Introduction
More people than ever before are living into old age. The increased longevity is partly due to the increased use of medicines. Despite the potential benefits of medicines, they can still cause significant harm. Medication-related harm (MRH) may be from adverse drug reactions or harm from inappropriate drug use, for example, nonadherence or medication error. The European Commission estimated in 2008 that MRH contribute to at least 100,800 deaths in member states annually and costs society €79 billion.1 Older adults are most at risk due to their high exposure to medicines and age-related pharmacokinetic and pharmacodynamic changes. A recent systematic review found that 1 in 10 hospitalized older adults are admitted due to MRH, and approximately the same proportion experience MRH as an inpatient.2 Avoidable health service use due to MRH is substantial. A study in the Netherlands estimated the average cost of an avoidable MRH hospitalization in an older adult at €5500.3
Top-down interventions to reduce MRH and unplanned admissions, such as pharmacist-led medicines review, have shown limited effectiveness. There is a need to consider a bottom-up approach, exploring patient-centred modifiable determinants. Health literacy is one such determinant that is being explored in relation to MRH. A survey of eight countries in the European Union (EU) found that 30–60% of people are not health literate, with the older population representing a particularly high-risk group.4 A ‘mandate’ to enhance health literacy has been sent out to policy- makers in the 2016 World Health Organization (WHO) 9th Global Conference on Health Promotion. In this editorial we consider how health literacy can be conceptualized as a fundamental principle in reducing MRH in the older adult.
Conceptualizing health literacy in the older person
Health literacy is “the degree to which individuals have the capacity to obtain, process and understand basic health information and services needed to make appropriate health decisions”.5 Health literacy can be viewed both as an asset for health and wellbeing, and a risk factor for disease. Low health literacy develops from a range of negative determinants over time (at the individual, health system or environmental level) and their intersectionality. Health literacy operates in various patient encounters that influence health outcomes, from the immediate healthcare environment, for example, at a GP surgery to support a participatory consultation, to wider community settings, for example, purchasing over-the-counter medicine. From the patient perspective, health literacy influences the identification of a health issue, to access and navigation of the health system, subsequent communication within the health system and thereon, the ability to co-manage the resolution of a health issue.6
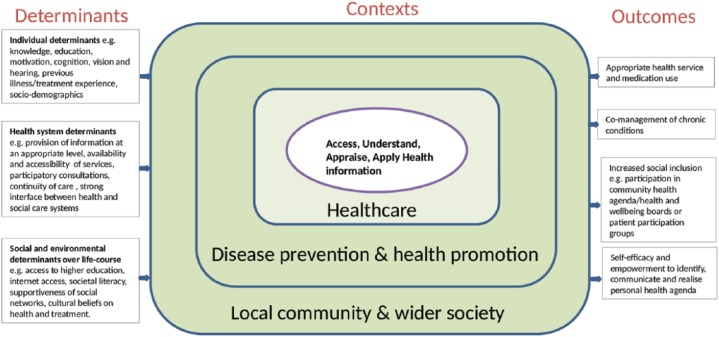
Figure 1 shows a simplified, adapted version of a conceptual model of health literacy7 in order to highlight pictorially some key determinants and outcomes of health literacy within the lived experience of an older person. One important health outcome is the appropriate use of medications.
Figure 1.
A conceptual model of the determinants, contexts and outcomes of health literacy in the older person (adapted from Sorensen et al, BMC Public Health 2012;12:80)
Health literacy: a modifiable determinant of MRH
Older patients identify a lack of knowledge about medicines and poor understanding of treatment aims as key problems related to medicines use.8 Low health literacy related to medicines utilization is a predictor of premature mortality in older adults, independent of cognition, comorbidities, education and socioeconomic status.9 In the English Longitudinal Study of Ageing, a 5-year follow up of 7500 older adults, participants answered four questions about the instructions on a packet of aspirin. One in two adults over the age of 80 years could not correctly answer all four questions. In this study, low health literacy (⩾ 2 errors) was independently associated with a 26% increased risk of mortality compared with those that fully understood the instructions for medication use (hazard ratio 1.26, confidence interval 1.03–1.56).
Low health literacy is associated with deprivation,4 an established risk factor for polypharmacy10 and hospitalization due to MRH.11 Low health literacy may be a critical mediator of this relationship,4 as it is strongly associated with reduced uptake of preventive healthcare, the incidence of chronic disease, lower participation in health-related decisions, and higher rates of unplanned health service utilization.12 Only one study has directly investigated the impact of low health literacy of older adults on the incidence of MRH.13 This prospective study of 310 retired US veterans followed up for 12 months showed a trend for low health literacy serving as a risk factor for adverse drug events. Whilst this relationship was not statistically significant, the authors postulated that the study was underpowered. The findings of this study should stimulate further investigation of this relationship in other healthcare systems and populations, and mapping of the causal pathways.
There is some evidence for a linear relationship between health literacy and medication adherence in older people,14 however, this relationship is inconsistent. The inconsistency might be explained by a ‘U-shaped’ relationship; those with lower health literacy tend to unintentionally nonadhere, and those with higher health literacy intentionally nonadhere.15 The capacity to self-manage and ‘intentionally’ nonadhere when encountering medication problems may indeed serve as a protective factor against the occurrence or exacerbation of harm. This aligns with the argument that health literacy is a pivotal empowerment strategy, enabling people to seek out information and increase autonomy over their health.16,17 Health literacy can additionally support greater patient involvement in medical decision making,18 enabling patients to critique decisions that they deem unsafe, whether this be misdiagnosis and/or inappropriate prescribing. This is of importance in the older population, where evidence for the use of many commonly prescribed medicines is lacking, especially in patients with multimorbidity.19 Engaging with a patient’s therapeutic preferences can provide a powerful counter-measure to polypharmacy provoked by guidelines focused on single-disease management. For instance, a qualitative exploration of the therapeutic priorities of older patients with both hypertension and risk of falls showed that patients with multimorbidity were significantly less likely to prioritize blood pressure reduction over an increased MRH risk from antihypertensive use.20
Addressing low health literacy
Health professionals working with older patients can use a single validated question to screen for low health literacy in the time-pressured clinical setting: “How confident are you filling out medical forms by yourself?”21 Answers are “extremely”, “quite a bit”, “somewhat”, “a little bit” or “not at all”. Those that respond “a little bit” or “not at all” are likely to have inadequate health literacy and can be supported with evidence-based measures.
The US-based Agency for Healthcare Research and Quality developed a ‘Universal Precautions Toolkit’, which describes several interventions that can be used in clinical practice to: (a) simplify communication and prevent miscommunication; (b) make the health system and environment easier to navigate; (c) empower individuals to self-manage their conditions.22 A key example of this is ‘teach-back’, which requires the clinician to ask the patient to repeat back in their own words the key information that has been provided and, if necessary, repeat the information for improving provider–patient communication. This has been shown in a randomized trial of emergency department care to significantly improve patient comprehension of discharge medications.23
Patients with low health literacy are more likely to find medication labelling confusing leading to misunderstanding of usage instructions. Drug dosing should be written explicitly, for example, replacing ‘three times a day’ with specific timings, and ensuring the drug name and dosage on medication labels are highlighted, underlined and printed in a large font.24 In areas with multi-ethnic communities, multilingual treatment instructions have been shown in a randomized trial to improve older adults understanding of instructions for medication usage, dosing and regimen consolidation.25 Other measures to support health literacy include alternative forms of information provision, for example, videos and clear face-to-face contact when consulting with a patient with hearing difficulty that might lip read.24
A successful example from the UK of patients themselves designing a health literacy intervention is the ‘My Medication Passport.’26 This is a pocket-sized booklet that supports patients in recording their medication list and related information in a way that is comprehensible for them. Evaluation of the patients’ experience with these passports showed that they supported their confidence to discuss their medicines with healthcare professionals, and to share medication-related information with family and carers.26
A recommendation from the EU-funded Intervention Research on Health Literacy among Ageing populations (IROHLA) is the development of e-health apps for tablets, designed with older users, which can be used to order medicines, give alerts on medicines intake and support adherence (www.irohla.eu). In time, these technologies could improve the integration of treatment, in real time, between multiple health providers and improve patient–provider communication through a shared e-platform of personalized medicines-related information.
In conclusion, health literacy has high face validity, and some empirical evidence, as a modifiable determinant of MRH in older adults. Whilst policy-makers respond to the WHO’s mandate for increasing health literacy at the population level, clinicians must be vigilant in their daily practice to the health literacy needs of their patients (and carers). Screening for low health literacy can be easily implemented in routine clinical settings, and should be used to target additional support with medicines. Patients with low health literacy are likely to benefit from closer review of their usage of medicines, encouragement to participate in medication-related decisions, and aids to increase their understanding of therapeutic aims and potential harms. Addressing low health literacy can provide an alternative, patient-centred approach for reducing MRH.
Contributor Information
Nikesh Parekh, Division of Medicine, Brighton and Sussex Medical School, Audrey Emerton Building, Eastern Road, Brighton, BN2 1EL, UK.
Khalid Ali, Division of Medicine, Brighton and Sussex Medical School, Brighton, UK.
Kevin Davies, Division of Medicine, Brighton and Sussex Medical School, Brighton, UK.
Chakravarthi Rajkumar, Division of Medicine, Brighton and Sussex Medical School, Brighton, UK.
References
- 1. European Commission. Proposal for a regulation amending, as regards pharmacovigilance of medicinal products for human use. Regulation (EC) No 726/2004. Impact assessment, https://ec.europa.eu/health//sites/health/files/files/pharmacos/pharmpack_12_2008/pharmacovigilance-ia-vol1_en.pdf (2008, accessed 29 August 2017).
- 2. Alhawassi M, Krass I, Bajorek V, et al. A systematic review of the prevalence and risk factors for adverse drug reactions in the elderly in the acute care setting. Clin Interv Aging 2014; 9: 2079–2086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Leendertse AJ, Van Den Bemt PM, Poolman JB, et al. Preventable hospital admissions related to medication (HARM): cost analysis of the HARM study. Value Health 2011; 14: 34–40. [DOI] [PubMed] [Google Scholar]
- 4. Sørensen K, Rgen J, Pelikan M, et al. Health literacy in Europe: comparative results of the European health literacy survey (HLS-EU). Eur J Public Health 2015; 25: 1053–1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nielsen-Bohlman L, Panzer AM, Kindig DA. (eds); Institute of Medicine. Health literacy: a prescription to end confusion. Washington, DC: National Academies Press, 2004, p. 32. [PubMed] [Google Scholar]
- 6. Jordan JE, Buchbinder R, Osborne RH. Conceptualising health literacy from the patient perspective. Patient Educ Couns 2010; 79:36–42. [DOI] [PubMed] [Google Scholar]
- 7. Sørensen K, Van Den Broucke S, Fullam J, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health 2012; 12: 80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mohammed MA, Moles RJ, Chen TF. Medication-related burden and patients’ lived experience with medicine: a systematic review and metasynthesis of qualitative studies. BMJ Open 2016; 6: e010035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bostock S, Steptoe A. Association between low functional health literacy and mortality in older adults: longitudinal cohort study. BMJ 2012; 344: e1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Guthrie B, Makubate B, Hernandez-Santiago V, et al. The rising tide of polypharmacy and drug-drug interactions: population database analysis 1995–2010. BMC Med 2015; 13: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. McKay AJ, Newson RB, Soljak M, et al. Are primary care factors associated with hospital episodes for adverse drug reactions? A national observational study. BMJ Open 2015; 5: e008130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Berkman ND, Sheridan SL, Donahue KE, et al. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med 2011; 155: 97–107. [DOI] [PubMed] [Google Scholar]
- 13. Mosher HJ, Lund BC, Kripalani S, et al. Association of health literacy with medication knowledge, adherence, and adverse drug events among elderly veterans. J Heal Commun 2012; 17(Suppl. 3): 241–251. [DOI] [PubMed] [Google Scholar]
- 14. Geboers B, Brainard JS, Loke YK, et al. The association of health literacy with adherence in older adults, and its role in interventions: a systematic meta-review. BMC Public Health 2015; 15: 903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lindquist LA, Go L, Fleisher J, et al. Relationship of health literacy to intentional and unintentional non-adherence of hospital discharge medications. J Gen Intern Med 2012; 27: 173–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Geboers B, de Winter AF, Spoorenberg SL, et al. The association between health literacy and self-management abilities in adults aged 75 and older, and its moderators. Qual Life Res 2016; 25: 2869–2877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bravo P, Edwards A, Barr PJ, et al. Conceptualising patient empowerment: a mixed methods study. BMC Health Serv Res 2015; 15: 252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Aboumatar HJ, Carson KA, Beach MC, et al. The impact of health literacy on desire for participation in healthcare, medical visit communication, and patient reported outcomes among patients with hypertension. J Gen Intern Med 2013; 28: 1469–1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Parekh N, Page A, Ali K, et al. A practical approach to the pharmacological management of hypertension in older people. Ther Adv Drug Saf 2017; 8: 117–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tinetti ME, McAvay GJ, Fried TR, et al. Health outcome priorities among competing cardiovascular, fall injury, and medication-related symptom outcomes. J Am Geriatr Soc 2008; 56:1409–1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Keene Woods N, Chesser AK. Validation of a single question health literacy screening tool for older adults. Gerontol Geriatr Med 2017; 3: e233372141771309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Brega AG, Barnard J, Mabachi NM, et al. , et al. AHRQ health literacy universal precautions toolkit. 2nd ed., https://www.ahrq.gov/professionals/quality-patient-safety/quality-resources/tools/literacy-toolkit/index.html (2015, accessed 10 July 2017).
- 23. Griffey RT, Shin N, Jones S, et al. The impact of teach-back on comprehension of discharge instructions and satisfaction among emergency patients with limited health literacy: a randomized, controlled study. J Commun Healthc 2015; 8: 10–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sudore RL, Schillinger D. Interventions to improve care for patients with limited health literacy. J Clin Outcomes Manag 2009; 16: 20–29. [PMC free article] [PubMed] [Google Scholar]
- 25. Bailey SC, Sarkar U, Chen AH, et al. Evaluation of language concordant, patient-centered drug label instructions. J Gen Intern Med 2012; 27: 1707–1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Barber S, Thakkar K, Marvin V, et al. Evaluation of my medication passport: a patient-completed aide-memoire designed by patients, for patients, to help towards medicines optimisation. BMJ Open 2014; 4: e005608. [DOI] [PMC free article] [PubMed] [Google Scholar]