Abstract
Objectives
To evaluate acute effects of glossopharyngeal insufflation (GI) on lung function, airway pressure (Paw), blood pressure and heart rate (HR) in people with cervical spinal cord injury (CSCI).
Design
Case-control design.
Setting
Karolinska Institutet, Stockholm, Sweden.
Participants
Ten participants with CSCI suffering from lesions between C4 and C8, and ASIA classification of A or B were recruited. Ten healthy particpants familiar with GI were recruited as a reference group.
Outcome measures
Spirometry, mean arterial blood pressure (MAP), Paw, and HR were measured in a sitting and a supine position before, during, and after GI.
Results
GI in the study group in a sitting position increased total lung capacity (TLC) by 712 ml: P < 0.001, vital capacity (VC) by 587 ml: P < 0.0001, Paw by 13 cm H2O: P < 0.01, and HR by 10 beats/min: P < 0.001. MAP decreased by 25 mmHg, P < 0.0001. Significant differences were observed between groups comparing baseline with GI. The reference group had a higher increase in; TLC (P < 0.01), VC (P < 0.001), Paw (P < 0.001) and HR (P < 0.05) and a higher decrease in MAP (P < 0.001). With GI in a sitting compared to a supine position, TLC, MAP, HR, Paw remained unchanged in the study group, while residual volume decreased in the supine position (P < 0.01).
Conclusion
There was a difference between the groups in the increase in TLC; VC; Paw, HR and in the decrease in MAP with GI, however MAP, HR and Paw responded in similar way in both groups in a sitting as well as a supine position. If performed correctly, the risks of GI resulting in clinically significant hemodynamic changes is low, although syncope may still occur.
Keywords: Airway pressure, Blood pressure, Glossopharyngeal breathing, Lung function, Physiotherapy
Introduction
People with cervical spinal cord injury (CSCI) usually have weak respiratory muscles which leads to reduced inspiratory capacity.1 Vital capacity (VC) decreases due to the weak respiratory muscles, which also makes the lungs and thorax more restricted.1,2
People with CSCI generate lower intrathoracic and expiratory pressure compared to healthy individuals, which reduces the cough efficiency. The reduced ability to cough and clear pulmonary secretions effectively leads to reduced airway clearance. As a result of this, atelectasis, retention of secretions, infection, and impaired gas exchange may develop.3
The higher cervical and more complete level of an injury, the greater the respiratory muscle impairment.4 As a consequence of these respiratory abnormalities, pulmonary complications are among the most common causes of mortality and morbidity.5
Glossopharyngeal insufflation (GI) is an alternative breathing technique used by patients with reduced lung volumes in order to maintain adequate ventilation, maintain thoracic range of motion and improve cough function when respiratory muscles are weak.6,7 The technique is also commonly used by competitive breath-hold divers to increase their lung volume above total lung capacity (TLC) before dives, thereby improving diving performance.8
Previous studies have described the mechanics and pointed out the risks involved when performing glossopharyngeal breathing.9,10 During glossopharyngeal breathing, high intrathoracic pressure may develop with a concurrent depressant effect on the arterial pressure. This will have a similar effect to a valsalva manoeuvre, where a person voluntarily strains to increase the intrathoracic pressure, which may cause orthostatic syncope from the reduction in venous return.11 Many reports have shown that significant hemodynamic abnormalities occur during glossopharyngeal breathing. Arterial blood pressure falls, and heart rate (HR) increases in healthy individuals.11,12 In a study by Loring et al.,13 the transpulmonary pressures increased up to 80 cm of H2O with glossopharyngeal breathing, and the intrapulmonary pressures increased up to 109 of cm H2O. Those results indicated that some healthy individuals are able to withstand repeated insufflations to transpulmonary pressures higher than within normal range of pressure. Autonomic dysreflexia has been shown to occur in patients with CSCI,14 and it is possible that these patients may be more susceptible to reduction in blood pressure during GI compared to healthy people.
Previous studies have reported cases where participants suffered from lightheadedness and fainting while performing GI. In a study by Nygren-Bonnier et al.,15 the participants with CSCI had occasional symptoms during GI such as dizziness, increased tightening of the chest, localized numbness, and fainting (syncope). Only a few studies have investigated the risks with GI among patients, and those studies only include patients with poliomyelitis and CSCI.15,16 To our knowledge, there are no studies that have compared patients with decreased lung volume to individuals with normal lung volumes, and the effects of GI on lung function, blood pressure and airway pressure. Data on the difference between a sitting and a supine position with GI is also lacking. The potential benefits with GI depend on filling gas volume in the lungs, despite limitations due to the reduction in blood pressure. While the pulmonary mechanics will differ slightly in supine versus upright position, the former will have a positive effect on venous return, possibly increasing the ability to maintain blood pressure. We hypothesized that patients would be able to fill larger volumes of air into the lungs in the supine position compared to a sitting position. We also hypothesized that the differences in a sitting versus a supine position would generate similar reactions in airway pressure and blood pressure in both patients and the healthy controls, i.e. dysreflexia would not be an issue in this maneuver.
The aim of this study was to evaluate the effects of GI on lung function, blood pressure, heart rate (HR), and airway pressure (Paw), pressure against pressure sensor with relaxed thorax) in a sitting and a supine position in patients with CSCI, and to compare the effects with a reference group of competitive and recreational breath-hold divers that regularly use GI to improve performance.
Methods
Participants
Participants from a previous study on GI and training were asked to participate.15 The inclusion criteria were as follows: spinal cord injury with a lesion between the levels of C4 and C8, time between injury and inclusion at least 1 year, an American Spinal Injury Association17 impairment classification of A, B or C, ventilatory independent, 18–70 years of age, and familiar with and able to perform GI. Exclusion criteria were chronic obstructive pulmonary disease and symptomatic infection characterized by fever. Out of 20 eligible participants 11 accepted to participate, one of which was excluded due to inability to follow the study protocol. Finally 10 participants entered the study; 9 men and 1 woman (mean age 42.5 year, range 24–64 year, mean height 176.4 cm, range 150–189 cm, mean weight 62.6 kg, range 45–73 kg, and mean years of injury 20.5 year, range 5–42 years). They had spinal cord injuries with lesions between the levels of C5 and C8, an American Spinal Injury Association impairment classification of A or B (C5 AISB: 1 participant, C6 AISA: 5 participants, C6 AISB: 2 participants, C7 AIS B: 1 participant, C8 AISB:1 participant). As a reference group of healthy participants able to perform GI, breath-hold divers in the same geographical area were included from a previous study.9 The inclusion criteria for this group were; healthy, 18–70 years of age, normal lung volume, and familiar with and able to perform GI. The study was conducted in conformity with the principles of the Declaration of Helsinki and was approved by the Central Ethical Review Board in Stockholm. All participants gave their written informed consent before participation.
Procedure
GI is a technique that is performed by using the muscles of the mouth, cheeks, lips, tongue, soft palate, larynx, and pharynx to piston boluses of air into the lungs. In glossopharyngeal breathing, the patients first perform a TLC maneuver and then beyond that, they perform cycles of as many gulps of air as possible, followed by the relaxing of the larynx and passive expulsion of the air.6,15,16 All measurements were performed by two test leaders. Measurements were performed before, during, and after performing cycles of maximal GI first in a sitting position, and thereafter before and during maximal cycles of GI in a supine position. The participants first carried out a maximal inhalation, then performed GI using as many gulps of air as possible without the onset of discomfort.15 Immediately following GI, the participants opened their airways while relaxing the thorax, against a small mouthpiece from which mouth airway pressure (Paw) was obtained. A moment later, the pressure was released and the participant exhaled to RV in order to measure the VC. At the end of the expiration, a valve was opened to an anaesthetic bag pre-filled with 3 litres of pure dry oxygen, which the participants re-breathed until nitrogen was equilibrated. This allowed their RV to be determined by the nitrogen dilution method (inert gas was calculated as 1-(FO2+FCO2), corrected for H2O). All participants performed GI through the mouth. Lung function, MAP, Paw, and HR were measured simultaneously while performing GI. Each participant performed the procedure three times, in a sitting position at baseline, in a sitting position with GI, in a supine position with GI, and finally in a sitting position after the intervention. The best of three values were used in the analysis.
Measurements
Spirometry was carried out using the nitrogen washout method. A pressure detector analyzer (SPD102DAHyb, Smartec BV, Breda, The Netherlands), partial pressure of carbon dioxide (PCO2), and partial pressure of oxygen (PO2) (Datex Capnomac Ultima, Datex-Engstrom Division, Instrumentarium Corp., Datex-Engstrom, Finland) was calibrated against mixtures of known concentration (AGA Gas AB, Lidingö, Sweden). The expired air volume was measured with a heated (37°C) pneumotachometer (Hans Rudolph model 3700, Hans Rudolph heater control, Hans Rudolf, Inc., Shawnee, KS, USA) connected to a differential pressure transmitter (Sanborn 270, Sanborn Co, Wallham, MT, USA) and amplifier (311A Tranducer amplifier-indicator;Hewlett Packard, Palo Alto, CA, USA). Calibration of the volume measurement took place prior to every trial with a 3 litre Hans Rudolph calibration syringe, and the pressure detector was calibrated against a water column. Mean arterial blood pressure (MAP) was measured continuously with a photoplethysmographic finger-cuff device (Finapres 2300, Ohmeda, Englewood, CO, USA). Pulse pressure and MAP was calculated as: systolic – diastolic = pulse pressure. Pulse pressure/3 + diastolic = MAP (10). A pressure transducer connected to the mouthpiece measured Paw in cmH2O. Heart rate was measured with 3-lead ECG. Analogue signals were sampled at 200 Hz by using an A/D converter (MP150 BioPac Systems, Inc., Goleta, CA, USA), stored in a personal computer and subsequently analyzed by Acqknowledge 3.7.3 software (Biopac Systems Inc., Goleta, CA, USA).
Statistical analysis
Descriptive statistics are presented as mean ± one standard deviation and/or median and range. Repeated measure ANOVA was used to analyze the overall change between the two groups, and between baseline and with GI, both in a sitting and supine position. Any differences between baseline and with GI values, as well as between groups and between a sitting and supine position were assessed using Student's paired and unpaired t-test, after the repeated measure ANOVA. For correlations, Pearson's correlation was used. A statistical significance was set at P < 0.05. STATISTICA software (10.0, Dell Software Inc, Tulsa, OK, USA) was used for all analyses.
Results
Sitting position
The participants in the study group increased the following variables significantly in a sitting position with GI: TLC: 712 ml, P < 0.001, VC: 587 ml, P < 0.0001, Paw: 13 cm H2O, P < 0.01, HR: 10 beats/min P < 0.0001 (Table 1). MAP with GI decreased with 25 mmHg, P < 0.001 (Table 1). There was no difference in RV. A strong correlation was observed regarding the difference in TLC and the difference in Paw, r = 0.81, P < 0.01) (Fig. 1), and a moderate correlation regarding the increase in TLC and the increase in HR r = 0.69, P < 0.05 (Fig. 2). There were no significant differences after the intervention with GI in a sitting position in any of the variables.
Table 1.
Lung function, airway pressure, blood pressure and heart rate at baseline and with Glossopharyngeal Insufflation (GI) in a sitting position.
| Study group at baseline | Study group with GI | P-valuea | Reference group at baseline | Reference group with GI | P-valueb | P-valuec | P-valued | |
|---|---|---|---|---|---|---|---|---|
| TLC (ml) | 5787±1473 | 6499±1476 | 0.001 | 7889±1161 | 9461±1391 | 0.00001 | 0.002 | 0.002 |
| VC (ml) | 2988±1014 | 3575±984 | 0.00008 | 5966±941 | 7480±1211 | 0.00005 | 0.000002 | 0.0007 |
| RV (ml) | 2790±856 | 2925±861 | 0.27 | 1923±382 | 1981±384 | 0.40 | 0.01 | 0.57 |
| Paw (cmH2O) | 27±6 | 40±13 | 0.005 | 37±9 | 74±21 | 0.00002 | 0.007 | 0.0007 |
| MAP (mmHG) | 85±16 | 60±18 | 0.00002 | 102±18 | 59±14 | 0.00000 | 0.04 | 0.001 |
| Heart rate (beats/min) | 67±15 | 77±16 | 0.0009 | 74±15 | 102±24 | 0.003 | 0.29 | 0.03 |
TLC, total lung capacity; VC, vital capacity; RV, residual volume; Paw, airway pressure; MAP, mean arterial blood pressure.
aWithin study group.
bWithin reference group.
cBetween groups at baseline.
dBetween baseline and with GI between groups.
Figure 1.
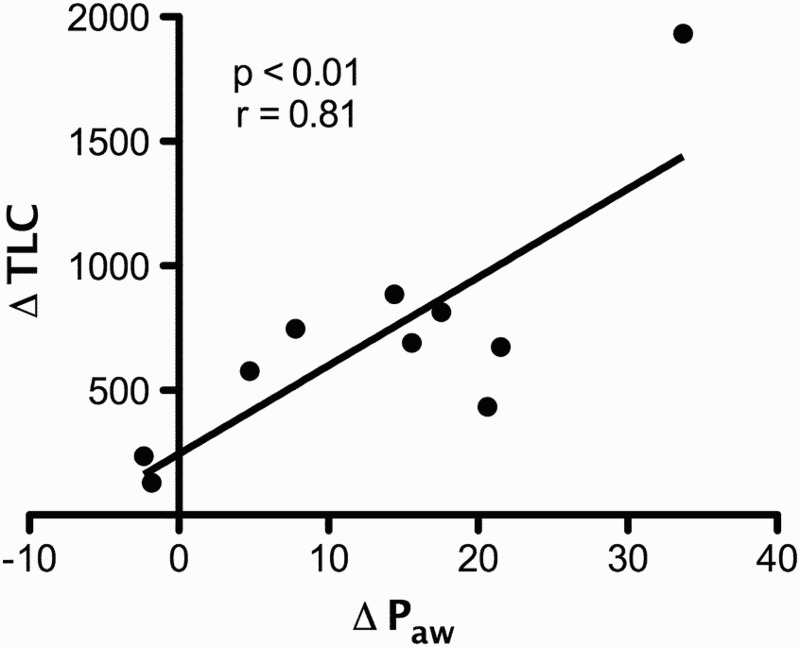
Correlation in the study group in a sitting position between difference in total lung capacity (TLC) and difference in relaxed airway pressure (Paw), r = 0,81, P < 0.01.
Figure 2.
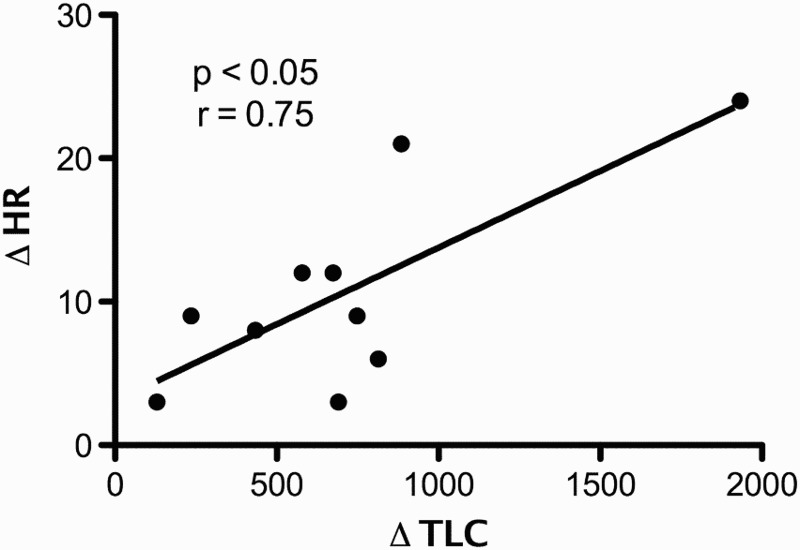
Correlation in the study group in a sitting position between difference in total lung capacity (TLC) and difference in heart rate (HR), r = 0,75, P < 0.05.
The study group and the reference group differed at baseline in the following variables: TLC, VC, RV, Paw, and MAP (Table 1). There was no difference in HR at baseline. In a sitting position there was significant difference between the groups at baseline compared with GI. The reference group had a higher increase in; TLC (P < 0.01), VC (P < 0.001), Paw (P < 0.001) and HR (P < 0.05) MAP (P < 0.001) (Table 1 and Fig. 3B), Paw (P < 0.001) and HR (P < 0.05) and a higher decrease in MAP (P < 0.001) (Table 1 and Fig. 3C). There was no difference in RV between the groups.
Figure 3.
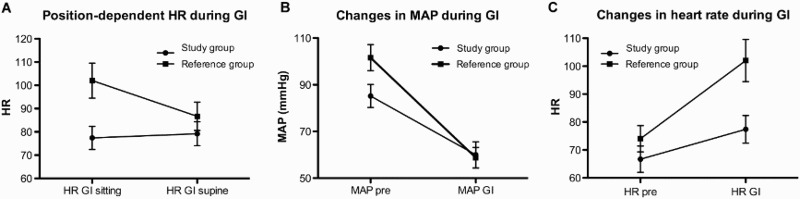
A Difference between the study- and reference group in position-dependent heart rate (HR) during glossopharyngeal insufflations (GI), P < 0.003. B Difference between the study- and reference group in changes in mean arterial pressure (MAP) during GI in a sitting position, P < 0.001. C Difference between the study group and the reference group in changes in HR during GI in a sitting position, P < 0.03.
Supine position
While performing GI in a sitting compared to a supine position, TLC, MAP, HR, and Paw remained unchanged in the study group whereas RV increased significantly in a sitting position, P < 0.01 (Table 2). The difference in RV a sitting compared to a supine position also differed between the groups, P < 0.01 (Table 2). The reference group had a higher HR in a sitting position compared to the study group, (P < 0.01) (Table 2 and Fig. 3A).
Table 2.
Lung function, airway pressure, blood pressure and heart rate at baseline and with Glossopharyngeal Insufflation (GI) in a sitting and supine position.
| Variables | Study group sitting | Study group supine | P-valuea | Reference group sitting | Reference group supine | P-valueb | P-valuec |
|---|---|---|---|---|---|---|---|
| TLC (ml) | 6499±1476 | 6394±1551 | 0.62 | 9461±1391 | 9532±1572 | 0.44 | 0.44 |
| VC (ml) | 3575±984 | 3863±1175 | 0.24 | 7480±1211 | 7597±1310 | 0.27 | 0.50 |
| RV (ml) | 2925±861 | 2532±790 | 0.007 | 1981±384 | 1935±378 | 0.45 | 0.01 |
| Paw (cmH2O) | 40±13 | 45±23 | 0.26 | 74±21 | 73±19 | 0.73 | 0.24 |
| MAP (mmHG) | 60±18 | 60±10 | 0.96 | 59±14 | 50±10 | 0.07 | 0.26 |
| Heart rate (beats/min) | 77±16 | 79±16 | 0.65 | 102±24 | 87±19 | 0.0005 | 0.003 |
TLC, total lung capacity; VC, vital capacity; RV, residual volume; Paw, airway pressure; MAP, mean arterial blood pressure.
aWithin study group.
bWithin reference group.
cDifference compring sitting and supine between groups.
Discussion
The principal finding was that participants with CSCI and a healthy reference group had similar reactions to the increase in intrathoracic pressure caused by GI, with decreased MAP and increased HR.
As shown in a previous study,15 the participants with CSCI in the present study were able to increase their lung volumes (VC and TLC) approximately 600–700 ml (11–16%) while performing GI. Other studies have shown that the VC can increase with a range of 22–39% with GI.6,8,9,15 The increase in Paw (33%) and HR (14%), and decrease in MAP (42%) were also in accordance with other studies9,15 and similar to the reference group.
None of the groups showed any difference in RV with GI, but the study group had a higher RV at baseline than the reference group. There was also a difference in RV with GI between a sitting and a supine position; the study group had a higher RV in a sitting position. This indicates that the participants with CSCI are more able to empty their lungs in a supine position, which is in accordance with other studies about the paradoxical effect of postural position on lung function for this group of patients.18
The correlation between TLC and Paw shows that the airway pressure increases along with the increasing volume of air during GI. This is previously shown by Schiffer and Lindholm9 in breath-hold divers. Increased airway pressure may pose a risk for developing arterial gas embolism while performing GI.9,19 However, this is probably of more importance in healthy individuals who deliberately overfill their lungs in order to improve diving performance, than it is to patients with decreased lung volumes with the purpose to normalize lung volume.
The reference group obtained a bigger difference in MAP and HR while performing GI, compared to the study group. However, the important result was that both groups responded the same way, and that the participants with CSCI seemed to tolerate the effects of GI in the same way as healthy breath-hold divers.
The study group had no difference in HR between a sitting and a supine position compared to the reference group, where HR decreased from a sitting to a supine position with GI. This could be due to the autonomic dysfunction that the blood pressure and HR do not respond in the same way as in healthy individuals.20
The MAP decreased during GI. However, the decrease was just temporary and restored when breathing normal again. Other studies have shown similar results, but in another group of participants. Novalija et al.12 (21) showed a decrease in MAP of 48% in breath-hold divers.
Collier et al. have also shown that the arterial blood pressure dropped in patients with reduced respiratory muscle function when they performed glossopharyngeal breathing.16 A study by Dzamonja et al.10 showed that breath-hold divers who performed GI achieved a higher intrathoracic pressure during GI, which impedes the venous return to the heart and leads to a reduction in stroke volume and blood pressure. This is most likely the main contributor to the decreased blood pressure during GI among the participants in this study. None of the participants showed any symptoms of autonomous dysreflexia, and the monitoring of the blood pressure during GI did not indicate any risk of that.
One of the participants suffered from syncope during GI, which has been reported earlier,15 and is considered to be caused by the reduction in preload as a result of the increased intrathoracic pressure when performing GI. Syncope during GI appears to pose a greater risk to persons with a lower basal MAP, whereas the risk of developing AGE seems to be greater to persons with higher basal MAP.9 It is therefore important to inform the participants to be aware of this, and if necessary perform GI in a supine position. It is especially important for people with CSCI if they have reduced ability to regulate peripheral resistance to maintain blood pressure and also HR.20
The technique of GI can vary among the participants and thereby affect the lung volumes. However, the participants were recruited from a previous training study of GI and therefore the technique of the participants in the present study should be considered as good.
Implications
The results in this study can be used to improve and adjust the instructions and dose of GI. The response in MAP and HR were similar in the healthy individuals, and therefore GI seems to also be tolerated well by people with CSCI. However, considering symptoms and also the episodes of fainting, GI must be learned properly in a clinical setting by an educated instructor in order to limit the risks.
Conclusion
All participants in the study group increased their TLC, Paw and pulse with GI. MAP decreased during GI. There was a difference between the groups in all variables except RV with GI in a sitting position. However even though there was a difference in the increase in TLC; VC; Paw, HR or decrease in MAP with GI, blood pressure and heart rate responded in the same way in both groups, in a sitting as well as a supine position. If performed with good technique, the risks of GI regarding changes in lung function, circulation, and airway pressure can be considered low for individuals with CSCI, although syncope may still occur.
Disclaimer statements
Contributors None.
Funding This study was supported by The Swedish Association for Survivors of Accident and Injury, The Swedish Association of Persons with Neurological Disabilities.
Conflict of interest None.
Ethics approval The study was approved by the Central Ethical Review Board in Stockholm.
ORCID
Malin Nygren-Bonnier http://orcid.org/0000-0001-6731-8468
Peter Lindholm http://orcid.org/0000-0002-0840-9244
References
- 1.Scanlon PD, Loring SH, Pichurko BM, McCool FD, Slutsky AS, Sarkarati M, et al. Respiratory mechanics in acute quadriplegia. Lung and chest wall compliance and dimensional changes during respiratory maneuvers. Am Rev Respir Dis 1989;139(3):615–20. doi: 10.1164/ajrccm/139.3.615 [DOI] [PubMed] [Google Scholar]
- 2.Estenne M, De Troyer A.. Relationship between respiratory muscle electromyogram and rib cage motion in tetraplegia. Am Rev Respir Dis 1985;132(1):53–9. [DOI] [PubMed] [Google Scholar]
- 3.Brown R, DiMarco AF, Hoit JD, Garshick E.. Respiratory dysfunction and management in spinal cord injury. Respir Care 2006;51(8):853–68; discussion 869–70. [PMC free article] [PubMed] [Google Scholar]
- 4.Baydur A, Adkins RH, Milic-Emili J.. Lung mechanics in individuals with spinal cord injury: effects of injury level and posture. J Appl Physiol 2001;90(2):405–11. [DOI] [PubMed] [Google Scholar]
- 5.DeVivo MJ, Krause JS, Lammertse DP.. Recent trends in mortality and causes of death among persons with spinal cord injury. Arch Phys Med Rehabil 1999;80(11):1411–9. doi: 10.1016/S0003-9993(99)90252-6 [DOI] [PubMed] [Google Scholar]
- 6.Dail CW, Affeldt JE, Collier CR.. Clinical aspects of glossopharyngeal breathing; report of use by one hundred postpoliomyelitic patients. JAMA 1955;158(6):445–9. doi: 10.1001/jama.1955.02960060003002 [DOI] [PubMed] [Google Scholar]
- 7.Bach JR, Alba AS, Bodofsky E, Curran FJ, Schultheiss M.. Glossopharyngeal breathing and noninvasive aids in the management of post-polio respiratory insufficiency. Birth Defects Orig Artic Ser 1987;23(4):99–113. [PubMed] [Google Scholar]
- 8.Lindholm P, Nyren S.. Studies on inspiratory and expiratory glossopharyngeal breathing in breath-hold divers employing magnetic resonance imaging and spirometry. Eur J Appl Physiol 2005;94(5–6):646–51. doi: 10.1007/s00421-005-1358-8 [DOI] [PubMed] [Google Scholar]
- 9.Schiffer TA, Lindholm P.. Transient ischemic attacks from arterial gas embolism induced by glossopharyngeal insufflation and a possible method to identify individuals at risk. Eur J Appl Physiol 2013;113(3):803–10. doi: 10.1007/s00421-012-2494-6 [DOI] [PubMed] [Google Scholar]
- 10.Dzamonja G, Tank J, Heusser K, Palada I, Valic Z, Bakovic D, et al. Glossopharyngeal insufflation induces cardioinhibitory syncope in apnea divers. Clin Auton Res 2010;20(6):381–4. doi: 10.1007/s10286-010-0075-5 [DOI] [PubMed] [Google Scholar]
- 11.Potkin R, Cheng V, Siegel R.. Effects of glossopharyngeal insufflation on cardiac function: an echocardiographic study in elite breath-hold divers. J Appl Physiol 2007;103(3):823–7. doi: 10.1152/japplphysiol.00125.2007 [DOI] [PubMed] [Google Scholar]
- 12.Novalija J, Lindholm P, Loring SH, Diaz E, Fox JA, Ferrigno M.. Cardiovascular aspects of glossopharyngeal insufflation and exsufflation. Undersea Hyperb Med 2007;34(6):415–23. [PubMed] [Google Scholar]
- 13.Loring SH, O'Donnell CR, Butler JP, Lindholm P, Jacobson F, Ferrigno M.. Transpulmonary pressures and lung mechanics with glossopharyngeal insufflation and exsufflation beyond normal lung volumes in competitive breath-hold divers. J Appl Physiol 2007;102(3):841–6. doi: 10.1152/japplphysiol.00749.2006 [DOI] [PubMed] [Google Scholar]
- 14.Vaidyanathan S, Soni BM, Sett P, Watt JW, Oo T, Bingley J.. Pathophysiology of autonomic dysreflexia: long-term treatment with terazosin in adult and paediatric spinal cord injury patients manifesting recurrent dysreflexic episodes. Spinal Cord 1998;36 (11):761–770. doi: 10.1038/sj.sc.3100680 [DOI] [PubMed] [Google Scholar]
- 15.Nygren-Bonnier M, Wahman K, Lindholm P, Markström A, Westgren N, Klefbeck B.. Glossopharyngeal pistoning for lung insufflation in people with cervical spinal cord injury. Spinal Cord. 2009;47(5):418–22. doi: 10.1038/sc.2008.138 [DOI] [PubMed] [Google Scholar]
- 16.Collier CR, Dail CW, Affeldt JE.. Mechanics of glossopharyngeal breathing. J Appl Physiol 1956;8(6):580–4. [DOI] [PubMed] [Google Scholar]
- 17.Maynard FM Jr, Bracken MB, Creasey G, Ditunno JF Jr, Donovan WH, Ducker TB, et al. International standards for neurological and functional classification of spinal cord injury. American spinal injury association. Spinal Cord 1997;35(5):266–274. [DOI] [PubMed] [Google Scholar]
- 18.Estenne M and De Troyer A.. Mechanism of the postural dependence of vital capacity in tetraplegic subjects. Am Rev Respir Dis 1987;135(29):367–71. [DOI] [PubMed] [Google Scholar]
- 19.Linér MH, Andersson JP.. Suspected arterial gas embolism after glossopharyngeal insufflation in a breath-hold diver. Aviat Space Environ Med 2010;81(1):74–6. doi: 10.3357/ASEM.2571.2010 [DOI] [PubMed] [Google Scholar]
- 20.Dallmeijer AJ, Hopman MT, van As HH, van der Woude LH.. Physical capacity and physical strain in persons with tetraplegia; the role of sport activity. Spinal Cord. 1996;34(12):729–35. doi: 10.1038/sc.1996.133 [DOI] [PubMed] [Google Scholar]


