Abstract
Background
Central venous catheters are inserted ubiquitously in critical care and have roles in drug administration, fluid management and renal replacement therapy. They are also associated with numerous complications. The true number of central venous catheters inserted per year and the proportion of them associated with complications are unknown in the UK.
Methods
We performed a prospective audit at five hospitals, as a feasibility pilot for a larger, nationwide audit. Using a novel secure online data collection platform, developed earlier and adapted for this project, all central venous catheters inserted for patients admitted to the Intensive Care Units were documented at five pilot sites across the UK.
Results
A total of 117 data collection forms were submitted. Users found the electronic data collection system easy to use. All data fields were ready for analysis immediately after data input. Out of the 117 central venous catheters, 17 were haemodialysis catheters and five pulmonary artery introducers. Experienced practitioners (at least three years’ experience) inserted 85% of the central venous catheters. The site of insertion was the internal jugular vein for 80%, femoral for 12% and subclavian for 8% of central venous catheters. Most central venous catheters were inserted in ICU (49%) or theatres (42%). Ultrasound was used for 109 (93%) of central venous catheter insertions and its use was not associated with fewer complications. In 15 cases venopuncture was attempted more than once (all with ultrasound) and this was associated with significantly increased risk of complications. There were eight immediate complications (6.8%): five related to venopuncture and inability to pass a guidewire, two carotid artery punctures and one associated with significant arrhythmia.
Conclusion
This study demonstrates the ease and feasibility of collecting detailed descriptive data on central line insertion and its immediate complications in the UK over two weeks. In our proposed nationwide audit, organisation-level data on local policies and standard operating procedures is required to complete the picture on this important aspect of intensive care practice.
Keywords: Central venous catheter, vascular access, audit, complications, quality improvement
Introduction
Central venous catheters (CVCs) are associated with numerous complications, both immediate (during insertion) and late. Data from the USA suggest that up to 15% of line insertions are associated with complications.1
It has been estimated that up to 200,000 CVCs are inserted in the UK annually; however, these data are almost 25 years old.2,3 There has been a significant change in the need for and provision of CVC insertion. There have also been changes in technique, with ultrasound guidance rising to prominence after several studies demonstrated its superiority over the landmark technique backing the recommendation by the National Institute for Health and Care Excellence in 2002.4 Ultrasound guidance is now being advocated by professional bodies such as the Association of Anaesthetists of Great Britain and Ireland (AAGBI) safe vascular access group and the Swedish Society of Anaesthesiology and Intensive Care Medicine amongst others.5–7
A National Audit of CVC insertion rates and their complications had previously been proposed to the Royal College of Anaesthesia National Audit Project team but had been overlooked in favour of other projects. Following the success of a local audit in the Wessex region, we designed our study to assess the feasibility of a two-week national audit of CVC insertion and complications.8
Methods
The audit was carried out prospectively at five hospitals in the UK:
John Radcliffe Hospital, Oxford (Teaching hospital with 16 critical care beds, with 43% surgical and 57% medical admissions)
Churchill Hospital, Oxford (Teaching hospital with eight critical care beds, with 72% surgical and 28% medical admissions)
Heartlands Hospital, Birmingham (Teaching hospital with 11 level 3 and eight level 2 beds, with 51% surgical and 49% medical admissions)
Good Hope Hospital, Sutton Coldfield (DGH with nine critical care beds, with 36% surgical and 64% medical admissions)
Royal Gwent Hospital, Newport (large DGH with 16 critical care beds, with 46% surgical and 54% medical admissions)
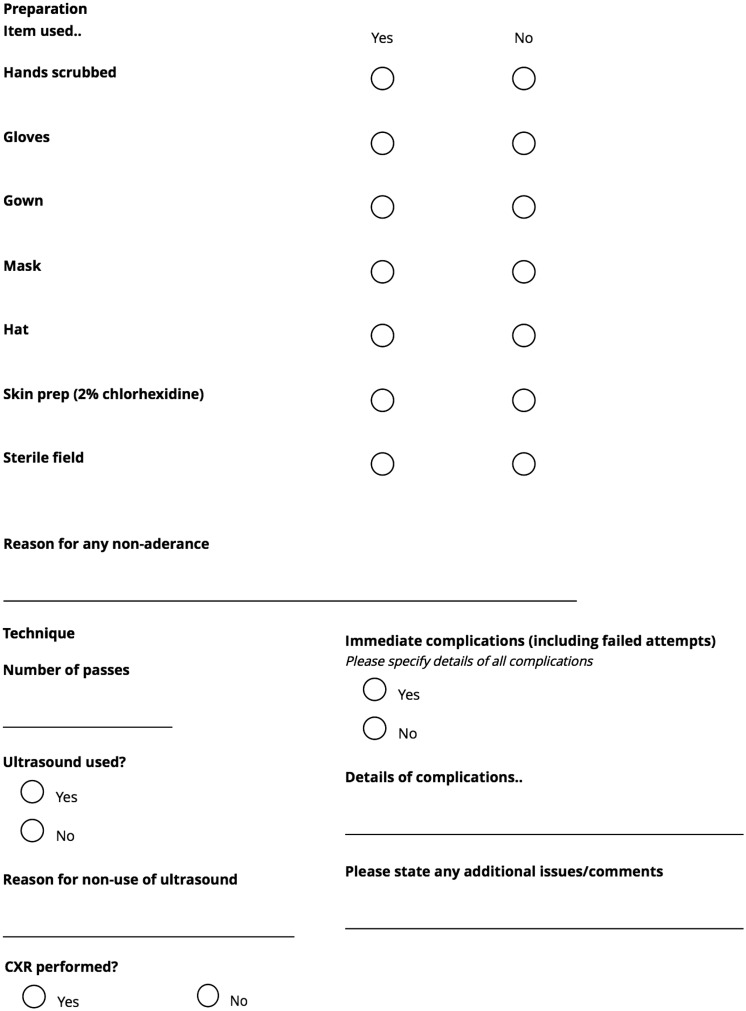
Each hospital chose a two-week period in May 2016 to collect data on every newly inserted CVC for adult patients admitted to, or currently on the intensive care units. For the purpose of this audit, CVCs, haemodialysis catheters and pulmonary artery (PA) catheter introducers were included in the data collection. Tunnelled central access catheters and peripherally inserted central catheters were excluded from the data collection. Data were collected for each new CVC inserted into a patient admitted to the critical care units. Location of procedure (such as operating theatre, ED, ICU) and the anatomical site of catheter insertion were additional data points (Figure 1). The anonymised information was collected on a secure digital data collection platform, which had been previously developed for a large national point-prevalence study and described in detail.9,10 In order to allow follow-up of potential incidents, patient identifiable data were kept in a secure location at each site. Immediate complications were defined according to the Safe Vascular Access guideline of the AAGBI.5
Figure 1.
The ICNAP-1 dataset. ICNAP-1: The Intensive Care National Audit Project-1.
Data were analysed using SPSS 20.0. Frequencies are described as percentages. Chi-square test was used to determine whether there was a significant difference between the expected frequencies and the observed frequencies in one or more categories.
Results
One hundred and seventeen forms were submitted to the online data platform for 117 procedures. All data were included in the final analysis.
Most of the inserted CVCs were multi-lumen central lines (n = 95, 81%). Seventeen (15%) haemodialysis catheters for renal replacement therapy and five (4%) PA catheter introducers were also inserted (Figure 2). The majority of lines (99 out of 107, 85%) were inserted by an experienced practitioner of at least three years’ practice (Figure 3). The internal jugular vein was the most commonly accessed site, with 94 catheters (80% of lines) being placed there (Figure 4). The most common indication for CVC insertion was administration of vasopressors (Figure 5).
Figure 2.

Types of lines inserted. CVC: central venous catheter; PA: pulmonary artery.
Figure 3.

Seniority of operator inserting lines. CT2: Core Trainee Year 2; NCCG: Non-Consultant Career Grade Doctor; ST3: Specialty Trainee Year 3.
Figure 4.

Site of insertion of lines.
Figure 5.
Indications for lines. RRT: renal replacement therapy; TPN: total parenteral nutrition. (More than one response was allowed, hence numbers may add up to more than the number of lines inserted.)
The majority of lines were inserted in ICU (n = 57, 49%) or operating theatres (n = 49, 42%), with other areas including ED accounting for 11 lines (9%).
Ultrasound was used for 109 (93%) of lines.
There were eight immediate complications, yielding a complication rate of 6.8%. A full breakdown is shown below (Table 1).
Table 1.
Immediate complications of central line insertion.
| Complication | Number |
|---|---|
| Venous puncture/tear (due to inability to pass the guidewire) | 5 |
| Carotid artery puncture | 2 |
| Significant arrhythmia | 1 |
There was no statistical difference between the complication rate of ultrasound guided and non-ultrasound guided line insertions (seven in 109 (7.3%) for US guided and one in eight (12.5%) for non-US guided insertions; p = 0.597). Multiple insertion attempts were associated with higher complication rates (p < 0.001 Chi-square test).
Discussion
The main finding of our feasibility study is that immediate complications of central line insertions are more common than previously reported: 8/117 (6.8%). We also confirmed the ability of our data collection methods to be rapidly accessible on multiple devices and scalable for a national audit.
Our results of the somewhat unexpectedly high complication rates highlight the need for a large-scale national audit, with agreed methodology and definitions for complications, to understand the true burden of CVC-related complications in the critically ill.3 Interestingly, a recent study performed in another region of the UK with similar methodology demonstrated different results.11 Out of 487 CVC insertions, which included 57 tunnelled lines the ‘serious complication rate’ was 3%.11 Lathey and colleagues used a restricted list of serious complications as outcome measures, whilst our study benefited from using the complications described in the AAGBI guideline published just before the trial period.5 It is also important to note that although the percentage of complications were more than double in our series, the relative risk of complications did not differ significantly when compared to those observed in the Lathey study (RR: 2.22 95%CI 0.96-5.11, p = 0.061).
The majority of lines were inserted into the right internal jugular vein, using ultrasound guidance. This would reflect current evidence, suggesting that the right internal jugular site is associated with the lowest risk of mechanical complications, and that ultrasound is associated with a reduction in complication rates over the landmark technique.4,12 Despite this, the rate of mechanical complications in our data series is higher than we would have expected with those strategies, at 6.8%.4 The reasons for this are unclear; it is possible that operators were not experienced with ultrasound or used improper technique, such as not fully visualising the needle during access, and not fully visualising the guidewire.7,13 This is at odds with the reported seniority of the operators, however could further highlight the ongoing educational need for all staff groups and not just residents.14–16 It may be that real time ultrasound fills practitioners with a false sense of security, making them slightly more “cavalier” during the procedure.17
In our study, the 117 central lines were inserted in five hospitals with 68 critical care beds in total during the two-week period. If this data is extrapolated to all the intensive care units in the UK over 52 weeks, it would suggest that slightly more than 120,000 CVCs are being placed annually in the UK’s critical care patient population - a significant difference from the previous estimate.2,3 It has been demonstrated, that CVC use did not change significantly over the last decade in the US, despite increased awareness about the risks of the procedure.18 In fact, in 168 US hospitals CVC use increased from 33.4% to 43.8% over an 8 years period, with significant variability between hospitals with “high-intensity” and “low-intensity” catheter use. Meanwhile, PA catheter use steadily declined in this cohort and similar findings were reported from other datasets.18,19 A contemporary snapshot of the UK practice found slightly higher insertion rates of CVCs: 430 catheters in 15 centres over a two-week period in 2015.11 Although there is no information about the size and profile of the participating hospitals in the Lathey study, it is plausible that similar differences of practice exist in the UK as was found in the US.11,18
In our hospitals, very few CVCs are inserted in critically ill patients outside the ICU or theatres. As the number of CVC insertions in the UK concentrated in the hands of anaesthesia and critical care practitioners, it is possible that they like to perform the procedure in a familiar and controlled environment.3,5 However, this practice may be associated with delays in potentially disease-altering therapy (inotropic infusions for instance). A recent large study in the US found that similarly to our cohort, CVCs are commonly placed in surgical patients before ICU admission, while medical patients have their catheters inserted either in ED or on the units.18 Lathey et al.11 found almost identical distribution of insertion sites, confirming that in the UK about half of the CVCs used on the ICUs are placed outside of the walls of critical care units.
Our pilot study has many strengths. The data were collected over multiple sites in different regions, yet data collection was smooth. The secure online platform was easy to use and yielded instantaneous results and could be queried at any time. It demonstrated the ease with which a national audit of CVCs could be performed using this platform.9
Our audit has a number of limitations. First, data were not collected in real time as the lines were being inserted; this potentially led to some CVC insertions being missed. Also, this meant that the descriptions of the procedure were inferred from the notes rather than observed in real time, allowing for recall bias, since most clinicians fill in the line insertion procedure in retrospect. Only immediate complications were assessed, and those complications rely on accurate identification by clinicians. We also excluded PICC lines and tunnelled lines, as very few were inserted on our units. We focused our efforts on determining immediate complications and might have missed important other complications, such as CVC-related infections or thrombotic events.
Future directions for this study would involve running it nationwide, collecting data from all intensive care units in the UK, sharing the learning and combining resources with similarly minded groups across the UK. A phase one approach to collect data on standard unit policies regarding what training and level of supervision is provided before an operator is allowed to insert a CVC and a survey of healthcare providers’ perception of adequacy of training and availability of supervision would need to be considered. The data could be used as a benchmarking tool, allowing intensive care units to modify their local practice towards a national standard of central line insertion. A second phase of the study would involve assessing immediate and delayed complication rates, such as complications described here and also line infections and thrombosis. These data are yet to be obtained on a large intensive care population in the UK. A national registry of CVC insertion could be easily developed using the methods described in this paper; this could potentially contribute to improved CVC safety in every ICU in the UK.
Conclusion
In this pilot study across five UK Intensive Care Units, we have demonstrated the feasibility of collecting data on central line insertion in critically ill patients over a two-week period. One hundred and seventeen lines were inserted, with an immediate complication rate of 6.8%. These data will be used to perform a larger study across the entire UK ICU community.
Acknowledgements
We would like to thank J Hull, K Archer and T Oyede, Heart of England NHS Foundation Trust, Birmingham, for their help with data collection.
Declaration of conflicting interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: OO: On editorial board of JICS, hosts JICS podcast. The rest of the authors declare no potential conflicts of interest.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.McGee DC, Gould MK. Preventing complications of central venous catheterization. N Engl J Med 2003; 348: 1123–1133. [DOI] [PubMed] [Google Scholar]
- 2.Waghorn DJ. Intravascular device-associated systemic infections: a 2 year analysis of cases in a district general hospital. J Hosp Infect 1994; 28: 91–101. [DOI] [PubMed] [Google Scholar]
- 3.Smith RN, Nolan JP. Central venous catheters. BMJ 2013; 347: f6570. [DOI] [PubMed] [Google Scholar]
- 4.Brass P, Hellmich M, Kolodziej L, et al. Ultrasound guidance versus anatomical landmarks for internal jugular vein catheterization. Cochrane Database of Systematic Reviews 2015; 1: CD006962. [DOI] [PMC free article] [PubMed]
- 5.Bodenham Chair A, Babu S, Bennett J, et al. Association of Anaesthetists of Great Britain and Ireland: Safe vascular access 2016. Anaesthesia 2016; 71: 573–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Frykholm P, Pikwer A, Hammarskjöld F, et al. Clinical guidelines on central venous catheterisation. Swedish Society of Anaesthesiology and Intensive Care Medicine. Acta Anaesthesiol Scand 2014; 58: 508–524. [DOI] [PubMed] [Google Scholar]
- 7.Lamperti M, Bodenham AR, Pittiruti M, et al. International evidence-based recommendations on ultrasound-guided vascular access. Intensive Care Med 2012; 38: 1105–1117. [DOI] [PubMed] [Google Scholar]
- 8.Wong A, Masterson G. Improving quality in intensive care unit practice through clinical audit. J Intensive Care Soc 2015; 16: 5–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sharif B, Lundin RM, Morgan P, et al. Developing a digital data collection platform to measure the prevalence of sepsis in Wales. J Am Med Inform Assoc 2016; 23: 1185–1189. [DOI] [PubMed] [Google Scholar]
- 10.Szakmany T, Lundin RM, Sharif B, et al. Sepsis prevalence and outcome on the general wards and emergency departments in Wales: results of a multi-centre, observational, point prevalence study. PLoS One 2016; 11: e0167230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lathey RK, Jackson RE, Bodenham A, et al. A multicentre snapshot study of the incidence of serious procedural complications secondary to central venous catheterisation. Anaesthesia 2017; 72: 328–334. [DOI] [PubMed] [Google Scholar]
- 12.Parienti J-J, Mongardon N, Mégarbane B, et al. Intravascular complications of central venous catheterization by insertion site. N Engl J Med 2015; 373: 1220–1229. [DOI] [PubMed] [Google Scholar]
- 13.Kornbau C, Lee KC, Hughes GD, et al. Central line complications. Int J Crit Illn Inj Sci 2015; 5: 170–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peltan ID, Shiga T, Gordon JA, et al. Simulation improves procedural protocol adherence during central venous catheter placement: a randomized controlled trial. Simul Healthc 2015; 10: 270–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maizel J, Bastide M-A, Richecoeur J, et al. Practice of ultrasound-guided central venous catheter technique by the French intensivists: a survey from the BoReal study group. Ann Intensive Care 2016; 6: 76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Werner HC, Vieira RL, Rempell RG, et al. An educational intervention to improve ultrasound competency in ultrasound-guided central venous access. Pediatr Emerg Care 2016; 32: 1–5. [DOI] [PubMed] [Google Scholar]
- 17.Reusz G, Csomos A. The role of ultrasound guidance for vascular access. Curr Opin Anaesthesiol 2015; 28: 710–716. [DOI] [PubMed] [Google Scholar]
- 18.Gershengorn HB, Garland A, Kramer A, et al. Variation of arterial and central venous catheter use in United States intensive care units. Anesthesiology 2014; 120: 650–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Koo KKY, Sun JCJ, Zhou Q, et al. Pulmonary artery catheters: evolving rates and reasons for use. Crit Care Med 2011; 39: 1613–1618. [DOI] [PubMed] [Google Scholar]