Abstract
Background
Preterm birth is a major health problem in developing and developed countries leading to rising health care costs and long-term neurodevelopmental disability. The study aims to evaluate the role of new quantitative markers, like the elastography of cervix (shear wave speed estimation), fetal adrenal zone enlargement, and corrected fetal adrenal gland volume; in preterm birth prediction and analyze their relative importance. Thus, these markers may be beneficial in early preterm birth detection and prevent the related morbidities.
Methods
Thirty pregnant females (from 28 to 37 weeks of gestational age), showing clinical signs and delivery outcome of preterm birth were included in the study with an equal number of not-in-labor antenatal females at ≥37 weeks as controls. These patients were categorized as preterm and term groups. Both the groups were subjected to trans-abdominal ultrasonography where cervical length, cervical shear wave speed (dynamic elastography) and fetal adrenal gland parameters were measured.
Results
Shear wave speed estimation of the antenatal cervix showed the highest sensitivity and specificity (96.7% and 87% respectively) in the prediction of preterm birth and also showed a strong correlation with fetal adrenal gland enlargement. Fetal adrenal zone enlargement was also shown to be a reliable marker of preterm birth, however, with reduced sensitivity and specificity than shear wave speed.
Conclusion
The elastographic advancement and fetal adrenal biometry derived quantitative markers can be used as an objective and standard criterion for accurate prediction of preterm birth.
Keywords: Preterm birth, elastography, adrenal gland, tissue elasticity imaging, cervix
Introduction
Preterm birth (PTB) is defined as the onset of delivery prior to 37 completed weeks or 259 days of gestation but after the age of viability.1 The age of viability may range from 20 to 28 weeks2 and hence the definition varies in developed and developing countries. Based on the gestational age, those born below 28 weeks are termed extreme preterm and those above 32 weeks are late preterm. This study was conducted in a developing country with 28 weeks as the gestational age of viability.
Preterm labor (PTL) is a major health problem and one of the recent annual reports have estimated that 15 million babies are born preterm worldwide.3 The incidence varies from 5% to 18% across the globe reaching around 7.3% in the UK4 and 9.63% in the United States.3 About 85% of the worldwide cases of preterm birth are concentrated in Asia and Africa, comprising 54% and 31% respectively.1 Hence, increasing burden of disease and annual cost associated with care of preterm infants demanded a search for a new and reliable quantitative marker of preterm labor prediction.
Initiation of the process of parturition can be attributed to a complex interaction of various fetal and maternal hormonal pathways, which are primarily driven by the fetal hypothalamic-pituitary-adrenal (HPA) axis.5 The fetal zone of the adrenal gland plays a central role by producing dehydroepiandrosterone-sulfate (DHEA-S), which can be sonographically correlated to the adrenal gland and fetal zone enlargement (FZE).6 The end-process of all the pathways is cervical remodeling leading to cervical softening and ripening.7
This physiological cascade can be indirectly utilized for prediction of PTB by assessing the degree of adrenal gland enlargement and also estimating the softening/elasticity properties of the antenatal cervix.8 These quantitative markers have been studied in isolation previously but their comparison has not yet been performed. This study sought to test the significance and accuracy of fetal adrenal gland enlargement and cervical elastography in the prediction of PTB.
Material and methods
This was a prospective observational case-control study, approved by the institutional review board and conducted over a 10 month period. The study involved 30 pregnant women delivered between 28 and 37 weeks of gestational age due to clinically established PTL. An equal number (n = 30) of nonlaboring pregnant women at the gestational age ≥37 weeks were enrolled as controls. A written consent was taken from all the patients. Patients with advanced PTL (cervical dilatation ≥3 cm), multiple gestations, preeclampsia, eclampsia, previous history of cervical surgery (cerclage), polyhydramnios, oligohydramnios, diabetes mellitus, maternal heart disease, and fetal abnormalities incompatible with life were excluded from the study.
The diagnosis of PTL was based on clinical criteria of regular uterine contractions (>4 in 20 minutes or >8 in 60 minutes), each of duration more than 40 seconds and associated with cervical dilatation >1 cm and <3 cm.9 Premature rupture of membranes (PROM) and leaking of amniotic fluid was considered as PTL. These patients were classified as the preterm and controls as the term group. Next, all the patients were sent for obstetric ultrasonography (USG) within 24 hours of admission, where fetal biometry, fetal adrenal gland assessment, cervical length measurement, and elastography of cervix were done. All the measurements were performed trans-abdominally (TA). The examination was done on an Acuson S2000 diagnostic ultrasound system (Siemens Healthcare, Erlangen, Germany) with transducer frequencies of 3.5 MHz and 9–11 MHz.
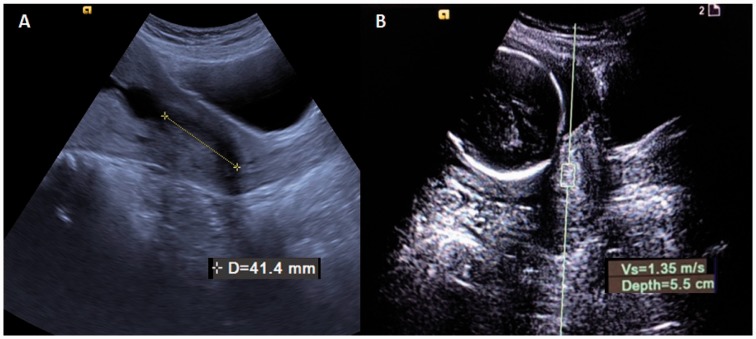
Sono-elastography of cervix
Standard obstetric USG was followed by the cervical length estimation using the same abdominal transducer. The cervix was focussed in the mid-sagittal plane and the length was measured from the internal to the external os (Figure 1(a)). The cervical elastographic assessment was also done on the same ultrasound system by the same radiologist (blinded to clinical diagnosis), using dynamic elastography based on acoustic radiation force impulse (ARFI) technique. This technique employed virtual touch tissue quantification (VTQ) elasticity model to generate shear wave speed (SWS) of a small block of the cervix. A rectangular box of size 10 × 6 mm2 was placed on the anterior wall close to the internal os (where depth from skin surface was <80 mm) and the software gives the SWS in meters per second (Figure1(b)). Average of the three measurements was charted for every patient to exclude measurement bias. The measurements were reproducible in all the cases where cervix could be visualized. There were only three cases where fetal head shadow completely obscured the internal os or cervix was too deep for the elastography box to reach and hence, were excluded and not counted in the study.
Figure 1.
Sono-elastographic images of the cervix on trans abdominal scan in the mid-sagittal plane: (a) measurement of cervical length and (b) elastography using VTQ technique and the rectangular box in the cervix for measurement of shear wave speed (in m/s).
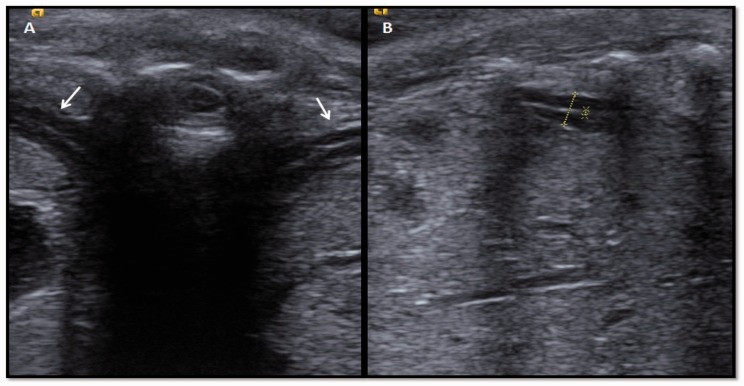
Fetal adrenal gland biometry
Fetal adrenal gland assessment was done by another radiologist (blinded to clinical and elastographic findings), on the same ultrasound system using linear array transducer of 9–11 MHz frequency and linear obstetrics preset. Fetal adrenals were focussed in the axial plane, by smoothly navigating the transducer cranially above the level of kidneys. The central hyperechoic part of the fetal adrenal gland (fetal zone) was measured in the sagittal or coronal plane (by 90° transducer rotation) along with the maximum dimension of the gland in the same plane (Figure 2), to give fetal zone depth (d) and total gland depth (D). The d/D ratio was charted as a percentage and called as a marker of fetal zone enlargement (FZE).10 The total gland dimensions were taken in three orthogonal planes and gland volume was estimated using the ellipsoid formula (a*b*c*0.52). This was further divided by the estimated fetal weight (EFW) in kilograms to yield corrected fetal adrenal gland volume (cAGV) in cubic millimeters per kilograms (mm3/kg). EFW was calculated automatically using Hadlock formula based on four common fetal measurements i.e. biparietal diameter (BPD), head circumference (HC), abdominal circumference (AC), and femur length (FL). These measurements were done on both adrenal glands; however, left-sided measurements were used due to its semilunar shape. In patients with increased abdominal fat, the fetal adrenals were assessed using a 3.5 MHz curvilinear probe.
Figure 2.
Sonography of fetal adrenal glands: (a) fetal adrenals (right and left) in trans-axial plane (white arrows); (b) showing fetal zone depth estimation of left adrenal gland in the coronal plane.
Statistical analysis
The clinical and sono-elastographic data was stored on separate spreadsheets for preterm and term groups using Microsoft Excel 2010 (Microsoft Corp., Redmond, WA, USA). All statistical analysis was done using SPSS Statistics software for Windows (Version 23.0. IBM Corp., Armonk, NY, USA). Normality of variables and homogeneity of variances was tested using the Shapiro–Wilk test and Levene’s test, respectively. Intergroup comparison of the test variables was done using Student’s t-test. Receiver operating characteristics (ROC) curve was designed for all the variables to determine their best predictive cut-off values. The level of statistical significance was determined at p < 0.05. Pearson ranked correlation coefficient was used to assess the relationship of SWS with FZE and cAGV for both the groups under study. The degree of agreement and proportional bias between the measurements of both adrenal glands were investigated using Bland–Altman and linear regression plots.
Results
The patient profile and sono-elastographic measures of both groups of patients are shown in Table 1. The age range of the preterm cohort was 22 to 32 years and that of the term was 22 to 34 years with mean age of 27 and 28 years respectively. Mean gestational age at the time of ultrasonography and at delivery was charted for both the groups, which showed the mean interval of nearly 2.0 weeks for preterm patients. Mean values of the continuous variables like SWS, cervical length, FZE and cAGV were tabulated as outcome measures in Table 1 and compared for statistical significance using Student’s t-test. The test revealed that preterm pregnant women had statistically significant lower shear wave speed (t(58) = −9.841, p < 0.001) than those delivered at term. The markers of fetal adrenal gland enlargement i.e. FZE and cAGV showed higher values in the preterm group than the term group and that too with statistical significance, FZE (t(58) = 4.807, p < 0.001) and cAGV (t(58) = 6.3431, p < 0.001).
Table 1.
Descriptive statistics of preterm and term groups
| Variables | Total (N = 60) | Preterm (N = 30) | Term (N = 30) | p-Valuea |
|---|---|---|---|---|
| Patient profile | ||||
| Age, y, mean (SD) | 27.57 (2.99) | 26.97 (2.56) | 28.17 (3.30) | 0.121 |
| Parity, median (range) | 1 (0–4) | 1 (0–4) | 0 (0–3) | NA |
| Gestational age at admission, weeks, mean (SD) | 35.1 (3.1) | 32.5 (2.3) | 37.5 (0.6) | <0.001* |
| History of preterm, n (%) | 21 (35) | 9 (30) | 12 (40) | NA |
| Presence of ROM, n (%) | 12 (20) | 7 (23.3) | 5 (16.7) | NA |
| Output | ||||
| Gestational age at delivery, weeks, mean (SD) | 36.2 (2.3) | 34.5 (2.0) | 38.0 (1.2) | <0.001* |
| Cervical length, cm, mean (SD) | 2.03 (0.37) | 1.98 (0.36) | 2.08 (0.37) | 0.299 |
| Shear wave speed, m/s, mean (SD) | 2.87 (.75) | 2.27 (0.42) | 3.45 (0.50) | <0.001* |
| Fetal zone enlargement, %, mean (SD) | 48.85 (4.07) | 51.43 (3.22) | 46.26 (3.08) | <0.001* |
| Corrected adrenal gland volume, mm3/kg, mean (SD) | 425.22 (58.17) | 456.02 (53.34) | 394.43 (45.58) | <0.001* |
SD: standard deviation; NA: not applied; ROM: rupture of membranes.
Comparison between preterm and term groups.
p < 0.05.
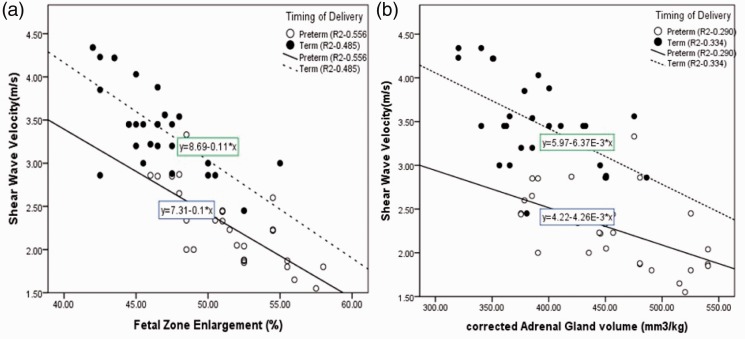
The correlation matrix (Table 2) between all the variables under study, showed a strong inverse relationship of SWS with FZE and cAGV (p < 0.05) in both the groups. Similar result pattern was demonstrated by group scatter plots (Figure 3), where the preterm cohort was showing lower SWS with higher FZE as well as cAGV. FZE and cAGV were positively correlated but showed significance only in the preterm cohort.
Table 2.
Correlation matrix in between test variables of both groups under study.
| Cervical length (cm) |
Shear wave speed (m/s) |
Corrected adrenal gland volume (mm3/kg) |
Fetal zone enlargement (%) |
|||||
|---|---|---|---|---|---|---|---|---|
| Variables | Preterm | Term | Preterm | Term | Preterm | Term | Preterm | Term |
| Cervical length (cm) | ||||||||
| r-value | 1 | 1 | −0.224 | 0.141 | 0.225 | −0.103 | 0.129 | 0.075 |
| p-value | 0.234 | 0.459 | 0.231 | 0.587 | 0.499 | 0.694 | ||
| Shear wave speed (m/s) | ||||||||
| r-value | −0.224 | 0.141 | 1 | 1 | −0.539** | −0.578** | −0.746** | −0.696** |
| p-value | 0.234 | 0.459 | 0.002 | 0.001 | 0.000 | 0.000 | ||
| Corrected adrenal gland volume (mm3/kg) | ||||||||
| r-value | 0.225 | −0.103 | −0.539** | −0.578** | 1 | 1 | 0.521** | 0.166 |
| p-value | 0.231 | 0.587 | 0.002 | 0.001 | 0.003 | 0.381 | ||
| Fetal zone enlargement (%) | ||||||||
| r-value | 0.129 | 0.075 | −0.746** | −0.696** | 0.521** | 0.166 | 1 | 1 |
| p-value | 0.499 | 0.694 | 0.000 | 0.000 | 0.003 | 0.381 | ||
r-value: Pearson’s correlation coefficient.
Correlation is significant at 0.05 level (2-tailed).
Figure 3.
Group scatter plots showing linear correlation of shear wave speed with FZE (a) and cAGV (b) in both preterm and term cohorts. Line of regression was shown with line formula, y = a + bx; R2 is regression coefficient.
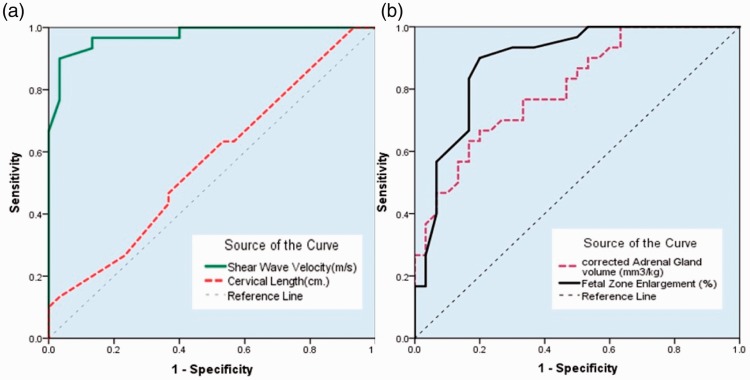
ROC curves were plotted (Figure 4) with Table 3 showing cut-off values of variables (derived from ROC curves) and their corresponding sensitivities and specificities. SWS at the cut-off value of 2.87 m/s showed the highest area under the curve, AUC (0.973), sensitivity (96.7%), and specificity (87%) for prediction of preterm birth. Fetal adrenal gland biometry also showed the significant AUC; however, FZE was more sensitive and specific than cAGV. The study revealed that fetal zone enlargement of approximately 50% of the total gland, correctly identifies the risk of preterm delivery in 90% of the patients.
Figure 4.
ROC curves of different variables in the prediction of timing of delivery/preterm labor: (a) ROC curve of shear wave speed and cervical length; (b) showing curves for fetal zone enlargement (FZE) and corrected adrenal gland volume (cAGV).
Table 3.
Sensitivity and specificity of the test variables at their ROC curve derived cut-offs
| Test variables | AUC | Cut-off value | Sensitivity | Specificity |
|---|---|---|---|---|
| Shear wave speed (m/s) | 0.973 | 2.87 | 96.7% | 87% |
| Cervical length (cm) | 0.569 | 2.0 | 63% | 47% |
| Fetal zone enlargement (%) | 0.887 | 47.7 | 90% | 80% |
| Corrected adrenal gland volume (mm3/kg) | 0.802 | 415 | 76% | 67% |
ROC: receiver operating characterstics; AUC: area under ROC curve.
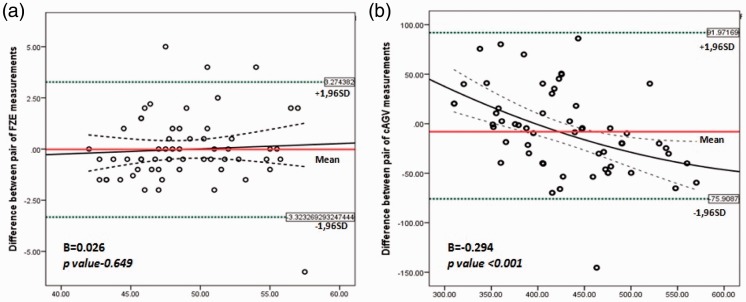
Bland–Altman plots for pairs of the FZE (Figure 5(a)) and cAGV (Figure 5(b)) measurements showed a statistically significant degree of concordance (B = 0.026) in FZE estimation, with regression line-of-fit approaching the mean and zero value. There was no significant proportional bias in FZE measurements of both the adrenal glands (p = 0.649) and the difference between measurements remained stable as the average increased, within 95% confidence interval. This agreement was not seen in cAGV measurements of both adrenals, where a significant proportional bias was found (p < 0.001) with regression line-of-fit deviating from the mean and zero values (B = −0.294).
Figure 5.
Bland–Altman plots with quadratic regression line of fit (curved dotted line), demonstrating degree of agreement between pairs of FZE (a) and cAGV (b) measurements of both adrenal glands, by the same observer. Mean difference (red line) and ±1.96SD agreement limits (95% confidence interval, dotted green lines) are shown. B = unstandardized coefficient.
Discussion
This study highlights that fetal adrenal gland biometry and elastography of the antenatal cervix are beneficial in prediction of preterm birth. The correlation between SWS of the cervix, trans-abdominal (TA) cervical length, and fetal adrenal enlargement is also demonstrated with the relative difference in their levels of accuracy. Quantitative assessment of the at-risk population is useful to implement therapeutic measures thus reducing the prematurity related complications. Our study also showed that FZE of both the adrenal glands are in agreement with each other and hence, eliminates the ambiguity in adrenal gland selection.
About 85% of preterm deliveries occur spontaneously and the rest of them are elective.1,11 The impact of prematurity extends beyond the individual and family due to the immediate consequences like neonatal respiratory distress, sepsis as well as the long term effects of cerebral palsy and chronic lung infection. There is a 40-fold increased risk of neonatal demise in preterm births as compared to the term-born neonates;12 hence, the risk assessment of prematurity is a prime importance to reduce the infant mortality and related morbidities. Various clinical, biochemical, and sonographic methods are employed in routine clinical practice, which includes modified Bishop’s score, sonographic cervical length measurement and fetal fibronectin test. Other chemical markers previously studied in this context were maternal plasma corticotrophin-releasing hormone (CRH) and cortisol levels.13 Each of these markers has their own shortcomings related to the degree of accuracy, availability, cost effectiveness, and subjectivity in their assessment.
Cervical length assessment is an integral part of comprehensive obstetric ultrasound examination. Based on a multi-center study by Iams et al.,14 the “short cervix” is defined as less than 25 mm or less than 10th centile length at 24–28 weeks of gestation. A recent study has also emphasized the fact that a 25 mm cut-off should be used only for cases not experiencing threatened preterm labor.15 However, all the studies were done at or before 28 weeks of gestation and employed trans-vaginal approach. Several other reports also demonstrated the gradual shortening of the cervix beyond 30 weeks of the gestation and hence, it has no predictive value for any definition of preterm birth. The controversy stays due to the fact that 50% of patients with a cervical length <25 mm may deliver at term.14 In our study, the mean value of the cervical length was approx. 20 mm in both the groups with insignificant p-value of 0.29. Therefore, the concept of “short and shortening” cervix may be a more effective tool in PTB prediction, but it requires serial cervical assessment.16 The measurements of cervical length obtained in this study are not scientifically valid because of TA acquisition technique.
Parturition and labor onset is a complex biological cascade, which is a hormone-based loop. The origin of this pathway resides with activation of fetal hypothalamus and pituitary glands in response to fetal stress. This further activates the fetal adrenal gland where the central zone of the gland responds by the release of glucocorticoids, predominantly DHEA-S. Interplay of fetal adrenal gland and placenta upregulates placental CRH, which further causes the release of prostaglandins like PGE2 and PGF2α and leads to onset of labor.5,17 Premature activation of placental CRH, acts as a biological clock in early onset of labor and delivery.18,19 Thus, the activation of the placenta via fetal steroid precursors can be correlated with enlargement of the fetal adrenal gland, which had also been proved by a previous autopsy study indicating higher gland weight in neonates delivered preterm.20
A few previous studies were done on fetal adrenal gland volume where the measurements were done using 3D-volumetric methods. Turan et al showed that adrenal gland volume was significantly higher in fetus born preterm. The first study21 revealed that cAGV of more than 422 mm3/kg is 92% sensitive and 99% specific for delivery within 5 days and in a later study,10 they proposed the cut-off value of 420 mm3/kg with 81% sensitivity and 87% specificity. A study contradicted these results by showing statistically significant (p = 0.006) smaller adrenal glands in the spontaneous preterm births.22 We also found that cAGV was higher in preterm deliveries with 67% sensitivity and 76% specificity at cut-off value of 415 mm3/kg (p < 0.001). The assessment of the fetal adrenal central zone was also done in one of these studies,21 where the fetal zone enlargement (d/D or FZE) of more than 49.7% was found to be 100% sensitive. Our study also found enlargement of the fetal zone of the adrenal gland with 90% sensitivity and 80% specificity at cut off value of 47.7%. The study by Hoffman et al.,23 however, did not find any of the fetal adrenal measures predictive of PTB. The area under the curve for d/D ratio was found to be 0.52 while it was 0.887 in the present study. These contradictory findings are attributed to the fact that none of their participants delivered within 2 weeks of ultrasound assessment and the mean time interval between the ultrasound and delivery was 55.3 days ranging from 18 to 93 days. Thus, it supports the fact that the fetal adrenal gland undergoes enlargement during a short interval of time ranging from 7 to 14 days and is highly predictive during this phase. This concept is reinforced by the endocrine research, which showed that maternal plasma CRH and cortisol levels are significantly higher in females giving birth within 24 hours, during 28 to 36 weeks of gestation.11 A recent study compared cAGV and FZE with cervical length and fetal fibronectin and found the highest sensitivity of cAGV and FZE to predict PTB within 7 days.24 Guler et al.5 also found statistically significant higher FZE values in preterm labor cases with mean value of 55.4% while our data revealed the mean value of 51.4%.
Dynamic shear-wave elastography of the antenatal cervix is a novel tool, which has been employed scarcely in the previous studies.25–27 In an earlier study,27 the shear wave velocity (SWV or SWS) was found to be less in preterm cases than in the term with higher sensitivity and specificity (93% and 90% respectively) at the cut-off of 2.83 m/s. In this study, the mean SWS was 2.27 m/s and 3.45 m/s in the preterm and term groups, respectively with p < 0.001. Cut-off value was found to be similar i.e. 2.87 m/s with sensitivity of 96.5% and specificity of 87%. The concept has been proved previously by an ex vivo study using histopathological uterine cervix samples.6 Elastographic assessment of antenatal cervix was found to be the best predictor in comparison with fetal adrenal gland biometry and cervical length measurement. Other researchers have done static elastography and strain ratio measurements28–31 on the antenatal cervix, which were out of scope of this study. Elastographic index grading was also not included in this study.
Strengths of the study include the comparison of fetal adrenal gland biometry with cervical elastography. Previous studies have evaluated the role of all these parameters in isolation or with cervical length. Further, the primary variables under study (fetal adrenal gland measures (FZE and cAGV) and elastography of antenatal cervix (SWS)) were assessed independently by two radiologists to assess the reliability and reproducibility. Both adrenal glands had never been compared previously for the significance of any proportional bias in their measurements. The main limitation of the study is small sample size and single-center approach. Another limitation is the use of trans-abdominal probe for cervical assessment, which is indirectly advantageous over the more invasive trans-vaginal procedure. NICE guidelines on preterm labor and birth4 recommend transvaginal (TVS) cervical length measurement as a diagnostic test. Hence, the TA measurements of cervical length in this study cannot be standardized and compared to other markers. The adrenal gland was measured by 2D technique rather than 3D, which may have given a more accurate value; however, the application of 3D-ultrasound is technically challenging in adrenal gland assessment. Cervico-vaginal fetal fibronectin is also considered as an alternate test but only secondary to TVS. Fibronectin level >50 ng/mL is considered positive; however, it was not employed in our study due to its lesser sensitivity, higher cost, and lack of easy availability.4
The measurement of elastography and fetal adrenal gland biometry are not standardized procedures and there is an absence of gestational age related nomograms for these two variables. The studies are needed with large sample sizes and a multi-center approach to predict the normal values of the fetal adrenal gland parameters and elastographic characteristics of the cervix. The new, low cost, noninvasive, and sensitive markers for preterm labor assessment are also required to be sought and evaluated.
In conclusion, shear wave elastography of the antenatal cervix and fetal adrenal zone enlargement are potential new markers for prediction of preterm delivery, which can aid in identifying the at-risk population and reduce the prematurity-related complications.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval
Ethical approval was obtained from the Ethical Committee of Teerthanker Mahaveer Medical College and Research Centre.
Guarantor
AA
Contributors
SA, AA and PJ researched literature and conceived the study. AA, PJ and SS designed the audit. AA, SC and SS were involved in protocol development. SA & AA helped in patient recruitment and data analysis. SA wrote the first draft of the manuscript. SA and AA wrote the final version of the manuscript. All authors reviewed and approved the final version of the manuscript.
References
- 1.Beck S, Wojdyla D, Say L, et al. The worldwide incidence of preterm birth: A systematic review of maternal mortality and morbidity. Bull World Health Organ 2010; 88: 31–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Svigos JM, Dodd JM and Robinson JS. Threatened and actual preterm labor including mode of delivery. In: High risk pregnancy management options. 4th ed. New York: Elsevier Inc., 2012, pp. 1075–1090.
- 3.The Lancet. The unfinished agenda of preterm births . Lancet 2016; 388: 2323–2323. [DOI] [PubMed] [Google Scholar]
- 4.National Institute for Health and Care Excellence. Preterm labour and birth. NICE guideline (NG25), 2005. [PubMed]
- 5.Guler AE, Pehlivan H, Cakmak B, et al. Assessment of fetal adrenal gland enlargement in term and preterm labor cases. Int J Res Med Sci 2015; 3: 1035–1040. [Google Scholar]
- 6.Agarwal A, Agarwal S. Role of imaging and its advances in prediction of preterm birth. Int J Radiol Rad Ther 2017; 2: 1–5. [Google Scholar]
- 7.Carlson LC, Feltovich H, Palmeri ML, et al. Estimation of shear wave speed in the human uterine cervix. Ultrasound Obstet Gynecol 2014; 43: 452–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Swiatkowska-Freund M, Traczyk-Los A, Preis K, et al. Prognostic value of elastography in predicting premature delivery. Ginekol Pol 2014; 85: 204–207. [DOI] [PubMed] [Google Scholar]
- 9.Arias F, Daftary SN and Bhide AG. Preterm labor. In: Practical guide to high-risk pregnancy and delivery. 3rd ed. India: Elsevier, 2011, pp. 217–239.
- 10.Turan OM, Turan S, Funai EF, et al. Ultrasound measurement of fetal adrenal gland enlargement: An accurate predictor of preterm birth. Am J Obstet Gynecol 2011; 204: 311–311. [DOI] [PubMed] [Google Scholar]
- 11.Romero R, Espinoza J, Goncalves LF, et al. The role of inflammation and infection in preterm birth. Semin Reprod Med 2007; 25: 21–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Spong CY. Prediction and prevention of recurrent spontaneous preterm birth. Obstet Gynecol 2007; 110: 405–415. [DOI] [PubMed] [Google Scholar]
- 13.Korebrits C, Ramirez MM, Watson L, et al. Maternal corticotropin-releasing hormone is increased with impending preterm birth. J Clin Endocrinol Metab 1998; 83: 1585–1591. [DOI] [PubMed] [Google Scholar]
- 14.Iams JD, Goldenberg RL, Meis PJ, et al. The length of the cervix and the risk of spontaneous premature delivery. National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network. N Engl J Med 1996; 29: 567–572. [DOI] [PubMed] [Google Scholar]
- 15.Berghella V, Palacio M, Ness A, et al. Cervical length screening for prevention of preterm birth in singleton pregnancy with threatened preterm labor: Systematic review and meta-analysis of randomized controlled trials using individual patient-level data. Ultrasound Obstet Gynecol 2017; 49: 322–329. [DOI] [PubMed] [Google Scholar]
- 16.Whittle WL, Fong KW and Windrim R. Cervical ultrasound and preterm birth. In: Diagnostic ultrasound. 4th ed. Philadelphia: Elsevier Mosby, 2011, pp. 1528–1530.
- 17.Lindsay JR, Nieman LK. The hypothalamic-pituitary-adrenal axis in pregnancy: Challenges in disease detection and treatment. Endocr Rev 2005; 26: 775–799. [DOI] [PubMed] [Google Scholar]
- 18.Wadhwa PD, Porto M, Garite TJ, et al. Maternal corticotropin-releasing hormone levels in the early third trimester predict length of gestation in human pregnancy. Am J Obstet Gynecol 1998; 179: 1079–1085. [DOI] [PubMed] [Google Scholar]
- 19.Ochedalski T, Zylińska K, Laudański T, et al. Corticotrophin-releasing hormone and ACTH levels in maternal and fetal blood during spontaneous and oxytocin-induced labour. Eur J Endocrinol 2001; 144: 117–121. [DOI] [PubMed] [Google Scholar]
- 20.Anderson AB, Laurence KM, Davies K, et al. Fetal adrenal weight and the cause of premature delivery in human pregnancy. J Obstet Gynaecol Br Commonw 1971; 78: 481–488. [DOI] [PubMed] [Google Scholar]
- 21.Turan OM, Turan S, Funai EF, et al. Fetal adrenal gland volume: A novel method to identify women at risk for impending preterm birth. Obstet Gynecol 2007; 109: 855–862. [DOI] [PubMed] [Google Scholar]
- 22.Hoffman SY, Lee L, Thomas AM, et al. Fetal adrenal gland volume and preterm birth: A prospective third-trimester screening evaluation. J Matern Fetal Neonatal Med 2016; 29: 1552–1555. [DOI] [PubMed] [Google Scholar]
- 23.Hoffman MK, Turan OM, Parker CB, et al. Ultrasound measurement of the fetal adrenal gland as a predictor of spontaneous preterm birth. Obstet Gynecol 2016; 127: 726–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ibrahim MI, Sherif A, El-Kady M, et al. Can three-dimensional ultrasound measurement of fetal adrenal gland enlargement predict preterm birth? Arch Gynecol Obstet 2015; 292: 569–578. [DOI] [PubMed] [Google Scholar]
- 25.Muller M, Aït-Belkacem D, Hessabi M, et al. Assessment of the cervix in pregnant women using shear wave elastography: A feasibility study. Ultrasound Med Biol 2015; 41: 2789–2797. [DOI] [PubMed] [Google Scholar]
- 26.Hernandez-Andrade E, Aurioles-Garibay A, Garcia M, et al. Effect of depth on shear-wave elastography estimated in the internal and external cervical os during pregnancy. J Perinat Med 2014; 42: 549–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Agarwal A, Agarwal S and Chandak S. Role of acoustic radiation force impulse and shear wave velocity in prediction of preterm birth: A prospective study. Acta Radiol. Epub ahead of print 7 September 2017. DOI: 10.1177/0284185117730689. [DOI] [PubMed]
- 28.Swiatkowska-Freund M, Pankrac Z, Preis K. Intra and inter-observer variability of evaluation of uterine cervix elastography images during pregnancy. Ginekol Pol 2014; 85: 360–364. [DOI] [PubMed] [Google Scholar]
- 29.Molina FS, Gómez LF, Florido J, et al. Quantification of cervical elastography: A reproducibility study. Ultrasound Obstet Gynecol 2012; 39: 685–689. [DOI] [PubMed] [Google Scholar]
- 30.Hernandez-Andrade E, Hassan SS, Ahn H, et al. Evaluation of cervical stiffness during pregnancy using semiquantitative ultrasound elastography. Ultrasound Obstet Gynecol 2013; 41: 152–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fruscalzo A, Londero AP, Schmitz R. Quantitative cervical elastography during pregnancy: Influence of setting features on strain calculation. J Med Ultrason 2015; 42: 387–394. [DOI] [PubMed] [Google Scholar]