Abstract
Background
High intensity interval training (HIIT) is a robust and time-efficient approach to improve multiple health indices including maximal oxygen uptake (VO2max). Despite the intense nature of HIIT, data in untrained adults report greater enjoyment of HIIT versus continuous exercise (CEX). However, this has yet to be investigated in persons with spinal cord injury (SCI).
Objective
To examine differences in enjoyment in response to CEX and HIIT in persons with SCI.
Design
Repeated measures, within-subjects design.
Setting
University laboratory in San Diego, CA.
Participants
Nine habitually active men and women (age = 33.3 ± 10.5 years) with chronic SCI.
Intervention
Participants performed progressive arm ergometry to volitional exhaustion to determine VO2peak. During subsequent sessions, they completed CEX, sprint interval training (SIT), or HIIT in randomized order.
Outcome Measures
Physical activity enjoyment (PACES), affect, rating of perceived exertion (RPE), VO2, and blood lactate concentration (BLa) were measured.
Results
Despite a higher VO2, RPE, and BLa consequent with HIIT and SIT (P < 0.05), PACES was significantly higher (P = 0.03) in response to HIIT (107.4 ± 13.4) and SIT (103.7 ± 12.5) compared to CEX (81.6 ± 25.4). Fifty-five percent of participants preferred HIIT and 45% preferred SIT, with none identifying CEX as their preferred exercise mode.
Conclusion
Compared to CEX, brief sessions of submaximal or supramaximal interval training elicit higher enjoyment despite higher metabolic strain. The long-term efficacy and feasibility of HIIT in this population should be explored considering that it is not viewed as more aversive than CEX.
Keywords: Paralysis, Physical activity enjoyment, Arm ergometry, Oxygen uptake, Affect
Introduction
Spinal cord injury (SCI) presents severe physiological, psychological, and financial challenges to the affected individual. Data1 report that incidence of new SCI in the United States has increased to approximately 12,500 cases per year. One serious consequence of SCI is impaired locomotion which leads to a relatively sedentary lifestyle and increased risk of chronic disease.2 In fact, only 50% of persons with SCI obtain an adequate amount of physical activity.3 As physical activity is a contributing factor affecting chronic disease risk in able-bodied adults4 as well as in individuals with SCI,5 identifying optimal exercise modes in SCI is paramount to improve overall health status.
Popular modalities of exercise typically completed by people with SCI include aerobic exercise,6 resistance training,7 leisure sports (tennis, basketball, etc.), and wheeling.3 Advantages to these modalities are that they are more accessible than those used in specialized rehabilitation centers such as locomotor training,8 functional electrical stimulation,9 or vibration exercise10 which are expensive and require guidance of trained personnel. Regular participation in these modalities satisfies exercise-based recommendations for persons with SCI11 and likely helps them reduce severity of various long-term health related complications after SCI. Nevertheless, beyond the importance of accessibility of exercise for this population or specific benefits to health status and physical function is the level of pleasure and enjoyment experienced12 which may be related to long-term adherence13 and likely beneficial changes to health status. Nevertheless, to our knowledge, little data exist regarding these indices in SCI. Consequently, much remains to be learned regarding attitudes and perceptions of exercise of various modalities and intensities in individuals with SCI.
In the last decade, high intensity interval training (HIIT) has been shown to be a suitable alternative to moderate continuous exercise (CEX) for significantly improving cardiorespiratory fitness (VO2max),14 fat utilization,15 and insulin sensitivity16 which overall increases health status and exercise tolerance. HIIT is characterized by completion of repeated bursts of exercise (60–240 seconds in duration) at intensities approaching or equal to the workload associated with maximal oxygen uptake (Wmax) which typically elicit 80–100 percent maximal heart rate. A more intense form of HIIT is sprint interval training (SIT) typically characterized by repeated 10–30 s efforts at power outputs ranging from 170–300% Wmax. Each bout is followed by recovery, with total training duration lower than that of CEX. As time is often cited as the greatest barrier to habitual exercise,17 this seems advantageous to all individuals. In fact, there are reports that persons with diabetes,18 heart disease,19 and obesity20 can perform HIIT without any side effects while experiencing robust adaptations such as increases in cardiorespiratory fitness and insulin sensitivity typically associated with CEX. More recently, acute bouts of HIIT have been reported to be more enjoyable than CEX in active men21 as well as untrained adults22 which highlight its potential in other deconditioned populations such as SCI. To our knowledge, only two studies have examined efficacy of HIT in persons with SCI,23,24 and data show that men with chronic SCI are quite tolerant of HIIT and experience significant increases (+ 20–24%) in cardiorespiratory fitness in response to HIIT.
This study aimed to compare physiological and perceptual responses between CEX and two widely-utilized modalities of interval training (HIIT and SIT) in persons with SCI. Data will add to the dogma concerning identifying effective exercise-based recovery options to improve physical function, exercise adherence, and health status in this population. It was hypothesized that persons with SCI will view both forms of interval training as being more enjoyable than CEX.
Methods
Participants
Men and women who were habitually active (8.1 ± 4.4 hours/wk) and at least 12 months post-SCI were recruited for this study from a local SCI rehabilitation facility as well as through word-of-mouth. They regularly participated in exercise modalities including wheeling, resistance training, locomotor training, surfing, stretching, and assisted/unassisted walking, yet none had previously performed HIIT. Two had tetraplegia and eight had paraplegia. Prospective participants were free of disease and any musculoskeletal ailment preventing them from completing exercise required in this study. Inclusion criteria were injury lower than C2 and non-ventilator dependent, physician permission to engage in intense exercise, lack of medication use which may affect psychological and physiological responses as measured in the study, and age 18–60 years. Participants initially completed a health-history questionnaire and physical activity survey25 to verify their eligibility and subsequently provided written informed consent. All study procedures were approved by the University Institutional Review Board.
Experimental design
Participants completed four exercise sessions in the laboratory over a 2–3-week period. All sessions were held at the same time of day within participants and were preceded by a 3-hour fast and abstention from exercise for 24 hours. On the first day, peak oxygen uptake (VO2peak) was determined during progressive arm ergometry to exhaustion. The subsequent three sessions consisted of CEX, HIIT, or SIT, whose order was randomized. A minimum of 2 days and a maximum of 7 days separated each trial. During these sessions, gas exchange data, blood lactate concentration, and perceptual responses were measured.
Assessment of peak oxygen uptake (VO2peak)
Participants arrived at the lab dressed in exercise attire for initial determination of VO2peak. They self-reported their height and body mass, and following 5 minutes of seated rest, pre-exercise blood lactate concentration (BLa) was obtained from a fingertip blood sample (Nova Biomedical, Waltham, MA, USA). After a 5-minute warmup at 7 W, individuals performed arm cranking on the wall-mounted ergometer (Lode Angio, Groningen, the Netherlands) for 8–12 minutes at a self-selected cadence until volitional exhaustion, which was identified as cadence less than 30 rev/minute. The height of the arm ergometer was established during this trial and maintained within participants for all subsequent trials, so the shoulder joint was horizontal to the arm cranks. During exercise, power output was increased in a ramp-like manner by 3 W/minute for persons with tetraplegia and 13 W/minute for persons with paraplegia, and pulmonary gas exchange data were obtained via a metabolic cart (ParvoMedics True One, Sandy, UT, USA) which was calibrated prior to exercise according to manufacturer specifications. Three minutes after this bout, BLa was determined. After an 8–10-minute active recovery at 7 W, participants exercised at 105% of their maximum workload (Wmax) until exhaustion to ensure that VO2peak was attained in the initial trial. This bout also served to familiarize participants with HIIT to be completed in subsequent sessions.
Completion of CEX, HIIT, and SIT
These sessions were performed in randomized order according to a Latin Squares design.26 All sessions began with a 5-minute warmup at 10% Wpeak. Continuous exercise consisted of 25 min of arm cranking at 45%Wpeak. HIIT was comprised of eight 60-second bouts at 70% Wpeak separated by 90 seconds of active recovery at 10% Wpeak, while SIT required eight 30-second “all-out” efforts at 105% Wpeak separated by 120 seconds of active recovery at 10% Wpeak.
During all bouts, pulmonary gas exchange data and heart rate (HR, Polar, Woodbury, NY, USA) were continuously obtained every 15 seconds. Values for VO2 and HR were averaged from three successive values at rest, at the end of the warm-up, and at 25, 50, 75, and 100% of session completion. This represented minutes 5, 10, 15, and 20 for HIIT/SIT and 6.25, 12.5, 18.75, and 25.0 for CEX, respectively. Blood lactate concentration was measured pre-exercise as well as at 25, 50, 75, and 100% of session completion (3 minutes post-exercise). As participants were using their hands to crank the ergometer, at each time point they briefly stopped cranking with one hand and a fingertip blood sample was immediately acquired from the non-exercising limb.
The following psychological measures were also acquired prior to exercise and at 25, 50, 75, and 100% of session completion as well as at 5 minutes post-exercise: rating of perceived exertion (0–10 Category Ratio scale (CR-10)),27 affect (11-point scale, ranging from +5 very good to –5 very bad),28 and exercise enjoyment (1–7 scale).29 These measures were recorded throughout CEX and at the termination of individual HIIT and SIT bouts to better reflect the perception of exercise rather than the transition into recovery. Specific instructions were read to each participant before each session. The meaning of the CR-10 scale was communicated by instructing participants to report perceptions of their exertion in terms of their breathing, heart rate, and level of fatigue. For affect, they were read the following text: While participating in exercise, it is common to experience changes in mood. Some individuals find exercise pleasurable; whereas, others find it to be unpleasant. Additionally, feeling may fluctuate across time. That is, one might feel good and bad a number of times during exercise. For exercise enjoyment, they were instructed to use the following scale to indicate how much you are enjoying this exercise session at this instant. Participants were asked to respond to each scale in terms of how they felt at that moment. In addition, at cessation of each session, participants were requested to list specific words to describe each modality of exercise.
Ten minutes post-exercise, the Physical Activity Enjoyment Scale (PACES)30 was completed to assess level of enjoyment of each bout. This instrument contains 18 questions scored on a 1–7 Likert scale. After completion of all three sessions, participants were asked which modality of exercise they ultimately preferred (HIIT, SIT, or CEX).
Data analysis
Data are reported as mean ± standard deviation (SD) and were analyzed with SPSS version 20.0 (IBM Corp, Armonk, NY, USA). Two-way ANOVA with repeated measures was used to examine differences in variables across exercise bout (CEX, HIIT, and SIT) and time. One-way ANOVA with repeated measures was used to identify differences in PACES between bouts. If a significant F ratio was obtained, Tukey's post hoc test was used to identify differences between means. The Greenhouse-Geisser correction was used to account for the sphericity assumption of unequal variances across groups. Effect size was determined using partial eta-squared (η2p). Statistical significance was set at P < 0.05.
Results
One male participant completed the VO2peak test and then suffered an unrelated injury, so withdrew from the study. Descriptive characteristics of the eight men and one woman with SCI who completed all requirements of the study are shown in Table 1. Session duration differed between CEX (30 min) and HIIT/SIT (25 min) and total energy expenditure was higher (F2,16 = 13.1, P < 0.001, η2p = 0.62) in CEX (118.1 ± 37.8 kcal) versus HIIT (102.0 ± 35.2 kcal) and SIT (96.6 ± 31.6 kcal).
Table 1.
Participant physical characteristics.
| Participant | Age (yr) | DOI (yr) | Injury level | BMI (kg/m2) | VO2max (L/min) |
|---|---|---|---|---|---|
| F | 28 | 12.0 | T2 | 19.0 | 0.67 |
| M | 57 | 20.0 | C5 | 22.2 | 0.66 |
| M | 25 | 1.1 | T6 | 21.7 | 1.23 |
| M | 40 | 1.1 | T9 | 22.2 | 1.86 |
| M | 27 | 2.2 | T3 | 22.9 | 1.27 |
| M | 36 | 10.0 | C5 | 21.5 | 1.15 |
| M | 25 | 1.4 | T5 | 22.7 | 1.94 |
| M | 27 | 10.0 | T7 | 22.4 | 1.55 |
| M | 26 | 3.5 | T3 | 20.8 | 1.00 |
| Mean ± SD | 33.3 ± 10.5 | 6.8 ± 6.2 | NA | 22.6 ± 3.1 | 1.30 ± 0.45 |
F, female; M, male; DOI, duration of injury; T, thoracic; C, cervical; BMI, body mass index.
Differences in VO2 and HR in response to HIIT, SIT, and CEX
Oxygen uptake (VO2) was significantly different across time (F1.1,8.7 = 51.1, P < 0.001, η2p = 0.86), and a significant main effect (F1.3,10.3 = 4.9, P = 0.04, η2p = 0.38) and boutXtime interaction (F1.9,15.6 = 3.3, P = 0.03, η2p = 0.29) were observed. Post hoc analyses showed higher VO2 in HIIT versus CEX at 75% of session duration and at end-exercise, when VO2 was higher in response to HIIT and SIT versus CEX (Fig. 1A). Significant differences in HR were seen across time (F1.3,10.0 = 102.0, P < 0.001, η2p = 0.92) as well as a significant main effect (F1.7,13.3 = 7.0, P = 0.01, η2p = 0.47) and boutXtime interaction (F3.7,29.8 = 6.1, P = 0.001, η2p = 0.43). At all exercise time points, HR was higher in SIT/HIIT versus CEX (Fig. 1B). During HIIT and SIT, HR surpassed 90% of peak values.
Figure 1.
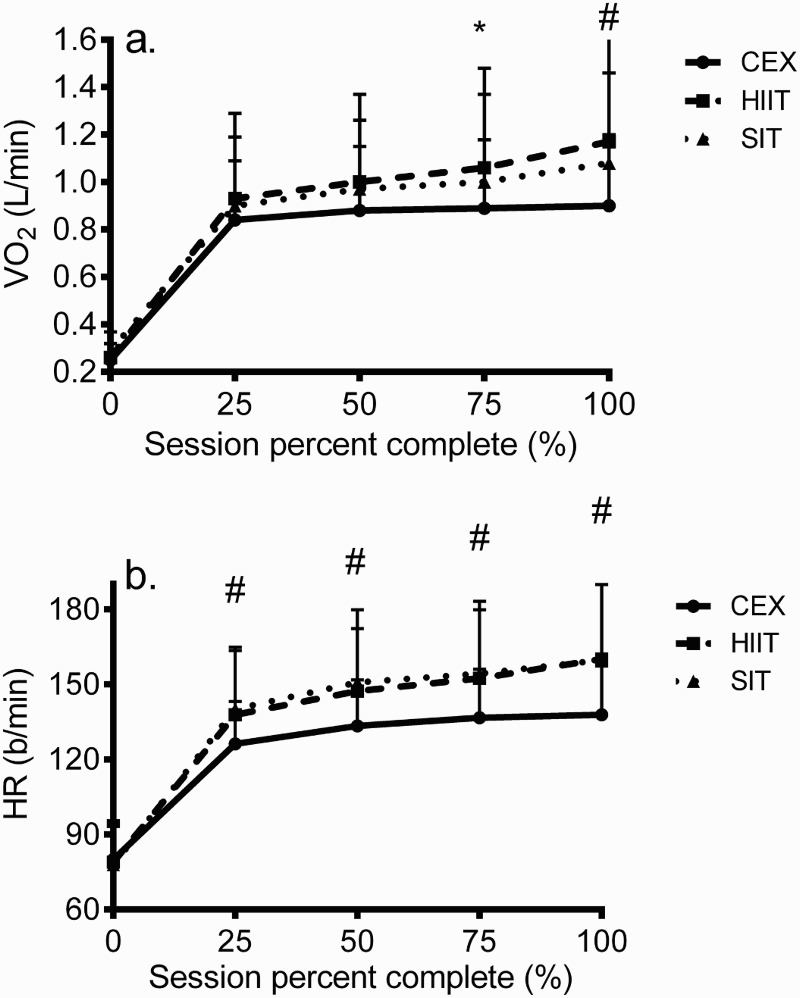
Differences in a) oxygen uptake and b) heart rate in response to sessions of CEX, HIIT, and SIT in persons with SCI. Data are mean ± SD. * = P < 0.05 between HIIT and CEX; # = P < 0.05 between HIIT/SIT and CEX.
Differences in BLa in response to HIIT, SIT, and CEX
Blood lactate concentration was significantly different across time (F1.6,12.7 = 36.7, P < 0.001, η2p = 0.82) and bouts (F2,16 = 16.2, P < 0.001, η2p = 0.67), and data showed a significant boutXtime interaction (F3.5,28.9 = 11.6, P < 0.001, η2p = 0.59). Post hoc analyses revealed that BLa was different at 25% (SIT vs. CEX), at 75% (HIIT and SIT vs. CEX), and at 50 and 100% (HIIT vs. SIT vs. CEX) of session duration (Fig. 2).
Figure 2.
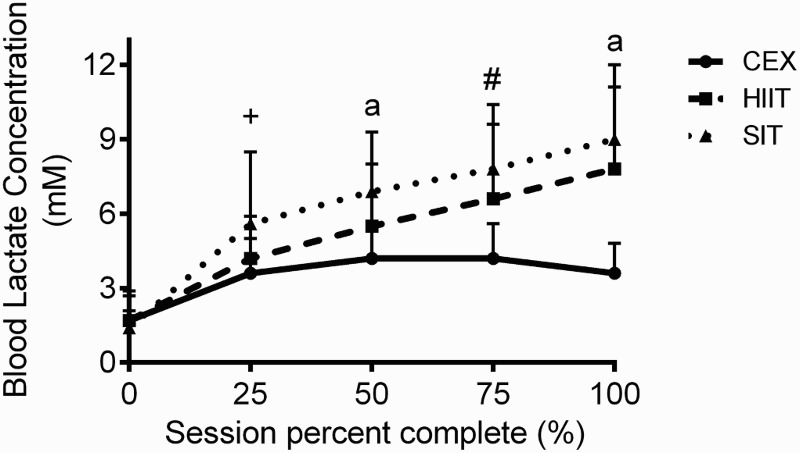
Differences in blood lactate concentration in response to sessions of CEX, HIIT, and SIT in persons with SCI. Data are mean ± SD. + = P < 0.05 between SIT and CEX; # = P < 0.05 between HIIT/SIT and CEX; a = P < 0.05 between all modes.
Differences in physical activity enjoyment in response to HIIT, SIT, and CEX
Figure 3 reveals differences in PACES between bouts. PACES was significantly different (F1.0,8.2 = 6.7, P = 0.03, η2p = 0.46), with post hoc analyses demonstrating that SIT (103.7 ± 12.5) and HIIT (107.4 ± 13.4) revealed higher enjoyment versus CEX (81.6 ± 25.4). Across all participants, 5/9 (55%) preferred HIIT and 4/9 (45%) preferred SIT, with no subject citing preference for CEX. All participants reported that HIIT and SIT were “challenging” and/or “energizing,” and 66% characterized these modes as “exhilarating and stimulating”; whereas, six participants described CEX as “boring” and “monotonous” with only two participants describing it as “enjoyable” or “stimulating.”
Figure 3.
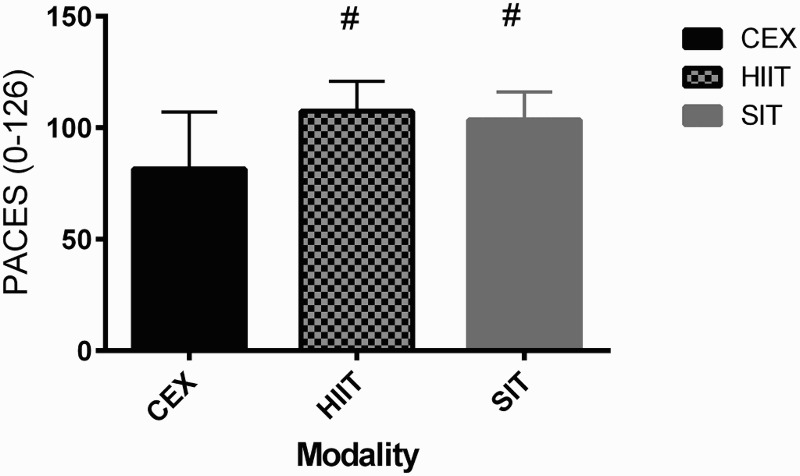
Differences in Physical Activity Enjoyment in response to sessions of CEX, HIIT, and SIT in persons with SCI. Data are mean ± SD. # = P < 0.05 versus CEX.
Differences in RPE, affect, and exercise enjoyment in response to HIIT, SIT, and CEX
Rating of perceived exertion differed significantly across time (F1.5,11.6 = 120.7, P < 0.001, η2p = 0.94) and bout (F2,16 = 9.7, P = 0.02, η2p = 0.55). A significant boutXtime interaction was observed (F10,80 = 3.7, P < 0.001, η2p = 0.32). Post hoc analyses showed that RPE during HIIT and SIT was higher than CEX at 50, 75, and 100% of session duration (Fig. 4A). Affect declined across time (F1.7,13.5 = 3.9, P = 0.049, η2p = 0.33) but no main effect of bout (P = 0.23) or boutXtime interaction (P = 0.51) was demonstrated (Fig. 4B). Affect measured 5 min post-exercise was more positive (P < 0.05) than all exercise values and was similar to the pre-exercise value. Exercise enjoyment gradually increased during exercise from baseline but this failed to reach significance (P = 0.53) (Fig. 4C). In addition, no main effect of bout (P = 0.09) or boutXtime interaction (P = 0.52) was revealed.
Figure 4.
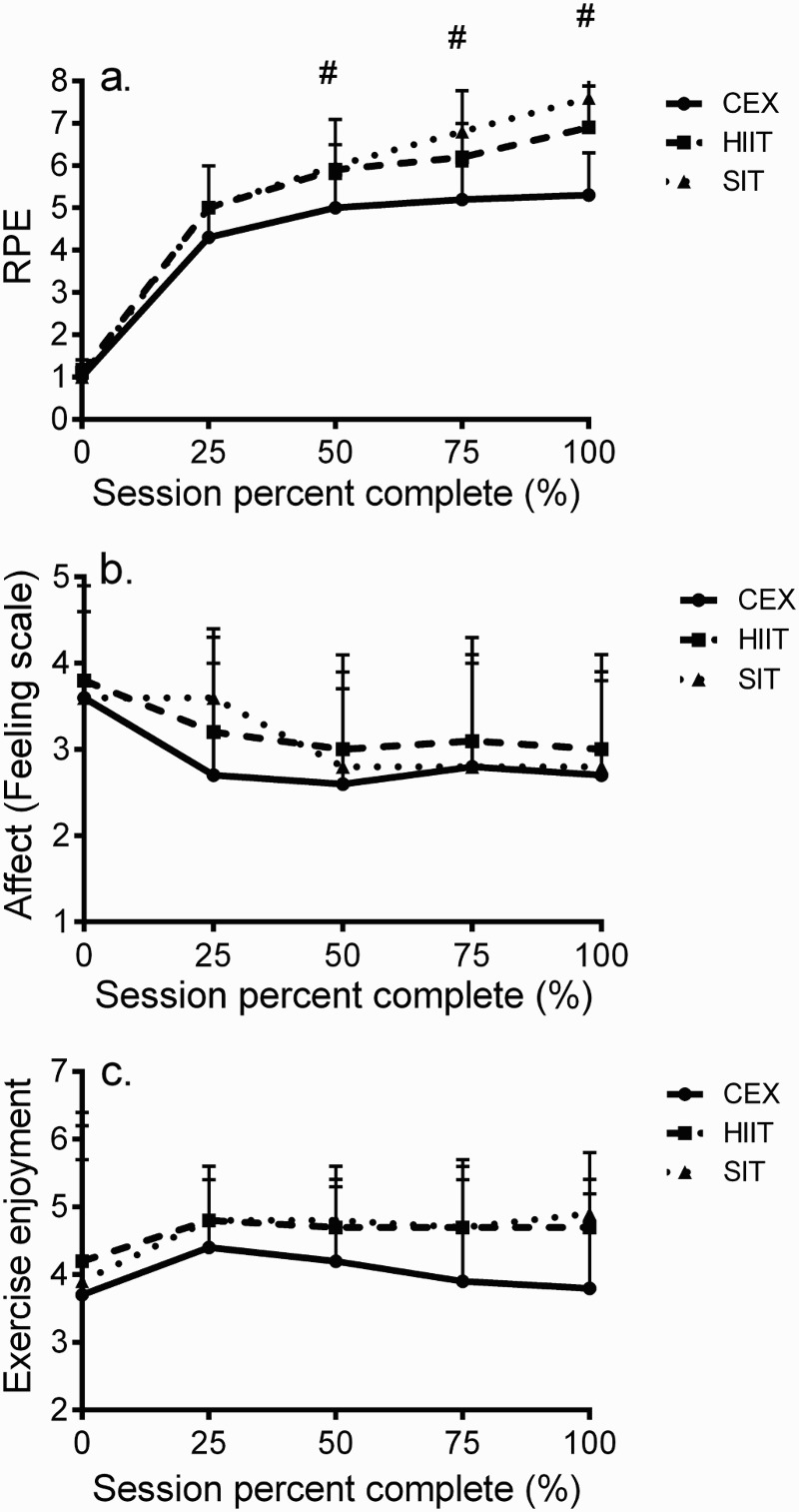
Differences in A) ratings of perceived exertion, B) affect, and C) exercise enjoyment in response to sessions of CEX, HIIT, and SIT in persons with SCI. Data are mean ± SD. # = P < 0.05 between HIIT/SIT and CEX.
Discussion
Completion of acute bouts of high intensity interval training elicits higher enjoyment compared to continuous exercise in active20 and untrained adults.21 Due to its robust physiological adaptations13,14,17 as well as lower training volume which may reduce exercise duration, HIIT seems to be an attractive alternative to CEX in various populations. Nevertheless, its potential in persons with SCI is poorly understood and no study has explored differences in enjoyment between HIIT and CEX in this population. Our data show that enjoyment as measured with the PACES scale was significantly higher in response to HIIT and SIT compared to CEX despite intensity of HIIT surpassing 90% HRpeak. In addition, no participant cited preference for continuous exercise compared to either regime of interval training.
Significant differences in oxygen uptake (Fig. 1A) and blood lactate concentration (Fig. 2) between HIIT/SIT and CEX confirm the greater metabolic strain of interval training versus continuous exercise. Data from a study in young able-bodied adults31 also showed higher BLa and VO2 in response to high volume HIIT versus 20 min of CEX. The greater oxygen uptake seen in both interval training regimes reflects higher reliance on oxidative metabolism for ATP supply; whereas, greater recruitment of higher threshold fast twitch muscle fibers and subsequent reliance on glycolysis mediate the significantly higher BLa observed in response to HIIT and SIT versus CEX. Our perceptual findings also parallel recent data exhibited in active and untrained adults. In active men, Bartlett et al.21 demonstrated higher enjoyment measured via PACES in response to interval running (6×3-minute bouts at 90% VO2max separated by 3 minutes recovery at 50% VO2max) versus 50 min of running at 70% VO2max. Bouts were matched for average heart rate, oxygen uptake, and total energy expenditure although RPE was higher in response to interval running. In untrained men and women, Jung et al.22 compared affective and enjoyment responses between HIIT (1 minute at 100%Wpeak separated by 1 minute at 20% Wpeak) and moderate (40 minutes at 40% Wpeak) and heavy CEX (20 minutes at 80% Wmax). Results showed significantly lower affect in response to HIIT and heavy CEX versus moderate CEX, which adheres to the Dual-Mode theory.12 Yet, perceived enjoyment was similar between HIIT and moderate CEX, and when asked which exercise mode was preferred, 60% chose HIIT and 30% chose moderate CEX. Similar findings were also exhibited by Martinez et al.32 who showed that shorter bouts of HIIT led to more positive affect than heavy CEX. So, despite the greater VO2, BLa, and HR evoked by HIIT and SIT (Figs. 1 and 2), it is not viewed as more unpleasant than moderate or heavy CEX.
Several explanations have been identified to explain the greater enjoyment seen in response to HIIT compared to CEX. One explanation is the unique structure of HIIT consisting of brief, intense bursts of exercise separated by recovery.22 It is thought that these frequent breaks reduce participants’ perception of difficulty and increase feelings of pleasure of this modality. In addition, completion of each bout of HIIT provides a sense of accomplishment that does not occur in CEX until the completion of the entire bout.22 Lastly, the lower total exercise volume of HIIT and especially SIT may reduce perception of difficulty and increase feelings of pleasure. Overall, HIIT and SIT do not seem to cause severely negative perceptions in individuals unaccustomed to intense exercise, and may in fact augment perceptual responses versus more prolonged bouts of exercise during which effort must be sustained over extended periods.
To our knowledge, only two studies have explored efficacy of chronic HIIT in this population. Brurok et al.23 required six men with chronic complete SCI to perform 24 sessions of hybrid HIIT at intensities equal to 85–90% Wpeak from arm ergometry and current amplitude of 80% of 140 mA during FES cycling. VO2peak was increased by 24.4% which was mediated by a significant increase in stroke volume. In response to 6 weeks of virtual reality hybrid HIIT, a 20% increase in VO2peak was shown.24 These findings suggest that HIIT is feasible in this population. Nevertheless, in neither study were perceptual or acute physiological responses examined, and no comparison was made to continuous exercise. Consequently, these data leave much to be clarified regarding suitability of HIIT in persons with SCI.
Data regarding changes in oxygen uptake (Fig. 1A), heart rate (Fig. 1B), and blood lactate concentration (Fig. 2) confirm the strenuous nature of HIIT and SIT performed in the current study. Oxygen uptake attained 82% and 90% of VO2peak during SIT and HIIT. Peak HR during HIIT (160.1 ± 31.1 b/minute) and SIT (159.6 ± 30.2 b/minute) was comparable to peak HR from the baseline graded exercise test (160.6 ± 29.1 b/minute) demonstrating the significant cardiovascular stimulus of our interval training regimes. In fact, these HR values are higher than those seen for combined arm and leg cycling at 80% HRpeak.33 Peak BLa was equal to 7.6 ± 3.3 and 9.0 ± 3.0 mM in response to HIIT and SIT which were higher than that determined at 75% and 100% of CEX (4.2 ± 1.4 mM and 3.6 ± 1.2 mM). Previous findings32 show slightly lower BLa values during steady state FES leg cycling in sedentary men with complete SCI compared to HIIT and SIT. In contrast, similar BLa values (6.4–8.5 mM) were demonstrated in nine men with chronic SCI performing steady-state arm ergometry combined with FES leg cycling, but completion of hybrid exercise on a commercially available arm and leg tricycle at intensity equal to 80% VO2peak led to higher BLa (5.7–10.8 mM).34 This marked production of BLa is surprising considering that our participants were not using their lower extremity as is the case with FES cycling, although many of our participants with paraplegia attempted to engage their trunk musculature during sessions of HIIT or SIT.
Affect declined during all exercise modes (Fig. 4B) but was not different between CEX, HIIT, and SIT. This result is opposed by previous data35 which demonstrated less positive affect during HIIT versus CEX. Similar data were shown by Jung et al.22 in which affect was less positive in response to HIIT compared to moderate CEX, although responses were comparable between HIIT and vigorous CEX. An explanation for this may lie in the significant blood lactate accumulation seen throughout all exercise modes, which has been suggested to elicit reductions in affect.12 In addition, arm ergometry may augment ability to express feelings of exertion during exercise compared to exercise involving large muscle groups.36 Thus, the perceptual sensitivity for the processing of physiological information may be increased during small muscle mass exercise.37
There are a few limitations to the present study. Our sample was relatively small although it was diverse in age as well as injury severity and completeness which broadens our findings to a larger portion of individuals with SCI. Despite this, differences in outcome measures between exercise modalities were highly significant and parallel responses seen in able-bodied populations. Previous studies employing HIIT in this population23,24 combined arm ergometry with lower-body FES, which would elicit a larger exercising muscle mass and higher absolute increases in VO2 and HR. We acknowledge that HIIT and SIT as performed in the current study may not be feasible in persons with SCI lacking adequate upper body strength. The specific workload used to implement CEX equal to 45% Wpeak resulted in significant increases in BLa (Fig. 2), which suggests that it was more intense than work rates typically assigned for moderate continuous exercise. Nevertheless, HR, VO2, and BLa were lower during CEX compared to HIIT/SIT, which emphasizes that it was substantially less strenous than acute interval training. It has been reported12 that the time it takes for a significant increase in affect to occur once exercise ceases may take longer following more intense exercise such as HIIT while the influence of the interoceptive cues dissipates, so our reported values recorded immediately after each HIIT/SIT bout should be similar to those taken during exercise. Lastly, our sample was habitually active, so data cannot be applied to persons with SCI who are sedentary. However, our mean VO2max was considerably lower than average values (VO2peak = 1.51 L/minute) previously reported in persons with SCI.38
Conclusion
Our findings demonstrate that acute sessions of low-volume HIIT and SIT are more enjoyable than CEX despite a higher oxygen uptake, heart rate, and blood lactate concentration, indicating a substantially greater cardiorespiratory and metabolic stress. Moreover, as no side effects were reported and participants preferred interval training versus CEX, its potential as an element of exercise-based rehabilitation in persons with SCI should be further explored. As adaptations including VO2peak may be maximized by training at a higher intensity of VO2peak,39 chronic interval training may serve as a robust and time-efficient approach to augment cardiorespiratory fitness and health status in this population who face elevated risks of chronic disease.
Acknowledgements
The authors thank the participants for their effort and dedication to the study as well as Eric T. Harness for assistance in participant recruitment.
Disclaimer statements
Contributors None.
Disclosure of funding Funding was obtained for this project from a University GPSM grant, yet no federal funding (NIH, NSF, etc.) was obtained.
Conflict of interest No author had any conflict of interest in the completion of this work.
Ethics approval None.
References
- 1.National Spinal Cord Injury Statistical Center, Facts and Figures at a Glance Birmingham, AL: University of Alabama at Birmingham, February 2015, pp. 1–2. [Google Scholar]
- 2.Bauman WA, Spungen AM.. Coronary heart disease in individuals with spinal cord injury: assessment of risk factors. Spinal Cord 2008;46(7):466–76. doi: 10.1038/sj.sc.3102161 [DOI] [PubMed] [Google Scholar]
- 3.Ginis KA, Latimer AE, Arbour-Nicitopoulos KP, Buchholz AC, Bray SR, Craven BC, et al Leisure time physical activity in a population-based sample of people with spinal cord injury part I: demographic and injury-related correlates. Arch Phys Med Rehabil 2010;91(5):722–8. doi: 10.1016/j.apmr.2009.12.027 [DOI] [PubMed] [Google Scholar]
- 4.Garber CE, Blissmer B, Deschenes MR, American College of Sports Medicine Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sport Exerc 2011;43:1334–59. doi: 10.1249/MSS.0b013e318213fefb [DOI] [PubMed] [Google Scholar]
- 5.Myers J, Lee M, Kiratli J.. Cardiovascular disease in spinal cord injury: an overview of prevalence, risk, evaluation, and management. Am J Phys Med Rehabil 2007;86:142–52. doi: 10.1097/PHM.0b013e31802f0247 [DOI] [PubMed] [Google Scholar]
- 6.Lewis JE, Nash MS, Hamm LF, Martins SC, Groah SL.. The relationship between perceived exertion and physiologic indicators of stress during graded arm exercise in persons with spinal cord injuries. Arch Phys Med Rehabil 2007;88(9):1205–11. doi: 10.1016/j.apmr.2007.05.016 [DOI] [PubMed] [Google Scholar]
- 7.Gorgey AS, Mather KJ, Cupp HR, Gater DR.. Effects of resistance training on adiposity and metabolism after spinal cord injury. Med Sci Sports Exerc 2012;44(1):165–74. doi: 10.1249/MSS.0b013e31822672aa [DOI] [PubMed] [Google Scholar]
- 8.Giangregorio LM, Hicks AL, Webber CE, Phillips SM, Craven BC, Bugaresti JM, et al Body weight supported treadmill training in acute spinal cord injury: impact on muscle and bone. Spinal Cord 2005;43:649–57. doi: 10.1038/sj.sc.3101774 [DOI] [PubMed] [Google Scholar]
- 9.Shields RK, Dudley-Javoroski S.. Musculoskeletal adaptations in chronic spinal cord injury: effects of long-term soleus electrical stimulation training. Neurorehabil Neural Repair 2007;21:169–79. doi: 10.1177/1545968306293447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Nes IJ, Guerts AC, Hendricks HT, Duysen J.. Short-term effects of whole-body vibration on postural control in unilateral chronic stroke patients: preliminary evidence. Am J Phys Med Rehabil 2004;83(11):867–73. doi: 10.1097/01.PHM.0000140801.23135.09 [DOI] [PubMed] [Google Scholar]
- 11.Evans N, Wingo B, Sasso E, Hicks A, Gorgey AS, Harness E.. Exercise recommendations and considerations for persons with spinal cord injury. Arch Phys Med Rehabil 2015;96(9):1749–50. doi: 10.1016/j.apmr.2015.02.005 [DOI] [PubMed] [Google Scholar]
- 12.Ekkekakis P, Parfitt G, Petruzzello SJ.. The pleasure and displeasure people feel when they exercise at different intensities—decennial update and progress towards a tripartite rationale for exercise intensity prescription. Sports Med 2011;41(8):641–71. doi: 10.2165/11590680-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 13.Williams DM, Dunsiger S, Ciccoli JT, Lewis BA, Albrecht AE, Marcus BH.. Acute affective responses to a moderate-intensity exercise stimulus predicts physical activity participation 6 and 12 months later. Psychol Sport Exerc 2008;9:231–45. doi: 10.1016/j.psychsport.2007.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nybo L, Sundstrup E, Jakobsen MD, Mohr M, Hornstrup T, Simonsen L, et al High-intensity training versus traditional exercise interventions for promoting health. Med Sci Sports Exerc 2010;42(10):1951–8. doi: 10.1249/MSS.0b013e3181d99203 [DOI] [PubMed] [Google Scholar]
- 15.Astorino TA, Schubert MM, Palumbo E, Stirling D, McMillan DW.. Effect of two doses of interval training on maximal fat oxidation in sedentary women. Med Sci Sports Exerc 2013;45(10):1878–86. doi: 10.1249/MSS.0b013e3182936261 [DOI] [PubMed] [Google Scholar]
- 16.Babraj JA, Vollaard NBJ, Keast C, Guppy FM, Cottrell G, Timmons JA.. Extremely short duration high intensity interval training substantially improves insulin action in young sedentary males. BMC Endocr Disord 2009;9:3. doi: 10.1186/1472-6823-9-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Trost SG, Owen N, Bauman AE, Sallis JF, Brown W.. Correlates of adults’ participation in physical activity: review and update. Med Sci Sports Exerc 2002;34(12):1996–2001. doi: 10.1097/00005768-200212000-00020 [DOI] [PubMed] [Google Scholar]
- 18.Little JP, Gillen JB, Percival ME, Safdar A, Tarnopolsky MA, Punthakee Z, et al. Low-volume high-intensity interval training reduces hyperglycemia and increases muscle mitochondrial capacity in patients with type 2 diabetes. J Appl Physiol 2011;111(6):1554–60. doi: 10.1152/japplphysiol.00921.2011 [DOI] [PubMed] [Google Scholar]
- 19.Wisløff U, Støylen A, Loennechen JP, Bruvold M, Rognmo Ø, Haram PM, et al. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation 2007;115(24):3086–94. doi: 10.1161/CIRCULATIONAHA.106.675041 [DOI] [PubMed] [Google Scholar]
- 20.Whyte LJ, Gill JMR, Cathcart AJ.. Effect of 2 weeks of sprint interval training on health-related outcomes in sedentary overweight/obese men. Metabolism 2010;59(10):1421–8. doi: 10.1016/j.metabol.2010.01.002 [DOI] [PubMed] [Google Scholar]
- 21.Bartlett JD, Close GL, Maclaren DPM, Gregson W, Drust B, Morton JP.. High-intensity interval running is perceived to be more enjoyable than moderate-intensity continuous exercise: implications for exercise adherence. J Sports Sci 2011;29(6):547–53. doi: 10.1080/02640414.2010.545427 [DOI] [PubMed] [Google Scholar]
- 22.Jung ME, Bourne JE, Little JP.. Where does HIT fit? An examination of the affective response to high-intensity intervals in comparison to continuous moderate- and continuous vigorous-intensity exercise in the exercise intensity-affect continuum. PLoS One 2014;9:e114541. doi: 10.1371/journal.pone.0114541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brurok B, Helgerud J, Karlsen T, Leivseth G, Hoff J.. Effect of aerobic high-intensity hybrid training on stroke volume and peak oxygen consumption in men with spinal cord injury. Am J Phys Med Rehabil 2011;90(5):407–14. doi: 10.1097/PHM.0b013e31820f960f [DOI] [PubMed] [Google Scholar]
- 24.Hasnan N, Engkasan JP, Husain R, Davis GM.. High-intensity virtual-reality arm plus FES-leg interval training in individuals with spinal cord injury. Biomed Tech 2013;58(Suppl. 1). [DOI] [PubMed] [Google Scholar]
- 25.Washburn RA, Zhu W, McAuley E, Frogley M, Figoni SF.. The physical activity scale for individuals with physical disabilities: development and evaluation. Arch Phys Med Rehabil 2002;83(2):193–200. doi: 10.1053/apmr.2002.27467 [DOI] [PubMed] [Google Scholar]
- 26.Devillers A, Hall JI.. Rank 3 latin square designs. J Combinatorial Theory Series 2006;113(5):894–902. doi: 10.1016/j.jcta.2005.06.004 [DOI] [Google Scholar]
- 27.Borg G. Borg's perceived exertion and pain scales. Champaign, IL, Human Kinetics, 1998, p. 39. [Google Scholar]
- 28.Hardy CJ, Rejeski WJ.. Not what, but how one feels: the measurement of affect during exercise. J Sport Exerc Psychol 1989;11:304–17. doi: 10.1123/jsep.11.3.304 [DOI] [Google Scholar]
- 29.Stanley DM, Williams SE, Cumming J.. Preliminary validation of a single-item measure of exercise enjoyment: the exercise enjoyment scale. J Sport Exerc Psychol 2009;31:S138–9. [Google Scholar]
- 30.Kendzierski D, DeCarlo KJ.. Physical activity enjoyment scale: two validation studies. J Sport Exerc Psychol 1991;13(1):50–64. doi: 10.1123/jsep.13.1.50 [DOI] [Google Scholar]
- 31.Gosselin LE, Kozlowski KF, DeVinney-Boymel L, Hambridge C.. Metabolic response of different high-intensity aerobic interval exercise protocols. J Str Cond Res 2012;26(10):2866–71. doi: 10.1519/JSC.0b013e318241e13d [DOI] [PubMed] [Google Scholar]
- 32.Martinez N, Kilpatrick MW, Salomon K, Jung ME, Little JP.. Affective and enjoyment responses to high-intensity interval training in overweight-to-obese and insufficiently active adults. J Sport Exerc Psych 2015;37(2):138–49. doi: 10.1123/jsep.2014-0212 [DOI] [PubMed] [Google Scholar]
- 33.Hasnan N, Ektas N, Tanhoffer AIP, Tanhoffer R, Fornusek C, Middleton JW, et al Exercise responses during functional electrical stimulation cycling in individuals with spinal cord injury. Med Sci Sports Exerc 2013;45(6):1131–8. doi: 10.1249/MSS.0b013e3182805d5a [DOI] [PubMed] [Google Scholar]
- 34.Mutton DL, Scremin AME, Barstow TJ, Scott MD, Kunkel CF, Cagle TG.. Physiologic responses during functional electrical stimulation leg cycling and hybrid exercise in spinal cord injured subjects. Arch Phys Med Rehabil 1997;78(7):712–8. doi: 10.1016/S0003-9993(97)90078-2 [DOI] [PubMed] [Google Scholar]
- 35.Oliveira BRR, Slama FA, Deslandes AC, Furtado ES, Santos TM.. Continuous and high-intensity interval training: which promotes higher pleasure? PLoS One 2013;8(11):e79965. doi: 10.1371/journal.pone.0079965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gamerale F. Perceived exertion, heart rate, oxygen uptake and blood lactate in different work operations. Ergonomics 1972;15(5):545–54. doi: 10.1080/00140137208924456 [DOI] [PubMed] [Google Scholar]
- 37.Pandolf KB, Billings DS, Drolet LL, Pimental NA, Sawka MN.. Differential ratings of perceived exertion and various physiological responses during prolonged upper and lower body exercise. Eur J Appl Physiol Occup Physiol 1984;53(1):5–11. doi: 10.1007/BF00964681 [DOI] [PubMed] [Google Scholar]
- 38.Haisma JA, van der Woude LVH, Stam HJ, Bergen MP, Sluis TAR, Bussmann JBJ.. Physical capacity in wheelchair-dependent persons with a spinal cord injury: a critical review of the literature. Spinal Cord 2006;44(11):642–52. doi: 10.1038/sj.sc.3101915 [DOI] [PubMed] [Google Scholar]
- 39.Helgerud J, Hoydal K, Wang E, Karlsen T, Berg P, Bjerkaas M, et al Aerobic high-intensity intervals improve VO2max more than moderate training. Med Sci Sports Exerc 2007;39(4):665–71. doi: 10.1249/mss.0b013e3180304570 [DOI] [PubMed] [Google Scholar]


