < 0.001], the effect of time was different among the MDT classifications. There was no statistically significant difference in NPRS scores at baseline among the MDT classifications [F(2–79) = 2.81, p = 0.15]; however, a statistically significant difference was present among the MDT classifications in their NPRS values at primary [F(2–79) = 10.81, p < 0.001] and secondary [F(2–79) = 5.7, p = 0.008] study target points (Table 3). The Derangement classification had significantly lower NPRS scores than the Dysfunction group indicating pain reduction at week 2 (p = 0.001) and week 4 (p = 0.02). The Spinal classification also had significantly lower NPRS scores in comparison to the Dysfunction group at week 2 (p < 0.001) and week 4 (p = 0.009). Derangement and Spinal classifications had no statistically significant difference in their NPRS scores at week 2 (p = 0.488) and week 4 (p = 0.557) (Table 4). The NPRS mean scores with 95% confidence intervals for each of the MDT classifications are shown in Figure 2 as a function of time. Seventy-two percent (59 out of 82) of participants had their data collected for all the three data collection points. For the remaining 27% who were discharged prior to their third data collection point, LOCF was utilized to fill in the missing data.
Table 3.
Baseline and follow-up primary outcome scores and results of analysis comparing MDT classifications.
| Assessment time/variable | MDT classifications |
p-value | ||
|---|---|---|---|---|
| Derangement (n = 35) | Dysfunction (n = 20) | Spinal (n = 27) | ||
| Baseline | ||||
| NPRS, mean (SD) | 5.4 (1.9) | 4.7 (2.1) | 5.7 (1.6) | 0.15* |
| UEFI, mean (SD) | 56.0 (15.1) | 54.2 (16.0) | 52.3 (16.3) | 0.66* |
| Week 2 | ||||
| NPRS, mean (SD) | 1.53 (1.71) | 3.35 (1.87) | 1.26 (1.32) | <0.001 |
| UEFI, mean (SD) | 72.89 (7.40) | 59.30 (14.85) | 72.81 (5.76) | <0.001 |
| Week 4 | ||||
| NPRS, mean (SD) | 0.86 (1.16) | 1.77 (1.47) | 0.68 (1.12) | 0.008 |
| UEFI, mean (SD) | 75.68 (5.47) | 65.45 (16.07) | 76.40 (4.18) | <0.001 |
Abbreviations: MDT, Mechanical Diagnosis and Therapy; NPRS, Numeric Pain Rating Scale; UEFI, Upper Extremity Functional Index; SD, standard deviation.
not significant.
Table 4.
Contrasts between pairs of MDT classifications for main outcomes at primary and secondary study target points.
| Contrasts | Value of contrast (SE) |
P-value |
||
|---|---|---|---|---|
| Week 2 | Week 4 | Week 2 | Week 4 | |
| NPRS | ||||
| DER vs. DYS | −1.82 (0.51) | −0.92 (0.38) | 0.001 | 0.02 |
| DER vs. Spinal | 0.27 (0.39) | 0.17 (0.29) | 0.49* | 0.56* |
| DYS vs. Spinal | 2.09 (0.49) | 1.09 (0.39) | <0.001 | 0.009 |
| UEFI | ||||
| DER vs. DYS | 13.58 (3.55) | 10.24 (3.71) | 0.001 | 0.01 |
| DER vs. Spinal | 0.07 (1.67) | −0.72 (1.22) | 0.97* | 0.56* |
| DYS vs. Spinal | −13.51 (3.50) | −10.96 (3.68) | 0.001 | 0.007 |
Abbreviations: DER, Derangement; DYS, Dysfunction; MDT, Mechanical Diagnosis and Therapy; NPRS, Numeric Pain Rating Scale; NS, not significant; UEFI, Upper Extremity Functional Index; SD, standard deviation.
not significant.
Figure 2.
Mean NPRS score from baseline to discharge in each MDT classification.
Abbreviations: DER, Derangement; DYS, Dysfunction; MDT, Mechanical Diagnosis and Therapy; NPRS, Numeric Pain Rating Scale.
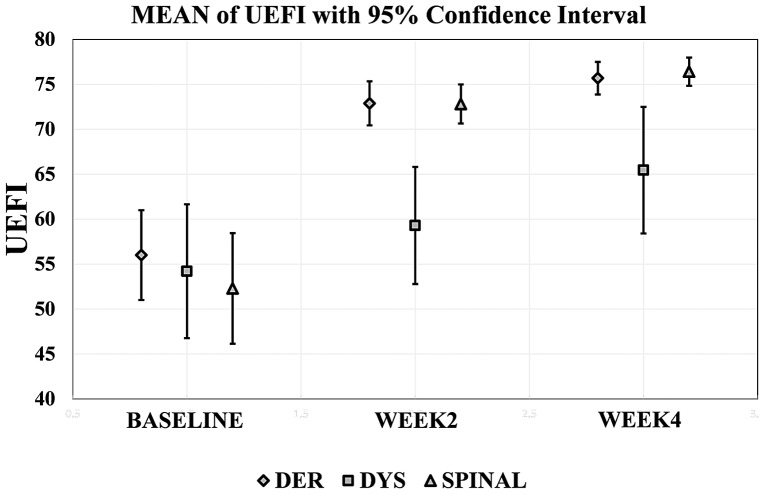
For the UEFI outcome measure, a significant interaction effect was present between our between-group variable of MDT classifications and the within-group variable of time [Greenhouse-Geisser corrected F(2.31–91.08) = 7.08, p = 0.001]. This indicates that although the UEFI scores were affected by the factor of time [Greenhouse-Geisser corrected F(1.15–91.08) = 122.99, p < 0.001], the effect of time was different among the MDT classifications. There was no statistically significant difference in UEFI scores at baseline among the MDT classifications [F(2–79) = 0.441, p = 0.664]; however, a statistically significant difference was present among the MDT classifications in their UEFI values at primary [F(2–79) = 15.87, p < 0.001] and secondary [F(2–79) = 10.47, p < 0.001] study target points (Table 3). The Derangement classification had significantly higher UEFI scores than the Dysfunction group indicating improvement in their function at week 2 (p = 0.001) and week 4 (p = 0.01). The Spinal classification also had significantly higher UEFI scores in comparison to the Dysfunction group at week 2 (p < 0.001) and week 4 (p = 0.007). Derangement and Spinal classifications had no statistically significant difference in their UEFI scores at week 2 (p = 0.966) and week 4 (p = 0.558) (Table 4). The UEFI mean scores with 95% confidence intervals for each of the MDT classifications are shown in Figure 3 as a function of time.
Figure 3.
Mean UEFI score from baseline to discharge in each MDT classification.
Abbreviations: DER, Derangement; DYS, Dysfunction; MDT, Mechanical Diagnosis and Therapy; UEFI, Upper Extremity Functional Index.
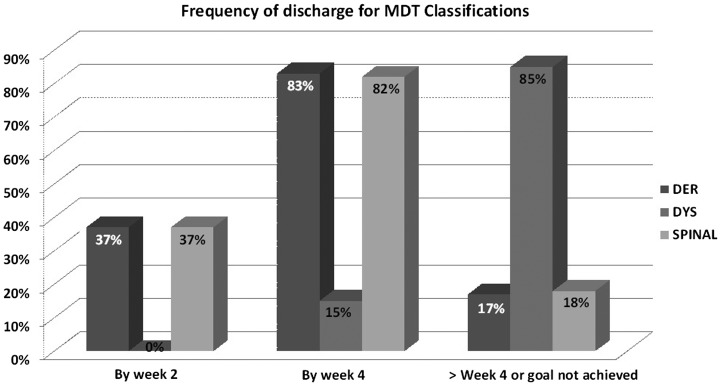
The frequency of discharge at the first target point was 37% for both Derangement and Spinal classifications, and there was no discharge for Dysfunction classification at this target point. The frequency of discharge at the second target point was 83 and 82% for Derangement and Spinal classifications, respectively, and 15% for Dysfunction classification (Figure 4).
Figure 4.
Frequency of discharge for MDT classifications at primary and secondary target points.
Abbreviations: DER, Derangement; DYS, Dysfunction; MDT, Mechanical Diagnosis and Therapy.
Discussion
To the best of our knowledge, this is the first study to address the clinical application of the MDT system in patients with shoulder disorders. Over time, patients in the Derangement and Spinal groups demonstrated very similar pain and function responses to treatment and showed significantly greater improvement in comparison to patients with Dysfunction. These treatment responses existed at both the primary and secondary study target time points of week 2 and 4, respectively. Consistent with this, compared to patients in the Dysfunction group, a high percentage of patients with Derangement and Spinal classifications achieved their treatment goals relatively quickly and were discharged from treatment at weeks 2 and 4. This highlights the point that the Spinal extremity classification is in fact a cervical spine Derangement and like the shoulder Derangement, classification is anticipated to demonstrate a rapid treatment response.
Therefore, it appears in this non-randomized cohort that when MDT-trained clinicians are allowed to match the intervention to a specific MDT classification, the outcome is aligned with the response expectation of the classification. Hence, shoulder Derangement or shoulder pain that has a cervical Derangement will respond and resolve rapidly. Dysfunctions will respond, but in a more graduated manner, achieving discharge status at a later point.
As shown in Table 1, distribution of the MDT classifications in our patient population was comparable to those reported by May and Rosedale [15]. They did not look at Cervical Derangement as a separate classification for patients with shoulder disorders, however it is interesting to note that only 2% of the total upper and lower extremity patients were classified with spinal problems in their survey. This contrasts dramatically with the 29% of shoulder pain patients diagnosed with Cervical Derangements in this cohort. It is possible that this reflects an increase in the recognition of Cervical Derangements as a source of shoulder pain by MDT clinicians or that the study clinicians surveyed by May and Rosedale effectively screened out the cervical spine in most of their extremity patients.
There were several limitations to this study. First, due to the use of a ‘treatment-as-usual’ approach, it was not possible to have a pre-specified number of treatment sessions for each one of our study participants. As a result, it is possible that the patients in each category received a different number of treatment sessions, ultimately affecting treatment outcome. However, our treating clinicians had no awareness of the study objectives, suggesting they had little motivation to affect the outcome of each classification category other than to treat the patient as best as they could, given the clinical findings and MDT classification category. Secondly, exercise compliance was not investigated; therefore, it is uncertain whether the poorer results of the Dysfunction patients resulted from poor exercise compliance or the actual nature of the MDT classification. Third, there was no treatment group assigned to a control condition or conventional physiotherapy intervention removing the ability to compare MDT classification with other treatment approaches. Fourth, a greater proportion of patients included in this study had a pain duration of less than 12 weeks (Table 2). Therefore it may be that most of these patients would have recovered without any intervention. Fifth, there was also no randomization because the MDT method was selected as the only method of intervention and the patients were required to be treated within their respective MDT classification groups. Finally, the treating physiotherapists were MDT-trained practitioners and the treatment results may not be generalizable to other physiotherapists. As a next step, randomized controlled trials are needed to compare the MDT system with conventional treatment for patients with shoulder disorders.
Considering the well-described limitations of conventional patho-anatomic models for diagnosis and treatment of patients with shoulder complaints [3–6,10], the MDT system, may be worthy of further investigation to fill the current gap in diagnosis and management of patients with extremity problems. The encouraging aspect of the study results is that two-thirds of our study participants (66.6%) were classified as either a shoulder Derangement or a cervical Spinal Derangement. If further studies confirm that patients classified as Derangements conform to their expected rapid response to tailored MDT treatments, there is potential to significantly impact quality of life and health care utilization for a majority of patients with shoulder problems.
Notes on contributors
Afshin Heidar Abady completed his Bachelor of Science and Master of Science programs in physiotherapy with Iran University of Medical Sciences, Tehran, Iran. He is currently pursuing his PhD program in Health and Rehabilitation Sciences at Western University in London, Canada. He is simultaneously pursuing his transitional Doctor of Physical Therapy (t-DPT) program through Andrews University in Michigan, USA. He is certified in McKenzie system of Mechanical Diagnosis and Therapy (MDT) through The McKenzie Institute Canada. He is licensed to practice physiotherapy through the college of physiotherapists of Ontario, Canada.
Richard Rosedale graduated from Guy’s Hospital School of Physiotherapy in 1992 and soon after immigrated to Canada to start work at London Health Sciences Centre. He has over 20 years of experience in orthopaedics and occupational health. After obtaining his Diploma in Mechanical Diagnosis and Therapy in 1997 he became faculty of the McKenzie Institute in 2003 and is currently an international instructor. He is an MDT Diploma examiner and member of the McKenzie Institute’s International Education Committee. He has authored and co-authored numerous publications exploring MDT, including an RCT of MDT for patients with knee OA.
Bert M Chesworth is an associate professor at Western University. He does musculoskeletal rehabilitation research and supervises graduate students in the School of Physical Therapy. He teaches a course in the Graduate Program in Health and Rehabilitation Sciences and is the Director of the School of Physical Therapy.
Michael A Rotondi is an associate professor of Biostatistics at York University. In addition to his methodological work in inter-observer agreement studies and cluster randomized trials, he is an active collaborative health researcher. Current major projects include: Leading a study to develop new statistical methods that will enable examination of risk factors for chronic health conditions in the urban Aboriginal community in Canada; and Co-leading a randomized trial to investigate the effectiveness of an iPhone-based diabetes monitoring system for improving glycemic control in teenagers with type I diabetes.
Tom J Overend is an associate professor at Western University. He does research and supervises graduate students in the School of Physical Therapy. Overend teaches a course in the School of Health Studies and looks after the PT Field Seminar in the Health and Rehabilitation Sciences graduate program. He is also the acting chair of the Health and Rehabilitation Sciences graduate program for 2016–17. He was a Director of the School of Physical Therapy from 2009–2014.
Supplemental data
Supplemental data for this article can be accessed at https://doi.org/10.1080/10669817.2017.1313929.
Disclosure statement
No potential conflict of interest was reported by the authors.
Supplementary Material
Acknowledgements
We thank the following MDT trained physiotherapists for volunteering as study collaborators for this study: Susan Bamberger, Dip. MDT; Jane Borgehammar, Dip. MDT; Chris Chase, Dip. MDT; Jonathan Doulton, Dip. MDT; Anja Franz, Dip. MDT; Keith Fernandes, Cert. MDT; Kim Greene, Dip. MDT; Josh Kidd, Dip. MDT; Melissa Kolski, Dip. MDT; Audrey Long, Dip. MDT; Joe Maccio, Dip. MDT; Brian McClenahan, Dip. MDT; John Salituri, Cert. MDT; Allan Sawyer, Cert. MDT; Allicia Wilson, Cert. MDT.
References
- [1].Winters JC, Sobel JS, van der Windt DAWM, et al. NHG Standaard Schouderklachten (versie 1999) [Guidelines for shoulder complaints of the Dutch College of General Practitioners (version 1999)]. Huisarts en Wetenschap. 1999;42:222e31. [Google Scholar]
- [2].Croft P, Pope D, Silman A.. The clinical course of shoulder pain: prospective cohort study in primary care. Primary Care Rheumatology Society Shoulder Study Group. BMJ. 1996. Sep 7;313(7057):601–602. 10.1136/bmj.313.7057.601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Hughes P, Taylor NF, Green RA. Most clinical tests cannot accurately diagnose rotator cuff pathology: a systematic review. Aust J Physiother. 2008;54:159–170. 10.1016/S0004-9514(08)70022-9 [DOI] [PubMed] [Google Scholar]
- [4].Walton DM, Sadi J. Identifying SLAP lesions: a meta-analysis of clinical tests and exercise in clinical reasoning. Phys Ther Sport. 2008;9:167–176. 10.1016/j.ptsp.2008.07.001 [DOI] [PubMed] [Google Scholar]
- [5].Beaudreuil J, Nizard R, Thomas T, et al. Contribution of clinical tests to the diagnosis of rotator cuff disease: a systematic review. Jt Bone Spine. 2009;76:15–19. 10.1016/j.jbspin.2008.04.015 [DOI] [PubMed] [Google Scholar]
- [6].Gadogan A, Laslett M, Hing W, et al. Inter-examiner reliability of orthopaedic special tests used in the assessment of shoulder pain. Man Ther. 2011;16:131–135. 10.1016/j.math.2010.07.009 [DOI] [PubMed] [Google Scholar]
- [7].Schellingerhout JM, Verhagen AP, Thomas S, et al. Lack of uniformity in diagnostic labeling of shoulder pain: time for a different approach. Man Ther. 2008;13:478–483. 10.1016/j.math.2008.04.005 [DOI] [PubMed] [Google Scholar]
- [8].Green S, Buchbinder R, Glazier R, et al. Systematic review of randomised controlled trials of interventions for painful shoulder: selection criteria, outcome assessment, and efficacy. BMJ. 1998. Jan 31;316(7128):354–360. 10.1136/bmj.316.7128.354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Boden BD, Davis DO, Dina TS, et al. A prospective and blind intervention of magnetic resonance imaging of the knee. abnormal findings in asymptomatic subjects. Clin Orthop Relat Res. 1992. Sep;282: 177–185. [PubMed] [Google Scholar]
- [10].Schibany N, Zehetgruber H, Kainberger F, et al. Rotator cuff tears in asymptomatic individuals: aclinical and ultrasonographic screening study. Eur J Radiol. 2004;51:263–268. 10.1016/S0720-048X(03)00159-1 [DOI] [PubMed] [Google Scholar]
- [11].Bedson J, Croft PR. The discordance between clinical and radiographic knee osteoarthritis: a systematic search and summary of the literature. BMC Musculoskelet Disord. 2008;9:116. 10.1186/1471-2474-9-116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Yusuf E, Kortekaas MC, Watt I, et al. Do knee abnormalities visualized on MRI explain knee pain in knee osteoarthritis? A systematic review. Ann Rheum Dis. 2011. Jan;70(1):60–67. Epub 2010 Sep 10.1136/ard.2010.131904 [DOI] [PubMed] [Google Scholar]
- [13].Silvis ML, Mosher TJ, Smetana BS, et al. High prevalence of pelvic and hip magnetic resonance imaging findings in asymptomatic collegiate and professional hockey players. Am J Sport Med. 2011;39(4):715–721. 10.1177/0363546510388931 [DOI] [PubMed] [Google Scholar]
- [14].Lewis JS. Rotator cuff tendinopathy: a model for the continuum of pathology and related management. Br J Sports Med. 2010;44(13):918–923. 10.1136/bjsm.2008.054817 [DOI] [PubMed] [Google Scholar]
- [15].May S, Rosedale R. A survey of the McKenzie classification system in the extremities: prevalence of mechanical syndromes and preferred loading strategies. Phys Ther. 2012;92(9):1175–1186. 10.2522/ptj.20110371 [DOI] [PubMed] [Google Scholar]
- [16].Guide to physical therapist practice American physical therapy association. Phys Ther.2nd ed. 2001;81:9–746. [PubMed] [Google Scholar]
- [17].Koes BW, van Tulder MW, Thomas S. Diagnosis and treatment of low back pain. BMI. 2006;332:1430–1434. 10.1136/bmj.332.7555.1430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].McKenzie RA. The lumbar spine. Mechanical Diagnosis and Therapy. Waikanae: Spinal Publications; 1981. [Google Scholar]
- [19].May S. The McKenzie classification system in Extremities: a reliability study using McKenzie assessment forms and experienced clinicians. J Manipulative Physiol Ther. 2009. Sep;32(7):556–563). 10.1016/j.jmpt.2009.08.007 [DOI] [PubMed] [Google Scholar]
- [20].Clare HA, Adams R, Maher CG. A systematic review of efficacy of McKenzie therapy for spinal pain. Aust J Physiother. 2004;50:209–216. 10.1016/S0004-9514(14)60110-0 [DOI] [PubMed] [Google Scholar]
- [21].May S, Littlewood C, Bishop A. Reliability of procedures used in the physical examination of non-specific low back pain: a systematic review. Aust J Physiother. 2006;52:91–102. 10.1016/S0004-9514(06)70044-7 [DOI] [PubMed] [Google Scholar]
- [22].Cook C, Hegedus EJ, Ramey K. Physical therapy exercise intervention based onclassification using the patient response method: a systematic review of the literature. J Man Manip Ther. 2005;13:152–162. 10.1179/106698105790824950 [DOI] [Google Scholar]
- [23].Machado LAC, de, Souza MvS, Ferreira PH, et al. The McKenzie method for low back pain. A systematic review of the literature with a meta-analysis approach. Spine. 2006;31:E254–E262. 10.1097/01.brs.0000214884.18502.93 [DOI] [PubMed] [Google Scholar]
- [24].Hettinga DM, Jackson A, Klaber Moffett J, et al. A systematic review and synthesis of higher quality evidence of the effectiveness of exercise interventions for nonspecific low back pain of at least 6 weeks duration. Phys Ther Rev. 2007;12:221-232. 10.1179/108331907X222958 [DOI] [Google Scholar]
- [25].Slade SC, Keating J. Unloaded movement facilitation exercise compared to no exercise or alternative therapy on outcomes for people with non-specific chronic low back pain: a systematic review. J Man Manip Ther. 2007;30:301–311. 10.1016/j.jmpt.2007.03.010 [DOI] [PubMed] [Google Scholar]
- [26].May S, Donelson R. Evidence-informed management of chronic low back pain with the McKenzie method. Spine J. 2008;8:134–141. 10.1016/j.spinee.2007.10.017 [DOI] [PubMed] [Google Scholar]
- [27].Aina A, May S, Clare H. The centralization phenomenon of spinal symptoms—a systematic review. Man Ther. 2004;9:134–143. 10.1016/j.math.2004.03.004 [DOI] [PubMed] [Google Scholar]
- [28].McKenzie RA, May S. The human extremities: mechanical diagnosis and therapy. Waikanae: Spinal Publications; 2000. [Google Scholar]
- [29].Long A. The centralisation phenomenon. Its usefulness as a predictor of outcome in conservative treatment of chronic low back pain. Spine. 1995;20:2513–2520. 10.1097/00007632-199512000-00010 [DOI] [PubMed] [Google Scholar]
- [30].Sufka A, Hauger B, Trenary M, et al. Centralisation of low back pain and perceived functional outcome. J Orthop Sports Phys Ther. 1998;27:205–212. 10.2519/jospt.1998.27.3.205 [DOI] [PubMed] [Google Scholar]
- [31].Long A, May S, Fung T. The comparative prognostic value of directional preference and centralization: a useful tool for front-line clinicians? J Man Manip Ther. 2008;16:248–254. 10.1179/106698108790818332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Werneke M, Hart DL, Cutrone G, et al. Association between directional preference and centralization in patients with low back pain. J Orthop Sports Phys Ther. 2011;41(1):22–31. 10.2519/jospt.2011.3415 [DOI] [PubMed] [Google Scholar]
- [33].Aina A, May S. A shoulder derangement. Man Ther. 2005;10:159–163. 10.1016/j.math.2005.01.001 [DOI] [PubMed] [Google Scholar]
- [34].Kidd JA. Treatment of shoulder pain utilizing mechanical diagnosis and therapy principles. J Man Manip Ther. 2013;21:168–173. 10.1179/2042618613Y.0000000037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Littlewood C, May S. A contractile dysfunction of the shoulder. Man Ther. 2007;12:80–83. 10.1016/j.math.2005.11.002 [DOI] [PubMed] [Google Scholar]
- [36].Aytona MC, Dudley K. Rapid resolution of chronic shoulder pain classified as derangement using the McKenzie method: a case series. J Man Manip Ther. 2013;21:207–212. 10.1179/2042618613Y.0000000034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Turner K. An audit of extremity patients. McKenzie Institute UK Newsletter. 2004;13(1):2–25. [Google Scholar]
- [38].May S. Classification by McKenzie mechanical syndromes; Report on directional preference and extremity patients. Int J Mech Diagn Ther. 2006;1(3):7–11. [Google Scholar]
- [39].Heidar Abady A., Rosedale R., Overend T, et al. Inter-examiner reliability of The McKenzie system of mechanical diagnosis and therapy (MDT) in assessing patients with shoulder pain. J Man Manip Ther. 2014. Nov; 22(4): 199–205. 10.1179/2042618614Y.0000000068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Stratford PW, Binkley JM, Stratford DM. Development and initial validation of the upper extremity functional index. Physiother Can. 2001;53(4):259–267. [Google Scholar]
- [41].Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain. 1986;27(1):117–126. 10.1016/0304-3959(86)90228-9 [DOI] [PubMed] [Google Scholar]
- [42].Hefford C, Abbott JH, Arnold R, et al. The patient-specific functional scale: validity, reliability, and responsiveness in patients with upper extremity musculoskeletal problems. J Orthop Sports Phys Ther. 2012;42(2):56–65. 10.2519/jospt.2012.3953 [DOI] [PubMed] [Google Scholar]
- [43].Jensen MP, McFarland CA. Increasing the reliability and validity of pain intensity measurement in chronic pain patients. Pain. 1993;55(2):195–203. 10.1016/0304-3959(93)90148-I [DOI] [PubMed] [Google Scholar]
- [44].Stratford PW, Spadoni G. The reliability, consistency, and clinical application of a numeric pain rating scale. Physiother Can. 2001;53(2):88–114. [Google Scholar]
- [45].Mintken PE, Glynn P, Cleland JA. Psychometric properties of the shortened disabilities of the arm, shoulder, and hand questionnaire (QuickDASH) and numeric pain rating scale in patients with shoulder pain. J Shoulder Elbow Surg. 2009;18(6):920–926. 10.1016/j.jse.2008.12.015 [DOI] [PubMed] [Google Scholar]
- [46].Michener LA, Snyder AR, Leggin BG. Responsiveness of the numeric pain rating scale in patients with shoulder pain and the effect of surgical status. J Sport Rehabil. 2011;20(1):115–128. 10.1123/jsr.20.1.115 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.